Abstract
Background and objectives
With global efforts to develop and deliver a COVID-19 vaccine rapidly, vaccine hesitancy stands as a barrier to these efforts. We aimed to estimate the proportion of Syrian adult population intending to be vaccinated against COVID-19 and, principally, to assess the demographic and attitudinal factors associated with it in order to approach suitable solutions.
Methods
An anonymous online questionnaire was conducted between 23rd December 2020 and 5th January 2021 in various provinces in Syria. A total of 3402 adults were sampled to reflect the population demographic factors. Attitudinal factors included Covid-19 fears, risks, and beliefs on the origin. Vaccination hesitancy and knowledge were also measured. The intention to get vaccinated against COVID-19 was the primary endpoint.
Results
According to their statements, 1222 participants (35.92%) will consent to get vaccinated against COVID-19. Our findings indicate that male gender, younger age, rural residence, not having children, smoking, fear about COVID-19, individual perceived severity, believing in the natural origin of the coronavirus, and high vaccination knowledge were positive predictors of embracing COVID-19 vaccine when it is available.
Conclusion
COVID-19 vaccine acceptance rate is considerably poor across Syrian population compared to populations in developed countries. Vaccine hesitancy is closely bound to the fear of side effects and doubts about vaccine efficacy. Factors such as conspiracy beliefs and myths about the vaccine lower vaccine uptake. Thus, interventional educational campaigns are increasingly required to overcome misinformation and avert low vaccination acceptance rates.
Keywords: COVID-19, Vaccine hesitancy, Syria, Pandemic
Introduction
The outbreaks in human history are old and tragic. Diseases such as polio, smallpox, and rabies were once significant threats to our existence, but the discovery of vaccines was a breakthrough by reducing the incidence rates of such diseases [1]. According to the World Health Organization (WHO), vaccination averts 2–3 million deaths a year [2]. Moreover, since 1990, there has been a 61% decline in mortality rate among children between five and nine years old due to a decline in infectious diseases [3].
Till 14th February 2021 around 107 million cases of coronavirus disease 2019 (COVID-19) and 2 million deaths have been reported worldwide [4]. This newly emerging pandemic overwhelmed medical facilities and overloaded the burden on healthcare systems. The situation is more strenuous in war-torn Syria, where the preexisting burden on the declining healthcare system surged due to the outbreak of COVID-19. The pandemic impact was prominent in terms of overloaded hospitals, insufficient resources, and poor surveillance systems [5, 6].
To lessen the COVID-19 burden on population health concerning both death rates and exhausting healthcare systems, an effective vaccine must be developed and distributed soon. Recently, multiple vaccines have been industrialized and approved for emergency use in a relatively short time compared to other vaccines developed in the past. Namely, Oxford-AstraZeneca, Pfizer-BioNTech, and Moderna COVID-19 vaccines [7, 8]. Besides vaccine availability, effectiveness, and safety, it is important that the vaccine is tolerable by the targeted population [9].
Vaccine hesitancy raises challenges to public health agencies in order to achieve a sufficient degree of immunization necessary to protect vulnerable individuals [9]. The WHO defines vaccine hesitancy as the rejection or delay in vaccine uptake in the presence of an existing vaccine [2]. An example of such a challenge in public health is the report published by the Centre for Disease Control and Prevention in the United States that assessed the prevalence of seasonal influenza vaccine hesitancy in up to 50% of the study population [10].
This study aims to (i) estimate the intention to get vaccinated against COVID-19 among the adult Syrian population, (ii) determine demographic and attitudinal factors associated with participants intentions, and (iii) measure the population’s general knowledge about vaccinations.
Methods
Sample and procedure
A cross-sectional study collected data through an anonymous online questionnaire from Social Media networks, including Facebook, Twitter, and Telegram, covering the period between 23rd December 2020 and 5th January 2021 among the adult general population, while covering various provinces in Syria. We developed a standardized questionnaire based on a literature review [11–15].
Questionnaire
All questions were administered in Arabic language as Arabic is the native language of the Syrian population.
Demographic questionnaire
The demographic questionnaire collected data on age, gender, geographic location, region of residence (urban or rural), educational degree, employment status before and during COVID-19 pandemic, working in the healthcare sector, marital status, parenthood status, smoking status, and if the participant had chronic medical conditions.
Coronavirus questionnaire
This section addressed: (1) Fears about COVID-19, (2) Perceived risk of contracting COVID-19, (3) Perceived severity of COVID-19 on your life, (4) Previous COVID-19 infection, (5) Beliefs on coronavirus origin, and (6) Intention to get vaccinated when COVID-19 vaccine is available in Syria on a 5-level Likert scale: 1 (strongly disagree), 2 (disagree), 3 (undecided), 4 (agree), or 5 (strongly agree). Responders declining the COVID-19 vaccine option or undecided yet were automatically directed to a specific question addressing reasons for refusing the vaccine. Participants could choose one or more of the following statements: “Fear of side effects”, “Doubts about the efficiency of the vaccine”, “The vaccine is not important”, “This is not the right time”, “I just refuse the vaccine”, and “other reasons”.
Vaccine hesitancy
Vaccine hesitancy was evaluated using three questions: “Have you ever refused a vaccine for yourself or a child because you considered it as useless or dangerous?” “Have you ever postponed a vaccine recommended by a physician because of doubts about it?” “Have you ever had a vaccine for a child or yourself despite doubts about its efficacy” [16]. If a participant answered yes to any of these proposals, he or she was considered to be “vaccine hesitant”.
Knowledge about vaccines
This section evaluated participants’ knowledge about vaccines with nine statements, each one providing 3 options: correct, incorrect, or do not know [17]. “Incorrect” or “do not know” options were scored as zero, and “correct” was scored as one. Therefore, higher scores indicated better knowledge of vaccines.
The last section of the questionnaire presented people with questions on how often they used the following sources for gaining information about vaccinations: healthcare providers (doctor, nurse, ...), the internet and media, and reliable sources (WHO website, medical journals, …). Possible answers ranged from never (1) to always (6).
Statistical analysis
Data were entered in Microsoft Excel software and the statistical analysis was carried out using SPSS version 25.0. Descriptive statistics of the raw data were presented as frequencies and percentages. We combined responses regarding COVID-19 vaccine acceptance into two categories: 1 (Agree), or 0 (Disagree), and ran multiple binomial logistic regression (multivariate analysis) to model demographic and attitudinal factors predictive of participants’ willingness to get vaccinated against COVID-19. We considered P value < 0.05 to be significant.
Results
There were a total of 3402 participants who completed the online questionnaire (Table 1). The response rate cannot be calculated as participants are recruited based on open invitations via social networks that do not provide information on people who viewed the online post.
Table 1.
Association between participants characteristics and their acceptance of COVID19 vaccine
| Variable | Category | Total N(%) | Do Not Agree N(%) | Agree N(%) | Chi-Square |
|---|---|---|---|---|---|
| Sex | Male | 1219 (35.83) | 656 (53.81) | 563 (46.19) | < 0.0001 |
| Female | 2183 (64.17) | 1524 (69.81) | 659 (30.19) | ||
| Age | > 30 | 1732 (50.91) | 1196 (69.05) | 536 (30.95) | < 0.0001 |
| 18–30 | 1670 (49.09) | 984 (58.92) | 686 (41.08) | ||
| Residency province | West | 1376 (40.45) | 880 (63.95) | 496 (36.05) | 0.299 |
| Northern-East | 265 (7.79) | 162 (61.13) | 103 (38.87) | ||
| Middle | 594 (17.46) | 369 (62.12) | 225 (37.88) | ||
| South | 1167 (34.3) | 769 (65.9) | 398 (34.1) | ||
| Region of residence | Rural | 973 (28.6) | 596 (61.25) | 377 (38.75) | 0.03 |
| Urban | 2429 (71.4) | 1584 (65.21) | 845 (34.79) | ||
| Marital status | Married | 1690 (49.68) | 1168 (69.11) | 522 (30.89) | < 0.0001 |
| Not married | 1712 (50.32) | 1012 (59.11) | 700 (40.89) | ||
| Having kids | Yes | 1535 (45.1) | 1068 (69.58) | 467 (30.42) | < 0.0001 |
| None | 1867 (54.9) | 1112 (59.56) | 755 (40.44) | ||
| Highest level of education | Post-graduate | 545 (16.02) | 346 (63.49) | 199 (36.51) | 0.184 |
| School | 492 (14.46) | 334 (67.89) | 158 (32.11) | ||
| High Education | 2272 (66.78) | 1436 (63.2) | 836 (36.8) | ||
| None | 93 (2.73) | 64 (68.82) | 29 (31.18) | ||
| Pre-coronavirus employment status | Employed | 1996 (58.67) | 1278 (64.03) | 718 (35.97) | 0.94 |
| Not employed | 1406 (41.33) | 902 (64.15) | 504 (35.85) | ||
| Employment change due to coronavirus | Newly employed | 114 (3.35) | 71 (62.28) | 43 (37.72) | 0.453 |
| Furlough | 148 (4.35) | 86 (58.11) | 62 (41.89) | ||
| Newly Unemployed | 187 (5.5) | 121 (64.71) | 66 (35.29) | ||
| None | 2953 (86.8) | 1902 (64.41) | 1051 (35.59) | ||
| Financial income | Salary + Other | 682 (20.05) | 439 (64.37) | 243 (35.63) | 0.108 |
| Freelancing | 398 (11.7) | 241 (60.55) | 157 (39.45) | ||
| Family | 1354 (39.8) | 853 (63) | 501 (37) | ||
| Salary only | 968 (28.45) | 647 (66.84) | 321 (33.16) | ||
| Healthcare worker | Student | 526 (15.46) | 282 (53.61) | 244 (46.39) | < 0.0001 |
| Yes | 449 (13.2) | 268 (59.69) | 181 (40.31) | ||
| No | 2427 (71.34) | 1630 (67.16) | 797 (32.84) | ||
| Smoking status | Yes | 1509 (44.36) | 930 (61.63) | 579 (38.37) | 0.008 |
| No | 1893 (55.64) | 1250 (66.03) | 643 (33.97) | ||
| Chronic medical conditions | Yes | 464 (13.64) | 283 (60.99) | 181 (39.01) | 0.136 |
| No | 2938 (86.36) | 1897 (64.57) | 1041 (35.43) | ||
| Fears about COVID-19 | Yes | 2229 (65.52) | 1341 (60.16) | 888 (39.84) | < 0.0001 |
| No | 1173 (34.48) | 839 (71.53) | 334 (28.47) | ||
| Perceived risk of contracting COVID-19 | Likely | 3243 (95.33) | 2068 (63.77) | 1175 (36.23) | 0.087 |
| Unlikely | 159 (4.67) | 112 (70.44) | 47 (29.56) | ||
| Perceived severity of effect of COVID-19 to one’s life | Serious | 1049 (30.83) | 626 (59.68) | 423 (40.32) | < 0.0001 |
| Not serious | 2353 (69.17) | 1554 (66.04) | 799 (33.96) | ||
| Had COVID-19? | Yes, a positive test | 170 (5) | 112 (65.88) | 58 (34.12) | 0.079 |
| No, a negative test | 1646 (48.38) | 1066 (64.76) | 580 (35.24) | ||
| May have had it but not been tested | 161 (4.73) | 88 (54.66) | 73 (45.34) | ||
| Not had it but not been tested | 1425 (41.89) | 914 (64.14) | 511 (35.86) | ||
| Beliefs on the origin of the virus | Artificial/ Do not know | 2711 (79.69) | 1902 (70.16) | 809 (29.84) | < 0.0001 |
| Natural | 691 (20.31) | 278 (40.23) | 413 (59.77) | ||
| General Vaccine Hesitancy | Not hesitant | 2545 (74.81) | 1622 (63.7) | 923 (36.3) | 0.467 |
| Hesitant | 857 (25.19) | 558 (65.1) | 299 (34.9) | ||
| Vaccination Knowledge | 0 | 126 (3.7) | 107 (84.92) | 19 (15.08) | < 0.0001 |
| 1 | 168 (4.94) | 136 (80.95) | 32 (19.05) | ||
| 2 | 371 (10.91) | 290 (78.17) | 81 (21.83) | ||
| 3 | 507 (14.9) | 364 (71.79) | 143 (28.21) | ||
| 4 | 489 (14.37) | 330 (67.48) | 159 (32.52) | ||
| 5 | 429 (12.61) | 272 (63.4) | 157 (36.6) | ||
| 6 | 436 (12.82) | 252 (57.8) | 184 (42.2) | ||
| 7 | 361 (10.61) | 187 (51.8) | 174 (48.2) | ||
| 8 | 280 (8.23) | 143 (51.07) | 137 (48.93) | ||
| 9 | 235 (6.91) | 99 (42.13) | 136 (57.87) | ||
| Healthcare provider | Never | 467 (13.73) | 319 (68.31) | 148 (31.69) | < 0.0001 |
| Occasionally | 197 (5.79) | 145 (73.6) | 52 (26.4) | ||
| Sometimes | 276 (8.11) | 187 (67.75) | 89 (32.25) | ||
| Often | 437 (12.85) | 283 (64.76) | 154 (35.24) | ||
| Usually | 554 (16.28) | 363 (65.52) | 191 (34.48) | ||
| Always | 1471 (43.24) | 883 (60.03) | 588 (39.97) | ||
| Media | Never | 991 (29.13) | 652 (65.79) | 339 (34.21) | 0.594 |
| Occasionally | 612 (17.99) | 396 (64.71) | 216 (35.29) | ||
| Sometimes | 490 (14.4) | 317 (64.69) | 173 (35.31) | ||
| Often | 555 (16.31) | 343 (61.8) | 212 (38.2) | ||
| Usually | 341 (10.02) | 210 (61.58) | 131 (38.42) | ||
| Always | 413 (12.14) | 262 (63.44) | 151 (36.56) | ||
| Reliable resources | Never | 774 (22.75) | 548 (70.8) | 226 (29.2) | < 0.0001 |
| Occasionally | 275 (8.08) | 183 (66.55) | 92 (33.45) | ||
| Sometimes | 364 (10.7) | 245 (67.31) | 119 (32.69) | ||
| Often | 469 (13.79) | 311 (66.31) | 158 (33.69) | ||
| Usually | 521 (15.31) | 327 (62.76) | 194 (37.24) | ||
| Always | 999 (29.37) | 566 (56.66) | 433 (43.34) |
Most participants were female (64.2%). There were 49.1% participants aged 18–30, and 50.9% aged 31 or above. For health status, 13.6% of them reported having chronic conditions. 71.4% of respondents were residing in urban regions. Regarding work-related characteristics, 58.7% of them were working before the pandemic, while 5.5% lost their job due to coronavirus. Vaccine hesitancy was observed in 857 (25.2%) respondents. 2229 (65.5%) respondents had fears about COVID-19, 3243 (95.3%) considered themselves at risk of contracting COVID-19, and 1049 (30.8%) perceived COVID-19 as being serious to their own lives (Table 1).
According to their statements, 1222 participants (35.92%) will consent to get vaccinated against COVID-19. In multivariable analysis (Table .2), male gender, younger age, rural residence, not having children, smoking, fear about COVID-19, individual perceived severity, believing in the natural origin of the coronavirus, and high vaccination Knowledge remained associated with COVID-19 vaccine acceptance. Surprisingly, no significant influence arose from studying or working within the medical field on respondents’ acceptance or rejection of COVID-19 vaccine.
Table 2.
Factors associated with intentions to accept COVID-19 vaccination when it is available
| Crude OR (95%CI) | P value | Adjusted OR (95%CI) | P value | |
|---|---|---|---|---|
| Sex | ||||
| Female | 0.50 (0.44, 0.58) | < 0.0001 | 0.53 (0.44, 0.62) | < 0.0001 |
| Male | Reference | Reference | ||
| Age | ||||
| 18–30 | 1.56 (1.35, 1.79) | < 0.0001 | 1.32 (1.06, 1.64) | 0.012 |
| >/30 | Reference | Reference | ||
| Residency province | ||||
| Northern-East | 1.13 (0.86, 1.48) | 0.38 | 1.09 (0.8, 1.49) | 0.57 |
| Middle | 1.08 (0.89, 1.32) | 0.44 | 1.07 (0.86, 1.33) | 0.57 |
| South | 0.92 (0.78, 1.08) | 0.31 | 0.93 (0.78, 1.12) | 0.45 |
| West | Reference | Reference | ||
| Region of residence | ||||
| Urban | 0.84 (0.72, 0.98) | 0.03 | 0.82 (0.69, 0.97) | 0.018 |
| Rural | Reference | Reference | ||
| Marital status | ||||
| Not married | 1.55 (1.34, 1.78) | < 0.0001 | 0.95 (0.68, 1.34) | 0.79 |
| Married | Reference | Reference | ||
| Having kids | ||||
| No | 1.55 (1.35, 1.79) | < 0.0001 | 1.40 (1.00, 1.96) | 0.05 |
| Yes | Reference | Reference | ||
| Highest level of education | ||||
| School | 0.82 (0.64, 1.06) | 0.137 | 1 (0.74, 1.36) | 0.99 |
| High Education | 1.01 (0.83, 1.23) | 0.9 | 1.03 (0.83, 1.3) | 0.77 |
| None | 0.79 (0.49, 1.26) | 0.32 | 0.92 (0.52, 1.62) | 0.77 |
| Post-graduate qualification | Reference | Reference | ||
| Pre-coronavirus employment status | ||||
| Not employed | 0.995 (0.86, 1.15) | 0.94 | 0.87 (0.66, 1.14) | 0.32 |
| Employed | Reference | Reference | ||
| Employment change due to coronavirus | ||||
| Furlough | 1.19 (0.72, 1.96) | 0.495 | 1.26 (0.71, 2.22) | 0.43 |
| Newly Unemployed | 0.9 (0.56, 1.46) | 0.67 | 0.77 (0.44, 1.35) | 0.36 |
| None | 0.91 (0.62, 1.34) | 0.64 | 0.86 (0.56, 1.34) | 0.51 |
| Newly employed | Reference | Reference | ||
| Financial income | ||||
| Freelancing | 1.18 (0.91, 1.52) | 0.21 | 1.24 (0.92, 1.66) | 0.16 |
| Family | 1.06 (0.88, 1.29) | 0.54 | 1.14 (0.84, 1.55) | 0.4 |
| Salary only | 0.9 (0.73, 1.1) | 0.298 | 0.99 (0.79, 1.24) | 0.92 |
| Salary + Other | Reference | Reference | ||
| Healthcare worker | ||||
| Yes | 0.78 (0.61, 1.007) | 0.057 | 1.07 (0.77, 1.48) | 0.70 |
| No | 0.57 (0.47, 0.68) | < 0.0001 | 1.27 (0.97, 1.66) | 0.082 |
| Student in healthcare | Reference | Reference | ||
| Smoking status | ||||
| No | 0.83 (0.72, 0.95) | 0.008 | 0.79 (0.68, 0.93) | 0.005 |
| Yes | Reference | Reference | ||
| Chronic medical conditions | ||||
| No | 0.86 (0.7, 1.05) | 0.136 | 0.88 (0.7, 1.11) | 0.28 |
| Yes | Reference | Reference | ||
| fears about COVID-19 | ||||
| No | 0.60 (0.52, 0.70) | < 0.0001 | 0.54 (0.46, 0.64) | < 0.0001 |
| Yes | Reference | Reference | ||
| Perceived risk of contracting COVID-19 | ||||
| Unlikely | 0.74 (0.52, 1.05) | 0.088 | 0.83 (0.54, 1.25) | 0.37 |
| Likely | Reference | Reference | ||
| Perceived severity of effect of COVID-19 on own life | ||||
| Not serious | 0.76 (0.66, 0.88) | < 0.0001 | 0.78 (0.65, 0.92) | 0.004 |
| Serious | Reference | Reference | ||
| Beliefs on the origin of the virus | ||||
| Natural | 3.49 (2.94, 4.15) | < 0.0001 | 2.56 (2.11, 3.1) | < 0.0001 |
| Artificial | Reference | Reference | ||
| General Vaccine Hesitancy | ||||
| Hesitant | 0.94 (0.8, 1.11) | 0.467 | 1.01 (0.85, 1.21) | 0.88 |
| Not hesitant | Reference | Reference | ||
| Knowledge | 1.24 (1.20, 1.28) | < 0.0001 | 1.23 (1.19, 1.28) | < 0.0001 |
The most common reason for refusal and hesitancy to accept COVID-19 vaccination was “fear of side effects”, and other reasons included “doubts about vaccine efficiency”, “the vaccine is not important”, “not the right time to be vaccinated”, and “just refuse the vaccine” (Fig. 1).
Fig. 1.
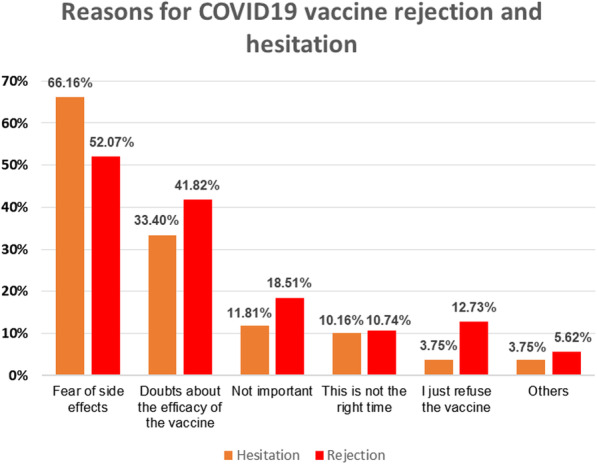
Reasons for COVID-19 vaccine rejection and hesitation
Discussion
This study was conducted during the second wave of COVID-19 pandemic in Syria and after the emergence of multiple promising vaccines around the world.
Despite the relatively difficult experience of our population with the pandemic and its severe socioeconomic consequences, the results describe 17% refusing vaccination, 35% accepting, and 46% undecided. This level of acceptance rate is considerably low in comparison with other countries (Fig. 2) [12, 18]. In this regard, we will discuss the factors that may have played a role in these findings, the short and long-term repercussions of such numbers, and propose solutions to improve vaccine acceptance rates.
Fig. 2.
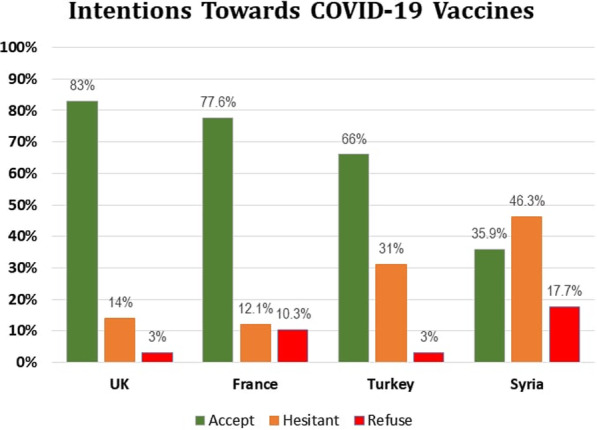
Intentions to get COVID-19 vaccination among different countries
Factors associated with vaccination intentions
According to our data, gender as a predictor of willingness for vaccination against SARS-CoV-2 presented a statistically significant difference. Males were more likely to accept the vaccine than females, which could be attributed to the higher sex-based risks of complications and mortality, in addition to the potential economic impacts of the pandemic on the father’s role as a primary source of household income [19, 20]. Whereas females were more reluctant to be vaccinated than males, as they tend to collect medical information from various sources when it comes to their families’ health [20].
The results also indicate that older people – who are also at greater risk of complications and mortality [21] – were more likely to refuse COVID-19 vaccine than younger adults. Their concerns about vaccine safety may be the reason for this disparity. On the other hand, younger people are more exposed to educational campaigns and scientific discussions related to vaccine development protocols due to their higher literacy skills [22, 23]. This leads us to think about the importance of targeting the elderly with sensitizing campaigns in order to enhance their willingness for vaccination.
Individuals who had children were more reluctant to be vaccinated compared to those who did not have children. Misconceptions alongside the fear of consequences of vaccination or leaving family members behind may explain this reluctance [24].
Interestingly, residents in rural areas were more willing to get vaccinated than urban residents. The reason for this disparity could be attributed to the online distribution method of the questionnaire that may have reached more educated groups of rural populations than disadvantaged ones, which in turn skewed the results toward acceptance. Furthermore, our data was unable to reveal a statistically significant difference between healthcare workers and the general population in terms of vaccine acceptance. This finding needs to be examined carefully, as their higher literacy skills on healthcare-related issues and recent guidelines do not seem to be a significant factor in their willingness for vaccination as expected. The former is particularly important due to the fact that the already devastated healthcare system in Syria dealing with a pandemic of this size without taking preventive measures such as vaccination could result in calamitous consequences.
In Syria, the acceptance rates were almost half compared to studies conducted in other countries (Fig. 2) [12, 18]. One of the most important pillars to whether to get vaccinated or not is the individual’s knowledge of both the disease and the role of immunization in stopping its spread. Conspiracy beliefs and misinformation were one of the main obstacles to adhere to prevention measures at the early stages of the pandemic, and the same thing is happening now with the educational programs about the importance of vaccination and herd immunity [25, 26]. Despite the scientific consensus on the natural origin of the virus [27], as well as the sensitizing campaigns and social network algorithms to encounter misinformation, only 20.31% of participants in our survey believed in the natural origin of the coronavirus.
The roots of these beliefs can be traced back to several factors. For instance, cognitive biases – like “confirmation bias”, “The availability Heuristic Bias”, “Belief biases” – make the idea of the artificial origin of the virus easier and more appealing to believe [28]. Information sources play a major role in building these beliefs among individuals [29]; participants in our survey who depend on reliable scientific sources and healthcare providers were more willing to accept the vaccine. This focuses on the importance of credible information, especially during the rapid changes and the dissemination of faulty news.
The above is particularly important because cognitive biases, the declining socioeconomic status (SES), and the collapsed healthcare system are among the most prominent features of the nearly decade-old ongoing war; this increases the randomness of the course of the pandemic in such war-torn countries compared to the rest of the world. On the other hand, making use of these factors to enhance the population’s acceptance of the vaccine is also possible, as the fear of contracting COVID-19 alongside the individual’s perception of the seriousness and consequences of infection is associated with increased willingness to accept the vaccine, as shown in our analysis.
The special case of Syria
From a broader perspective, hesitation or rejection of the vaccine, together with the aforementioned factors, would constitute a vicious cycle in which the already devastated SES and healthcare systems would take turns reactivating it. The deteriorating SES – represented by overcrowded communities suffering from food shortages, low immunity, lack of proper education, and underprivileged healthcare settings – will make of these communities a suitable milieu for misleading information and conspiracy beliefs; thus, reducing the willingness to be vaccinated and increasing the rates of infection spread [30–32], which puts additional burdens on the already-weakened healthcare systems [31, 33]. On the other hand, the overwhelmed healthcare units will be less able to manage patients and monitor new cases, which in turn, will negatively affect the economy and population’s trust in their healthcare systems [31, 34, 35]; and thus, activating the cycle again. Moreover, logistical barriers to vaccination also play an important role; At a time when purchasing power, electricity, internet access, and fuel are scarce, logistics can prohibit vaccines from reaching individuals willing to get vaccinated. Even though approaching such a scenario in a precise statistical framework is not applicable with our study design under the rapid changes in SES as well as lack of national demographic references that can be used as statistical variables, we can conclude by observing several experiences of war-torn countries, including Syria, that the problem does not stop here, but it may rather reach the reemergence of nearly eliminated diseases [31], such as the spread of polio from Syria to Iraq between 2013 and 2014 [36, 37]. This opens the door for many questions about surveillance and management during the crisis:
In the event of an epidemic re-emergence or a mutation arising in the virus, what is the possibility of tracking new cases before spreading to other countries? If global herd immunity is reached prior to Syria, would an isolation of the country be mandated? And if so, what repercussions would Syria encounter while dealing with the successive waves of the pandemic?
Our data stop on the boundaries of these questions and cannot answer them, but we emphasize the importance of taking these points into consideration when health policymakers make relevant decisions – since one of the most important lessons learned from the world’s experience with the pandemic is that “time of action matters” [38].
Suggested solutions
After the massive spread of the pandemic in almost all countries of the world, it became clear that the solution is only possible through achieving herd immunity [9], which requires immunizing 55–80% of the population against the virus – as a recent study showed [39]. But in order to reach this threshold, there should be a level in which the population is prepared to achieve a sufficient degree of “scientific citizenship” that in turn increases willingness for vaccination [40].
Scientific citizenship implies creating a climate of communication between the scientific community and citizens on the basis of transparency, mutual trust, and active engagement, through which it is possible to confront misinformation and enhance community confidence in their healthcare institutions [25, 26, 40]. This includes: (A) Conducting educational campaigns that discuss individuals’ concerns about the pandemic and vaccine safety, as well as explaining recommendations through sensitizing dialogues [40]. (B) Emphasizing the prosocial benefits of immunization, as several studies have demonstrated that clarifying the social benefits of herd immunity increases the willingness for vaccination [41, 42] – particularly since the experience of locking down the country during the first wave had severely affected the SES of the population [20, 43]. (C) Supporting psychological research that investigates community behavior and its perspective about vaccines. (D) Interventions should be directed to encourage health workers and elderly people with chronic diseases to get vaccinated, which contributes to relieving pressure on health care units [13].
Strengths and limitations
To the best of our knowledge, this is the first study to investigate COVID-19 vaccine acceptance rates in Syria. The importance of this study comes from the fact it sheds light on a global problem in a war-torn developing country — and thus provides health policymakers with input in order to better steer actions, and can also be used as a simulation for other countries that have not yet investigated their population’s acceptance rates.
A key limitation of our study is the use of an online sampling method, which introduced sampling bias and hampered the generalizability despite the large sample size. Participants who do not have any educational degree formed a low proportion of our sample, possibly because they do not have access to social media networks, so future studies may use better approaches to accommodate for this category. Second, the cross-sectional design of this study precludes our ability to infer causality among dependent and independent variables. Third, this study is based on self-reported measures, which might contribute to social desirability bias and justify the high percentage of respondents who did not yet decide whether to endorse or reject the vaccine. Forth, the online sampling method implied some limitations such as the roughly low number of elderly, illiterate participants and citizens living in conflict areas like the Northeast provinces where Internet access is not constantly available. However, the proportion of these groups in the population is relatively low and the questionnaire surveyed a homogeneous sample from the various categories of the Syrian population within a short period of time, without making any modifications to the questionnaire or the methodology during the experiment. Therefore, no adjusted weights were applied to the variables.
Conclusion
Hesitation about COVID-19 vaccine has become the most prominent problem facing health organizations at the present time of the pandemic, and it is clear that efforts must be combined to improve acceptance rates. Among the factors we studied in this paper, male gender, younger age, rural residence, not having children, smoking, fear about COVID-19, individual perceived severity, believing in the natural origin of the coronavirus, and high vaccination knowledge had a positive role in our population’s acceptance rates for vaccination. The rates may differ from one country to another or from a certain pandemic stage to another within the same country, but for developing or war-torn countries, further potential burdens exist and should be taken into consideration while discussing measures to exit the current crisis on an international scale. This study focused on Syria, but at the same time it provides an insight into countries with similar conditions, which unfortunately do not have enough epidemiological reports to coordinate international efforts to help them.
Acknowledgments
This research wouldn’t have been done without all the help of enthusiastic and cooperative colleagues. We would like to thank: Dr. Majdy Rafeq Hmedy, Dr. Hazar Abdulrahman, Dr. Hassan Mayya, Dr. Sara Deeb, Dr. Hussein Ahmad, Dr. Hasan Mufid Darwish, and Dr. Jullian Sankari for their valuable contribution to this research study.
Authors’ contributions
A.Z., O.M., N.K. designed the study. O.M., A.Z., A.M., M.A., and N.K. collected the data with the help of research contributors. O.M. and R.S. analyzed the data. O.M., A.Z., N.K., A.M., and M.A. drafted the manuscript. O.M. and A.Z. co-first authors as they contributed equally to the research study. N.K. coordinated the research team. R.S. supervised the study. All the authors revised the manuscript. The author(s) read and approved the final manuscript.
Funding
There is no funding.
Availability of data and materials
The data analyzed during the current study are available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
The study ethical review was conducted by the Ethical Committee at the Faculty of Medicine, Tishreen University and approved according to the principles embodied in the Declaration of Helsinki. This study conducted as an online observational study. All participants received a thorough explanation about the research and that it is conducted for academic purposes only. All the necessary measures to safeguard participants’ anonymity and confidentiality of personal information were respected. Participation in the study was voluntary. Informed consent was obtained from all the participants as we noted that completing the questionnaire was considered as a consent to participate.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Okbah Mohamad and Ali Zamlout co-first authors.
References
- 1.Harrison EA, Wu JW. Vaccine confidence in the time of COVID-19. Eur J Epidemiol. 2020;35(4):325–330. doi: 10.1007/s10654-020-00634-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organization. Vaccines and immunization: Vaccine safety. 2020. https://www.who.int/news-room/q-a-detail/vaccines-and-immunization-vaccine-safety. Accessed 13 February 2021.
- 3.World Health Organization. Children: improving survival and well-being. 2020. https://www.who.int/news-room/fact-sheets/detail/children-reducing-mortality. Accessed 14 February 2021.
- 4.World Health Organization. WHO Coronavirus Disease (COVID-19) Dashboard. 2021. https://covid19.who.int. Accessed 14 February 2021.
- 5.Vision World International. World Vision Syria Response COVID-19 Situation Report (July 2020). 2020. https://www.wvi.org/publications/report/syria-crisis-response/world-vision-syria-response-covid-19-situation-report. Accessed 14 February 2021.
- 6.World Health Organization. WHO EMRO | HeRams | Syrian Arab Republic. 2021. http://www.emro.who.int/syr/herams/index.html. Accessed 14 February 2021.
- 7.U.S. Food and Drug Administration. COVID-19 Vaccines. 2021. https://www.fda.gov/emergency-preparedness-and-response/coronavirus-disease-2019-covid-19/covid-19-vaccines. Accessed 14 February 2021.
- 8.AstraZeneca. AstraZeneca’s COVID-19 vaccine authorised for emergency supply in the UK. 2021. https://www.astrazeneca.com/media-centre/press-releases/2020/astrazenecas-covid-19-vaccine-authorised-in-uk.html. Accessed 14 February 2021.
- 9.Schaffer DeRoo S, Pudalov NJ, Fu LY. Planning for a COVID-19 vaccination program. JAMA. 2020;323(24):2458–2459. doi: 10.1001/jama.2020.8711. [DOI] [PubMed] [Google Scholar]
- 10.Centers for Disease Control and Prevention. Flu Vaccination Coverage, United States, 2018–19 Influenza Season. 2019. https://www.cdc.gov/flu/fluvaxview/coverage-1819estimates.htm. Accessed 13 February 2021.
- 11.Barello S, Nania T, Dellafiore F, Graffigna G, Caruso R. 'Vaccine hesitancy' among university students in Italy during the COVID-19 pandemic. Eur J Epidemiol. 2020;35(8):781–783. doi: 10.1007/s10654-020-00670-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Detoc M, Bruel S, Frappe P, Tardy B, Botelho-Nevers E, Gagneux-Brunon A. Intention to participate in a COVID-19 vaccine clinical trial and to get vaccinated against COVID-19 in France during the pandemic. Vaccine. 2020;38(45):7002–7006. doi: 10.1016/j.vaccine.2020.09.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dror AA, Eisenbach N, Taiber S, Morozov NG, Mizrachi M, Zigron A, Srouji S, Sela E. Vaccine hesitancy: the next challenge in the fight against COVID-19. Eur J Epidemiol. 2020;35(8):775–779. doi: 10.1007/s10654-020-00671-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Freeman D, Loe B S, Chadwick A, Vaccari C, Waite F, Rosebrock L et al. COVID-19 vaccine hesitancy in the UK: the Oxford coronavirus explanations, attitudes, and narratives survey (Oceans) II. Psychol Med. 2020:1–15. [DOI] [PMC free article] [PubMed]
- 15.Wang K, Wong ELY, Ho KF, Cheung AWL, Chan EYY, Yeoh EK, Wong SYS. Intention of nurses to accept coronavirus disease 2019 vaccination and change of intention to accept seasonal influenza vaccination during the coronavirus disease 2019 pandemic: a cross-sectional survey. Vaccine. 2020;38(45):7049–7056. doi: 10.1016/j.vaccine.2020.09.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rey D, Fressard L, Cortaredona S, Bocquier A, Gautier A, Peretti-Watel P, et al. Vaccine hesitancy in the French population in 2016, and its association with vaccine uptake and perceived vaccine risk–benefit balance. Eurosurveillance. 2018;23(17):17–00816. doi: 10.2807/1560-7917.ES.2018.23.17.17-00816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zingg A, Siegrist M. Measuring people's knowledge about vaccination: developing a one-dimensional scale. Vaccine. 2012;30(25):3771–3777. doi: 10.1016/j.vaccine.2012.03.014. [DOI] [PubMed] [Google Scholar]
- 18.Salali G D, Uysal M S. COVID-19 vaccine hesitancy is associated with beliefs on the origin of the novel coronavirus in the UK and Turkey. Psychol Med. 2020:1–3. [DOI] [PMC free article] [PubMed]
- 19.Galbadage T, Peterson BM, Awada J, Buck AS, Ramirez DA, Wilson J, et al. Systematic Review and Meta-Analysis of Sex-Specific COVID-19 Clinical Outcomes. Front Med (Lausanne) 2020;7:348. doi: 10.3389/fmed.2020.00348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Holmes EA, O'Connor RC, Perry VH, Tracey I, Wessely S, Arseneault L, Ballard C, Christensen H, Cohen Silver R, Everall I, Ford T, John A, Kabir T, King K, Madan I, Michie S, Przybylski AK, Shafran R, Sweeney A, Worthman CM, Yardley L, Cowan K, Cope C, Hotopf M, Bullmore E. Multidisciplinary research priorities for the COVID-19 pandemic: a call for action for mental health science. Lancet Psychiatry. 2020;7(6):547–560. doi: 10.1016/S2215-0366(20)30168-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Garnier-Crussard A, Forestier E, Gilbert T, Krolak-Salmon P. Novel coronavirus (COVID-19) epidemic: what are the risks for older patients? J Am Geriatr Soc. 2020;68(5):939–940. doi: 10.1111/jgs.16407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kutner M, Greenberg E, Jin Y, Boyle B, Hsu Y-c, Dunleavy E. Literacy in Everyday Life: Results from the 2003 National Assessment of Adult Literacy. NCES 2007–490. National Center for Education Statistics. 2007.
- 23.Kutner M, Greenburg E, Jin Y, Paulsen C. The Health Literacy of America's Adults: Results from the 2003 National Assessment of Adult Literacy. NCES 2006–483. National Center for Education Statistics. 2006.
- 24.Calandrillo SP. Vanishing vaccinations: why are so many Americans opting out of vaccinating their children? Univ Mich J Law Reform. 2004;37(2):353–440. [PubMed] [Google Scholar]
- 25.van der Linden S, Maibach E, Cook J, Leiserowitz A, Lewandowsky S. Inoculating against misinformation. Science. 2017;358(6367):1141–1142. doi: 10.1126/science.aar4533. [DOI] [PubMed] [Google Scholar]
- 26.Wong NC. “Vaccinations are safe and effective”: inoculating positive HPV vaccine attitudes against antivaccination attack messages. Commun Rep. 2016;29(3):127–138. doi: 10.1080/08934215.2015.1083599. [DOI] [Google Scholar]
- 27.Calisher C, Carroll D, Colwell R, Corley RB, Daszak P, Drosten C, Enjuanes L, Farrar J, Field H, Golding J, Gorbalenya A, Haagmans B, Hughes JM, Karesh WB, Keusch GT, Lam SK, Lubroth J, Mackenzie JS, Madoff L, Mazet J, Palese P, Perlman S, Poon L, Roizman B, Saif L, Subbarao K, Turner M. Statement in support of the scientists, public health professionals, and medical professionals of China combatting COVID-19. Lancet. 2020;395(10226):e42–e43. doi: 10.1016/S0140-6736(20)30418-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Britt MA, Rouet J-F, Blaum D, Millis K. A reasoned approach to dealing with fake news. Policy Insights Behav Brain Sci. 2019;6(1):94–101. doi: 10.1177/2372732218814855. [DOI] [Google Scholar]
- 29.Romer D, Jamieson KH. Conspiracy theories as barriers to controlling the spread of COVID-19 in the U.S. Soc Sci Med. 2020;263:113356. doi: 10.1016/j.socscimed.2020.113356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Baldwin-Edwards M: Migration in the middle east and mediterranean: a paper prepared for the policy analysis and research programme of the global commission on international migration: university research Institute for Urban Environment and Human Resources; 2005.
- 31.Nnadi C, Etsano A, Uba B, Ohuabunwo C, Melton M, Wa Nganda G, et al. Approaches to Vaccination Among Populations in Areas of Conflict. J Infect Dis. 2017;216(suppl_1):S368–Ss72. doi: 10.1093/infdis/jix175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ngo NV, Pemunta NV, Muluh NE, Adedze M, Basil N, Agwale S. Armed conflict, a neglected determinant of childhood vaccination: some children are left behind. Hum Vaccin Immunother. 2020;16(6):1454–1463. doi: 10.1080/21645515.2019.1688043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Physicians for Human Rights. Anatomy of a Crisis; a Map of Attacks on Health Care in Syria; Findings as of May 2016. 2016. https://www.ecoi.net/en/document/1216551.html. Accessed 18 February 2021.
- 34.Nicola M, Alsafi Z, Sohrabi C, Kerwan A, Al-Jabir A, Iosifidis C, et al. The socio-economic implications of the coronavirus pandemic (COVID-19): a review. Int J Surg. 2020;78:185–193. doi: 10.1016/j.ijsu.2020.04.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Zhou F, Shefer A, Wenger J, Messonnier M, Wang LY, Lopez A, Moore M, Murphy TV, Cortese M, Rodewald L. Economic evaluation of the routine childhood immunization program in the United States, 2009. Pediatrics. 2014;133(4):577–585. doi: 10.1542/peds.2013-0698. [DOI] [PubMed] [Google Scholar]
- 36.Arie S. Polio virus spreads from Syria to Iraq. Bmj. 2014;348(apr02 3):g2481. doi: 10.1136/bmj.g2481. [DOI] [PubMed] [Google Scholar]
- 37.Ozaras R, Leblebicioglu H, Sunbul M, Tabak F, Balkan II, Yemisen M, Sencan I, Ozturk R. The Syrian conflict and infectious diseases. Expert Rev Anti-Infect Ther. 2016;14(6):547–555. doi: 10.1080/14787210.2016.1177457. [DOI] [PubMed] [Google Scholar]
- 38.Loewenthal G, Abadi S, Avram O, Halabi K, Ecker N, Nagar N, Mayrose I, Pupko T. COVID-19 pandemic-related lockdown: response time is more important than its strictness. EMBO Molecular Medicine. 2020;12(11):e13171. doi: 10.15252/emmm.202013171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Sanche S, Lin YT, Xu C, Romero-Severson E, Hengartner N, Ke R. High contagiousness and rapid spread of severe acute respiratory syndrome coronavirus 2. Emerg Infect Dis. 2020;26(7):1470–1477. doi: 10.3201/eid2607.200282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Provenzi L, Barello S. The science of the future: establishing a citizen-scientist collaborative agenda after Covid-19. Front Public Health. 2020;8:282. doi: 10.3389/fpubh.2020.00282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Betsch C, Böhm R, Korn L, Holtmann C. On the benefits of explaining herd immunity in vaccine advocacy. Nat Hum Behav. 2017;1(3):1–6. doi: 10.1038/s41562-017-0056. [DOI] [Google Scholar]
- 42.Obradovich N, Guenther SM. Collective responsibility amplifies mitigation behaviors. Clim Chang. 2016;137(1–2):307–319. doi: 10.1007/s10584-016-1670-9. [DOI] [Google Scholar]
- 43.Lee J. Mental health effects of school closures during COVID-19. Lancet Child Adolesc Health. 2020;4(6):421. doi: 10.1016/S2352-4642(20)30109-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data analyzed during the current study are available from the corresponding author on reasonable request.


