Abstract
Introduction/objectives
This study aims to assess the patients’ ability and willingness to utilize telemedicine (TM) along with identifying some of the barriers to a more widespread adoption of TM in rheumatology.
Methods
An observational, cross-sectional study of patients visiting a rheumatology clinic was conducted in 2018. We used a survey to assess patients’ attitude on the perceived effectiveness when comparing TM versus in-person visits, as well as patients’ access to technology, distance traveled by the patient to attend the clinic visit, and demographic parameters.
Results
A total of 214 patients were included. Negative correlations were found between the increase in age and access to technologies (front-facing camera (mean age difference − 12.8), telephone (mean age difference − 14.4), and stable internet connection (mean age difference − 15.1)), as well as believing that their needs could be met through TM (r − .224, p < 0.001) and thinking that TM could be an appropriate alternative method of healthcare (r − .298, p < 0.001). Younger patients reported more conflict between appointments and work hours (mean age difference − 11.73). Follow-up patients were more likely to feel that their visit could have been possible over the phone (mean difference − 1.13) or video conferencing (mean difference − 1.13) compared to new patients. Older patients were less likely to think that the purpose of their rheumatology visits could be achieved over the phone (r − .207, p = 0.003) or video conferencing (r − .331, p = 0.001). The further the distance traveled, the more the patients were willing to utilize TM compared to in-person visits (r 0.167, p = 0.019).
Conclusion
Out of necessity due to the COVID-19 pandemic, rheumatology clinics are increasingly turning to TM. The results of this study suggest that access and familiarity with technology may still be limited in certain demographics, particularly the elderly. Furthermore, this study helps to understand some of the additional barriers to more widespread adoption and patients’ perceived limitations of TM.
|
Key Points • This study aimed to assess rheumatology patients’ willingness to utilize telemedicine (TM) while determining the factors and barriers that may exist for a more widespread adoption of TM, using a cross-sectional survey in the setting of a rheumatologic clinic. • The age of the patient was the most significant contributing factor in a patient’s perception of TM, with older patients being less likely to think that the purpose of their rheumatology visits could be achieved over the phone or via videoconferencing. • The social trend of limited access to technology among the elderly population was reinforced by the results in this study. • Patients who had a greater commute to the clinic were more likely to willing to utilize TM consultations. • The results of this study highlight the elevated difficulty elderly patient populations have in utilizing TM. • With the current outbreak of COVID-19, the importance of utilizing TM specifically among the elderly population could prove vital. Future studies to focus on the elderly population and methods for helping these patients become familiar with TM would be beneficial. • Studies such as this can help to orchestrate future guidelines for TM in the field of rheumatology. Based on our study results, the new-patient encounter should be an in-person face-to-face encounter whenever possible, followed by TM visits for established patients who are able and open to using it, depending on the diagnosis and symptoms of the individual patients. |
Keywords: Rheumatology, Technology, Telemedicine
Introduction
The World Health Organization describes Telemedicine (TM) as “the delivery of health care services, where distance is a critical factor, by all health care professionals using information and communication technologies for the exchange of valid information for diagnosis, treatment and prevention of disease and injuries, research and evaluation, and for the continuing education of health care providers, all in the interest of advancing the health of individuals and their communities” [1].
TM is currently used to improve chronic care management and self-management in patients with chronic diseases. In the USA, 15% of physicians work in practices that utilize TM, while adoption by private insurers has been increasing 50% annually over the past decade [2]. TM provides remote health consultation, treatment, intervention, and assessment, which can improve patients’ health conditions at a relatively low cost [3, 4]. The use of TM has grown tremendously with the COVID-19 pandemic; its importance and utility are of greater value, and an area of increased research.
Advantages related to TM have been described in several reports, and include, but are not limited to: savings in time and healthcare cost through more efficient and effective methods of electronic referrals; allowing patients access to high-demand specialty care without the need for face-to-face consultations; improving patient satisfaction with increased disease activity monitoring for remote patients; and reducing wait times, travel expenses, waiting lists, and unnecessary appointments for patients who are seeking access to specialist outpatient services [5, 6].
Nevertheless, TM is not without its limitations and scrutiny. A major limitation of TM is a provider not being able to physically interact with, nor touch their patient. Instead with TM, physicians have to rely on the ability of the patient to “show” and describe the problem via televisual communication [7]. Patient privacy and confidentiality are also often under focus in the context of TM, due to concerns over patient consent and access to electronic data. In order to have a successful telemedicine experience, measures such as time/distance savings, convenience, ease of use, and time efficiency would be of great importance. Furthermore, technical support, access to high-speed internet, troubleshooting, and training for both the physicians and patients are factors to consider with the increased widespread adoption of TM [8].
Continuously optimizing patient satisfaction and quality of care are essential in fully integrating TM into clinics across the USA. Some studies have shown that there are no significant differences in patient satisfaction between face-to-face visits versus televisual primary care consultations [9]. Although telemedicine has been widely studied in primary care settings, the effectiveness and feasibility in other specialties have not been as well documented.
Recently, a study done by Wood and Caplan suggested that telemedicine can also be utilized in rheumatology, while keeping patient satisfaction high [10]. Regarding tele-rheumatology, patients may find rheumatic TM consults to be acceptable as well as both time and cost effective [11]. TM presents unique opportunities and benefits—particularly in rheumatology—as most rheumatic diseases are chronic in nature, requiring frequent and routine disease monitoring through trending lab values, patients’ self-report, and outpatient follow-up. Thus, it may be even more important for rheumatologists to become familiar with TM and utilize it effectively. This study aims to assess patients’ ability and willingness to utilize telemedicine as well as determining some of the barriers to a more widespread adoption of TM in rheumatology.
Methods
The main aim of this study was to assess rheumatology patients’ ability and willingness to utilize TM. To effectively address the aim, the Tele-Rheumatology Questionnaire (TRQ) was developed by the researchers of this study. The TRQ is composed of 17 questions. Of these 17 questions, five questions are focused on patients’ attitude towards the effectiveness of TM when compared to in-person visits; these were measured on a five-point Likert scale (1 = strongly agree, 2 = agree, 3 = neutral, 4 = disagree, 5 = strongly disagree). Eleven questions are closed-ended, yes-or-no type of questions: three were used to assess patients’ access to technology needed for TM (such as telephone, front-facing camera, and high-speed internet), seven addressed patient’s willingness to try TM in the future for various scenarios (i.e., try TM with stablish rheumatologist, try TM as an initial appointment, try TM to save time between appointments, try TM using telephone, try TM using video consultation, be part of future TM studies, try TM as a whole), and one asked if there was difficulty scheduling the current visit due to work. Lastly, one multiple choice question was included in the TRQ that addressed the distance traveled by the patient to attend the clinic visit; choices included less than 20 miles, 21–50 miles, or more than 50 miles. In addition to these 17 questions, five demographic questions were added to the TRQ, including age, sex, race, clinic status (new-patient or follow-up), and presence of an established diagnosis. This cross-sectional survey was given to patients who visited a rheumatology clinic in Central Florida in 2018 over the course of 6 months and met the inclusion criteria. Patients were offered the opportunity to participate if they fulfilled these criteria, which included a diagnosed or suspected rheumatic illness, currently seeing a rheumatologist at our clinic, were over 18 years of age, able to complete a questionnaire in English, and were capable of giving verbal and written consent. Individuals under the age of 18, unwilling to participate, and who were pregnant or were considered among other protected populations, were not included in the study. Data was analyzed using Statistical Package for Social Sciences (SPSS) and descriptive statistics were calculated.
Results
In total, 214 rheumatology patients participated in this study, of which 177 patients were females, 36 males, and 1 patient who did not self-identify. The average age of the patients was 58.3 ± 13.5 years. The breakdown of the medical reason for visit of the 214 patients is as follows: 119 were diagnosed with inflammatory arthritis, 6 with Sjögren’s syndrome, 26 with lupus, 3 with scleroderma and Raynaud’s, 15 with complex autoimmune disease, 8 with osteoporosis, 6 with inflammatory myopathy, 1 with inflammatory vasculitis, 1 presenting for an injection, and 29 who did not identify their established diagnosis or reason for visit. Additionally, 192 indicated they were follow-up visits, 5 were new, and 17 did not identify the visit type.
With regards to access to technology needed for TM appointments (Q1a. access to front-facing camera, Q1b. access to telephone calls, and Q2. access to stable internet) and patients’ willingness to try telemedicine in the future (Q11a), there were 211 patients who answered these four questions completely. Of these patients, 183 (86.7%) had access to all three technological modalities, while 28 (13.3%) indicated that they did not have access to one or more of these technologies. Of those who had access to all three, over 86% were willing to try telemedicine in the future, while of those who indicated they lacked access to at least one of the technologies, the percentage indicating they were willing to try TM in the future dropped to roughly 32%.
The age of the patient was determined to be the greatest contributing factor to the patients’ ability and willingness to utilize TM.
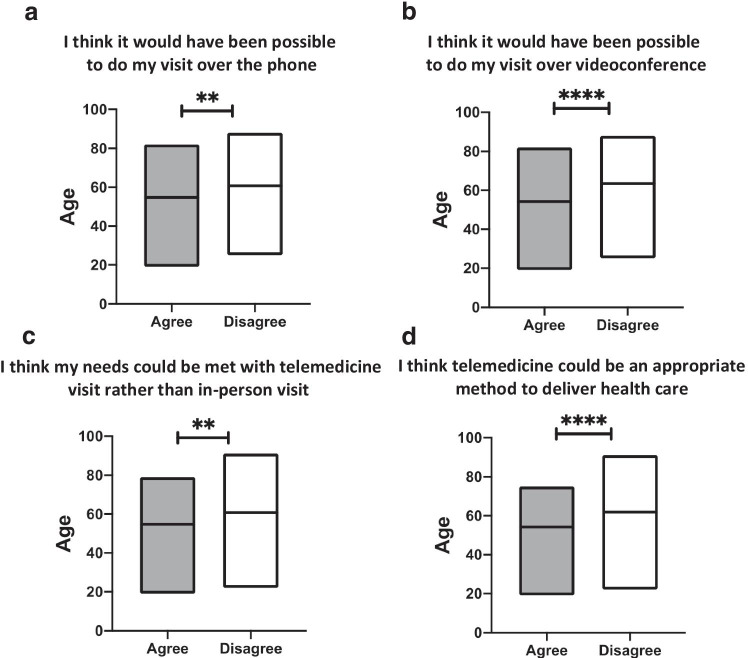
The older the patient, the less likely they were to feel that their visit could have been possible over the phone (r = − 0.207, p = 0.003) (Fig. 1a), less likely to feel that their visit could have been possible over video conferencing (r = − 0.331, p < 0.001) (Fig. 1b), less likely to feel that their needs could have been met with TM (r = − 0.224, p < 0.001) (Fig. 1c), and less likely to view TM as an appropriate method of health care (r = − 0.298, p < 0.001) (Fig. 1d).
Fig. 1.
Statistically significant finding between age and the following were identified: (a) statistically significant correlation between age and patients who responded that the purpose of the clinic visit could have been possible over telephone, in which a negative correlation of − 0.207 (p = 0.003) was seen. b Statistically significant correlation between age and patients who responded that the purpose of the clinic visit could have been possible over videoconference, in which a negative correlation of − 0.333 (p < 0.001) was seen. c Statistically significant correlation between age and patients who responded that their needs could have been met with telemedicine, in which a negative correlation of − 0.224 (p < 0.001) was seen. d Statistically significant correlation between age and patients who responded that telemedicine could be an appropriate method of healthcare, in which a negative correlation of − 0.298 (p < 0.001) was seen
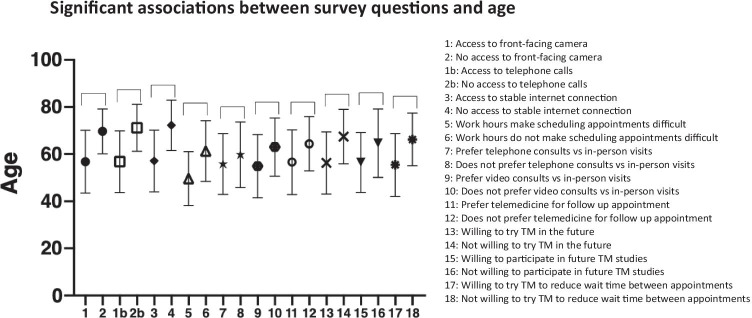
Single sample t test showed that “yes” responses in the closed-ended question portion of the TRQ were significantly associated with younger ages for the following: access to front-facing camera (mean difference in age = − 12.837, p < 0.001), access to telephone (mean difference in age = − 14.417, p < 0.001), access to stable internet connection (mean difference in age = − 15.107, p < 0.001), work hours that interfere with their current rheumatology appointments (mean difference in age = − 11.733, p < 0.001), would choose telephone consultation (mean difference in age = -3.973, p < 0.040), would choose live video consultation (mean difference in age = − 8.099, p < 0.001), willingness to utilize TM with new rheumatologists (mean difference in age = − 7.826, p < 0.001), willingness to try TM with established rheumatologist (mean difference in age = − 11.193, p < 0.001), willingness to try TM for other specialties (mean difference in age = − 8.167, p < 0.001), willingness to try TM in order to reduce time between appointments (mean difference in age = − 10.797, p < 0.001) (Fig. 2).
Fig. 2.
Statistically significant correlation between age and “yes and no” questions on the TRQ. The mean difference in age between 1 and 2 = − 12.837 (p < 0.001), between 1 and 2b = − 14.417 (p < 0.001), between 3 and 4 = − 15.107 (p < 0.001), between 5 and 6 = − 11.733 (p < 0.001), between 7 and 8 = − 3.973 (p < 0.040), between 9 and 10 = − 8.099 (p < 0.001), between 11 and 12 = − 7.826 (p < 0.001), between 13 and 14 = − 11.193 (p < 0.001), between 15 and 16 = − 8.167 (p < 0.001), between 17 and 18 = − 10.797 (p < 0.001)
Statistically significant differences between different subsets of diagnoses were found. For example, patients with osteoporosis were less likely to have access to a front-facing camera, access to stable internet connection, and willingness to use telemedicine if it reduced time between appointments, compared with patients with other diagnoses like inflammatory myopathy, complex autoimmune disease, lupus, and Sjögren’s syndrome (p < 0.02).
A statistically significant correlation was also identified between the patients’ distance traveled to come to the clinic and their wiliness to utilize TM; simply put, the further traveled, the more the patient was willing to utilize telephone consultations over in-person visits (r = 0.167, p = 0.019).
Lastly, when comparing established patients presenting for follow-up visits, versus new patients coming to establish care, the follow-up patients were more likely to feel that their visit could have been possible both over the phone (mean difference = 1.135, p = 0.038), as well as over video conferencing (mean difference 1.134, p = 0.05) compared to new patients.
Discussion
This study aimed to assess rheumatology patients’ willingness to utilize TM, while determining which factors and barriers may exist in a more widespread adoption of telemedicine, as well as their possible ability to utilize TM based on access to needed technology. The results from this study suggest that the age of the patient was the most significant contributing factor in their perception of TM. Older patients were less likely to think that the purpose of their rheumatology visits could have been achieved over the phone and even less likely over video conferencing (Fig. 1a,b). Negative correlations were also observed between increase in age and believing that their needs could be met through TM and thinking that TM could be an appropriate alternative method of healthcare (Fig. 1c,d).
One possible explanation for these observed patterns may be that older patients simply do not have access nor the familiarity with more modern technologies, such as web-based video conferencing and smartphones. A study conducted in 2019 by Pew Research Center observed that on average, 81% of individuals in the USA had access to smartphones [12]. While looking at different age groups, 96% of individual age 18–29 and 92% of individual age 30–49 had access to front-facing camera devices, whereas, only 53% of individual age 65 + had this same access.
This generational trend of limited access to technology among older individuals was reinforced by the results in this study. In the closed-ended portion of the TRQ, there were statistically significant differences in the mean ages of those who had access to a front-facing camera compared to those who did not, with individuals who had such access being 12.8 years younger. Similar trends were also observed in regard to access to a telephone (difference in mean age 14.4) and access to a stable internet connection (difference in mean age 15.1) (Fig. 2). The limited access to newer technology may also contribute to a lack of familiarity with these newer forms when compared to more traditional communication modalities, this may explain the stronger negative correlations among older patients who would prefer TM over the telephone, rather than via videoconferencing. While telephone calls are inherently simpler to operate, they are also more limited in terms of functionality when compared to videoconferencing, as the physician is unable to see the patient. Regardless, as telephones have been around longer, older individuals may be more comfortable with their use than with the use of newer front-facing/web-camera technology. This highlights the importance of allowing patients to become familiar with the different platforms and required equipment for TM.
Another possible explanation as to why older respondents had a lower willingness to participate in TM may be due to differences in disease severity and/or accompanying level of comorbidities. It is possible that if a patient had a greater burden of rheumatic disease, they would have the preference to come in for a physical face-to-face appointment for a more engaged/tactile examination of symptoms and disease progression.
Additionally, the distance traveled by the patients and their willingness to utilize TM demonstrated a statistically significant correlation, in which an increase in the distance needed to be traveled to the clinic was associated with an increase in the patient’s willingness to utilize telephone consultations. Perhaps, this is not surprising as one of the biggest advantages and driving force for TM has been to allow patients to seek care in remote locations, especially when seeking specialty care [13]. This may be particularly helpful for rheumatology given the low numbers of rheumatologist in comparison to the population [14].
Lastly, follow-up patients were more likely to be willing to utilize TM for rheumatology visits both over the telephone and via video conferencing, compared to their counterparts who were coming to establish care for the first time. This is significant as this suggests that patients with rheumatic illnesses may be more willing to utilize TM and increase the number of interactions with their rheumatologist, once a relationship has been established. However, the power of this assumption is limited as only five of the respondents were new patients who were coming to establish care. Interestingly, of the five respondents who indicated their consult type was for a “new appointment,” four of these positively affirmed that they would be willing to have a TM visit “as a follow-up appointment with an established rheumatologist.”
The 2019 study by Pew Research Center observed that females were somewhat less likely to adopt modern technological devices, such as smartphones, compared to their male counterparts, reporting that 79% of females owned smartphones as compared to 84% of males in the USA (with females more likely than men to own cellphones not designated as “smartphones,” 16% vs 14%, respectively) [12]. Nevertheless, in this study, statistically significant correlations between the sex of the patient and responses to TRQ were not observed. However, it is worth mentioning that 82.7% of the patients in this study were females.
Notably, we found that patient with osteoporosis reported lower access to front-facing camera, stable internet connection, and willingness to try telemedicine. This may be explained by the fact that osteoporosis is also a disease related with older age and thus, as previously mentioned factor of age and access to technology may play a role in this association.
Many rheumatologic diseases tend to be chronic, and frequent monitoring of disease activity has been associated with improvements in patient outcomes [15]. Therefore, if frequent monitoring could be effectively achieved and maintained using TM, it may lead to overall improvements in patient outcomes and sustained long-term benefits. A similar study monitoring cancer patient with mobile health applications saw positive improvements in patient-reported outcomes among patients who utilized mobile applications on their smartphones compared to those who only utilized traditional clinic visits [16].
A limitation of this study is the lack of specific rheumatological diagnoses in some of our patients, as general classes of diagnoses were used for some conditions; one example, the classification of “inflammatory arthritis,” of which there were 119 respondents, included the diagnosis of rheumatoid arthritis and psoriatic arthritis. Further breakdown of these diagnoses maintains a possibility of affecting one’s preference for telehealth services, and these were not specifically addressed. Additionally, copays and visit costs in Medicare and/or those that have commercial health insurance may contribute to a bias that was not teased out in this study; it is possible that a decrease in cost of TM vs in-person appointments would affect patients’ willingness. Moreover, the urgency of the visit was not specifically determined, asking if it was a routine follow-up or an urgent appointment due to an acute flareup of symptoms (or possibly for a specific reason such as a joint injection to combat acute inflammation). Lastly, though there was a question on whether patients would be more willing to utilize TM if they had work hours that interfered with appointments, neither the occupation nor the employment status of the patient was elicited. These are areas for potential inclusion in future studies.
The results of this study highlight the elevated difficulty elderly patient populations have in utilizing TM. Despite this, with the current outbreak of COVID-19, the importance of utilizing TM specifically among the elderly population could prove vital. Future studies to focus on the elderly population and methods for helping these patients become familiar with TM would be beneficial. For example, at the University of Central Florida Clinic, in order to help familiarize patients with the designated videoconferencing platform (Zoom), staff members call the patients prior to the visit to help walk the patient through downloading, installing, and using the software. Studies into the effectiveness of tutorials such as this, and what impact it may have on patients' experience and satisfaction with TM, would prove beneficial. Furthermore, additional studies into the different TM platforms and user-friendliness of each program, especially in the elderly population, should be performed.
A model for society’s adoption of a new innovation or idea was proposed by Dr. Everett Rogers PhD, in which adopters can be categorized into a predictable bell-shaped curve composed of innovators (2.5%), early adopters (13.5%), early majority (34%), late majority (34%), and laggards (16%). Furthermore, each adopter’s willingness and ability to adopt an innovation-in this case: TM- depends on their awareness, interest, evaluation, trial, and eventual adoption. As time progresses, the adoption rate continues to increase towards close to 100% with only a small percentage of laggards who have not or will not adopt. In this study, both the older individuals and those without access to high-speed internet and video capabilities were more non-accepting of TM.
According to the theory of innovations, this same group of elderly “late adopters” might become early adopters if a focus is placed on the influencing factors that affect their ability and motivation to see their doctor (such as excessive distance traveled, difficulty finding transportation, or during COVID-19-like pandemic or natural disaster). Put in another way, a paradigm shift in the delivery of medicine, such as TM, may eventually become the norm and accepted norm by most individuals if they perceive a benefit; from there, the rate of adoption can be influenced by techniques to make the innovation more acceptable, desirable, and easy to use.
To that end, currently, there are limited number of established rules and regulations regarding TM. The American Telemedicine Association (ATA) has compiled guidelines for TM for certain specialties. Importantly, however, there are not established guidelines for TM in rheumatology.
We hope that studies such as ours could help shed light into this rapidly developing field and help guide strategies for effectively utilizing TM in rheumatology. Following the results of our study, we suggest that new-patient encounters should optimally be a face-to-face in-person visit. However, if this cannot be done, in times like the pandemic or natural disaster, efforts should be made so that the second or third visit can be an in-person visit, as a hands-on physical exam of the patient is important in early disease monitoring and in establishing a patient-doctor relationship. Additionally, routine follow-up visits for chronic conditions or a non-urgent new problem for regularly established stable patients could be sufficiently addressed by TM, without a need for in-person visits. This may be dependent on the patient’s disease and activity level. If possible, face-to-face visit should be done at least once annually for chronic conditions or more frequently in severe/acute conditions, as determined by the provider. Furthermore, patients who are temporarily traveling out-of-town, or have a personal issue making it difficult to attend to an appointment in person, can often still be seen using TM as scheduled. Lastly, preferred communication means should be through video over telephone whenever possible, and effort should be placed to ensure that the patient and physician are comfortable in using the telemedicine modality; ideally having the support of Information Technology staff to assist in the event of a technological problem that arises. Utilizing these recommendations would help to ensure quality care be delivered effectively to all patients via TM.
Conclusion
With the current outbreak of the COVID-19 pandemic, numerous hospitals and practices, including rheumatology clinics, are increasingly turning to TM as the primary method—and sometimes only method—of seeing patients. Rapidly developing technology has allowed for greater adoption and growth of TM. TM was once exclusively reserved for those with access to expensive hardware and proprietary teleconsultation software [17]. Fortunately, with the rise of web-based commercial software and mobile applications, the cost and utility requirements of TM have diminished significantly in the last 10 years, such that anyone with a smartphone and an internet connection can now participate in TM. The results of this study suggest that this adoption of technology may still be limited in certain demographics, particularly the elderly, and this may be a factor in hindering a willingness of certain populations to utilized TM. Nevertheless, as TM continues to grow, it is important to assess the effectiveness of telemedicine, its ease of use, and patient satisfaction, and analyze barriers towards its more widespread adoption.
Acknowledgements
We thank Dr. Olga Karasik (Internal Medicine Associate Program Director, University of Central Florida) and Dr. Hiren Patel (Chief Resident, University of Central Florida, Internal Medicine Program) for all their suggestions and support.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors. This research was supported (in whole or in part) by HCA Healthcare and/or an HCA Healthcare affiliated entity.
Data availability
Data available on request from the authors. The data that support the findings of this study are available from the corresponding author upon request.
Code availability
All data collected was de identified using a randomized number coder between 1 and 200 that the participants were given when the survey.
Declarations
Ethics approval
Institutional reviews board, University of central Florida: Determination of exempt human research.
Consent to participate
Verbal and written informed consent was obtained from each participant for this study at the time of recruitment in the physician office.
Disclosures
None.
Disclaimer
The views expressed in this publication represent those of the author(s) and do not necessarily represent the official views of HCA Healthcare or any of its affiliated entities.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Ryu S. Telemedicine: opportunities and developments in member states: report on the second global survey on eHealth 2009 (Global Observatory for eHealth Series, Volume 2) Healthcare Informatics Research. 2012;18(2):153–155. doi: 10.4258/hir.2012.18.2.153. [DOI] [Google Scholar]
- 2.Dorsey ER, Topol EJ. Telemedicine 2020 and the next decade. Lancet. 2020;395(10227):859. doi: 10.1016/S0140-6736(20)30424-4. [DOI] [PubMed] [Google Scholar]
- 3.Wu G, Keyes LM. Group tele-exercise for improving balance in elders. Telemed J E Health. 2006;12(5):561–570. doi: 10.1089/tmj.2006.12.561. [DOI] [PubMed] [Google Scholar]
- 4.Vismara LA, McCormick C, Young GS, Nadhan A, Monlux K. Preliminary findings of a telehealth approach to parent training in autism. J Autism Dev Disord. 2013;43(12):2953–2969. doi: 10.1007/s10803-013-1841-8. [DOI] [PubMed] [Google Scholar]
- 5.Vimalananda VG, Gupte G, Seraj SM, Orlander J, Berlowitz D, Fincke BG, et al. Electronic consultations (e-consults) to improve access to specialty care: a systematic review and narrative synthesis. J Telemed Telecare. 2015;21(6):323–330. doi: 10.1177/1357633X15582108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Piga M, Cangemi I, Mathieu A, Cauli A. Telemedicine for patients with rheumatic diseases: systematic review and proposal for research agenda. Semin Arthritis Rheum. 2017;47(1):121–128. doi: 10.1016/j.semarthrit.2017.03.014. [DOI] [PubMed] [Google Scholar]
- 7.Anthone I, Floria M, Cărăuşu E (2017) E-health and bioengineering conference. 10.1109/EHB.2017.7995358
- 8.Almathami HKY, Win KT, Vlahu-Gjorgievska E. Barriers and facilitators that influence telemedicine-based, real-time, online consultation at patients' homes: systematic literature review. J Med Internet Res. 2020;22(2):e16407-e. doi: 10.2196/16407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Leggett P, Graham L, Steele K, Gilliland A, Stevenson M, O'Reilly D, et al. Telerheumatology–diagnostic accuracy and acceptability to patient, specialist, and general practitioner. Br J Gen Pract. 2001;51(470):746–748. [PMC free article] [PubMed] [Google Scholar]
- 10.Wood PR, Caplan L. Outcomes, satisfaction, and costs of a rheumatology telemedicine program: a longitudinal evaluation. J Clin Rheumatol. 2019;25(1):41–44. doi: 10.1097/RHU.0000000000000778. [DOI] [PubMed] [Google Scholar]
- 11.Davis P, Howard R, Brockway P. An evaluation of telehealth in the provision of rhematologic consults to a remote area. J Rheumatol. 2001;28:1910–1913. [PubMed] [Google Scholar]
- 12.Demographics of Mobile Device Ownership and Adoption in the United States. (2020, June 05). Retrieved October 18, 2020, from https://www.pewresearch.org/internet/fact-sheet/mobile/
- 13.Kruse C, Betancourt J, Ortiz S, Valdes Luna SM, Bamrah IK, Segovia N. Barriers to the use of mobile health in improving health outcomes in developing countries: systematic review. J Med Internet Res. 2019;21(10):e13263. doi: 10.2196/13263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.FitzGerald JD, Battistone M, Brown CR, Jr, et al. Regional distribution of adult rheumatologists. Arthritis Rheum. 2013;65(12):3017–3025. doi: 10.1002/art.38167. [DOI] [PubMed] [Google Scholar]
- 15.Lam NC, Ghetu MV, Bieniek ML. Systemic lupus erythematosus: primary care approach to diagnosis and management. Am Fam Physician. 2016;94(4):284–294. [PubMed] [Google Scholar]
- 16.Osborn J, Ajakaiye A, Cooksley T, Subbe CP. Do mHealth applications improve clinical outcomes of patients with cancer? A critical appraisal of the peer-reviewed literature. Support Care Cancer. 2020;28(3):1469–1479. doi: 10.1007/s00520-019-04945-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.O'Cathail M, Sivanandan MA, Diver C, Patel P, Christian J. The use of patient-facing teleconsultations in the National Health Service: scoping review. JMIR Med Inform. 2020;8(3):e15380. doi: 10.2196/15380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Roine R, Ohinmaa A, Hailey D. Assessing telemedicine: a systematic review of the literature. CMAJ. 2001;165(6):765–771. [PMC free article] [PubMed] [Google Scholar]
- 19.Caffery LJ, Farjian M, Smith AC. Telehealth interventions for reducing waiting lists and waiting times for specialist outpatient services: a scoping review. J Telemed Telecare. 2016;22(8):504–512. doi: 10.1177/1357633X16670495. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data available on request from the authors. The data that support the findings of this study are available from the corresponding author upon request.
All data collected was de identified using a randomized number coder between 1 and 200 that the participants were given when the survey.