Abstract
Objectives
This integrative review aimed to assess the benefits of the use of teledentistry for patients undergoing treatment of oral and head and neck cancer during the COVID-19 pandemic.
Materials and methods
We searched in PubMed, Cochrane, Scopus, Web of Science, Lilacs, Embase, Open Grey, Google Scholar, and Jstor databases for studies referring to the management, control, and assistance, through teledentistry, to patients with oral and head and neck cancer during the COVID-19 pandemic.
Results
We found 356 references in the databases, 209 after duplicates removal, 23 met criteria for full-text reading, and 11 studies were included for qualitative synthesis, in four categories: virtual visits, use of remote technology, patient’s satisfaction, multidisciplinary approach in teledentistry. We found that 78% of patients currently preferred teledentistry; 92% of patients would recommend the use of video consultation to other patients. The continuity of dental care, the reduction of patient visits to the hospital, the reduction of the risk of infection with the coronavirus, and limitation of face-to-face consultations to protect health professionals are benefits that reinforce the use of teledentistry by health institutions. Two studies showed patients’ satisfaction with the use of teledentistry in monitoring cancer patients and showed an improvement in quality of life.
Conclusions
The teledentistry, as a remote technology for monitoring patients with oral and head and neck cancer, is well accepted by patients in preliminary studies. Although these studies pointed out some benefits of using remote technologies for the care of cancer patients, further robust scientific evidence is still needed in this regard.
Supplementary Information
The online version contains supplementary material available at 10.1007/s00520-021-06398-0.
Keywords: COVID-19, Teledentistry, Telemedicine, Oral cancer, Head and neck cancer, Integrative review
Introduction
The emergence of the novel coronavirus (SARS-CoV-2) has resulted in a global public health crisis (COVID-19 pandemic), prompting the World Health Organization (WHO) to declare it a public health emergency of international concern. The pandemic has spread exponentially across the world causing, along with the so mentioned health burden, devastating global economic impacts [1]. The SARS-CoV-2 is highly contagious and can spread rapidly via respiratory secretions. Healthcare workers, particularly dentists, anesthetists, head and neck surgeons, ophthalmologists, and otolaryngologists, are at a high risk of infection [2]. As dental treatments invariably involve close inspection, examination, and diagnostic and therapeutic interventions of the naso-oro-pharyngeal region, dental professionals are most susceptible to get infected with coronavirus [3]. Owing to the transmission of COVID-19 through droplets and aerosols, which are inherent features of the dental practice, most of the countries followed a strategy of suspension of all elective dental care services and reserving it only for emergency cases [4].
For patients with cancer who already have decreased immunity, data from China suggest that the new virus poses additional fatal risks. The mortality of patients with cancer was 5.6% compared to 2.3% of the general population [5]. Cancer was actually found to be a major risk factor for COVID-19’s severe events in comparison with chronic obstructive pulmonary disease, diabetes, hypertension, and old age, with 39% of patients with cancer experiencing severe events (intensive care unit stays requiring ventilation or death) versus 8% of patients without cancer [6].
In the USA, the Centers for Disease Control and Prevention (CDC) recommended postponing all elective dental procedures [7]. Major American health societies related to clinical oncology, oncology radiology, otolaryngology, head and neck surgery, and oncology surgery have advised that care should be “taken to avoid delays in consultation and treatment which may adversely affect potentially curable patients.” Such institutions have encouraged telemedicine (TM) where appropriate and have advised limiting patient care to “time-sensitive and emergent problems” with a recommendation to consider telephone or video-based patient visits [8–15].
Regarding oral cancer, there is a complete absence of literature regarding the long‐term impact of pandemics on patients with oral potentially malignant disorders (OPMDs) and early‐stage oral cancer. Prior to this pandemic, even with readily available access for most patients to a fully intact healthcare infrastructure, less than 50% of patients with oral cancer were diagnosed at an early stage [16].
In this context, TM gains importance, as a valuable tool in the initial assessment of the patient and in the diagnosis of oral medicine conditions [17]. The popularity and prevalence of TM have grown rapidly during this pandemic as many physicians have sought ways to maintain a continuum of care with their patients [18]. Such initiatives have previously been shown to decrease costs, decrease visit time, and lead to high patient satisfaction in surgical fields [10, 19].
This study aimed to analyze, through an integrative literature review, the management, control, and assistance performed by the dental team, through teledentistry (TD), to patients with oral and head and neck cancer during the COVID-19 pandemic. The intention of this study was to answer the following question: “What are the benefits of the use of teledentistry for patients undergoing treatment of oral and head and neck cancer during the COVID-19 pandemic?”.
Methods
We conducted an integrative review (IR), a distinct unique method in which it is possible to summarize various studies to provide a more extensive understanding of a particular health problem [20]. To perform this IR, we have followed six steps: formulating the research question, searching the literature, extracting data from the primary studies, assessing the studies included in the IR, analyzing, and synthesizing the results, and presenting the IR [21]. The protocol of this study was registered on the Center for Open Science website (https://www.cos.io/, under the DOI number 10.17605/OSF.IO/BP5AN. The Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) [22] was adapted and used to report this IR since there is not a specific checklist to this literature review method yet.
Terminology definition
TM can be defined as the set of telematic technologies used to provide the patient with healthcare services — diagnosis, monitoring, therapy — at distance. It is therefore a distance delivery of health services. For the World Health Organization, TM literally means “remote healing” and indicates the use of technologies, information, and communication to improve the health outcomes of patients, increasing access to medical care and information [23]. TD (a subunit of telehealth along with TM) is the remote facilitating of dental care, guidance, education, or treatment via the use of information technology rather than through direct face-to-face contact with any patient [24]. Over the years, TD has proved to be beneficial for remote dental screening, making diagnosis, providing consultation, and proposing treatment plan [25, 26]. For this review, the concept of TD was standardized, acting on both dental and non-dental complications located in the oral cavity as a standard for conducting the search, selection, and analysis of studies.
Research question
The research question used to perform this IR was: “What are the benefits of the use of teledentistry for patients undergoing treatment of oral and head and neck cancer during the COVID-19 pandemic?”.
Search strategy
On October 19th, 2020, a broad search of studies without language restrictions in the following databases was performed: PubMed, Cochrane, Scopus, Web of Science, Lilacs (Latin American and Caribbean Literature), Embase, Library, and gray literature through Open Grey, Google Scholar, and Jstor. The search strategy used is in Additional file 1. A manual track down of lists of relevant articles was also done. Immediately after the literature investigation, the references were exported to the online reference manager Rayyan QCRI (https://rayyan.qcri.org/welcome) and duplicated references were removed.
Inclusion and exclusion criteria
We considered eligible for this IR studies referring to the performance, management, control, and assistance through TD delivered by dental surgeons (specialized in oral and maxillofacial surgery or members of a multidisciplinary oncology treatment team) to patients with oral and head and neck cancer during the COVID-19 pandemic. The stipulated period for applying the search strategies in the databases was from October 2019 to September 2020, due to the beginning of COVID-19 infection and subsequent pandemic.
Exclusion criteria comprised (1) in vitro studies; (2) studies in animal models; (3) guidelines, abstracts, book chapters, research protocols, and posters; (4) studies evaluating other medical/dental specialties; (5) studies with telemonitoring of other types of primaries cancer; (6) telemonitoring’s studies of other comorbidities (heart failure, chronic obstructive pulmonary disease (COPD), HIV, obstetric disease, asthma, hypertension, diabetes, etc.); (7) studies evaluating the use of TD for telediagnosis; (8) monitoring of oral and head and neck cancers performed by other professionals (otolaryngologists, nurses, etc.); and (9) studies evaluating oral cancer or head and neck cancer with subjects unrelated to TD.
Study selection
The articles’ selection was performed in two phases. In phase 1, two independent reviewers (HECS and GNMS) screened titles and abstracts of all studies, according to the eligibility criteria. In phase 2, both reviewers (HECS and GNMS) independently read the full texts according to the inclusion and exclusion criteria. In case of disagreements, both reviewers discussed and, if consensus was not reached, a third reviewer (AFL) analyzed the studies to reach a final decision.
Data collection process and items
Data extraction by two independent reviewers (HECS and GNMS) was also performed and posteriorly compared. Extracted data comprised author, year, and country; features of users and professionals who use remote technology; security criteria required by remote technology; groups (n*) and treatments; remote technology used or deployed; description of the use of the remote technology adopted; and main conclusions of each paper.
Eligibility
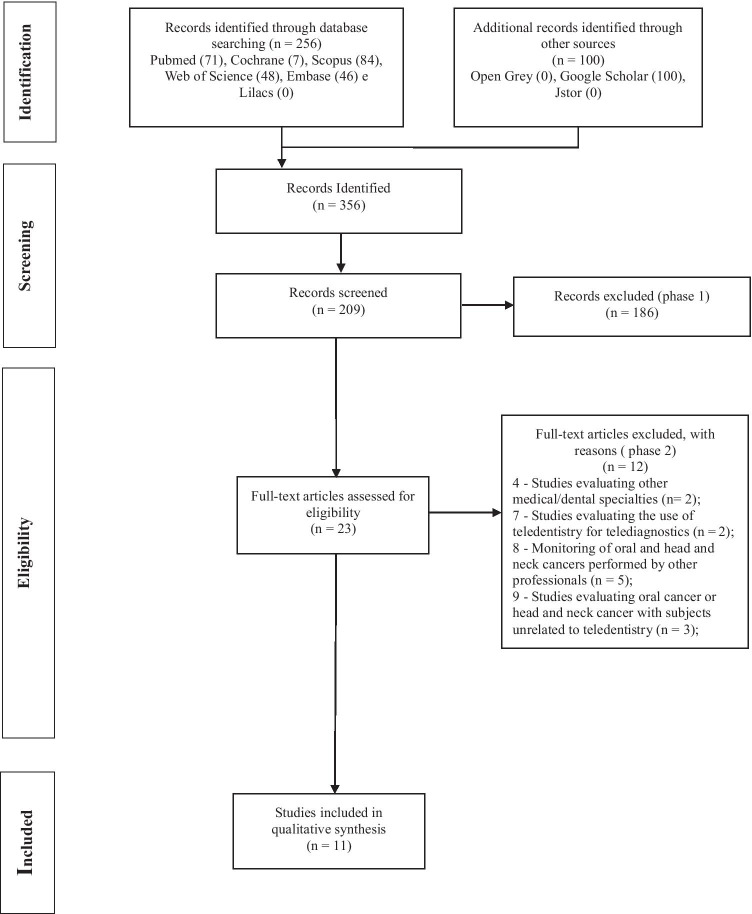
The electronic search of five databases resulted in 356 references. Removal of duplicated studies resulted in 209 references. Titles and abstracts from these studies were read and those not fulfilling the eligibility criteria were excluded. In addition, gray literature was searched. Jstor and Open Grey returned no references. From Google Scholar, the first 100 references were considered for evaluation. At the end of phase 1, 23 studies remained for full-text reading (phase 2). A manual search of reference lists did not provide additional studies. Full-text reading resulted in 11 eligible studies for qualitative analysis. Additional file 2 presents a list of excluded articles and reasons for exclusion. A flowchart of the complete process is shown in Fig. 1.
Fig. 1.
Flow diagram of the integrative review
Assessing the methodological quality of included studies
To assess the methodological quality of the studies, the Joanna Briggs Institute (JBI)—Critical Appraisal Tools (Joanna Briggs Institute, 2014) tools were used [27, 28]. Two review authors (HECS and GNMS) independently assessed the methodological quality of the included studies, using the checklists corresponding to the designs of the included studies, namely JBI critical appraisal checklist for case reports [27] and JBI critical appraisal checklist for Text and Opinion [28]. Disagreements were resolved by discussion and, where necessary, a third review author (AFL) was consulted. Data were extracted from selected articles and the answers were classified using the parameters “yes,” “no,” or “unclear.” “Yes” corresponded to high quality, “no” low quality, and “unclear” unknown or unclear quality.
The purpose of this appraisal is to assess the methodological quality of a study and to determine the extent to which it has addressed the possibility of bias in its design, conduct, and analysis. The results of this appraisal can then be used to inform synthesis and interpretation of the results of the study [27]. Scoring decisions were agreed upon by all reviewers before the critical appraisal commenced, and studies were characterized according to the following: (a) high methodological quality, if studies reached more than 70% scores of “yes”; (b) moderate methodological quality, if “yes” scores were between 50 and 69%; and (c) low methodological quality, if “yes” scores were below 49% [29].
Results
Study characteristics
Included studies were conducted in Brazil [30–32], England [33], Hong Kong [34], Italy [35, 36], India [37], Saudi Arabia [4], and USA [38, 39], all published in English.
Seven references were letters to the editor/editorials [4, 30–33, 36, 37], and four were case reports [34, 35, 38, 39] evaluating the application of remote technologies in the follow-up and monitoring of patients with oral cancer and head and neck cancer during the COVID-19 pandemic. The emphasis was on the mitigation of the evolution, severity, and complexity of the disease in the face of restrictions that the pandemic imposed on health systems. Table 1 summarizes details of studies regarding author, year, and country; features of users (patients) and professionals who used remote technology; security criteria required by remote technology; groups (n*) and treatments; remote technology used or deployed; description of the use of the remote technology adopted; and main conclusions.
Table 1.
Summary of descriptive characteristics of included articles (n = 11)
| Author, year, country | Characteristics of users and/or professionals who use remote technology (n) | Security criteria required by remote technology | Remote technology used or deployed | Description of the use of the remote technology adopted and evidence of management, control and assistance by teledentistry | Main conclusions |
|---|---|---|---|---|---|
| Al-Maweri SA, 2020, Saudi Arabia | Patients already diagnosed with oral potentially malignant disorders (n) | –––- | Zoom, Messenger, and Facebook |
• Scheduling, interview, do clinical examination, and even to conduct oral habits cessation counseling for their patients • Patients can take photographs of their mouths and send them to the dentists at regular intervals • Virtual education regarding clinical signs and risk factors of oral cancer |
During a pandemic other important health issues may be neglected by the public and ignored by the health systems and the dental profession has a role to engage in managing serious health issues such as “detecting oral cancers early” as an ethical responsibility |
| Alves FA, 2020, Brazil | Patients who are undergoing oncological treatment (n) | –––- | –––- |
• Virtual visits have greatly facilitated the provision of oral medicine care and support for both established and new consultations, allowing for effective triage of potentially urgent cases problems requiring immediate clinical attention • Telemedicine/dentistry or telehealth is used to facilitate patient–professional communication and is widely and effectively incorporated into oncology care |
In summary, our group has demonstrated various strategies, often coordinated at the institutional level, to maintain essential oral/dental care for cancer patients during the COVID-19 pandemic. We anticipate that there will be many lessons learned from this experience that will have the potential to improve access to oral medicine care for cancer patients in the future |
| Kanatas A & Rogers SN, 2020, England | Not reported | –––- | Remote telephone consultations accompanied by a questionnaire (PCI-HN) | There is potential merit for members of the head and neck team in using the PCI-HN as part of a telephone review consultation. This would serve to help standardize and guide the consultation, aid multi-professional communication, and avoid missing key issues | The PCI-HN may provide a very useful tool to aid remote consultations, but more clinical evidence is needed in order to ensure that such consultations are optimal for our head and neck patients |
| Barca I et al., 2020, Italy |
Cancer patients (54 males, 36 females, ratio, 1.5:1) Range age overall, 17 to 95 Mean age, 62.15 years 37, resident in Catanzaro 53, from other provinces of Calabria |
Data sent to the examiner’s smartphone using WhatsApp application that uses end-to-end encryption, so the communication by phone is secure The phone to where the photos were sent was only accessible to a small group of professionals through the use of specific authentication credentials The conservation, transmission, and use of patient data were in compliance with the ethical and legal responsibilities of confidentiality and professional secrecy, in full compliance with the General Data Protection Regulation (GDPR) |
WhatsApp or Telegram applications that use end-to-end encryption for telephone messaging The photos taken by the patient or with the help of a direct relative to acquire the following images: (1) a photo of the face and/or neck; (2) a photo of the oral cavity; (3) a photo of the maximum buccal opening with a visible millimeter ruler |
A Group For subgroup A1, the evaluation was carried out through CD visualization, photos taken by the patient or a family member, evaluation of symptoms For subgroup A2, signs of deterioration through the modification of the tissue morphological characteristics were considered; MRONJ -variation of the stage and the presence of infection signs were assessed B Group For both subgroups, the evaluation of the clinical picture was conducted both through the video call, the evaluation of the clinical photos sent and through the display of symptoms Questionnaire of satisfaction 73% found it easy to participate in the consultation, 20% moderate, and 7% difficult 78% prefer telemedicine today, 12% indigenous, and 10% face to face consultation 80% chose the video-phone consultation over the telephone consultation 92% would recommend video calling to others |
Telemedicine represents an excellent opportunity to improve accessibility to oncological and non-oncological treatments. Telemedicine is indicated above all in the follow-up of cancer patients, because they are immunosuppressed for previous chemo/radiation treatments and therefore subject to greater risk of contagion, in chronic as well as urgent visits for suspected malignancy and in patients who live far from a hospital |
| Crispo A et al., 2020, Italy | Cancer patients in IRCCS Fondazione G. Pascale (n) | –––- | E-mail for tests results; careful telephone monitoring symptoms |
• Establishment of waiting rooms for cancer patients Implementation of active surveillance to identify cases earlier, isolating them according to appropriate management and containment procedures • Visits of cancer patients treated with oral anticancer drugs are performed telematically • The first non-urgent visits have been postponed, for fear of contagion by COVID-19 infection • Use of telemedicine as tools in order to plan for personnel, including patient count, a definition of patients who may benefit from this approach and useful to cancer screening programs |
The follow-up of outpatients with telemedicine should be individualized and based on disease severity and initial treatment priorities In this pandemic situation, a multidisciplinary approach for the management of cancer patients should be improved where possible in order to give the most priority to patients, better equilibrating oncologic and COVID-19 needs |
| Kang JJ, et al., 2020, EUA | Cancer patients in Memorial Sloan Kettering Cancer Center (n) | –––- | Multidisciplinary Visits used the Zoom app |
• Radiation department has stopped all endoscopic procedures. Use of PET, CT, and/or magnetic resonance imaging—for radiation planning • No elective dental extractions before radiation • Nonsurgical management is preferred when surgery and Radiation Treatment have equal outcomes • Urgent essential cases may proceed after a rigorous preoperative review and negative preoperative COVID-19 testing. Patients who test positive — reassessed for surgery at a later date • An official swab test is performed, and if it is positive — stop treatment for 10 days and resume treatment if asymptomatic • Patients grateful for telemedicine visits, and no telemedicine-consultation, status-check, or follow-up patients has been requested an in-person visit • The communication with multidisciplinary colleagues by Zoom app is to anticipate barriers, prepare contingency plans, evaluate their efficacy, and refine/revise operations |
With the current global magnitude of the crisis and the immediate challenges of testing and PPE shortages in the USA, telemedicine has been the backbone of our strategy to protect against infection and continue the fight against cancer |
| Lopes MA, 2020, Brazil | Not reported | –––- | –––- |
• Telemedicine is used in remote areas where adequate structure to treat patients is lacking. Is an alternative not only for patient education but also to contribute to diagnosis, and treatment • Results of clinical imaging, radiography, CT, histopathology, and tumor board conferences can be verified via telemedicine • Virtual assistance to patients with cancer and to healthcare professionals, particularly dentists, helps prioritize higher-risk cases, while avoiding face-to-face contact. Only patients with highly suspicious malignant lesions would be referred to the oral medicine team for clinical examination and procedures |
Telemedicine in oral medicine has potential to support clinicians and patients and contribute to reducing unnecessary hospital visits and help preserve the resources for those who need them the most |
| Kochhar AS, 2020, India | Not reported | –––- | Dentists can provide support to patients undergoing radio and/or chemotherapy via telephone and where possible video calls |
• Dentists must motivate and re-emphasize oral hygiene measures • Information about what to anticipate during oncology treatment (such as mucositis, xerostomia, and possible dysgeusia), and actions to extenuate these effects • Counselling about the teeth mineralization before oral hygiene maneuvers become a discomfort and the risk of caries that arises due to dry mouth • The importance of long-term follow-up, especially due caries and osteoradionecrosis. Dental practitioners can request photographs or radiographs in diagnosis and advise home care measures • Constant check-ups, counseling, and support via tele-dentistry consultations to maintain and improve overall well-being of the patients and consequently, QOL |
It is imperative to provide continuous dental care to oral cancer patients, and dentists must ensure that there is no hindrance to the same, while reconsidering traditional treatments in light of the prodigious situation presented by the COVID-19 pandemic, in liaison with the oncologist |
| Lee AKF et al., 2020, Hong Kong | Cancer patients in United Christian Hospital and Tseung Kwan O Hospital |
The Information Technology Department of the Hospital Authority recommended to use the latest version of the Zoom client with a corporate account to enjoy enterprise security features A password should be set for every meeting and the meeting details and password should be exclusively disclosed to participants only The “Lock” function should be enabled the meeting to avoid intrusion |
To accomplish the telemedical sessions, Zoom was adopted Two sessions per week for doctor with six consultations per session Telemedicine sessions —10 min longer when compared with a face-to-face consultation of usually less than 10 min per patient |
• Telemedicine is utilized to reduce patient’s travel and hospital attendance to minimize the risk of cross infection • Telemedicine can provide preoperative counseling, education on postoperative care, dietary advice and exercise recommendations for neck and shoulders. In the postoperative phase, simple wound review and troubleshooting PPE: personnel were kept to a minimum perioperatively for intubation and extubation and for airway operations to reduce contact and conserve PPE • The distribution of priority patients with head and neck cancer between regional ENT units to provide timely surgery Tumors with more aggressive clinical behavior, high tumor volume, and rapid disease progression were prioritized due the possibility progression to airway obstruction requiring an emergency tracheostomy, metastases and higher morbidity and prolonged hospital stay for the patient |
Since the initiation of this multi-institutional collaboration, it has been able to alleviate the number of pending head and neck cancer operations by 20%. Novel methods such as telemedicine and regional collaboration with other centers have been implemented with some success, with plans for further development in the coming months |
| Meurer MI, 2020, Brazil | The State of Santa Catarina has 39 registered oral medicine (OM) specialists (one per 183,700 inhabitants) | The tele(oral)medicine module was implemented in the STT/SC web-based system, complying with the security criteria, according to the Brazilian regulations (i.e., confidentiality/encryption, authenticity, integrity, irrefutability and timestamping) |
The Santa Catarina State Integrated STT/SC offers coverage to 100% of the municipalities, and it integrates primary, secondary, and tertiary healthcare facilities in a single infrastructure Tele(oral)medicine module aggregates a set of functionalities: (a) the collection of clinical data by the dentist at the primary health units, (b) the remote support by a specialist to manage clinical conditions that can be treated at primary healthcare units, and (c) the proper referral of patients to secondary health units |
Dentists at primary healthcare units collect clinical data and images of oral lesions, registering the information via STT/SC portal The OM specialist then evaluates the case and provides a report, indicating the clinical management. When a more serious condition is suspected, an urgency priority is established and face-to-face consultation at a secondary healthcare unit is authorized. Elective cases, during the pandemic, are being monitored at primary healthcare units and being placed on a waiting list |
The telemedicine/telehealth tools are useful to provide clinical and supportive care to patients with oral diseases in these pandemic times. We also believe in the educational potential of the relationships established between professionals through the referral processes of patients, even if they are mediated by interactions at a distance |
| Shanti RM et al., 2020, EUA | Not reported | –––- |
BlueJeans (Mountain View, California) and Doximity (San Francisco, California) as video conferencing platforms |
• Acquisition of medical and dental records: clinical photographs, photographs provided by the patient of the lesion(s); copy of biopsy report(s) •Telehealth consultation: a spatial appreciation of a lesion is achieved and better assessment for cervical lymphadenopathy through video, which adds a degree of human touch to the visit •Determine urgency/timing of in-person visit: our rational for the use of the 3-month time point in low-risk lesions is based on literature •PPE patient SARS-CoV-2 negative: level 3 surgical mask with face shield and/or goggles during the in-person evaluation — patient untested or surgical procedure: N95, face shield, disposable medical safety gown, and disposable working cap • SARS-CoV-2 testing: with regard to testing stewardship, Telehealth evaluation allows for optimization of the efficiency of the in-person visit, evaluate any medications, conditions specials or obtaining any necessary “clearances” •Topical preparation of oral mucosal surfaces with povidone-iodine (PVP-I): the use PVP-I (1–7.5%) for 2 min to inactive SARS coronavirus •Technical considerations for tissue handling: use of either a surgical scalpel or a tissue biopsy technique with avoidance of use of laser due to viral transmission by laser-generated plume, use of absorbable sutures and minimize use of smoking-generating cautery to diminish vaporization of viral particles •Procedure setting: the procedure can be performed in the outpatient clinic setting or in the operating room depending on the status of the SARS-CoV-2 tests, and whether the lesion is easy or difficult to access |
The COVID-19 pandemic has required healthcare practitioners to make novel decisions that are new to us with development of creative pathways of care that focused on patient safety, mitigation efforts, and clinical management of disease processes. The care of patients with OPMDs requires special considerations especially as patients at high risk for severe COVID-19 illness are also higher risk for the development of OPMDs |
Subtitles: STT/SC, Telemedicine and Telehealth System; OC, oral cancer; HNC, head neck cancer; PCI-HN, Patient Concerns Inventory – Head and Neck; IRCCS, Istituto di Ricovero e Cura a Carattere Scientifico; QOL, quality of life; MRONJ, Medication-Related Osteonecrosis of the Jaws; PPE, personal protective equipment; CT, computed tomography; PET, positron emission tomography; SARS-CoV-2, severe acute respiratory syndrome coronavirus 2; PVP-I, povidone-iodine; OPMD, oral potentially malignant disorders
Overview of the findings
Oral cancer patients have a complex demand for care. Many of these demands include the dental procedures prior to cancer treatment, management, and prevention of side effects linked to cancer treatment, such as mucositis, infections, complications related to jaw osteonecrosis, uncontrolled pain, and follow-up of the patient after the treatment in control over time. The social distancing and the need generated by the COVID-19 pandemic to remain at home generated a difficulty in conducting face-to-face consultations, which leads to the possibility of delay in the treatment of patients with oral cancer. TD emerges as an alternative to this demand, which is urgent given the current situation of social isolation [4, 31, 37].
The studies were divided into four categories, accordingly with the theme related to TD, as follows: (1) virtual visits, (2) use of remote technology, (3) patient’s satisfaction, and (4) multidisciplinary approach in teledentistry.
Virtual visits
Some authors have observed that dentists may carry out virtual visits for follow-up, interviews, and clinical examinations with the guidance of oral habits for their patients [4, 37]. Two authors verified that patients could take photographs and copy of biopsy report [35, 39] of the mouth and refer them to the dentist to manage the evolution of the lesion. According to the authors, this also allows the control of the virtual education of the patients about the clinical signs and risk factors of oral cancer, through valid and reliable websites, reducing anxiety with information available in the common media [4, 37] and a spatial appreciation of in some oral lesions through using the mobile phone light, allowing the humanization of the virtual visit [39].
The authors found that virtual visits are an alternative to providing oral medicine care with the effective screening of potentially urgent cases. Teleassistance promotes better patient–professional communication before, during and after cancer care [31] to maintain and improve patient’s quality of life [37]. The authors believe that the assistance of the virtual visit to cancer patients could help to prioritize the ones with highly suspected malignant lesions, avoiding face-to-face contact, with referral for clinical examination and appropriate procedures [31, 32].
In another strategy evaluated in a study conducted at a hospital in Hong Kong, the authors realized that virtual visits could monitor the use of medications, thus reducing patient’s hospital attendance to minimize the risk of cross infection [34]. Thus, the authors recommended, according to the complexity of each case, that follow-up consultations of cancer patients undergoing treatment with oral antineoplastic drugs should be carried out telematically [36]. TM can provide preoperative counseling, education on postoperative care, dietary advice, and exercise recommendations for neck and shoulders. In the postoperative phase: simple wound review and troubleshooting [34].
Use of remote technology
Several remote technologies were used by included studies to conduct TD consultations. In a research [33], the author perceived that the telephone is one of the easiest alternatives and can be associated with a structured guide, as the PCI-HN (a list of items rather than questions that facilitates communication over the phone). The aim is to help standardize and guide consultation, assist multiprofessional communication, and prevent the loss of relevant information. The advantage is the reduction of face-to-face consultations in order to limit the spread of COVID-19 and protect patients and clinical staff, reduce travel costs for patients to the hospital and support providers to focus on a particular location, and carry out the consultations by less experienced staff members and the PCI-HN allows doctors to continue working at home.
In a study [34] conducted in Hong Kong, the authors used video conference applications like Zoom app for virtual consultations to avoid constant rescheduling of face-to-face consultations. The authors recommended to use the latest version of the Zoom client with a corporate account to enjoy enterprise security features, setting a password for every meeting and the “Lock” function enabled to avoid meeting intrusion.
In a study [30] conducted in the state of Santa Catarina, Brazil, the authors used TD models to increase the coverage of oral oncology services. The Santa Catarina State Integrated Telemedicine and Telehealth System (STT/SC) serves 100% of the municipalities, and it integrates primary, secondary, and tertiary healthcare facilities in a single infrastructure. This module has the functions of collecting clinical data by the dentist at the primary health units, providing remote support by a specialist to manage the clinical conditions that can be treated in primary healthcare units, and promoting appropriate referral of patients to secondary health units, complying with the security criteria, according to the Brazilian regulations.
Patient’s satisfaction
In a study [35] conducted at the University of Catanzaro, Italy, regarding patient satisfaction with the use of TD, the authors observed that, in a sample of 90 patients, 73% considered as easy to participate in the consultation, 20% moderate, and 7% difficult. TD was the patients’ preferred type of consultation (78%), followed by indigenous (12%) and face-to-face appointment (12%). Eighty percent of patients preferred videophone over the telephone examinations, and 92% would recommend video calling to others. Patients were often very grateful for TD visits, and no TD consultation has requested a visit in person for status verification or follow-up [38].
Multidisciplinary approach in TD
Three studies [34, 37, 38] indicated that communication with colleagues in a multidisciplinary way is essential to anticipate barriers, prepare contingency plans, evaluate their effectiveness, and refine/review operations as needed. Multidisciplinary tumor councils, academic meetings, or multidisciplinary tumor board meetings can meet regularly via applications, such as Zoom, which guarantees communication, compensation, and consensus for optimal patient care during the pandemic. However, one author [34] highlighted another way of multidisciplinary approach, the collaboration in the distribution of priority patients with head and neck cancer between different regional units to provide timely surgery, optimizing treatment during the pandemic.
Table 2 shows the summary of the benefits of using TD to monitor patients with oral and head and neck cancer.
Table 2.
Benefits of using teledentistry in select studies
| Thematic category | Evidence of the benefits of using teledentistry |
|---|---|
| Virtual visits |
- Allow to monitor the use of medications reducing patient’s hospital attendance to minimize the risk of cross infection [34, 37] - Provide preoperative counseling, education on postoperative care, dietary advice and exercise recommendations for neck and shoulders. In the postoperative phase: simple wound review and troubleshooting [34, 37] - Provide oral medicine care to potentially urgent cases with highly suspected malignant lesions [35, 36] - Allow follow-up, interviews, clinical examinations with the guidance of oral habits, control of the virtual education of the patients about the clinical signs and risk factors of oral cancer, reduce anxiety with information available in the common media, and permit a spatial appreciation of a lesion through video for their patients [4, 36, 40] - Promote better patient–professional communication before, during and after cancer care to maintain and improve patient’s quality of life [35, 36] - Management by the dentist of the evolution of the lesions through the use of photographs and copies of the biopsy reports of the mouth sent by the patients in virtual consultations [33] |
| Use of remote technology |
- Teledentistry is used to evaluate results of clinical imaging, radiography, computed tomography, and histopathology tests and carry out tumor board conferences [39] - Teledentistry for patients with cancer and to healthcare professionals, particularly dentists, helps prioritize higher-risk cases, while avoiding face-to-face contact [39] - The use of telephone associated or not with a structured guide, video conference applications like Zoom app and TD’s integrated models to increase the coverage of oral oncology services used for TD’s consultations [31, 32, 34] |
| Patient’s satisfaction |
- High rate of patient’s satisfaction with the use of teledentistry with 98% ease of use, with the use of video phones being chosen by 98% of patients and 92% would recommend video calling to others [33, 38] - Patients grateful for TD’s visits, and no TD’s consultation has requested a visit in person for status verification or follow-up [33, 38] |
| Multidisciplinary approach in teledentistry |
- Multidisciplinary action through the collaboration between different regional units to provide timely surgery was made possible, optimizing treatment during the pandemic [34, 37, 38] - Communication with colleagues in a multidisciplinary way through multidisciplinary tumor councils, academic meetings, or multidisciplinary tumor board meetings via applications such as Zoom [34] |
Methodological quality assessment among studies
None of the studies fulfilled all methodological quality criteria. However, the overall average of “yes” answers of the studies was 80%, and most assessed high quality. Only one study [38] was considered to be of moderate quality and one [39] to be of low methodological quality.
None of the studies [4, 30–33, 36, 37] assessed by the text and opinion checklist showed any inconsistency with the logically defended literature/sources.
Regarding the evaluation of the Methodological quality tool for Case Reports, two studies [38, 39] did not present patients’ demographic characteristics described clearly. Three studies [32, 35, 36] did not show patients’ history described clearly and presented as a timeline. Two studies [35, 39] were unclear for the post-intervention clinical condition and for diagnostic tests or assessment methods, respectively, and two studies [38, 39] did not clearly report the demographics of the participants. More information on methodological quality can be found in Table 3 (summarized assessment).
Table 3.
Evaluation of methodological quality according to the design of the study (n = 11)
| Study | Methodological quality assessed | Total (% score yes) | Methodological quality | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Q1 | Q2 | Q3 | Q4 | Q5 | Q6 | Q7 | Q8 | |||
| Barca I (2020) | Y | N | Y | Y | Y | U | Y | Y | 75% | High |
| Kang JJ, et al. (2020) | N | N | N | Y | Y | Y | Y | Y | 62,50% | Moderate |
| Lee AKF (2020) | Y | N | Y | Y | Y | N | Y | Y | 75% | High |
| Shanti RM et al. (2020) | N | N | Y | U | Y | N | N | Y | 37,50% | Low |
| Al-Maweri SA (2020) | Y | Y | Y | Y | Y | N | – | – | 83,33% | High |
| Alves FA (2020) | Y | Y | Y | Y | Y | N | – | – | 83,33% | High |
| Crispo A et al. (2020) | Y | Y | Y | Y | Y | N | – | – | 83,33% | High |
| Kanatas A (2020) | Y | Y | Y | Y | Y | N | – | – | 83,33% | High |
| Kochhar AS (2020) | Y | Y | Y | Y | Y | N | – | – | 83,33% | High |
| Lopes MA (2020) | Y | Y | Y | Y | Y | N | – | – | 83,33% | High |
| Meurer MI (2020) | Y | Y | Y | Y | Y | N | – | – | 83,33% | High |
Note: For Case Reports — (Q1) Were patient’s demographic characteristics clearly described? (Q2) Was the patient’s history clearly described and presented as a timeline? (Q3) Was the current clinical condition of the patient on presentation clearly described? (Q4) Were diagnostic tests or assessment methods and the results clearly described? (Q5) Was the intervention(s) or treatment procedure(s) clearly described? (Q6) Was the post-intervention clinical condition clearly described? (Q7) Were adverse events (harms) or unanticipated events identified and described? (Q8) Does the case report provide takeaway lessons?
For Text and Opinion — (Q1) Is the source of the opinion clearly identified? (Q2) Does the source of opinion have standing in the field of expertise? (Q3) Are the interests of the relevant population the central focus of the opinion? (Q4) Is the stated position the result of an analytical process, and is there logic in the opinion expressed? (Q5) Is there reference to the extant literature? (Q6) Is any incongruence with the literature/sources logically defended?
Abbreviations: N, no; U, unclear; Y, yes
Discussion
This IR evaluated the management, control, and assistance, through TD, of patients with oral and head and neck cancer during the COVID-19 pandemic. The aim was to assess the benefits of the use of TD for patients undergoing treatment of oral and head and neck cancer during the COVID-19 pandemic. Included studies showed that TD applied to the monitoring of patients with oral cancer and head and neck cancer was a useful tool in supporting patients during this pandemic period, with improved general well-being and quality of life.
As a remote technology for monitoring patients with oral and head and neck cancer, TD was well accepted by patients and professionals in preliminary studies. The benefits presented in this review are the continuity of dental care, reduced travels to the hospital for patient care, reduced risk of infection with the coronavirus, and limitation of face-to-face consultations to protect health professionals, among others.
Three studies discussed concerns on the safety of data exchanging between professionals and patients during the use of TD, either with a TeleHealth system [30], by Zoom video conference [34], or messaging applications like WhatsApp [35]. Photos and image encryption restrictions of people’s access to smartphones, and count corporate applications were used to increase the exchange data security [30, 35] while following the legislation regarding the guarantee of data privacy [30, 34].
TD has advantages not only during the COVID-19 pandemic because it reaches other aspects of dental care, benefiting patients in different situations. When providing low-cost, large-scale specialist support to primary public healthcare units, TD guarantees access to technology by low-income people, which optimizes care, reduces the waiting time for an appointment, and increases the resolution of the clinical case [30].
Activities such as further preoperative counseling, education of postoperative care, dietary advice, and neck and shoulder exercise recommendations could all be delivered by TD. In the postoperative phase, simple wound review and troubleshooting could also be performed [34]. The TM is well accepted especially by the patients residing in areas rather far from the health units, who had to travel a long way and, above all, be exposed to other patients who could be carriers of COVID-19 and other infectious agents [35]. It can be pointed out as advantages of TD the reduced face-to-face consultations to limit the spread of COVID-19 and protect the patients and the clinical teams. The consultations may be completed by less experienced members of the team including use in the nurse-led clinics. Consequently, experienced staff would become free to aid clinical and workforce planning in other pressure points [33].
The introduction of the telemedicine service is considered very beneficial, especially in terms of patient triage. The interruption of dental activities by health authorities leads to a decrease in the care of oncological patients who need treatment, focusing only on emergencies. There is a significant reduction in dental care, periodontal maintenance, and patient care at the oral disease clinic. However, this decrease is gradually offset by the growing telemedicine service. In this context, there is an increase in patient abstention from attending consultations to avoid the risk of infection. This fact is accentuated by restrictive measures by health authorities to protect patients at risk and staff. After an average period of 4 weeks of minimal activity, an increase in the flow of patients is observed, probably due to the increased demand for emergency dental treatment, despite the increasing number of active COVID‐19 patients and related deaths during the pandemic [40].
However, TD in monitoring patients with oral cancer and head and neck cancer presents challenges that need to be overcome. The lack of acceptance of TD by the dentists can be attributed to the fact that they may find it complex and may be resistant to new skills acquisition demand [41, 42]. They may be technologically challenged, afraid of making an inaccurate case evaluation, and concerned about increased costs and expenses. There may be constraints related to infrastructure, as poor internet access, shortage of hardware, lack of training, and lack of technical support and expertise. Organizational incompatibility of TD with the healthcare system, insufficient financial reimbursement, inadequate guidelines in coordination between remote and core center, and high cost of setup are other challenges related to its acceptance by dentists [42].
Two-dimensional representation of lesions and inability to perform tests like palpation, percussion, and auscultation are other limitations [25]. Even with imaging technology, it may be challenging to visualize certain mucosal areas [43]. Some professionals reported that they were not satisfied making a diagnosis using telecommunication images without clinical information. Access to patient information is one of the main limitations that could affect the validity of TD. Face-to-face examinations provide an opportunity to talk with patients to obtain information essential to diagnosis. Lack of information could decrease the dental professional’s confidence in making a diagnosis using only a TD system and therefore diminishes the validity score of TD [26].
There is a difference between the benefits of using TD and the face-to-face clinical examination. Oral lesions, especially those with the potential for malignancy, are not effectively monitored by TD alone. In these situations, TD has the potential to ensure only a temporary adjustment until the clinical examination is possible to be performed in person.
In the case of the lack of acceptance of TD by patients, the difficulty of face-to-face communication may lead patient apprehension regarding the inadequacy of proper communication of their problems to their dentists. Elderly patients, for example, may experience technology anxiety, isolation, feelings of neglect and fears, and difficulties regarding the delay in cancer treatment and access to support services during this pandemic period. Acceptability of TD by the patients will increase in parallel with the acceptability of telemedicine in general, which is increasing day-by-day [33, 44].
Two studies inferred the role of TD in the context of multi-professional and multi-institutional collaboration in monitoring patients with oral cancer and head and neck cancer. TD plays a decisive role in reducing the risk of spreading COVID-19. In this period of health emergency, the treatment of head and neck cancer [35] has shown a multidisciplinary approach (maxillofacial surgeon, radiotherapist, oncologist, nutritionist, etc.), through the involvement of other specialists in the videoconference and/or photography. It should be noted that novel methods, such as TD and regional collaboration with other centers, have been implemented with some success, in order to achieve the targeted waiting times to arrange early surgery for more urgent cases in different hospitals with a relief of the number of pending head and neck cancer operations by 20% [34, 36, 38].
Two studies presented patient’s satisfaction with the use of remote technology in the debate between TD and the monitoring of cancer patients. It should be highlighted that constant check-ups, counseling, and support can be performed through TD consultations to maintain and improve the general well-being of patients and, consequently, quality of life [37]. The high percentage of satisfaction that emerged from the analysis of the satisfaction questionnaires administered to the patient shows that TD was well accepted. Above contact, although remotely, has positively influenced the patient’s state of well-being, motivation, and sense of security, especially in this uncertain period [35].
These preliminary data corroborate current literature, suggesting a high satisfaction from both healthcare staff and service users [43, 45]. It can not only aid patient education but also contribute to diagnosis and treatment [32] in association with a possible face-to-face consultation for a definitive diagnosis, when necessary. There are limitations to real-time interactive video consultations in diagnosing disease and assessing patient problems, particularly in a dental context. The TD model has some limitations, such as the inability to approach texture and clearly delineate the borders of a lesion, particularly in the posterior oral cavity, with an unreliable data connection and poor image quality. Factors linked to the patient, such as the ability to connect to the software, lighting, manual dexterity, familiarity with mobile/tablet devices, and the knowledge of the service user to attend technology-based consultations. Due to these considerations, video conferencing has a limited role and should be used with care [35, 46].
The accessibility of oral cavity to user-friendly imaging devices makes telemedicine an appealing solution for the management of secondary lesions as oral mucositis. Given the popularity of mobile phone-integrated cameras, the idea of obtaining images of the oral surfaces seems feasible; however, the quality of these photos does not enable us to apply this concept universally [47].
As a limitation in carrying out the IR, it is possible to point out the few existing studies in the literature correlating TD and the monitoring of patients with oral cancer and head and neck cancer, both in the direct care of dental complications during cancer treatment and by aggravation caused by the cancer treatment itself. It is suggested that professionals involved and monitoring the quality of life of patients throughout cancer treatment carry out studies with a greater emphasis on the use of remote technology aimed at dentistry with the assessment of patient satisfaction, as a way of verifying the effectiveness of the use of TD.
Conclusion
TD, as a remote technology for monitoring patients with oral and head and neck cancer, is well accepted by patients and professionals in preliminary studies. The benefits presented in this IR are the continuity of dental health monitoring, reduced travel for patient care in the hospital, reduced risk of infection with the coronavirus, and limitation of face-to-face consultations to protect health professionals, among others. Nevertheless, this alternative of care presents many challenges, such as the lack of acceptance of TD by the dentists, fear of making an inaccurate diagnosis, concerns about increased costs, expenses, and necessary infrastructure, insufficient financial reimbursement, and inadequate guidelines. For the patients, the technology anxiety, isolation, feelings of neglection and fears, difficulties regarding the delay in cancer treatment, and access to support services during the COVID-19 pandemic should be considered. It is emphasized that studies with more robust scientific evidence are necessary to consolidate the benefits of using remote technologies for monitoring as a viable alternative for the monitoring of cancer patients.
Supplementary Information
Below is the link to the electronic supplementary material.
Author contribution
Helbert Silva and Glaucia Santos together with André Leite, Carla Mesquita, Paulo Figueiredo, Paula Reis, Cristine Stefani, and Nilce Melo conceived and designed the study. Helbert Silva and Glaucia Santos performed acquisition of data, analysis, and interpretation of data and, together with André Leite, Carla Mesquita, and Paulo Figueiredo, and performed drafting and critical revision of the manuscript for important intellectual content. André Leite, Carla Mesquita, and Paulo Figueiredo gave administrative-technical or material support. Paula Reis, Cristine Stefani, and Nilce Melo provided oversight during all manuscript writing process. Cristine Stefani and Nilce Melo revised it critically for content, and all authors approved the final version.
Availability of data and material
Not applicable.
Code availability
Not applicable.
Declarations
Conflict of interest
The authors declare no competing interests.
Ethics approval
Not applicable.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Helbert Eustáquio Cardoso da Silva, Email: helbertcardososilva@gmail.com.
Glaucia Nize Martins Santos, Email: nize.gal@gmail.com.
André Ferreira Leite, Email: andreleite@unb.br.
Carla Ruffeil Moreira Mesquita, Email: ruffeilcarla@gmail.com.
Paulo Tadeu de Souza Figueiredo, Email: paulofigueiredo@unb.br.
Paula Elaine Diniz dos Reis, Email: pauladiniz@unb.br.
Cristine Miron Stefani, Email: cmstefani@gmail.com.
Nilce Santos de Melo, Email: nilce@unb.br.
References
- 1.WHO (2020) https://www.who.int/emergencies/diseases/novel-coronavirus-2019. Accessed on 10/11/2020.
- 2.Vargas M, Servillo G. Improving staff safety during tracheostomy in COVID-19 patients. Head Neck. 2020;42(6):1278–1279. doi: 10.1002/hed.26163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Peng X, Xu X, Li Y, Cheng L, Zhou X, Ren B. Transmission routes of 2019-nCoV and controls in dental practice. Int J Oral Sci. 2020;12(1):9. doi: 10.1038/s41368-020-0075-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.AL-Maweri SA, Halboub E, Warnakulasuriya S, Impact of COVID-19 on the early detection of oral cancer: a special emphasis on high risk populations. Oral Oncology. 2020;106:104760. doi: 10.1016/j.oraloncology.2020.104760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China summary of a report of 72 314 cases from the Chinese Center for Disease Control and Prevention. JAMA. 2020;323(13):1239–1242. doi: 10.1001/jama.2020.2648. [DOI] [PubMed] [Google Scholar]
- 6.Liang W, Guan W, Chen R, et al. Cancer patients in SARS-CoV-2 infection: a nationwide analysis in China. Lancet Oncol. 2020;21:335–337. doi: 10.1016/S1470-2045(20)30096-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.US Centers for Disease Control and Prevention. Healthcare facilities: preparing for community transmission (2020) https://www.cdc.gov/coronavirus/2019-ncov/healthcare-facilities/guidance-hcf.html. Accessed on 10/11/2020.
- 8.American College of Surgeons. COVID-9 guidelines for triage of cancer surgery patients (2020) https://www.facs.org/covid-19/clinical-guidance/elective-case/cancer-surgery. Accessed on 10/11/2020.
- 9.COVID-19: guidance for triage of non-emergent surgical procedures (2020) https://www.facs.org/about-acs/covid-19/information-for-surgeons/triage. Accessed on 10/11/2020.
- 10.New recommendations regarding urgent and nonurgent patient care (2020) https://www.entnet.org/content/new-recommendations-regarding-urgent-and-nonurgent-patient-care-0. Accessed on 10/11/2020.
- 11.American Society for Therapeutic Radiation Oncology. COVID‐19 recommendations and information (2020) https://www.astro.org/Daily-Practice/COVID-19-Recommendations-and-Information/Summary. Accessed on 10/11/2020.
- 12.American Society of Clinical Oncology. ASCO coronavirus resources (2020) https://www.asco.org/asco-coronavirus-information. Accessed on 10/11/2020.
- 13.Givi B, Schiff BA, Chinn SB, et al. Safety recommendations for evaluation and surgery of the head and neck during the COVID-19 pandemic. JAMA Otolaryngol Head Neck Surg. 2020;146(6):579–584. doi: 10.1001/jamaoto.2020.0780. [DOI] [PubMed] [Google Scholar]
- 14.AAO-HNS Telemedicine Committee. Prioritizing novel approaches to telehealth for all practitioners (2020) https://www.entnet.org/content/prioritizing-novel-approaches-telehealth-all-practitioners. Accessed on 10/11/2020.
- 15.AHNS Leadership and Patient Care Division. How COVID-19 is affecting our head and neck community. https://www.ahns .info/covid-19–2020/. Accessed on 10/11/2020.
- 16.Yanik EL, Katki HA, Silverberg MJ, Manos MM, Engels EA, Chaturvedi AK. Leukoplakia, oral cavity cancer risk, and cancer survival in the U.S elderly. Cancer Prev Res. 2015;8(9):857–863. doi: 10.1158/1940-6207.CAPR-15-0091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Villa A, Sankar V, Shiboski C (2020) Tele(oral)medicine: a new approach during the COVID-19 crisis Oral Dis 20 10.1111/odi.13364.10.1111/odi.13364 [DOI] [PMC free article] [PubMed]
- 18.Hollander JE, Carr BG. Virtually perfect? Telemedicine for COVID-19. N Engl J Med. 2020;382(18):1679–1681. doi: 10.1056/NEJMp2003539. [DOI] [PubMed] [Google Scholar]
- 19.Cain SM, Moore R, Sturm L, et al. Clinical assessment and management of general surgery patients via synchronous telehealth. J Telemed Telecare. 2017;23:371–375. doi: 10.1177/1357633X16636245. [DOI] [PubMed] [Google Scholar]
- 20.Ghorbani M, Mohammadi E, Aghabozorgi R, Ramezani M. Spiritual care interventions in nursing: an integrative literature review. Support Care Cancer. 2021;29(3):1165–1181. doi: 10.1007/s00520-020-05747-9. [DOI] [PubMed] [Google Scholar]
- 21.Mendes KDS, Silveira RCCP, Galvão CM. Revisão integrativa: método de pesquisa para a incorporação de evidências na saúde e na enfermagem. Texto contexto - enferm. 2008;17(4):758–764. doi: 10.1590/S0104-07072008000400018. [DOI] [Google Scholar]
- 22.Page MJ, McKenzie J, Bossuyt P, Boutron I, Hoffmann T, Mulrow C, et al (2020) The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. 10.31222/osf.io/v7gm2 [DOI] [PMC free article] [PubMed]
- 23.Huang EY, Knight S, Guetter CR, et al. Telemedicine and telementoring in the surgical specialties: a narrative review. Am J Surg. 2019;218(4):760–766. doi: 10.1016/j.amjsurg.2019.07.018. [DOI] [PubMed] [Google Scholar]
- 24.Khan SA, Omar H. Teledentistry in practice: literature review. Telemed J E Health. 2013;19(7):565–567. doi: 10.1089/tmj.2012.0200. [DOI] [PubMed] [Google Scholar]
- 25.Estai M, Kanagasingam Y, Tennant M, Bunt S. A systematic review of the research evidence for the benefits of teledentistry. J Telemed Telecare. 2018;24(3):147–156. doi: 10.1177/1357633X16689433. [DOI] [PubMed] [Google Scholar]
- 26.Alabdullah JH, Daniel SJ. A systematic review on the validity of teledentistry. Telemed J e Health. 2018;24:639e48. doi: 10.1089/tmj.2017.0132. [DOI] [PubMed] [Google Scholar]
- 27.Joanna Briggs Institute (2017) JBI critical appraisal checklist for case series. Adelaide, SA: The Joanna Briggs Institute; Available from: https://joannabriggs.org/sites/default/files/2019-05/JBI_Critical_ Appraisal-Checklist_for_Case_Reports2017_0.pdf . Accessed on 10/11/2020.
- 28.Joanna Briggs Institute (2017) JBI critical appraisal checklist for Text and Opinion. Adelaide, SA: The Joanna Briggs Institute; Available from: https://joannabriggs.org/sites/default/files/2019-05/JBI_Critical_Appraisal-Checklist_for_Text_and_Opinion2017_0.pdf . Accessed on 10/11/2020.
- 29.Polmann H, Melo G, Conti Réus J, Domingos FL, de Souza BDM, Padilha AC, Duque TM, Porporatti AL, Flores-Mir C, De Luca CG. Prevalence of dentofacial injuries among combat sports practitioners: a systematic review and meta-analysis. Dent Traumatol. 2020;36(2):124–140. doi: 10.1111/edt.12508. [DOI] [PubMed] [Google Scholar]
- 30.Meurer MI, von Wangenheim A, Zimmermann C, Savaris A, Petrolini VA, Wagner HM. Launching a public statewide tele(oral)medicine service in Brazil during COVID-19 pandemic. Oral Dis. 2020 doi: 10.1111/odi.13528.10.1111/odi.13528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Alves FA, Saunders D, Sandhu S, Xu Y, Mendonça NF, de Treister NS (2020) Implication of COVID-19 in oral oncology practices in Brazil, Canada, and the United States Oral Dis 10.1111/odi.13493.10.1111/odi.13493 [DOI] [PMC free article] [PubMed]
- 32.Lopes MA, Santos-Silva AR, Vargas PA, Kowalski LP. Virtual assistance in oral medicine for prioritizing oral cancer diagnosis during the COVID-19 pandemic. Oral Surg Oral Med Oral Pathol Oral Radiol. 2020;130(1):127–128. doi: 10.1016/j.oooo.2020.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kanatas A, Rogers SN. The role of the Head and Neck cancer-specific Patient Concerns Inventory (PCI-HN) in telephone consultations during the COVID-19 pandemic. Br J Oral Maxillofac Surg. 2020;58(5):497–499. doi: 10.1016/j.bjoms.2020.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lee AKF, Cho RHW, Lau EHL, et al. Mitigation of head and neck cancer service disruption during COVID-19 in Hong Kong through telehealth and multi-institutional collaboration. Head Neck. 2020;42(7):1454–1459. doi: 10.1002/hed.26226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Barca I, Novembre D, Giofrè E, et al. Telemedicine in oral and maxillo-facial surgery: an effective alternative in post COVID-19 pandemic. Int J Environ Res Public Health. 2020;17(20):7365. doi: 10.3390/ijerph17207365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Crispo A, Montagnese C, Perri F, et al. COVID-19 emergency and post-emergency in Italian cancer patients: how can patients be assisted? Front Oncol. 2020;10:1571. doi: 10.3389/fonc.2020.01571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kochhar AS, Bhasin R, Kochhar GK, Dadlani H. Provision of continuous dental care for oral oncology patients during & after COVID-19 pandemic. Oral Oncol. 2020;106:104785. doi: 10.1016/j.oraloncology.2020.104785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kang JJ, Wong RJ, Sherman EJ, et al. The 3 Bs of cancer care amid the COVID-19 pandemic crisis: “be safe, be smart, be kind”-a multidisciplinary approach increasing the use of radiation and embracing telemedicine for head and neck cancer. Cancer. 2020;126(18):4092–4104. doi: 10.1002/cncr.33031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Shanti RM, Stoopler ET, Weinstein GS, et al. Considerations in the evaluation and management of oral potentially malignant disorders during the COVID-19 pandemic. Head Neck. 2020;42(7):1497–1502. doi: 10.1002/hed.26258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Umansky Sommer M, Davidovitch T, Platner O, Inerman A, Yarom N. The effect of COVID-19 pandemic on oral medicine services in a tertiary referral center. Oral Dis. 2020 doi: 10.1111/odi.13417.10.1111/odi.13417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Smith AC, Thomas E, Snoswell CL, et al. Telehealth for global emergencies: implications for coronavirus disease 2019 (COVID-19) J Telemed Telecare. 2020;26(5):309–313. doi: 10.1177/1357633X20916567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Estai M, Kruger E, Tennant M, Bunt S, Kanagasingam Y. Challenges in the uptake of telemedicine in dentistry. Rural Rem Health. 2016;16(4):3915. [PubMed] [Google Scholar]
- 43.Mair F, Whitten P. Systematic review of studies of patient satisfaction with telemedicine. BMJ. 2000;320(7248):1517–1520. doi: 10.1136/bmj.320.7248.1517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Petcu R, Kimble C, Ologeanu-Taddei R, Bourdon I, Giraudeau N. Assessing patient’s perception of oral teleconsultation. Int J Technol Assess Health Care. 2017;33(2):147–154. doi: 10.1017/S0266462317000319. [DOI] [PubMed] [Google Scholar]
- 45.Layfield E, Triantafillou V, Prasad A, et al. Telemedicine for head and neck ambulatory visits during COVID-19: evaluating usability and patient satisfaction. Head Neck. 2020;42(7):1681–1689. doi: 10.1002/hed.26285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Patel T, Wong J. The role of real-time interactive video consultations in dental practice during the recovery and restoration phase of the COVID-19 outbreak. Br Dent J. 2020;229(3):196–200. doi: 10.1038/s41415-020-1918-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Bonomo P, Elad S, Kataoka T, Bossi P. Mucositis Study Group of MASCC/ISOO. The impact of the COVID-19 outbreak on supportive care for oral mucositis: current concepts and practice. Support Care Cancer. 2021;4:1–4. doi: 10.1007/s00520-020-05966-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Russo JE, McCool RR, Davies L. VA telemedicine: an analysis of cost and time savings. Telemed J E Health. 2016;22(3):209–215. doi: 10.1089/tmj.2015.0055. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Not applicable.
Not applicable.