Abstract
Background
Data from Africa regarding sudden and unexpected COVID-19 community deaths and underlying pathological, demographic, and co-morbidity features require definition.
Methods
We performed a case series of COVID-19-related deaths seen at Forensic Post-Mortem examination of sudden and unexpected Community Deaths in Lusaka, Zambia, Africa. Whole-body Post-Mortem examinations were performed according to Standard Operating Procedures. Patient demographics, history, co-morbidities, pathological gross and microscopic findings, and cause(s) of death were recorded. Variables were grouped as frequencies and percentages. Comparison of data was made with autopsy findings of hospital COVID-19 deaths.
Findings
Of 21 COVID-19 decedents, 14/21 (66.7%) were male; 18/21, (85.7%) were below 55 years of age (mean age, 40 ± 12.3; range, 20-73). The median duration of symptoms was 1 day (range 0-2); 9/21 (42.9%) had co-morbidities, with hypertension and obesity being the most common. Main post-mortem findings were diffuse alveolar damage (DAD) (80.9%), saddle and shower emboli (38.1%, respectively), and pneumonia (14.3%). Pulmonary thromboembolism (76.2%), DAD (14.3%), and SARS-CoV-2 pneumonia (9.5%) were common causes of death.
Conclusions
COVID-19 is an important cause of death to consider in forensic investigations of sudden and unexpected community deaths. Risk factors for the younger age of COVID-19 deaths and thromboembolism need to be identified.
Keywords: Forensic, SARS-CoV-2, COVID-19, Lusaka-Zambia, Africa, community deaths, post-mortem examination
INTRODUCTION
As of June 30th, 2021, the ongoing SARS-CoV-2 pandemic has resulted in 180 million COVID-19 cases (with 3.9 million deaths) reported to the World Health Organisation (WHO). Of these, 5.4 million cases with 141,000 deaths have been reported from Africa (WHO Afro 2021). Currently, 150,000 COVID-19 cases have been recorded in Zambia, with 2,100 deaths (WHO COVID-19 dashboard – Zambia 2021).
A large number of COVID-19 deaths occurring on all continents (WHO Afro 2021) have been reported from hospitals or residential care facilities. Many of these had underlying co-morbid health conditions. While there have some reports of community deaths in people known to have COVID-19 in residential facilities in western countries (Youd and Moore, 2020), there are insufficient clinical, pathological, and co-morbidity data on sudden deaths due to COVID-19 in communities from Africa. There have been repeated calls for more accurate accounting of unexpected deaths attributable to COVID-19 from Africa, where other killer infectious diseases such as TB and HIV are also prevalent (Youd and Moore, 2020). Our Office of the State Forensic Pathologist (OSFP) performs post-mortem examinations of sudden and unexpected deaths in the community and hospitals, and an evaluation of these has identified some cases as COVID-19 deaths (Mucheleng'anga and Himwaze, 2020, Mucheleng'anga and Himwaze, 2021, Himwaze et al., 2021).
We conducted a case series analyses of whole-body post-mortem examinations of COVID-19 related deaths seen at forensic post-mortem examinations we had performed on sudden and unexpected community deaths in Lusaka, Zambia, Africa. A comparisionof the clinical, pathologic and co-morbidity data from these COVID-19 community deaths was made with a whole-body post-mortem case series of COVID-19 inpatient hospital deaths in Lusaka, Zambia was made (Mucheleng'anga and Himwaze, 2021).
MATERIAL AND METHODS
Ethics and Permission
The coroner gave authority to conduct the forensic post-mortem examinations through an Order for Postmortem Examination of sudden and unexpected deaths in the community. Forensic post-mortem are mandated by law; thus, no consent or ethical permission is required to conduct the post-mortem examination. Data from these post-mortemexaminations are stored at the Office of the State Forensic Pathologist. This case series has no patient identifiers. Permission was obtained from the Office of the State Forensic Pathologist (OSFP) to access this anonymized data. The OSFP granted permission to access post-mortem reports (post-mortem findings and causes of death) and publish the data.
Study design
We conducted retrospective case series analyses of whole-body forensic post-mortem examinations we had performed on people who died suddenly and unexpectedly in the community of Lusaka, Zambia. These cases were referred to the OSFP at the University Teaching Hospital (UTH) for forensic post-mortem examination, where the proximate cause of death at post-mortem examination was found to be COVID-19. All the cases in the series were SARS-CoV-2 reverse transcriptase-polymerase chain reaction (RT-PCR) positive. The study period was from March 2020 to December 2020. Information on circumstances surrounding the death, symptoms, and co-morbidities was obtained from the next of kin by the forensic or anatomic pathologist as per procedure before the post-mortem examination was conducted and the Coroners Order for Post-Mortem Examination.
Pre-post-mortem examination procedures
All medico-legal staff underwent safety training. The pathologists and their assistants had defined protocols on coordination during the post-mortem procedure. The mortuary and post-mortem rooms used to perform the post-mortem examination had a working refrigeration system, good lighting and water reticulation systems but no negative pressure ventilation. The post-mortem examinations were conducted between 24 to 72 hours after death.
Post-mortem examination procedures
Whole-body post-mortem examinations were performed by a forensic pathologist and an anatomical pathologist. Personal protective equipment, including a full gown, plastic apron, gloves (including cut-proof under gloves), face visor, boots, and N95 masks, were used. Bodies were washed in chlorine before autopsy. Post-mortem examinations were performed in line with guidelines in the Practice Manual for Medicolegal Death Investigations at the OSFP in Zambia. In all cases, we followed universal precautions using personal protective equipment (PPE) (hair caps, eye protection, goggles), long-sleeved, non-waterproof gown covered by a water-proof apron. A double pair of standard disposable surgical latex gloves were used; cut-resistant gloves were also used. We used guidance-in-place regarding dressing and undressing PPE when dealing with infected bodies as in the practice manual for medico-legal death investigations.
Tissues sampled and histological examination
We followed our protocol (Himwaze et al., 2021). Briefly, representative samples were obtained from the brain, lung, heart, liver, spleen, kidney, and gastrointestinal tract and submitted in standard tissue cassettes. These were fixed in 10% neutral buffered formalin for 72 hours. Samples were processed, embedded in paraffin, sectioned, mounted onto glass slides, and stained with Hematoxylin and Eosin (H&E). All slides were examined by a forensic pathologist and an anatomical pathologist.
Data collection and analyses
Data on the decedent demographics, history, circumstances, post-mortem examination findings, and opinion of the cause of death was entered in Excel and analyzed using STATA version 14. The variables were grouped and presented as frequencies and percentages.
The cause of death was formulated within the context of the circumstances surrounding the death, history of the case, post-mortem examination findings, and ancillary studies.
All assumptions for Chi-square testing were observed, and p values were determined. A p-value of less than 0.05 was considered statistically significant. Mann-Whitney was used to report non-parametric continuous variables.
RESULTS
Decedents demographics
Table 1A shows the demographics of the decedents who underwent forensic post-mortem examination.
Table 1A.
Demographic Characteristics
Table 1. Demographic characteristics, Symptoms, and Co-morbidities
| Variable | Community Deaths (n=21) N(%) |
|---|---|
| Sex | |
| Male | 14 (66.2) |
| Female | 7 (33.3) |
| Mean Age ± SD (Range)years | 40 ± 12.3 (20-73) |
| 15-25 | 2 (9.5) |
| 26-35 | 4 (19.1) |
| 36-45 | 10 (47.6) |
| 46-55 | 2 (9.5) |
| 56-65 | 2 (9.5) |
| 66-75 | 1 (4.8) |
N (%): number of cases (percentage)
Of the 21 community COVID-19 related deaths, 66.7% (14/21) were male. Overall, 85.7% (18/21) of the cases were below 55 years of age (mean age of 40 ± 12.3; age range: 20-73).
Symptoms and co-morbidities
The common symptoms and co-morbidities are given in Table 1B .
Table 1B.
Symptoms and co-morbidities
| Variable | Community Deaths (n=21) N(%) |
|---|---|
| SYMPTOMS | |
| Difficulty breathing | 7(33.3) |
| Cough | 6(28.6) |
| Fever | 1(4.8) |
| Headache | 3(14.3) |
| General Body Weakness | 3(14.3) |
| Chest Pains | 5(23.8) |
| Vomiting | 1(4.8) |
| Diarrhea | 1(4.8) |
| Joint Pains | 1(4.8) |
| Sneezing | 1(4.8) |
| Duration of symptoms in Days- Median (IQR) | 1(0-2) |
| CO-MORBIDITIES | |
| HIV positive | 1(4.8) |
| Hypertension | 3(14.3) |
| Tuberculosis | 1(4.8) |
| Diabetes | 1(4.8) |
| Obesity | 3(14.3) |
| Pregnancy | 1(4.8) |
| Pneumonia | 1(4.8) |
| Drug and alcohol use | 1(4.8) |
Common symptoms observed were difficulty breathing (33.3%), cough (28.6%), and chest pains (23.8%). The median duration of symptoms was 1 day (range 0-2). Overall, 9/21 (42.9%) of the cases had co-morbidities
Post-mortem examination findings
A summary of post-mortem examination findings and cause(s) of death are given in Table 2 . The commonest post-mortem examination findings were diffuse alveolar damage (80.9%), saddle and shower emboli (38.1%, respectively), and pneumonia (14.3%). Pulmonary thromboembolism due to SARS-CoV-2 was the most common cause of death (76.2%), followed by diffuse alveolar damage due to SARS-CoV-2 (14.3%) and pneumonia due to SARS-CoV-2 (9.5%).
Table 2.
Autopsy findings and causes of death
| Autopsy findings | Community Deaths (n=21) N(%) |
|---|---|
| Diffuse Alveolar Damage | 17(80.9) |
| Saddle Emboli | 8(38.1) |
| Shower Emboli | 8(38.1) |
| Pneumonia | 3(14.3) |
| Granular kidneys | 2(9.5) |
| Deep Venous Thrombosis | 3(14.3) |
| Tuberculosis | 2(9.5) |
| Autopsy Causes of death | |
| Diffuse Alveolar Damage | 3 (14.3) |
| Pneumonia | 2 (9.5) |
| Pulmonary Thromboembolism | 16 (76.2) |
Gross pathology and Microscopic Findings
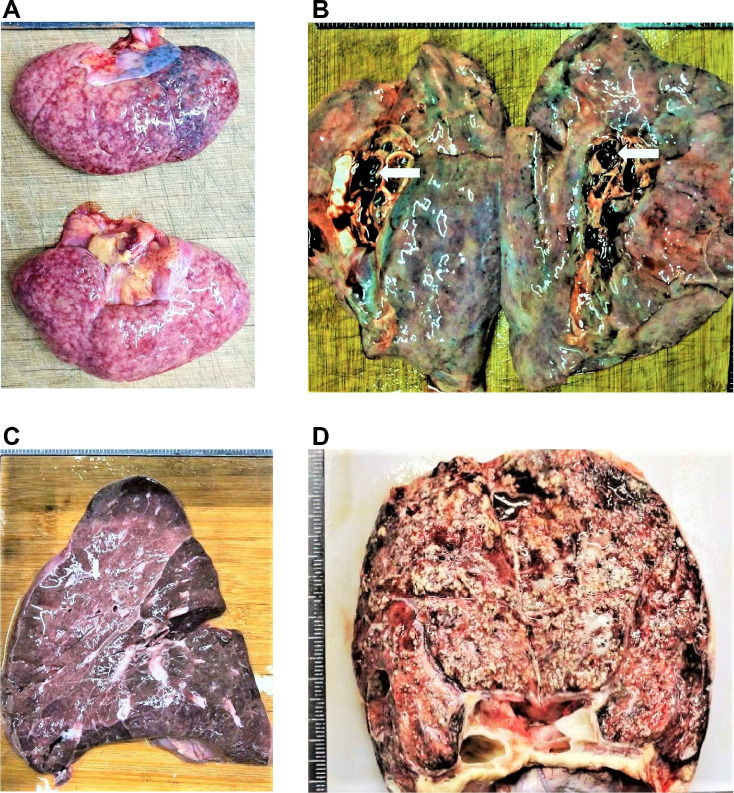
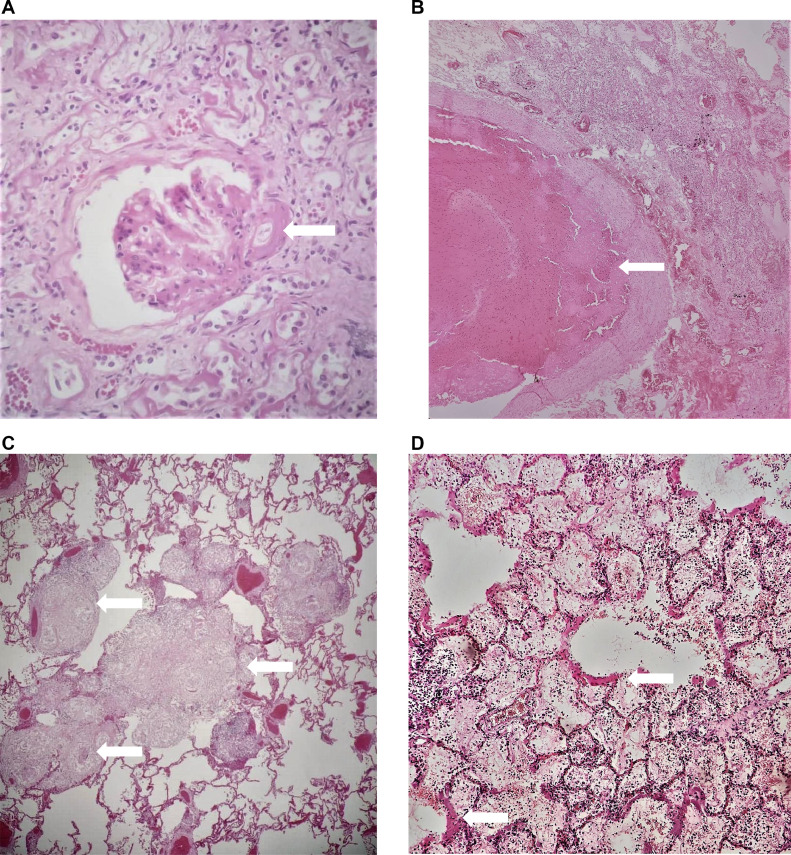
A selection of images representative of gross and microscopic autopsy findings are given in Figures 1 (1A-1D) and 2 (2A-2F).
Figure 1.
Gross Pathology Findings. (A): Kidneys: A case of chronic hypertension depicting kidneys with granular surfaces. (B): Lung: Pulmonary thromboembolism depicting a thrombus in the pulmonary vessels (white arrowhead). (C): Lung: Pneumonia depicting grey hepatization (D): Lung: Caseating lesions in a case of Pulmonary tuberculosis
Figure 2.
Microscopic pathology findings. (A): Kidney micrograph (X 40): A case of chronic hypertension depicting a hyalinized artery (white arrowhead). (B): Lung micrograph (X 20): A case of pulmonary thromboembolism depicting a thrombus in the pulmonary vessels (white arrowhead). (C): Lung micrograph (X 20): A case of tuberculosis depicting granulomatous inflammation (white arrowheads). (D): Lung micrograph (X 40): A case showing Diffuse Alveolar Damage. The hyaline membranes (white arrowheads) are observed to line the alveolar walls. (E): Lung micrograph (X 40): A case showing Organizing Pneumonia (white arrowhead).(F): Lung micrograph (X 20): A case of Acute Pneumonia depicting neutrophils in the alveolar spaces (white arrowheads).
Overall individual decedent characteristics and post-mortem examination findings
Table 3 summarizes the demographic, clinical, and post-mortem examination characteristics of each of the 21 decedents who underwent forensic whole-body post-mortem examination.
Table 3.
Summary of 21 Community Deaths Post-Mortem Examinations
| Case # | Sex/Age | Symptoms | Duration of illness | Co-morbidities | Gross and microscopic findings | Cause of death |
|---|---|---|---|---|---|---|
| 1 | M/58 | Cough and Difficulties breathing | 1 day | Diabetes and Hypertension | Heavy lungs (>1000 g each), shower thromboemboli, iliac artery thromboemboli, thromboemboli in the heart, granular kidneys, and DAD | Pulmonary thromboembolism due to COVID-19 |
| 2 | M/32 | Headache and Diarrhea | 1 day | None | Heavy lungs (>1000 g each), saddle thromboemboli, and DAD | Pulmonary thromboembolism due to COVID-19 |
| 3 | M/37 | Chest pains and Difficulties breathing | 5 hours | None | Saddle thromboemboli | Pulmonary thromboembolism due to COVID-19 |
| 4 | M/51 | Chest pains and difficulties breathing | 7 hours | None | Saddle thromboemboli | Pulmonary thromboembolism due to COVID-19 |
| 5 | M/20 | Painful legs and Difficulties breathing | 1 day | None | Heavy lungs (>1000 g each), saddle thromboemboli, and DAD | Pulmonary thromboembolism due to COVID-19 |
| 6 | F/38 | Cough and Difficulties breathing | 2 days | HIV and Disseminated Tuberculosis | Disseminated tuberculosis, heavy lungs (>1000 g each), shower thromboemboli, and DAD | Pulmonary thromboembolism due to COVID-19 |
| 7 | F/39 | Chest pains | 1 hour | None | Saddle thromboemboli | Pulmonary thromboembolism due to COVID-19 |
| 8 | M/42 | Fever, Cough, Joint pains, and Headache | 14 hours | Pneumonia | Shower thromboemboli, heavy lungs (>1000 g each), consolidation of lungs and neutrophils in alveolar spaces, and DAD | Pulmonary thromboembolism due to COVID-19 |
| 9 | M/38 | Unknown | 1 hour | None | Heavy lungs (>1000 g each), saddle thromboemboli | Pulmonary thromboembolism due to COVID-19 |
| 10 | F/27 | General body weakness | 7 days | Pulmonary tuberculosis | Shower thromboemboli, pulmonary tuberculosis, and DAD | Pulmonary thromboembolism due to COVID-19 |
| 11 | M/38 | Cough Difficulties breathing | 5 days | None | Shower thromboemboli and DAD | Pulmonary thromboembolism due to COVID-19 |
| 12 | M/44 | Cough Difficulties breathing | 1 day | Hypertension Obesity | Heavy lungs (>1000 g each), granular kidneys, and DAD | Diffuse Alveolar Damage due to COVID-19 |
| 13 | F/40 | Self-isolating, Sneezing, and coughing | 21 hours | Obese | Shower thromboemboli, heavy lungs (>1000 g each), and DAD | Pulmonary thromboembolism due to COVID-19 |
| 14 | F/59 | General body weakness | 1 day | Obese | Heavy lungs (>1000 g each) and DAD | Diffuse Alveolar Damage due to COVID-19 |
| 15 | F/43 | Chest pains in pregnancy | 1 day | None | Shower thromboemboli, heavy lungs (>1000 g each), deep venous thrombosis, and DAD | Pulmonary thromboembolism due to Deep Vein Thrombosis due to COVID-19 |
| 16 | M/32 | General body weakness | 1 day | None | Heavy lungs (>1000 g each), consolidation of lungs and neutrophils in alveolar spaces, and DAD | Pneumonia due to COVID-19 |
| 17 | M/28 | Vomiting | 2 days | Alcoholism Drug abuse | Shower thromboemboli, heavy lungs (>1000 g each), deep venous thrombosis, and DAD | Pulmonary thromboembolism due to Deep Vein Thrombosis due to COVID-19 |
| 18 | M/73 | Chest pains | 1 day | Hypertension | Shower thromboemboli, heavy lungs (>1000 g each), and DAD | Diffuse Alveolar Damage due to COVID-19 |
| 19 | M/43 | None | < 1 day | None | Shower thromboemboli, Heavy lungs (>1000 g each), and DAD | Pulmonary thromboembolism due to COVID-19 |
| 20 | 46/M | Headache | 1 day | None | Heavy lungs (>1000 g each), consolidation of lungs and neutrophils in alveolar spaces, and DAD | Pneumonia due to COVID-19 |
| 21 | F/25 | Convulsions | 5 hours | None | Deep Vein Thrombosis, heavy lungs (>1000 g each), saddle thromboemboli, brain (1250 g) unremarkable, and DAD | Pulmonary thromboembolism due to Deep Vein Thrombosis due to COVID-19 |
Comparison of Community Deaths versus Hospital inpatient Deaths
Table 4 gives a comparison of our Community autopsy series findings with the findings of our autopsy case series of COVID-19 inpatient hospital deaths in Lusaka, Zambia, published previously (Mucheleng'anga and Himwaze, 2021). COVID-19 decedents who died in the community compared to those who died in hospital had a higher proportion of diffuse alveolar damage (58.6% vs 41%; p= 0.005), saddle emboli (57% vs 43%: p= 0.17), and shower emboli (67% vs 33%; p= 0.04). A significantly higher proportion of thromboembolism was observed in the community versus hospital deaths (55% vs. 45%; p= 0.027).
Table 4.
Comparison of Community versus Hospital Autopsy findings and causes of death in Lusaka, Zambia
| Overall Deaths (N=50) N(%) | Community Deaths (n=21) N(%) | Hospital Deaths+ (n=29) N(%) | Statistic (p-value) N(%) | |
|---|---|---|---|---|
| Autopsy Findings | ||||
| Diffuse Alveolar Damage | 29(58.0) | 17(80.9) | 12(41.4) | 7.830 (0.005)* |
| Saddle Emboli | 14(28.0) | 8(38.1) | 6(20.7) | 1.830 (0.176) |
| Shower Emboli | 12(24.0) | 8(38.1) | 4(13.8) | 3.944 (0.047)* |
| Pneumonia | 12(24.0) | 3(14.3) | 9(31) | 1.873 (0.171) |
| Granular kidneys | 7(14.0) | 2(9.5) | 5(17.2) | 0.603 (0.684)# |
| Deep Venous Thrombosis | 6(12.0) | 3(14.3) | 3(10.3) | 0.179 (0.686)# |
| Disseminated Thrombi | 4(8.0) | 0(0.0) | 4(13.8) | 3.148 (0.129)# |
| Tuberculosis | 3(6.0) | 2(9.5) | 1(3.4) | 0.739 (0.565)# |
| Anemia | 1(2.0) | 0(0.0) | 1(3.4) | 0.739 (0.999)# |
| Kaposi Sarcoma | 1(2.0) | 0(0.0) | 1(3.4) | 0.739 (0.999)# |
| Colorectal adenocarcinoma | 1(2.0) | 0(0.0) | 1(3.4) | 0.739 (0.999)# |
| Cause(s) of Death | ||||
| Diffuse Alveolar Damage | 12 (24.0) | 3 (14.3) | 9 (31.0) | 1.873 (0.171) |
| Pneumonia | 9 (18.0) | 2 (9.5) | 7 (24.2) | 1.762 (0.271)# |
| Pulmonary Thromboembolism | 29 (58.0) | 16 (76.2) | 13 (44.8) | 4.918 (0.027)* |
Fisher's exact test; p<0.05
Himaze C et al, 20216
DISCUSSION
To our knowledge, this is the first case series from Africa of whole-body post-mortem data of COVID-19 sudden and unexpected deaths in the community who were subject to medico-legal death (forensic) investigations. These decedents were not suspected of having SARS-CoV-2 prior to death. We were able to determine the demographics, symptomatology, co-morbid conditions, and pathological features of community decedents with COVID-19 and compare these with our previous data from the COVID-19 case series of hospital inpatient deaths (Himwaze et al., 2021, Mucheleng'anga and Himwaze, 2021)
There were more males than females in our series. This is consistent with our previous autopsy study of 29 inpatient hospital deaths where there were more males (Mucheleng'anga and Himwaze, 2021) and is similar to findings of a study of UTH mortuary of medico-legal decedents (Himwaze et al., 2021). It has been suggested that males are more predisposed to sudden and unexpected deaths due to complications of disease arising from poor health-seeking habits (Himazwe et al., 2020). It has also been suggested that males may be more susceptible to SARS-CoV-2 infection due to their higher plasma angiotensin-converting enzyme 2 levels and less effective antiviral immune defenses (Griffith et al., 2021, Gadi et al., 2020).
Eighty-five percent (85.0%) of the cases in our series were below 55 years of age. The comparatively younger age may be attributed to Zambia's age structure, where people above the age of 55 years are less than 6% of the entire population (Index Mundi 2021). However, a study in Germany conducted in a medico-legal population showed more deaths in those above 65 years old (Edler et al., 2020). The difference may be attributed to differences in the age structure of the two populations (STATISTA 2019). In another case series in Germany, it was highlighted that COVID-19 is fatal in young people (Greuel et al., 2021). The younger age group in decedents in our series requires further study, and the underlying susceptibility and risk factors need to be investigated further so that risk factors can be identified and appropriate measures are taken..
Difficulty in breathing, cough, chest pain, headache and, general body weakness were the most common symptoms in our series. This is similar to our hospital autopsy study (Himwaze et al., 2021) and a study from China (Bian, 2020). The duration of symptoms was from a few hours to two days. The reason for the short duration of symptoms is unknown and needs further investigation. Forensic pathology experts suggest that the shorter duration of symptoms in the medico-legal population in natural deaths may be attributed to the self-rationalization of symptoms and a failure to seek medical attention (Spitz, 2006).
A majority (57.1%) of the cases did not have pre-existing co-morbid conditions. This differs from the German study that showed that most cases have pre-existing conditions (Edler et al., 2020). Although these findings are unique to our population, the reason for this finding requires further study. Among those cases with pre-existing conditions, obesity and hypertension were the most common co-morbidities in community deaths. The black population is predisposed to obesity and hypertension (Dustan, 1990).
Comparison of data from community COVID-19 deaths with our previous data from the COVID-19 case series of hospital inpatient deaths (Himwaze et al., 2021, Mucheleng'anga and Himwaze, 2021) showed hospital deaths had more co-morbidities, with HIV infection and hypertension being the most common. These may reflect the hospital admission criteria and COVID-19 guidelines, which select patients with moderate or severe respiratory symptoms, and all COVID-19 patients who present with co-morbidities upon admission. It may also reflect routine screening for HIV and hypertension on admission. In contrast, routine HIV testing is not performed at autopsy at the OSFP. HIV and hypertension as co-morbidities are unique to our population compared to the observations made in other autopsy studies.
We observed that 15/21 (71.4%) of our Community decedent cases revealed heavy lungs that were above 1000g each, a finding consistent with the severe inflammatory process in COVID-19. Diffuse Alveolar Damage (DAD), saddle and shower emboli, Deep Venous Thrombosis, and Pneumonia were the most common post-mortem findings in this series. A systematic review of post-mortem data showed that DAD was the most predominant feature in the lungs of COVID-19 at post-mortem examination. Pulmonary thromboembolic findings in COVID-19 appear to be consistent with the disease-specific hypercoagulability (Maiese et al., 2020). These findings are similar to other post-mortem examination studies outside of Africa (Edler et al., 2020).
Pulmonary thromboembolism due to SARS-CoV-2 was the most common immediate cause of death in our series. The reason for this finding is unknown and requires further investigation. Thromboembolic events are well known to occur during SARS-CoV-2 infection and may be attributed to microangiopathic changes (Falasca et al., 2020). Like COVID-19, two other prevalent diseases in Africa, Human Immunodeficiency Virus (HIV) (Dentan et al., 2014) and Tuberculosis (Kwas et al., 2014, Crum-Cianflone et al., 2008), can independently trigger venous thromboembolism and pulmonary embolism. Thus, HCWs in Africa must maintain a high level of awareness for the possibility of thromboembolism during this era of COVID-19. This also adds to the ongoing dialogue on the use of thromboprophylaxis in patients with TB, HIV, and COVID-19 and those with co-morbidities (Temgoua et al., 2020 Apr 27). In South Africa, rare thromboembolic events were observed during the COVID-19 vaccination rollout and have occurred mainly in people with risk factors for thromboembolism (Takuva et al., 2021).
DAD due to SARS-CoV-2 was the second most common immediate cause of death. SARS-CoV-2 infects the respiratory tract's epithelial lining cells, leading to DAD and eventually death (Elsoukkary et al., 2021). Finally, pneumonia due to SARS-CoV-2 was the third most common cause of death. We also noted that hospital deaths showed an organizing type of pneumonia while the community deaths showed acute pneumonia.
The limitation of our case series includes relatively small numbers of cases and a selection bias of cases that have medico-legal questions to answer. However, this case series highlights that in the COVID-19 era, forensic post-mortem examination could play a significant role in determining the exact cause(s) of death among those who die suddenly and unexpectedly in the community. COVID-19 is known to be associated with sudden death at home or after discharge from hospital (Matsuyama et al., 2020, Shirazi et al., 2021). Thus, the forensic post-mortem examination on those decedents who die after hospital discharge provides opportunities to better define pathogenesis and post-initial infection complications and sequelae. Routine forensic post-mortem examination sampling of tissues from community deaths could also help track SARS-CoV-2 variants’ evolution and determine the duration of the viability of SARS-CoV-2 in decedents.
The effects of the COVID-19 pandemic on the overall population mortality, community deaths, and mortality's impact on health services, remain unknown. While forensic pathology is not seen to be on the frontlines of public health, this case series highlights its significant role in identifying deaths due to COVID-19 (Mucheleng'anga and Himwaze, 2020, Mucheleng'anga and Himwaze, 2021, Himwaze et al., 2021). COVID-19 deaths add further to the longstanding urgent need for governments and funding agencies to invest more in autopsy services in Africa overall and into medico-legal death investigation facilities specifically. This will allow for more determination of COVID-19 as a cause of death, rather than relying on the crude indirect and inaccurate methods in use today, which generate controversy and debate (Temgoua et al., 2020 Apr 27, Takuva et al., 2021, Elsoukkary et al., 2021, Matsuyama et al., 2020, Shirazi et al., 2021). This would help understand the extent and impact of COVID-19 disease in people succumbing to COVID-19 in the community, help define further the impact of COVID-19 on other killer infections, and shed light on impact on public health and help develop policy guidelines.
Acknowledgments
ACKNOWLEDGEMENTS
Sir Prof Alimuddin Zumla, is co-Principal Investigator of the (PANDORA-ID-NET), the Pan-African Network For Rapid Research, Response, Relief and Preparedness for Infectious Disease Epidemics, supported by the EDCTP. He is in receipt of a UK National Institutes of Health Research, Senior Investigator Award and is a Mahathir Foundation Science Award laureate. We thank our pathology assistants and biomedical scientists.
CONFLICTS OF INTEREST
All authors declare no conflict of interest.
AUTHORS CONTRIBUTIONS
Conceptualization: Luchenga Adam Mucheleng'anga, Cordelia Maria Himwaze, and Alimuddin Zumla.
Methodology: Luchenga Adam Mucheleng'anga and Cordelia Maria Himwaze.
Software and formal analysis: Amos Hamukale.
Validation: Viktor Telendiy, Amos Hamukale, Llyod Mulenga, and Alimuddin Zumla.
Data curation: Luchenga Adam Mucheleng'anga, Cordelia Maria Himwaze, Viktor Telendiy
Writing: First and final drafts: Luchenga Adam Mucheleng'anga, Alimuddin Zumla, and Cordelia Maria Himwaze,
Review and editing: All authors contributed to the writing and editing of the manuscript.
Visualization: Luchenga Adam Mucheleng'anga, Cordelia Maria Himwaze, Amos Hamukale, and Alimuddin Zumla.
Supervision: Alimuddin Zumla and Luchenga Adam Mucheleng'anga.
FUNDING
This research did not receive any specific grant from any funding sources.
REFERENCES
- Bian Xiu-Wu, The COVID-19 Pathology Team Autopsy of COVID-19 patients in China. National Science Review. 2020;7(9):1414–1418. doi: 10.1093/nsr/nwaa123. https://doi.org/- Accessed on 19th June 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crum-Cianflone NF, Weekes J, Bavaro M. Thromboses among HIV-infected patients during the highly active antiretroviral therapy era. AIDS Patient Care. STDS. 2008;22(10):771–778. doi: 10.1089/apc.2008.0010. https://doi.org/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dentan C, Epaulard O, Seynaeve D, Gently C, Bosson JL. Active tuberculosis, and venous thromboembolism: Association according to international classification of diseases, ninth revision hospital discharge diagnosis codes. CID. 2014;58(4):495–501. doi: 10.1093/cid/cit780. https://doi.org/ [DOI] [PubMed] [Google Scholar]
- Dustan HP. Obesity and hypertension in blacks. Cardiovasc Drugs Ther. 1990;4(Suppl 2):395–402. doi: 10.1007/BF02603183. MarPMID: 2271401. [DOI] [PubMed] [Google Scholar]
- Edler C, Schröder AS, Aepfelbacher M, et al. Dying with SARS-CoV-2 infection-an autopsy study of the first consecutive 80 cases in Hamburg, Germany. Int J Legal Med. 2020;134(4):1275–1284. doi: 10.1007/s00414-020-02317-w. Epub 2020 Jun 4. Erratum in: Int J Legal Med. 2020 Sep;134(5):1977. PMID: 32500199; PMCID: PMC7271136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elsoukkary S, Mostyka M, Dillard A, et al. Autopsy Findings in 32 Patients with COVID-19: A Single-Institution Experience. Pathobiology. 2021;88:56–68. doi: 10.1159/000511325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Falasca L, Nardacci R, Colombo D, et al. Postmortem Findings in Italian Patients With COVID-19: A Descriptive Full Autopsy Study of Cases With and Without Comorbidities. J Infect Dis. 2020;222(11):1807–1815. doi: 10.1093/infdis/jiaa578. Nov 9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gadi N, Wu SC, Spihlman AP, Moulton VR. What's Sex Got to Do With COVID-19? Gender-Based Differences in the Host Immune Response to Coronaviruses. Front Immunol. 2020;28:2147. doi: 10.3389/fimmu.2020.02147. 11PMID: 32983176; PMCID: PMC7485092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greuel S, Ihlow J, Dragomir MP, et al. COVID-19: Autopsy findings in six patients between 26 and 46 years of age. Int J Infect Dis. 2021;108:274–281. doi: 10.1016/j.ijid.2021.05.069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Griffith DM, Sharma G, Holliday CS et al. Men and COVID-19: A Biopsychosocial Approach to Understanding Sex Differences in Mortality and Recommendations for Practice and Policy Interventions. https://www.cdc.gov/pcd/issues/2020/20_0247.htm. -Accessed on 25/03/ 2021. [DOI] [PMC free article] [PubMed]
- Himazwe C, Mucheleng'anga L, Siyumbwa SN, et al. Prevalence of Human Immunodeficiency Virus, Hepatitis B, and Hepatitis C Viral Infections among Forensic Autopsy Cases at the University Teaching Hospital in Lusaka, Zambia. Forensic Science International: Reports. 2020;2 doi: 10.1016/j.fsir.2020.100133. https://doi.org/ [DOI] [Google Scholar]
- Himwaze CM, Telendiy V, Hamukale A, et al. Post Mortem examination of Hospital Inpatient COVID-19 Deaths in Lusaka, Zambia – A descriptive Whole Body Autopsy Series. International Journal of Infectious Diseases. 2021 doi: 10.1016/j.ijid.2021.06.013. -in press S1201-9712(21)00502-6. DOI: https://doi.org/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- Index Mundi, Zambia Age structure https://www.indexmundi.com/zambia/age_structure.html. Accessed on 14/05/ 2021.
- Kwas H, Habibech S, Zendah I, Elmjendel I, Ghedira H. Pulmonary embolism and tuberculosis. Asian Cardiovascular and Thoracic Annals. 2014;22(4):487–490. doi: 10.1177/0218492313485071. https://doi.org/ [DOI] [PubMed] [Google Scholar]
- Maiese A, Manetti AC, La Russa R, et al. Autopsy findings in COVID-19-related deaths: a literature review. Forensic Sci Med Pathol. 2020;7:1–18. doi: 10.1007/s12024-020-00310-8. Epub ahead of print. PMID: 33026628; PMCID: PMC7538370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matsuyama T, Yamahata Y, Ohta B. Strategies for preventing sudden unexpected COVID-19 deaths at home. Resuscitation. 2020;157:106–107. doi: 10.1016/j.resuscitation.2020.09.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mucheleng'anga L, Himwaze C. The role of forensic pathology in the COVID-19 pandemic in Zambia. Forensic Science International. Reports. 2020;2 doi: 10.1016/j.fsir.2020.100147. 1 00147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mucheleng'anga L, Himwaze MC. Rapid response to Covid-19 deaths in Africa: prospective systematic post-mortem surveillance study. BMJ. 2021:372. doi: 10.1136/bmj.n334. doi: https://doi.org/(Published 17 February 2021) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shirazi S, Mami S, Mohtadi N, et al. Sudden cardiac death in COVID-19 patients, a report of three cases. Future Cardiol. 2021;17(1):113–118. doi: 10.2217/fca-2020-0082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spitz WU. 4th edition. Charles C, Springfield, II; 2006. Medico-legal Investigation of Death: Guidelines for the Application of Pathology to Crime Investigation. [Google Scholar]
- STATISTA. Population of Germany 2019 https://www.statista.com/statistics/454349/population-by-age-group-germany/. Accessed on 19.06.2021
- Takuva S, Takalani A, Garrett N, Goga A, Peter J, Louw V, et al. Thromboembolic Events in the South African Ad26.COV2.S Vaccine Study. N Engl J Med. 2021 doi: 10.1056/NEJMc2107920. Jun 2:NEJMc2107920Epub ahead of print. PMID: 34077639; PMCID: PMC8190951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Temgoua MN, Kuaté LM, Ngatchou W, Sibetcheu A, Toupendi ZN, et al. Thromboembolic risks in patients with COVID-19: major concern to consider in our management. Pan Afr Med J. 2020 Apr 27;35(Suppl 2):10. doi: 10.11604/pamj.2020.35.2.22945. PMID: 32528621; PMCID: PMC7266474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO Afro. Ref: https://www.afro.who.int/health-topics/coronavirus-covid-19 -accessed 30th June 2021
- WHO COVID-19 dashboard – Zambia. https://covid19.who.int/region/afro/country/zm - Accessed on 29.06. 2021.
- Youd E, Moore L. COVID-19 autopsy in people who died in community settings: the first series. J Clin Pathol. 2020;73(12):840–844. doi: 10.1136/jclinpath-2020-206710. [DOI] [PubMed] [Google Scholar]