Abstract
Objective:
Social isolation is highly common in late life and is associated with devastating mental health and physical outcomes. This study investigated whether components of social isolation (marital status, perceived social support, and interpersonal problems) predict change in depression severity over the course of a brief adherence intervention delivered in a primary care setting.
Method:
A sample of 189 older adults with major depressive disorder were randomized to either an adherence intervention, ‘Treatment Initiation Program (TIP),’ or treatment as usual. Marital status, perceived social support and interpersonal problems were assessed at baseline. A mixed-effects regression was used to test whether these factors predicted the change trajectory in depression severity over 24 weeks.
Results:
Being married (F(2,176) = 6.60; p=.001), reporting higher perceived social support (F(2,177) = 4.70; p=.01), and fewer interpersonal problems (F(2, 176) = 4.34; p = .01) predicted lower depression severity on average over the course of 24 weeks.
Conclusion:
Social variables such as living in partnership, perceiving others as supportive, and reporting few interpersonal problems may reduce older adults’ vulnerability to depression and enhance their ability to benefit from treatment. These findings can guide development of interventions that will target these social factors early in treatment to increase efficacy.
Objective
Social relationships play an important role in psychological health and wellness in late life (1). There is evidence that some older adults actively seek to increase their social engagement (e.g., neighborly socializing, religious service attendance, and volunteering) (2), but many older adults are at risk for reduced social contact and social network size due to factors such as loss of loved ones, decreased mobility, chronic illness, retirement, living alone, or change in economic status (3). Loneliness among adults 60 years and older has been associated with 59% increased risk of functional decline (e.g., difficulty with bathing, eating, and general mobility) and a 45% increased risk of death (4). Additionally, older adults who are more isolated engage in more unhealthy behaviors such as poor diets, tobacco use, and heavy alcohol use (5). Lonely older adults are 1.96 times more likely to die within 6 years than those who report low levels of loneliness, even while controlling for sociodemographic characteristics, social relationships, and health behaviors (6).
There is a strong link between social connection and depression among older adults (7). Both the objective lack of social contact and the subjective perception of poor social relationships are strongly associated with major psychological morbidities and lower perceived quality of life among older adults (8). This study explores whether three major components of social relationships - marital status, perceived social support, and interpersonal problems - are related to depression severity and treatment response among depressed older adults treated in primary care.
One’s marital status can factor into the degree of social isolation that an older adult experiences. Individuals who were previously but are no longer married (widowed, divorced, or separated) are lonelier those who are married or have never married (9). Research has shown that married older adults have lower rates of depression (10). There is evidence that marital status predicts the rate of change in depressive symptoms over time and that changes in marital status are associated with the trajectory of depression (11). Among patients with less severe depression, being married predicted early recovery for outpatients in community-based mental health settings (12). Furthermore, high levels of engagement with supportive individuals may serve as a protective factor. Engagement in rewarding activities with significant others predicts reduction in depression severity in “Engage,” a behavioral activation therapy for depression (13, 14).
The degree to which one feels supported, cared for and connected to others (perceived social support) (15) is significantly associated with positive psychological health outcomes (16). The subjective quality of one’s social relationships has an even greater impact on depression in late life than the objective quantity of social contact (17). Low perceived social support has been found to be a unique risk factor for depressive symptoms among middle-aged and older adults, distinct from demographic and psychosocial risk factors (18). In a longitudinal study, loneliness predicted increases in depressive symptomatology over five years, and this association is not attributed to initial depression severity, demographic variables, objective social isolation, stress, general negative affectivity, or social support (19). Low perceived social support also predicts poorer response to psychosocial interventions for late-life depression (20). In a treatment study, perceived positive social support was associated with decreased depression over time for a placebo group but not in treatment groups receiving antidepressants or psychotherapy (21).
Depressed individuals tend to experience difficulties in interpersonal relationships due to the association of depression with social deficits such as poor social skills, excessive reassurance seeking, and negative social behaviors (22). Individuals with more severe depressive symptoms have been found to have poorer recall of socially rewarding words, which suggests that the negativity bias of depressed individuals extends to how they process social information (23). There is also evidence that depressive symptoms interfere with judgments about the adequacy of social interaction (24), which may contribute to low perceived social support. “Interpersonal problems” refer to one’s reported difficulties in social relationships, such as confrontational interactions or perceived social rejection. Interpersonal problems predict poorer outcome to psychosocial interventions among patients with depression (25). Those with dominant social behavior or a more rigid interpersonal style demonstrate less change in symptom severity following evidence-based psychotherapy for depression (26). Among less severely depressed individuals, interpersonal problems independently predicted early recovery over 12 weeks of outpatient treatment in community-based mental health settings (12). Personality traits may impact treatment outcome via their influence on the therapeutic alliance among patients with major depressive disorder (27).
This study investigated the impact of marital status, perceived social support, and interpersonal problems on depression severity and treatment response among older adults. We present a secondary data analysis of a randomized controlled trial for the Treatment Initiation Program (TIP), a brief psychosocial intervention designed to improve antidepressant adherence among middle aged and older adults with a newly initiated prescription by a primary care provider (28). The primary outcome of the initial study found that TIP patients were three times more likely to be at least 80% adherent to their antidepressant at both 6 and 12 weeks. TIP did not significantly impact depressive symptoms compared to treatment as usual over the course of the study. However, patients showed a significant earlier reduction in depressive symptoms. Additional analyses found that greater adherence, but not adequate medication dosage, was associated with the likelihood of treatment response (29). The current investigation expands on these findings by exploring social predictors of treatment response. We hypothesized that patients with greater social connection as measured by marital status, perceived social support, and fewer interpersonal problems would show lower depression severity. Additionally, we hypothesized that individuals who are more socially connected would benefit more from interventions and demonstrate greater improvement in depressive symptoms. Given that both the intervention and treatment as usually were equally effective in reducing depression severity, we did not predict differential treatment effects. Findings from this study can better inform the role of social interaction on depression severity and treatment interventions.
Methods
Study Design
Potential patients for the study were identified at participating primary care sites and recruited within 10 days of receiving a prescription for an antidepressant. Patients who met eligibility criteria during the baseline assessment were randomized 1:1 (stratified by site) to either the TIP intervention or to treatment as usual, which involved routine monitoring by the primary care provider (PCP). The two site principal investigators oversaw the conduct and data analysis of the trial and data with an annual review by an independent data and safety monitoring board. This study was supported by the Weill Cornell Medicine and University of Michigan Institutional Review Boards. Additional details on the study design can be found in Sirey et al., 2017.
Patients
Patients were consecutively recruited from January 2011 through December 2014 from two primary care practices in New York and Michigan. All patients had been newly prescribed an antidepressant by their PCP for depressive symptoms. Patients were excluded if they had: (1) active suicidality; (2) current substance abuse, bipolar disorder, or psychosis; (3) significant cognitive impairment (MMSE<23); (4) terminal illness or current chemotherapy; or (5) an inability to communicate in English.
Measures
Research assessments were conducted at baseline, 6, 12 and 24 weeks by trained research assistants blind to group assignment.
Marital Status.
Marital status was categorized as married (n=83; 43.9%), never married (n=25; 13.2%), no longer married (n=53; 28%), and widowed (n=28; 15%). Those who are no longer married include patients who were separated or divorced.
Perceived Social Support.
The Duke Social Support Index (DSSI) is a self-report scale that measures multiple dimensions of social support. It has been found reliable and internally consistent in samples of community-dwelling older adults, and it has been used extensively in studies of aging (30). In this study, patients completed the 8-item “Perceived Social Support” subscale measuring perceived social support, which has been found to be associated with depression (31). Items include questions such as: “Do you feel you have a definite role (place) in your family and among your friends?” and “Can you talk about your deepest problems with at least some of your family and friends?”.
Interpersonal Problems.
The Inventory of Interpersonal Problems is a self-report used to measure the extent to which individuals present with problems in interpersonal relationships (32). Items include questions such as: “I fight with other people too much” and “I am too sensitive to rejection.” The abbreviated version used in this study (IIP-15) has been shown to be a reliable and valid screening tool in identifying common interpersonal dysfunction that cuts across personality disorder diagnoses (33). IIP scores were included in our model as continuous variables.
Mental Status.
The Mini-Mental State Examination (MMSE; (34)) is a screening test widely used to identify cognitive impairment among older adults. It covers a range of cognitive domains and is widely administered to determine eligibility in older adult studies (e.g., (14)).
Depression.
Depressive symptoms were measured using the Hamilton Depression Rating Scale (HAM-D; (35)), a semi-structured interview to determine depression severity. The HAM-D is the most widely used clinician-administered depression assessment scale. A meta-analytic review of its use in studies between 1960–2008 found it to be a reliable assessment of depression with good overall levels of internal consistency, inter-rater and test-retest reliability (36).
Adherence.
Adherence was measured using the Brief Medication Questionnaire (BMQ), is a self-report measure, validated against medication event monitoring system (MEMS) caps data, and used extensively in studies of older adults (37, 38). Adequate antidepressant adherence was defined as 80% adherence to assure that a majority of doses are taken to achieve a biological effect (39). Patients were considered adherent if they were taking the prescribed antidepressant medication 80%−100% of the time at both the 6th and the 12th week of follow-up. Patients who discontinued their antidepressant were classified as non-adherent.
Statistical Analyses
We used mixed-effects regression to model the trajectory of depression severity (HAMD scores) over 24 weeks. We investigated whether the variables of interest (perceived social support, marital status, and interpersonal problems) at baseline predicted trajectory of change in depression severity over time. Perceived social support (Duke Subjective Support Subscale) and interpersonal problems (IIP total score) were converted from continuous to categorical variables for the purpose of post-hoc comparisons and visualization. Each variable included three levels: a) low (<1 SD below the mean); b) moderate (> 1 SD below the mean and <1 SD above the mean); c) high (>1 SD above the mean). Our model included both main effects and predictor*time interaction for all predictors of interest. We then ran all models with predictors as continuous variables to ensure results were equivalent. The model included fixed effects for time and predictors of interest. We initially included fixed effects for treatment condition (TIP vs. TAU) and treatmentXtime interaction as well as for site and siteXtime. These effects were not significant and thus excluded from the final model. The lack of treatment effect on depression outcomes is in line with our previous reports of equivalent treatment response for TIP and TAU (28, 29). The final model included three main effects and interaction terms for subjective support*time, marital support*time, and IIP score*time. We also included a subject-specific random intercept. We adjusted the model for several potential covariates: cognitive functioning (MMSE), age, and gender. Additionally, given previous reports showing that higher adherence was associated with treatment response in this sample (28), we included adherence in our analysis. All analyses were conducted in R Statistical Software (40).
Results
Demographics and clinical characteristics of our sample are described in Table 1. Mixed-effects model showed overall improvement in depression severity over time (F(3,553) = 23.71, p<.001; η2 = 0.11, CI[0.07,0.15]) across both treatment groups. As hypothesized, the main effects were significant for our three predictors of interest, showing that reporting greater perceived social support (F(2,177) = 4.70; p=.01, η2 = 0.05, CI[0.01,011]; Figure 1); being married (F(2,176) = 4.71; p=.003, η2 = 0.07, CI[0.02,0.13]; Figure 2); and reporting less interpersonal problems (F(2, 176) = 4.34; p = .01, η2 = 0.04, CI[0.00, 0.10]; Figure 3) significantly predicted lower depression severity. Predictor*time interaction terms were not significant for the three predictors of interest (see Supplemental Materials for exploratory post-hoc comparisons of interaction terms). Significant covariates included age (F(1,177) = 12.85, p <.001, η2 = 0.07, CI[0.02,0.14], cognitive functioning (MMSE score; F(1,177) = 8.43; p = .004, η2 = 0.05, CI[0.01,0.11]), and adherence (F(1,176) = 9.94, p = .001, η2 = 0.05, CI[0.01,0.12]).
Table 1.
Baseline Demographics and Clinical Characteristics of the Sample (N = 189)
| Demographics and Clinical Characteristics | No. (%) |
|---|---|
| Age (mean, SD), y | 67.15 (8.34) |
| Female | 134 (70.1) |
| Hispanic | 24 (12.6) |
| Race/ethnicity | |
| Black | 35 (18.5) |
| White | 134 (70.8) |
| Asian | 8 (4.2) |
| Other | 12 (6.3) |
| Marital status | |
| Never married | 25 (13) |
| Married | 83 (44) |
| No longer married | 53 (28) |
| Widowed | 28 (15) |
| Educational level, mean (SD), y | 14.5 (3.0) |
| Employment status | |
| Full- or part-time | 46 (24.3) |
| Unemployed or on disability | 35 (25.1) |
| Retired | 106 (56.0) |
| Baseline DSSI, perceived social support subscale | 17.1 (3.35) |
| Baseline IIP | 13.72 (8.01) |
| Baseline HAM-D score | 18.3 (9.77) |
| MMSE score, mean (SD) | 27.8 (2.0) |
Note. DSSI = Duke Social Support Index; IIP = Inventory of Interpersonal Problems; HAM-D = Hamilton Depression Rating Scale; MMSE = Mini-Mental State Examination
Figure 1.
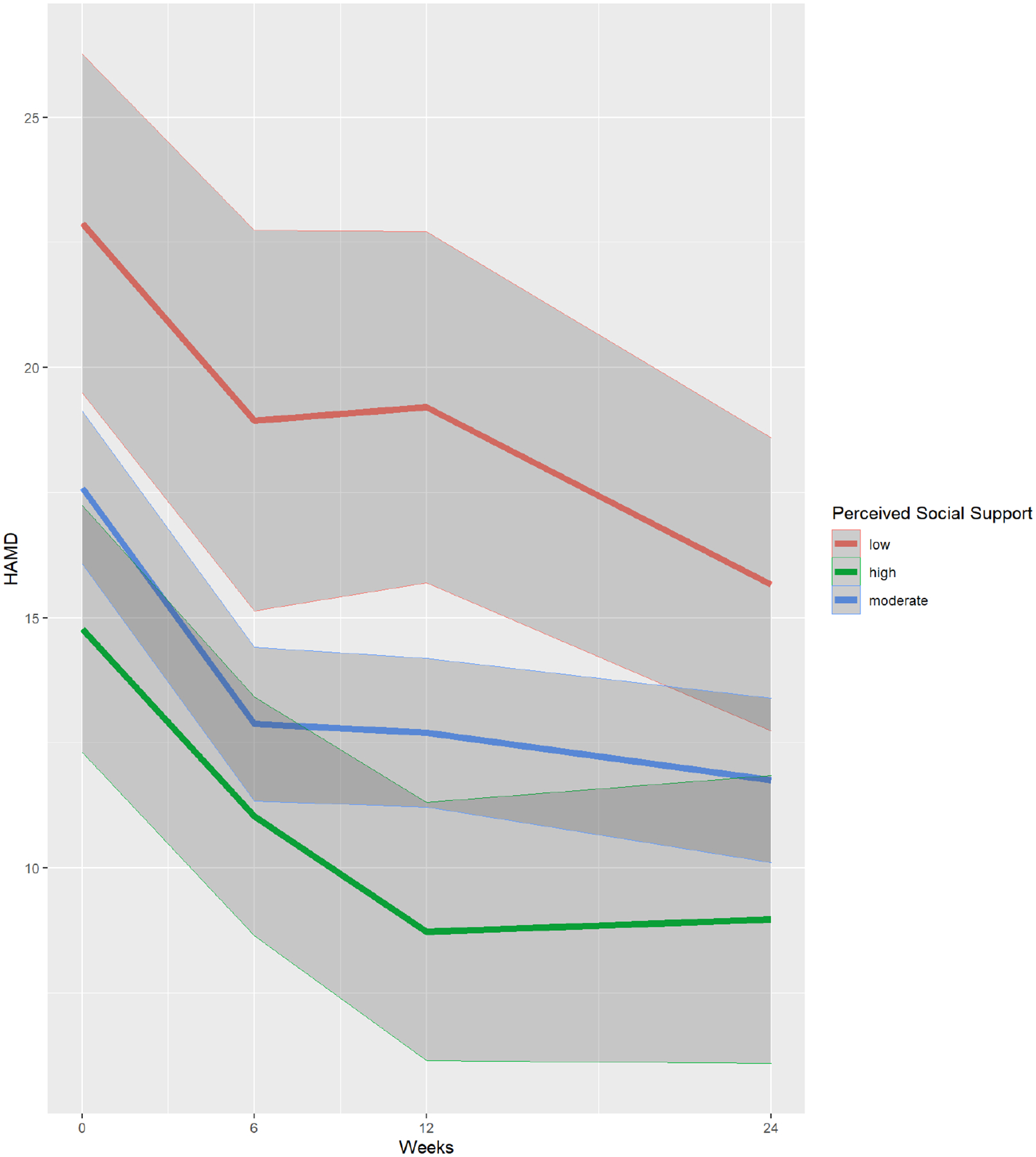
Perceived Social Support as a Predictor of Change in Depression Severity Over 24 Weeks
Note. HAMD = Hamilton Depression Severity Scale. Plot includes mean scores with 95% confidence interval. High scores on the IIP represent high interpersonal distress. IIP scores were included in the model as continuous variables. For visualization purposes, we divided the variable to three levels here: High (>1 SD above the mean); Moderate (<1 SD above the mean and >1 SD below the mean); and Low (>1 SD below the mean).
Figure 2.
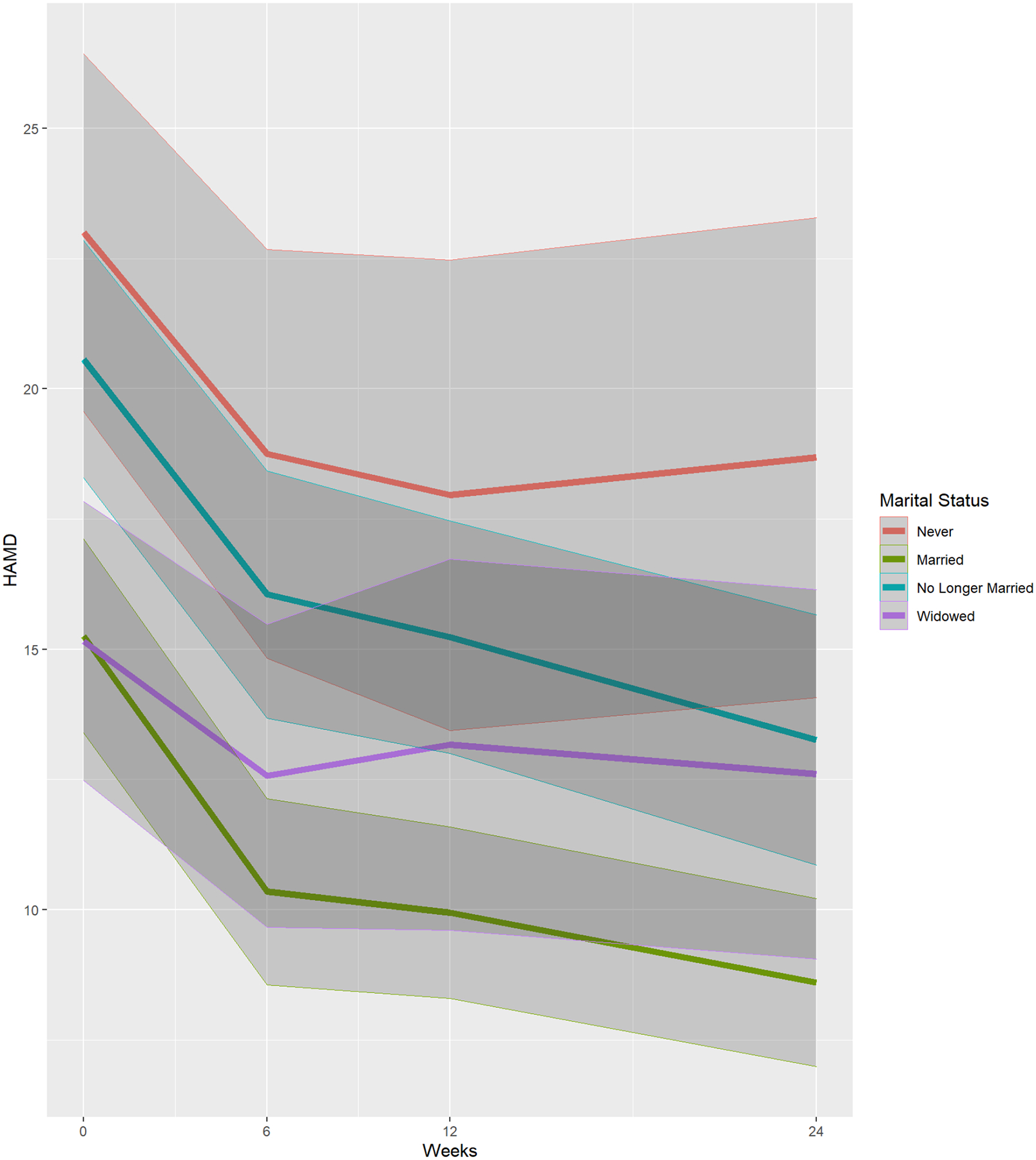
Marital Status as a Predictor of Change in Depression Severity over 24 Weeks
Note. HAMD = Hamilton Depression Severity Scale. Plot includes mean scores with 95% confidence interval. Marital Status was included in the model as a categorical variable with 3 levels: married; never married; no longer married or widowed.
Figure 3.
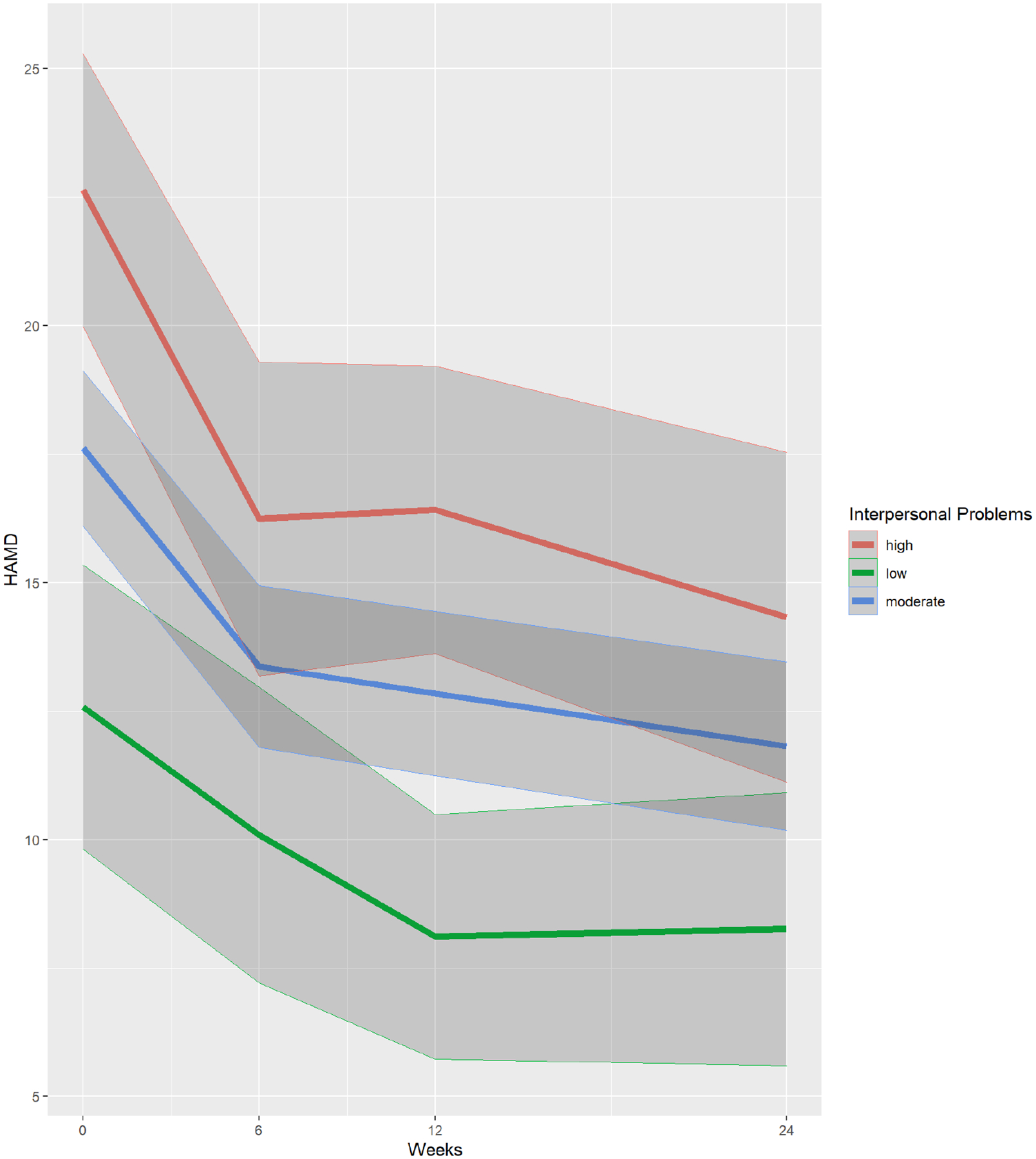
Interpersonal Problems as a Predictor of Change in Depression Severity over 24 Weeks
Note. HAMD = Hamilton Depression Severity Scale. Plot includes mean scores with 95% confidence interval. High scores represent high interpersonal distress. IIP scores were included in the model as continuous variables. For visualization purposes, we divided the variable to three levels here: High (>1 SD above the mean); Moderate (<1 SD above the mean and >1 SD below the mean); and Low (>1 SD below the mean).
Discussion
In this study we examined whether three aspects of social connection measured at the onset of antidepressant treatment for depressed older adults treated in a primary care setting predicted depression severity. Our results show that being married, reporting higher perceived social support, and fewer interpersonal problems were all predictors of lower depression severity on average over the course of 24 weeks. Effect sizes for these effects were in the medium range and clinically meaningful in this sample. Given that the intervention in this study was brief (including 3 sessions over 6 weeks), our results suggest that greater social connection predicts sustained gains from intervention and continued reduction in depression over time. These findings suggest that living in partnership, perceiving others as supportive, and exhibiting low levels of interpersonal problems are all protective factors for depressed middle-aged and older adults. Additionally, our results suggest that brief interventions can significantly improve depression severity among older adults who suffer from social isolation.
The results of this study are consistent with existing literature on the relationship between social connection and depression in late life. The positive benefits of marriage have been long documented, especially for men (41). These include healthier behaviors, reduced mortality, and greater household wealth. When partnership is considered on a continuum, higher levels of social attachment are associated with lower levels of psychological distress (42). In addition, the subjective perception of social support is strongly associated with depressive symptoms and has been shown to have more influence on wellbeing than the quantity of social contacts (1, 31, 43). Finally, there is a high association between depression and interpersonal problems, with estimates of comorbid depression and personality pathology among older adults ranging from 24% (44) to 61% (45). Higher levels of interpersonal problems may interfere with the ability to form stable relationships and contribute to increased distress in response to aging-related stressors. Personality pathology is also associated with poorer treatment outcomes and increased likelihood of depressive relapse after treatment (46).
There are several limitations to this study. First, the study did not include patients who refused to accept a prescription or those who had failed an earlier antidepressant trial. As a secondary data analysis, this study was limited by the availability of variables reflecting social connection. Additional measures of objective social contacts, loneliness, and interpersonal functioning would allow for a more robust investigation. Future studies should consider using longitudinal modeling approaches to explore other factors that may impact the trajectory of change in depression severity over time. Additionally, given that interaction effects in our study were not significant, post-hoc analyses should be considered exploratory and interpreted with caution, pending replication in other studies.
Our findings suggest that assessment of components of social interaction such as marital status, perceived social support, and interpersonal problems can inform our understanding of who is best positioned to benefit from treatment. Primary care providers have a unique opportunity to identify depression among isolated older adults whose symptoms may remain otherwise undetected. In this setting social isolation and poor social relationships could prompt the assessment of depressive symptoms, and in turn, maintaining high quality social contact should be recommended as part of depression treatment in addition to antidepressant adherence. Although the overall symptom severity was higher for older adults with low social connection, there is still evidence that depression interventions in primary care can lessen the severity of symptoms in isolated individuals. Depression treatment for older adults should include recommendations and interventions to improve social engagement.
Supplementary Material
Acknowledgements
Funding
Supported by the National Institute of Mental Health (R01 MH087562, R01 MH087557, and K23 MH123864-01).
Footnotes
Conflicts of Interest
No disclosures to report.
References
- 1.Golden J, Conroy RM, Bruce I, Denihan A, Greene E, Kirby M, & Lawlor BA (2009). Loneliness, social support networks, mood and wellbeing in community-dwelling elderly. International Journal of Geriatric Psychiatry, 24(7), 694–700. [DOI] [PubMed] [Google Scholar]
- 2.Cornwell B, Laumann EO, & Schumm LP. (2008). The Social Connectedness of Older Adults: A National Profile. American Sociological Review, 73(2), 185–203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Nicholson NR (2012). A review of social isolation: an important but underassessed condition in older adults. The Journal of Primary Prevention, 33, 137–152. [DOI] [PubMed] [Google Scholar]
- 4.Perissinotto CM, Cenzer IS, & Covinsky KE. (2012). Loneliness in older persons: A predictor of functional decline and death. Archives of Internal Medicine, 172(14), 1078–1083 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.National Academies of Sciences Engineering & Medicine. (2020). Social isolation and loneliness in older adults: Opportunities for the health care system. The National Academies Press. [PubMed] [Google Scholar]
- 6.Luo Y, Hawkley LC, Waite LJ, & Cacioppo JT. (2012). Loneliness, health, and mortality in old age: A national longitudinal study. Social Science & Medicine, 74(6), 907–914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Evans IE, Llewellyn DJ, Matthews FE, Woods RT, Brayne C, & Clare L (2019). Social isolation, cognitive reserve, and cognition in older people with depression and anxiety. Aging & Mental Health, 23(12), 1691–1700. [DOI] [PubMed] [Google Scholar]
- 8.National Academies of Sciences Engineering and Medicine. (2020). Social Isolation and Loneliness in Older Adults: Opportunities for the Health Care System. Retrieved from Washington, DC: [PubMed] [Google Scholar]
- 9.Peters A, & Liefbroer AC (1997). Beyond marital status: Partner history and well-being in old age. Journal of Marriage and the Family, 59(3), 687–699. [Google Scholar]
- 10.Vanderhorst RK, & McLaren S (2005). Social relationships as predictors of depression and suicidal ideation in older adults. Aging & Mental Health, 9(6), 517–525. [DOI] [PubMed] [Google Scholar]
- 11.Law RW, & Sbarra DA (2009). The effects of church attendance and marital status on the longitudinal trajectories of depressed mood among older adults. Journal of Aging and Health, 21(6), 803–823. [DOI] [PubMed] [Google Scholar]
- 12.Meyers BS, Sirey JA, Bruce M, Hamilton M, Raue P, Friedman SJ, … & Alexopoulos G (2002). Predictors of early recovery from major depression among persons admitted to community-based clinics: an observational study. Archives of General Psychiatry, 59(8), 729–735. [DOI] [PubMed] [Google Scholar]
- 13.Solomonov N, Bress JN, Sirey JA, Gunning FM, Flückiger C, Raue PJ, … & Alexopoulos GS (2019). Engagement in Socially and Interpersonally Rewarding Activities as a Predictor of Outcome in “Engage” Behavioral Activation Therapy for Late-Life Depression. The American Journal of Geriatric Psychiatry, 27(6), 571–578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Solomonov N, Lee J, Banerjee S, Flückiger C, Kanellopoulos D, Gunning FM, Sirey JA, Liston C, Raue PJ, Hull TD, Areán PA, & Alexopoulos GS (2020). Modifiable predictors of nonresponse to psychotherapies for late-life depression with executive dysfunction: a machine learning approach. Molecular Psychiatry. doi: 10.1038/s41380-020-0836-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gülaçtı F (2010). The effect of perceived social support on subjective well-being. Procedia-Social and Behavioral Sciences, 2(2), 3844–3849. [Google Scholar]
- 16.Cornwell EY, & Waite LJ. (2009). Social disconnectedness, perceived isolation, and health among older adults. Journal of Health and Social Behavior, 50(1), 31–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Schwarzbach M, Luppa M, Forstmeier S, König HH, & Riedel-Heller SG (2014). Social relations and depression in late life - A systematic review. International Journal of Geriatric Psychiatry, 29(1), 1–21. [DOI] [PubMed] [Google Scholar]
- 18.Cacioppo JT, Hughes ME, Waite LJ, Hawkley LC, & Thisted RA. (2006). Loneliness as a specific risk factor for depressive symptoms: cross-sectional and longitudinal analyses. Psychology and Aging, 21(1), 140–151. [DOI] [PubMed] [Google Scholar]
- 19.Cacioppo JT, Hawkley LC, & Thisted RA (2010). Perceived social isolation makes me sad: 5-year cross-lagged analyses of loneliness and depressive symptomatology in the Chicago Health, Aging, and Social Relations Study. Psychology and Aging, 25(2), 453–463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hallgren M, Lundin A, Tee FY, Burström B, & Forsell Y (2017). Somebody to lean on: Social relationships predict post-treatment depression severity in adults. Psychiatry Research, 249, 261–267. [DOI] [PubMed] [Google Scholar]
- 21.Oxman TE, & Hull JG (2001). Social support and treatment response in older depressed primary care patients. The Journals of Gerontology Series B: Psychological Sciences and Social Sciences, 56(1), P35–P45. [DOI] [PubMed] [Google Scholar]
- 22.Hames JL, Hagan CR, & Joiner TE (2013). Interpersonal processes in depression. Annual Review of Clinical Psychology, 9, 355–377. [DOI] [PubMed] [Google Scholar]
- 23.Lewis G, Kounali DZ, Button KS, Duffy L, Wiles NJ, Munafo MR, … & Lewis G. (2017). Variation in the recall of socially rewarding information and depressive symptom severity: a prospective cohort study. Acta Psychiatrica Scandinavica, 135(5), 489–498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Burholt V, & Scharf T (2013). Poor health and loneliness in later life: the role of depressive symptoms, social resources, and rural environments. Journals of Gerontology Series B: Psychological Sciences and Social Sciences, 49, 311–324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bagby RM, Quilty LC, Segal ZV, McBride CC, Kennedy SH, & Costa PT Jr (2008). Personality and differential treatment response in major depression: a randomized controlled trial comparing cognitive-behavioural therapy and pharmacotherapy. The Canadian Journal of Psychiatry, 53(6), 361–370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Quilty LC, Mainland BJ, McBride C, & Bagby RM (2013). Interpersonal problems and impacts: Further evidence for the role of interpersonal functioning in treatment outcome in major depressive disorder. Journal of Affective Disorders, 150(2), 393–400. [DOI] [PubMed] [Google Scholar]
- 27.Kushner SC, Quilty LC, Uliaszek AA, McBride C, & Bagby RM (2016). Therapeutic alliance mediates the association between personality and treatment outcome in patients with major depressive disorder. Journal of Affective Disorders, 201, 137–144. [DOI] [PubMed] [Google Scholar]
- 28.Sirey JA, Banerjee S, Marino P, Bruce ML, Halkett A, Turnwald M, … Kales HC (2017). Adherence to Depression Treatment in Primary Care: A Randomized Clinical Trial. JAMA Psychiatry, 74(11), 1129–1135. doi: 10.1001/jamapsychiatry.2017.3047 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sirey JA, Woods A, Solomonov N, Evans L, Banerjee S, Alexopoulos G, Kales HC (in press). Treatment Adequacy and Adherence as Predictors of Depression Response in Primary Care. American Journal of Geriatric Psychiatry. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Koenig HG, Westlund RE, George LK, Hughes DC, Blazer DG, & Hybels C. (1993). Abbreviating the Duke Social Support Index for use in chronically ill elderly individuals. Psychosomatics, 34(1), 61–69. [DOI] [PubMed] [Google Scholar]
- 31.George LK, Blazer DG, Hughes DC, & Fowler N (1989). Social support and the outcome of major depression. The British Journal of Psychiatry, 154(4), 478–485. [DOI] [PubMed] [Google Scholar]
- 32.Horowitz LM, Rosenberg SE, Baer BA, Ureño G, & Villaseñor VS (1988). Inventory of interpersonal problems: psychometric properties and clinical applications. Journal of Consulting and Clinical Psychology, 56(6), 885–892. [DOI] [PubMed] [Google Scholar]
- 33.Scarpa A, Luscher KA, Smalley KJ, Pilkonis PA, Kim Y, & Williams WC (1999). Screening for personality disorders in a nonclinical population. Journal of Personality Disorders, 13(4), 345–360. [DOI] [PubMed] [Google Scholar]
- 34.Folstein ME (1975). A practical method for grading the cognitive state of patients for the clinician. Journal of Psychiatric Research, 12, 198–198. [DOI] [PubMed] [Google Scholar]
- 35.Hamilton M (1960). A rating scale for depression. J Neurol Neurosurg Psychiatry, 23, 56–62. doi: 10.1136/jnnp.23.1.56 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Trajković G, Starčević V, Latas M, Leštarević M, Ille T, Bukumirić Z, & Marinković J (2011). Reliability of the Hamilton Rating Scale for Depression: a meta-analysis over a period of 49 years. Psychiatry Research, 189(1), 1–9. [DOI] [PubMed] [Google Scholar]
- 37.Svarstad BL, Chewning BA, Sleath BL, & Claesson C (1999). The Brief Medication Questionnaire: a tool for screening patient adherence and barriers to adherence. Patient Educ Couns, 37(2), 113–124. [DOI] [PubMed] [Google Scholar]
- 38.Rickles NM, & Svarstad BL (2007). Relationships between multiple self-reported nonadherence measures and pharmacy records. Res Social Adm Pharm, 3(4), 363–377. doi:S1551–7411(06)00118–5 [pii] 10.1016/j.sapharm.2006.11.001 [DOI] [PubMed] [Google Scholar]
- 39.Brook OH, van Hout HP, Stalman WA, & de Haan M (2006). Nontricyclic antidepressants: predictors of nonadherence. J Clin Psychopharmacol, 26(6), 643–647. doi: 10.1097/01.jcp.0000246217.34024.53 [DOI] [PubMed] [Google Scholar]
- 40.R Core Team. (2017). R: A language and environment for statistical computing. Vienna, Austria. [Google Scholar]
- 41.Waite LJ (1995). Does marriage matter? Demography, 32(4), 483–507. [PubMed] [Google Scholar]
- 42.Ross CE (1995). Reconceptualizing marital status as a continuum of social attachment. Journal of Marriage and the Family, 57(1), 129–140. [Google Scholar]
- 43.Wallsten SM, Tweed DL, Blazer DG, & George LK (1999). Disability and depressive symptoms in the elderly: The effects of instrumental support and its subjective appraisal. The International Journal of Aging and Human Development, 48(2), 145–159. [DOI] [PubMed] [Google Scholar]
- 44.Kunik ME, Mulsant BH, Rifai AH, Sweet RA, Pasternak R, & Zubenko GS (1994). Diagnostic rate of comorbid personality disorder in elderly psychiatric inpatients. The American Journal of Psychiatry, 151(4), 603–605. [DOI] [PubMed] [Google Scholar]
- 45.Molinari V, & Marmion J (1995). Relationship between affective disorders and Axis II diagnoses in geropsychiatric patients. Journal of Geriatric Psychiatry and Neurology, 8(1), 61–64. [PubMed] [Google Scholar]
- 46.Morse JQ, & Lynch TR (2004). A preliminary investigation of self-reported personality disorders in late life: prevalence, predictors of depressive severity, and clinical correlates. Aging & Mental Health, 8(4), 307–315. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


