Introduction
Taxanes, such as docetaxel, are chemotherapeutics used to treat various malignancies. In this report, we discuss a patient with prostate cancer who developed a taxane-induced sclerodermoid reaction, a rare adverse effect of these medications.
Case report
A 69-year-old man with a history of prostate cancer treated with radiation presented to the clinic with progressively worsening and persistent foot pain. Three years prior to the presentation, he was diagnosed with prostate cancer that required proton beam therapy and hormone therapy. Because of the cancer recurrence, he later enrolled in a clinical trial that used docetaxel and degarelix. Shortly thereafter, he noted bilateral swelling of his feet that initially responded well to furosemide treatment. These symptoms gradually progressed into sharp, burning pain that radiated along his inner thighs. Gabapentin treatment provided mild improvement. During this visit, he complained of taut skin, constant paresthesia, and intermittent razor-like pain in both feet. He denied any muscle weakness, bowel or bladder disturbances, or similar symptoms elsewhere. Physical examination of his feet revealed erythematous, indurated, leathery-like skin that extended up to the thighs, bilateral hair loss, and onychodystrophy (Fig 1). The upper extremities, cardiopulmonary, and abdominal examinations were unremarkable. Laboratory studies were ordered, and a 4-mm punch biopsy specimen from the right leg was obtained for histopathology (Fig 2).
Fig 1.

Bilateral feet demonstrating alopecia, erythema, induration, and onychodystropy.
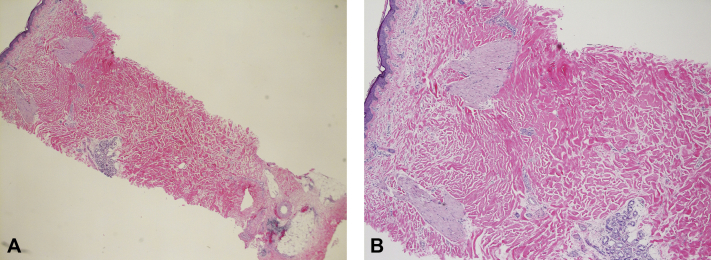
Fig 2.
Histopathology of punch biopsy taken from the anterior aspect of the right thigh. A, Low magnification. B, Medium magnification. (A and B, Hematoxylin-eosin stain.)
Histopathologic examination revealed an increased dermal thickness and thickened, focally homogenized collagen bundles in the reticular dermis, consistent with dermal sclerosis. Superficial and deep perivascular infiltrate of lymphocytes and plasma cells were also observed. Serology results were negative for antinuclear, antitopoisomerase, anticentromere, and anticardiolipin antibodies. Comprehensive metabolic panel, complete blood cell count, erythrocyte sedimentation rate, and C-reactive protein were unremarkable. The history, physical examination findings, and biopsy results confirmed a diagnosis of a docetaxel-induced sclerodermoid reaction. The patient declined methotrexate therapy because of polypharmacy and the potential side effects. The induration and paresthesia have slowly improved since he completed the docetaxel course 9 months ago. Prostate cancer has responded well to the chemotherapy.
Discussion
Docetaxel and paclitaxel belong to the taxane class of chemotherapeutics that are widely used to treat various malignancies. Their primary mechanism of action is the disruption of microtubule polymerization.1 Common adverse effects of these medications include neutropenia, myelosuppression, cardiotoxicity, neurotoxicity, and hypersensitivity reactions.2 Taxane-induced sclerodermoid reaction is a rare side effect, with only a handful of cases having been documented. The lower extremities are most frequently affected and can lead to severe limitations in joint mobility. Although the pathogenesis of this phenomenon is unclear, paraneoplastic, pseudo–graft-versus-host disease, and autoimmune etiologies have been hypothesized.3
Diagnosis of taxane-induced sclerodermoid reaction requires a high clinical suspicion. Several months after the initiation of docetaxel or paclitaxel treatment, patients may complain of painful acral erythema (erythrodysesthesia), which can resolve before the subsequent dose, paresthesia, and peripheral edema that is responsive to diuretics.4 Many patients who are placed on such chemotherapies are likely on other medications that can muddy the diagnosis. Immunofluorescence, serology, and routine laboratory tests are often unremarkable. A full-thickness skin biopsy with histopathology reveals fibrous septae of the subcutaneous fat and thickened collagen bundles, along with diffuse perivascular inflammatory cell infiltrates.1,2 Discontinuation of the taxane tends to resolve the edema and scleroderma-like skin changes within a year. Evidence of steroids in the management is conflicting, although concomitant use with methotrexate may lead to a more rapid regression.5
The differential diagnoses include systemic sclerosis (scleroderma), eosinophilic fasciitis, and radiation-induced skin fibrosis. The key features that distinguish docetaxel-induced sclerodermoid reaction from systemic sclerosis (scleroderma) include the timing of the rapid progression of dermal involvement, improvement after discontinuing the medication, and absence of autoimmune endothelial injury on biopsy specimens.2 Aside from taxanes, other mimics of systemic sclerosis may include exposure to organic solvents (eg, vinyl chloride, benzene, toluene), medications (eg, bleomycin, valproate, carbidopa, pentazocine), and certain substances (eg, rapeseed oil, L-tryptophan).3,6 Eosinophilic fasciitis is another scleroderma-like disorder causing acutely painful, swollen extremities, and indurated peau d'orange skin that ultimately progresses into contractures and disability.7 Histopathology reveals a sclerosing process with a lymphocytic infiltrate containing eosinophils; laboratory tests will be notable for a mildly elevated erythrocyte sedimentation rate and polyclonal hypergammaglobulinemia.7 Radiation-induced skin fibrosis is a chronic condition that develops within 4 to 12 months after radiotherapy, and it is characterized by soft tissue atrophy, alopecia, scarring, retraction, and stiffness.8 Histology of radiation-induced skin fibrosis shows evidence of extensive hyalinization of reticular collagen.
Conflicts of interest
None disclosed.
Acknowledgments
We thank the patient for granting permission to publish this information and Raymond Zhu, MD, for contributing to the final pathology interpretation.
Footnotes
Funding sources: None.
IRB approval status: Not applicable.
References
- 1.Battafarano D.F., Zimmerman G.C., Older S.A., Keeling J.H., Burris H.A. Docetaxel (Taxotere) associated scleroderma-like changes of the lower extremities. A report of three cases. Cancer. 1995;76(1):110–115. doi: 10.1002/1097-0142(19950701)76:1<110::aid-cncr2820760117>3.0.co;2-9. [DOI] [PubMed] [Google Scholar]
- 2.Sibaud V., Lebœuf N.R., Roche H. Dermatological adverse events with taxane chemotherapy. Eur J Dermatol. 2016;26(5):427–443. doi: 10.1684/ejd.2016.2833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Farrant P.B.J., Mortimer P.S., Gore M. Scleroderma and the taxanes. Is there really a link? Clin Exp Dermatol. 2004;29(4):360–362. doi: 10.1111/j.1365-2230.2004.01519.x. [DOI] [PubMed] [Google Scholar]
- 4.Pedersen J.V., Jensen S., Krarup-Hansen A., Riis L. Scleroderma induced by paclitaxel. Acta Oncol. 2010;49(6):866–868. doi: 10.3109/02841861003702510. [DOI] [PubMed] [Google Scholar]
- 5.Kilic M.O., Yalaza M., Bilgic C.I., Dener C. Docetaxel-induced scleroderma in a breast cancer patient: a case report. J Breast Health. 2015;11(2):95–97. doi: 10.5152/tjbh.2015.1879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Perez M.I., Kohn S.R. Systemic sclerosis. J Am Acad Dermatol. 1993;28(4):525–547. doi: 10.1016/0190-9622(93)70072-2. [DOI] [PubMed] [Google Scholar]
- 7.Oza V.S., Walsh R., North J., Berger T.G., Murase J.E. Treatment of eosinophilic fasciitis with sirolimus. JAMA Dermatol. 2016;152(4):488–490. doi: 10.1001/jamadermatol.2016.0048. [DOI] [PubMed] [Google Scholar]
- 8.Borrelli M.R., Shen A.H., Lee G.K., Momeni A., Longaker M.T., Wan D.C. Radiation-induced skin fibrosis: pathogenesis, current treatment options, and emerging therapeutics. Ann Plast Surg. 2019;83(4S suppl 1):S59–S64. doi: 10.1097/SAP.0000000000002098. [DOI] [PMC free article] [PubMed] [Google Scholar]