Abstract
Background
Transient global amnesia (TGA) is a clinical syndrome characterized by a temporary short-term memory loss with inability to retain new memories, usually lasting 2 to 8 h. TGA may be related to several medical procedures, including angiography, general anesthesia, gastroscopy.
Case presentation
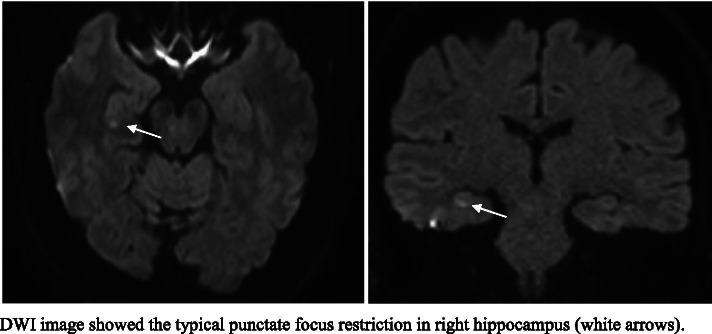
We report a 58-year-old woman who experiencing TGA one hour after the execution of her first-time nasopharyngeal swab for COVID-19. Brain MRI showed a typical punctate Diffusion Weight Image (DWI) hippocampal lesion.
Conclusions
This is the first report of TGA after the execution of nasopharyngeal swab for COVID-19. This association lengthen the list of medical procedures associated with TGA, and we discuss the possible plausible mechanisms by which a nasopharyngeal swab could trigger TGA.
Keywords: COVID-19, SARS-COV-2, TGA, Nasopharyngeal swab, Case report
Background
Several medical procedures have been found to be associated with transient global amnesia (TGA), With cerebral and coronary angiography as the most common antecedents [1].
Proposed triggers are the same as non-procedure-related TGA and include acute pain, migraine, Valsalva maneuver-associated activities, and different stress-related events. These latter, including emotional, psychological, and physical stress, are thought to influence hippocampal status through several different mechanisms, ultimately leading to neuro-inflammation, oxidative stress, and neurotoxicity [2]. The characteristic memory disturbances and hippocampal lesions are thought to result from non-specific vasomotor changes (vasospasm, hippocampal hypoperfusion) or from peri-procedural use of specific drugs, peculiarly affecting susceptible, memory-relevant structures of the temporal-limbic circuit [3].
The nasopharyngeal swab is usually perceived as uncomfortable and produces a bad memory in the tested population; it is the gold standard technique for diagnosing Coronavirus disease 19 (COVID-19) active infection, and several millions of tests are being performed. Adverse effects include short lasting pain, epistaxis, headache, ear and nose discomfort, rhinorrhea [4].
Disproportionate terrors about the swab are somehow fueled by media and sensationalistic journalism: people who have had the COVID-19 swab test say it feels like their “brain is being pierced by an oversized cotton bud”. A case of cerebrospinal fluid leak has been recently reported, pertaining a patient with a previously undiagnosed skull base defect at the fovea ethmoidalis [5].
Nasopharyngeal swab has not been previously reported among the procedures associated with TGA, likely because nasopharyngeal swab was not such a common procedure until these latter months.
Case presentation
We report of a 58-year-old woman, who did not suffer from any pre-existing medical conditions, with the only exception of being mildly overweight (BMI 31.25). In particular, she did not smoke, she had no history of migraine, and she did not receive any hormone replacement therapy after menopause, that occurred at age 51. One hour after the execution of her first-time (later revealing as negative) nasopharyngeal swab, while driving home, she likely experienced amnesia: the bystanders reported that the woman pulled over the car, lowered the window and called for rescue, telling she was unable to find the right direction; when she was asked where she was going, she answered she did not remember and began to behave anxiously. The bystanders reported that she could tell her name and other personal information, and that she could herself remember the unlock code of her phone and call her husband. The husband noticed she was disoriented, repeatedly asking the same questions about where she was and what she was doing. This episode lasted for about two hours then reverted; the day after, she was conducted to our attention for evaluation. A memory gap for the episode persisted: she could remember having had the swab tested, then having paid for the test, having left the hospital, and reached the car after the procedure, but she could not remember the following events, including those witnessed by the by-standers and including the call to her husband and its arrival on the place where she had left her car.
Neurological examination was normal. Brain MRI, performed one day after TGA, revealed a hippocampal punctate area of DWI restriction (Fig. 1), confirming the clinical suspect. Supra-aortic vessels Duplex ultrasonography and EEG were negative, ruling out mimics. The strict temporal relationship between nasopharyngeal swab and TGA may have been simply coincidental, but we are usually prone to investigate each time carefully the triggers for TGA, since TGA recent anamnesis is often full of peculiar, even bizarre, but usually biologically fitting antecedents.
Fig. 1.
Brain MRI
Discussion and conclusions
We believe that the swab may have acted as a TGA trigger, via a series of potentially plausible mechanisms:
First, direct touch stimulation of the lower nasal and pharyngeal structures, innervated by the sensory terminations of the Xth nerve, may cause cerebral vasomotor phenomena via central vagal nuclei, which are known to be involved in sympathetic cardiovascular regulation.
Second, the procedure itself may be intended as a Valsalva-like maneuver: indeed, the nasopharyngeal swab could cause a temporary stop at the glottis, or, even more peripherally, at the nasopharynx or at the nostrils.
Last, the swab is often loaded with emotional stress, both directly related to the local pain and discomfort, and, in the pandemic context, also more generically related to worrying for the result and its practical consequences. Indeed, stress-related triggers (including emotional and psychological stress) my lead to hippocampal dysfunction via several mechanism, involving glutamate neurotoxicity, release of vasoactive stress hormones such as angiotensin I and II, and oxidative stress [2].
With this note, we would suggest that nasopharyngeal swab might lengthen the list of medical procedures associated with TGA, by multiple potential mechanisms. In our patient, the free time-interval between the procedure and the onset of TGA supports the occurrence of an indirect mechanism, such as emotional stress and pain, rather than Valsalva-like or direct vasomotor effects via the vagus nerve. Indeed, direct pain to the brain parenchyma is believed to have a role even in TGAs following cerebral angiography, that is by far the most common procedure associated with TGA.
Reluctantly paraphrasing sensationalistic magazines, we suggest that a nasopharyngeal swab can, in fact, “pierce your brain”, or rather your hippocampus, in the form of a short-time memory loss: perhaps that is what you need to forget the swab and this pandemic emergency, Freud would have said.
Acknowledgements
Not applicable
Abbreviations
- TGA
Transient global amnesia
- COVID-19
Coronavirus disease 19
- DWI
Diffusion Weight Image
Authors’ contributions
Dr. IC and Dr. SR were involved in the work-up of the patient, planning and conducting investigations, and providing clinical care. Dr. LA reviewed and revised the manuscript and the literature. Dr.Dr. SR, Dr. AZ, Dr. IC planned the case report, drafted the initial manuscript, reviewed, and revised the manuscript and the literature. All the author approved the final manuscript as submitted.
Funding
The department of molecular medicine of Pavia University funded this study.
Availability of data and materials
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.
Declarations
Ethics approval and consent to participate
No investigations or interventions were performed outside routine clinical care for this patient. As this is a case report, without experimental intervention into routine care, no formal research ethics approval was required; Written, fully informed consent was given and recorded to all study procedures.
Consent for publication
Written, fully informed consent was given and recorded from the patient for both print and online publication.
Competing interests
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Jeong M, Kim WS, Kim AR, Park JJ, Choi DH, Kim HY. Medical procedure-related transient global amnesia. Eur Neurol. 2018;80(1–2):68–70. doi: 10.1159/000493163. [DOI] [PubMed] [Google Scholar]
- 2.Liampas I, Raptopoulou M, Siokas V, Bakirtzis C, Tsouris Z, et al. Conventional cardiovascular risk factors in transient global amnesia: systematic review and proposition of a novel hypothesis. Front Neuroendocrinol. 2021;61:100909. doi: 10.1016/j.yfrne.2021.100909. [DOI] [PubMed] [Google Scholar]
- 3.Jang J-W, Park SY, Hong J-H, Park YH, Kim JE, Kim S. Different risk factor profiles between transient global amnesia and transient ischemic attack: a large case-control study. Eur Neurol. 2014;71(1–2):19–24. doi: 10.1159/000354023. [DOI] [PubMed] [Google Scholar]
- 4.Gupta K, Bellino PM, Charness ME. Adverse effects of nasopharyngeal swabs: three-dimensional printed versus commercial swabs. Infect Control Hosp Epidemiol. 2020;1:641–642. doi: 10.1017/ice.2020.297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sullivan CB, Schwalje AT, Jensen M, Li L, Dlouhy BJ, Greenlee JD, et al. Cerebrospinal fluid leak after nasal swab testing for Coronavirus disease 2019. JAMA Otolaryngol Neck Surg. 2020 doi: 10.1001/jamaoto.2020.3579. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.