Abstract
Background
Neonatal infectious spondylodiscitis is a rare bony infection with atypical clinical presentation and non-specific systemic symptoms. Diagnosis and treatment are often delayed resulting in vertebral destruction and severe complications. We retrospectively reviewed the case of an infant with infectious spondylodiscitis resulting in T12 body destruction and marked angular kyphosis.
Case-report
A 4-week-old infant developed an infectious spondylodiscitis resulting in destruction of the T12 vertebral body and involvement of disc between T12 and L1. At 6 months of age, X-ray showed a marked thoracolumbar angular kyphosis above 50 Cobb degrees. Therefore, the patient underwent single time surgery with double anterior and posterior approach. At 9 years follow up, clinical and radiological findings show a stable correction with good aesthetic appearance.
Conclusion
Neonatal spondylodiscitis could lead to marked kyphosis similar to the congenital one. Since treatment with casts and tutors is often inefficacious, prompt surgery should be considered. The double anterior and posterior approach is the best option in this condition.
Keywords: Spondylodiscitis, Infant, Bony destruction, Kyphosis
Introduction
Primary pyogenic spinal infections are uncommon entities in children. The estimated incidence of discitis and spondylodiscitis is 1–2 cases per year per 32,500 pediatric hospital evaluations [1], representing approximately 3% of all the cases of osteoarticular infections [2]. The age distribution of pediatric spondylodiscitis is triphasic: the first peak occurs in early childhood (79%), between the age of 6 months and 4 years, a smaller later peak in the juvenile and adolescent group (20%), and only exceptional infections in children aged under 6 months (1%) [3]. The lumbar region is the spine level predominately involved, and the most common causative organism is Staphylococcus aureus [4]. Unlike older children, neonates and infants with spondylodiscitis are often systemically ill with the involvement of multiple infectious foci. Therefore, early diagnosis and treatment are crucial as the vertebrae can be severely damaged or entirely destroyed [5, 6].
We present an infant who developed hematogenous spondylodiscitis resulting in vertebral body destruction and marked angular kyphosis. The deformity was surgically treated, leading to a stable overtime correction.
Case presentation
A 4-week-old boy presented to the emergency department with a history of hyporeactivity, feeding difficulties and failure to thrive. On examination, he was pale, hyporeactive with dystrophic appearance. After 10 days of hospitalization, he developed low-grade fever (37.5 °C maximum temperature) and a tender spinal tumefaction in the thoracolumbar region. The lower extremities did not present limitations of movement, asymmetries, or pain under passive mobilization. The whole-body magnetic resonance imaging (MRI) showed the destruction of the T12 vertebral body with the involvement of disc between T12 and L1 (Fig.1). The laboratory tests showed a white blood cell count of 18.3 × 109 per liter, with a differential of 54.9% neutrophils and 28.0% lymphocytes. The C-reactive protein was 1.19 mg/dL (normal value < 0.5 mg/dL). A vertebral body osteomyelitis was suspected and an empiric antibiotic therapy with tobramycin, vancomycin and amphotericin was started. Blood cultures were positive for Staphylococcus aureus and intravenous vancomycin only was continued for total 6 weeks. A thorough physical reevaluation could not highlight a primary focus of Staphylococcus infection leading to the spondylodiscitis.
Fig. 1.
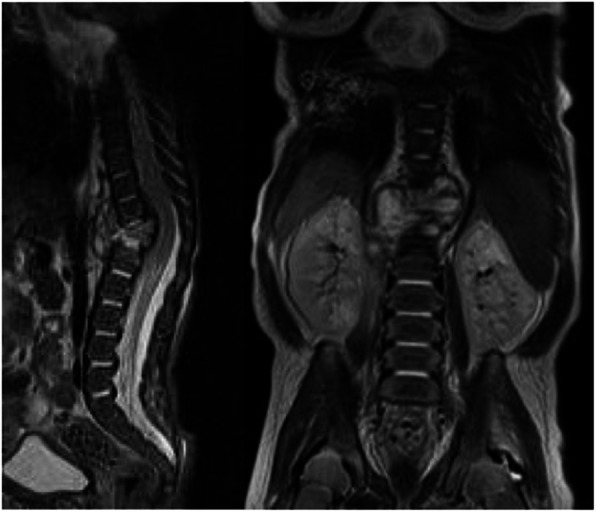
MRI at 5 weeks of age showing the destruction of the T12 vertebral body with involvement of disc between T12 and L1
At the age of 6 months, X-ray showed almost complete destruction of T12 body and L1 body partially, with evidence of thoracolumbar angular kyphosis above 50 Cobb degrees. Kyphosis worsened in the following months despite the Milwaukee brace use (Fig. 2). Therefore, at the age of 2 years, he underwent circumferential vertebral fusion from T11 to L2: the hooks were posteriorly instrumented, while a titanium cage of bank bone graft was positioned anteriorly, through left retroperitoneal access (Fig. 3).
Fig. 2.
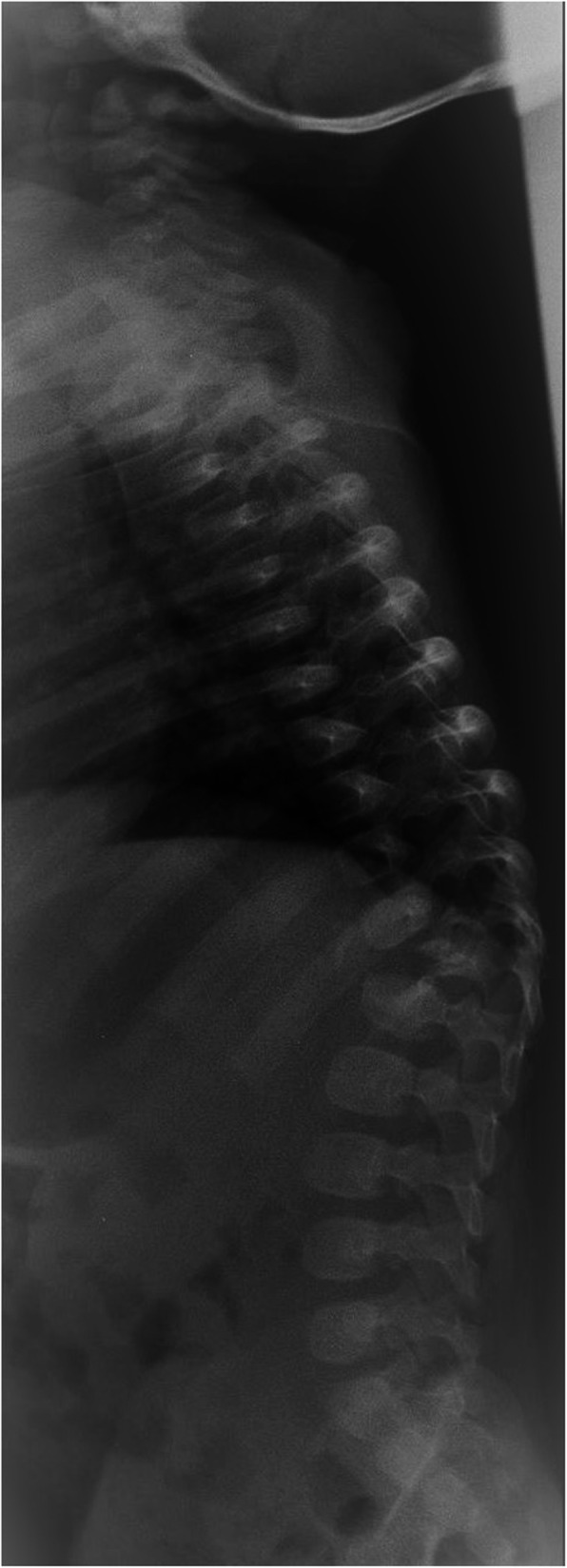
Lateral radiograph at 6 months of age shows the almost complete destruction of T12 vertebral body, resulting in angular kyphosis above 50°
Fig. 3.
Pre-operatory clinical aspect (a), plain radiographs at 2 years of age showing the persistent and progressive kyphosis (b) and post-operatory standing lateral radiograph showing the double approach with posterior hooks and anterior bank bone graft titanium cage from T11 to L2 (c)
At present, 9 years after the operation, the patient leads a normal life, no neurological deficiencies were detected, and X-ray shows a stable correction with spine sagittal curves within the physiological limits (Fig. 4).
Fig. 4.
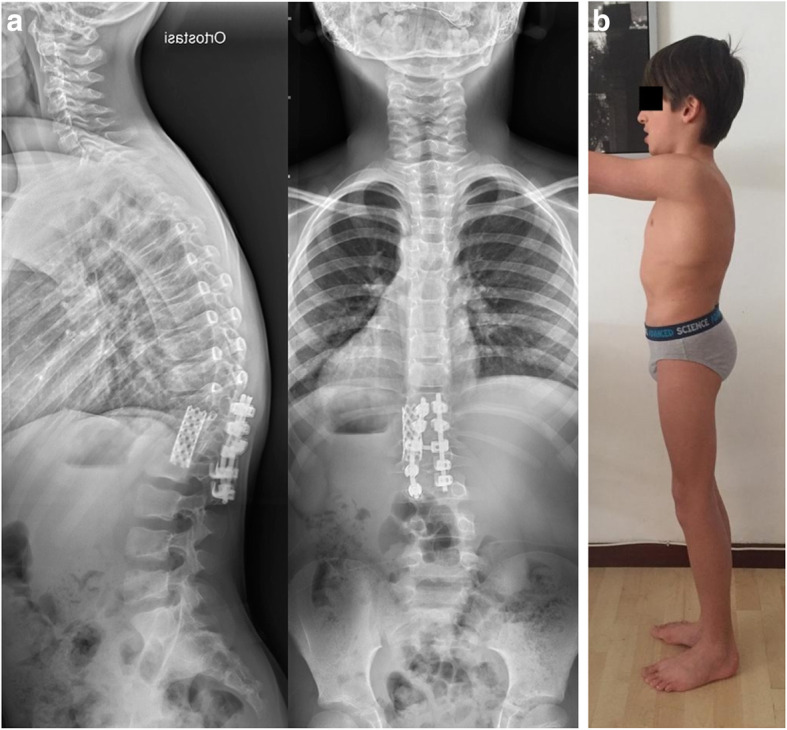
Standing radiographs (a) and clinical aspect (b) showing the permanent deformity correction at 9 years of age
Discussion
Neonatal infectious spondylodiscitis accounts for 2 to 4% of bony infections in neonates [7]. Risk factors include prematurity with low birth weight, catheterization of the umbilical vessel, and other invasive procedures [8].
Staphylococcus aureus is the most prevalent cause in approximately 80 to 90% of cases. Other agents, less commonly identified, are coagulase-negative Staphylococcus, α-hemolytic Streptococcus, Streptococcus pneumoniae, Escherichia coli and Salmonella spp. [4]. In most patients, pathogens reach the spine by hematogenous route, involving first the disc and subsequently the adjacent vertebral endplates through supply vessels that generally persist until the seventh year of life4. Due to the atypical presentation, diagnosis is usually delayed leading to extensive vertebral destruction and subsequent deformation [5, 6]. Magnetic resonance is the first-choice imaging, allowing the delineation of spinal cord compression, bony destruction, and abscess extension [9]. Invasive investigations, such as biopsy or aspirations, should be conducted on children who fail to improve with antibiotic treatment or when the presence of atypical organisms is suspected [5].
The fusion of kyphosis of this type requires the execution of a posterior and anterior arthrodesis to obtain a result that remains stable over time. Considering the patient size, an autologous bone grafting was not feasible. In the anterior surgery, it is advisable to use support with good mechanical strength; although a strut graft could be taken into account, we preferred using a titanium cervical cage filled with bank bone grafts. This rigid structure showed moderate subsidence but was overall stable in maintaining the correction obtained. This stability was obtained, limiting the fusion to five vertebrae, with little consequences on the trunk motility and good aesthetic appearance.
Conclusion
Neonatal spondylodiscitis could lead to vertebral body destruction with resulting angular kyphosis. It is often similar to congenital forms in terms of the type of deformity, radiological aspect, and indications for treatment [10, 11]. Treatment with plaster or orthopedic brace is doomed to failure. Surgery must be performed at an early stage, as soon as worsening occurs to avoid the onset of more severe deformities, possible neurological damage, and higher surgical risks.
Acknowledgments
The authors thank Martina Bradaschia for the English revision of the manuscript.
Authors’ contributions
All authors listed on the manuscript has seen and approved the submission of this version of the manuscript and takes full responsibility for the manuscript.
Funding
No funds were received in support of this work.
Availability of data and materials
No supporting data are available.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
The authors declare that we have obtained the written consent from the parents of the patient for publication of the photographs in all forms and media.
Competing interests
No relevant financial activities outside the submitted work.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Sara Romano, Email: sara.romano17@gmail.com.
Francesca Vittoria, Email: francesca.vittoria@burlo.trieste.it.
Elisabetta Cattaruzzi, Email: elisabetta.cattaruzzi@burlo.trieste.it.
Egidio Barbi, Email: egidio.barbi@burlo.trieste.it.
Marco Carbone, Email: marco.carbone@burlo.trieste.it.
References
- 1.Cushing AH. Diskitis in children. Clin Infect Dis. 1993;17(1):1–6. doi: 10.1093/clinids/17.1.1. [DOI] [PubMed] [Google Scholar]
- 2.Ferroni A, Al Khoury H, Dana C, et al. Prospective survey of acute osteoarticular infections in a French paediatric orthopedic surgery unit. Clin Microbiol Infect. 2013;19(9):822–828. doi: 10.1111/clm.12031. [DOI] [PubMed] [Google Scholar]
- 3.Dayer R, Alzahrani MM, Saran N, et al. Spinal infections in children. A multicenter retrospective study. Bone Joint J. 2018;100:542–548. doi: 10.1302/0301-620X.100B4.BJJ-2017-1080.R1. [DOI] [PubMed] [Google Scholar]
- 4.Principi N, Esposito S. Infectious discitis and spondylodiscitis in children. Int J Mol Sci. 2016;17(4):539. doi: 10.3390/ijms17040539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fernandez M, Carrol CL, Baker CJ. Discitis and vertebral osteomyelitis in children: an 18-year review. Pediatrics. 2000;105(6):1299–1304. doi: 10.1542/peds.105.6.1299. [DOI] [PubMed] [Google Scholar]
- 6.Tsirikos AI, Tome-Bermejo F. Spondylodiscitis in infancy. A potentially fatal condition that can lead to major spinal complications. J Bone Joint Surg (Br) 2012;94(10):1399–1402. doi: 10.1302/0301-620X.94B10.29602. [DOI] [PubMed] [Google Scholar]
- 7.Eismont FJ, Bohlman HH, Soni PL, et al. Vertebral osteomyelitis in infants. J Bone Joint Surg (Br) 1982;64:32–35. doi: 10.1302/0301-620X.64B1.7068717. [DOI] [PubMed] [Google Scholar]
- 8.van Daleen IV, Heeg M. Neonatal infectious spondylitis of the cervical spine presenting with quadriplegia. A Case Report. Spine. 2000;25:1450–1452. doi: 10.1097/00007632-200006010-00019. [DOI] [PubMed] [Google Scholar]
- 9.Hadjipavlou AG, Mader JT, Necessary JT, Muffoletto AJ. Hematogenous pyogenic spinal infections and their surgical management. Spine. 2000;25(13):1668–1679. doi: 10.1097/00007632-200007010-00010. [DOI] [PubMed] [Google Scholar]
- 10.McMaster MJ, Singh H. Natural history of congenital kyphosis and kyphoscoliosis: a study of 112 patients. J Bone Joint Surg. 1999;81(10):1367–1383. doi: 10.2106/00004623-199910000-00002. [DOI] [PubMed] [Google Scholar]
- 11.McMaster MJ, Singh H. The surgical management of congenital kyphosis and kyphoscoliosis. Spine. 2001;19:2146–2155. doi: 10.1097/00007632-200110010-00021. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
No supporting data are available.



