To the editor:
Several reports of newly diagnosed or relapses of immune-mediated renal diseases following vaccination with anti–severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) mRNA and AstraZeneca vaccines recently emerged in the litterature.1 , 2
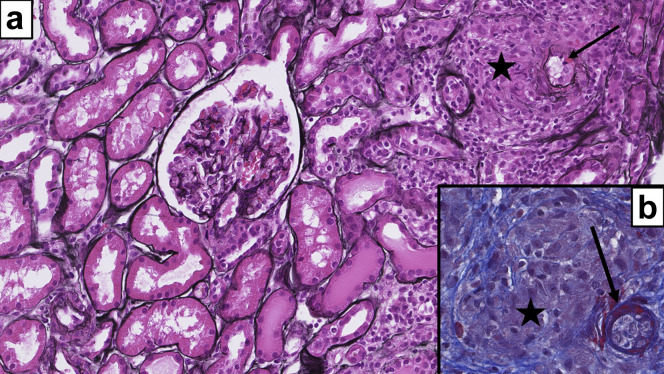
We report the case of a 77-year-old man who developed an acute granulomatous nephritis associated with vasculitis after the first dose of the AstraZeneca vaccine. The patient had no significant medical history, and serum creatinine (SCr) was 1.2 mg/dl a month before vaccination with a protein-to-creatinine ratio at 0.07 g/g (N = 0.15) of creatinine. Four weeks after injection, the patient presented with fever, night sweating, and anorexia. He was not taking any medication. Laboratory tests revealed acute kidney injury (SCr, 2.7 mg/dl), normal proteinuria, no hematuria, and a C-reactive protein (CRP) level of 200 mg/L. Nasopharyngeal swab for SARS-CoV-2 was negative by polymerase chain reaction, as were anti–SARS-CoV-2 and anti-neutrophil cytoplasmic antibodies (repeated twice 15 days apart). Fluorine-18-fluorodeoxyglucose positron emission tomography scan showed diffuse hypermetabolism of medium vessels, suggesting vasculitis. The kidney biopsy revealed diffuse interstitial edema with noncaseating nonnecrotizing granulomas around small vessels (Figure 1 ); one showed fibrinoid necrosis. There were no immune deposits. Serum QuantiFERON for tuberculosis was negative, and there were no radiological or biological findings suggestive of sarcoidosis. The patient was started on methylprednisolone, with normalization of SCr and CRP levels within 4 weeks. Interestingly, the patient eventually mounted a humoral response 8 weeks after vaccination.
Figure 1.
(a,b) On light microscopy, the renal parenchyma is infiltrated by chronic interstitial inflammatory cells and poorly formed granulomas (stars). Some of these granulomas surrounded small vessels, which rarely showed segmental fibrinoid necrosis (arrows). Glomeruli are normal. (a) Jones silver stain, original magnification ×20; (b) Masson trichrome stain, original magnification ×40.
The association of vasculitis with influenza and pertussis vaccines has already been described but without granulomatous pattern.3 Although causality between the renal lesions and the AstraZeneca vaccine cannot be definitively proven, the timing—and the absence of other causes—makes the link between the 2 plausible.4
References
- 1.Morlidge C., El-Kateb S., Jeevaratnam P., Thompson B. Relapse of minimal change disease following the AstraZeneca COVID-19 vaccine. Kidney Int. 2021;100:459. doi: 10.1016/j.kint.2021.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Masset C., Kervella D., Kandel-Aznar C. Relapse of IgG4-related nephritis following mRNA COVID-19 vaccine. Kidney Int. 2021;100:465–466. doi: 10.1016/j.kint.2021.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Patel C., Shah H.H. Vaccine-associated kidney diseases: a narrative review of the literature. Saudi J Kidney Dis Transpl. 2019;30:1002–1009. doi: 10.4103/1319-2442.270254. [DOI] [PubMed] [Google Scholar]
- 4.Shah S., Carter-Monroe N., Atta M.G. Granulomatous interstitial nephritis. Clin Kidney J. 2015;8:516–523. doi: 10.1093/ckj/sfv053. [DOI] [PMC free article] [PubMed] [Google Scholar]