Abstract
Introduction: Fiscal federalism and fiscal decentralization are distinct policy options in public services in general and healthcare in particular, with possibly opposed effects on equity, effectiveness, and efficiency. However, the pertinent discourse often reflects confusion between the concepts or conflation thereof.
Methods: This paper performs a narrative review of theoretical literature on decentralization. The study offers clear definitions of the concepts of fiscal federalism and fiscal decentralization and provides an overview of the potential implications of each policy for healthcare systems.
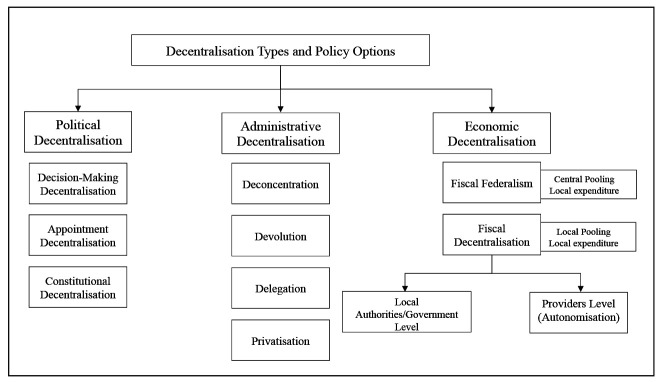
Results: The interpretation of the literature identified three different dimensions of decentralization: political, administrative, economic. Economic decentralization can be further implemented through two different policy options: fiscal federalism and fiscal decentralization. Fiscal federalism is the transfer of spending authority of a centrally pooled public health budget to local governments or authorities. Countries like the UK, Cuba, Denmark, and Brazil mostly rely on fiscal federalism mechanisms for healthcare financing. Fiscal decentralization consists of transferring both pooling and spending responsibilities from the central government to local authorities. Contrarily to fiscal federalism, the implementation of fiscal decentralization requires as a precondition the fragmentation of the national pool into many local pools. The restructuring of the pooling system may limit the cross-subsidization effect between high- and low-income groups and areas that a central pool guarantees; thus, severely affecting local equality and equity. With the limited availability of local public resources in poorer regions, the quality of services drops, increasing the disparity gap between areas. Evidence from Italy, Spain, China, and Ivory Coast -countries with a strong fiscal decentralization element in their healthcare services- suggests that fiscal decentralization has positive effects on the infant mortality rate. However, it decreases healthcare resources as well as access to services, fostering spatial inequities.
Conclusion: If public resources are and remain adequate, allocation follows equitable criteria, and local communities are involved in the decision-making debate, fiscal federalism -rather than fiscal decentralization- appear to be an adequate policy option to improve the healthcare services and population’s health nationwide and achieve health sector economic decentralization. HIPPOKRATIA 2020, 24(3): 107-113.
Keywords: Decentralization, economic decentralization, fiscal decentralization, fiscal federalism, health sector decentralization, spatial inequities
Introduction
It is widely agreed that decentralization as a policy option in public services in general and healthcare, in particular, means the transfer of political, administrative, and financial responsibilities from the national government to lower levels of authorities within a country1. The effects of decentralization policies have been widely discussed in the health policy arena2-6. The World Bank and the World Health Organization argue explicitly that among all types of decentralization, the transfer of financial responsibilities -henceforth called economic decentralization- boosts economic efficiency and accountability of the health sector. Economic decentralization is considered the most crucial element of decentralization1,7-9.
Economic decentralization has been implemented worldwide. However, it has meant different things in different countries. In Brazil10, Cuba11, Denmark12, and England13, the central government finances the healthcare system according to a certain resource allocation formula, whereas local bodies are responsible for setting their own healthcare spending priorities. By contrast, healthcare services in China14,15, Italy16,17, Nigeria18, and Spain19-21 are jointly financed by the central government and regional authorities. Similarly, in the Ivory Coast, the responsibility for raising taxes and financing healthcare and education services have been allocated to municipalities22.
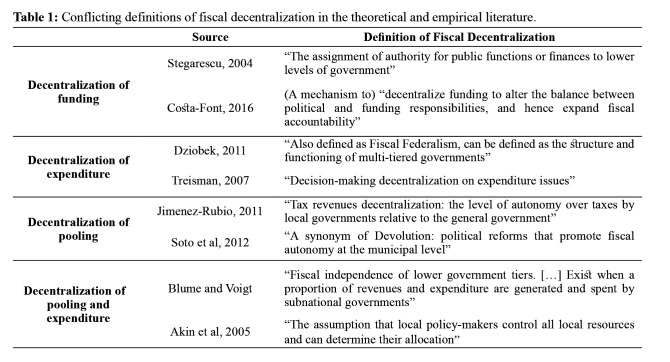
Interestingly, however, the literature dealing with economic decentralization reveals conflicting approaches on different policies and at any rate reflects disagreements as to the scope of the concept23-27. Indeed, there is no consensus regarding the pertinent financial responsibilities, i.e., pooling and spending7,9,23,26. Nor is there agreement on their implications8,24,25,28-30. For instance, some scholars claim that economic decentralization means giving local authorities more financial control over their services23,26. However, they do not clarify whether “financial control” means control over pooling, spending, or both7,9. Others perceive economic decentralization as local autonomy strictly concerning the spending of designated central government funds4,7,8. The inconsistencies are also semantic, with scholars using a single term with different meanings or different terms with the same meaning27,31.
Economic decentralization remains a vague and poorly understood concept that has affected the assessment of the impact of different economic decentralization policies on healthcare systems5,7,27,32. Most notably, the indicators used to assess these policies often fail to capture the scope of the control given to local bodies and might lead to biased conclusions27,29. Against this backdrop, the need for conceptual clarification is urgent.
Methods
This study conceptualizes the different types of health sector decentralization and provides an informed perspective on economic decentralization in healthcare. We perform a narrative review of major decentralization theories, following the methodological approach outlined by Greenhalgh et al33 and widely employed in the recent academic literature34,35. Narrative reviews are the most appropriate tools to understand, summarize, and provide an informed perspective on theoretical issues36. Using a narrative -rather than a systematic- approach to literature reviews does not compromise a study’s merits. In fact, systematic is not a synonym for high quality. It rather encloses a set of methodologies characterized by specific focus, thorough search, high rejection-to-inclusion ratio, and attention on technical rather than interpretive methods33. On the opposite, narrative reviews’ primary focus is to provide an informed perspective, insight, and interpretation on a specific topic to advance its theoretical understanding33,36. For this purpose, narrative reviews furnish arguments that are informed by evidence collected through a definite search strategy, although not necessarily systematic33,37.
Initial literature on decentralization theories was identified through a scoping search on PubMed and Web of Science. Search terms included: ((“administrative” AND OR “political” AND OR “Fiscal”) AND (“decentralisation” OR “decentralization”) AND (“theory” OR “theories”)).
Further material was identified through retrospective snowballing technique38. We have included any peer-reviewed article, book chapter, and conference proceeding in English discussing fundamental conceptual notions on political, administrative, and/or economic decentralization. We also selected literature published in any year. Empirical studies and systematic reviews were excluded from the analysis of decentralization theories; however, we scoured their reference lists to identify additional theoretical material that our search string may have failed to capture. We divided theoretical literature according to three different types of decentralization: political, administrative, and economic. The analysis was built using conceptual definitions and perspectives from theoretical literature applied to case-country examples drawn from the empirical studies we encountered.
Aspects of decentralization
As suggested above, economic decentralization, whatever it means, is not a standalone policy but an aspect of decentralization in general8. Thus, the first step in clarifying the concept of economic decentralization requires that we understand the other aspects of decentralization - political and administrative. The theoretical literature on decentralization has not further progressed over the last 20 years. However, it furnishes a starting point to analyze different aspects of decentralization. This will allow us to work out where economic decentralization fits within this wider policy complex.
Political decentralization concerns the transfer of political authority and planning responsibilities from the central government to local governments or authorities28. It involves three possibly inclusive options: decision-making decentralization confers formal decision-making responsibility regarding one or more policy issues on local governments/authorities32. Appointment decentralization involves giving local communities the power to elect their local representatives. Constitutional decentralization grants locally elected representatives and the central government joint veto and legislative powers on local and national policies28.
Political decentralization can be implemented through any of these options or any combination thereof. For example, in Spain, each autonomous community has a regional government with a locally elected parliament that holds local policy planning responsibilities20,21. At the national level, the Inter-Territorial Council of the Spanish National Health Service (CISNS) -a body formed by all autonomous communities’ health ministries- holds legislative and veto powers pertaining to national health policies, such as pharmaceutical legislation19. This example reflects a combination of all political decentralization options.
Administrative decentralization differs from political decentralization in that it focuses not on policy but management39,40. It is the transfer of specific administrative and managerial responsibilities from the central government to local bodies39.
Rondinelli identifies four administrative decentralization options: devolution, deconcentration, delegation, and privatization. Devolution is a combination of political and administrative decentralization. Here, central governmental bodies transfer administrative and policy powers to local authorities (e.g., municipalities)39. European Nordic countries (Norway - until 2002, Sweden, and Finland), where municipalities provide and administer primary care, rehabilitative and preventative services, are examples of devolution in healthcare8,12,41,42. A similar structure also exists in Cuba, where municipal assemblies manage health supplies and the training of local physicians11,43.
Deconcentration involves the transfer of some managerial aspects to local departments within the government8,39. An example is the shift of responsibilities for commissioning local hospital activities, community services, secondary care, and mental health services from the English Department of Health to Clinical Commissioning Groups (CCGs), the latter being National Health Service’s (NHS) bodies subject to NHS England and the Secretary of Health13. The 2002 reconcentration reform of Norway is another example of deconcentration in healthcare12. In the attempt to recentralize functions from the overburdened local management system, the reform reassigned administrative control over hospitals from counties to five independent regional bodies (Regional Health Authorities)12,42,44. A shift from devolution to deconcentration42.
Delegation refers to central government outsourcing of partial managerial responsibilities to actors operating outside the government structure39. As a case of delegation in healthcare, UK’s Private Finance Initiatives (PFIs) legitimize private firms to design, build, and operate hospital facilities. The responsibility to pay the total cost of the project, however, remains to the government13,45.
Privatization (in the context of administrative decentralization) means the full transfer of government assets to for-profit or not-for-profit organisations39. Note that, with the possible exception of devolution, the implementation of administrative decentralization is strongly associated with privatization of the public service or it embracing a business-like culture32.
Economic decentralization incorporates two distinct policy options: fiscal federalism, i.e., the decentralization of the authority of spending46, and fiscal decentralization, i.e., the decentralization of both the responsibility for pooling as well as the authority of spending47 (Figure 1).
Figure 1. Aspects of decentralization and policy options; based on Treisman28, Rondinelli et al.39, Oates48, and Weingast et al47.
Fiscal federalism
Fiscal federalism is the transfer of spending authority of a centrally pooled public health budget to local governments or authorities. Under fiscal federalism, the national government first raises healthcare financing resources centrally through some form of taxation and distributes them to local levels using allocation formulas. Following that, the local level decides how to spend the received budget46,48.
According to Oates48, fiscal federalism’s social role is to diversify public services in accord with local preferences, thereby maximizing local, and thus also general, social welfare. Fiscal federalism is also supposed to help the central government control national expenditure, thereby promoting technical efficiency (the production of the maximum output from the minimum level of input) and allocative efficiency (a state in which the production of goods and services represent individual needs and demands)46,49. All this is achieved through a rational division of labor among entities that are increasingly informed about the people’s needs, the local community being at the top of the chain.
Fiscal federalism in healthcare systems: policy implications
Fiscal federalism can indeed serve as a flexible path towards economic decentralization. Nevertheless, its actual implications for the country’s healthcare system depend on the political and socioeconomic context.
One area of concern is the issue of cross-regional heterogeneity. Healthcare needs are heterogeneous by definition, as a huge number of factors determines them50. Community needs in historically more impoverished areas may be more demanding than those in more developed regions, requiring further governmental support9,48,50. Fiscal federalism implemented while neglecting these differences poses the risk of weakening healthcare services in deprived areas. Typically, there are two options for addressing cross-regional heterogeneity under fiscal federalism. One option is to provide a comprehensive package of essential services nationwide, as suggested by Oates46. The other option is to allocate resources using an equitable formula, thereby adequately responding to local demands and avoiding preventable health inequalities9,10. The UK’s York Model and the Swedish Stockholm Model are typical examples of such formulas51,52.
Another area of concern is related to the national government’s ability under fiscal federalism to plan and regulate the amount of healthcare resources to be spent by each local authority. For instance, in Cuba, the government reallocated resources over the last two decades from health managers to local policlinics aiming to reduce administrative waste in favor of improving access to care for local communities11,43. By contrast, there is always the risk that in an austere economic environment, fiscal federalism can lead preferably to significant cuts at the local level in order to contain public expenditure7,46,53.
Finally, there is the issue of community participation. Fiscal federalism is presented as a mechanism of high local responsiveness through which local communities can directly participate in setting up local spending priorities46. Between 1996 and 2001, Kerala democratically elected councils at the district, block, village, municipal, and urban levels. These bodies could determine the allocation of funding according to their local population’s health and healthcare priorities: an example of effective public involvement under fiscal federalism54. Note, then, that active community participation requires a special political structure and culture, which may not always exist48,55. The UK’s Manchester Devolution Deal, under which Localities and Enterprises Partnerships (LEPs) were made responsible for the region’s share of the healthcare budget, manifests the opposite effect. Here, the attempt to promote community participation under fiscal federalism seems to have transformed into a technocratic process carried out by LEPs away from the public eye and excluding local residents56.
Fiscal decentralization
Fiscal decentralization is a more rigid path towards economic decentralization. Here, the responsibilities of pooling and the authority of spending are shifted from the national to local levels. Thus, the pooling responsibility can be shifted to local governments or authorities, for example, through the introduction of earmarked local taxation47,57. Financial responsibilities for pooling and spending equally can be transferred at the provider’s level, giving public hospitals financial autonomy to generate and reinvest their surpluses, for example, by increasing user fees or by accepting private patients. The latter, a process referred to as autonomization, has become common in NHS England, where hospitals can apply for foundation trust status, which transforms them into financially independent public corporations13,58. Similarly, Norwegian hospitals and regional health authorities have been reorganized as health enterprises following the 2002 reconcentration reform12,42.
It is noteworthy that fiscal decentralization typically requires prior implementation of some forms of political and administrative decentralization, for example, appointment or constitutional decentralization and devolution or delegation (in the case of autonomization).
The literature reveals multiple and conflicting definitions of fiscal decentralization (Table 1). This confusion is the source of the conceptual disagreements on economic decentralization highlighted in the current review’s introduction.
Table 1. Conflicting definitions of fiscal decentralization in the theoretical and empirical literature.
Fiscal decentralization theorists criticized fiscal federalism for the lack of competition and market participation and proposed fiscal decentralization as a tool to challenge the monopolistic power of national governments in pooling resources and determining regional shares47,57. Fiscal decentralization develops in the assumption that local services are provided more efficiently if both responsibility of pooling and authority of spending are localized; that is if local authorities are financially free of any central regulatory restrictions47,59. Such providers can compete against each other in an open market environment, both in terms of taxes/private contributions (fiscal package) and the quantity and quality of the services provided within this “package”60.-62
Fiscal decentralization in healthcare systems: policy implications
Efficiency-focused, policymakers often fail to acknowledge the impact fiscal decentralization can have on cross-regional healthcare inequities. Fiscal decentralization assists in reorganizing the pooling system from central to local, as a necessary step in making local bodies accountable for their financial choices and incentivizing them to take efficiency-maximizing decisions47,57,59. Such restructuring of the pooling system severely affects local equity and equality. To be more illustrative, a central financing pool guarantees under certain conditions high cross-subsidization between high- and low-risk individuals and thus functions as an equalization tool; the shifting to local, fragmented pools limits this redistributive effect63. This characteristic, being intrinsic, renders fiscal decentralization a regressive financing policy option in essence.
The change of pooling structure may further widen the socioeconomic and health inequities gap between richer and poorer areas. More prosperous areas have a large tax base capable of generating high revenues for the healthcare system. Conversely, areas with a high poverty rate must rely on a relatively narrow tax base with lower financial returns60. Fiscal decentralization theorists acknowledge this gap. However, they insist that it incentivizes deprived areas to imitate the fiscal behavior and policy choices of their wealthier counterparts57. International bodies, notably the World Bank and the World Health Organization, comment that securing a minimum standard level of care nationwide can further aid in reducing inequities under fiscal decentralization1. Implementing fiscal decentralization, the government in Italy, for example, allocates funds for the provision of some essential public healthcare activities, while regional authorities finance and run the rest16,64. However, this approach addresses regional inequities only partly since regions continue to depend on their local pools largely.
Notwithstanding the support of national financial contributions, qualitative studies from China suggest that fiscal decentralization has led to the collapse of village health stations and worsening local healthcare provision in the country’s most deprived areas14,65. Similarly, evidence from Ivory Coast indicates that municipal revenues available for public services are higher in urban than rural areas. Thus, urban local governments are more likely to increase access to public healthcare services than their poorer counterparts22.
Econometric literature highlights the positive correlation between fiscal decentralization and reduction of infant mortality rates16,20,21. However, the extent to which health outcomes improve is dependent on the level of regional wealth, with more prosperous areas faring better than their poorer counterparts21,25,44.
The second area of concern is the variation in the quantity and quality of services across areas. Without equitable distribution of centrally-pooled resources, wealthier areas are free to manage their surpluses, if any, ad libitum, while deprived regions suffer from limited resources and are therefore forced to find alternative ways to meet the needs57. One example is introducing cost-containing measures such as patients’ cost-sharing (increasing local taxes and/or co-payments) and capping services. Such actions expose vulnerable local communities to the risk of catastrophic health expenditure. In Italy, evidence suggests that the initial implementation of fiscal decentralization has led to increased healthcare deficits, particularly in deprived regions16,17. In response, regional authorities were effectively forced by the central government to introduce reductions in health services and cost-sharing measures16,64. This measure has been interpreted as a move towards recentralization. However, it has proved to be a top-down stewardship approach to improve budgetary performance without dismantling the fiscal decentralization process64.
Although impoverished regions are typically more exposed, wealthy regions are not immune under fiscal decentralization to impact austere macro-economic conditions either. Catalonia, one of the wealthiest regions in Spain, provides an example. During the economic recession of 2010, central public revenues declined. The government responded by introducing nationwide austerity measures. As Catalonia could not equate its pre-crisis levels of local healthcare revenues, it embarked on a series of severe regional healthcare cutbacks -including cuts in hospital beds, staff, salaries, and emergency care- in addition to the national ones19,66.
The final area of concern under fiscal decentralization is the issue of cross-regional patients’ mobility. In a fiscally decentralized healthcare system, patients are free to choose where to be treated according to the best fiscal package provided60. According to fiscal decentralization theorists, patients’ mobility stimulates competition over the quality of care among localities and providers. In reality, however, patients from low- and middle-income regions typically seek services in wealthier areas where quality and care availability is higher. This forces the deprived regions to cut quantity and quality of care further60,67. In Italy, hosting regions are reimbursed from patients’ home regions for the services provided, diverting funds destined to local healthcare services and creating increasingly perpetual regional inequities67.
Conclusion
Decentralization is not a set of clear-cut steps but a continuum of policies ranging from flexible (e.g., decision-making decentralization, deconcentration, fiscal federalism) to rigid (e.g., constitutional decentralization, delegation, fiscal decentralization), which, in different contexts and combinations, entail different outcomes.
Under fiscal federalism, the pooling of healthcare resources occurs at the central level. Funds are then distributed to localities responsible for setting up their healthcare spending priorities based on the allocated budget. Central governments can control their public healthcare expenditure and address regional heterogeneity by providing equitably tailored budgets. Local communities may be involved in setting local spending priorities according to their preferences and consumption patterns. Fiscal federalism is not a magic bullet, however. Its efficacy is subject to the available resources, the way they are allocated, and the decision-making mechanisms at local levels. Steadily reducing the budget, failing to take into account pre-existing regional differences, and disregarding communities’ participation are factors that may hinder fiscal federalism’s efficacy.
By contrast, fiscal decentralization consists of transferring the responsibility for pooling and spending resources from the central to local levels to give localities more financial independence from the central government. Increased autonomy comes at a price, though: creating local pools reduces the cross-subsidization effect and financial risks protection that a national pool guarantees, rendering fiscal decentralization a regressive choice. This not only exacerbates cross-regional inequities but can also be a gateway to rigid healthcare policies: with limited availability of public resources, quality of services drops, encouraging patients in more impoverished regions to seek care elsewhere.
Moreover, in the context of neoliberal austerity, the choice between fiscal federalism and fiscal decentralization is meaningless, as both options lead to regressive outcomes, notably the commercialization and privatization of the healthcare system16,19. Wittingly or not, then, conceptual vagueness and ambiguity might conceal and thereby serve such intentions. Conversely, if public resources are and remain adequate, allocation follows equitable criteria, and local communities are involved in the decision-making debate, fiscal federalism can, indeed, improve healthcare services and population’s health nationwide.
Decentralization policies are deemed to have been developed to favor dialogue between government and communities. Their implementation ought to reflect this principle.
Conflict of interest
Listed authors declare that they have no affiliations with or involvement in any organization or entity with any financial interest (such as honoraria; educational grants; participation in speakers’ bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements), or non-financial interest (such as personal or professional relationships, affiliations, knowledge or beliefs) in the subject matter or materials discussed in this manuscript.
Acknowledgement
The authors wish to acknowledge the invaluable help of Dr. Jonathan Filippon in reviewing and editing a previous draft of this manuscript.
References
- 1.World Bank. Decentralization. 2013. Available at: http://www.worldbank.org/en/topic/communitydrivendevelopment/brief/Decentralization. date accessed: 26/04/2020.
- 2.Channa A, Faguet JP. Decentralization of Health and Education in Developing Countries: A Quality-Adjusted Review of the Empirical Literature. World Bank Res Obs. 2016;31:199–241. [Google Scholar]
- 3.Dwicaksono A, Fox AM. Does Decentralization Improve Health System Performance and Outcomes in Low- and Middle-Income Countries? A Systematic Review of Evidence From Quantitative Studies. Milbank Q. 2018;96:323–368. doi: 10.1111/1468-0009.12327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sumah AM, Baatiema L, Abimbola S. The impacts of decentralisation on health-related equity: A systematic review of the evidence. Health Policy. 2016;120:1183–1192. doi: 10.1016/j.healthpol.2016.09.003. [DOI] [PubMed] [Google Scholar]
- 5.Cobos Muñoz D, Merino Amador P, Monzon Llamas L, Martinez Hernandez D, Santos Sancho JM. Decentralization of health systems in low and middle income countries: a systematic review. Int J Public Health. 2017;62:219–229. doi: 10.1007/s00038-016-0872-2. [DOI] [PubMed] [Google Scholar]
- 6.Abimbola S, Baatiema L, Bigdeli M. The impacts of decentralization on health system equity, efficiency and resilience: a realist synthesis of the evidence. Health Policy Plan. 2019;34:605–617. doi: 10.1093/heapol/czz055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Robalino DA, Picazo OF, Voetberg A. Does Fiscal Decentralization Improve Health Outcomes? Evidence from a Cross-Country Analysis. Policy Research Working Papers. The World Bank Group. 2001. Available at: https://elibrary.worldbank.org/doi/abs/10.1596/1813-9450-2565. date accessed: 26/04/2020.
- 8.Costa-Font J, Greer SL. Federalism and Decentralization in European Health and Social Care. Palgrave Macmillan UK. 2016:13–39. [Google Scholar]
- 9.Prud’homme R. The Dangers of Decentralization. World Bank Res Obs. 1995;10:201–220. [Google Scholar]
- 10.Mendes Á, Leite MG, Carnut L. A methodology for apportioning federal SUS resources: the health needs index. Rev Saúde Pública. 2020;54:77. doi: 10.11606/s1518-8787.2020054001661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.PAHO El sistema de salud en Cuba: avances y desafíos. Available at: https://iris.paho.org/handle/10665.2/34931. 2018. date accessed: 26/04/2020.
- 12.Saltman RB. Decentralization, re-centralization and future European health policy. Eur J Public Health. 2008;18:104–106. doi: 10.1093/eurpub/ckn013. [DOI] [PubMed] [Google Scholar]
- 13.Boyle S. United Kingdom (England): Health System Review. Health Systems in Transition. 2011; 13: 1-486. Available at: https://www.euro.who.int/__data/assets/pdf_file/0004/135148/e94836.pdf. date accessed: 26/04/2020. [PubMed]
- 14.Jin Y, Sun R. Does fiscal decentralization improve healthcare outcomes? Empirical evidence from China. Public Finance Manag. 2011;11:234–261. [Google Scholar]
- 15.Uchimura H, Jütting JP. Fiscal Decentralization, Chinese Style: Good for Health Outcomes? World Dev. 2009;37:1926–1934. [Google Scholar]
- 16.Cavalieri M, Ferrante L. Does fiscal decentralization improve health outcomes? Evidence from infant mortality in Italy. Soc Sci Med. 2016;164:74–88. doi: 10.1016/j.socscimed.2016.07.017. [DOI] [PubMed] [Google Scholar]
- 17.Di Novi C, Piacenza M, Robone S, Turati G. Does fiscal decentralization affect regional disparities in health? Quasi-experimental evidence from Italy. Reg Sci Urban Econ. 2019;78:103465. [Google Scholar]
- 18.Akpan EO. Fiscal Decentralization and Social Outcomes in Nigeria. Eur J Bus Manag. 2011;3:167–183. [Google Scholar]
- 19.Gené-Badia J, Gallo P, Hernández-Quevedo C, García-Armesto S. Spanish health care cuts: penny wise and pound foolish? Health Policy. 2012;106:23–28. doi: 10.1016/j.healthpol.2012.02.001. [DOI] [PubMed] [Google Scholar]
- 20.Jiménez-Rubio D, García-Gómez P. Decentralization of health care systems and health outcomes: Evidence from a natural experiment. Soc Sci Med. 2017;188:69–81. doi: 10.1016/j.socscimed.2017.06.041. [DOI] [PubMed] [Google Scholar]
- 21.Montero-Granados R, de Dios Jiménez J, Martín J. Decentralisation and convergence in health among the provinces of Spain (1980–2001) Soc Sci Med. 2007;64:1253–1264. doi: 10.1016/j.socscimed.2006.10.016. [DOI] [PubMed] [Google Scholar]
- 22.Sanogo T. Does fiscal decentralization enhance citizens’ access to public services and reduce poverty? Evidence from Côte d’Ivoire municipalities in a conflict setting. World Dev. 2019;113:204–221. [Google Scholar]
- 23.Stegarescu D. The effects of economic and political integration on fiscal decentralization: evidence from OECD countries. Can J Econ. 2004;42:694–718. [Google Scholar]
- 24.Dziobek C, Mangas CAG, Kufa P. Measuring Fiscal Decentralization-Exploring the IMF’s Databases. IMF Work Pap. 2011. Available at: https://www.imf.org/external/pubs/ft/wp/2011/wp11126.pdf. date accessed: 26/04/2020.
- 25.Soto VE, Farfan MI, Lorant V. Fiscal decentralisation and infant mortality rate: The Colombian case. Soc Sci Med. 2012;74:1426–1434. doi: 10.1016/j.socscimed.2011.12.051. [DOI] [PubMed] [Google Scholar]
- 26.Voigt S, Blume L. The economic effects of federalism and decentralization—a cross-country assessment. Public Choice. 2012;151:229–254. [Google Scholar]
- 27.Samadi AH, Keshtkaran A, Kavosi Z, Vahedi S. The Effect of Fiscal Decentralization on Under-five Mortality in Iran: A Panel Data Analysis. Int J Health Policy Manag. 2013;1:301–306. doi: 10.15171/ijhpm.2013.60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Treisman D. Cambridge University Press. 2007. The architecture of government: Rethinking political decentralization; pp. 21–52. [Google Scholar]
- 29.Jimenez-Rubio D. The impact of fiscal decentralization on infant mortality rates: evidence from OECD countries. Soc Sci Med. 2011;73:1401–1407. doi: 10.1016/j.socscimed.2011.07.029. [DOI] [PubMed] [Google Scholar]
- 30.Akin J, Hutchinson P, Strumpf K. Decentralisation and government provision of public goods: The public health sector in Uganda. J Dev Stud. 2005;41:1417–1443. [Google Scholar]
- 31.Fritscher AM, Zamora CR. An Evaluation of the 1997 Expenditure Decentralization Reform in Mexico. Public Finance Rev. 2016;44:563–588. [Google Scholar]
- 32.Ashton T, Tenbensel T, Cumming J, Barnett P. Decentralizing resource allocation: early experiences with district health boards in New Zealand. J Health Serv Res Policy. 2008;13:109–115. doi: 10.1258/jhsrp.2008.007133. [DOI] [PubMed] [Google Scholar]
- 33.Greenhalgh T, Thorne S, Malterud K. Time to challenge the spurious hierarchy of systematic over narrative reviews? Eur J Clin Invest. 2018;48:e12931. doi: 10.1111/eci.12931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lal A, Erondu NA, Heymann DL, Gitahi G, Yates R. Fragmented health systems in COVID-19: rectifying the misalignment between global health security and universal health coverage. Lancet. 2021;397:61–67. doi: 10.1016/S0140-6736(20)32228-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Faggion CMJ, Bakas NP, Wasiak J. A survey of prevalence of narrative and systematic reviews in five major medical journals. BMC Med Res Methodol. 2017;17:176. doi: 10.1186/s12874-017-0453-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Nevo I, Slonim-Nevo V. The Myth of Evidence-Based Practice: Towards Evidence-Informed Practice. Br J Soc Work. 2011;41:1176–1197. [Google Scholar]
- 37.Dixon-Woods M, Cavers D, Agarwal S, Annandale E, Arthur A, Harvey J, et al. Conducting a critical interpretive synthesis of the literature on access to healthcare by vulnerable groups. BMC Med Res Methodol. 2006;6:35. doi: 10.1186/1471-2288-6-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Sayers A. Tips and tricks in performing a systematic review. Br J Gen Pract. 2007;57:425. [PMC free article] [PubMed] [Google Scholar]
- 39.Rondinelli DA, Nellis J, Cheeba GS. Decentralization in Developing Countries: A Review of Recent Experience. World Bank Staff Work Papers. 1984. Available at: http://documents1.worldbank.org/curated/en/868391468740679709/pdf/multi0page.pdf. date accessed: 26/04/2020.
- 40.Mills A, Vaughan JP, Smith DL, Tabibzadeh I. World Health Organization. Health system decentralization: concepts, issues and country experience. Available at: https://apps.who.int/iris/handle/10665/39053. 1990. date accessed: 26/04/2020.
- 41.Saltman RB, Bankauskaite V, Vrangbaek K. Open University Press - McGraw-Hill Education, London, UK. 2007. Decentralization in health care: strategies and outcomes. 1st Edition; pp. 22–39. [Google Scholar]
- 42.Magnussen J, Hagen TP, Kaarboe OM. Centralized or decentralized? A case study of Norwegian hospital reform. Soc Sci Med. 2007;64:2129–2137. doi: 10.1016/j.socscimed.2007.02.018. [DOI] [PubMed] [Google Scholar]
- 43.Spiegel JM, Yassi A. Lessons from the margins of globalization: appreciating the Cuban health paradox. J Public Health Policy. 2004;25:85–110. doi: 10.1057/palgrave.jphp.3190007. [DOI] [PubMed] [Google Scholar]
- 44.Arends H. More with Less? Fiscal Decentralisation, Public Health Spending and Health Sector Performance. Swiss Polit Sci Rev. 2017;23:144–174. [Google Scholar]
- 45.Hellowell M, Pollock AM. The private financing of NHS hospitals: politics, policy and practice. Econ Aff. 2009;29:13–19. [Google Scholar]
- 46.Oates WE. An essay on fiscal federalism. J Econ Lit. 1999;37:1120–1149. [Google Scholar]
- 47.Weingast BR. Second Generation Fiscal Federalism: Implications for Decentralized Democratic Governance and Economic Development. Available at: https://web.stanford.edu/~jrodden/weingast.pdf. 2007. date accessed: 26/04/2020.
- 48.Oates WE. Lexington Books, Lexington, Massachussetts. 1977. The Political Economy of Fiscal Federalism; pp. 5–18. [Google Scholar]
- 49.Musgrave RA. Neb J Econ Bus. 1971. Economics of Fiscal Federalism; pp. 3–13. [Google Scholar]
- 50.Evans RG. Health for all or Wealth for Some? Conflicting Goals in Health Reform. Centre for Health Services and Policy Research. 1998;98:12d. [Google Scholar]
- 51.Diderichsen F, Varde E, Whitehead M. Resource allocation to health authorities: the quest for an equitable formula in Britain and Sweden. BMJ. 1997;315:875–878. doi: 10.1136/bmj.315.7112.875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Smith PC. Resource allocation and purchasing in the health sector: the English experience. Bull World Health Organ. 2008;86:884–888. doi: 10.2471/BLT.07.049528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Maarse H. The Privatization of Health Care in Europe: An Eight-Country Analysis. J Health Polit Policy Law. 2006;31:981–1014. doi: 10.1215/03616878-2006-014. [DOI] [PubMed] [Google Scholar]
- 54.Elamon J, Franke RW, Ekbal B. Decentralization of Health Services: The Kerala People’s Campaign. Int J Health Serv. 2004;34:681–708. doi: 10.2190/4L9M-8K7N-G6AC-WEHN. [DOI] [PubMed] [Google Scholar]
- 55.Smith BC. Allen & Unwin, London. 1985. Decentralization: The Territorial Dimension of the State. 1st Edition. G; pp. 100–121. [Google Scholar]
- 56.Wall R, Vilela NB. Deal or no deal: English Devolution, a top-down approach. Lex Localis - J Local Self-Gov. 2016;14:655–670. [Google Scholar]
- 57.Ferejohn JA, Weingast BR. Hoover Press, Stanford, CA. 1997. The New Federalism: Can the States Be Trusted? ; pp. 10–25. [Google Scholar]
- 58.Harding A, Preker AS. Understanding Organizational Reforms: The Corporatization of Public Hospitals. 2000. Available at: https://www.who.int/management/facility/hospital/Corporatization.pdf. date accessed: 26/04/2020.
- 59.Martinez-Vazquez J, McNab RM. Fiscal Decentralization and Economic Growth. World Dev. 2003;31:1597–1616. [Google Scholar]
- 60.Tiebout CM. A Pure Theory of Local Expenditures. J Polit Econ. 1956;64:416–424. [Google Scholar]
- 61.Bossert TJ, Larrañaga O, Giedion U, Arbelaez JJ, Bowser DM. Decentralization and equity of resource allocation: evidence from Colombia and Chile. Bull World Health Organ. 2003;81:95–100. [PMC free article] [PubMed] [Google Scholar]
- 62.Brennan G, Buchanan JM. Cambridge University Press, Cambridge, UK. 1980. The Power to Tax: Analytic Foundations of Fiscal Constitution; pp. 197–215. [Google Scholar]
- 63.World Health Organization. The world health report 2000 - Health systems: improving performance. 2000. Available at: https://www.who.int/whr/2000/en/ date accessed: 26/04/2020.
- 64.Mauro M, Maresso A, Guglielmo A. Health decentralization at a dead-end: towards new recovery plans for Italian hospitals. Health Policy. 2017;121:582–587. doi: 10.1016/j.healthpol.2017.04.003. [DOI] [PubMed] [Google Scholar]
- 65.Gu X-Y, Tang S-L, Cao S-H. The financing and organization of health services in poor rural China: A case study in Donglan County. Int J Health Plann Manage. 1995;10:265–282. doi: 10.1002/hpm.4740100404. [DOI] [PubMed] [Google Scholar]
- 66.Costa-Font J, Gil J. Exploring the pathways of inequality in health, health care access and financing in decentralized Spain. J Eur Soc Policy. 2009;19:446–458. [Google Scholar]
- 67.Balia S, Brau R, Marrocu E. Interregional patient mobility in a decentralized healthcare system. Reg Stud. 2018;52:388–402. [Google Scholar]