Abstract
Objective:
Some eating behaviors are associated with negative nutrition-related outcomes in adults, but research is lacking in adolescent samples. The current study examined whether dietary restraint moderates the relationship between disinhibition and weight outcomes and overall diet quality in a community sample of 16-year old adolescents.
Methods:
Participants were recruited from a longitudinal study examining self-regulation and cardiometabolic risk. Data for this cross-sectional study were collected from questionnaires and laboratory visits when participants were approximately 16 years old (n=178). Disinhibition and restraint were assessed using two subscales of the Three-Factor Eating Questionnaire. Diet quality was determined using Healthy Eating Index-2010 (HEI-2010) scores that were calculated using dietary data from 24-hour dietary recalls. Two separate hierarchical linear regression analyses tested whether restraint moderated the associations of disinhibition with BMI-for-age percentile and HEI-2010 scores.
Results:
After adjusting for covariates, restraint moderated the association between disinhibition and HEI-2010 scores (β=−.21, p=.03). There was a main effect for disinhibition on BMI-for-age percentiles (β=.58, p=.02), but this relationship was not moderated by the level of restraint.
Conclusions:
The relationship between disinhibition and overall diet quality differed among adolescents according to level of dietary restraint. Although disinhibition independently predicted weight status, the level of restraint had no influence on this association. Future studies should examine restraint in relation to energy intake and weight concerns to better understand how it influences weight and dietary outcomes in this population.
Keywords: adolescent, diet quality, healthy eating index, obesity, disinhibition, restraint
1. Introduction
Adolescence is recognized as a critical time point for establishing lifelong health behaviors (1–3). The prevalence of obesity rises throughout adolescence and evidence suggests that individuals who are overweight during this period are at increased risk for tracking excessive adiposity into adulthood (4,5). Furthermore, many adolescents consume poor diets, failing to meet the minimum recommendations for fruits, vegetables, whole grains, and dairy products while exceeding the maximum recommended intakes of saturated fat and added sugars (6–8). Healthy eating is one of the key factors that influence long-term obesity and other chronic disease risks, therefore a better understanding of the behaviors that influence dietary intake during adolescence is warranted (9).
Healthy weight maintenance depends on balancing energy intake with energy expenditure over time (10,11). Although basic energy balance is regulated through homeostatic signals to sustain life, humans also experience hedonic drivers of food intake, which influence the desire to obtain pleasure through eating (10). The current food environment in Western countries tends to promote hedonic aspects of eating via disproportionate access to palatable and energy-dense foods that have been linked to poor dietary outcomes and increased obesity risks (12–14). However, some individuals are able to maintain a healthy weight while others become overweight or obese (15,16).
Eating behaviors, including disinhibition and dietary restraint, appear to influence the variability of weight and diet-related outcomes among individuals (17–19). While disinhibition refers to one’s tendency to overeat palatable foods, or to eat in excess as a response to emotional or stressful situations (18,20), dietary restraint is most often defined as one’s conscious control or restriction of food intake, generally for the purpose of reducing or maintaining weight (21–23). The extant literature investigating the links between disinhibition, restraint and weight outcomes focuses largely on adults and/or clinical populations enrolled in obesity treatment programs (21,22). In these studies, a greater level of disinhibition is associated with a higher Body Mass Index (BMI) (19,20,24). The associations between restraint and weight outcomes (e.g. BMI) are less clear, and seemingly dependent on weight status and dieting history (24–26). Restraint has been shown, in some studies, to have a positive association with weight and BMI, but this association is not necessarily causal and might be due to the tendency of some overweight individuals to attempt to control weight (25,27). Further, evidence suggests that it is the interaction between these eating behaviors that predicts weight, and that dietary restraint might act to moderate the positive association between disinhibition and BMI (19,24,28,29). For example, cross-sectional studies have shown that high levels of restraint reduce the effects of disinhibition on weight, such that individuals with high disinhibition and high restraint weighed less than individuals with high disinhibition and low restraint (28,29).
In terms of the influence of disinhibited or restrained eating on individuals’ diet-related outcomes, research is scarce and the few existing studies focus on selected nutrients or food groups rather than general dietary pattern (25,30,31). For instance, a high level of disinhibition has been associated with a greater intake of saturated fat, high-sugar and high-salt foods, sugar-sweetened beverages and unhealthy snacks (30,32). In contrast, higher dietary restraint has been correlated with lower intakes of total energy and dietary fat and a greater consumption of healthy foods, such as fruit and vegetables (30,33). Understanding how eating behaviors interact to influence overall diet quality rather than the consumption of individual nutrients or food groups is essential because improved overall diet quality plays a key role in the prevention of chronic disease (34).
Despite the well-recognized role of healthy eating early in life on long-term health outcomes, the research assessing diet and weight-related outcomes among adolescents is limited and has primarily focused on the influence of unhealthy weight-control practices, while largely neglecting the potential conjoint effects of disinhibition and dietary restraint on these important outcomes in non-clinical populations (35,36). Thus, the purpose of this study was to explore the associations between disinhibition and restraint in relation to BMI-for-age percentile and overall diet quality in a community sample of adolescents. Based on the existing literature largely limited to adults, we expected that: 1) disinhibition will independently predict BMI-for-age percentile and overall diet quality, 2) restraint will independently predict overall diet-quality, and 3) restraint will moderate the association between disinhibition and BMI-for-age percentile and overall diet quality in our sample of adolescents.
2. Materials and Methods
2.1. Participants and Procedures
Cross-sectional data for the current study were collected from participants of the RIGHT Track Study, a longitudinal study assessing self-regulation and cardiometabolic risk. A complete description of the recruitment, screening procedures and participant characteristics is presented elsewhere (Wideman et al., 2016). Briefly, participants were recruited at age 2 through child daycare centers, the local Woman, Infant and Children (WIC) program, and the county health department in Greensboro, NC between 1994–1996. Participants in the original sample (n=293) were representative of the surrounding community in terms of race and socioeconomic status (Wideman et al., 2016). Socioeconomic status (SES) was determined using the Hollingshead Index which measures social status of a child or adolescent based on the marital status, employment status, educational attainment, and occupational prestige of the parent (37). Data for the current cross-sectional study were collected beginning in spring 2014 when participants were approximately 16 years old. Participants reported on health behaviors using online questionnaires. Other health data, including anthropometric measurements, were collected in the lab by trained research assistants. Written consent from the adolescent and an accompanying parent were obtained prior to any data collection. Study procedures were reviewed and approved by the Institutional Review Board at the University of North Carolina Greensboro.
2.2. Study Measures and Variables
2.2.1. Eating Behaviors
Participants reported on their current eating behaviors using the Three-Factor Eating Questionnaire (TFEQ) (38), assessing disinhibition and cognitive restraint of eating. The disinhibition subscale of the TFEQ consists of 16-items which measure the individuals’ tendency to overeat in response to external stimuli, such as high levels of emotion or presence of palatable foods (e.g. “Sometimes when I start eating, I just can’t seem to stop”) (20,38). The restraint subscale of the TFEQ consists of 21 items that are associated with the intent to control food intake for weight management (e. g., “I deliberately take small helpings as a means of controlling my weight”) (38). Responses were dichotomized and coded 0 or 1, with the exception of a single item from the restraint subscale (e.g. “On a scale of 0 to 5, where 0 means no restraint in eating and 5 means total restraint, which number would you give yourself”) which was not collected in the original longitudinal study. Total scores for each subscale were calculated by summing respective responses, with higher scores indicating a greater level of the specific type of eating behavior. Crohnbach’s alpha scores for the subscales of disinhibition and restraint were 0.77 and 0.81 respectively. A total of 178 participants provided complete data from the TEFQ at the 16-year visit.
2.2.2. Diet Quality
Participants were asked to complete three 24-hour dietary recalls (2 weekdays and 1 weekend day) immediately following their lab visit. Detailed procedures related to the dietary recalls in the RIGHT Track study can be found elsewhere (Wideman et al., 2016). The 24-hour dietary recalls were collected by the Nutrition Obesity Research center (NORC) at the University of North Carolina Chapel Hill and analyzed using the Nutrition Data System for Research (NDSR) software. Dietary data from the available dietary recalls were averaged and the overall diet quality for each participant was determined using the Healthy Eating Index 2010 (HEI-2010) scoring system that was based on the official Dietary Guidelines for Americans that were current at the time of the study (39,40). From the reported intakes, 12 dietary component sub-scores were calculated and added together to create an overall diet quality score ranging from 0–100, with greater values indicating better adherence to the federal dietary guidelines (39,40). The total scores were then averaged to determine the overall diet quality score. Since the recommendations for food group amounts vary according to the individual’s dietary energy intake, HEI-2010 scores are calculated based on intake of each component per 1,000 kcal. The detailed procedures for calculating overall HEI-2010 scores are reported elsewhere (39). In the current study, 148 participants provided dietary recalls at age 16: 137 completed 3 recalls, 6 completed 2 recalls and 5 participants completed 1 recall. There were no significant differences in the HEI score between the participants who completed 3 versus 2 versus 1 dietary recall; thus, data from all participants who provided 1–3 dietary recalls were included in the final analyses.
2.2.3. Body Mass Index (BMI)
Participants’ height and weight were measured using standard procedures by trained research assistants and used to calculate BMI (BMI= kg/m2) (41). Height was measured using a stadiometer (SECA, Chino CA) to the nearest 0.1 cm. Weight was measured using a medical scale to the nearest 0.1 kg (Detecto-Medic, Brooklyn NY). BMI-for-age percentile was determined for each participant using the CDC SAS program that calculates age- and gender-specific percentiles using the 2000 CDC growth charts (42). Since both a BMI z-score and a BMI-for-age percentile are adjusted for a child’s age and gender, and a BMI z-score corresponds to a growth chart percentile by comparing it to a normal distribution table, the BMI-for-age percentile was chosen as the main outcome variable (43). Several participants with otherwise complete data had missing height and weight at the 16-y laboratory visit (n=26); thus, missing BMI-for-age percentiles were imputed using the expectation/maximization likelihood treatment of missing data described by Schafer (44). The imputation procedure consisted of modeling the available measurements from anthropometric data collected during the participant’s laboratory visits at ages 4, 5, 7, 10, 15 and 17. The model’s parameters were then used to define the data distribution from which to impute the missing BMI-for-age percentile values. To fully account for the data variability, and assuming that data were missing at random, ten sets were created in which all observed data were represented and missing data estimated, and the meaned values from the datasets were used in the analyses (44).
2.3. Statistical Analyses
Statistical analyses for the current study were conducted using SPSS 25.0 (25.0 SPSS Inc., Chicago, IL, 2017) and using SAS version 9.4 for the BMI-for-age percentile calculations (SAS Institute Inc., Cary, NC). Two separate hierarchical linear regression analyses were performed to test whether dietary restraint moderated the associations of disinhibition with weight (i.e., BMI-for-age percentile) and overall diet quality (i.e., HEI-2010 score). Continuous predictor variables, i.e. disinhibition and restraint, were first centered and an interaction term was created by multiplying the centered variables (45–47). Covariates in the model with BMI-for-age percentile as the dependent variable included gender, race and SES. In the regression model with HEI-2010 score, covariates included gender, race, SES and BMI-for-age percentile. The interaction was probed using the Johnson-Neyman technique, available from the PROCESS macro version 3.1 for SPSS (45), which identified specific scores for dietary restraint where the relationship between disinhibition and the outcome variable transitioned to significance (46). Statistical significance was set at a p-value of < 0.05.
3. Results
3.1. Descriptives
A total of 178 participants provided data for the main variables of interest and thus were included in the analyses for the current study. The sample’s characteristics are presented in Table 1. Adolescents in the sample adhered poorly to the Dietary Guidelines, as indicated by the low mean diet quality score (Table 1). Pearson bivariate correlations between the main variables and covariates of the study are presented in Table 2.
Table 1.
Sociodemographic, Anthropometric, and Dietary Characteristics of the Study Sample (n = 178)
| Descriptive Statistics | ||
|---|---|---|
| Variable | Mean ± SD | n (%) |
| Age | 16.6±0.4 | |
| Gender | ||
| Female | 103 (58) | |
| Male | 75 (42) | |
| Race/Ethnicitya,b | ||
| White | 116 (65) | |
| Non- White | 62 (35) | |
| SESb | 43.6±13.7 | |
| BMI-for-age Percentilec | 65.4±25.6 | |
| Weight Status Categoriesd | ||
| Underweight | 3 (2) | |
| Healthy weight | 125 (70) | |
| Overweight | 30 (17) | |
| Obese | 20 (11) | |
| Disinhibition Scoree | 4.7±2.8 | |
| Restraint Scoree | 6.3±4.1 | |
| HEI-2010 Scoree | 49.1±12.3 | |
| Kcalg | 1802±656 | |
Note.
Race included two categories based on the inclusion criteria of the larger study.
SES; socioeconomic status; 14% of the sample had missing information on SES at 16y lab visit. Available SES from closest time point was used (age 10 for all but 3 cases).
15% of the sample had missing information for height and weight at 16y lab visit.
BMI-forage percentile; body mass index-for-age percentile; cut offs developed by the CDC were used to categorize adolescents into weight categories: underweight=BMI <5%; healthy weight=BMI 5th-84.99 %; overweight=BMI 85th-94.99%; obese=BMI 95th-100 percentile.
Disinhibition scores ranging 0–16; restraint scores ranging 0–20.
HEI-2010; Healthy Eating Index; subjects with complete recalls (n=148).
Kcal; kilocalories per day average from complete recalls (n=148).
Table 2.
Bivariate Correlations Between Study Variables
| Variable | Gender | Race | SES | Restraint Score | Disinhibition Score | BMI-for-age % | HEI Score |
|---|---|---|---|---|---|---|---|
| Gender | |||||||
| Racea | 0.07 | ||||||
| SESb | −0.13 | −0.32 | |||||
| Restraint Scorec | .27** | −0.08 | 0.11 | ||||
| Disinhibition Scorec | 0.08 | −0.05 | 0.02 | .16* | |||
| BMI-for-age %d | 0.09 | .18* | −0.09 | .15* | .18* | ||
| HEI Scoree | 0.09 | −0.21 | .18* | .22** | 0.01 | −0.13 |
Note.
Significant at p<0.01 level.
Correlation is significant at the 0.05 level.
Race included two categories based on the inclusion criteria of the larger study, white/non-white.
SES; socioeconomic status.
Disinhibition scores ranging 0–16; restraint scores ranging 0–20.
BMI-for-age %; Body mass index-for-age percentile; calculated using SAS program developed by CDC.
HEI; Healthy Eating Index; subjects with complete recalls (n=148).
3.2. Regression Analysis for BMI-for-age Percentiles
Accounting for gender, race, and SES, the regression model was significant and explained 10% of the variance in adolescents’ BMI-for-age percentiles (R2=.10; F=3.13; p=.01). There was a significant main effect of disinhibition on BMI-for-age percentiles, indicating that individuals with higher disinhibition also had greater BMI-for-age percentiles (Table 3). There was not a significant interaction effect between disinhibition and restraint on the outcome (Table 3).
Table 3.
Results of Multiple Regression Analyses Predicting BMI-for-age Percentile from Disinhibition and Restraint Scores
| 95.0% CI | |||||||
|---|---|---|---|---|---|---|---|
| Variables | β | SE | Beta | t | Sig. | Lower | Upper |
| Block 1: Control Variables | |||||||
| Gender | 0.48 | 3.98 | 0.01 | 0.12 | 0.90 | −7.37 | 8.33 |
| Race | 10.23 | 4.14 | 0.19 | 2.47 | 0.01* | 2.06 | 18.41 |
| SESa | −0.07 | 0.15 | −0.04 | −0.49 | 0.63 | −0.36 | 0.22 |
| Block 2: Predictor | |||||||
| Disinhibition Score | 1.75 | 0.70 | 0.19 | 2.52 | 0.01* | 0.38 | 3.12 |
| Block 3: Moderator | |||||||
| Restraint Score | 0.94 | 0.48 | 0.15 | 1.96 | 0.05 | −0.01 | 1.90 |
| Block 4: Interaction Term | |||||||
| Disinhibition X Restraint | −0.23 | 0.17 | −0.10 | −1.34 | 0.18 | −0.57 | 0.11 |
p<.05;
SES; socioeconomic status
3.3. Regression Analysis for Diet Quality
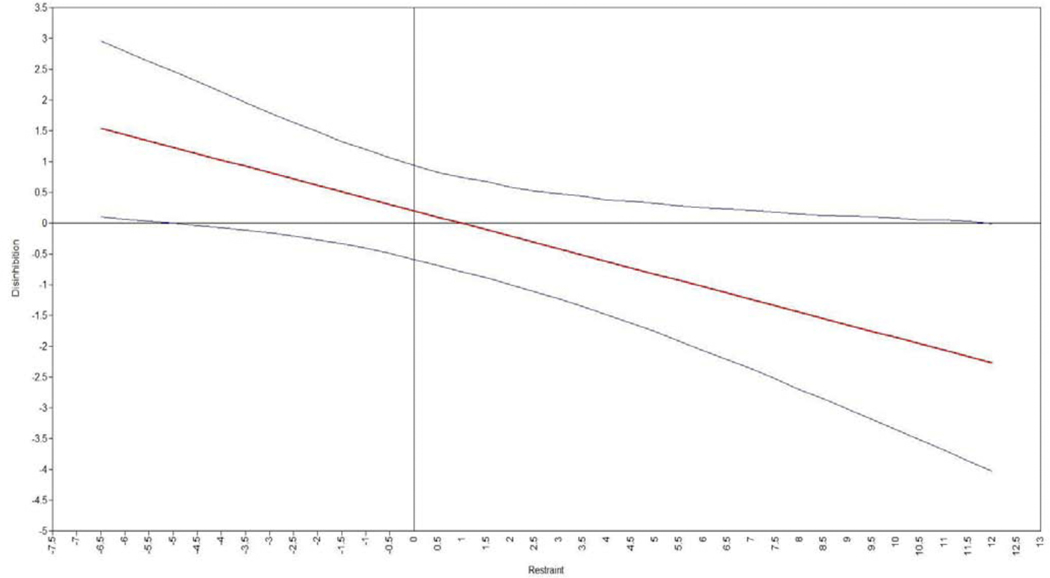
Accounting for gender, race, SES and BMI-for-age percentiles, the regression model explained 14% of the variance in the diet quality score (R2=.14; F=3.38; p=.002). The interaction effect between disinhibition and restraint in predicting diet quality was significant and explained a significant but small amount of variance beyond the main effect of disinhibition alone (R2 change= .03, F2 change=5.04, p=.03), suggesting that the association between disinhibition and diet quality was influenced by adolescent’s level of restraint (Table 4). The Johnson-Neyman technique showed that the moderating effect was significant when the mean restraint scores were <−6.23 [(equivalent to a non-centered score of 0.6), 2.0% of the restraint scores below this cutoff] and >7.80 [(equivalent to a non-centered score of 14.1), 5.4% of restraint scores above this cutoff] (Figure 1). The effect of restraint between these cutoff values was non-significant, suggesting that very high and very low levels of dietary restraint moderates the relationship between disinhibition and diet quality.
Table 4.
Results of Multiple Regression Analyses Predicting HEI-2010 Score from Disinhibition Score and Restraint Score
| 95.0% CI | |||||||
|---|---|---|---|---|---|---|---|
| Variables | β | SE | Beta | t | Sig. | Lower | Upper |
| Block 1: Control Variables | |||||||
| Gender | 1.58 | 2.08 | 0.06 | 0.76 | 0.45 | −2.54 | 5.69 |
| Race | −2.99 | 2.16 | −0.12 | −1.38 | 0.17 | −7.27 | 1.28 |
| SESa | 0.11 | 0.07 | 0.12 | 1.47 | 0.14 | −0.04 | 0.26 |
| BMI-for-age Percentileb | −0.06 | 0.04 | −0.14 | −1.66 | 0.10 | −0.14 | 0.01 |
| Block 2: Predictor | |||||||
| Disinhibition Score | 0.20 | 0.36 | 0.05 | 0.56 | 0.58 | −0.51 | 0.91 |
| Block 3: Moderator | |||||||
| Restraint Score | 0.58 | 0.25 | 0.20 | 2.32 | 0.02* | 0.09 | 1.07 |
| Block 4: Interaction Term | |||||||
| Disinhibition X Restraint | −0.21 | 0.09 | −0.18 | −2.24 | 0.03* | −0.39 | −0.03 |
p<.05;
SES; socioeconomic status.
Body mass index-for-age percentile
Figure 1.
Conditional Effects of Disinhibition as a Function of Dietary Restraint on Overall Diet Quality
Discussion
The main contribution of the current study is the examination of eating behaviors that may impact the BMI and diet quality of adolescents—a population with a high prevalence of unhealthy eating and obesity (47,48). It is well established that health behaviors track from adolescence into adulthood (49), and, as seen in adult populations, dysregulated eating behaviors are associated with negative weight-related health outcomes (18,50). Thus, it is critical to better understand the interactions of these eating behaviors to determine who might benefit most from particular intervention designs. The current study contributes to our current knowledge of disinhibition, restraint and their associations with weight and diet quality in a community sample of adolescents, as opposed to previous studies that have largely examined these eating behaviors in adults and/or overweight/obese individuals. Although further research with adolescents is still warranted, some findings presented here might be used when informing interventions for improving overall diet quality and/or weight outcomes in this population.
Higher levels of disinhibition were independently associated with higher BMI-for-age percentiles. This finding was expected and is consistent with findings from adult populations where disinhibition scores were positively associated with BMI and weight outcomes (19,24,51). The proposed mechanism of this relationship is related to the vulnerability of disinhibited eaters to consume high-energy, high-fat, and high-sugar foods, resulting in a positive energy balance (20,30,32). In contrast, dietary restraint alone, after controlling for gender, race, and SES, was not associated with BMI-for-age percentiles. A possible explanation for this finding is that the TFEQ measure of restraint does not differentiate between “perceived” and “physiological” restriction of food (41); subsequently, some individuals might score high on dietary restraint, meaning they eat less than desired but still exceed their physiological energy needs leading to higher BMI. This might be especially true for individuals with a tendency to overeat palatable foods, and those who are more vulnerable to the influences of today’s obesogenic food environments (15,35).
Some studies with adult samples suggest that restraint does not independently influence weight, but may attenuate the relationship between disinhibition and weight outcomes (19,24,28,29). Therefore, it was hypothesized that restraint would moderate the positive association between disinhibition and BMI-for-age percentile. In our adolescent sample, however, this interaction effect was not significant. It is important to note that the effect of restraint and disinhibition on weight outcomes is complex (19,24,28) and that the interplay between eating behaviors may be influenced by other factors that were not captured in the study, such as adolescents’ dieting status at the time of the study, body image, or weight concerns. For example, a study by Savage et al. (2009) examined associations between disinhibition, restraint and weight between dieters and non-dieters and found significant differences in the moderating ability of restraint on levels of disinhibition between groups by dieting status (28). Among non-dieters, higher disinhibition predicted higher weight to a greater extent when restraint was higher, whereas in dieters, higher disinhibition predicted higher weight when restraint was lower. Thus, additional factors related to weight control behaviors must be considered in future investigations of these associations.
With respect to dietary intake, scores for disinhibition were not independently associated with adolescents’ diet quality, whereas dietary restraint alone was associated with improved diet quality. These findings appear to contradict results from previous studies which have linked higher disinhibition to less healthful food selection and increased restraint to a consumption of healthier foods (30,52,53). These studies, however, tended to focus on a single food or nutrient and do not reflect a measure of overall diet quality and/or adherence to a healthy eating pattern (39). It is possible that disinhibited eaters have enough variability in their diet composition that scores for diet quality are neither positively nor negatively affected. On the other hand, it is well established that adolescence is a unique developmental period, marked by physiological growth and changes to both behavioral and cognitive systems (11). Food choices and food-related behaviors of adolescents are determined by a broad range of factors including parental and peer influence, time considerations, food availability, and convenience (35). Since personal factors are related to the initiation of behaviors among adolescents, they must be considered in greater depth when examining the relationship between eating behaviors and overall diet quality in future research.
One particular factor that has been related to diet quality is dieting efforts, which we did not account for in the current study. In previous studies among adolescents, unhealthy weight control behaviors, like skipping meals, were associated with lower intakes of fruits, vegetables and key micronutrients, whereas moderate weight-control behaviors, like replacing sugar-sweetened beverage with water, were associated with increased consumption of fruits and vegetables (36,54). Since our study focused on a broader construct of restraint only, future research should investigate specific subscales of restraint that influence food choices among adolescents.
The association between disinhibition and diet quality differed according to the level of adolescents’ dietary restraint. At very high levels of restraint, adolescents with low disinhibition had higher scores for overall diet quality, whereas at very low levels of restraint, adolescents with low disinhibition had lowered diet quality scores. This suggests that higher levels of dietary restraint might be necessary to positively influence overall diet quality, even among individuals with low disinhibition. It is possible that individuals with low disinhibition are less sensitive to food cues and cravings (55). Therefore, at high levels of restraint, these individuals are more likely to demonstrate improved diet quality whereas at low levels of restraint, a lack of cognitive control of eating results in low diet quality (55). On the other hand, for a majority of adolescents, the level of restraint did not impact the hedonic aspects of eating to moderate overall diet quality. This is not surprising given the poor diet quality scores in the sample. Given the abundant access to palatable foods in the current so-called obesogenic society, it is possible that the tendency toward eating opportunistically in such an environment overwhelms the ability to cognitively control food intake (14,15). It is also possible that restraint scores did not reflect long-term behavior, but rather inconsistent periods of dietary restriction which might then be followed by periods of disinhibition (27). This is in line with previous studies which found the level of disinhibition to be the best predictor of overall food consumption (56,57). However, the relationship between eating behaviors, such as restraint and disinhibition, with overall diet quality among adolescents needs to be explored further in future research.
This study had several strengths and limitations. One of the strengths was that data were collected during a time point when individuals were beginning to formulate behaviors that reflect personal choices. Therefore, findings from these analyses provide valuable insights into dysregulated eating patterns and their associations with health outcomes during this transitional period. Another strength was that overall diet quality, rather than individual foods or food groups, was estimated using three 24-hour dietary recalls and utilizing a multi-pass method that enhances the accuracy of food recall among individuals (58). Several limitations of the study must be also noted. Due to the cross-sectional design, we were not able to determine causal relationships between eating behaviors and weight outcomes or diet-quality. In addition, the sample was limited to a subset of adolescents originally involved in the RIGHT Track study at 2 years old so was not representative of 16-year-old adolescents in the U.S. Since the original enrollment, there has been some attrition due to relocation and loss to follow-up. Thus, there is a potential for bias in the current sample as those who have remained in the study may have intrinsic reason for doing so (Wideman et al., 2016). Finally, the assessment of eating behaviors was conducted using the TFEQ, which is a self-reported questionnaire and therefore cannot capture actual behaviors of adolescents in food-related situations and may have increased reporting bias during the study.
Conclusions:
The present study suggests that the association of disinhibition with diet quality is moderated by dietary restraint but only at very high and very low levels of this eating behavior. For the majority of adolescents in our sample, the effects of restraint did not impact the relationship between disinhibition and diet quality. Dietary restraint did not moderate the association between disinhibition and BMI-for-age percentiles. Overall, the research presented here suggests that additional factors likely influence the association between eating behaviors and nutrition-related outcomes among adolescents. Future research should examine these potential factors in larger samples of adolescents to advance our current understanding of how eating behaviors function in relation to diet quality and BMI during this period of transition.
Highlights.
Disinhibition predicted higher BMI-for-age percentiles among adolescents
Dietary restraint was associated with BMI-for-age percentiles and diet quality
Dietary restraint moderated the association between disinhibition and diet quality
Future work should examine subscales of restraint in relation to these outcomes
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.CDC. Adolescence: Preparing for Lifelong Health and Wellness [Internet]. Centers for Disease Control and Prevention. 2018. [cited 2019 May 24]. Available from: https://www.cdc.gov/grand-rounds/pp/2015/20150818-adolescent-wellness.html [Google Scholar]
- 2.Craigie AM, Lake AA, Kelly SA, Adamson AJ, Mathers JC. Tracking of obesity-related behaviours from childhood to adulthood: A systematic review. Maturitas. 2011. November 1;70(3):266–84. [DOI] [PubMed] [Google Scholar]
- 3.Healthy Behaviors in Adolescence [Internet]. HHS.gov. 2016. [cited 2019 May 24]. Available from: https://www.hhs.gov/ash/oah/adolescent-development/physical-health-and-nutrition/healthy-behavior/index.html
- 4.Predicting adult obesity from childhood obesity: a systematic review and meta- analysis - Simmonds - 2016 - Obesity Reviews - Wiley Online Library; [Internet]. [cited 2019 May 23]. Available from: https://onlinelibrary.wiley.com/doi/full/10.1111/obr.12334 [DOI] [PubMed] [Google Scholar]
- 5.Ogden CL. Prevalence of Obesity Among Youths by Household Income and Education Level of Head of Household — United States 2011–2014. MMWR Morb Mortal Wkly Rep [Internet]. 2018. [cited 2018 Apr 30];67. Available from: https://www.cdc.gov/mmwr/volumes/67/wr/mm6706a3.htm [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Krebs-Smith SM, Guenther PM, Subar AF, Kirkpatrick SI, Dodd KW. Americans do not meet federal dietary recommendations. J Nutr. 2010. October;140(10):1832–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Banfield EC, Liu Y, Davis JS, Chang S, Frazier-Wood AC. Poor Adherence to US Dietary Guidelines for Children and Adolescents in the National Health and Nutrition Examination Survey Population. J Acad Nutr Diet. 2016. January;116(1):21–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cutler GJ, Flood A, Hannan P, Neumark-Sztainer D. Major patterns of dietary intake in adolescents and their stability over time. J Nutr. 2009. February;139(2):323–8. [DOI] [PubMed] [Google Scholar]
- 9.Popkin BM, Gordon-Larsen P. The nutrition transition: worldwide obesity dynamics and their determinants. Int J Obes Relat Metab Disord J Int Assoc Study Obes. 2004. November;28 Suppl 3:S2–9. [DOI] [PubMed] [Google Scholar]
- 10.Lutter M, Nestler EJ. Homeostatic and hedonic signals interact in the regulation of food intake. J Nutr. 2009. March;139(3):629–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Das JK, Salam RA, Thornburg KL, Prentice AM, Campisi S, Lassi ZS, et al. Nutrition in adolescents: physiology, metabolism, and nutritional needs. Ann N Y Acad Sci. 2017. April;1393(1):21–33. [DOI] [PubMed] [Google Scholar]
- 12.Miller PE, Reedy J, Kirkpatrick SI, Krebs-Smith SM. The United States food supply is not consistent with dietary guidance: evidence from an evaluation using the Healthy Eating Index-2010. J Acad Nutr Diet. 2015. January;115(1):95–100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gordon-Larsen P. Food Availability/Convenience and Obesity12345. Adv Nutr. 2014. November 3;5(6):809–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Caspi CE, Sorensen G, Subramanian SV, Kawachi I. The local food environment and diet: a systematic review. Health Place. 2012. September;18(5):1172–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mattes R, Foster GD. Food environment and obesity. Obesity. 2014. December 1;22(12):2459–61. [DOI] [PubMed] [Google Scholar]
- 16.Birch LL, Davison KK. Family environmental factors influencing the developing behavioral controls of food intake and childhood overweight. Pediatr Clin North Am. 2001. August;48(4):893–907. [DOI] [PubMed] [Google Scholar]
- 17.Bouhlal S, McBride CM, Trivedi NS, Agurs-Collins T, Persky S. Identifying eating behavior phenotypes and their correlates: A novel direction toward improving weight management interventions. Appetite. 2017. April 1;111:142–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.French SA, Epstein LH, Jeffery RW, Blundell JE, Wardle J. Eating behavior dimensions. Associations with energy intake and body weight. A review. Appetite. 2012. October;59(2):541–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hays NP, Bathalon GP, McCrory MA, Roubenoff R, Lipman R, Roberts SB. Eating behavior correlates of adult weight gain and obesity in healthy women aged 55–65 y. Am J Clin Nutr. 2002. March;75(3):476–83. [DOI] [PubMed] [Google Scholar]
- 20.Bryant EJ, King NA, Blundell JE. Disinhibition: its effects on appetite and weight regulation. Obes Rev Off J Int Assoc Study Obes. 2008. September;9(5):409–19. [DOI] [PubMed] [Google Scholar]
- 21.French SA, Mitchell NR, Wolfson J, Finlayson G, Blundell JE, Jeffery RW. Questionnaire and laboratory measures of eating behavior: Associations with energy intake and BMI in a community sample of working adults. Appetite. 2014. January;72:50–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bond MJ, McDowell AJ, Wilkinson JY. The measurement of dietary restraint, disinhibition and hunger: an examination of the factor structure of the Three Factor Eating Questionnaire (TFEQ). Int J Obes Relat Metab Disord J Int Assoc Study Obes. 2001. June;25(6):900–6. [DOI] [PubMed] [Google Scholar]
- 23.Hawks SR, Madanat HN, Christley HS. Behavioral and Biological Associations of Dietary Restraint: A Review of the Literature. Ecol Food Nutr. 2008. September 25;47(5):415–49. [Google Scholar]
- 24.Williamson DA, Lawson OJ, Brooks ER, Wozniak PJ, Ryan DH, Bray GA, et al. Association of body mass with dietary restraint and disinhibition. Appetite. 1995. August;25(1):31–41. [DOI] [PubMed] [Google Scholar]
- 25.Provencher V, Drapeau V, Tremblay A, Després J-P, Lemieux S. Eating behaviors and indexes of body composition in men and women from the Québec family study. Obes Res. 2003. June;11(6):783–92. [DOI] [PubMed] [Google Scholar]
- 26.Johnson F, Wardle J, Griffith J. The Adolescent Food Habits Checklist: reliability and validity of a measure of healthy eating behaviour in adolescents. Eur J Clin Nutr. 2002. July;56(7):644–9. [DOI] [PubMed] [Google Scholar]
- 27.Schaumberg K, Anderson DA, Anderson LM, Reilly EE, Gorrell S. Dietary restraint: what’s the harm? A review of the relationship between dietary restraint, weight trajectory and the development of eating pathology. Clin Obes. 2016. April;6(2):89–100. [DOI] [PubMed] [Google Scholar]
- 28.Savage JS, Hoffman L, Birch LL. Dieting, restraint, and disinhibition predict women’s weight change over 6 y. Am J Clin Nutr. 2009. July;90(1):33–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lawson OJ, Williamson DA, Champagne CM, DeLany JP, Brooks ER, Howat PM, et al. The association of body weight, dietary intake, and energy expenditure with dietary restraint and disinhibition. Obes Res. 1995. March;3(2):153–61. [DOI] [PubMed] [Google Scholar]
- 30.Contento IR, Zybert P, Williams SS. Relationship of cognitive restraint of eating and disinhibition to the quality of food choices of Latina women and their young children. Prev Med. 2005. March;40(3):326–36. [DOI] [PubMed] [Google Scholar]
- 31.Johnson F, Pratt M, Wardle J. Dietary restraint and self-regulation in eating behavior. Int J Obes 2005. 2012. May;36(5):665–74. [DOI] [PubMed] [Google Scholar]
- 32.Leblanc V, Provencher V, Bégin C, Gagnon-Girouard M-P, Corneau L, Tremblay A, et al. Associations between eating patterns, dietary intakes and eating behaviors in premenopausal overweight women. Eat Behav. 2012. April;13(2):162–5. [DOI] [PubMed] [Google Scholar]
- 33.Ard JD, Desmond RA, Allison DB, Conway JM. Dietary Restraint and Disinhibition Do Not Affect Accuracy of 24-Hour Recall in a Multiethnic Population. J Am Diet Assoc. 2006. March 1;106(3):434–7. [DOI] [PubMed] [Google Scholar]
- 34.Camhi SM, Whitney Evans E, Hayman LL, Lichtenstein AH, Must A. Healthy eating index and metabolically healthy obesity in U.S. adolescents and adults. Prev Med. 2015. August;77:23–7. [DOI] [PubMed] [Google Scholar]
- 35.Neumark-Sztainer D, Story M, Perry C, Casey MA. Factors influencing food choices of adolescents: findings from focus-group discussions with adolescents. J Am Diet Assoc. 1999. August;99(8):929–37. [DOI] [PubMed] [Google Scholar]
- 36.Larson NI, Neumark-Sztainer D, Story M. Weight control behaviors and dietary intake among adolescents and young adults: longitudinal findings from Project EAT. J Am Diet Assoc. 2009. November;109(11):1869–77. [DOI] [PubMed] [Google Scholar]
- 37.Hollingshead AB. Four Factor Index of Social Status [1975]. 1975. Jan [cited 2017 Oct 11]; Available from: http://ubir.buffalo.edu/xmlui/handle/10477/1879
- 38.Stunkard AJ, Messick S. The three-factor eating questionnaire to measure dietary restraint, disinhibition and hunger. J Psychosom Res. 1985;29(1):71–83. [DOI] [PubMed] [Google Scholar]
- 39.Guenther PM, Casavale KO, Reedy J, Kirkpatrick SI, Hiza HAB, Kuczynski KJ, et al. Update of the Healthy Eating Index: HEI-2010. J Acad Nutr Diet. 2013. April;113(4):569–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.McGuire SUS Department of Agriculture and U.S. Department of Health and Human Services, Dietary Guidelines for Americans, 2010. 7th Edition, Washington, DC: U.S. Government Printing Office, January 2011. Adv Nutr Bethesda Md. 2011. May;2(3):293–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Onyango AW, De Onis M, Organization WH. WHO child growth standards: training course on child growth assessment. 2008; [Google Scholar]
- 42.SAS Program ( ages 0 to < 20 years ) | Resources | Growth Chart Training | Nutrition | DNPAO | CDC [Internet]. [cited 2018 Sep 21]. Available from: https://www.cdc.gov/nccdphp/dnpao/growthcharts/resources/sas.htm
- 43.Must A, Anderson SE. Body mass index in children and adolescents: considerations for population-based applications. Int J Obes. 2006. April;30(4):590–4. [DOI] [PubMed] [Google Scholar]
- 44.Schafer JL. Multiple imputation: a primer. Stat Methods Med Res. 1999. March;8(1):3–15. [DOI] [PubMed] [Google Scholar]
- 45.Bolin JH. Hayes, Andrew F. (2013). Introduction to Mediation, Moderation, and Conditional Process Analysis: A Regression-Based Approach. New York, NY: The Guilford Press. J Educ Meas. 2014;51(3):335–7. [Google Scholar]
- 46.Johnson PO, Fay LC. The Johnson-Neyman technique, its theory and application. Psychometrika. 1950. December;15(4):349–67. [DOI] [PubMed] [Google Scholar]
- 47.Fryar CD, Carroll MD, Ogden CL. Prevalence of obesity among children and adolescents: United States, trends 1963–1965 through 2009–2010. Natl Cent Health Stat. 2012;1960. [Google Scholar]
- 48.Ogden CL, Carroll MD, Lawman HG, Fryar CD, Kruszon-Moran D, Kit BK, et al. Trends in Obesity Prevalence Among Children and Adolescents in the United States, 1988–1994 Through 2013–2014. JAMA. 2016. June 7;315(21):2292–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Birch LL, Fisher JO. Development of eating behaviors among children and adolescents. Pediatrics. 1998. March;101(3 Pt 2):539–49. [PubMed] [Google Scholar]
- 50.Neumark-Sztainer D, Wall M, Guo J, Story M, Haines J, Eisenberg M. Obesity, disordered eating, and eating disorders in a longitudinal study of adolescents: how do dieters fare 5 years later? J Am Diet Assoc. 2006. April;106(4):559–68. [DOI] [PubMed] [Google Scholar]
- 51.Bellisle F, Clément K, Le Barzic M, Le Gall A, Guy-Grand B, Basdevant A. The Eating Inventory and body adiposity from leanness to massive obesity: a study of 2509 adults. Obes Res. 2004. December;12(12):2023–30. [DOI] [PubMed] [Google Scholar]
- 52.Lindroos AK, Lissner L, Mathiassen ME, Karlsson J, Sullivan M, Bengtsson C, et al. Dietary intake in relation to restrained eating, disinhibition, and hunger in obese and nonobese Swedish women. Obes Res. 1997. May;5(3):175–82. [DOI] [PubMed] [Google Scholar]
- 53.Lähteenmäki L, Tuorila H. Three-factor eating questionnaire and the use and liking of sweet and fat among dieters. Physiol Behav. 1995. January 1;57(1):81–8. [DOI] [PubMed] [Google Scholar]
- 54.Story M, Neumark-Sztainer D, Sherwood N, Stang J, Murray D. Dieting status and its relationship to eating and physical activity behaviors in a representative sample of US adolescents. J Am Diet Assoc. 1998. October;98(10):1127–35, 1255. [DOI] [PubMed] [Google Scholar]
- 55.Nansel TR, Lipsky LM, Eisenberg MH, Haynie DL, Liu D, Simons-Morton B. Greater Food Reward Sensitivity Is Associated with More Frequent Intake of Discretionary Foods in a Nationally Representative Sample of Young Adults. Front Nutr. 2016;3:33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Westenhoefer J, Broeckmann P, Münch AK, Pudel V. Cognitive control of eating behaviour and the disinhibition effect. Appetite. 1994. August;23(1):27–41. [DOI] [PubMed] [Google Scholar]
- 57.Van Strien T, Cleven A, Schippers G. Restraint, tendency toward overeating and ice cream consumption. Int J Eat Disord. 2000. November;28(3):333–8. [DOI] [PubMed] [Google Scholar]
- 58.Casey PH, Goolsby SLP, Lensing SY, Perloff BP, Bogle ML. The Use of Telephone Interview Methodology to Obtain 24-hour Dietary Recalls. J Am Diet Assoc. 1999. November 1;99(11):1406–11. [DOI] [PubMed] [Google Scholar]