Highlights
-
•
After implementing optimized model, we observed 34% reduction in supply chain costs.
-
•
Costs increased for Provincial store but decreased for Zones and health facilities.
-
•
Streamlined distribution practices supported cost reductions for transportation.
-
•
After implementing optimized model, costs increased in control Zones and facilities.
Keywords: Vaccine supply chain, EPI, Activity based costing, Costs, Democratic Republic of the Congo
Abstract
Objective
In 2017, an optimized immunization supply chain (iSC) model was implemented in Equateur Province, Democratic Republic of the Congo. The optimized model aimed to address iSC challenges and featured direct deliveries to service delivery points (SDPs), longer replenishment intervals and increased cold chain capacity. This assessment examines iSC costs before and 5 months after implementing the optimized model.
Materials & Methods
We used a nonexperimental pre-post study design to compare iSC costs before and after implementation. We applied an activity-based costing approach with a comparison arm to assess procurement, management, storage and transportation costs for three iSC tiers: Province (n = 1); Zone (n = 4) and SDP (n = 15). We included data from 3 treatment Zones and 11 treatment SDPs; 1 control Zone and 4 control SDPs. We used sample and population data to estimate iSC costs for the entirety of Equateur Province.
Results
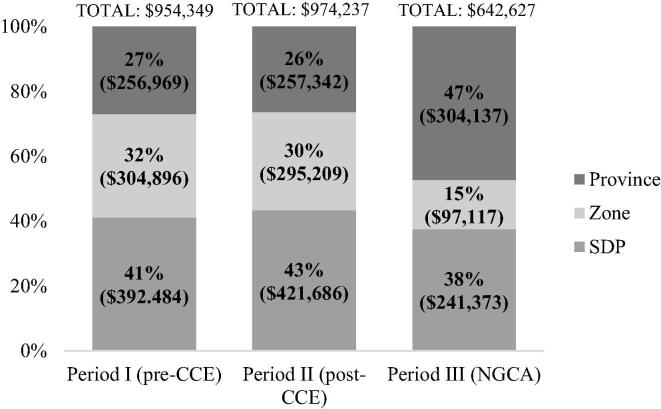
In the period immediately before implementing the optimized model, estimated annual iSC costs were $974,237. Following implementation, estimated annual iSC costs were $642,627—a 34% ($331,610) reduction. This change in costs was influenced by a 43% ($180,313) reduction in SDP costs, a 67% ($198,092) reduction in Zonal costs and an 18% ($46,795) increase in Provincial costs. After implementing the optimized model, average iSC costs for treatment Zones was $6,895 (SD: $6,072); for the control Zone was $21,738; for treatment SDPs was $989 (SD: $969); and for control SDPs was $1,356 (SD: $1,062).
Conclusions
We observed an absolute reduction in iSC costs in treatment Zones while control Zone post-implementation iSC costs remained the same or increased. The greatest cost reductions were for storage and transport at Zones and SDPs. Although cost implications of this model must continue to be evaluated over time, these findings are promising and will inform decisions around project expansion.
1. Introduction
Since 2010, the global vaccination coverage rate has plateaued at 85% [1]. In 2017, there were an estimated 20 million children with insufficient access to routine vaccination services—approximately 60% of whom lived in resource-constrained countries including the Democratic Republic of the Congo (DRC) [2]. Complex health system challenges such as geographic inaccessibility, unsustainable financing mechanisms, vaccine stock outs and ineffective commodity distribution systems contribute to gaps in vaccination coverage [3], [4], [5]. Efficient supply chains that ensure product availability at the service delivery point (SDP) are critical for closing the vaccination gap [6], [7]. However, immunization supply chains (iSC) in many low- and middle-income countries have not been substantially updated since they were designed in the 1970s and, therefore, lack capacity to meet current vaccination targets [8], [9]. Consequently, there is a growing movement to redeisgn iSC so that they are streamlined and sustainably financed for improved vaccination coverage [10], [5], [11].
Existing iSC must be modernized to efficiently leverage resources in order to accommodate current health systems needs and coverage targets even in resource-constrained settings [2], [7]. Computational simulated modeling studies suggest that streamlining iSC by reducing the number of supply chain tiers can improve system performance and reduce health system costs [12], [13], [14]. However, there are limited evaluations from diverse, real-world contexts corrborating these findings [21], [15], [16], [17]. Understanding the real-world cost implications of modernized iSC over time is important for understanding if these models can function efficiently, sustainably and at scale [18].
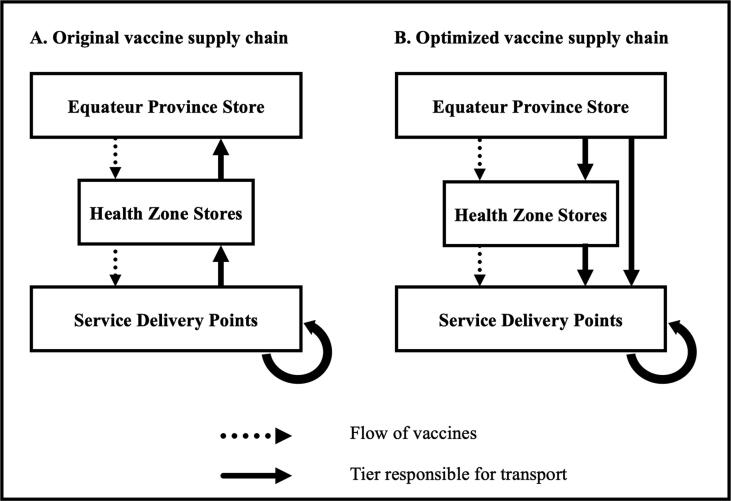
It is in this context that an optimized iSC model was developed, implemented and assessed in DRC [19]. In July 2017, the optimized iSC model was implemented in three Health Zones within Equateur Province (See Fig. 1 for details on iSC configuration). This model is called the Next Generation Supply Chain Initiative (in French, Nouvelle Génération des Chaînes d’Approvisionnement, or NGCA) and aims to improve commodity availability in Equateur Province—a rural, geographically dispersed and logistically challenged region in northwestern DRC—where only 42.6% of children <24 months have received all doses of the DPT (diphtheria, tetanus toxoids and pertussis) vaccine [20]. Supply chain related barriers including infrastructure challenges and complex geography compromise commodity availability and immunization coverage. An optimized iSC model was designed in a manner consistent with recent evidence supporting direct distribution for improved system effectiveness and efficiency [8], [21], [22]. Key features of the optimized iSC include:
-
•
Transitioning to routine (rather than ad hoc) delivery of vaccines and consumables
-
•
Increasing storage capacity to support lengthened replenishment cycles
-
•
Consolidating transportation responsibilities to higher iSC levels
Fig. 1.
Original and optimized vaccine supply chain configuration.
This evaluation preliminarily assesses the cost implications of the NGCA Initiative. We assessed the early impact of NGCA by comparing iSC costs before and five months after implementation. We hypothesized that the NGCA Initiative would correspond to reduced iSC costs. Findings from this assessment will contribute to the knowledge base outlining the cost implications of iSC redesign and empower iSC decision-makers with evidence to determine if the NGCA Initiative should be scaled up within and beyond Equateur Province.
2. Materials and Methods
2.1. Vaccine supply chain configuration
2.1.1. Original iSC configuration
The subnational iSC in Equateur Province has three tiers. The highest tier is the Provincial storage and administrative site which procures vaccines for the province and allocates funds for vaccine distribution. Equateur Province is subdivided into 18 Health Zones which, collectively, represent the subsequent iSC tier. Zonal warehouses collect vaccines from the Provincial store and provide vaccines to SDPs—the final tier of the iSC. Healthcare workers from SDPs equipped with cold chain equipment (CCE) travel monthly to zonal warehouses to collect vaccines. CCE-enabled SDPs collect stock to support their own needs and provide vaccines for neighboring SDPs that lack CCE. Trips to collect products from zonal stores can take from 0 to 2 days which may compromise vaccine potency. Healthcare workers often use their own resources and/or personal transportation such as motorcycles, rowboats or bicycles. See Fig. 1 for additional iSC configuration details.
2.1.2. Optimized iSC configuration
In 2017, VillageReach collaborated with the DRC Ministry of Health (with funding from the Government of the Democratic Republic of the Congo and the Bill & Melinda Gates Foundation) to implement a small-scale initiative that aims to improve iSC performance in Equateur Province by addressing inefficiencies related to ad-hoc distribution and collection. In the optimized iSC, logistical responsibilities are consolidated at the Provincial level, where health officials coordinate direct delivery of vaccines to Zones and SDPs. Key features of the optimized iSC include: direct deliveries from the Provincial storage site to Zones and SDPs, lengthening replenishment intervals from 30 to 60 days and including other health commodities in deliveries.
2.2. Study design
We used activity-based costing and a non-experimental pre-post study design with a comparison arm to evaluate iSC costs before and five months following implementation of an optimized iSC model (i.e., the NGCA Initiative) [23]. Equateur Province has 1 Provincial administrative and storage site, 18 Health Zones and 284 SDPs. From the Provincial administrative and storage site, 6 Health Zones are accessible by road and 12 are accessible by boat. Immunization supply chain performance widely varies across the Province. Thus, in 2016 VillageReach and the DRC Ministry of Health conducted a situation analysis of all Equateur Health Zones to identify three Health Zones for inclusion in the small-scale implementation of the optimized iSC. Stakeholders prioritized Health Zones with difficult geographic accessibility, poor stock availability and low vaccination coverage (mean DTC3 coverage rate of 57%, according to the Provincial stock management tool).
We used purposive sampling to select the three treatment Health Zones. Two of the treatment Health Zones are accessible by water and the remaining Health Zone is accessible by water or by land. One additional water-accessible Health Zone was selected as a comparator as it shared key characteristics (e.g., population size, total number of SDPs, number of CCE-enabled SDPs and geographic accessibility) with a treatment Zone. 11 SDPs were sampled from the three intervention Health Zones and 4 SDPs from the control Health Zone. The following criteria were used to select SDPs: status as a storage site (i.e., whether or not the SDP is CCE-enabled) and source of vaccine resupply (i.e., whether or not the SDP received vaccines from the Provincial storage site, Zonal storage site or a neighboring SDP equipped with CCE).
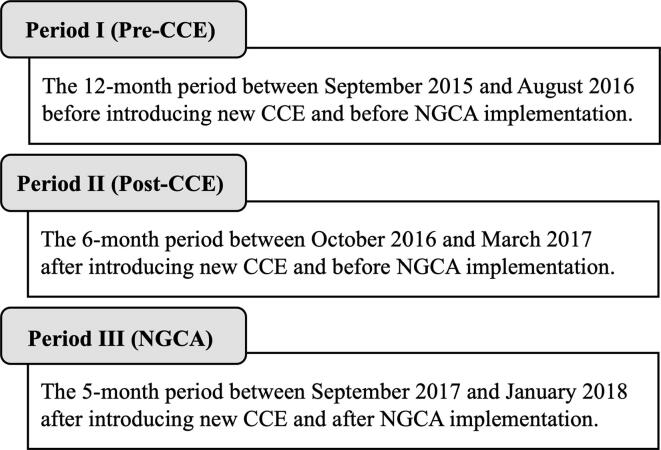
In September 2016, Equateur Province received 100 additional pieces of new solar-powered CCE. To accommodate the anticipated cost implications of this particularity, this assessment compares iSC costs across three different periods (see Fig. 2):
-
•
Period I (pre-CCE): Before CCE introduction and before implementation of the NGCA Initiative. Twelve-month period from September 2015 to August 2016.
-
•
Period II (post-CCE): After CCE introduction and before implementation of the NGCA Initiative. Six-month period from October 2016 to March 2017.
-
•
Period III (NGCA): After CCE introduction and after implementation of the NGCA Initiative. Five-month period from September 2017 to January 2018.
Fig. 2.
Periods considered in this assessment.
Because these time periods are variable in length, data from all periods are annualized to facilitate cross-period comparison.
This assessment did not involve human subjects and did not require patient records review. Data collection and analysis commenced after appropriate permissions and waivers were secured from central authorities in Kinshasa and provincial authorities in Equateur Province.
2.3. Data collection
We conducted baseline data collection for Period I and Period II in August and September of 2017. We conducted post-implementation data collection for Period III in February 2018. For all assessment periods, iSC costing data were captured for the three subnational iSC tiers—Province, Zone and SDP. We used Excel-based survey instruments to collect costing data. Survey instruments were adapted from the USAID | DELIVER PROJECT’s Supply Chain Costing Tool approach which has been described elsewhere [24]. Before commencing data collection activities, survey instruments were translated into French, pilot tested in Equateur and adapted to the local context. Two-person enumeration teams familiar with the local context, immunization logistics and health system were trained by the study lead on practices to support unbiased data collection. Data collectors were additionally trained to conduct data logic checks at the time of the in-person interview to resolve data quality concerns in real time. Immediately following data collection visits, all data collectors convened with the study lead for data review meetings to discuss and address data gaps and quality concerns. To resolve data concerns, interviewees were subsequently contacted via follow-up call, WhatsApp message and/or in-person when they visited the Provincial administrative site. Further, interviewees received minor monetary compensation for participating. In addition to in-person interviews, financial records were also used to determine costs at all levels. Together, these efforts were leveraged to address challenges of data inconsistencies as well as challenges related to reporting bias. Cost inputs were recorded in Congolese francs (CDF) or United States Dollars ($), as appropriate.
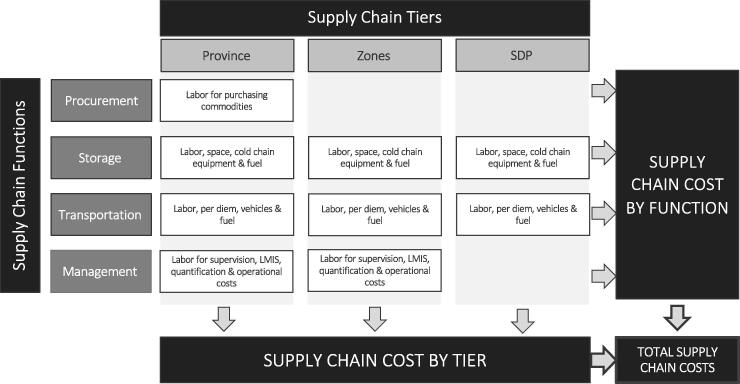
2.4. Data analysis
Following an approach similar to the USAID | DELIVER PROJECT, we collected resource-use data, for all three periods, to enable the estimation of Provincial costs for the following supply chain functions: procurement, storage, transportation and management [25]. Resource-use refers to the use of financial or other material resources that are required to operate the iSC. This includes, but is not limited to, customs fees for commodities, health care worker and other iSC staff time supporting the procurement, storage, transportation and management iSC functions, depreciation of fixed resources such as vehicles and cold chain equipment, bus fare to collect or distribute commodities, per diems, and annual costs that can be attributed to constructing or renting building space for the storage of commodities. See Fig. 3 for additional details on costs components considered. This cost categorization reflects USAID | DELIVER classifications and definitions that have been applied in similar costing evaluations [26], [27]. We estimated total iSC costs by supply chain function (i.e., storage, transportation, management and procurement) and tier. The costing data captured from Zones and SDPs were used to extrapolate costs to the entirety of Equateur Province using a population multiplier based on 2015 population data. Provincial cost estimates for Periods I and II were established using cost data from treatment as well as control Zones and SDPs (i.e., Zonal multiplier of 3.61 and SDP multiplier of 16.63). With respect to Zones, the Period I and II sample represents 27.7% of the population health area while the SDP sample represents 6% of the population. Thus, we multiplied the Zonal sample costs by 1/27.7% (i.e., 3.61) and SDP sample costs by 1/6% (i.e., 16.63) in order to establish estimates for Zones and SDPs in Equateur, respectively. Provincial cost estimates for Period III were established using 2015 population data and cost data from the treatment Zones and SDPs (i.e., Zonal multiplier of 4.69 and SDP multiplier of 22.19). For Period III, the Zonal sample represents 21.3% of the population health area while the SDP sample represents 4.5% of the population. Thus, we multiplied the Zonal sample costs by 1/21.3% (i.e., 4.69) and SDP sample costs by 1/4.5% (i.e., 22.19) to establish estimates for all Zones and all SDPs, respectively.
Fig. 3.
Cost components considered in this assessment.
In order to provide a more accurate depiction of changes in iSC costs across assessment periods, and to account for fluctuating currency, all results are annualized and denominated in US$ using an exchange rate of 913 CDF per US$ (Period I); 1182 CDF per US$ (Period II); and 1563 CDF per US$ (Period III) [28]. Importantly, estimates reflect operational costs of the optimized iSC model and do not reflect any initial investments required to commence implementation of the NGCA Initiative such as procurement of new cold chain equipment, technical support, implementation assessments and/or any leadership and governance strengthening undertaken to support sustainability and continued government ownership. Total iSC costs do not include the value of vaccines. Data analyses were executed using Microsoft Excel (Redmond, WA, USA).
3. Results
3.1. Costs by iSC tier
The annualized total cost estimates for Period I, Period II and Period III are $954,349, $974,237 and $642,627, respectively (Table 1; Table 2). As indicated in Table 1, Table 2, from Period I to II, overall costs borne by the Provincial-level remained stable with a < 1% ($373) increase in costs; however, we observed an 18% ($46,795) increase in Provincial-level costs from Period II to III. From Period I to II, overall Zonal costs remained relatively stable with a 3% ($9,687) reduction in costs; however, we observed a 67% ($198,092) reduction in overall Zonal-level costs from Period II to III. From Period I to II, overall SDP costs increased by 7% ($29,189); however, we observed a 43% ($180,300) reduction in overall SDP costs from Period II to III.
Table 1.
Comparative sample costs for Periods I and II.
| Period I | Period II | % Δ | |
|---|---|---|---|
| Province Procurement Costs | $826 | $4,606 | +458% |
| Zone Procurement Costs | $0 | $0 | 0% |
| SDP Procurement Costs | $0 | $0 | 0% |
| Total Procurement Costs | $826 | $4,606 | +458% |
| Province Storage Costs | $58,097 | $84,864 | +46% |
| Zone Storage Costs | $61,821 | $78,921 | +28% |
| SDP Storage Costs | $110,650 | $211,502 | +91% |
| Total Storage Costs | $230,568 | $312,373 | +36% |
| Province Transport Costs | $187,347 | $157,173 | −16% |
| Zone Transport Costs | $208,369 | $189,482 | −9% |
| SDP Transport Costs | $281,834 | $210,171 | −25% |
| Total Transport Costs | $677,550 | $515,927 | −24% |
| Province Management Costs | $10,699 | $10,699 | 0% |
| Zone Management Costs | $34,706 | $26,806 | –23% |
| SDP Management Costs | $0 | $0 | 0% |
| Total Management Costs | $45,404 | $30,392 | -33% |
| Province Total Costs | $256,969 | $257,342 | +<1% |
| Zone Total Costs | $304,896 | $295,209 | −3% |
| SDP Total Costs | $392,484 | $421,673 | +7% |
| Total Supply Chain Costs (Sample) | $954,349 | $974,237 | +2% |
Table 2.
Comparative sample costs for Periods II and III.
| Period II | Period III | % Δ | |
|---|---|---|---|
| Province Procurement Costs | $4,606 | $4,916 | +7% |
| Zone Procurement Costs | $0 | $0 | 0% |
| SDP Procurement Costs | $0 | $0 | 0% |
| Total Procurement Costs | $4,606 | $4,916 | +7% |
| Province Storage Costs | $84,864 | $82,665 | −3% |
| Zone Storage Costs | $78,921 | $43,252 | −45% |
| SDP Storage Costs | $211,510 | $204,298 | −3% |
| Total Storage Costs | $312,381 | $330,215 | −6% |
| Province Transport Costs | $157,173 | $205,857 | +31% |
| Zone Transport Costs | $189,482 | $45,116 | −76% |
| SDP Transport Costs | $210,176 | $37,075 | −82% |
| Total Transport Costs | $515,932 | $288,048 | −44% |
| Province Management Costs | $10,699 | $10,699 | 0% |
| Zone Management Costs | $26,806 | $8,748 | −67% |
| SDP Management Costs | $0 | $0 | 0% |
| Total Management Costs | $30,392 | $19,447 | −36% |
| Province Total Costs | $257,342 | $304,137 | +18% |
| Zone Total Costs | $295,209 | $97,117 | −67% |
| SDP Total Costs | $421,686 | $241,373 | −43% |
| Total Supply Chain Costs (Sample) | $974,237 | $642,627 | −34% |
3.2. Costs by iSC function
Considering the four main iSC functions, in Periods I and II, transportation represented the greatest iSC cost, followed by storage, management and procurement. In Period III, storage was the most substantial iSC cost, followed by transportation, management and procurement. From Period I to II there was a 24% ($161,623) reduction in transportation costs across all iSC tiers. From Period II to III there was a 44% ($227,879) reduction in transportation costs. From Period I to II there was a 36% ($82,805) increase in storage costs across all iSC tiers which coincided with the introduction of new CCE at SDPs across the Province. From Period II to III there was a 6% ($17,842) increase in storage costs across all iSC tiers.
3.3. Costs by iSC tier and function
At the Provincial level, storage costs increased by 46% ($26,767) from Period I to Period II. From Period II to III, there was a 3% ($2,199) reduction in Provincial storage costs. From Period I to II, there was a 16% ($30,174) reduction in Provincial transportation costs. From Period II to III, there was a 31% ($48,684) increase in Provincial transportation costs.
From Period II to III, there was a 45% ($35,669) reduction in Zonal storage costs which can be attributed to reductions in storage labor requirements, reduced expenditure on CCE fuel and maintenance costs and by currency devaluation. From Period II to III, there was a 76% ($144,366) reduction in Zonal transportation costs. From Period II to III, there was a 67% ($18,058) reduction in Zonal management costs due to decreased labor requirements at the Zone.
From Period I to II, there was a 91% ($100,852) increase in SDP storage costs. From Period II to III, there was a 3% ($7,204) reduction in SDP storage costs. From Period I to II there was a 25% ($71,662) decrease in SDP transportation costs. From Period II to III, there was an 82% ($173,096) decrease in SDP transportation costs.
3.4. Estimated iSC costs at scale
We estimated overall iSC costs of the NGCA Initiative operating across the entire Province of Equateur to be $642,626. We estimated overall Period II iSC costs to be $974,237 (Table 2). Comparing Period II to III cost estimates, this represents an estimated overall iSC cost savings of 34% ($331,610) if the NGCA Initiative were operating at scale within Equateur Province. We found that overall iSC costs remained relatively stable from Period I to Period II and were roughly split 25%, 35% and 40% moving down the iSC from the Province to the Zones and to the SDPs, respectively. By comparison, Period III costs were redistributed across iSC tiers and were split 47%, 15% and 38% from the Province, Zones and SDPs, respectively (Fig. 4). Extrapolated overall Provincial-level costs increased by 18% ($46,795) from Period II to III. Extrapolated overall Zonal costs decreased by 67% ($198,092) from Period II to III. Extrapolated overall SDP costs decreased by 42% ($180,300) from Period II to III.
Fig. 4.
Proportional supply chain cost estimates.
3.5. Estimated iSC costs in intervention vs control Zones and SDPs
In addition to comparing iSC across time periods, we also compared pre- and post-implementation costs from the control and treatment Zones and SDPs. In Period II, a Zone included in the NGCA implementation spent, on average $24,462 (SD $20,492) on iSC costs whereas the control Zone spent $8,497 on iSC costs. In Period II, an SDP included in the NGCA implementation spent, an average of $1,867 (SD $1,766) on iSC costs whereas an SDP from the control Zone spent, an average of $1,207 (SD $1,017) on iSC costs. In Period III, a Zone included in the NGCA implementation spent, an average of $6,895 (SD $6,072) on iSC costs whereas the control Zone spent $21,738 on iSC costs. In Period III, an SDP included in the NGCA implementation spent, an average of $989 (SD $969) on iSC costs whereas an SDP from the control Zone spent, an average of $1,356 (SD $1,062) on iSC costs (Table 3).
Table 3.
Comparative sample and control costs for Periods I, II and III.
| Period I – Avg (SD) |
Period II – Avg (SD) |
Period III – Avg (SD) |
||||
|---|---|---|---|---|---|---|
| SAMPLE | CONTROL | SAMPLE | CONTROL | SAMPLE | CONTROL | |
| Zone Storage Costs | $4,444 ($1,743) | $1,857 ($0) | $5,753 ($2,542) | $4,631 ($0) | $3,071 ($1,000) | $3,935 ($0) |
| SDP Storage Costs | $448 ($552) | $431 ($620) | $904 ($685) | $695 ($754) | $837 ($826) | $694 ($656) |
| Avg Storage Costs | $4,892 | $2,287 | $6,657 | $5,326 | $3,908 | $4,629 |
| Zone Transport Costs | $18,483 ($19,490) | $2,347 ($0) | $16,888 ($17,072) | $1,893 ($0) | $3,203 ($5,542) | $16,890 ($0) |
| SDP Transport Costs | $1,217 ($1,949) | $889 ($751) | $963 ($1,292) | $512 ($322) | $152 ($187) | $662 ($505) |
| Avg Transport Costs | $19,700 | $3,236 | $17,851 | $2,405 | $3,355 | $17,552 |
| Zone Management Costs | $2,357 ($2,033) | $2,555 ($0) | $1,821 ($1,570) | $1,973 ($0) | $621 ($333) | $913 ($0) |
| SDP Management Costs | $0 ($0) | $0 ($0) | $0 ($0) | $0 ($0) | $0 ($0) | $0 ($0) |
| Avg Management Costs | $2,357 | $2,555 | $1,821 | $1,973 | $621 | $913 |
| Zone Total Costs | $25,284 ($20,391) | $6,758 ($0) | $24,462 ($20,492) | $8,497 ($0) | $6,895 ($6,072) | $21,738 ($0) |
| SDP Total Costs | $1,666 ($2,224) | $1,320 ($1,368) | $1,867 ($1,766) | $1,207 ($1,017) | $989 ($969) | $1,356 ($1,062) |
| Avg Total Costs | $26,949 | $8,078 | $26,329 | $9,704 | $7,884 | $27,163 |
4. Discussion
This assessment provides real world, pre- and post-implementation data characterizing cost implications of an optimized iSC model in a rural and geographically complex area of DRC. These preliminary findings contribute to the expanding evidence base that corroborates findings from computational simulation modeling suggesting that streamlined distribution practices have the potential to reduce overall iSC costs.
In the period immediately before implementing the optimized system (i.e., Period II), iSC costs were $974,237. Following implementation of the optimized system (i.e., Period III) iSC costs were $642,627 which represents a 34% ($331,610) reduction in overall iSC costs. Following implementation of the optimized iSC, cost reductions were observed for the storage, transportation and management functions. This change in costs was primarily driven by a 76% ($144,366) reduction in transportation costs at the Zone and 82% ($173,096) reduction in transportation costs at the SDP. In the optimized iSC model, there was an increase in the number of cold-chain enabled SDPs. Furthermore, SDPs and Zones were no longer responsible for travelling to the Provincial store to collect commodities. This had important implications for Zone and SDP storage and transportation costs as well as iSC costs across tiers. The preliminary cost savings observed in this assessment are promising and indicate potential of the implementation (if operating at scale within Equateur Province) to substantially reduce overall Provincial iSC costs.
Cost reductions observed at SDPs and Zones can largely be attributed to a reduction in transportation costs due to expanded solar CCE capacity which allowed SDPs to store more commodities while simultaneously enabling longer replenishment intervals, thereby reducing (or, in many instances, eliminating) trips for commodity collection and reducing transportation as well as CCE fuel costs. Reduced Zonal costs can further be attributed to fewer personnel requirements to support the storage and management functions due to an increase in the number of CCE-enabled SDPs (which suppresses inventory handling and management at the Zone) and with the Provincial storage and administrative site playing a more active role in iSC commodity management. The marginal increase in Provincial costs can largely be attributed to increased Provincial-level responsibility for the transportation function due to direct deliveries from the Province to Zones as well as SDPs in the NGCA Initiative.
These findings confirmed our hypothesis that the optimized iSC model was less costly than the baseline system. The juxtaposition of increased iSC costs in control Zones and SDPs preliminarily supports a causal link between the NGCA implementation and reduced iSC costs. Furthermore, these findings indicate that consolidating resource-intensive functions to higher tiers of the iSC corresponds to a redistribution and reduction in overall iSC costs—with additional cost-savings potential if the implementation were operating at scale. This represents an intuitive finding considering economies of scale wherein cost efficiencies may be observed when larger scale operations are achieved. That is, when supply chain costs decrease alongside an increase in the volume of commodities moving through the system, the supply chain is expected to operate with greater cost efficiency. One of the key features of this implementation was doubling the replenishment interval. This was a pragmatic adaptation with important cost implications. Sarac et al. note that elongated replenishment frequencies have important implications for supply chain cost and performance such as lengthened forecasting intervals which may threaten requisition accuracy and promote surplus stock or stock outs; increased vaccine wastage and/or holding costs of surplus stock as well as increased costs associated with addressing stockout challenges [29]. We experienced significant challenges collecting performance data to evaluate cost-effectiveness. Prior to NGCA, stockouts were observed in the implementing SDPs for which historical performance data were available. In the five-months following the NGCA implementation, no stockouts were observed in implementing SDPs. Not only do our findings suggest that the NGCA implementation was indeed more cost-effective relative to the status quo iSC, they suggest that lengthened replenishment intervals did not harmfully impact iSC cost and performance.
Our results support computational simulation modeling evidence suggesting that cost efficiencies may be achieved by implementing a more streamlined iSC. Assi et al. used computer simulated modeling to assess the cost implications of removing the regional level from the Niger iSC. They observed a 7% reduction in logistics cost per dose delivered. Prosser et al., coupled a small-scale implementation with computerized simulated modeling to explore cost implications of streamlined vaccine delivery in Cabo Delgado Province, Mozambique. Using cost per fully-immunized child (i.e., children under age 24 months receiving the third dose of the DPT vaccine) as their performance metric, they found the streamlined iSC to be 17% more cost-effective relative to the control. Vledder et al., leveraged a large-scale randomized trial to evaluate cost and health implications of a two-tiered versus three-tiered essential medicine supply chain in Zambia [30]. They found that the two-tiered system was 3.5 times more cost-effective than the three-tiered system with respect to averting stock-outs.
Importantly, findings from our assessment contribute to country-specific evidence that can be leveraged to advance progress towards closing the vaccination coverage gap. Prior to implementing NGCA, national and provincial stakeholders identified barriers to commodity availability and championed for a streamlined approach to addressing these challenges. Our findings suggest that shifting responsibility and costs to higher iSC levels consolidated distribution management to better resourced iSC levels and resulted in streamlined deliveries with lower costs. While this evaluation revealed iSC cost reductions five months following the NGCA implementation, we might expect to more fully understand NGCA’s financial implications 3 to 5 years post-implementation.
This analysis has limitations that must be taken into consideration. We attempted to conduct a resource mapping exercise to identify current and future iSC funding sources. Unfortunately, we were unable to collect detailed information outlining partner support due to data sharing concerns. This is an important limitation for contextualizing the results in this manuscript. Without insights into partner resourcing, it is challenging to fully assess implementation sustainability.
Second, stakeholders purposively prioritized Health Zones with performance and accessibility challenges; thus, extrapolation of these findings must be judiciously considered. This analysis focused on river-based SDPs—which may result in an overestimation of costs and reduce generalizability of study findings. Still, these findings provide important insights considering that 67% of Health Zones must be accessed by water and the remaining ground-based Health Zones similarly experience high transportation costs due to difficult terrain in the region.
Third, the time period used for a costing evaluation typically includes one stable operational year; however, the introduction of new CCE in September 2016 added complexity due to changing costs during the baseline period. To address this particularity, two baseline periods of variable length were costed. Data from Periods II and III were annualized to facilitate comparison.
Finally, it is important to note the devaluation of the CDF. In Period I, the average exchange rate was 913 (CDF to US$), whereas in Period II the average exchange rate was 1182—a 23% decline [31]. Furthermore, the devaluation of the CDF corresponded with a 28% increase in inflation during Period II [32]. We report findings in US$ using the exchange rate for each corresponding study period. This was done to improve interpretability of iSC costs and facilitate comparison across periods. We acknowledge the complexities present during the implementation period and have attempted to identify and articulate the diverse influences to iSC costs.
Our results may be used for continued evaluation of the NGCA Initiative and to promote efficient iSC resource allocation. This methodology is applicable in diverse settings and may be used to expand the body of evidence for iSC costs. These findings are being used to advocate for project scale-up.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
Acknowledgments
We thank the Government of the Democratic Republic of the Congo, health facility staff, communities and institutions who made this research possible.
Funding
This project is funded by the Government of the Democratic Republic of the Congo through two agencies of the Ministry of Health: the Projet de Développement du Systeme de Santé (with funding from the World Bank) and the Cellule d’Appui et de Gestion Financière (with funding from the Global Fund to Fight AIDS, Tuberculosis and Malaria). Funding is also provided from the Bill & Melinda Gates Foundation [OPP1195513]. The views, conclusions and recommendations expressed herein are solely those of the authors and do not necessarily reflect the official policy or position of the Bill & Melinda Gates Foundation.
Footnotes
These findings were presented at the Global Health Supply Chain Summit’s 11th Annual Meeting on November 29, 2018 in Lusaka, Zambia.
References
- 1.United Nations, Population Division. (2018). The World Population Prospects - the 2017 revision. New York: WHO/UNICEF Joint Reporting Form.
- 2.World Health Organization. (2018). 2018 assessment report of the Global Vaccine Action Plan: strategic advisory group of experts on immunization (No. WHO/IVB/18.11). World Health Organization.
- 3.Favin M., Steinglass R., Fields R., Banerjee K., Sawhney M. Why children are not vaccinated: a review of the grey literature. Int Health. 2012;4(4):229–238. doi: 10.1016/j.inhe.2012.07.004. [DOI] [PubMed] [Google Scholar]
- 4.Rainey J.J., Watkins M., Ryman T.K., Sandhu P., Bo A., Banerjee K. Reasons related to non-vaccination and under-vaccination of children in low and middle income countries: findings from a systematic review of the published literature, 1999–2009. Vaccine. 2011;29(46):8215–8221. doi: 10.1016/j.vaccine.2011.08.096. [DOI] [PubMed] [Google Scholar]
- 5.Zaffran M., Vandelaer J., Kristensen D., Melgaard B., Yadav P., Antwi-Agyei K.O., Lasher H. The imperative for stronger vaccine supply and logistics systems. Vaccine. 2013;31:B73–B80. doi: 10.1016/j.vaccine.2012.11.036. [DOI] [PubMed] [Google Scholar]
- 6.WHO Immunization Practices Advisory Committee. (2014). Immunization supply chain and logistics: a neglected but essential system for national immunization programmes: A call-to-action for national programmes and the global community by the WHO Immunization Practices Advisory Committee, Geneva, Switzerland.
- 7.Songane M. Challenges for nationwide vaccine delivery in African countries. Int J Health Economics Manage. 2018;18(2):197–219. doi: 10.1007/s10754-017-9229-5. [DOI] [PubMed] [Google Scholar]
- 8.Lee B.Y., Haidari L.A., Prosser W., Connor D.L., Bechtel R., Dipuve A., Brown S.T. Re-designing the Mozambique vaccine supply chain to improve access to vaccines. Vaccine. 2016;34(41):4998–5004. doi: 10.1016/j.vaccine.2016.08.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Andrus J.K., Jauregui B., De Oliveira L.H., Ruiz Matus C. Challenges to building capacity for evidence-based new vaccine policy in developing countries. Health Aff. 2011;30(6):1104–1112. doi: 10.1377/hlthaff.2011.0361. [DOI] [PubMed] [Google Scholar]
- 10.Numbi F.K.M., Kupa B.M. The potential of next-generation supply chains to ease DRC's“ Casse-tête”. Vaccine. 2017;35(17):2105–2106. doi: 10.1016/j.vaccine.2016.11.096. [DOI] [PubMed] [Google Scholar]
- 11.Kaufmann J.R., Miller R., Cheyne J. Vaccine supply chains need to be better funded and strengthened, or lives will be at risk. Health Aff. 2011;30(6):1113–1121. doi: 10.1377/hlthaff.2011.0368. [DOI] [PubMed] [Google Scholar]
- 12.Assi T.M., Brown S.T., Kone S., Norman B.A., Djibo A., Connor D.L., Lee B.Y. Removing the regional level from the Niger vaccine supply chain. Vaccine. 2013;31(26):2828–2834. doi: 10.1016/j.vaccine.2013.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Brown S.T., Schreiber B., Cakouros B.E., Wateska A.R., Dicko H.M., Connor D.L., Rajgopal J. The benefits of redesigning Benin's vaccine supply chain. Vaccine. 2014;32(32):4097–4103. doi: 10.1016/j.vaccine.2014.04.090. [DOI] [PubMed] [Google Scholar]
- 14.Shittu E., Harnly M., Whitaker S., Miller R. Reorganizing Nigeria’s vaccine supply chain reduces need for additional storage facilities, but more storage is required. Health Aff. 2016;35(2):293–300. doi: 10.1377/hlthaff.2015.1328. [DOI] [PubMed] [Google Scholar]
- 15.Prosser W., Phillips N., McWhorter R., Kalangwe A. VillageReach and UNICEF; Seattle and Copenhagen: 2016. A system design approach for comprehensive immunization supply chain strengthening: a case study from Mozambique. [Google Scholar]
- 16.Aina M., Igbokwe U., Jegede L., Fagge R., Thompson A., Mahmoud N. Preliminary results from direct-to-facility vaccine deliveries in Kano Nigeria. Vaccine. 2017;35(17):2175–2182. doi: 10.1016/j.vaccine.2016.11.100. [DOI] [PubMed] [Google Scholar]
- 17.Prosser W., Jaillard P., Assy E., Brown S.T., Matsinhe G., Dekoun M., Lee B.Y. System redesign of the immunization supply chain: Experiences from Benin and Mozambique. Vaccine. 2017;35(17):2162–2166. doi: 10.1016/j.vaccine.2016.09.073. [DOI] [PubMed] [Google Scholar]
- 18.Mvundura M., Kien V.D., Nga N.T., Robertson J., Van Cuong N., Tung H.T., Levin C. How much does it cost to get a dose of vaccine to the service delivery location? Empirical evidence from Vietnam's Expanded Program on Immunization. Vaccine. 2014;32(7):834–838. doi: 10.1016/j.vaccine.2013.12.029. [DOI] [PubMed] [Google Scholar]
- 19.VillageReach., 2015. Exploring new distribution models for vaccines and other health commodities adapted to the on the ground realities of the Equateur and Tshuapa Provinces. Seattle, WA: VillageReach, http://www.villagereach.org/wp-content/uploads/2015/11/DRC-Supply-Chain-Assessment-FINAL-English-version.pdf.
- 20.Ministère du Plan et Suivi de la Mise en oeuvre de la Révolution de la Modernité (MPSMRM), Ministère de la Santé Publique (MSP), and ICF International. (2014). Enquête Démographique et de Santé en République Démocratique du Congo 2013–2014.
- 21.Vledder, M., Friedman, J., Sjoblom, M., Brown, T., & Yadav, P., 2010. Enhancing public supply chain management in Zambia. World Bank Evidence to Policy Paper. Washington, DC, The World Bank.
- 22.Yadav P. Health product supply chains in developing countries: diagnosis of the root causes of underperformance and an agenda for reform. Health Syst. Reform. 2015;1(2):142–154. doi: 10.4161/23288604.2014.968005. [DOI] [PubMed] [Google Scholar]
- 23.World Health Organization., 2008. WHO guide for standardization of economic evaluations of immunization programmes (No. WHO/IVB/08.14). Geneva: World Health Organization.
- 24.McCord, J., Tien, M., & Sarley, D., 2013. Guide to public health supply chain costing: a basic methodology. Arlington, VA: USAID | DELIVER PROJECT, Task Order 4, https://www.jsi.com/JSIInternet/Inc/Common/_download_pub.cfm?id=18156&lid=3.
- 25.Tien, M., Baruwa, E., & Young, D., 2013. Supply chain costing tool: Users manual. Arlington, VA: USAID | DELIVER PROJECT, Task Order 4.
- 26.Mwencha, M., Rosen, J. E., Spisak, C., Watson, N., Kisoka, N., & Mberesero, H., 2017. Upgrading supply chain management systems to improve availability of medicines in Tanzania: evaluation of performance and cost effects. Global Health: Science and Practice, GHSP-D. Doi: 10.9745/GHSP-D-16-00395 [DOI] [PMC free article] [PubMed]
- 27.Sarley, D., Baruwa, E., & Tien, M., 2010. Zimbabwe: Supply chain costing of health commodities. Arlington, VA: USAID | DELIVER PROJECT, Task Order 4.
- 28.freecurrencyrates.com accessed Sept, 2017.
- 29.Sarac A., Absi N., Dauzère-Pérès S. A literature review on the impact of RFID technologies on supply chain management. Int J Prod Econ. 2010;128(1):77–95. [Google Scholar]
- 30.Vledder, M., Friedman, J., Sjöblom, M., Brown, T., & Yadav, P., 2019. Improving Supply Chain for Essential Drugs in Low Income Countries: Results from a Large Scale Randomized Experiment in Zambia. Health Systems & Reform. [DOI] [PubMed]
- 31.freecurrencyrates.com accessed Sept, 2017.
- 32.https://tradingeconomics.com/congo/inflation-cpi accessed Nov 2017.