Abstract
Background
This study aimed to assess the prevalence of missed canals in endodontically treated teeth and their association with apical periodontitis in a Saudi Arabian population using CBCT.
Materials and Methods
A total of 208 CBCT radiographs were investigated. For each tooth, radiographs of axial, coronal, and sagittal segments were acquired to appraise the external as well as the internal structure of the root canal system and apical area. In root canal-treated teeth, unfilled canals appearing from the cementoenamel junction to the apex were defined as missed untreated canals; and a periapical lesion was considered when disruption of the lamina dura was detected, and the low-density area associated with the radiographic apex was at least twice the width of the periodontal ligament space. The data were presented as frequencies and percentages. The Z-test was used to analyze the differences in proportions with the significance level set at P value <0.05.
Results
The overall prevalence of missed canals among endodontically treated teeth was 18%. The prevalence of missed canals was higher in maxillary first molars with 40.6%. The overall prevalence of apical periodontitis among teeth with missed canals was 90%. It was 84.2% in the maxilla and 100% in the mandible. The second mesiobuccal canal in the maxillary first molars and mesiobuccal and distobuccal canals in mandibular teeth were the most missed canals.
Conclusion
Apical periodontitis in root canal-treated teeth with missed canals was high (90%), with most identified missed canals in maxillary and mandibular first molars.
1. Introduction
The principal objectives of root canal therapy (RCT) are to perform adequate biomechanical shaping, cleaning, and filling the entire root canal system (RCS) 3-dimensionally (3D). Inability to do so inevitably leads to an unfavourable outcome [1]. Studies have shown many factors attributed to endodontic failure, including but not limited to persistent bacterial infection [2], inadequate root filling [3], and untreated/missed canals [4]. Few studies reported RCT failure due to missed canals ranging from 12% to 42% in different populations [5–8].
The importance of locating all existing canals within the RCS to achieve optimal prognosis has been discussed by many authors, and potential negative effects of untreated canals on the treatment result have been debated with overwhelming evidence of missed canals in failed cases requiring endodontic retreatment [5, 9, 10]. Apical periodontitis (AP) was observed in 98% of the teeth with untreated canals, which was a significantly greater frequency in comparison with teeth with all canals treated [6]. Clinician's lack of knowledge of the RCS and its complexity may result in missing of canals during RCT. These canals serve as a pool of microorganisms, which is the main cause of forming or persistent apical periodontitis [11] and may have a negative impact on the prognosis [12, 13]. The conventional intraoral radiograph was used in old studies [14–17] to evaluate the posttreatment apical periodontitis, and because of its inherited limitations as a 2-dimensional (2D) method to assess a 3D object, locating missed treated canals was a challenge. Recently, cone-beam computed tomographic (CBCT) imaging allows for precise visualization of a given tooth in 3D [7]. The prevalence of missed canals in endodontically treated teeth and their association with apical lesions have been evaluated by means of CBCT in recent studies in different populations [6–8], where it showed more accurate and reliable results.
Upon literature search, no study was conducted in Saudi Arabia utilizing CBCT to evaluate the prevalence of missed canals and their association with AP. The need to do so is paramount to emphasize the importance of understanding the root canal anatomy before initiating RCT and to highlight the most affected teeth and manage them accordingly.
So, the aim of this study, therefore, was to assess the prevalence of missed canals in endodontically treated teeth and their association with apical periodontitis in a Saudi Arabian population utilizing in vivo CBCT.
2. Materials and Methods
This cross-sectional study included 208 CBCT images which were retrospectively collected from the archive of the College of Dentistry, Jazan University, Saudi Arabia, between January 2017 and July 2019. These CBCTs belong to patients (100 males and 108 females) referred to the College of Dentistry for dental treatment (no patient was exposed to radiography for the sake of the study; all CBCTs were taken for other diagnostic purposes). Ethical approval from the Standing Committee for Scientific Research Ethics at Jazan University was obtained before commencing the study (ref no.: REC41/1-008). All endodontically treated and nontreated posterior maxillary and mandibular teeth were included except third molars. Distorted/unclear images, retained primary teeth, or remaining roots on the CBCT radiographs were excluded. Initially, more than 250 full mouth CBCT scans were collected, and after applying the inclusion and exclusion criteria, only 208 scans were included in the study. The CBCT machine, 3D Accuitomo 170 (MORITA, Japan), was used with the following features: 90 Kv, 5–8 mA, 17.5 s exposure time, and 0.25 mm voxel size. The software imaging program MORITA i‐Dixel 3D was used for processing of the CBCT radiographs. Each scan was evaluated by 3 calibrated general practitioners as a group; when the group encountered a doubt, an expert endodontist in reading CBCT was consulted for the final decision.
For each tooth, radiographs of axial, coronal, and sagittal segments were acquired to appraise the external as well as the internal structure of the root canal system and apical area. For the purpose of this study, unfilled canals, appearing from the cementoenamel junction to the apex, were defined as missed untreated canals. AP was considered when disruption of the lamina dura was detected, and the low-density area associated with the radiographic apex was at least twice the width of the periodontal ligament space [18, 19].
2.1. Statistical Analysis
The collected data were analyzed using a statistical software program for Windows (SPSS V25; IBM, Chicago, IL). The results were presented as frequencies and percentages. The Z-test was used to analyze the differences in proportions with the significance level set at P value <0.05.
3. Results
The prevalence of RCT among 3046 screened teeth (1529 maxillary and 1517 mandibular) was 5.4% (n = 165 teeth). The overall prevalence of missed canals among endodontically treated teeth was 18% (n = 30 out of 165). The prevalence in the maxilla was higher than in the mandible (19 compared to 11). The prevalence of missed canals was higher in maxillary first molars with 40.6% (CI95% = 24%–58%; P=0.380) followed by maxillary first premolars with 13.6% (CI95% = 0%–28%; P < 0.001), while the lowest prevalence was found in maxillary second premolars with 4.3% (CI95% = 0%–13%; P < 0.001). All missed canals in the mandible were found in the first molars with a prevalence of 25% (CI95% = 12%–38%; P < 0.001) (Table 1). Apical periodontitis was highly associated with missed canals. The overall prevalence of AP among teeth with missed canals was 90% (27 out of 30). It was 84.2% in the maxilla (Table 2) and 100% in the mandible (Table 3). The second mesiobuccal (MB2) canal in the maxillary first molars was tthe most missed treated canal (Figure 1), followed by the distobuccal canal. In the mandible, the mesiobuccal and distobuccal canals were the most missed canals, followed by mesiolingual and distolingual canals (Figure 2).
Table 1.
Prevalence of apical periodontitis and missed canals among endodontically treated teeth.
| Apical periodontitis | Missed treated canals | |||
|---|---|---|---|---|
| Yes | No | Yes | No | |
| Maxillary teeth (N = 89) | ||||
| First premolars (N = 22) | 12 (54.5) | 10 (45.5) | 3 (13.6) | 19 (86.4) |
| Second premolars (N = 23) | 18 (78.3) | 5 (21.7) | 1 (4.3) | 22 (95.7) |
| First molars (N = 32) | 25 (78.1) | 7 (21.9) | 13 (40.6) | 19 (59.4) |
| Second molars (N = 12) | 10 (83.3) | 2 (16.7) | 2 (16.7) | 10 (83.3) |
| Total | 65 (73.0) | 24 (27.0) | 19 (21.3) | 70 (78.7) |
|
| ||||
| Mandibular teeth (N = 76) | ||||
| First premolars (N = 2) | 1 (50.0) | 1 (50.0) | 0 (0.0) | 2 (100.0) |
| Second premolars (N = 13) | 6 (46.2) | 7 (53.8) | 0 (0.0) | 13 (100.0) |
| First molars (N = 44) | 39 (88.6) | 5 (11.4) | 11 (25.0) | 33 (75.0) |
| Second molars (N = 17) | 12 (70.6) | 5 (29.4) | 0 (0.0) | 17 (100.0) |
| Total | 58 (76.3) | 18 (23.7) | 11 (14.5) | 65 (85.5) |
Table 2.
Apical periodontitis among maxillary teeth with missed treated canals.
| Teeth | Canal | Radiolucency | |
|---|---|---|---|
| Yes | No | ||
| First premolars (N = 3) | Buccal | 1 (33.3) | 0 (0.0) |
| Palatal | 2 (66.7) | 0 (0.0) | |
|
| |||
| Second premolars (N = 1) | Buccal | 0 (0.0) | 0 (0.0) |
| Palatal | 0 (0.0) | 1 (100.0) | |
|
| |||
| First molars (N = 13) | Mesiobuccal | 8 (61.5) | 2 (15.4) |
| Distobuccal | 3 (23.1) | 0 (0.0) | |
| Palatal | 0 (0.0) | 0 (0.0) | |
|
| |||
| Second molars (N = 2) | Mesiobuccal | 1 (50.0) | 0 (0.0) |
| Distobuccal | 1 (50.0) | 0 (0.0) | |
| Palatal | 0 (0.0) | 0 (0.0) | |
Table 3.
Apical periodontitis among mandibular teeth with missed treated canals.
| Teeth | Canal | Apical periodontitis | |
|---|---|---|---|
| Yes | No | ||
| First premolars (N = 0) | One root | — | — |
|
| |||
| Second premolars (N = 0) | One root | — | — |
|
| |||
| First molars (N = 11) | Mesiobuccal | 3 (27.3) | 0 (0.0) |
| Mesiolingual | 2 (18.2) | 0 (0.0) | |
| Distobuccal | 3 (27.3) | 0 (0.0) | |
| Distolingual | 2 (18.2) | 0 (0.0) | |
| Mesial | 0 (0.0) | 0 (0.0) | |
| Distal | 1 (9.0) | 0 (0.0) | |
|
| |||
| Second molars (N = 0) | Mesiobuccal | — | — |
| Mesiolingual | — | — | |
| Distobuccal | — | — | |
| Distolingual | — | — | |
| Mesial | — | — | |
| Distal | — | — | |
Figure 1.
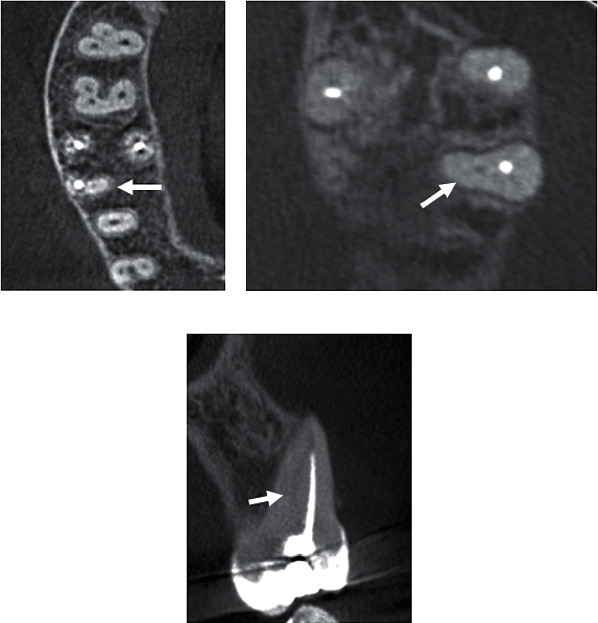
CBCT slices of the maxillary first molar: (a, b) axial section with the missed MB2 canal (arrows); (c) coronal section with the missed MB2 canal (arrow).
Figure 2.
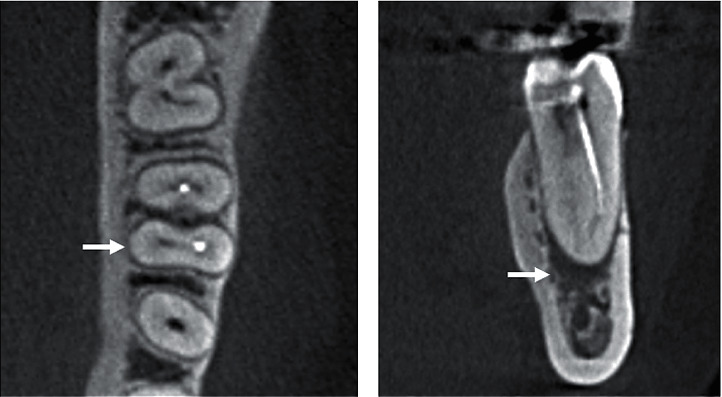
CBCT slices of the mandibular first molar: (a) axial section with the missed ML canal (arrow); (b) coronal section with the missed ML canal and the presence of apical radiolucency (arrow).
4. Discussion
In vivo CBCT scan was used in this study to evaluate the frequency of missed canals and their association with AP in RCT teeth. CBCT has many benefits that provides 3D images allowing the analysis of multiple slices per tooth [20], and it is less susceptible to errors in identifying RCS than conventional and digital periapical radiographs [5, 21]. In addition, comparative studies showed more accurate results of CBCT compared to conventional radiographs in detecting AP, especially in a small lesion with minimal apical bone destruction [22–25]. Thus, the inherited limitations of conventional radiography may negatively affect the detection of missed canals and AP in old studies, where it might show false negative results.
Endodontic literature has shown clearly that a high frequency of missed canals in RCT teeth needs nonsurgical endodontic retreatment. Hoen and Pink [5] found missed canals in 42% of all teeth that were retreated nonsurgically, while Karabucak et al. [7] reported the overall prevalence of missed canals to be 23%, but Costa et al. [6] and Baruwa et al. [8] found a quite small prevalence of 12%. In the present study, the overall frequency of missed canals among endodontically treated teeth was 18%, which is in between compared to the previous studies. The difference between our study and the previously reported data could be attributed to the study sample, methodology, and population; however, the results somewhat confirmed the same finding. In our study, we found the frequency of AP in RCT teeth with missed canals as 90%. Karabucak et al. [7] and Baruwa et al. [8] reported slightly lower percentage (82.8% and 82.6%, respectively), while Costa et al. [6] found a very high prevalence of 98% among teeth with missed treated canals. All studies showed a strong association between missed canals and apical periodontitis.
Maxillary molars presented with a complex RCS where the mesiobuccal (MB) root had 2 canals (the second one is known as MB2) [26–29]. The MB root has been reported to have the highest frequency of missed treated canals in many previous studies, with 85%, 65%, and 62.8% [6–8]. These findings are comparable to our finding where 61% of MB had missed treated canals, while in mandibular teeth, MB and DB canals in the first molars were the most missed treated canals in our sample (27.3% and 27.3%, respectively). This is in contrast with previously reported data on the same tooth where 62% and 62.9% of missed canals were found in the distal root [7, 8]. The difference between our finding and others might be related to the small sample size of the present study. Interestingly, in the present study, the mandibular first molar was the only RCT tooth that presented missed canals. The high rate of missed canals in this tooth might be related to the anatomic variability, both in the number of roots and root canals [30–32].
The main limitation of our cross-sectional study apart from the sample size is its nature, which evaluated the teeth at a given point of time, and the information about the situation of apical periodontitis and when the treatment is done is unknown, which means that some lesions might be healing once the treatment is just done, so a cause-effect relation cannot be established [33]. In addition, many factors could affect the treatment outcome, including techniques, materials, asepsis, preoperative status of the tooth, and expertise of the clinicians [34–36].
5. Conclusion
Within the limitation of the present study, the frequency of AP in RCT teeth with missed canals was high (90%), with most identified missed canals in maxillary and mandibular first molars. All measures available including CBCT and dental operative microscope should be used to maximize the identification of the RCS.
Data Availability
The data supporting the findings of this study are available from the corresponding author upon reasonable request.
Conflicts of Interest
The authors declare that they have no conflicts of interest.
References
- 1.Vertucci F. J. Root canal morphology and its relationship to endodontic procedures. Endodontic Topics. 2005;10(1):3–29. doi: 10.1111/j.1601-1546.2005.00129.x. [DOI] [Google Scholar]
- 2.Nair P. N. R., Sjögren U., Krey G., Kahnberg K.-E., Sundqvist G. Intraradicular bacteria and fungi in root-filled, asymptomatic human teeth with therapy-resistant periapical lesions: a long-term light and electron microscopic follow-up study. Journal of Endodontics. 1990;16(12):580–588. doi: 10.1016/s0099-2399(07)80201-9. [DOI] [PubMed] [Google Scholar]
- 3.Ray H. A., Trope M. Periapical status of endodontically treated teeth in relation to the technical quality of the root filling and the coronal restoration. International Endodontic Journal. 1995;28(1):12–18. doi: 10.1111/j.1365-2591.1995.tb00150.x. [DOI] [PubMed] [Google Scholar]
- 4.Nair P. N. R. On the causes of persistent apical periodontitis: a review. International Endodontic Journal. 2006;39(4):249–281. doi: 10.1111/j.1365-2591.2006.01099.x. [DOI] [PubMed] [Google Scholar]
- 5.Hoen M., Pink F. Contemporary endodontic retreatments: an analysis based on clinical treatment findings. Journal of Endodontics. 2002;28(12):834–836. doi: 10.1097/00004770-200212000-00010. [DOI] [PubMed] [Google Scholar]
- 6.Costa F. F. N. P., Pacheco-Yanes J., Siqueira J. F., et al. Association between missed canals and apical periodontitis. International Endodontic Journal. 2019;52(4):400–406. doi: 10.1111/iej.13022. [DOI] [PubMed] [Google Scholar]
- 7.Karabucak B., Bunes A., Chehoud C., Kohli M. R., Setzer F. Prevalence of apical periodontitis in endodontically treated premolars and molars with untreated canal: a cone-beam computed tomography study. Journal of Endodontics. 2016;42(4):538–541. doi: 10.1016/j.joen.2015.12.026. [DOI] [PubMed] [Google Scholar]
- 8.Baruwa A. O., Martins J. N. R., Meirinhos J., et al. The influence of missed canals on the prevalence of periapical lesions in endodontically treated teeth: a cross-sectional study. Journal of Endodontics. 2020;46(1):34–39. doi: 10.1016/j.joen.2019.10.007. [DOI] [PubMed] [Google Scholar]
- 9.Huumonen S., Kvist T., Grondahl K., Molander A. Diagnostic value of computed tomography in re-treatment of root fillings in maxillary molars. International Endodontic Journal. 2006;39(10):827–833. doi: 10.1111/j.1365-2591.2006.01157.x. [DOI] [PubMed] [Google Scholar]
- 10.Von Arx T. Frequency and type of canal isthmuses in first molars detected by endoscopic inspection during periradicular surgery. International Endodontic Journal. 2005;38(3):160–168. doi: 10.1111/j.1365-2591.2004.00915.x. [DOI] [PubMed] [Google Scholar]
- 11.Wolcott J., Ishley D., Kennedy W., Johnson S., Minnich S., Meyers J. A 5 yr clinical investigation of second mesiobuccal canals in endodontically treated and retreated maxillary molars. Journal of Endodontics. 2005;31(4):262–264. doi: 10.1097/01.don.0000140581.38492.8b. [DOI] [PubMed] [Google Scholar]
- 12.Cantarone G., Berutti E., Castelucci A. Missed anatomy: frequency and clinical impact. Endodontic Topics. 2006;15(1):3–31. doi: 10.1111/j.1601-1546.2009.00240.x. [DOI] [Google Scholar]
- 13.Witherspoon D. E., Small J. C., Regan J. D. Missed canal systems are the most likely basis for endodontic retreatment of molars. Texas Dental Journal. 2013;130(2):127–139. [PubMed] [Google Scholar]
- 14.Tronstad L., Asbjørnsen K., Døving L., Pedersen I., Eriksen H. M. Influence of coronal restorations on the periapical health of endodontically treated teeth. Dental Traumatology. 2000;16(5):218–221. doi: 10.1034/j.1600-9657.2000.016005218.x. [DOI] [PubMed] [Google Scholar]
- 15.Eckerbom M., Magnusson T. Evaluation of technical quality of endodontic treatment—reliability of intraoral radiographs. Dental Traumatology. 1997;13(6):259–264. doi: 10.1111/j.1600-9657.1997.tb00052.x. [DOI] [PubMed] [Google Scholar]
- 16.Tsuneishi M., Yamamoto T., Yamanaka R., et al. Radiographic evaluation of periapical status and prevalence of endodontic treatment in an adult Japanese population. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology, and Endodontology. 2005;100(5):631–635. doi: 10.1016/j.tripleo.2005.07.029. [DOI] [PubMed] [Google Scholar]
- 17.Siqueira J. F., Rôças I. N., Alves F. R. F., Campos L. C. Periradicular status related to the quality of coronal restorations and root canal fillings in a Brazilian population. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology, and Endodontology. 2005;100(3):369–374. doi: 10.1016/j.tripleo.2005.03.029. [DOI] [PubMed] [Google Scholar]
- 18.Abella F., Patel S., Duran-Sindreu F., Mercadé M., Bueno R., Roig M. Evaluating the periapical status of teeth with irreversible pulpitis by using cone-beam computed tomography scanning and periapical radiographs. Journal of Endodontics. 2012;38(12):1588–1591. doi: 10.1016/j.joen.2012.09.003. [DOI] [PubMed] [Google Scholar]
- 19.Zhang M.-M., Liang Y.-H., Gao X.-J., Jiang L., Van der Sluis L., Wu M.-K. Management of apical periodontitis: healing of post-treatment periapical lesions present 1 year after endodontic treatment. Journal of Endodontics. 2015;41(7):1020–1025. doi: 10.1016/j.joen.2015.02.019. [DOI] [PubMed] [Google Scholar]
- 20.Matherne R. P., Angelopoulos C., Kulild J. C., Tira D. Use of cone-beam computed tomography to identify root canal systems in vitro. Journal of Endodontics. 2008;34(1):87–89. doi: 10.1016/j.joen.2007.10.016. [DOI] [PubMed] [Google Scholar]
- 21.Domark J. D., Hatton J. F., Benison R. P., Hildebolt C. F. An ex vivo comparison of digital radiography and cone-beam and micro computed tomography in the detection of the number of canals in the mesiobuccal roots of maxillary molars. Journal of Endodontics. 2013;39(7):901–905. doi: 10.1016/j.joen.2013.01.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Paula-Silva F. W. G. D., Wu M.-K., Leonardo M. R., Bezerra da Silva L. A., Wesselink P. R. Accuracy of periapical radiography and cone-beam computed tomography scans in diagnosing apical periodontitis using histopathological findings as a gold standard. Journal of Endodontics. 2009;35(7):1009–1012. doi: 10.1016/j.joen.2009.04.006. [DOI] [PubMed] [Google Scholar]
- 23.Velvart P., Hecker H., Tillinger G. Detection of the apical lesion and the mandibular canal in conventional radiography and computed tomography. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology, and Endodontology. 2001;92(6):682–688. doi: 10.1067/moe.2001.118904. [DOI] [PubMed] [Google Scholar]
- 24.Estrela C., Bueno M. R., Leles C. R., Azevedo B., Azevedo J. R. Accuracy of cone beam computed tomography and panoramic and periapical radiography for detection of apical periodontitis. Journal of Endodontics. 2008;34(3):273–279. doi: 10.1016/j.joen.2007.11.023. [DOI] [PubMed] [Google Scholar]
- 25.Patel S., Wilson R., Dawood A., Mannocci F. The detection of periapical pathosis using periapical radiography and cone beam computed tomography—part 1: pre-operative status. International Endodontic Journal. 2012;45(8):702–710. doi: 10.1111/j.1365-2591.2011.01989.x. [DOI] [PubMed] [Google Scholar]
- 26.Martins J. N. R., Marques D., Silva L., Jo E. Prevalence studies on root canal anatomy using cone-beam computed tomographic imaging: a systematic review. Journal of Endodontics. 2019;45(4):372–386. doi: 10.1016/j.joen.2018.12.016. [DOI] [PubMed] [Google Scholar]
- 27.Gulabivala K., Opasanon A., Ng Y.-L., Alavi A. Root and canal morphology of Thai mandibular molars. International Endodontic Journal. 2002;35(1):56–62. doi: 10.1046/j.1365-2591.2002.00452.x. [DOI] [PubMed] [Google Scholar]
- 28.Mashyakhy M., Chourasia H. R., Halboub E., Almashraqi A. A., Khubrani Y., Gambarini G. Anatomical variations and bilateral symmetry of roots and root canal system of mandibular first permanent molars in Saudi Arabian population utilizing cone- beam computed tomography. Saudi Dental Journal. 2019;31(4):481–486. doi: 10.1016/j.sdentj.2019.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kruse C., Spin-Neto R., Reibel J., Wenzel A., Kirkevang L.-L. Diagnostic validity of periapical radiography and CBCT for assessing periapical lesions that persist after endodontic surgery. Dentomaxillofacial Radiology. 2017;46(7) doi: 10.1259/dmfr.20170210.20170210 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Burry J. C., Stover S., Eichmiller F., Bhagavatula P. Outcomes of primary endodontic therapy provided by endodontic specialists compared with other providers. Journal of Endodontics. 2016;42(5):702–705. doi: 10.1016/j.joen.2016.02.008. [DOI] [PubMed] [Google Scholar]
- 31.Friedman S., Abitbol S., Lawrence H. Treatment outcome in endodontics: the Toronto study. Phase 1: initial treatment. Journal of Endodontics. 2003;29(12):787–793. doi: 10.1097/00004770-200312000-00001. [DOI] [PubMed] [Google Scholar]
- 32.Ng Y.-L., Mann V., Gulabivala K. A prospective study of the factors affecting outcomes of nonsurgical root canal treatment: part 1: periapical health. International Endodontic Journal. 2011;44(7):583–609. doi: 10.1111/j.1365-2591.2011.01872.x. [DOI] [PubMed] [Google Scholar]
- 33.Lin Y.-H., Lin H.-N., Chen C.-C., Chen M.-S. Evaluation of the root and canal systems of maxillary molars in Taiwanese patients: a cone beam computed tomography study. Biomedical Journal. 2017;40(4):232–238. doi: 10.1016/j.bj.2017.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Mohara N. T., Coelho M. S., De Queiroz N. V., et al. Root anatomy and canal configuration of maxillary molars in a Brazilian subpopulation: a 125-$μ$m cone-beam computed tomographic study. European Journal of Dentistry. 2019;13(1):82–87. doi: 10.1055/s-0039-1688736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Pan J. Y. Y., Parolia A., Chuah S. R., Bhatia S., Mutalik S., Pau A. Root canal morphology of permanent teeth in a Malaysian subpopulation using cone-beam computed tomography. BMC Oral Health. 2019;19(1):p. 14. doi: 10.1186/s12903-019-0710-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Al-Shehri S., Al-Nazhan S., Shoukry S., Al-Shwaimi E., Al-Sadhan R., Al-Shemmery B. Root and canal configuration of the maxillary first molar in a Saudi subpopulation: a cone-beam computed tomography study. Saudi Endodontic Journal. 2017;7(2):69–76. doi: 10.4103/1658-5984.205128. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data supporting the findings of this study are available from the corresponding author upon reasonable request.


