Abstract
Background:
Reablement is 1 approach to conduct rehabilitation in the community (ie, home environment), which aims to enhance an individual's functional ability to perform everyday activities that individuals perceive as important. We investigated the effects of a home-reablement program on different rehabilitation outcomes in people with stroke.
Methods:
A single-blind randomized clinical trial was conducted. Twenty-six people with stroke were randomly assigned to the home-reablement group or control group. For 6 weeks, participants in the home-reablement group received training for activities of daily living (ADL) that they perceived as important but difficult to perform. Participants in the control group received conventional rehabilitation in the hospital. Outcome measures included the Fugl–Meyer Assessment for the upper-extremity (FMA-UE) and the Stroke Impact Scale 3.0 (SIS 3.0) subscales.
Results:
No statistically significant differences between the 2 groups were noticed in the FMA-UE and the SIS 3.0 subscales (P = .226–1.000). Small effect size (success rate difference = 0.12–0.25) were noticed in the FMA-UE and the 5 SIS 3.0 subscales. The home-reablement group exhibited a greater proportion of participants with scores greater than the minimal detectable change in the FMA-UE and the 6 SIS 3.0 subscales (ie, strength, ADL/instrumental ADL, mobility, emotion, memory, and participation).
Conclusions:
People with stroke that underwent the 6-week home-reablement program showed potential for improving their motor function, ADL/instrumental ADL, emotion, memory, and activity participation.
Keywords: community health services, rehabilitation, stroke, treatment outcome
1. Introduction
According to the report of the World Health Organization, cardiovascular diseases (eg, coronary heart disease and stroke) are the number 1 cause of death worldwide.[1] Of the 17.9 million deaths due to cardiovascular disease, 85% were caused by heart disease and stroke.[1] The incidence rate for the first-ever stroke in people over 36 years was 330 cases per 100,000 people per year.[2] Stroke causes motor, cognition, and emotional impairment, which leads to decrease participation in activities of daily living (ADL).[3] With regard to the loss of upper limb function, 30% to 66% of patients do not regain arm function by 6 months after stroke, and only 5% to 20% of people fully regain arm function.[4] Depression, anxiety, and apathy are common mood disruptions with an average prevalence ranging from 30% to 50% post-stroke.[5] The predictive role of inflammatory markers in stroke pathogenesis has been reported.[6,7] Quality of life (QOL) is a multidimensional concept for monitoring physical, psychological, and social aspects of life through individuals’ perceptions. QOL has been considered an important outcome measure that exhibits evidence of intervention in people with stroke.[8]
Reablement is a rehabilitation approach conducted in the community (eg, home environment), which encourages people to relearn and regain ADL skills that they perceive as important. Reablement is a goal-oriented, person-centered, and intensive (eg, 6 weeks) intervention that enhances functional performance and independent living.[9] The insufficient number of caregivers has become an important issue in the world. The World Report on Disability estimated that 1 billion people, or 15% of the world population, have experienced disability and that 2% are severely disabled.[10] To reduce the burden on caregivers and the cost of care, emphasis has been placed on functional recovery using each patients’ individual strengths to establish a treatment plan.[11,12] Home reablement can reduce the length of hospital stays for patients and reduce costs by 15% compared to conventional rehabilitation.[13] The goal of reablement is to reduce the need for caregivers.[12]
Due to the relevance of rehabilitation in a home environment and the limited evidence on the effects of reablement on people with stroke, we conducted a home-reablement program that focused on ADL training for people with stroke. We investigated the treatment effects of home-reablement on different rehabilitation outcomes in people with stroke.
2. Method
2.1. Participants
We conducted a single-blind randomized controlled pilot trial. Twenty-six community-dwelling patients were recruited from the Department of Physical Medicine and Rehabilitation at a hospital in northern Taiwan between February, 2018 and September, 2018. The inclusion criteria were (1) stroke diagnosis; (2) age >20; (3) modified Rankin Scale score of 2–4 points and can maintain a sitting position for at least half an hour in a wheelchair or bed without any assistance; (4) ability to follow instructions and cooperate with the procedures; and (5) willing to participate in this study and sign a consent form. The exclusion criteria were (1) orthopedic disorder (eg, rheumatoid arthritis); (2) progressive disease (eg, parkinsonism and dementia); and (3) peripheral nerve injury. The study protocol was registered at ClinicalTrials.gov (NCT03828851) and was approved by the Institutional Review Board of the hospital.
2.2. Procedures
Suitable outpatient participants were randomized into the home-reablement group and control group using a random number table generated from Excel. The participants were evaluated by 2 trained occupational therapists who were blinded to the participants’ allocations. The 2 occupational therapists received at least 4 hours of training to become familiar with the measures (the Canadian Occupational Performance Measure, Fugl–Meyer Assessment for the upper-extremity [FMA-UE], and the Stroke Impact Scale 3.0 [SIS 3.0]). Participants were first interviewed using the Canadian Occupational Performance Measure to identify 2 to 3 ADL goals that they perceived as important but difficult to perform. Outcome measures (the FMA-UE and Stroke SIS 3.0) were evaluated at baseline and after 6 weeks by the same blinded occupational therapists at each participants’ house. The home-reablement group received ADL training in their home once a week for 6 weeks conducted by the other occupational therapist who did not administer measures. The control group received conventional rehabilitation in a hospital setting, including 30 minutes of physical therapy and 30 minutes of occupational therapy twice a week for motor and cognitive training.
2.3. Intervention
The home-reablement group received goal-directed ADL training 50 minutes per day, 1 day a week, for 6 weeks. During the first week, the occupational therapist who administered the home program focused on the 2 to 3 ADL tasks that participants considered important but difficult to perform. The occupational therapist who did not administer the measures confirmed the extent to which participants wanted to improve and observed their ability to perform the ADL tasks. From the second to the sixth week, the occupational therapist taught the ADL tasks and provided implementation strategies, such as task analysis, task redesign, and work simplification.
2.4. Outcome measures
The FMA-UE was used to assess the motor function of the upper extremity. The FMA-UE contains 33 items that assess the movement of the shoulder, elbow, forearm, wrist, hand, and coordination.[14] Each item is rated as a 2-level (0–2) or 3-level (0–1–2) score, and the total FMA-UE score ranges from 0 to 66. A higher score represents a better upper-extremity motor function. The FMA-UE has been reported as a reliable, valid, and responsive measure for people with stroke.[15,16] The minimal detectable change (MDC) of the FMA-UE was 3.2 points.[17]
The SIS 3.0 is a disease-specific QOL measure for people with stroke.[18] It contains 59 items measured by 8 subscales: strength, hand function, ADL/instrumental ADL (IADL), mobility, communication, emotion, memory, and participation.[19] The items are rated on a 5-point Likert scale (1–5). Each subscale score is calculated and ranges from 0 to 100. A higher subscale score indicates a greater ability to perform the subscale function.[20] We calculated the MDC values of each subscale from the intraclass correlation coefficient according to a previous study of reliability that evaluated the SIS 3.0 in people with stroke.[21] The MDC values of strength, hand function, ADL/IADL, mobility, communication, emotion, memory, and participation were 15.5, 22.6, 17.1, 14.1, 24.1, 19.6, 20.9, and 32.9, respectively. The SIS 3.0 has been reported as a reliable and valid measure for people with stroke.[21,22]
2.5. Statistical analysis
This was a pilot study with a small sample. We used nonparametric statistics to analyze the data. The Mann–Whitney U test and Chi-square test were applied to compare baseline characteristics (continuous and categorical variables, respectively) between the home-reablement group and the control group. Intention-to-treat analysis (using baseline scores) was used for filling in the missing data. Change scores were computed between the 2 assessments at baseline and after 6 weeks. The Mann–Whitney U test was applied to investigate the differences in the FMA-UE and SIS 3.0 scores between the 2 groups (two-tailed, α = 0.05). We estimated the effect size for nonparametric statistics (ie, success rate difference [SRD]). The SRD criteria were: 0.11 to 0.27, small effect size; 0.28 to 0.43, moderate effect size; and >0.43, large effect size.[23] Moreover, the MDC proportion was analyzed for the FMA-UE and the 8 subscales of the SIS 3.0 in the 2 groups. The MDC proportion is the proportion of participants whose change scores in the FMA-UE and SIS 3.0 exceeded the MDC values.
Because there were no previous studies of reablement in people with stroke for us to perform a power calculation, we applied the rule of thumb of a pilot study (ie, a sample size of 12 per group) in this study.[24,25]
3. Results
The patient enrollment flow diagram is shown in Figure 1. Forty-two people with stroke were referred by 1 physician. Sixteen patients were excluded, including 13 patients who refused to participate and 3 patients who refused to receive assessments. The others (n = 26) with signed informed consent were assigned randomly to the home-reablement group (n = 12) and the control group (n = 14). Two participants in the control group dropped out. Table 1 shows the demographic and clinical characteristics of the participants in the 2 groups. There were no statistically significant differences (P < .05) between the 2 groups in age, gender, education, time since onset, stroke type, and side of the hemisphere. Seventeen participants had ischemic stroke and 3 patients had been treated with thrombolysis.
Figure 1.
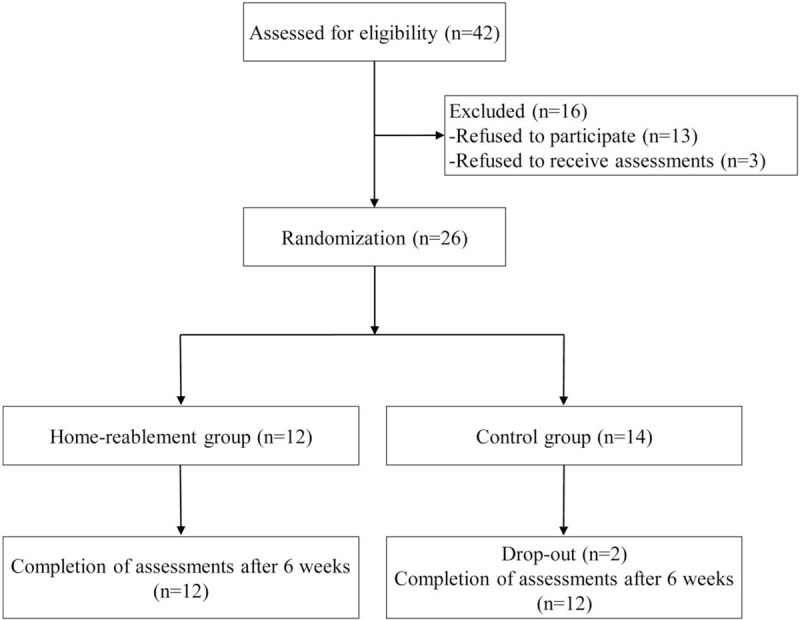
Flow diagram of the study.
Table 1.
Demographic and clinical characteristics of participants.
| Characteristic | Home-reablement (n = 12) | Control (n = 14) | P |
| Age (years), mean (SD) | 70.83 (6.51) | 65.36 (16.74) | .247 |
| Gender, n (%) | .899 | ||
| Female | 4 (33.33) | 5 (35.71) | |
| Male | 8 (66.67) | 9 (64.29) | |
| Time since onset (months), mean (SD) | 22.83 (17.70) | 53.50 (43.69) | .117 |
| Education, n (%) | .965 | ||
| ≥Elementary school | 3 (25.00) | 3 (21.43) | |
| Junior high school | 1 (8.33) | 2 (14.28) | |
| Senior high school | 3 (25.00) | 3 (21.43) | |
| ≤College | 5 (41.67) | 6 (42.86) | |
| Stroke type, n (%) | |||
| Hemorrhagic | 5 (41.67) | 4 (28.57) | .484 |
| Ischemic | 7 (58.33) | 10 (71.43) | |
| Side of the hemisphere, n (%) | |||
| Right | 4 (33.33) | 8 (57.14) | .225 |
| Left | 8 (66.67) | 6 (42.86) | |
SD = standard deviation.
No statistically significant differences were noticed in the FMA-UE and SIS 3.0 baseline scores between the home-reablement group and the control group (P = .056–.857) (Table 2). The changes in the FMA-UE and SIS 3.0 scores were not statistically significant (P = .226–1.000) between the 2 groups. Small effect sizes were observed in the FMA-UE (SRD = 0.25) and in the 5 SIS 3.0 subscales (SRD = 0.12–0.16) (Table 2). The SRD values were <0.11 in the 3 SIS 3.0 subscales (ie, communication, memory, and participation).
Table 2.
Descriptive and inferential statistics of the FMA-UE and SIS 3.0.
| Baseline | Post6 weeks–baseline | ||||||
| Outcome | Group | mean (SD) | z value (P value) | mean (SD) | z value (P value) | SRD | MDC proportion |
| FMA-UE | Home-reablement | 38.17 (26.90) | −0.953 (.340) | 2.36 (5.08) | −1.212 (.226) | 0.25 | 41.7 |
| Control | 27.29 (22.18) | – | −0.08 (4.55) | – | – | 21.4 | |
| SIS 3.0-strength | Home-reablement | 43.23 (32.25) | −0.597 (.551) | 2.84 (14.35) | −0.847 (.397) | 0.15 | 16.7 |
| Control | 35.71 (33.83) | – | 0.48 (20.96) | – | – | 21.4 | |
| SIS 3.0-hand function | Home-reablement | 53.75 (36.94) | −0.853 (.394) | −0.45 (12.34) | −0.826 (.409) | 0.16 | 0.0 |
| Control | 41.78 (32.32) | – | −6.15 (16.48) | – | – | 0.0 | |
| SIS 3.0-ADL/IADL | Home-reablement | 56.67 (28.13) | −0.463 (.643) | 3.64 (13.43) | −1.111 (.267) | 0.12 | 25.0 |
| Control | 51.25 (29.08) | – | −1.92 (9.36) | – | – | 0.0 | |
| SIS 3.0-mobility | Home-reablement | 55.56 (29.49) | −0.258 (.797) | 1.01 (12.38) | −0.613 (.540) | 0.16 | 8.3 |
| Control | 52.98 (30.42) | – | −1.50 (11.20) | – | – | 7.1 | |
| SIS 3.0-communication | Home-reablement | 82.14 (18.21) | −1.214 (.225) | 0.32 (10.77) | −0.088 (.929) | 0.08 | 0.0 |
| Control | 66.58 (28.62) | – | 5.49 (19.21) | – | – | 14.3 | |
| SIS 3.0-emotion | Home-reablement | 61.11 (21.42) | −1.554 (.120) | 2.78 (16.24) | −0.875 (.381) | 0.15 | 16.7 |
| Control | 49.60 (13.16) | – | −0.43 (10.69) | – | – | 0.0 | |
| SIS 3.0-memory | Home-reablement | 74.70 (15.86) | −0.181 (.857) | −3.25 (17.60) | −0.616 (.538) | 0.00 | 8.3 |
| Control | 68.37 (28.43) | – | 0.82 (9.47) | – | – | 0.0 | |
| SIS 3.0-participation | Home-reablement | 64.84 (23.31) | −1.907 (.056) | 3.98 (20.64) | 0.000 (1.000) | 0.00 | 8.3 |
| Control | 40.63 (29.62) | – | 4.33 (14.52) | – | – | 0.0 | |
ADL/IADL = activities of daily living/instrumental activities of daily living, FMA-UE = Fugl–Meyer Assessment for the upper-extremity, MDC proportion = proportion of minimal detectable change, SD = standard deviation, SIS3.0 = Stroke Impact Scale 3.0, SRD = success rate difference.
The results of MDC proportion are shown in Table 2. In the FMA-UE, the MDC proportions of the home-reablement and control groups were 41.7% and 21.4%, respectively. The MDC proportions of the SIS 3.0 subscales were 0.0% to 25.0% in the home-reablement group and 0.0% to 21.4% in the control group. For the hand function and communication SIS 3.0 subscales, none of the home-reablement group participants experienced score changes greater than their MDC values. Other than the hand function subscale, none of the participants experienced score changes greater than their MDC values in the communication subscale of the home-reablement group and in the 4 SIS 3.0 subscales (ie, ADL/IADL, emotion, memory, and participation) of the control group.
4. Discussion
In this study, we compared the effectiveness of a home-reablement program on upper extremity motor function and subscales of the QOL measure between the home-reablement and control groups. The home-reablement group received goal-directed ADL training, while the control group received motor and cognitive training. There were no significant mean differences between the 2 groups in motor function and stroke-specific health outcomes. However, there were individual participants of the home-reablement group who showed changes greater than the MDC values in motor function, ADL/IADL, emotion, memory, and activity participation. The proportion of participants with scores greater than the MDC values (ie, MDC proportion) demonstrates significant improvement at the individual level.[26] This pilot study provides initial evidence for the effectiveness of a home-reablement program in people with stroke.
Regarding the motor functions measured by the FMA-UE, a small effect size between the 2 groups was found and the MDC proportion of the home-reablement group was greater than that of the control group. That is, more participants in the home-reablement program showed greater improvement in overall motor function of the upper extremity than those in the control group. In the home-reablement group, participants performed ADL tasks that they perceived as important but difficult to perform, such as dressing, feeding, toileting, and transferring. These abovementioned ADL tasks are correlated with motor functions of the upper extremity.[27–30] Thus, participants of the home reablement group executed ADL tasks in their home environment, which may enhance their overall upper extremity motor function. For the motor functions in the SIS 3.0 subscales (ie, hand function, mobility, and strength), no participants showed a score change higher than the MDC value of the hand function subscale in the 2 groups (MDC proportion = 0). One possible reason is that the items of the hand function subscale (eg, turn a doorknob and tie a shoelace) were not administered in the ADL training. Although participants did not perceive a significant improvement in hand function, the home-reablement group showed lower degeneration in hand function according to the mean difference in pre- and post-scores. The mobility subscale of the SIS 3.0 demonstrated a slightly higher MDC proportion in the home-reablement group than that in the control group, positive mean difference in pre and post-scores, and small effect size between the 2 groups. In the strength subscale of the SIS 3.0, the MDC proportion of the control group was slightly higher than that of the home-reablement group. However, the strength subscale in the home-reablement group showed a higher mean difference between pre- and post-scores than the control group and a small effect size between the 2 groups. According to our findings on motor function in the SIS 3.0, home-based reablement may have the potential to reduce degeneration in hand function and increase mobility and muscle strength for people with stroke. The home-based reablement program in this study was conducted once a week for 6 weeks. Future studies could increase the frequency (eg, twice a week) and lengthen the study period (eg, 12 weeks) to examine the efficacy of the home-reablement program for people with stroke.
The ADL/IADL subscale of the SIS 3.0 showed a higher MDC proportion in the home-reablement group, compared to the other subscales. Moreover, the MDC proportion of the ADL/IADL subscale in the control group was zero. Reablement in the home environment can encourage context-dependent learning and this study used ADL as a means of treatment.[31] Participants who practiced in a familiar environment could apply their skills to real-world activities.[32] Therefore, the home-reablement program could have contributed to the greater improvement and generalization of performing ADL tasks in daily life.
In the 3 SIS 3.0 subscales (emotion, memory, and participation), the MDC proportions of the home-reablement group were greater than those of the control group. However, the MDC proportion of the communication subscale in the control group was greater than that of the home-reablement group. One possible reason is that the home-reablement program pairs 1 therapist to 1 participant. The mode of 1 therapist to 1 participant may provide more emotional support and individualized strategies for remembering and solving problems in daily life, which in turn, enhances their activity participation at home.[33,34] Relatively, the mode of 1 to 1 may decrease the chance to communicate with others in a group. Therefore, except for individualized intervention, healthcare professionals who conduct reablement programs may consider designing some group training sessions in the community.
Three limitations should be noticed in this study. First, the sample size was small, the participants were recruited from only 1 hospital in northern Taiwan, and the distribution of stroke subtypes was not provided, restricting the generalizability of the results. Future studies with larger sample sizes and information on stroke subtypes are warranted to validate our findings. Second, this study did not measure the motor function of the lower extremity. About 91.6% of the participants (ie, 11 participants) in the home-reablement group received ambulation training in this study. It is necessary to measure the motor function of the lower extremity in the home-reablement program because a high percentage of participants considered walking as an important ADL. Third, inflammatory markers were not measured in this study. A home-based program has been shown to reduce inflammatory markers.[35] Inflammatory markers have displayed a predictive role toward the prognosis of cardiovascular events.[36]
5. Conclusions
The 6-week home-reablement program showed no statistically significant effects on patients’ rehabilitation outcomes. We noticed that people with stroke had the potential to enhance their motor function, ADL/IADL, emotion, memory, and activity participation after undergoing a home-reablement program. Future reablement studies with larger sample sizes are needed.
Author contributions
Conceptualization: En-Chi Chiu.
Formal analysis: Fang-Chi Chi, En-Chi Chiu.
Investigation: Pei-Tsen Chen, En-Chi Chiu.
Resources: Pei-Tsen Chen.
Writing – original draft: Fang-Chi Chi, En-Chi Chiu.
Writing – review & editing: Pei-Tsen Chen, En-Chi Chiu.
Footnotes
Abbreviations: ADL = activities of daily living, FMA-UE = Fugl–Meyer Assessment for the upper-extremity, IADL = instrumental activities of daily living, MDC = minimal detectable change, QOL = quality of life, SIS 3.0 = Stroke Impact Scale 3.0, SRD = success rate difference.
How to cite this article: Chiu EC, Chi FC, Chen PT. Investigation of the home-reablement program on rehabilitation outcomes for people with stroke: A pilot study. Medicine. 2021;100:26(e26515).
This study was financially supported by Cardinal Tien Hospital (grant no. CTH107B-2N04) and the Ministry of Science and Technology, Taiwan (grant no. MOST 107-2314-B-227-008-MY3).
The authors have no conflicts of interest to disclose.
The datasets generated during and/or analyzed during the present study are available from the corresponding author on reasonable request.
References
- [1].World Health Organization. Cardiovascular diseases (CVDs). https://www.who.int/news-room/fact-sheets/detail/cardiovascular-diseases-(cvds). Published 2017. Accessed February 16, 2021. [Google Scholar]
- [2].Hu HH, Sheng WY, Chu FL, Lang CH, Chiang BN. Incidence of stroke in Taiwan. Stroke 1992;23:1237–41. [DOI] [PubMed] [Google Scholar]
- [3].Arbesman M, Lieberman D, Berlanstein DR. Method for the evidence-based reviews on occupational therapy and stroke. Am J Occup Ther 2015;69:69011800201–5. [DOI] [PubMed] [Google Scholar]
- [4].French B, Thomas LH, Coupe J, et al. Repetitive task training for improving functional ability after stroke. Cochrane Database Syst Rev 2016;11:Cd006073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Babulal GM, Huskey TN, Roe CM, Goette SA, Connor LT. Cognitive impairments and mood disruptions negatively impact instrumental activities of daily living performance in the first three months after a first stroke. Top Stroke Rehabil 2015;22:144–51. [DOI] [PubMed] [Google Scholar]
- [6].Tuttolomondo A, Pecoraro R, Casuccio A, et al. Peripheral frequency of CD4+ CD28− cells in acute ischemic stroke: relationship with stroke subtype and severity markers. Medicine 2015;94:e813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Tuttolomondo A, Di Raimondo D, Pecoraro R, et al. HLA and killer cell immunoglobulin-like receptor (KIRs) genotyping in patients with acute ischemic stroke. J Neuroinflammation 2019;16:88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Gray LJ, Sprigg N, Bath PM, et al. Sex differences in quality of life in stroke survivors: data from the Tinzaparin in Acute Ischaemic Stroke Trial (TAIST). Stroke 2007;38:2960–4. [DOI] [PubMed] [Google Scholar]
- [9].Tuntland H, Kjeken I, Langeland E, et al. Predictors of outcomes following reablement in community-dwelling older adults. Clin Interv Aging 2017;12:55–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Kostanjsek N, Good A, Madden RH, et al. Counting disability: global and national estimation. Disabil Rehabil 2013;35:1065–9. [DOI] [PubMed] [Google Scholar]
- [11].Metzelthin SF, Rooijackers TH, Zijlstra GAR, et al. Effects, costs and feasibility of the 'Stay Active at Home’ Reablement training programme for home care professionals: study protocol of a cluster randomised controlled trial. BMC Geriatr 2018;18:276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Sims-Gould J, Tong CE, Wallis-Mayer L, Ashe MC. Reablement, reactivation, rehabilitation and restorative interventions with older adults in receipt of home care: a systematic review. J Am Med Dir Assoc 2017;18:653–63. [DOI] [PubMed] [Google Scholar]
- [13].Allen L, Richardson M, McIntyre A, et al. Community stroke rehabilitation teams: providing home-based stroke rehabilitation in Ontario, Canada. Can J Neurol Sci 2014;41:697–703. [DOI] [PubMed] [Google Scholar]
- [14].Fugl-Meyer AR, Jääskö L, Leyman I, Olsson S, Steglind S. The post-stroke hemiplegic patient. 1. A method for evaluation of physical performance. Scand J Rehabil Med 1975;7:13–31. [PubMed] [Google Scholar]
- [15].Hsieh YW, Wu CY, Lin KC, Chang YF, Chen CL, Liu JS. Responsiveness and validity of three outcome measures of motor function after stroke rehabilitation. Stroke 2009;40:1386–91. [DOI] [PubMed] [Google Scholar]
- [16].Platz T, Pinkowski C, van Wijck F, Kim IH, di Bella P, Johnson G. Reliability and validity of arm function assessment with standardized guidelines for the Fugl–Meyer Test, Action Research Arm Test and Box and Block Test: a multicentre study. Clin Rehabil 2005;19:404–11. [DOI] [PubMed] [Google Scholar]
- [17].See J, Dodakian L, Chou C, et al. A standardized approach to the Fugl–Meyer assessment and its implications for clinical trials. Neurorehabil Neural Repair 2013;27:732–41. [DOI] [PubMed] [Google Scholar]
- [18].Duncan PW, Wallace D, Lai SM, Johnson D, Embretson S, Laster LJ. The stroke impact scale version 2.0. Evaluation of reliability, validity, and sensitivity to change. Stroke 1999;30:2131–40. [DOI] [PubMed] [Google Scholar]
- [19].Duncan PW, Bode RK, Min Lai S, Perera S. Rasch analysis of a new stroke-specific outcome scale: the Stroke Impact Scale. Arch Phys Med Rehabil 2003;84:950–63. [DOI] [PubMed] [Google Scholar]
- [20].Mulder M, Nijland R. Stroke Impact Scale. J Physiother 2016;62:117. [DOI] [PubMed] [Google Scholar]
- [21].Ochi M, Ohashi H, Hachisuka K, Saeki S. The reliability and validity of the Japanese version of the Stroke Impact Scale version 3.0. J UOEH 2017;39:215–21. [DOI] [PubMed] [Google Scholar]
- [22].Vellone E, Savini S, Fida R, et al. Psychometric evaluation of the Stroke Impact Scale 3.0. J Cardiovasc Nurs 2015;30:229–41. [DOI] [PubMed] [Google Scholar]
- [23].Aspinal F, Glasby J, Rostgaard T, Tuntland H, Westendorp RG. New horizons: reablement – supporting older people towards independence. Age Ageing 2016;45:572–6. [DOI] [PubMed] [Google Scholar]
- [24].Julious SA. Sample size of 12 per group rule of thumb for a pilot study. Pharm Stat 2005;4:287–91. [Google Scholar]
- [25].van Belle G. Statistical Rules of Thumb. New York: John Wiley; 2002. [Google Scholar]
- [26].Chiu EC, Lee SC, Lai KY, Gu FY. Test-retest reliability and minimal detectable change of the Comprehensive Occupational Therapy Evaluation Scale (COTES) in people with schizophrenia. Am J Occup Ther 2020;74:74052051101–7. [DOI] [PubMed] [Google Scholar]
- [27].Fujita T, Sato A, Yamamoto Y, et al. Relationship between dressing and motor function in stroke patients: a study with partial correlation analysis. J Phys Ther Sci 2015;27:3771–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Schaefer SY, Patterson CB, Lang CE. Transfer of training between distinct motor tasks after stroke: implications for task-specific approaches to upper-extremity neurorehabilitation. Neurorehabil Neural Repair 2013;27:602–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Kawanabe E, Suzuki M, Tanaka S, Sasaki S, Hamaguchi T. Impairment in toileting behavior after a stroke. Geriatr Gerontol Int 2018. 18. [DOI] [PubMed] [Google Scholar]
- [30].Iosa M, Morone G, Ragaglini MR, Fusco A, Paolucci S. Motor strategies and bilateral transfer in sensorimotor learning of patients with subacute stroke and healthy subjects. A randomized controlled trial. Eur J Phys Rehabil Med 2013;49:291–9. [PubMed] [Google Scholar]
- [31].Mjøsund HL, Moe CF, Burton E, Uhrenfeldt L. Integration of physical activity in reablement for community dwelling older adults: a systematic scoping review. J Multidiscip Healthc 2020;13:1291–315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Dobkin BH. A rehabilitation-internet-of-things in the home to augment motor skills and exercise training. Neurorehabil Neural Repair 2017;31:217–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Bennett B, Barnston S, Smith R. Emotional support after stroke, part 1: two models from hospital practice. Br J Neurosci Nurs 2007;3:19–23. [Google Scholar]
- [34].McEwen S, Polatajko H, Baum C, et al. Combined cognitive-strategy and task-specific training improve transfer to untrained activities in subacute stroke: an exploratory randomized controlled trial. Neurorehabil Neural Repair 2015;29:526–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [35].Di Raimondo D, Tuttolomondo A, Buttà C, et al. Metabolic and anti-inflammatory effects of a home-based programme of aerobic physical exercise. Int J Clin Pract 2013;67:1247–53. [DOI] [PubMed] [Google Scholar]
- [36].Della Corte V, Tuttolomondo A, Pecoraro R, Di Raimondo D, Vassallo V, Pinto A. Inflammation, endothelial dysfunction and arterial stiffness as therapeutic targets in cardiovascular medicine. Curr Pharm Des 2016;22:4658–68. [DOI] [PubMed] [Google Scholar]


