PURPOSE:
African American patients with cancer underutilize advance care planning (ACP) and palliative care (PC). This feasibility study investigated whether community health workers (CHWs) could improve ACP and PC utilization for African American patients with advanced cancer.
METHODS:
African American patients diagnosed with an advanced solid organ cancer (stage IV or stage III disease with a palliative performance score < 60%) were enrolled. Patients completed baseline surveys that assessed symptom burden and distress at baseline and 3 months post-CHW intervention. The CHW intervention consisted of a comprehensive assessment of multiple PC domains and social determinants of health. CHWs provided tailored support and education on the basis of iterative assessment of patient needs. Intervention feasibility was determined by patient and caregiver retention rate above 50% at 3 months.
RESULTS:
Over a 12-month period, 24 patients were screened, of which 21 were deemed eligible. Twelve patients participated in the study. Patient retention was high at 3 months (75%) and 6 months (66%). Following the CHW intervention, symptom assessment as measured by Edmonton Symptom Assessment System improved from 33.8 at baseline to 18.8 (P = .03). Psychological distress improved from 5.5 to 4.7 (P = .36), and depressive symptoms from 42.2 to 33.6 (P = .09), although this was not significant. ACP documentation improved from 25% at baseline to 75% at study completion. Sixty-seven percentage of patients were referred to PC, with 100% of three decedents using hospice.
CONCLUSION:
Utilization of CHWs to address PC domains and social determinants of health is feasible. Although study enrollment was identified as a potential barrier, most recruited patients were retained on study.
INTRODUCTION
Although treatment for cancer has improved and death has decreased,1 disparities in outcome remain for minority patients.2 The delivery of high-quality end-of-life (EOL) care remains challenging for African American patients with cancer.3 Compared with Caucasians, African American patients are less likely to share care preferences or complete advance directives, have a living will, or have a do-not-resuscitate order.4-6 They are more likely to choose aggressive care for incurable illness and less frequently access hospice services.7 Institutional, individual, and cultural barriers partially explain these disparities in EOL care quality.8-10 Although palliative care (PC) is endorsed by multiple medical societies11,12 and has potential to bridge disparities in EOL outcomes,13,14 uptake is limited in oncology practice.15
Multiple rigorously studied interventions have reduced disparities in cancer care.16-19 Community health workers (CHWs) represent one strategy to improve care quality within fragmented health systems.20,21 CHWs are trusted individuals from local communities,22 who undergo training to support advocacy, community building and outreach, cultural competency, care coordination, and system navigation to promote health behavior change. Several studies demonstrate effectiveness in chronic disease control,23 mental health,24 care quality,25 and health utilization.26 CHWs have worked with at-risk populations,27,28 with some interventions targeting PC domains.17,19,29 Yet, the challenges of conducting PC trials are well-documented, with difficulties in participant recruitment, high rates of patient attrition, and missing data because of progressive disease and death.30
Despite the evidence that advance care planning (ACP) improves EOL outcomes,31-33 clinicians have limited time29 and are often averse to difficult conversations.34 Although PC teams assist in these discussions, there remains a workforce shortage and providers are difficult to access outside the hospital setting.35 Therefore, novel strategies are needed to ensure appropriate communication with seriously ill patients and families, particularly for communities historically disenfranchised by health systems.36,37 In this feasibility study, we sought to establish the use of a CHW intervention to increase utilization of PC by African American patients with advanced cancer by removing barriers to assessment and management of PC domains.38 Herein, we focus on infrastructure development, training of a CHW, study retention, and barriers to implementation.
METHODS
The aim of this pilot study was to investigate the feasibility of a CHW intervention to improve PC utilization by African American patients with advanced cancer. All aspects of the intervention content were determined and reviewed through engagements with stakeholders along the PC continuum via our previous work.39 Implementation science frameworks (Consolidated Framework for Implementation Research and Reach, Effectiveness, Adoption, Implementation, and Maintenance) were used from study inception to identify crucial components of the intervention to ensure sustainability.40 Five stakeholder focus groups, composed of 13-15 participants, informed and refined the intervention prior to piloting. As per the seven P’s taxonomy, stakeholder engagement included providers (oncologists, CHWs, and PC clinicians), patients and their caregivers, purchasers or hospital administrators, policy makers, and principal investigators (quality, implementation, and PC researchers).41 The remaining two Ps of the taxonomy (payers and product makers) were not included given the scope of the question.
Participants were engaged across longitudinal stakeholder engagement sessions. A semistructured guide was prepared by the study team. The guide focused on identifying the behaviors that most consistently affect PC use and the viability of CHWs as a mechanism to address these behaviors. This included barriers and facilitators informed by Consolidated Framework for Implementation Research and Reach, Effectiveness, Adoption, Implementation, and Maintenance and culminated with stakeholder input regarding the developed implementation interventions. The intervention was deemed feasible if the study retention rate was > 50% at 3 months. Study retention was chosen as the metric given known attrition rates of 50% and higher within PC trials and the multilevel barriers to PC utilization for African American patients.42-44 Clinicians and the CHW met monthly to share program success and challenges and used peer-to-peer communication to maximize program uptake.
CHW Selection, Navigator Framework, and Training
Invitations were sent to recruit a CHW from the local community. We required a bachelor’s degree or at least three years of experience as a CHW, but maintained that the CHW was not a licensed provider, such as a nurse or social worker. The recommended characteristics included being empathetic, communicative, and comfortable with discussions on spirituality, and given our intervention, of African American race. Following selection, the CHW received 2 weeks of skills training and focused on patient and caregiver empowerment, value assessments, and symptom management. Our goal for the navigator was to serve as a link for patients and caregivers to oncologists and PC providers. In this role, CHWs would provide psychosocial support and general care information and facilitate ACP, symptom management, and PC uptake. These objectives provided the foundation of navigator training with a focus on helping patients achieve optimal health, rather than emphasizing treatment.
The navigator training curriculum was developed and delivered by a multidisciplinary team that included expert faculty (from oncology, PC, nursing, social work, and chaplain services), with independent NIH funding in health disparities, PC, and patient communication, and experience working with PC teams and/or African American religious institutions. We used multiple training modalities, for 9 hours per day. These included self-paced modules, in-person workshops, and rotations on the PC service and outpatient hospice. The CHW received feedback on communication skills, from both experienced nurse practitioners and the director of palliative medicine (T.J.S.). Core training components included the following:
Navigation basics: focused on health promotion, empowerment, and navigation principles. This included communication skills, distress screening, and problem solving to overcome barriers to PC utilization, experiences of the patient with cancer, and compassion fatigue.
Advanced navigation: Topics included reasons for emergency room visits, cultural, physical, psychological, and spiritual aspects of care, caregiver interactions, motivational interviewing, and social determinants of health.
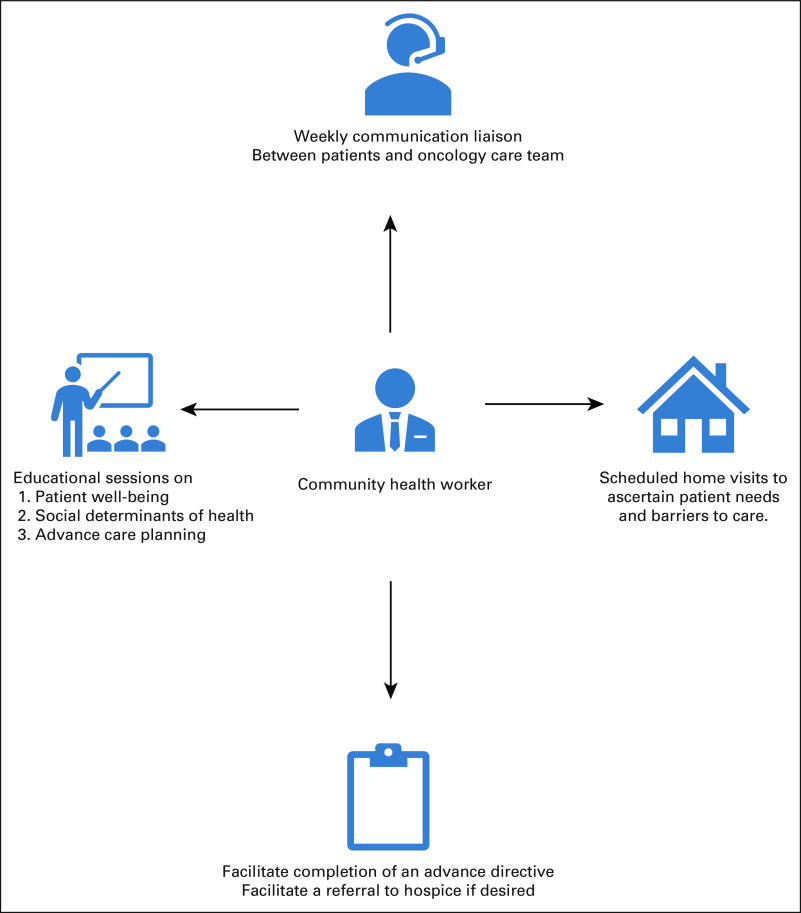
Advance care planning: CHWs were trained to facilitate ACP conversations with patients and caregivers. Content included choosing a healthcare proxy, documenting care preferences, and implications uploading documents into the electronic health record (Fig 1).
FIG 1.
The components of the community health worker interventions.
Target Population and Triage Mechanisms
Patients were recruited during scheduled clinic visits at an National Cancer Institute-designated comprehensive cancer center. Inclusion criteria included (1) self-identifying as African American, (2) diagnosed with an advanced solid organ cancer (stage IV or stage III disease with the palliative performance score < 60%), and (3) age 18 or older. Patients were assessed for enrollment regardless of timing of diagnosis or disease progression, given high levels of distress, psychosocial needs, and symptoms appropriate for supportive care.45,46 These criteria also align with recommendations by ASCO.11 Our exclusion criteria included pregnant women and patients with substance use disorder.
Patient Navigation
Following screening, eligible patients were enrolled and encouraged to select a caregiver who would be consented for the study, working together as dyad. However, patients without a designated caregiver were also enrolled. Following enrollment, research assistants met with patients to complete these surveys at baseline and 3 months: National Cancer Comprehensive Network Physical and Psychological Distress (Distress Thermometer), Center for Epidemiological Studies-Depression (CES-D), Edmonton Symptom Assessment System Revised Version (ESAS-r), and Functional Assessment of Chronic Illness Therapy—Palliative Care (FACIT-Pal).47-50
The Psychological Distress Scale is a single item asking patients to rate their distress on a scale of 0 = none to 10 = extreme distress.47 A mark of five or above indicates a need for intervention. The CES-D assesses the number, types, and duration of depressive symptoms through 20 items, on a 4-point Likert scale ranging from 0 to 3. Scores range from 0 to 60 with higher scores indicating more depressive symptoms. ESAS-r consists of ten 0-10 self-report scales that evaluate a combination of psychological and physical symptoms, in addition to a global sense of well-being, with higher scores indicating more severe symptoms. The FACIT-Pal is a 46-item measure of self-reported health–related quality of life. Scores range from 0 to 184, with higher scores indicating better quality of life.
One week following enrollment, the CHW coordinated an initial visit with the patient at their home or a clinical location. A semistructured interview guide was followed in the first two sessions, on the basis of previous stakeholder engagement, to learn patient stories and understand individual needs.38 These conversations allowed for tailored, patient-driven action plans. Patient educational sessions had content organized in three domains: patient well-being, social determinants of health, and ACP. Participants were contacted by phone weekly. Caregivers were strongly encouraged to participate in the educational sessions, but this was not required. Each patient was offered five CHW visits over the study period with each visit recorded and transcribed for qualitative assessment. CHWs communicated with the oncology team to discuss any perceived patient issues, which may necessitate PC referral. Similarly, the oncology and PC teams communicated with the CHW any patient-related concerns. The CHW office was co-located with the PC team to allow regular communication and emotional support.
Navigation Tools and Outcome Measures
The CHW used distress screening to identify unmet biopsychosocial needs to streamline navigation services.51 Outcome measures included (1) attitudes and preferences toward CHW discussions for PC assessed by transcribed recordings, (2) number of advance directives completed and present in the medical record, (3) number of patients aware of hospice and referred, (4) distress thermometer, (5) FACIT-Pal, (6) ESAS-r, and (7) CES-D. Process measures included the number of sessions missed, reasons for nonadherence, duration of each session, referrals to PC, and healthcare utilization (number of hospitalizations and visits to the emergency department).
Data were entered into a database and audited for accuracy. Descriptive statistics were computed, and distributions were examined for normality. Nonparametric analysis was used, as is appropriate for sample sizes of 20 or fewer subjects. The study used the Giorgi method for qualitative data analysis,52 to develop descriptions related to human experiences—in this case, patient navigation with a CHW. The first author (R.S.) drafted the initial coding scheme and revised it following the initial two transcripts, incorporating research team feedback. Each meaning unit was identified and coded using NVivo52; units were organized into groups as themes emerged, and the analysis was refined in this iterative process. Two independent coders (R.S. and R.N.) analyzed 20% of all transcripts independently, and differences were reconciled by consensus. Kappa coefficients were generated to evaluate coding precision, and the final kappa (> 0.85) indicated a high level of agreement. The Johns Hopkins Medical Institutional Review Board approved this study.
RESULTS
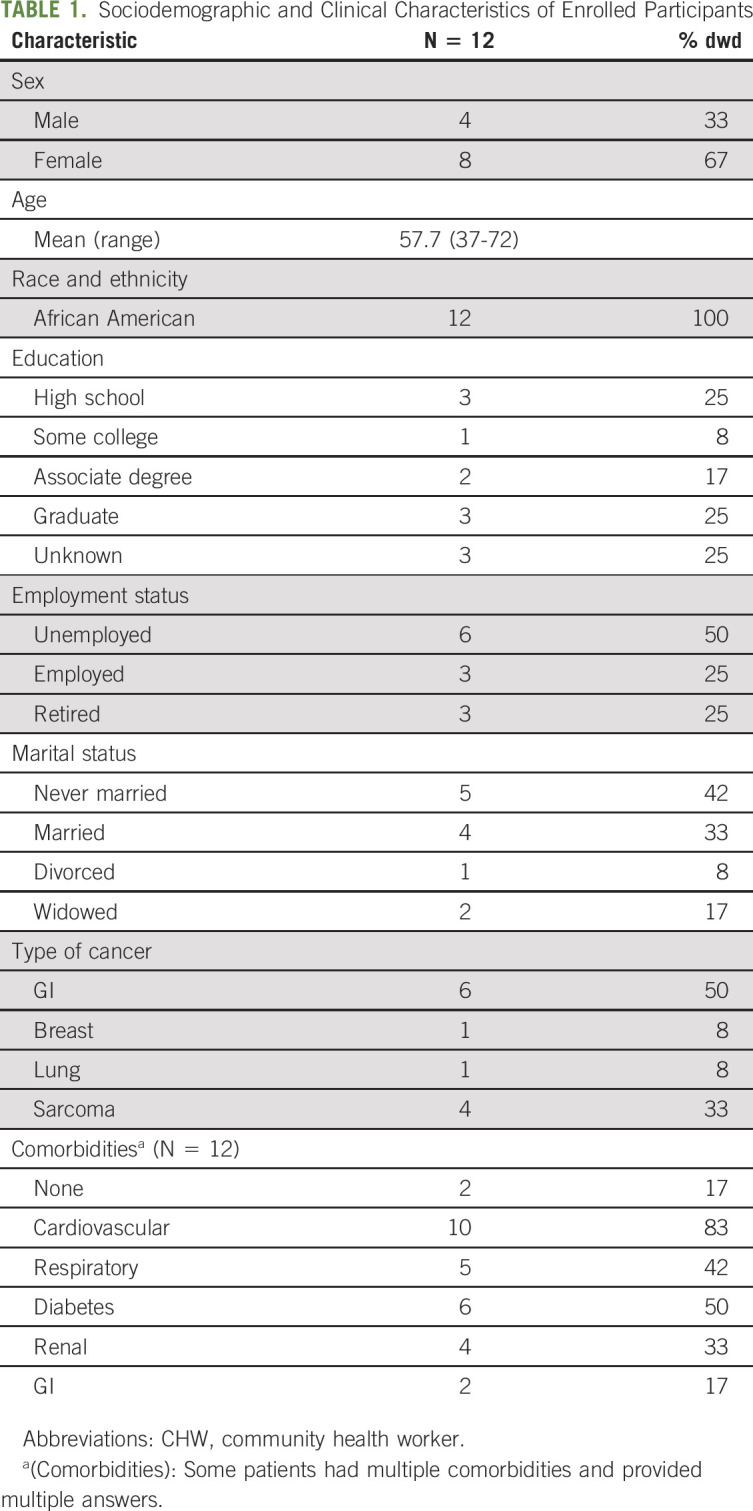
From August 1, 2018, to August 1, 2019, patients were screened, approached, and enrolled. Twenty-four consecutive patients were assessed for eligibility with nine patients ineligible for either stage of disease or performance status. Thus, 15 patients were eligible and consented. Three patients were lost to follow-up after signing consent, leaving 12 patients to undergo the full intervention. Participants had a mean age of 58 years (range, 37-72), and most patients were female (67%). The majority were unemployed (53%); only 25% graduated from college, and 33% were married. Cancer diagnosis included GI (50%), sarcoma (33%), and lung (8%) and breast cancers (8%). Most patients (85%) had at least 1 comorbidity (Table 1). The majority of patients (75%) were on active therapy.
TABLE 1.
Sociodemographic and Clinical Characteristics of Enrolled Participants
On average, the CHW spent 40 minutes per session with each patient and was able to complete at least four sessions with 67% of participants. The majority of patients were never hospitalized (75%), and multiple (> 1) visits to the emergency room were infrequent (25%). At baseline, only 25% of patients had completed an advance directive. This increased to 75% by the end of the study. All advance directives were documented in the chart, with the exception of 1 participant. The majority of patients (67%) were referred to PC. The patient retention rate was high at 3 months (9 of 12 or 75%). Three patient deaths were noted before the 6-month follow-up, and all died with hospice. One additional patient was lost to follow-up at 5 months, and therefore, retention remained high at 6 months (8 of 12 or 66%).
Recorded transcripts detailed patient and caregiver reception toward CHW discussions regarding PC. Patients and caregivers reported a sense of comfort discussing EOL care informally outside of the physician’s office. Several patients felt it was important to receive guidance from their pastor, and two expressed frustration sharing bad news with family members. In three cases where ACP was deflected, the CHW reminded families of available resources, such as social work, nursing, and chaplains. Below are some examples:
In one instance, the CHW focused on the importance of ACP and how it can prevent an unwanted outcome, such as dying in the hospital alone and without family. This was in response to a patient comment that his aunt should have never died alone.
For at least two patients, the CHW discussed legacy building and identified religion as important when considering EOL choices. The CHW facilitated conversation with their pastor for support and followed up in future meetings.
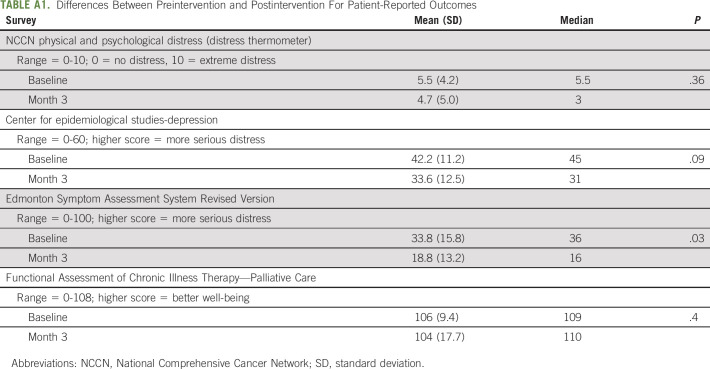
Patient-reported outcomes are outlined in Appendix Table A1, online only. At baseline, patient distress, as measured by the National Comprehensive Cancer Network distress Thermometer, was 5.5 (5 is threshold for intervention). At 3-month follow-up, mean distress numerically improved to 4.7 (P = .36), as did depressive symptoms, 42.2 at baseline to 33.6 at follow-up (P = .09), although not significantly. Symptoms, as measured by the ESAS-r, significantly improved from 33.8 at baseline to 18.8 at follow-up (P = .03). Physical function remained stable as measured by FACIT-Pal (P = .4) (Data Supplement, online only).
Feasibility challenges are presented in Table 2. Only 15 patients were accrued over 12 months, which was largely driven by research staff turnover. Although 67% of patients were ultimately seen by PC, visits were not concurrent with oncology appointments. The CHW reported initial discomfort navigating PC domains, which improved over time: “It felt different because I understood more than before and became more at ease.” Communication challenges between patients and the CHW were embedded in prior family experiences, reflecting fear of loss, dying alone, and a painful death. Still, patients felt that communication with the CHW was meaningful: “You've been a tremendous help in peaceful talking and getting around. Like, the challenge is not there as much as I think it would have been had you not been put in place.”
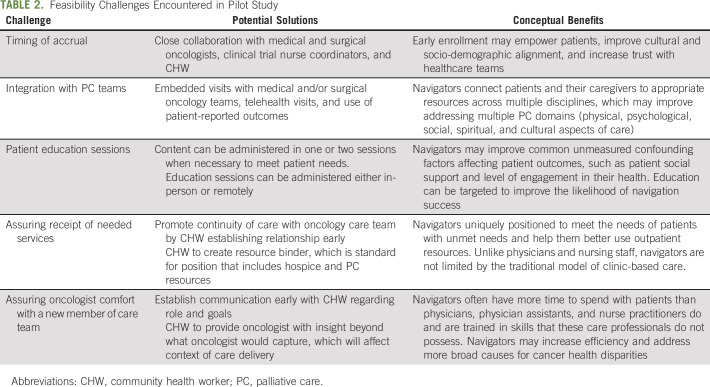
TABLE 2.
Feasibility Challenges Encountered in Pilot Study
DISCUSSION
To our knowledge, this is the first study to evaluate the feasibility of a CHW to improve PC utilization and promote ACP for African American patients with cancer. We found this intervention feasible with a high retention rate (75% at 3 months and 66% at 6 months). Additionally, there was a potential benefit for some patients, as evidenced by the PC referral rate, number of completed advance directives, and universal utilization of hospice by decedents. Importantly, this study addresses two major gaps that allow failure of PC to propagate, namely, (1) evaluation of implementation and dissemination in study planning and (2) addressing the needs of underrepresented minorities.
Although we were successful in accruing and retaining patients, several feasibility challenges were noted (Table 2). Patients and caregivers were reluctant to schedule five visits with the CHW and expressed frustration arranging additional visits with PC teams. Closer collaboration is needed to minimize the burden of additional visits. Educational session content can be combined into fewer sessions to meet patient preferences. Patient outreach was challenging; in one case, the CHW called eight times before scheduling the initial patient visit. Oncologists were less experienced using palliative performance scale, as opposed to Eastern Cooperative Oncology Group, which created challenges in recruitment. Despite these limitations, flexibility with the mode of patient education session delivery, as deemed appropriate by the patient and caregiver dyads and the CHW, limited inconveniences.
Although health systems employ various personnel on healthcare teams, few share common background with minority patients. In our pilot study, only 25% of patients had graduated college and 50% were unemployed. Social network theory53 supports the notion that CHWs contribute meaningfully to healthcare teams by establishing trust, support, and practical guidance through shared experiences.54 In this study, the CHW engaged with patients traditionally marginalized from the healthcare system.36,37 More than 60% of patients met with the CHW more than four times, and advance directive completion and PC referral were above historical standards at our cancer center.55
With tactical training and support, the CHW provided components of PC that do not require a clinician, such as introducing ACP, sharing resources for hospice, and providing psychosocial support (Table 2). These processes are important for African American patients who report distrust with healthcare systems.56,57 The patient retention could perhaps be attributed to the CHW’s ability to discuss sensitive content in a way more easily understood by patients and caregivers. In addition, the CHW spent an average of 40 minutes per session with patents, suggesting that the CHW had more time to engage issues and provisions of care not addressed in a routine clinic visit.
Our feasibility pilot study differs in important ways from ongoing developments addressing disparities in EOL care. Technology-based approaches are popular,58,59 but not pragmatic for patients who lack access or are uncomfortable with their use. A burgeoning implementation science literature and several randomized clinical trials support integration of CHWs or lay health workers to improve PC delivery in high-risk communities.17,19,25,39 Although these studies are promising, none focus on the African American community. Other interventions, such as culturally competent hospice educational materials,60 videos to improve health literacy,61 and integration of peer support,62 fail to address the multilevel issues, which drive healthcare disparities, unlike the present work.
This pilot study has several limitations. First, it was limited to a single center and single CHW with a predominately older population of African American descent, potentially limiting the generalizability to members of other racial minority groups and younger patients. External validity is limited as participants who enroll may differ from those who decline. Recruitment in an outpatient oncology clinic was successful, albeit slow to accrue given a high turnover of study coordinators (three research coordinators over 12 months for reasons unrelated to the study). Several strengths make this pilot study well-suited for practical use by health systems (Table 2). Our study was standardized in its approach to hiring, training, supervision, and workflow, while maintaining flexibility as deemed fit by the CHW. In addition, this study was conducted at the patient level and the 2-week communication skills curriculum resulted in an action plan that was carried out by the CHW.
In conclusion, this pilot study demonstrated feasibility and highlighted key areas for improving PC utilization and ACP discussions for African American patients with cancer. A larger multisite randomized trial is planned. The ultimate goal of health disparities research is to reduce or eliminate them by implementing models that consider the needs and preferences across various racial and ethnic groups. The efforts from this work continue to promote care equity for African Americans with advanced cancer.
Appendix
TABLE A1.
Differences Between Preintervention and Postintervention For Patient-Reported Outcomes
SUPPORT
Supported by Agency for Healthcare Research and Quality, 1K08HS024736. R.S. is supported by the National Institute on Aging, T32AG000247. K.F. is supported by American Cancer Society, CRP-17-112-06-COUN.
AUTHOR CONTRIBUTIONS
Conception and design: Ramy Sedhom, Karen M. Freund, Thomas J. Smith, Lisa Cooper, Fabian M. Johnston
Administrative support: Thomas J. Smith
Collection and assembly of data: Ramy Sedhom, Thomas J. Smith, Lisa Cooper, Fabian M. Johnston
Data analysis and interpretation: Ramy Sedhom, Richard Nudotor, Thomas J. Smith, Lisa Cooper, Jill T. Owczarzak, Fabian M. Johnston
Manuscript writing: Ramy Sedhom, Richard Nudotor, Karen M. Freund, Thomas J. Smith, Lisa Cooper, Jill T. Owczarzak, Fabian M. Johnston
Final approval of manuscript: Ramy Sedhom, Richard Nudotor, Karen M. Freund, Thomas J. Smith, Lisa Cooper, Jill T. Owczarzak, Fabian M. Johnston
Accountable for all aspects of the work: All authors
AUTHORS' DISCLOSURES OF POTENTIAL CONFLICTS OF INTEREST
Can Community Health Workers Increase Palliative Care Use for African American Patients? A Pilot Study
The following represents disclosure information provided by authors of this manuscript. All relationships are considered compensated unless otherwise noted. Relationships are self-held unless noted. I = Immediate Family Member, Inst = My Institution. Relationships may not relate to the subject matter of this manuscript. For more information about ASCO's conflict of interest policy, please refer to www.asco.org/rwc or ascopubs.org/op/authors/author-center.
Open Payments is a public database containing information reported by companies about payments made to US-licensed physicians (Open Payments).
Thomas J. Smith
Employment: UpToDate
Honoraria: Athenex, Association of Community Cancer Centers (ACCC)
Patents, Royalties, Other Intellectual Property: Royalties from Oxford Textbook of Cancer Communication, co-editor.
No other potential conflicts of interest were reported.
REFERENCES
- 1.Cancer Facts & Figures 2019. American Cancer Society, Atlanta, Ga, January 8, 2019. https://www.cancer.org/latest-news/facts-and-figures-2019.html
- 2.DeSantis CE, Miller KD, Goding Sauer A, et al. : Cancer statistics for African Americans, 2019. CA Cancer J Clin 69:211-233, 2019 [DOI] [PubMed] [Google Scholar]
- 3.Welch LC, Teno JM, Mor V: End-of-life care in black and white: Race matters for medical care of dying patients and their families. J Am Geriatr Soc 53:1145-1153, 2005 [DOI] [PubMed] [Google Scholar]
- 4.Sanders JJ, Robinson MT, Block SD: Factors impacting advance care planning among African Americans: Results of a systematic integrated review. J Palliat Med 19:202-227, 2016 [DOI] [PubMed] [Google Scholar]
- 5.Mack JW, Paulk ME, Viswanath K, et al. : Racial disparities in the outcomes of communication on medical care received near death. Arch Intern Med 170:1533-1540, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Johnson KS, Kuchibhatla M, Tulsky AA: What explains racial differences in the use of advance directives and attitudes toward hospice care? J Am Geriatr Soc 56:1953-1958, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cohen LL: Racial/ethnic disparities in hospice care: A systematic review. J Palliat Med 11:763-768, 2008 [DOI] [PubMed] [Google Scholar]
- 8.Washington KT, Bickel-Swenson D, Stephens N: Barriers to hospice use among African Americans: A systematic review. Health Soc Work 33:267-274, 2008 [DOI] [PubMed] [Google Scholar]
- 9.Chapman EN, Kaatz A, Carnes M: Physicians and implicit bias: How doctors may unwittingly perpetuate health care disparities. J Gen Intern Med 28:1504-1510, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Smith AK, McCarthy EP, Paulk E, et al. : Racial and ethnic differences in advance care planning among patients with cancer: Impact of terminal illness acknowledgment, religiousness, and treatment preferences. J Clin Oncol 26:4131-4137, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ferrell BR, Temel JS, Temin S, et al. : Integration of palliative care into standard oncology care: American Society of Clinical Oncology Clinical Practice Guideline Update. J Clin Oncol 35:96-112, 2017 [DOI] [PubMed] [Google Scholar]
- 12.Smith TJ, Temin S, Alesi ER, et al. : American Society of Clinical Oncology provisional clinical opinion: The integration of palliative care into standard oncology care. J Clin Oncol 30:880-887, 2012 [DOI] [PubMed] [Google Scholar]
- 13.Enguidanos S, Vesper E, Goldstein R: Ethnic differences in hospice enrollment following inpatient palliative care consultation. J Hosp Med 8:598-600, 2013 [DOI] [PubMed] [Google Scholar]
- 14.Norton SA, Hogan LA, Holloway RG, et al. : Proactive palliative care in the medical intensive care unit: Effects on length of stay for selected high-risk patients. Crit Care Med 35:1530-1535, 2007 [DOI] [PubMed] [Google Scholar]
- 15.Bakitas MA, El-Jawahri A, Farquhar M, et al. : The TEAM approach to improving oncology outcomes by incorporating palliative care in practice. J Oncol Pract 13:557-566, 2017 [DOI] [PubMed] [Google Scholar]
- 16.Kline RM, Rocque GB, Rohan EA, et al. : Patient navigation in cancer: The business case to support clinical needs. J Oncol Pract 15:585-590, 2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Patel MI, Ramirez D, Agajanian R, et al. : Association of a lay health worker intervention with symptom burden, survival, health care use, and total costs among medicare enrollees with cancer. JAMA Netw Open 3:e201023, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hendricks BA, Lofton C, Azuero A, et al. : The project ENABLE cornerstone randomized pilot trial: Protocol for lay navigator-led early palliative care for African-American and rural advanced cancer family caregivers. Contemp Clin Trials Commun 16:100485, 2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Fischer SM, Kline DM, Min SJ, et al. : Effect of apoyo con carino (support with caring) trial of a patient navigator intervention to improve palliative care outcomes for latino adults with advanced cancer: A randomized clinical trial. JAMA Oncol 4:1736-1741, 2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Fouad MN, Acemgil A, Bae S, et al. : Patient navigation as a model to increase participation of African Americans in cancer clinical trials. J Oncol Pract 12:556-563, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Jandorf L, Braschi C, Ernstoff E, et al. : Culturally targeted patient navigation for increasing African Americans' adherence to screening colonoscopy: A randomized clinical trial. Cancer Epidemiol Biomarkers Prev 22:1577-1587, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Paskett ED, Harrop JP, Wells KJ: Patient navigation: An update on the state of the science. CA Cancer J Clin 61:237-249, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kim K, Choi JS, Choi E, et al. : Effects of community-based health worker interventions to improve chronic disease management and care among vulnerable populations: A systematic review. Am J Public Health 106:E3-E28, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Barnett ML, Gonzalez A, Miranda J, et al. : Mobilizing community health workers to address mental health disparities for underserved populations: A systematic review. Adm Policy Ment Health 45:195-211, 2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gottlieb LM, Wing H, Adler NE: A systematic review of interventions on patients' social and economic needs. Am J Prev Med 53:719-729, 2017 [DOI] [PubMed] [Google Scholar]
- 26.Jack HE, Arabadjis SD, Sun L, et al. : Impact of community health workers on use of healthcare services in the United States: A systematic review. J Gen Intern Med 32:325-344, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Asgary R, Naderi R, Wisnivesky J: Opt-out patient navigation to improve breast and cervical cancer screening among homeless women. J Womens Health (Larchmt) 26:999-1003, 2017 [DOI] [PubMed] [Google Scholar]
- 28.Cole H, Thompson HS, White M, et al. : Community-based, preclinical patient navigation for colorectal cancer screening among older black men recruited from barbershops: The MISTER B trial. Am J Public Health 107:1433-1440, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Patel MI, Periyakoil VS, Moore D, et al. : Delivering end-of-life cancer care: Perspectives of providers. Am J Hosp Palliat Care 35:497-504, 2018 [DOI] [PubMed] [Google Scholar]
- 30.LeBlanc TW, Lodato JE, Currow DC, et al. : Overcoming recruitment challenges in palliative care clinical trials. J Oncol Pract 9:277-282, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Mack JW, Weeks JC, Wright AA, et al. : End-of-life discussions, goal attainment, and distress at the end of life: Predictors and outcomes of receipt of care consistent with preferences. J Clin Oncol 28:1203-1208, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Mack JW, Cronin A, Keating NL, et al. : Associations between end-of-life discussion characteristics and care received near death: A prospective cohort study. J Clin Oncol 30:4387-4395, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Teno JM, Gruneir A, Schwartz Z, et al. : Association between advance directives and quality of end-of-life care: A national study. J Am Geriatr Soc 55:189-194, 2007 [DOI] [PubMed] [Google Scholar]
- 34.Lamont EB, Christakis NA: Prognostic disclosure to patients with cancer near the end of life. Ann Intern Med 134:1096-1105, 2001 [DOI] [PubMed] [Google Scholar]
- 35.Kamal AH, Bull JH, Swetz KM, et al. : Future of the palliative care workforce: Preview to an impending crisis. Am J Med 130:113-114, 2017 [DOI] [PubMed] [Google Scholar]
- 36.Baciu A, Negussie Y, Geller A, et al. (eds): Communities in Action: Pathways to Health Equity. National Academies Press (US), Washington, DC, 2017 [PubMed] [Google Scholar]
- 37.Hebert PL, Sisk JE, Howell EA: When does a difference become a disparity? Conceptualizing racial and ethnic disparities on health. Health Affair 27:374-382, 2008 [DOI] [PubMed] [Google Scholar]
- 38.Johnston FM, Neiman JH, Parmley LE, et al. : Stakeholder perspectives on the use of community health workers to improve palliative care use by African Americans with cancer. J Palliat Med 22:302-306, 2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kubi B, Enumah ZO, Lee KT, et al. : Theory-based development of an implementation intervention utilizing community health workers to increase palliative care use. J Pain Symptom Manage 60:10-19, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Demiris G, Parker Oliver D, Capurro D, et al. : Implementation science: Implications for intervention research in hospice and palliative care. Gerontologist 54:163-171, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Concannon TW, Meissner P, Grunbaum JA, et al. : A new taxonomy for stakeholder engagement in patient-centered outcomes research. J Gen Intern Med 27:985-991, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Hui D, Glitza I, Chisholm G, et al. : Attrition rates, reasons, and predictive factors in supportive care and palliative oncology clinical trials. Cancer 119:1098-1105, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Oriani A, Dunleavy L, Sharples P, et al. : Are the MORECare guidelines on reporting of attrition in palliative care research populations appropriate? A systematic review and meta-analysis of randomised controlled trials. BMC Palliat Care 19:6, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Hagen NA, Biondo PD, Brasher PM, et al. : Formal feasibility studies in palliative care: Why they are important and how to conduct them. J Pain Symptom Manage 42:278-289, 2011 [DOI] [PubMed] [Google Scholar]
- 45.Downing M, Lau F, Lesperance M, et al. : Meta-analysis of survival prediction with Palliative Performance Scale. J Palliat Care 23:245-252, 2007 [PubMed] [Google Scholar]
- 46.Anderson F, Downing GM, Hill J, et al. : Palliative performance scale (PPS): A new tool. J Palliat Care 12:5-11, 1996 [PubMed] [Google Scholar]
- 47.Holland JC, Andersen B, Breitbart WS, et al. : Distress management clinical practice guidelines in oncology. J Natl Compr Canc Netw 11:190-208, 2013. 23411386 [Google Scholar]
- 48.Hann D, Winter K, Jacobsen P: Measurement of depressive symptoms in cancer patients: Evaluation of the Center for Epidemiological Studies Depression Scale (CES-D). J Psychosomatic Res 46:437-443, 1999 [DOI] [PubMed] [Google Scholar]
- 49.Bruera E, Kuehn N, Miller MJ, et al. : The Edmonton Symptom Assessment System (ESAS): A simple method for the assessment of palliative care patients. J Palliat Care 7:6-9, 1991 [PubMed] [Google Scholar]
- 50.Lyons KD, Bakitas M, Hegel MT, et al. : Reliability and validity of the Functional Assessment of Chronic Illness Therapy-Palliative care (FACIT-Pal) scale. J Pain Symptom Manage 37:23-32, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Smith SK, Loscalzo M, Mayer C, et al. : Best practices in oncology distress management: Beyond the screen. Am Soc Clin Oncol Educ Book 38:813-821, 2018 [DOI] [PubMed] [Google Scholar]
- 52.Malterud K: Qualitative research: Standards, challenges, and guidelines. Lancet 358:483-488, 2001 [DOI] [PubMed] [Google Scholar]
- 53.Wood JV: Theory and research concerning social comparisons of personal attributes. Psychol Bull 106:231-248, 1989 [Google Scholar]
- 54.Bedell P, Wilson JL, White AM, et al. : “Our commonality is our past:” A qualitative analysis of re-entry community health workers' meaningful experiences. Health Justice 3:19, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Heng J, Sedhom R, Smith TJ: Lack of advance care planning before terminal oncology intensive care unit admissions. J Palliat Med 23:5-6, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Durant RW, Wenzel JA, Scarinci IC, et al. : Perspectives on barriers and facilitators to minority recruitment for clinical trials among cancer center leaders, investigators, research staff, and referring clinicians: Enhancing Minority Participation in Clinical Trials (EMPaCT). Cancer 120:1097-1105, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Niranjan SJ, Martin MY, Fouad MN, et al. : Bias and stereotyping among research and clinical professionals: Perspectives on minority recruitment for oncology clinical trials. Cancer 126:1958-1968, 2020 [DOI] [PubMed] [Google Scholar]
- 58.Basch E, Deal AM, Dueck AC, et al. : Overall survival results of a trial assessing patient-reported outcomes for symptom monitoring during routine cancer treatment. JAMA 318:197-198, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Parikh RB, Kakad M, Bates DW: Integrating predictive analytics into high-value care the dawn of precision delivery. JAMA 315:651-652, 2016 [DOI] [PubMed] [Google Scholar]
- 60.Enguidanos S, Kogan AC, Lorenz K, et al. : Use of role model stories to overcome barriers to hospice among African Americans. J Palliat Med 14:161-168, 2011 [DOI] [PubMed] [Google Scholar]
- 61.Volandes AE, Ariza M, Abbo ED, et al. : Overcoming educational barriers for advance care planning in Latinos with video images. J Palliat Med 11:700-706, 2008 [DOI] [PubMed] [Google Scholar]
- 62.Hanson LC, Armstrong TD, Green MA, et al. : Circles of care: Development and initial evaluation of a peer support model for African Americans with advanced cancer. Health Educ Behav 40:536-543, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]