PURPOSE:
Providers have cited fear of taking away hope from patients as one of the principal reasons for deferring advance care planning (ACP). However, research is lacking on the relationship between ACP and hope. We sought to investigate the potential association between ACP and hope in advanced cancer.
METHODS:
This is a cross-sectional analysis of baseline data from a primary palliative care intervention trial. All patients had advanced solid cancers. Three domains of ACP were measured using validated questions to assess discussion with oncologists about end-of-life (EOL) planning, selection of a surrogate decision maker, and completion of an advance directive. Hope was measured using the Hearth Hope Index (HHI). Multivariable regression was performed, adjusting for variables associated with hope or ACP.
RESULTS:
A total of 672 patients were included in this analysis. The mean age was 69.3 ± 10.2 years; 54% were female, and 94% were White. Twenty percent of patients (132 of 661) reported having a discussion about EOL planning, 51% (342 of 668) reported completing an advance directive, and 85% (565 of 666) had chosen a surrogate. There was no difference in hope between patients who had and had not had an EOL discussion (adjusted mean difference in HHI, 0.55; P = .181 for adjusted regression), chosen a surrogate (adjusted HHI difference, 0.31; P = .512), or completed an advance directive (adjusted HHI difference, 0.11; P = .752).
CONCLUSION:
In this study, hope was equivalent among patients who had or had not completed 3 important domains of ACP. These findings do not support concerns that ACP is associated with decreased hope for patients with advanced cancer.
INTRODUCTION
Advance care planning (ACP) is an important component of high-quality care for patients with advanced cancer.1-3 Defined as a process to help to ensure that patients receive care consistent with their goals and values,4 ACP may include one or more of the following: discussing values and preferences for future care, identifying a surrogate decision maker, and completing an advance directive.4 While oncologists recognize the importance of ACP,5,6 these activities continue to occur infrequently and late for patients with advanced disease.7-9 One of the principal reasons that physicians cite for failing to engage patients in ACP until late in a patient’s disease course is concern about giving up hope.10
Most patients with advanced cancer identify hope as important.11 Hope may alleviate psychological distress near the end of life (EOL) and may contribute to patients’ abilities to cope with their diagnoses.11,12 While conducting semistructured interviews with patients with cancer receiving palliative treatment, Nierop-van Baalen et al13 identified hope as a concept that provides resilience and prevents passivity. Limited data have even suggested a correlation between hopelessness and survival among patients with advanced breast cancer, with patients who show increased hopelessness having a relative risk of death of 3.4 compared with those with less hopelessness.14 However, to date, only one study has reported on the correlation between ACP (using an online decision aid) and hope15 and found no change in hope with this intervention. Elucidation of the relationship between ACP and hope may allow providers to better understand the impact of recommended ACP activities.
We therefore designed an analysis to examine associations between ACP and hope among patients with advanced cancer. Our primary aim was to determine whether patients who have engaged in ACP activities have different levels of hope from patients who have not. We hypothesized that patients with advanced cancer who have completed ACP will have equivalent hope to patients who have not completed ACP.
METHODS
Overview and Framework
Our study is a secondary cross-sectional analysis of baseline data collected as part of the A Primary Palliative Care Intervention for Patients with Advanced Cancer (CONNECT) study (ClinicalTrials.gov identifier: NCT02712229). Full details of the study design have been published previously.16 Data for this analysis were collected at the time of patient enrollment into the study before any palliative interventions. Examination of data from this time point allows us to determine whether associations exist between ACP and hope among patients with advanced cancer, independent of directed ACP or palliative care interventions.
Sample
This study enrolled patients from 17 medical oncology practices within the University of Pittsburgh Medical Center Hillman Cancer Center network in western Pennsylvania between July 2016 and October 2019. Clinic sites were chosen that lacked access to specialty palliative care because the subsequent trial involved randomization to usual care or primary (nurse-led) palliative care.
Patients eligible for the study were adults with advanced solid tumors for whom the oncologist would not be surprised if the patient died within the next year.17 Eligible patients had an Eastern Cooperative Oncology Group (ECOG) performance status of 0 (fully active, able to carry on all predisease performance without restriction), 1 (restricted in physically strenuous activity but ambulatory and able to carry out work of a light or sedentary nature [eg, light house work, office work]), or 2 (ambulatory and capable of all self-care but unable to carry out any work activities and up and about > 50% of waking hours)18 and anticipated receiving ongoing oncology care at their current site. Patients were excluded if they were unable to speak or read English, unable to consent to treatment, or had hematologic malignancies.16 All patients signed informed consent before participating. This study was approved by the University of Pittsburgh institutional review board.
Measures
All enrolled patients completed a baseline questionnaire. ACP was measured using 3 questions that have previously been used with seriously ill patient populations19,20: EOL planning discussion (“Have you and any of your health care providers at the cancer center discussed any particular wishes you have about the care you would want to receive if you were dying?”), surrogate decision maker (“Have you chosen a family member or friend to make decisions for you if you were no longer able to make decisions for yourself?”), and advance directive (“Have you completed a living will or advance directive?”). Hope was assessed by the Herth Hope Index (HHI).21,22 According to previous research that looked at the various instruments to measure hope, the HHI is the tool most commonly used in oncology.23 This validated scale contains 12 questions on a 4-point Likert scale that encompass 3 domains of hope: temporality and future, positive readiness and expectancy, and interconnectedness with self and others. The scale itself is scored from 12 to 48, with higher scores indicating higher levels of hope. A prior meta-analysis of interventions designed to address hope found that the HHI is responsive to change in patients with cancer.24 To date, there is no study of what represents a clinically significant (as opposed to statistically significant) difference in hope. To establish clinical equivalence, we needed to determine a margin of clinical significance. In the absence of a previously derived minimal clinically important difference, the decision was made to turn to expert opinion and consult with the author of the scale. After discussion conducted in November 2019, a 6-point difference was selected as the minimal clinically relevant difference.
Additional information collected during baseline questionnaires included demographic information, cancer type and current treatment, ECOG performance status as determined by the patient’s oncologist, symptom burden (assessed by the Edmonton Symptom Assessment Scale [ESAS]; range, 0-100, with higher numbers indicating worse symptom burden),25 and symptoms of anxiety and depression as measured by the Hospital Anxiety and Depression Scale (HADS; range, 0-21 each for anxiety and depression, with higher scores indicating worse anxiety or depression symptoms).26
Statistical Analysis
To describe the study population, continuous variables are presented as mean ± SD; categorical variables are presented as frequency (percentage). Comparisons between patients who answered yes versus no for each of the 3 ACP domains were performed using t tests for continuous variables and χ2 tests for categorical variables.
The two one-sided t tests procedure was used to test for equivalence of hope between patients who had undergone ACP versus those who had not, using an equivalence margin of 6 points (corresponding to an average difference of half a point across 12 Likert scale questions). In the absence of a previously derived minimal clinically important difference, this margin was selected on the basis of expert consultation with the author of the index, which was conducted in November 2019. We also performed multivariable linear regression analyses while controlling for factors identified as potential confounders on the basis of our clinical experience and a review of the literature.27-33 The predefined variables included age27-33; sex28,31,32; marital status33,34; socioeconomic status35,36; education level29-32,36; religious importance30,32,37; anxiety/emotional distress36,38-40; and clinic site, which served as a proxy for provider.41-43 All statistical analyses were performed using SAS 9.4 software (SAS Institute, Cary, NC).
RESULTS
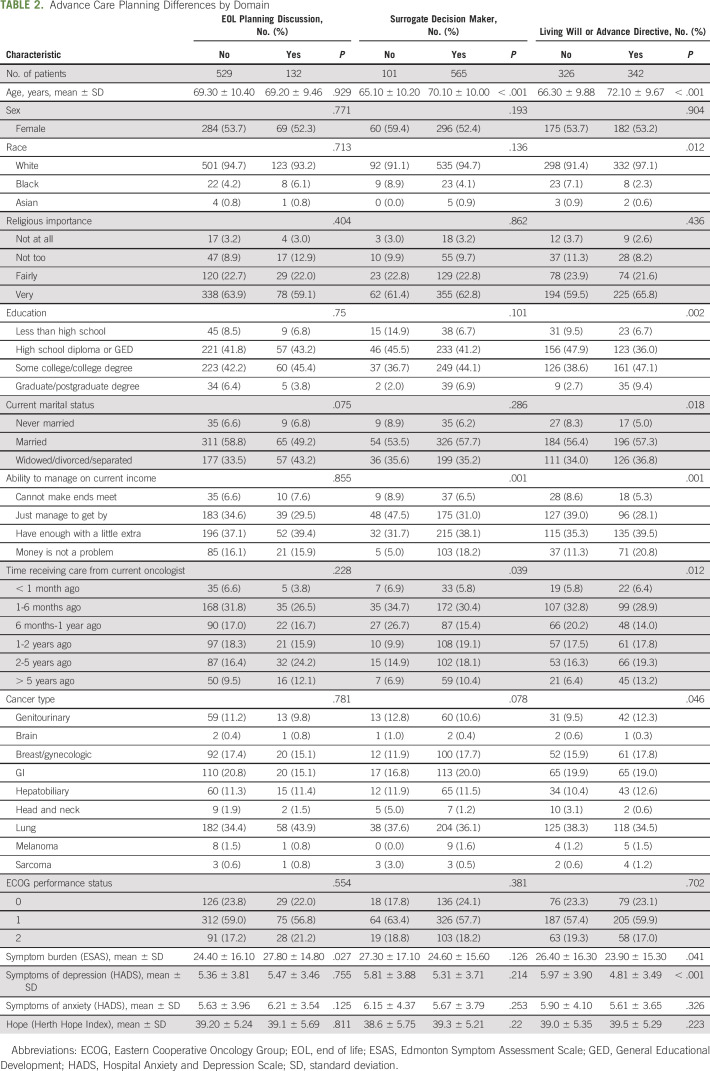
A total of 672 patients completed the baseline assessment. The mean age for our population was 69.3 ± 10.2 years, and the most common malignancies were lung (36%), GI (17%), and breast/gynecologic (17%; Table 1). The majority of patients answered all 3 ACP questions. Response rates were 98% (n = 661) for the question about having an EOL conversation with their physician, 99% (n = 666) for the question about a surrogate decision maker, and 99% (n = 668) for the question about an advance directive.
TABLE 1.
Demographic and Clinical Characteristics of the Study Population
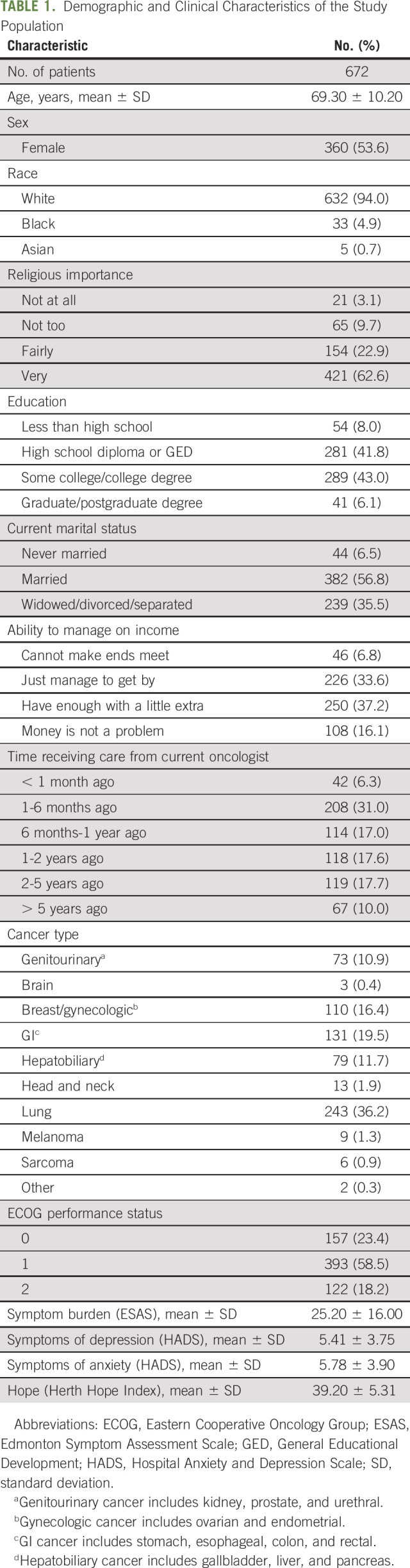
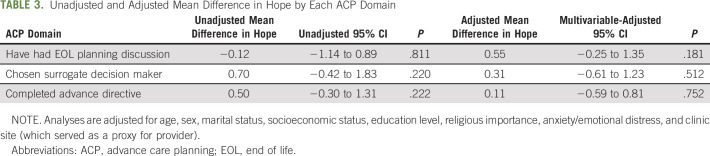
Twenty percent of the patients (132 of 661) reported that that they had had an EOL planning discussion with their cancer center provider. There were no differences in EOL planning discussion by age, sex, race, education, religion, marital status, cancer type, ECOG performance status, or treatment status (Table 2). In unadjusted analyses, there was no difference in hope between those who had and had not had an EOL planning discussion with their provider (HHI, 39.2 ± 5.24 v 39.1 ± 5.69, respectively; P = .811; Fig 1).
TABLE 2.
Advance Care Planning Differences by Domain
FIG 1.
Box plots of Herth Hope Index scores by advance care planning domain: (A) end-of-life discussion, (B) surrogate decision maker, and (C) advance directive.
A total of 565 (84.8%) of 666 patients reported that they had chosen a surrogate decision maker. Patients who had designated a surrogate decision maker were significantly more likely to be older, comfortable with their current income, and less recently diagnosed (Table 2). There was no difference in hope between patients who had and had not designated a surrogate decision maker (HHI, 39.3 ± 5.21 v 38.6 ± 5.75, respectively; P = .220; Fig 1)
Three hundred forty-two patients (51.2%) had completed an advance directive. Patients who had completed an advance directive were significantly more likely to be older, more highly educated, retired, comfortable with their current income, and less recently diagnosed with cancer (Table 2). Depression scores were also significantly lower in those who completed an advance directive (HADS depression score, 4.81 ± 3.49 v 5.97 ± 3.90, respectively; P < .001). There was no difference in hope between those who had and had not completed an advance directive (HHI, 39.5 ± 5.29 v 39.0 ± 5.35, respectively; P = .223; Fig 1)
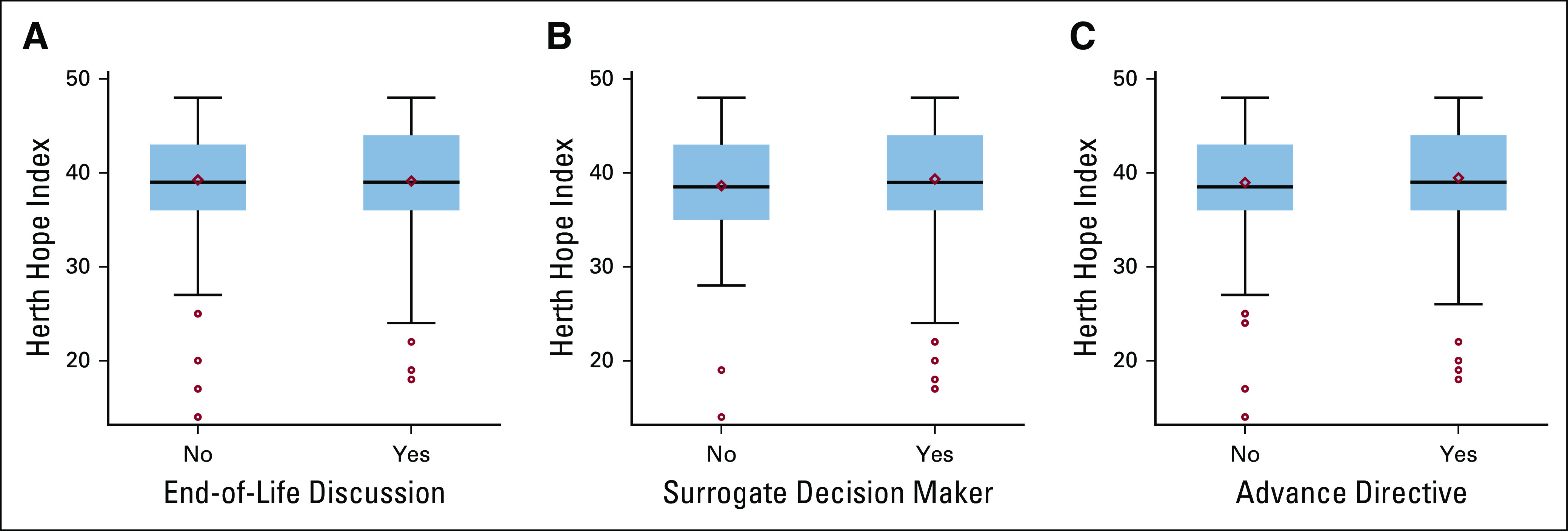
After adjusting for age, sex, marital status, socioeconomic status, education level, religious importance, anxiety, symptom burden (ESAS), time receiving care from current oncologist, and clinic site, there remained no difference in hope by each individual ACP domain (Table 3). Additional testing was performed to confirm statistical equivalence. Setting a margin of clinical significance of 6 points on the HHI (mean, 0.5 points per question difference), testing was performed to determine whether hope was clinically equivalent for each ACP domain. The equivalence tests provided evidence that the difference in hope was less than the prespecified margin of 6 points for those who had engaged in each of the ACP domains compared with those who had not. For all 3 domains, both the adjusted and the unadjusted hope scores were equivalent within a 6-point margin (for all, P < .001).
TABLE 3.
Unadjusted and Adjusted Mean Difference in Hope by Each ACP Domain
DISCUSSION
The primary aim of our study was to determine whether an association existed between ACP and hope in patients with advanced cancer. Our results indicate that hope is equivalent for patients who have and have not had an EOL discussion with their oncologist, designated a surrogate decision maker, or completed an advance directive, even after controlling for variables known to be associated with either hope or ACP. No other studies to our knowledge have tested for equivalence in hope between patients who have engaged in ACP and those who have not. However, our data are consistent with other studies in the field that have not demonstrated a relationship between ACP and hope.15 This work, by Green et al,15 looked at the impact of a web-based ACP intervention on hope in a population of 200 patients with advanced malignancy. The researchers found that compared with simply providing patients with the American Hospital Association guidelines on ACP, provision of a web-based ACP intervention did not affect hope. Similarly, previous qualitative research has been done to understand hope among patients with advanced lung cancer. In one study, it was found that although hope for a cure (sometimes called false hope) is prevalent in this population, hope for a good future and for living well in the time that remains is also common. The notion that patients hope to have some control surrounding the end of their life also suggests that ACP does not interfere with hope.44
Hope is an important component in caring for patients with advanced cancer at EOL,11,45 and providers often cite fear of giving up hope as the principal reason for deferring ACP discussions with their patients.13 Our data provide evidence that hope is equivalent among patients who have and have not completed 3 domains of ACP. These findings may help to reassure physicians who defer discussions about EOL wishes or surrogate decision makers or who delay introducing advance directives because of concerns about patients losing hope.
Although our data show that many variables are associated with ACP in a univariable analysis, when controlling for these variables in a multivariable analysis, they ultimately have no impact on the relationship between ACP and hope (Table 3). From the standpoint of hope, patients should be considered candidates for ACP regardless of their age, cancer type, religiosity, or clinic location. Indeed, our findings provide further support to previous research that has indicated that open and honest conversation, even at EOL, helps to maintain hope.46,47 ACP provides patients with a locus of control that may help to maintain hope at EOL.46,48,49
Low rates of engagement in ACP in our study are consistent with prior literature in advanced cancer populations. In a previous study of 185 patients with advanced cancer, 70% reported that they would like to have a conversation with their physician about EOL goals and preferences, but only 11% reported engaging in these conversations.50 Similarly, in a study of 118, only approximately half of patients with advanced cancer were found to have any formal advance directive documented in their chart.51 These data are consistent with our finding that 20% of patients with advanced cancer reported an EOL discussion, and 51% had an advance directive.
These findings must be interpreted in the context of the following limitations. First, the patients in this study all voluntarily enrolled in a study that involved a primary palliative care intervention. At baseline, patients and providers who were amenable to receiving palliative care may have been more open to ACP because the two are intricately linked. Second, our population was 94% White and 1.3% Hispanic. This finding is representative of the homogeneity of suburban and rural western Pennsylvania, where most counties report demographics consistent with our findings.52 We recognize that there is racial and cultural variation in attitudes toward and acceptance of ACP. Our racially and ethnically homogeneous population may limit broad generalizability. Third, because this is a cross-sectional analysis, we were unable to determine when ACP occurred, although any ACP would theoretically have been at some point before completing the baseline questionnaire. In addition, cross-sectional data allowed us to determine association but precluded us from determining causation. Finally, all ACP outcomes are patient reported. At times, providers may view a discussion they had as an EOL conversation, and patients may not have interpreted it this way or may not have recalled it. As such, the degree of engagement in ACP may be under-reported.
In conclusion, patient hope is equivalent after engaging in ACP in the form of an EOL discussion with a provider, designation of a surrogate decision maker, or completion of an advance directive. With no association between ACP and hope, providers may be able to feel more comfortable with having ACP conversations with their patients.
ACKNOWLEDGMENT
We thank Kaye Herth, PhD, RN, Minnesota State University, College of Allied Health and Nursing, for allowing us to use the HHI and for her expertise in defining a minimal clinically significant difference.
PRIOR PRESENTATION
Accepted for presentation at the 2020 Annual Academy of Hospice and Palliative Medicine. (Meeting subsequently canceled due to COVID-19).
SUPPORT
Supported by National Cancer Institute grant R01CA197103. This project used resources provided through the Clinical Protocol and Data Management and Protocol Review and Monitoring System, which are supported in part by award P30CA047904. Supported by the Palliative Research Center at the University of Pittsburgh.
AUTHOR CONTRIBUTIONS
Conception and design: Michael G. Cohen, Douglas White, Edward Chu, Yael Schenker
Administrative support: Robert M. Arnold
Provision of study material or patients: Yael Schenker
Collection and assembly of data: Michael G. Cohen, Margaret Rosenzweig, Yael Schenker
Data analysis and interpretation: Michael G. Cohen, Andrew D. Althouse, Robert M. Arnold, Hailey W. Bulls, Douglas White, Edward Chu, Kenneth Smith, Yael Schenker
Manuscript writing: All authors
Final approval of manuscript: All authors
Accountable for all aspects of the work: All authors
AUTHORS' DISCLOSURES OF POTENTIAL CONFLICTS OF INTEREST
Is Advance Care Planning Associated With Decreased Hope in Advanced Cancer?
The following represents disclosure information provided by authors of this manuscript. All relationships are considered compensated unless otherwise noted. Relationships are self-held unless noted. I = Immediate Family Member, Inst = My Institution. Relationships may not relate to the subject matter of this manuscript. For more information about ASCO's conflict of interest policy, please refer to www.asco.org/rwc or ascopubs.org/op/authors/author-center.
Open Payments is a public database containing information reported by companies about payments made to US-licensed physicians (Open Payments).
Robert M. Arnold
Other Relationship: UpToDate, VitaTalk
Edward Chu
Consulting or Advisory Role: Proteus Digital Health
Kenneth Smith
Research Funding: Nico Corporation (Inst)
No other potential conflicts of interest were reported.
REFERENCES
- 1.Dying in America: Improving quality and honoring individual preferences near the end of life. Mil Med 180:365-367, 2015 [DOI] [PubMed] [Google Scholar]
- 2. National Cancer Institute: PDQ Supportive and Palliative Care Editorial Board. Planning the Transition to End-of-Life Care in Advanced Cancer (PDQ): Health Professional Version. PDQ Cancer Information Summaries. Bethesda, MD, National Cancer Institute, 2002. [Google Scholar]
- 3.Rakatansky H: AMA code of medical ethics available online. Virtual Mentor 3, 2001 [DOI] [PubMed] [Google Scholar]
- 4.Sudore RL, Lum HD, You JJ, et al. : Defining advance care planning for adults: A consensus definition from a multidisciplinary Delphi panel. J Pain Symptom Manage 53:821-832.e1, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tulsky JA: Beyond advance directives: Importance of communication skills at the end of life. JAMA 294:359-365, 2005 [DOI] [PubMed] [Google Scholar]
- 6.Nedjat-Haiem FR, Cadet TJ, Amatya A, et al. : Healthcare providers’ attitudes, knowledge, and practice behaviors for educating patients about advance directives: A national survey. Am J Hosp Palliat Care 36:387-395, 2019 [DOI] [PubMed] [Google Scholar]
- 7.Sharp T, Moran E, Kuhn I, et al. : Do the elderly have a voice? Advance care planning discussions with frail and older individuals: A systematic literature review and narrative synthesis. Br J Gen Pract 63:e657-e668, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Holley JL, Hines SC, Glover JJ, et al. : Failure of advance care planning to elicit patients’ preferences for withdrawal from dialysis. Am J Kidney Dis 33:688-693, 1999 [DOI] [PubMed] [Google Scholar]
- 9.Brown AJ, Shen MJ, Urbauer D, et al. : Room for improvement: An examination of advance care planning documentation among gynecologic oncology patients. Gynecol Oncol 142:525-530, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nierop-van Baalen C, Grypdonck M, van Hecke A, et al. : Health professionals’ dealing with hope in palliative patients with cancer, an explorative qualitative research. Eur J Cancer Care (Engl) 28:e12889, 2019 [DOI] [PubMed] [Google Scholar]
- 11.McClement SE, Chochinov HM: Hope in advanced cancer patients. Eur J Cancer 44:1169-1174, 2008 [DOI] [PubMed] [Google Scholar]
- 12.Fitzgerald Miller J: Hope: A construct central to nursing. Nurs Forum 42:12-19, 2007 [DOI] [PubMed] [Google Scholar]
- 13.Nierop-van Baalen C, Grypdonck M, van Hecke A, et al. : Hope dies last … a qualitative study into the meaning of hope for people with cancer in the palliative phase. Eur J Cancer Care (Engl) 25:570-579, 2016 [DOI] [PubMed] [Google Scholar]
- 14.Dean C, Surtees PG: Do psychological factors predict survival in breast cancer? J Psychosom Res 33:561-569, 1989 [DOI] [PubMed] [Google Scholar]
- 15.Green MJ, Schubart JR, Whitehead MM, et al. : Advance care planning does not adversely affect hope or anxiety among patients with advanced cancer. J Pain Symptom Manage 49:1088-1096, 2015 [DOI] [PubMed] [Google Scholar]
- 16.Becker CL, Arnold RM, Park SY, et al. : A cluster randomized trial of a primary palliative care intervention (CONNECT) for patients with advanced cancer: Protocol and key design considerations. Contemp Clin Trials 54:98-104, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Curtis JR, Engelberg R, Young JP, et al. : An approach to understanding the interaction of hope and desire for explicit prognostic information among individuals with severe chronic obstructive pulmonary disease or advanced cancer. J Palliat Med 11:610-620, 2008 [DOI] [PubMed] [Google Scholar]
- 18.Oken MM, Creech RH, Tormey DC, et al. : Toxicity and response criteria of the Eastern Cooperative Oncology Group. Am J Clin Oncol 5:649-655, 1982 [PubMed] [Google Scholar]
- 19.Sudore RL, Heyland DK, Lum HD, et al. : Outcomes that define successful advance care planning: A delphi panel consensus. J Pain Symptom Manage 55:245-255.e8, 2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sudore RL, Heyland DK, Barnes DE, et al. : Measuring advance care planning: Optimizing the advance care planning engagement survey. J Pain Symptom Manage 53:669-681.e8, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Herth K: Abbreviated instrument to measure hope: Development and psychometric evaluation. J Adv Nurs 17:1251-1259, 1992 [DOI] [PubMed] [Google Scholar]
- 22. Herth K: Development and refinement of an instrument to measure hope. Sch Inq Nurs Pract 5:39-51, 1991; discussion 53-56. [PubMed] [Google Scholar]
- 23.Piccinelli C, Clerici CA, Veneroni L, et al. : Hope in severe disease: A review of the literature on the construct and the tools for assessing hope in the psycho-oncologic setting. Tumori 101:491-500, 2015 [DOI] [PubMed] [Google Scholar]
- 24.Li P, Guo Y-J, Tang Q, et al. : Effectiveness of nursing intervention for increasing hope in patients with cancer: A meta-analysis. Rev Lat Am Enfermagem 26:e2937, 2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bruera E, Kuehn N, Miller MJ, et al. : The Edmonton Symptom Assessment System (ESAS): A simple method for the assessment of palliative care patients. J Palliat Care 7:6-9, 1991 [PubMed] [Google Scholar]
- 26.Zigmond AS, Snaith RP: The Hospital Anxiety and Depression Scale. Acta Psychiatr Scand 67:361-370, 1983 [DOI] [PubMed] [Google Scholar]
- 27.Chu D, Yen Y-F, Hu H-Y, et al. : Factors associated with advance directives completion among patients with advance care planning communication in Taipei, Taiwan. PLoS One 13:e0197552, 2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Stream S, Nolan A, Kwon S, et al. : Factors associated with combined do-not-resuscitate and do-not-intubate orders: A retrospective chart review at an urban tertiary care center. Resuscitation 130:1-5, 2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hirschman KB, Abbott KM, Hanlon AL, et al. : What factors are associated with having an advance directive among older adults who are new to long term care services? J Am Med Dir Assoc 13:82.e7-82.e11, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ruff H, Jacobs RJ, Fernandez MI, et al. : Factors associated with favorable attitudes toward end-of-life planning. Am J Hosp Palliat Care 28:176-182, 2011 [DOI] [PubMed] [Google Scholar]
- 31.Inoue M: The influence of sociodemographic and psychosocial factors on advance care planning. J Gerontol Soc Work 59:401-422, 2016 [DOI] [PubMed] [Google Scholar]
- 32.Huang IA, Neuhaus JM, Chiong W: Racial and ethnic differences in advance directive possession: Role of demographic factors, religious affiliation, and personal health values in a national survey of older adults. J Palliat Med 19:149-156, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Li L-R, Lin M-G, Liang J, et al. : Effects of intrinsic and extrinsic factors on the level of hope and psychological health status of patients with cervical cancer during radiotherapy. Med Sci Monit 23:3508-3517, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Cooney TM, Shapiro A, Tate CE: End-of-life care planning: The importance of older adults’ marital status and gender. J Palliat Med 22:902-907, 2019 [DOI] [PubMed] [Google Scholar]
- 35.Barwise A, Juhn YJ, Wi C-I, et al. : An individual housing-based socioeconomic status measure predicts advance care planning and nursing home utilization. Am J Hosp Palliat Care 36:362-369, 2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Mahendran R, Chua SM, Lim HA, et al. : Biopsychosocial correlates of hope in Asian patients with cancer: A systematic review. BMJ Open 6:e012087, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Zarzycka B, Śliwak J, Krok D, et al. : Religious comfort and anxiety in women with cancer: The mediating role of hope and moderating role of religious struggle. Psychooncology 28:1829-1835, 2019 [DOI] [PubMed] [Google Scholar]
- 38.Balsanelli ACS, Grossi SAA: Predictors of hope among women with breast cancer during chemotherapy. Rev Esc Enferm USP 50:898-904, 2016 [DOI] [PubMed] [Google Scholar]
- 39.Fischer IC, Cripe LD, Rand KL: Predicting symptoms of anxiety and depression in patients living with advanced cancer: The differential roles of hope and optimism. Support Care Cancer 26:3471-3477, 2018 [DOI] [PubMed] [Google Scholar]
- 40.Tang ST, Chen J-S, Wen F-H, et al. : Advance care planning improves psychological symptoms but not quality of life and preferred end-of-life care of patients with cancer. J Natl Compr Canc Netw 17:311-320, 2019 [DOI] [PubMed] [Google Scholar]
- 41.Campbell TC, Carey EC, Jackson VA, et al. : Discussing prognosis: Balancing hope and realism. Cancer J 16:461-466, 2010 [DOI] [PubMed] [Google Scholar]
- 42.Salmon P, Hill J, Ward J, et al. : Faith and protection: The construction of hope by parents of children with leukemia and their oncologists. Oncologist 17:398-404, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Lovell A, Yates P: Advance care planning in palliative care: A systematic literature review of the contextual factors influencing its uptake 2008-2012. Palliat Med 28:1026-1035, 2014 [DOI] [PubMed] [Google Scholar]
- 44.Robinson CA: “Our best hope is a cure.” Hope in the context of advance care planning. Palliat Support Care 10:75-82, 2012 [DOI] [PubMed] [Google Scholar]
- 45.Alidina K, Tettero I: Exploring the therapeutic value of hope in palliative nursing. Palliat Support Care 8:353-358, 2010 [DOI] [PubMed] [Google Scholar]
- 46.Butt CM: Hope in adults with cancer: State of the science. Oncol Nurs Forum 38:E341-E350, 2011 [DOI] [PubMed] [Google Scholar]
- 47.Clayton JM, Hancock K, Parker S, et al. : Sustaining hope when communicating with terminally ill patients and their families: A systematic review. Psychooncology 17:641-659, 2008 [DOI] [PubMed] [Google Scholar]
- 48.Clayton JM, Butow PN, Arnold RM, et al. : Fostering coping and nurturing hope when discussing the future with terminally ill cancer patients and their caregivers. Cancer 103:1965-1975, 2005 [DOI] [PubMed] [Google Scholar]
- 49.Brown AJ, Sun CC, Urbauer DL, et al. : Feeling powerless: Locus of control as a potential target for supportive care interventions to increase quality of life and decrease anxiety in ovarian cancer patients. Gynecol Oncol 138:388-393, 2015 [DOI] [PubMed] [Google Scholar]
- 50.Waller A, Turon H, Bryant J, et al. : Medical oncology outpatients’ preferences and experiences with advanced care planning: A cross-sectional study. BMC Cancer 19:63, 2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Ahluwalia SC, Chuang FL, Antonio ALM, et al. : Documentation and discussion of preferences for care among patients with advanced cancer. J Oncol Pract 7:361-366, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Data USA: Westmoreland County, PA & Allegheny County, PA. https://datausa.io/profile/geo/westmoreland-county-pa?compare=allegheny-county-pa.