PURPOSE:
Hope is a modifiable entity that can be augmented. We evaluated the feasibility, acceptability, and efficacy of a short intervention to increase hopefulness in patients with advanced breast cancer and oncologists.
METHODS:
We enrolled eligible participants to two cohorts: one for patients with metastatic breast cancer and one for medical, radiation, or surgical oncologists. The intervention, a half-day hope enhancement workshop, included groups of 10-15 participants within each cohort. Participants in both cohorts completed preworkshop, postworkshop, and 3-month evaluations, which included the Adult Hope Scale (AHS), Herth Hope Index (HHI), and Patient-Reported Outcomes Measurement Information System-Global Health (PROMIS-GH) measures in patients, and the AHS, HHI, and a burnout self-assessment tool in physicians.
RESULTS:
We consented 13 patients and 26 oncologists for participation in the workshop and 76.9% (n = 10) of consented patients and 100% (n = 26) of consented physicians participated. Postworkshop, all participants planned to incorporate what they learned into their daily lives. In patients, AHS scores increased from preworkshop to postworkshop, and the mean change of 5.90 was significant (range 0-15, SD: 4.7, t = 3.99, P = .0032). HHI scores also increased, although the mean change was not significant. AHS and HHI scores did not significantly change in oncologists from preworkshop to postworkshop. At 3 months, less than half of the participants responded to the evaluation.
CONCLUSION:
We found that conducting a hope-enhancement workshop for patients with metastatic breast cancer and oncologists was feasible, generally acceptable to both populations, and associated with increased hopefulness in patients. Next steps should focus on confirming this effect in a randomized study and maintaining this effect in the postworkshop interval.
INTRODUCTION
Patients with metastatic breast cancer have limited life expectancy and face many hardships.1,2 The cancer will likely cause physical symptoms including pain, nausea, and fatigue, and most patients will receive several lines of therapy, which have concomitant side effects. Patients may also experience emotional burden from distress, anxiety, and depression, as well as psychosocial and financial stressors.3-5
Physicians who care for patients with advanced cancer also deal with many challenges. They prescribe toxic therapies, are frequently powerless to change outcomes, and witness suffering and death. These experiences can culminate in depression, exhaustion, and burnout, which can have additional consequences such as lack of empathy for patients and deterioration of personal relationships outside of work.6
One difficulty for patients with advanced cancer and oncologists is living with the loss of hope. Although this concern lurks, it is rarely discussed. Moreover, hope is vitally important but elusive to define.7 Snyder's conception of hope has been adopted by many in oncology.8 This construct separates hope from treatment outcome and posits that patients can have hope even with incurable disease.9,10 Snyder's model maintains that having a desire to set goals, designing pathways to achieve those goals, and following those paths can increase hopefulness. The model asserts that hope is not static, but a modifiable entity that can be augmented.
Prior studies in patients with chronic illnesses confirmed that the level of hope can change and that interventions to increase hope can also improve coping and quality of life.11-14 In patients with advanced cancer, both a 1-week hope enhancement program and an 8-week program increased hopefulness.15,16 The 8-week intervention continued to benefit patients 3, 6, and 9 months after it concluded. Given the time constraints of patients, a large gap pertains to whether a much shorter (eg, half-day) intervention can have an immediate impact and sustained benefit vis-à-vis hope enhancement.17
In physicians and other healthcare providers, hope has been shown to have an inverse relationship with burnout, increase job satisfaction, and be associated with reduced self-perceived medical errors.18-20 Burnout reduction interventions have been successful in physicians, but it is unknown if an intervention can increase hopefulness.21 In this pilot study, we aimed to determine the feasibility, acceptability, and preliminary efficacy of a half-day hope-enhancement workshop for patients with metastatic breast cancer and for oncologists.
METHODS
Study Population and Recruitment
There were two separate cohorts for participants: one for patients and one for physicians. Patients were of age 18 years or older with a diagnosis of stage IV breast cancer and had an Eastern Cooperative Oncology Group (ECOG) performance status of 0-3. Physicians were either a trainee or faculty with an MD or equivalent degree and practiced one of three oncologic disciplines: medical oncology, radiation oncology, or surgical oncology. All participants were English-speaking and had email access.
We recruited patients from the Johns Hopkins breast cancer clinics, and they took part in a workshop at Johns Hopkins Hospital (JHH) in Baltimore, MD. We recruited and enrolled physicians to workshops at two sites: JHH and Tel Aviv Medical Center (TAMC) in Tel Aviv, Israel. Israeli patients were not offered study participation since some did not have English proficiency and the workshop tools have not yet been translated or validated.
Study Procedures
Recruitment materials included Institutional Review Board (IRB)-approved electronic and posted advertisements and recruitment started 6 weeks prior to the workshop. We asked participants to complete assessments prior to the workshop, immediately after the workshop, and 3 months following the workshop.
For patients, assessments included the Adult Hope Scale (AHS), the Herth Hope Index (HHI), the Patient-Reported Outcomes Measurement Information System-Global Health (PROMIS-GH) measure, and additional questions about the workshop. For physicians, assessments included the AHS, HHI, a short burnout self-assessment tool, and additional questions about the workshop. The AHS measures hope according to Snyder's conception and higher scores are associated with increased hopefulness.9 The HHI measures the multidimensional nature of hope, and a higher score is associated with increased hopefulness.22-24 The PROMIS-GH metric is a measure of overall well-being and is scored on physical health and mental health subscales.25 Higher scores represent better physical or mental health. The burnout self-assessment tool assigns a score to predict the risk of burnout, and higher scores indicate a higher likelihood of burnout.26
Participants completed assessments in an electronic form supported by Qualtrics software from a laptop or mobile device. Each participant used a unique study ID and did not enter personal identification information into this platform. The JHH IRB and the TAMC IRB approved the study protocol (ClinicalTrials.gov identifier: NCT03074071).
Workshop Structure
Each workshop accommodated 10-15 participants. There was one patient and one physician workshop at JHH, and there was one physician workshop at TAMC. The patient and physician workshops were identical, and the purpose of each was to enhance the internal hopefulness in patients and physicians. The workshop did not aim to change how physicians communicate with patients about hope during clinical encounters. The workshops were developed based on Snyder's conception of hope and led by trained facilitators. The hope-enhancement workshop consisted of brief exercises to build each participant's strength in nominating goals that were personally relevant and designing pathways to achieve these objectives. The workshop began with a short didactic lecture that summarized hope theory. Participants then received a hope map and selected personal goals that could be accomplished within 6 months, defined a pathway to reach that goal, and considered potential obstacles and how to navigate these. Participants discussed their plans in an open forum and received feedback from the group. Finally, participants were led through a mental rehearsal that helped them envision overcoming obstacles in pursuit of their goals. Participants were encouraged to ask questions throughout the workshop. The total duration was approximately 4 hours. There were no incentives for study participation beyond reimbursement of parking costs.
Outcome Measures
The primary objective for this study was feasibility, measured as the proportion of consented participants who completed the workshop. The secondary objectives were to examine acceptability and preliminary efficacy of the intervention. Acceptability was assessed with yes/no and multiple-choice questions and open-ended questions. The main efficacy measure was mean change in AHS score from preworkshop to postworkshop. Additional efficacy measures included mean change from preworkshop to postworkshop HHI scores, PROMIS-GH scores in patients, and burnout self-assessment scores in physicians. Comparison of preworkshop AHS, HHI, PROMIS-GH, and burnout self-assessment scores to 3-month scores also occurred.
Statistical Analysis
The study sample size was based on convenience to conduct the workshops in groups of 10-15 participants each. We assessed patients and physicians in separate cohorts for feasibility, acceptability, and efficacy. For feasibility, the study was successful if 75% of those consented in each cohort participated in the workshop.
Acceptability was assessed as the proportion of patients who selected a certain answer in response to a yes/no or multiple-choice question. Efficacy assessment relied on the following participant-reported outcomes: AHS, HHI, and PROMIS-GH measures for patients, and the AHS, HHI, and burnout self-assessment tool for physicians. Participants completed assessments for these measures preworkshop, postworkshop, and at 3 months. For each measure, we looked at the distribution of scores at each time point. We used paired t-tests to assess the mean change in scores between preworkshop and postworkshop and preworkshop and 3 months. All efficacy analyses were done using Stata version 15.
RESULTS
Patients
Feasibility of the workshop.
We consented 13 patients to this study, and 10 patients (76.9%) participated in the hope-enhancement workshop. All patients enrolled to this study were women, and the median age was 52.5 years (range, 48-65 years). Nine out of 10 women reported their race as Caucasian and one patient reported her race as other. Two out of 10 patients identified as Hispanic or Latino. Seven out of 10 patients identified as Christian, including five patients who identified as Catholic; the three other patients reported no religion.
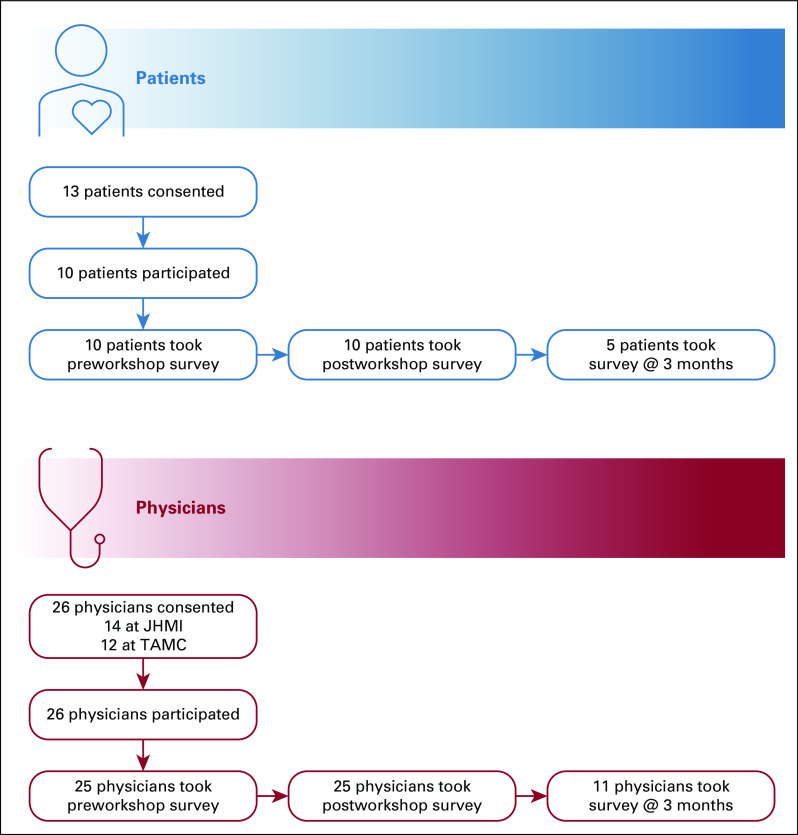
All 10 patients completed the preworkshop and postworkshop assessments. At 3 months, only half of the patients (n = 5) completed the assessment. Patients did not receive reminders or other prompts to complete the 3-month survey. On average, patients required < 10 minutes to complete the battery of questionnaires. An overview of consented patients is shown in Figure 1A.
FIG 1.
Overview of patients and physicians consented to participate in the hope-enhancement workshop.
Acceptability and efficacy of the workshop.
Postworkshop, all patients (100%, n = 10) rated their experience favorably among the three options, favorably, neutral, or unfavorably, and all would recommend the workshop to other patients. All patients (100%, n = 10) answered yes to the question on whether goal-setting and/or regoaling can contribute to increased hopefulness, were inclined to incorporate goal-setting ideas into their daily lives, and had a specific goal in mind. All patients responded that no aspect of the HEW made them uncomfortable. At 3 months, of the five patients who responded, four reported using principles from the HEW with three working on the goal they had outlined. Some thought-provoking comments are shared in Appendix Table A1, online only.
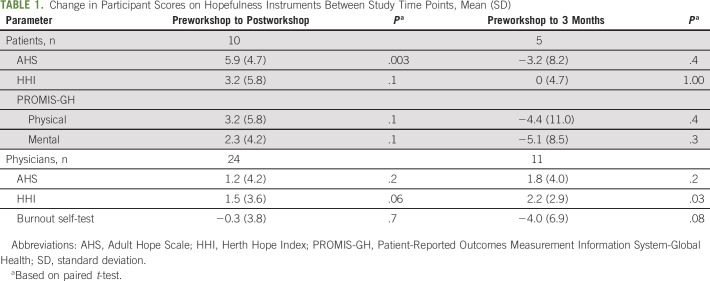
Results from the various efficacy assessments over the course of the study are shown in Table 1. AHS scores increased from preworkshop to postworkshop, and the mean change of 5.90 was significant (SD: 4.7, t = 3.99, P = .003). HHI scores also increased, although the mean change was not significant. At 3 months, only half of the patients completed the assessment.
TABLE 1.
Change in Participant Scores on Hopefulness Instruments Between Study Time Points, Mean (SD)
Oncologists
Feasibility of the workshop.
We consented 26 oncologists to this study, 14 at JHMI and 12 at TAMC, and all physicians participated in the hope-enhancement workshop. Evaluations from the two groups of physicians were pooled and examined together. Thirteen physicians were medical oncologists, 12 physicians were radiation oncologists, and one physician was a surgical oncologist. Eight physicians were trainees and the rest were faculty.
All 26 physicians took the preworkshop evaluation, but one person submitted 1 week after the completion of the workshop. This evaluation was not included in our analysis. Postworkshop, 24 of 26 physicians submitted the assessment. All 24 completed the AHS, HHI, and MBI instruments, but only 18 completed the other questions. At 3 months, only 11 of the 26 physicians submitted the evaluation. Physicians did not receive reminders or other prompts to complete the 3-month survey. An overview of consented oncologists is shown in Figure 1B.
Acceptability and efficacy of the workshop.
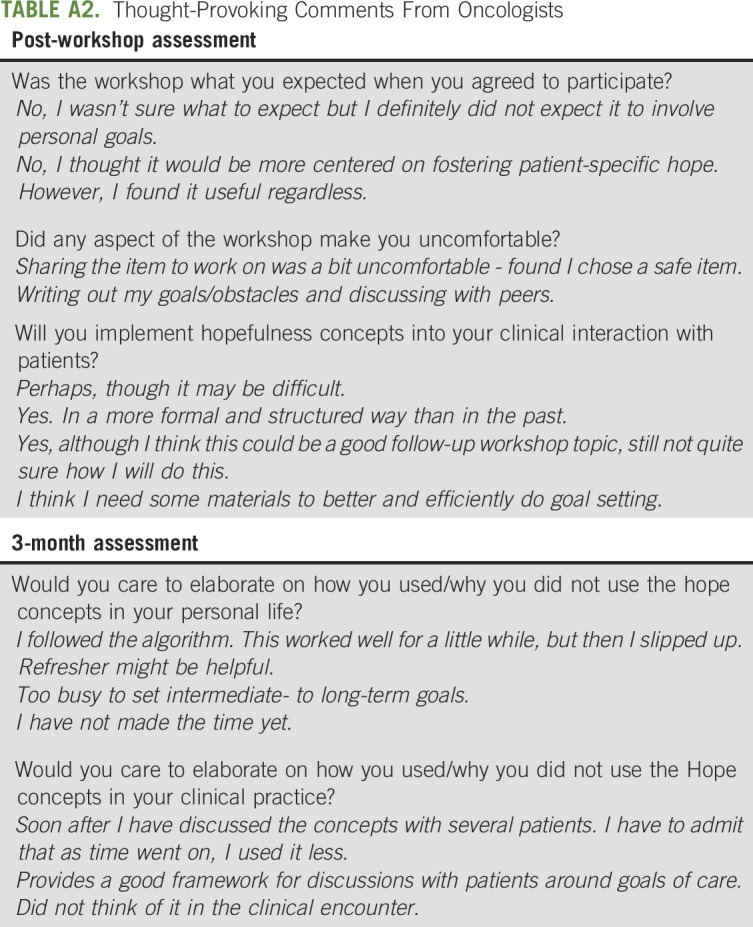
Out of 18 physicians, 16 (88.9%) rated their experience favorably and two physicians (11.1%) rated their experience as neutral. All would recommend the HEW to a colleague (100%, n = 18). All physicians (100%, n = 18) agreed that goal-setting could increase hopefulness and were inclined to incorporate principles learned into their daily lives, and all but one (94%, n = 17) had a specific goal in mind. Many (72%, n = 13) planned to incorporate hopefulness into their interactions with patients, but some noted this may be challenging or they may need additional training. More than half (55%, n = 10) thought the HEW was different than they expected, and some specifically noted that they expected it to be more focused on helping patients. A notable minority (27%, n = 5) responded that aspects of the HEW made them uncomfortable, particularly sharing their goals with the group.
At 3 months, only one-third of responding physicians (36%, n = 4) used the concepts learned in their personal lives, and less than half (45%, n = 5) used what they learned in the clinic. Interestingly, most (73%, n = 8) still planned to incorporate hope-enhancement strategies in the future and some (45%, n = 5) recommended a reinforcement of principles after the HEW. Some thought-provoking comments are shared in Appendix Table A2, online only.
Results of the various assessments over the course of the study are shown in Table 1. In the physician cohort, there were no significant mean changes in AHS scores, HHI scores, or the other assessments at the different time points.
DISCUSSION
We piloted a short half-day intervention to increase hopefulness in two separate groups: patients with metastatic breast cancer and oncologists. We determined this workshop was feasible in both groups. The intervention was also generally acceptable to both patients and physicians who agreed that goal-setting could increase hopefulness. Postworkshop, all were inclined to apply what they learned to their daily lives, and most had a specific goal in mind. Many physicians planned to incorporate what they learned into the clinic. One caveat is that some physicians found certain aspects of the workshop uncomfortable, and this will be discussed in further detail below. In patients, AHS scores increased from preworkshop to postworkshop, and the mean change was significant. HHI scores also increased, although the mean change was not significant. In physicians, the mean changes in AHS and HHI scores preworkshop and postworkshop were much smaller and not significant. At 3 months, only half of the patients and fewer than half of the oncologists responded to the evaluation.
Our study was small and designed only to assess preliminary efficacy, and therefore, the following discussion of efficacy end points must be considered exploratory. We used both the AHS and HHI to measure hopefulness. The hope-enhancement workshop is based on Snyder's conception of hope in which goal-setting can increase hopefulness, and the AHS is designed to measure this dimension of hope. The HHI touches on additional domains including spirituality, interconnectedness, and other facets of hope, which were not highlighted during the workshop. This is potentially why the magnitude of effect on AHS was greater than on HHI for patients in our study.
An innovation of our study was showing that even a short half-day intervention may enhance hope in patients. Earlier studies have relied on longer interventions to improve hopefulness.15,16 Patients with advanced cancer have many competing medical and personal priorities and a shorter intervention could be more acceptable. Unfortunately, in our study, hope enhancement was not maintained, and at 3 months, only half of the patients responded to the evaluation. This cannot be attributed solely to changing health status of the patients, as the survey response rate was poor even among physicians. An earlier study also found that the magnitude of benefit for patients of a hope-enhancement intervention declined over time.16 One solution could be sustained contact with workshop participants to reinforce the workshop's principles, which should start soon after completion of the workshop. Postworkshop follow-up could be mobile application-based rather than in person. Indeed, mobile technology has aided other healthcare interventions including for management of diabetes, symptoms related to HIV, atrial fibrillation, hypertension, and weight loss.27-33 We are currently defining the functionalities to incorporate into a smartphone application for oncology patients for maintenance of hopefulness. In addition, we are also considering modifications to conduct the workshop on videoconferencing platforms, which would allow us to comport with social-distancing guidelines and pursue accelerated scale up.
Compared to patients, the oncologists had the same mean AHS score and a lower mean HHI score at baseline, highlighting that there are many threats to hopefulness in addition to a diagnosis of advanced cancer. There is a body of work suggesting that physician hopefulness may be inversely associated with burnout and may have other positive effects. We are not aware of previous studies attempting to augment physician hopefulness, which highlights the steep learning curve to modifying hope in oncologists. A recent study speculated that oncologists have inherent discomfort with the concept of hopefulness.34 A sizable number of oncologists reported that the sharing aspects of the workshop made them uncomfortable, compared with none of the patients. One oncologist explicitly commented that they chose a safe goal to share. Others could have felt similarly constrained, limiting the workshop's efficacy.
Furthermore, some oncologists thought the workshop would focus on enhancing hope in patients, not for themselves. After the workshop, many oncologists wanted to incorporate hopefulness into their clinical encounters but thought that they may need additional training. Next steps for oncologists could include shaping the workshop to apply to the care of their patients. In addition, we have begun to develop patient and caregiver educational materials that can assist physicians in introducing hopefulness as a parameter of well-being. This could optimize the meaning oncologists find in their work, which may in turn reduce burnout.
An additional limitation of our study was that the patient group was relatively homogeneous. All patients were female and within a narrow age range, most patients were Caucasian, and most patients identified as Christian. Further work in a more diverse patient population is required to determine the generalizability of the intervention for patients. Additionally, we did not ask participants about their social supports, marital status, dependent children, employment status, educational background, spirituality, or other additional factors that could affect hope. Subsequent studies should collect this information and assess the potential impact on hope modification. A contrasting limitation in physicians may be that the group of participating oncologists was too heterogeneous by including faculty and trainees. The inclusion of both groups could have heightened discomfort surrounding the sharing aspects of the workshop.
Another important limitation of this study that has already been touched on was its small size and lack of random assignment. A larger, randomized study is needed to determine if the intervention can increase hopefulness in patients. Toward this end, the Southwest Oncology Group (SWOG) has expressed interest in studying hope enhancement for patients and healthcare providers using the model described herein (M. O'Rourke, personal communication, May 11, 2020).
In conclusion, a short intervention to increase hopefulness in patients with metastatic breast cancer and oncologists was feasible, acceptable, and was associated with increased hopefulness in patients immediately postworkshop. Follow-up was poor in both patients and oncologists at 3 months. Next steps should include earlier follow-up and more sustained contact with participants postworkshop as well as considering how the workshop can help oncologists care for their patients.
ACKNOWLEDGMENT
The authors would like to acknowledge Dr Orit Gutfield who enabled conduct of the trial at Tel Aviv Medical Center.
APPENDIX
TABLE A1.
Thought-Provoking Comments From Patients
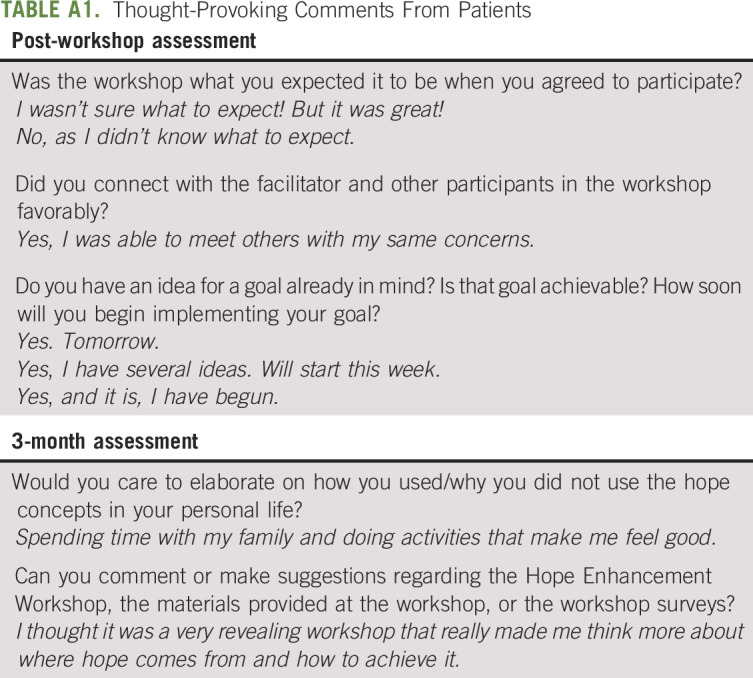
TABLE A2.
Thought-Provoking Comments From Oncologists
Dan Ariely
Patents, Royalties, Other Intellectual Property: Founder of Shapa—a numberless scale that helps people control their weight
Vered Stearns
Research Funding: AbbVie, Pfizer, MedImmune, Novartis, Puma Biotechnology, Biocept
Other Relationship: Immunomedics
B. Douglas Smith
Honoraria: Novartis Pharmaceuticals UK Ltd, Pfizer, Agios, Bristol Myers Squibb
Consulting or Advisory Role: CSL Behring, Celgene
Thomas J. Smith
Honoraria: Athenex, Association of Community Cancer Centers (ACCC)
Patents, Royalties, Other Intellectual Property: Royalties from Oxford Textbook of Cancer Communication, co-editor
(OPTIONAL) Open Payments Link: https://openpaymentsdata.cms.gov/physician/202382/general-payments
No other potential conflicts of interest were reported.
PRIOR PRESENTATION
Presented in part at the ASCO Supportive Care in Oncology Symposium, San Francisco, CA, October 2019.
SUPPORT
Supported by the Pamm Gross Kahane Research Institute of Life's Door (P.D.C., B.W.C.), the Center for Advanced Hindsight of Duke University (D.A.), and the Sidney Kimmel Comprehensive Cancer Center Core grant P30-CA006973 (V.S.).
AUTHOR CONTRIBUTIONS
Conception and design: Mirat Shah, Anna Ferguson, Phyllis Dvora Corn, Dan Ariely, B. Douglas Smith, Thomas J. Smith, Benjamin W. Corn
Administrative support: Thomas J. Smith
Provision of study materials or patients: Vered Stearns
Collection and assembly of data: Mirat Shah, Phyllis Dvora Corn, B. Douglas Smith, Thomas J. Smith
Data analysis and interpretation: Mirat Shah, Phyllis Dvora Corn, Ravi Varadhan, Vered Stearns, Thomas J. Smith
Manuscript writing: All authors
Final approval of manuscript: All authors
Accountable for all aspects of the work: All authors
AUTHORS' DISCLOSURES OF POTENTIAL CONFLICTS OF INTEREST
Developing Workshops to Enhance Hope Among Patients With Metastatic Breast Cancer and Oncologists: A Pilot Study
The following represents disclosure information provided by authors of this manuscript. All relationships are considered compensated unless otherwise noted. Relationships are self-held unless noted. I = Immediate Family Member, Inst = My Institution. Relationships may not relate to the subject matter of this manuscript. For more information about ASCO's conflict of interest policy, please refer to www.asco.org/rwc or ascopubs.org/op/authors/author-center.
Open Payments is a public database containing information reported by companies about payments made to US-licensed physicians (Open Payments).
Dan Ariely
Patents, Royalties, Other Intellectual Property: Founder of Shapa—a numberless scale that helps people control their weight
Vered Stearns
Research Funding: AbbVie, Pfizer, MedImmune, Novartis, Puma Biotechnology, Biocept
Other Relationship: Immunomedics
B. Douglas Smith
Honoraria: Novartis Pharmaceuticals UK Ltd, Pfizer, Agios, Bristol Myers Squibb
Consulting or Advisory Role: CSL Behring, Celgene
Thomas J. Smith
Honoraria: Athenex, Association of Community Cancer Centers (ACCC)
Patents, Royalties, Other Intellectual Property: Royalties from Oxford Textbook of Cancer Communication, co-editor
(OPTIONAL) Open Payments Link: https://openpaymentsdata.cms.gov/physician/202382/general-payments
No other potential conflicts of interest were reported.
REFERENCES
- 1.Thientosapol ES, Tran TT, Della-Fiorentina SA, et al. : Survival times of women with metastatic breast cancer starting first-line chemotherapy in routine clinical practice versus contemporary randomised trials. Intern Med J 43:883-888, 2013 [DOI] [PubMed] [Google Scholar]
- 2.Kiely BE, Soon YY, Tattersall MH, et al. : How long have I got? Estimating typical, best-case, and worst-case scenarios for patients starting first-line chemotherapy for metastatic breast cancer: A systematic review of recent randomized trials. J Clin Oncol 29:456-463, 2011 [DOI] [PubMed] [Google Scholar]
- 3.Aranda S, Schofield P, Weih L, et al. : Mapping the quality of life and unmet needs of urban women with metastatic breast cancer. Eur J Cancer Care (Engl) 14:211-222, 2005 [DOI] [PubMed] [Google Scholar]
- 4.Ganz PA, Stanton AL: Living with Metastatic Breast Cancer. Adv Exp Med Biol 862: 243-254, 2015 [DOI] [PubMed] [Google Scholar]
- 5.Mosher CE, Johnson C, Dickler M, et al. : Living with metastatic breast cancer: A qualitative analysis of physical, psychological, and social sequelae. Breast J 19:285-292, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Shanafelt T, Dyrbye L: Oncologist burnout: Causes, consequences, and responses. J Clin Oncol 30:1235-1241, 2012 [DOI] [PubMed] [Google Scholar]
- 7.Corn BW, Feldman DB, Wexler I: The science of hope. Lancet Oncol 21:e452-e459, 2020 [DOI] [PubMed] [Google Scholar]
- 8.Snyder CR, Harris C, Anderson JR, et al. : The will and the ways: Development and validation of an individual-differences measure of hope. J Pers Soc Psychol 60:570-585, 1991 [DOI] [PubMed] [Google Scholar]
- 9.Buckley J, Herth K: Fostering hope in terminally ill patients. Nurs Stand 19:33-41, 2004 [DOI] [PubMed] [Google Scholar]
- 10.Duggleby W, Wright K: Elderly palliative care cancer patients' descriptions of hope-fostering strategies. Int J Palliat Nurs 10:352-359, 2004 [DOI] [PubMed] [Google Scholar]
- 11.Ghazavi Z, Khaledi-Sardashti F, Kajbaf MB, et al. : Effect of hope therapy on the hope of diabetic patients. Iran J Nurs Midwifery Res 20:75-80, 2015 [PMC free article] [PubMed] [Google Scholar]
- 12.Fraser C, Keating M: The effect of a creative art program on self-esteem, hope, perceived social support, and self-efficacy in individuals with multiple sclerosis: A pilot study. J Neurosci Nurs 46:330-336, 2014 [DOI] [PubMed] [Google Scholar]
- 13.Alberto J, Joyner B: Hope, optimism, and self-care among Better Breathers Support Group members with chronic obstructive pulmonary disease. Appl Nurs Res 21:212-217, 2008 [DOI] [PubMed] [Google Scholar]
- 14.Bahmani B, Motamed Najjar M, Sayyah M, et al. : The effectiveness of cognitive-existential group therapy on increasing hope and decreasing depression in women-treated with haemodialysis. Glob J Health Sci 8:219-225, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Duggleby WD, Degner L, Williams A, et al. : Living with hope: Initial evaluation of a psychosocial hope intervention for older palliative home care patients. J Pain Symptom Manage 33:247-257, 2007 [DOI] [PubMed] [Google Scholar]
- 16.Herth K: Enhancing hope in people with a first recurrence of cancer. J Adv Nurs 32:1431-1441, 2000 [DOI] [PubMed] [Google Scholar]
- 17.Feldman DB, Dreher DE: Can hope be changed in 90 minutes? Testing the efficacy of a single-session goal-pursuit intervention for college students. J Happiness Stud 13:745-59, 2012 [Google Scholar]
- 18.Vetter MH, Vetter MK, Fowler J: Resilience, hope and flourishing are inversely associated with burnout among members of the Society for Gynecologic Oncology. Gynecol Oncol Rep 25:52-55, 2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Duggleby W, Cooper D, Penz K: Hope, self-efficacy, spiritual well-being and job satisfaction. J Adv Nurs 65:2376-2385, 2009 [DOI] [PubMed] [Google Scholar]
- 20.Hayashino Y, Utsugi-Ozaki M, Feldman MD, et al. : Hope modified the association between distress and incidence of self-perceived medical errors among practicing physicians: Prospective cohort study. PLoS One 7:e35585, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.West CP, Dyrbye LN, Rabatin JT, et al. : Intervention to promote physician well-being, job satisfaction, and professionalism: A randomized clinical trial. JAMA Intern Med 174:527-533, 2014 [DOI] [PubMed] [Google Scholar]
- 22.Herth K: Abbreviated instrument to measure hope: Development and psychometric evaluation. J Adv Nurs 17:1251-1259, 1992 [DOI] [PubMed] [Google Scholar]
- 23.Benzein E, Berg A: The Swedish version of Herth Hope Index--an instrument for palliative care. Scand J Caring Sci 17:409-415, 2003 [DOI] [PubMed] [Google Scholar]
- 24.Ripamonti CI, Buonaccorso L, Maruelli A, et al. : Hope Herth Index (HHI): A validation study in Italian patients with solid and hematological malignancies on active cancer treatment. Tumori 98:385-392, 2012 [DOI] [PubMed] [Google Scholar]
- 25.PROMIS : Global Health: A Brief Guide to PROMIS Global Health Instruments. http://www.healthmeasures.net/images/PROMIS/manuals/PROMIS_Global_Scoring_Manual.pdf [Google Scholar]
- 26.Tools M : Burnout Self-Test: Checking Yourself for Burnout. https://www.mindtools.com/pages/article/newTCS_08.htm [Google Scholar]
- 27.Bradley LE, Forman EM, Kerrigan SG, et al. : Project HELP: A remotely delivered behavioral intervention for weight regain after bariatric surgery. Obes Surg 27:586-598, 2017 [DOI] [PubMed] [Google Scholar]
- 28.Bollyky JB, Bravata D, Yang J, et al. : Remote lifestyle coaching plus a connected glucose meter with certified diabetes educator support improves glucose and weight loss for people with type 2 diabetes. J Diabetes Res 2018:3961730, 2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hartman SJ, Nelson SH, Cadmus-Bertram LA, et al. : Technology- and phone-based weight loss intervention: Pilot RCT in women at elevated breast cancer risk. Am J Prev Med 51:714-721, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Pal K, Eastwood SV, Michie S, et al. : Computer-based diabetes self-management interventions for adults with type 2 diabetes mellitus. Cochrane Database Syst Rev 2013:Cd008776, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Schnall R, Cho H, Mangone A, et al. : Mobile health technology for improving symptom management in low income persons living with HIV. AIDS Behav 22:3373-3383, 2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Guo Y, Chen Y, Lane DA, et al. : Mobile health technology for atrial fibrillation management integrating decision support, education, and patient involvement: mAF app trial. Am J Med 130:1388-1396.e6, 2017 [DOI] [PubMed] [Google Scholar]
- 33.Milani RV, Lavie CJ, Bober RM, et al. : Improving hypertension control and patient engagement using digital tools. Am J Med 130:14-20, 2017 [DOI] [PubMed] [Google Scholar]
- 34.Corn BW, Feldman D, Schapira L, et al. : Oncologist's reluctance to use the terms hope and cure: A bibliometric analysis of articles from high-impact journals. JNCI Cancer Spectr 4:pkaa065, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]