Abstract
Objective
To examine the effect of the consumption of ultraprocessed food on diet quality, and cardiometabolic risk (CMR) in an occupational cohort.
Design
Cross-sectional.
Setting
Occupational cohort.
Participants
53 163 British police force employees enrolled (2004–2012) into the Airwave Health Monitoring Study. A total of 28 forces across the UK agreed to participate. 9009 participants with available 7-day diet record data and complete co-variate data are reported in this study.
Main outcome measures
A CMR and Dietary Approaches to Stop Hypertension score were treated as continuous variables and used to generate measures of cardiometabolic health and diet quality. Secondary outcome measures include percentage of energy from fat, saturated fat, carbohydrate, protein and non-milk extrinsic sugars (NMES) and fibre grams per 1000 kcal of energy intake.
Results
In this cohort, 58.3%±11.6 of total energy intake was derived from ultraprocessed (NOVA 4) foods. Ultraprocessed food intake was negatively correlated with diet quality (r=−0.32, p<0.001), fibre (r=−0.20, p<0.001) and protein (r = −0.40, p<0.001) and positively correlated with fat (r=0.18, p<0.001), saturated fat (r=0.14, p<0.001) and nmes (r=0.10, p<0.001) intake. Multivariable analysis suggests a positive association between ultraprocessed food (NOVA 4) consumption and CMR. However, this main effect was no longer observed after adjustment for diet quality (p=0.209). Findings from mediation analysis indicate that the effect of ultraprocessed food (NOVA 4) intake on CMR is mediated by diet quality (p<0.001).
Conclusions
Ultraprocessed food consumption is associated with a deterioration in diet quality and positively associated with CMR, although this association is mediated by and dependent on the quality of the diet. The negative impact of ultraprocessed food consumption on diet quality needs to be addressed and controlled studies are needed to fully comprehend whether the relationship between ultraprocessed food consumption and health is independent to its relationship with poor diet quality.
Keywords: dietary patterns, metabolic syndrome
What this paper adds.
WHO has recently highlighted that the processing of foods is often coupled with a decline in the nutritional profile of the diet.
Classification systems have been created to aid categorisation of foods according to the grade at which they are processed. The most popular system is the NOVA Classification of Foods.
Studies have shown that foods categorised as ultra-processed are often high in fat and low in fibre.
High intakes of ultra-processed foods have been linked to increased risk of non-communicable diseases, including cardiovascular disease and some cancers.
This study demonstrates a deterioration in diet quality and cardiometabolic health with increasing intakes of ultra-processed food.
The association between ultra-processed food intake and poor health is mediated by diet quality.
Background
The increase in the world population over the last 100 years has been accompanied by an increase in quality of the food supply. This has been achieved through improved agriculture techniques and the processing of foods which ensure a robust ‘farm to folk’ food supply. The processing of food allows increased storage, safety and nutritional quality of food. Some 75% of food sales worldwide are processed.1 By 2050, the world will have to feed 9 billion people.2 The demand for food will be 60% greater than it is today. At the same time, the United Nations has set ending hunger, achieving food security and improved nutrition, and promoting sustainable agriculture as the second of its 17 Sustainable Development Goals for the year 2030.2 Given the interconnection of the food supply within and between countries it is difficult to see how this can be achieved without processing of food.
Although, food processing is integral to feeding the worlds growing population, the consumption of ultraprocessed foods has been associated with a deterioration in diet quality and non-communicable disease risk.3–10 Several classification systems have been proposed to classify foods according to their degree of processing11–13 of which NOVA is the most used, and the only one that defines the category of ultraprocessed foods. The NOVA system classifies all foods into four groups: unprocessed food (NOVA 1), processed culinary ingredients (NOVA 2), processed food (NOVA 3) and ultraprocessed food (NOVA 4).14 Ultraprocessed foods (NOVA 4) have been defined as industrial formulations of ingredients made up entirely or mostly of substances extracted from foods (fats, oils, sugar, starch and proteins) or synthesised in laboratories from food substrates or other organic sources for example food additives and flavourings.14 According to this classification system ultraprocessed foods (NOVA 4) include carbonated soft drinks, sweet or savoury snacks, confectionary, mass produced packaged breads, buns, pastries, cakes, biscuits and desserts, prepacked breakfast cereals, preprepared meals, including pies, pasta and pizza dishes, reconstituted meat and meat products, ‘instant’ soup and noodle dishes as well as many other items.14
Within the UK alone 56.8%–63.4% of energy intake comes from food that would be classified as ultraprocessed (NOVA 4).1 15 With respect to cardiometabolic health, this classification system has been used to demonstrate a link between ultraprocessed food (NOVA 4) consumption, obesity, type 2 diabetes as well as hypertension and other cardiovascular health outcomes.6 16–23 Studies have also shown that ultra-processed foods (NOVA 4) consumption is associated with a diet that is higher in fat, saturated fat and lower in fibre.8 12 15 24–27 To our current knowledge, the relationship between diet quality as measured using a dietary index score, cardiometabolic risk (CMR) and ultraprocessed food intake has not yet been explored in a UK adult population. Here, we use the Airwave Health Monitoring Study to explore this association in a UK adult occupational cohort.
Method
Data collection
Baseline data from participants within the Airwave Health Monitoring Study were used for the purpose of this study. The Airwave Health Monitoring Study is a longitudinal observational study of members of the police force in Great Britain. Recruitment procedures have been described in detail elsewhere.28 For this study, healthy participants with available baseline dietary data as of the end of June 2019 and complete covariate data were included (online supplemental figure, figure 1 participant flow chart). Participants completed 7 days diet diaries and visited an assessment clinic for blood sample collection, blood pressure and standardised anthropometrical measurement.
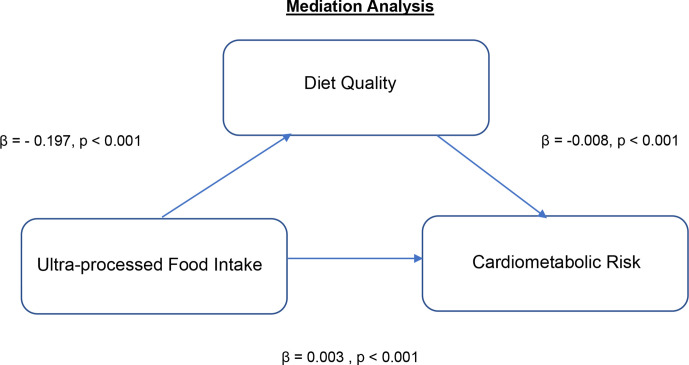
Figure 1.
Correlation matrix for the relationship between NOVA 4, diet quality and macro-nutrient intake. The numbers within the matrix indicate the coefficient of correlation between pairs of variables each.
bmjnph-2020-000225supp001.pdf (40.7KB, pdf)
Dietary assessment
Dietary intake was measured using 7-day estimated weight food diaries. Participants were provided with written information and visual aids to assist with portion estimation. Participants were requested to provide any appropriate additional information, for example, method of cooking and names of food brands. Weekly and daily nutritional intake per participant was calculated using the nutritional analysis software Dietplan V.7.0 (Forest field Software, Horsham, UK) which is based on the McCance and Widdowson’s seventh Edition Composition of Foods UK Nutritional Data set (UKN).29 Nutritional analysis of the 7-day diet records was conducted by a team of trained nutritionists and dietitians. To ensure consistency and reduce inter-coder and intra-coder errors, coders adhered to a study-specific dietary assessment protocol.
Diet quality was assessed by measuring adherence to the Dietary Approaches to Stop Hypertension (DASH) diet. Higher Adherence to the DASH diet has been associated with reduced CMR.30 A DASH index was used to calculate adherence.31 This is a 10-point food-based index that assesses diet quality by estimating levels of consumption of different food groups. Points are allocated on meeting targets for consumption of food groups. For example, with relation to fruit and vegetable food group, 10 points are assigned to a participant who meets daily intake as indicated by the index. Participants are allocated points proportional to the target intake. A higher score indicates a higher adherence to the DASH diet and as a result a diet of better quality.
NOVA classification of UKN composition database
We categorised 6885 UKN/study-specific food and beverage codes into NOVA 1, 2, 3 or 4 group in accordance with the NOVA food classification.14 This number represents 100% of the codes used to described dietary intake in this population.
The NOVA classification system requires ingredient information of food/beverage product for product categorisation. As this information was not always available on the nutritional analysis software Dietplan V.7.0, it was assumed that all codes described as ‘homemade’ fall into the NOVA 3 category and those described as ‘retail’ classified as NOVA 4. This decision was taken on the premise that foods described as ‘retail’ are more likely to contain non-nutrient ingredients which are used to identify a NOVA 4 food. There were some exceptions to this rule. For example, when a food or recipe was described as homemade with NOVA 4 food ingredients that is, lasagne homemade made with cook in pasta sauce this food or recipe was assigned NOVA 4. Information attached to food code was used to inform these exceptions. Furthermore, in the case where code description failed to specify whether a food item is of homemade or/retail origin, other information, for example, processing term in food descriptor (canned, tinned) or brand name was taken as an indicator of its origin. Consumption of ultraprocessed was determined by calculating the percentage energy consumed from those foods and beverages categorised as NOVA 4.
CMR calculation
A CMR score was generated for each participant as previously described.32 This score is composed of five components that are indicative of cardiometabolic health. Each component is worth one point. Scoring standards for each component are detailed below. The maximum score is 5 and minimum 0. A person with a score ≥3 is considered at high CMR.
1. Central obesity: waist circumference ≥94 cm—men, waist circumference ≥80 cm—women.
2. Dyslipidaemia: High Density Lipoprotein (HDL) <1.0 mmol/L, men and <1.3 mmol/L women and/or non-HDL ≥4.0 mmol/L and/or prescribed cholesterol lowering medication.
3. High blood pressure: systolic ≥130 mm Hg, and/or diastolic ≥85 mm Hg, and/or prescribed hypotensive medication.
4. Inflammation: High sensitivity Hs-CRP ≥3 mg/L<10 mg/L.
5. Impaired blood glucose control: HbA1c ≥5.7% and/or prescribed medication for glucose control.
Co-variate data
Covariates included are age in years and body mass index (BMI) kg/m2 presented as continuous variables as well as sex, household income (< £25 999, £26 000–£37 999, £38 000–£57 999, £58 000–£77 999, > £80 000) as a measure of socioeconomic class, highest education to date (left before GCSE/equivalent, GSCE/equivalent, A-level/equivalent or Higher), physical activity level (PAL) (high, medium, low), smoking status (current smoker, do not smoke) and dietary misreporting status (under, acceptable, over,) as calculated using the Goldberg cut-off energy intake: basal metabolic rate.33
Patient and public involvement
Public involvement in the Airwave Study comes from engagement with the Police Federation, Home Office, National Police Chiefs’ Council and the police officers and employees involved in the Airwave cohort. The Federation is represented on the Study’s Access Committee, and all three organisations were represented on the Steering Group along with UNISON (representing police staff). The Police Federation work in partnership with us on the enquiries made using the Airwave data set. They have been very supportive in lines of enquiry that provide understanding of lifestyle and the health of the police force.
Statistical analysis
Both continuous and categorical demographic variables were used to explore sample characteristics. Student’s t-test was used to compare sex differences in continuous data and χ2 test for independence to assess differences across categorical variables.
The analysis of variance (ANOVA) test for independence was performed to investigate difference in ultra-processed food intake (NOVA 4) between under, acceptable and over reporters.
We used Pearson correlation to assess associations between ultraprocessed food intake (NOVA 4), diet quality, macronutrient intake (plotted using the ggcorrplot R package) and multivariable linear regression for associations between ultraprocessed food intake (NOVA 4) and diet quality. A backward stepwise approach was taken in building the regression model. The final model included adjustment for known confounders for example, age, sex, smoking status, highest education, level of dietary misreporting and socioeconomic status.
Linear regression modelling was also used to explore the effect of ultraprocessed food (NOVA 4) consumption on CMR independent of diet quality. The final model was adjusted for known confounders: age, sex, DASH Score, level of misreporting, smoking status, PAL, BMI (kg/m2), highest education and socioeconomic status.
We conducted causal mediation analysis to investigate whether the effect of ultraprocessed food (NOVA 4) consumption on CMR is mediated by diet quality. To conduct this analysis, we used the R package ‘mediation’ and chose a model-based approach. Mediator and outcome models were adjusted for the following covariates: age, sex, BMI, smoking status, level of misreporting, highest education, PAL and socioeconomic status. To compute the point estimate of the indirect effect, we used the nonparametric bootstrap rather than the quasi-Bayesian Monte Carlo simulation for variance estimation via the boot=TRUE argument, sims=1000. All statistical tests were conducted using R software. Level of significance was set at p<0.05.
Results
Descriptive characteristics
A total of 9009 healthy participants with complete 7-day diet record and covariate data were included in this study. The average age was 40.9±9.2 years (60.8% men). The mean percentage of total energy intake from ultraprocessed foods (NOVA 4) was 58.3%±11.6. Sociodemographic, lifestyle and health characteristics are detailed in online supplemental table 1).
Difference in ultra-processed food intake (NOVA 4) across dietary reporting acceptability categories
More than half of the study population were categorised as acceptable reporters and a significant difference in the distribution of participants was observed across the reporting acceptability categories (p<0.05). The intake of ultra-processed food (NOVA 4) intake increased across reporting categories from participants under-reporting to participants over-reporting. The mean energy intake from NOVA 4 foods was significantly lower in participants categorised under-reporting energy intake than participants with acceptable and over reporting (table 1).
Table 1.
Ultraprocessed food intake across dietary reporting acceptability categories
| Dietary reporting acceptability categories | ||||||
| Under | Acceptable | Over | All | *p value | ||
| Total | n (%) | 3455 (38.4) | 5382 (59.7) | 172 (1.9) | 9009 (100.0) | <0.001 |
| NOVA 4 (% Kcal) | Mean (SD) | 57.2 (12.2) | 58.9 (11.2) | 61.2 (11.1) | 58.3 (11.6) | <0.001 |
*p<0.05 significant.
Relationship between ultra-processed food intake (NOVA 4), diet quality and macro-nutrient intake
Pearson correlation analysis (figure 1) shows a positive correlation between intake of ultra-processed food (NOVA 4), intakes of carbohydrate, non-milk extrinsic sugar, fat and saturated fat as well as diet energy density. A negative correlation was observed between ultra-processed food (NOVA 4) intake, protein, fibre and diet quality.
Multi-variable regression analysis was used to further explore the association between ultra-processed food intake (NOVA 4) and diet quality. Both unadjusted (model 1) and adjusted (model 2) model indicate a negative association between ultra-processed food (NOVA 4) intake and diet quality (table 2).
Table 2.
Association between ultra-processed food (NOVA 4) and diet quality
| Model 1 | Model 2 | |||||
| Effect, diet quality | SD | P value | Effect, diet quality | SD | P value | |
| NOVA 4 (% Kcal) | −0.212 | 0.007 | <0.001 | −0.197 | 0.007 | <0.001 |
Model 1: crude+age
Model 2: model 1+education+socioeconomic status+level of misreporting.
Relationship between ultraprocessed food intake (NOVA 4) and CMR
A multivariate regression was conducted to explore association between ultraprocessed food (NOVA 4) intake and CMR. As outlined in table 3, results show a deterioration in CMR with increasing NOVA 4 consumption. After controlling for diet quality, this relationship was no longer significant.
Table 3.
Association between ultraprocessed food (NOVA 4) and CMR
| Model 1 | Model 2 | |||||
| Effect CMR | SD | P value | Effect, CMR | SD | P value | |
| NOVA 4 (% Kcal) | 0.003 | 0.001 | 0.001 | 0.001 | 0.001 | 0.209 |
Model 1: crude+age+sex+BMI smoking status+education+socioeconomic status+PAL+level of misreporting.
Model 2: model 1+DASH score.
BMI, body mass index; CMR, cardiometabolic risk; DASH, Dietary Approaches to Stop Hypertension; PAL, physical activity level.
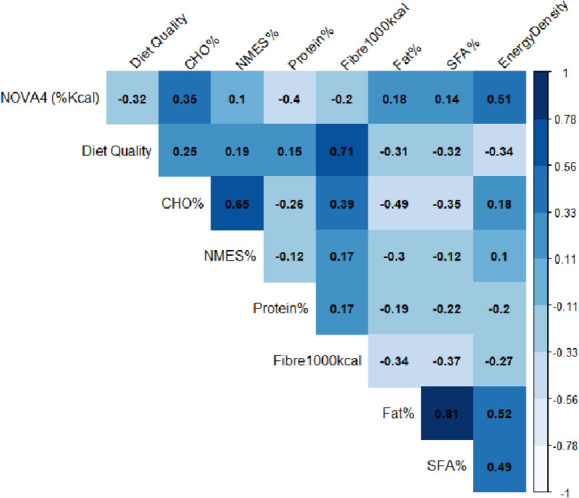
Mediation analysis
The effect of ultraprocessed food (NOVA 4) intake on CMR is mediated by diet quality (figure 2). There is a negative (inverse) association between ultraprocessed food (NOVA 4) and diet quality and between diet quality and CMR. The indirect effect was (−0.197)*(−0.008)=0.0016 (95% CI 0.0011, 0.0022, p<0.001).
Figure 2.
Standard regression coefficients for the relationship between ultraprocessed food (NOVA 4) intake and CMR as mediated by diet quality. CMR, cardiometabolic risk.
Discussion
Preceding research in this area ranged from studies that examined the relationship between ultra-processed food intake, chronic disease and health,7 10 to those that compared the nutrient composition of foods according to grade of processing,27 34 35 while, other studies explored variance in dietary composition between those considered high versus low consumers ofultra-processed food.4 7 10 22–24 36–40 However, to our understanding, there is no strong evidence to suggest that within a UK population the effect of ultra-processed food intake on disease risk and health is independent of diet quality.
We report here a high proportion of ultraprocessed (NOVA 4) consumption in the Airwave cohort with more than half of total energy intake derived from foods categorised as NOVA 4. Other studies in the UK, France and Canada have reported similar intakes.1 15 19 41 These findings are consistent across studies using indirect (food expenditure survey data) and direct (24 hours recall/dietary record data) methodologies to capture food consumption. Our findings reinforce the evidence that the consumption of ultraprocessed foods is increasing.19
We also show a negative impact of ultra-processed (NOVA 4) food consumption on diet quality and nutrient composition. Ultraprocessed (NOVA 4) food consumption was positively associated with energy density, intake of fat, saturated fat and non-milk extrinsic sugars but negatively with fibre, protein intake and diet quality. Our findings are consistent with preceding research in this area. Within the UK, high intakes of ultra-processed foods have been positively associated with fat, saturated fat and inversely associated with fibre and protein intakes.15 41 In non-UK populations, ultra-processed food consumption has been negatively associated with diet quality in studies using both priori (diet indexes) and non priori approaches (principle component analysis) to measure diet quality.3 4 17
We show in a multivariate analysis a deterioration in CMR with increasing ultraprocessed (NOVA 4) food intake. Although this main effect was no longer significant after adjustment for diet quality. Furthermore, findings from mediation analysis show that the impact of ultraprocessed food (NOVA 4) intake on CMR is mediated by diet quality and therefore an effect of ultraprocessed (NOVA 4) food intake on CMR independent of diet quality was not observed. Previous studies in this area have reported a worsening in health and non-communicable disease risk and morality with increasing ultraprocessed food intake.3–5 7 10 15 18 23 38 39 42 43 In the few these studies that have adjusted for diet quality a change in effect was not observed.3–5
Strengths and limitations
This study is to our knowledge to first to show that the impact of ultra-processed food intake on CMR is mediated through the deterioration of diet quality. There is also strength in the methodological approach taken in this study. For example, diet quality was determined using a validated diet quality index. This approach is thought to be most advantageous in comparison to posteriori approaches which generate dietary patterns based on available data without a priori hypothesis and these patterns may not represent the optimal.44 Furthermore, this study used 7-day diet records to capture dietary intake. This prospective dietary collection method offers detailed information without the limitations associated with recall and Food Frequency Questionnaire (FFQ) techniques. However, it is not short of its own limitations including dietary misreporting a limitation to any subjective measure of dietary.45 Studies have demonstrated a positive change in dietary behaviour in light of recording intake. This often means that the intake captured is a false representation of the persons habitual diet.45 However, to control for this inherent limitation, the Goldberg cut-off for energy intake: basal metabolic rate equation was conducted for each participant and included in association models to adjust for level of misreporting.33 The study also has some other limitations. First, we used cross-sectional data. As a result, a temporal relationship between ultra-processed food intake, diet quality, nutrient composition and CMR could not be assessed. Other shortcomings relate to the categorisation of food codes into NOVA groupings according to the NOVA classification system. Food codes did not always have an accompanied ingredient list which sometimes caused ambiguity to what NOVA group a food code should be placed which may have led to an overestimation in ultraprocessed food intake.
Conclusion
Food processing is necessary to keep up with feeding the world’s growing population. However, there is strong evidence to show that the consumption of food that has been ultraprocessed is negatively associated with diet quality and health. In this study, we show that the consumption of ultraprocessed food increases CMR through the worsening of the overall quality of the diet. This is the first study in this field to observe this association. The negative impact of ultraprocessed food consumption on diet quality needs to be addressed and controlled studies are needed to fully comprehend whether the relationship between ultraprocessed food consumption and health is independent to its relationship with poor diet quality.
Acknowledgments
GF and PE is an NIHR senior investigator. PE acknowledges support from the NIHR Biomedical Research Centre, the NIHR Health Protection Research Unit on Health Effects of Environmental Hazards (HPRU-2012–10141), and the Medical Research Council-Public Health England (MRC-PHE) Centre for Environment and Health (MR/L01341X/1). PE is a UK Dementia Research Institute (DRI) foundation Professor, UK DRI at Imperial College London. The UK DRI is funded by the Medical Research Council, Alzheimer’s Society and Alzheimer’s Research UK. PE is an Associate Director of the Health Data Research UK (HDR-UK) London Centre funded by HDR UK. This work used computing resources of the UK MEDical BIOinformatics partnership—aggregation, integration, visualisation and analysis of large, complex data (UK MED-BIO) supported by the Medical Research Council (MR/L01632X/1). The Section for Nutrition Research is funded by grants from the MRC, Biotechnology and Biological Sciences Research Council (BBSRC) and NIHR Imperial Biomedical Research Centre. We thank all participants in the Airwave Health Monitoring Study.
We also thank the following members of the Airwave Health Monitoring Study research team at Imperial College London.
Footnotes
Twitter: @gfrost59
Contributors: GF, JG, AA, AK conceived the study, JG, AA, AK undertook the analysis. All authors contributed to the interpretation of the data and writing the manuscript.
Funding: The Airwave Health Monitoring Study is funded by the Home Office (grant number 780-TETRA) and the Medical Research Council (grant number MR/L01341X/1), with additional support from the National Institute for Health Research (NIHR) Imperial Biomedical Research Centre (BRC). The diet coding was supported through discretionary departmental funds.
Disclaimer: The views expressed are those of the authors and not necessarily those of the Home Office, the Imperial BRC, the NHS, the NIHR or the Department of Health and Social Care.
Competing interests: PE reports grant funding from the Home Office. GF reports grant funding from Nestle, Heptares and Quorn.
Provenance and peer review: Not commissioned; externally peer reviewed by John Mathers, Newcastle University, UK
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data are available in a public, open access repository. All data are available throughout the Dementia Platform https://portal.dementiasplatform.uk/
Ethics statements
Patient consent for publication
Not required.
References
- 1. Moubarac J-C, Claro RM, Baraldi LG, et al. International differences in cost and consumption of ready-to-consume food and drink products: United Kingdom and Brazil, 2008-2009. Glob Public Health 2013;8:845–56. 10.1080/17441692.2013.796401 [DOI] [PubMed] [Google Scholar]
- 2. United Nations . The sustainable development goals report, 2017. [Google Scholar]
- 3. Srour B, Fezeu LK, Kesse-Guyot E, et al. Ultra-processed food intake and risk of cardiovascular disease: prospective cohort study (NutriNet-Santé). BMJ 2019;365:l1451. 10.1136/bmj.l1451 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Fiolet T, Srour B, Sellem L, et al. Consumption of ultra-processed foods and cancer risk: results from NutriNet-Santé prospective cohort. BMJ 2018;360:k322. 10.1136/bmj.k322 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Zhang Z, Jackson SL, Martinez E. Association between ultraprocessed food intake and cardiovascular health in US adults: a cross-sectional analysis of the NHANES 2011-2016. [DOI] [PMC free article] [PubMed]
- 6. Askari M, Heshmati J, Shahinfar H, et al. Ultra-processed food and the risk of overweight and obesity: a systematic review and meta-analysis of observational studies. Int J Obes 2020;44:2080–91. 10.1038/s41366-020-00650-z [DOI] [PubMed] [Google Scholar]
- 7. Chen X, Zhang Z, Yang H, et al. Consumption of ultra-processed foods and health outcomes: a systematic review of epidemiological studies. Nutr J 2020;19:86. 10.1186/s12937-020-00604-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Marrón-Ponce JA, Flores M, Cediel G, et al. Associations between consumption of Ultra-Processed foods and intake of nutrients related to chronic non-communicable diseases in Mexico. J Acad Nutr Diet 2019;119:1852–65. 10.1016/j.jand.2019.04.020 [DOI] [PubMed] [Google Scholar]
- 9. Monteiro CA, Levy RB, Claro RM, et al. Increasing consumption of ultra-processed foods and likely impact on human health: evidence from Brazil. Public Health Nutr 2011;14:5–13. 10.1017/S1368980010003241 [DOI] [PubMed] [Google Scholar]
- 10. Pagliai G, Dinu M, Madarena MP, et al. Consumption of ultra-processed foods and health status: a systematic review and meta-analysis. Br J Nutr 2021;125:1–11. 10.1017/S0007114520002688 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.et alBecker W, Unwin I, Ireland J. Proposal for structure and detail of a EuroFIR standard on food composition data, 2006. Available: http://www.eurfir.net/ [Accessed 15 Feb 2021].
- 12. Slimani N, Deharveng G, Southgate DAT, et al. Contribution of highly industrially processed foods to the nutrient intakes and patterns of middle-aged populations in the European prospective investigation into cancer and nutrition study. Eur J Clin Nutr 2009;63 Suppl 4:S206–25. 10.1038/ejcn.2009.82 [DOI] [PubMed] [Google Scholar]
- 13. The food classification and description system FoodEx 2 (revision 2). EFSA Support Publ 2017;12. [Google Scholar]
- 14. Monteiro CA, Cannon G, Levy RB, et al. Ultra-processed foods: what they are and how to identify them. Public Health Nutr 2019;22:936–41. 10.1017/S1368980018003762 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Rauber F, da Costa Louzada ML, Steele EM, et al. Ultra-Processed food consumption and chronic non-communicable Diseases-Related dietary nutrient profile in the UK (2008⁻2014). Nutrients 2018;10. 10.3390/nu10050587. [Epub ahead of print: 09 May 2018]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Srour B, Fezeu LK, Kesse-Guyot E, et al. Ultraprocessed food consumption and risk of type 2 diabetes among participants of the NutriNet-Santé prospective cohort. JAMA Intern Med 2020;180:283–91. 10.1001/jamainternmed.2019.5942 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Zhang Z, Jackson SL, Martinez E, et al. Association between ultraprocessed food intake and cardiovascular health in US adults: a cross-sectional analysis of the NHANES 2011-2016. Am J Clin Nutr 2021;113:428–36. 10.1093/ajcn/nqaa276 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Nardocci M, Polsky JY, Moubarac J-C. Consumption of ultra-processed foods is associated with obesity, diabetes and hypertension in Canadian adults. Can J Public Health 2020. 10.17269/s41997-020-00429-9. [Epub ahead of print: 10 Nov 2020]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Monteiro CA, Moubarac J-C, Levy RB, et al. Household availability of ultra-processed foods and obesity in nineteen European countries. Public Health Nutr 2018;21:18–26. 10.1017/S1368980017001379 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Rauber F, Chang K, Vamos EP, et al. Ultra-processed food consumption and risk of obesity: a prospective cohort study of UK Biobank. Eur J Nutr 2020. 10.1007/s00394-020-02367-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Rauber F, Steele EM, Louzada MLdaC, et al. Ultra-processed food consumption and indicators of obesity in the United Kingdom population (2008-2016). PLoS One 2020;15:e0232676. 10.1371/journal.pone.0232676 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Silva FM, Giatti L, de Figueiredo RC, et al. Consumption of ultra-processed food and obesity: cross sectional results from the Brazilian longitudinal study of adult health (ELSA-Brasil) cohort (2008–2010). Public Health Nutr 2018;21:2271–9. 10.1017/S1368980018000861 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Nardocci M, Leclerc B-S, Louzada M-L, et al. Consumption of ultra-processed foods and obesity in Canada. Can J Public Health 2019;110:4–14. 10.17269/s41997-018-0130-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Moubarac J-C, Batal M, Louzada ML, et al. Consumption of ultra-processed foods predicts diet quality in Canada. Appetite 2017;108:512–20. 10.1016/j.appet.2016.11.006 [DOI] [PubMed] [Google Scholar]
- 25. Batal M, Johnson-Down L, Moubarac J-C, et al. Quantifying associations of the dietary share of ultra-processed foods with overall diet quality in first nations peoples in the Canadian provinces of British Columbia, Alberta, Manitoba and Ontario. Public Health Nutr 2018;21:103–13. 10.1017/S1368980017001677 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Costa Louzada MLda, Martins APB, Canella DS, et al. Ultra-processed foods and the nutritional dietary profile in Brazil. Rev Saude Publica 2015;49:38. 10.1590/S0034-8910.2015049006132 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Luiten CM, Steenhuis IH, Eyles H, et al. Ultra-processed foods have the worst nutrient profile, yet they are the most available packaged products in a sample of new Zealand supermarkets. Public Health Nutr 2016;19:530–8. 10.1017/S1368980015002177 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Elliott P, Vergnaud A-C, Singh D, et al. The Airwave health monitoring study of police officers and staff in Great Britain: rationale, design and methods. Environ Res 2014;134:280–5. 10.1016/j.envres.2014.07.025 [DOI] [PubMed] [Google Scholar]
- 29. McCance RA, Widdowson E. McCance and Widdowson’s The Composition of Foods integrated dataset, 2002. Available: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/788485/McCance_Widdowson_Comp_Foods_Integrated_Dataset_User_Guide_2019__1_.pdf [Accessed 26 Nov 2020].
- 30. Chiavaroli L, Viguiliouk E, Nishi SK, et al. Dash dietary pattern and cardiometabolic outcomes: an umbrella review of systematic reviews and meta-analyses. Nutrients 2019;11. 10.3390/nu11020338 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Günther ALB, Liese AD, Bell RA, et al. Association between the dietary approaches to hypertension diet and hypertension in youth with diabetes mellitus. Hypertension 2009;53:6–12. 10.1161/HYPERTENSIONAHA.108.116665 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Gibson R, Eriksen R, Singh D, et al. A cross-sectional investigation into the occupational and socio-demographic characteristics of British police force employees reporting a dietary pattern associated with cardiometabolic risk: findings from the Airwave health monitoring study. Eur J Nutr 2018;57:2913–26. 10.1007/s00394-017-1562-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Black AE. Critical evaluation of energy intake using the Goldberg cut-off for energy intake:basal metabolic rate. A practical guide to its calculation, use and limitations. Int J Obes Relat Metab Disord 2000;24:1119–30. 10.1038/sj.ijo.0801376 [DOI] [PubMed] [Google Scholar]
- 34. Vergeer L, Veira P, Bernstein JT, et al. The calorie and nutrient density of More- versus Less-Processed packaged food and beverage products in the Canadian food supply. Nutrients 2019;11:2782–7. 10.3390/nu11112782 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Crino M, Sacks G, Dunford E, et al. Measuring the healthiness of the packaged food supply in Australia. Nutrients 2018;10:702–17. 10.3390/nu10060702 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Canella DS, Louzada MLdaC, Claro RM, et al. Consumption of vegetables and their relation with ultra-processed foods in Brazil. Rev Saude Publica 2018;52:50. 10.11606/s1518-8787.2018052000111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Baraldi LG, Martinez Steele E, Canella DS, et al. Consumption of ultra-processed foods and associated sociodemographic factors in the USA between 2007 and 2012: evidence from a nationally representative cross-sectional study. BMJ Open 2018;8:e020574. 10.1136/bmjopen-2017-020574 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Moubarac J-C, Martins APB, Claro RM, et al. Consumption of ultra-processed foods and likely impact on human health. Evidence from Canada. Public Health Nutr 2013;16:2240–8. 10.1017/S1368980012005009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Blanco-Rojo R, Sandoval-Insausti H, López-Garcia E, et al. Consumption of Ultra-Processed Foods and Mortality: A National Prospective Cohort in Spain. Mayo Clin Proc 2019;94:2178–88. 10.1016/j.mayocp.2019.03.035 [DOI] [PubMed] [Google Scholar]
- 40. Louzada MLdaC, Baraldi LG, Steele EM, et al. Consumption of ultra-processed foods and obesity in Brazilian adolescents and adults. Prev Med 2015;81:9–15. 10.1016/j.ypmed.2015.07.018 [DOI] [PubMed] [Google Scholar]
- 41. Adams J, White M. Characterisation of UK diets according to degree of food processing and associations with socio-demographics and obesity: cross-sectional analysis of UK national diet and nutrition survey (2008–12). Int J Behav Nutr Phys Act 2015;12. 10.1186/s12966-015-0317-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Schnabel L, Buscail C, Sabate J-M, et al. Association between Ultra-Processed food consumption and functional gastrointestinal disorders: results from the French NutriNet-Santé cohort. Am J Gastroenterol 2018;113:1217–28. 10.1038/s41395-018-0137-1 [DOI] [PubMed] [Google Scholar]
- 43. Rico-Campà A, Martínez-González MA, Alvarez-Alvarez I, et al. Association between consumption of ultra-processed foods and all cause mortality: sun prospective cohort study. BMJ 2019;365:l1949. 10.1136/bmj.l1949 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Hu FB. Dietary pattern analysis: a new direction in nutritional epidemiology. Curr Opin Lipidol 2002;13:3–9. 10.1097/00041433-200202000-00002 [DOI] [PubMed] [Google Scholar]
- 45. Shim J-S, Oh K, Kim HC. Dietary assessment methods in epidemiologic studies. Epidemiol Health 2014;36:e2014009. 10.4178/epih/e2014009 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjnph-2020-000225supp001.pdf (40.7KB, pdf)
Data Availability Statement
Data are available in a public, open access repository. All data are available throughout the Dementia Platform https://portal.dementiasplatform.uk/