Abstract
Background
We used the United Nations High Commissioner for Refugees Standardised Expanded Nutrition Survey data to evaluate the effect of a change in food ration on child growth in refugee camps in eastern Chad.
Methods
We compared trends of wasting and stunting prevalence over time and the association between the coexistence of being both stunted and wasted using Pearson’s χ2 test. We analysed the effect of an approximate 50% reduction in the general food distribution, with the introduction of a 20 g daily ration of small quantity lipid-based nutrient supplements given to all children aged 6–23 months, on child growth. This was done using interrupted time-series analysis to observe differences in levels and trends in mean height-for-age z-score (HAZ) and weight-for-height z-score (WHZ) over time and by age group (6–24 months and 24–59 months).
Results
Overall the prevalence of stunting and wasting decreased significantly over time. The odds of being both stunted and wasted was 1.38 higher than having one or the other condition separately (p<0.001, 95% CI=1.29 to 1.47). Trends in mean HAZ and WHZ before and after a ration change in 2014 indicate that growth had either slowed down or worsened. In the period following the ration change, children 24–59 months saw a significant decrease in mean HAZ of 0.04 per year (p=0.02, 95% CI=−0.07 to –0.01) and for the younger age group, there was a significant decrease in mean WHZ of 0.06 per year (p=0.03, 95% CI=−0.12 to –0.01).
Conclusions
The dual burden of stunting and wasting is a considerable challenge in refugee camp settings. Changes to the food distribution had adverse effects on child growth for both age groups. Broadening the scope of interventions aimed at children in camps is essential when tackling malnutrition with increased efforts essential during periods of wider food assistance shortages.
Keywords: malnutrition
What this paper adds.
What is already known?
Sparse evidence exists on stunting trends within humanitarian and protracted crises.
In crisis contexts, nutrition-specific responses typically focus on wasting and little is known about whether there is any added beneficial impact on stunting reduction.
What are the new findings?
Overall, in most camps, the nutritional situation improved for both stunting and wasting.
Small quantity lipid-based nutrients (SQ-LNS) for children 6–23 months old was not enough to sustain the previous progress in nutrition status during a period of wider food assistance cuts.
The coexistence of wasting and stunting in refugee camps supports the growing need to address all forms of malnutrition by broadening the scope of interventions aimed at children in these settings.
What do the new findings imply?
Increased efforts to support the growth of all children under 5 years are needed and relying on SQ-LNS to compensate for a large cut in the general ration is inappropriate.
Introduction
At the beginning of 2020, the number of people considered to be forcibly displaced was estimated to be around 79.5 million. Of these, around 80% had fled to countries or territories suffering from acute food insecurity and malnutrition.1 Approximately 26 million were classified as refugees, half of whom were children under the age of 18, and 20.4 million fell under the mandate of the United Nations High Commissioner for Refugees (UNHCR).1 While camps were initially intended to offer temporary shelter, around 15.7 million (77%) refugees were resident in established, long-term camps.1
UNHCR mandated refugee populations (camps and out-of-camp) are situated worldwide with the largest camps located in Africa and Asia. In established camps, mortality rates, including child and maternal mortality, have been found to be lower than those of the surrounding host population2 3 which has been attributed to increased spending on refugee populations.4 While malnutrition is no longer considered the main driver of mortality in such contexts,5 UNHCR remains concerned regarding the high prevalence of anaemia and persistently high stunting prevalence throughout all its camps, a burden echoed in the 2020 Global Nutrition Report.6
Stunting (ie, low height-for-age z-score (HAZ)) is widely used as a measure of chronic malnutrition and/or linear growth faltering in children. Changes in the prevalence of stunting in populations are interpreted as an indicator of a shift (positive or negative) in the nutrition situation due to public health and nutrition programming. Over the past decade, there has been increasing global interest towards reducing the high burden of childhood stunting in low-income and middle-income countries.7 However, according to a recent statement released by the Joint Child Malnutrition Estimates group (UNICEF/WHO/World Bank), and despite some countries making very good progress,8 stunting reduction progress overall has been ‘too slow’. Currently, the global proportion of children who are stunted (HAZ <−2) is estimated to be 21.3% which equates to 144 million children worldwide.9 Nearly half of this burden occurs in protracted and fragile contexts where roughly 24% of the world’s population lives and this is projected to have nearly doubled by 2050.10 However, in these settings, the focus of policy, research and programming remains primarily on the treatment of wasting in children under 5 years of age in order to prevent excess mortality with very little attention given to stunting.
With this in mind, and with an increasing focus on tackling malnutrition in all its forms, a number of initiatives are exploring whether stunting can be prevented or reduced through nutrition-specific preventative approaches that also target wasting. This has likely arisen through the identified commonalities in drivers that stunting and wasting are thought to share,11 12 as well as the evidence available on the coexistence of wasting and stunting at the individual level13 14 and the increased risk of becoming stunted for children who are or have been wasted.15 The 2021 Lancet series on maternal and child nutrition progress update (following from the 2013 series) reported that a substantial reduction in the burden of undernutrition could be achieved if low-income populations had access to 11 evidence-based nutrition-specific interventions that target maternal nutrition during pregnancy, infant and young child nutrition, and the management of acute malnutrition.16 17 However, evidence suggests that interventions with this narrow focus may have only a limited impact on stunting18–20 and that efforts to tackle stunting need to be focused on a number of key context-specific determinants such as those at community level21 and potentially through a multisector approach22–24 although efforts to demonstrate the effectiveness of multisector approaches have yet to provide sufficient evidence of impact. Furthermore, a recent review suggests that there could be fewer direct determinants (and, therefore, fewer effective interventions) for stunting than previously suggested and that stunting may be better considered as a robust marker of poverty and a deficient environment.7
Generally, there has been a lack of scrutiny of stunting trends within humanitarian and protracted crises and more evidence is needed to better understand potentially effective responses to tackle both stunting and wasting together in general and specifically within these contexts. By examining stunting and wasting trends over time and in specific crisis-affected areas, we can start to identify where nutrition-specific approaches are having some effect and where efficiencies in the response to both can be made.
UNHCR and its partners have been collecting data on the health and nutrition status of refugees for many years. The method most frequently used is repeated cross-sectional surveys following a survey design known as the Standardised Expanded Nutrition Survey (SENS).25 The SENS database consist mainly of data from regular repeated cross-sectional surveys based on the standardised monitoring and assessment of relief and transitions method for survey design and anthropometric assessments adapted (ie, expanded) to cover the specific multisector requirements of refugee settings. An effort to systematically collect survey reports and survey datasets for storage in a central repository started in 2009. By mid 2018, the global SENS database comprised 931 survey reports and corresponding survey datasets.
Using available data from the SENS database, this analysis first describes the trends in the prevalence of stunting and wasting in children under 5 years of age from 2010 to 2017 in 12 camps in eastern Chad. In 2014, the general food distribution (GFD) ration was reduced, due to funding constraints, and the provision of small quantity lipid based nutrient supplements (SQ-LNS) was introduced for all children aged 6–23 months. A second analysis was carried out to understand the effect of a change in the provision of food distributions on stunting and wasting prevalence. This analysis observes the growth trends of two age groups, 6–23 months (younger) and 24–59 months (older). In particular, we are interested in the nature of the effect of change and the provision of SQ-LNS on (1) the prevention of stunting, particularly in the younger age group as it is during this period of rapid normal growth that linear growth faltering mostly occurs, and (2) the reduction of the prevalence of stunting, particularly in the older age group where being stunted is more likely observed than in the younger age group, since linear growth faltering from birth is cumulative26 and thus manifests as being stunted in older children.27
Methods
Data source
Because of its geographical position, and borders with countries affected by conflicts, Chad has been host to large number of refugees for more than 10 years. In eastern Chad, the majority of refugees who came from Dafur, Sudan were mainly women and under 20 years old. The camps were relatively stable, having been set up around 2003/2004 and migration, usually occurring before the start of the rainy season (July to September) was generally low. There were no major adverse weather or climatic events reported. Malnutrition and disease occurrence were cyclical and similar for each camp: food insecurity increased from November to February, acute malnutrition from March until September (and this was generally higher in the more northerly areas) and malaria peaked in November/December. Nearly all camps had 90%–100% coverage of measles vaccination and each camp had a clinic supported by UNHCR and managed by a Non-Governmental Organisation (NGO), providing preventative and curative services for for example, diarrhoea, respiratory infections, malaria and accidents, including maternal and newborn healthcare and basic laboratory facilities. Secondary referral systems were also in place to cater for those with health issues too complicated to be managed by camp health facilities. Primary health care, infant and young child feeding programmes, treatment of moderate acute malnutrition with corn soya blend or ready-to-use supplementary foods, and the systematic treatment of children with severe acute malnutrition is available with therapeutic milks (F75, F100), resomal, amoxicillin and ready-to-use therapeutic foods was available in all camps. Water, sanitation and hygiene interventions were in place including the provision of water for drinking and for personal hygiene and the availability of latrines often at the household level.
Prior to 2014 camps had access to a full GFD providing 2100 kcal/person/day and which was estimated to provide the general energy requirements of children aged 6–23 months (900 kcal/day). However, in 2014 the GDF ration was cut, by 40%–60% compared with the full ration, prompting necessary action to enhance prevention and management of malnutrition within the camps. From 2014, UNHCR together with World Food Programme (WFP) and other partners provided a nutrition treatment and prevention package to pregnant and lactating women and to children under 5 years of age in all eastern Chad camps with a global acute malnutrition prevalence above 10%. Refugees received a GFD ration alongside a 20 g daily ration of SQ-LNS (providing 110 kcal/day) given to all children aged 6–23 months regardless of their nutrition status. Together, the reduced GFD ration and the SQ-LNS provided all essential micronutrients and between approximately 470 and 650 kcal/day, representing a 24%–48% reduction in energy from the pre-2014 ration. This continued (with minimal break in supply) until the end of 2018 (with a 6-month gap in 2015 when the WFP took over and provided 200 g/child/day of Super Cereal Plus instead of SQ-LNS).
Data analysis
Data were analysed using Stata V.14.1.28
Anthropometric z-scores were created using the package zscore06 command in Stata. According to the standard WHO cut-offs, data were considered as extreme (biologically implausible), likely the result in the errors in measurement or data entry, and coded as missing if the calculated HAZ fell outside <−6 or >+6 or outside <−5 or >+5 for the calculated WHZ.29
Binary variables for the prevalence of stunting (defined as HAZ <−2), wasting (defined as WHZ <−2) were created (1 yes, 2 no). A variable was created identifying which of the two age groups (1=6–23 months, 2=24–59 months) sampled children belonged to.
All analyses were considered significant at the 5% level where necessary.
Descriptive analyses were first carried out to observe the trends in the prevalence of stunting and wasting by age group over time in each camp and for all camps (aggregated data). We used the Pearson’s χ2 test to examine the differences in prevalence of stunting and wasting over time for each subgroup and to look at the association of the coexistence of stunting and wasting. The aggregated data were then examined using single group interrupted time-series analysis (ITSA) (box 1) to observe differences in levels and trends in mean HAZ and WHZ over time for each age group. Means were used to compare the changes in the distribution of the indices (HAZ and WHZ) rather than comparing prevalence below a given cut-off as the latter may underestimate the population affected.30 An initial observation of the data showed that an increase in the population mean HAZ/WHZ was correlated with a decrease in prevalence.31
Box 1. Examples of impact models used in interrupted time-series analysis (ITSA).
The interrupted time-series analysis (ITSA) is a quasi-experimental method to establish the likely causal effect of an intervention. The ITSA design offers an examination of preintervention and postintervention changes in levels and trends or slopes of an outcome variable using a minimum of three variables: the outcome at time (t) (Yt) and the time since the start of the study (T) in units representing data frequency, for example, months or years and a dummy variable indicating the preintervention (coded 0) and postintervention (coded 1) periods. A standard segmented model, where segments represent different intercept and slope coefficients for the preintervention and postintervention periods, is used:
where β0 estimates the base level of the outcome at the beginning of the series (T), β1 estimates the underlying preintervention trend (the base trend of the outcome over time), β2 estimates the change in level following the intervention and β3 estimates the change in trend in the postintervention period (using the interaction between time and intervention).
Some examples of impact models are illustrated in the figure below taken from Bernal et al.37 The dashed vertical line represents the point in time an intervention was implemented. While these examples indicate specific examples, it is worth pointing out that impacts may manifest as combinations of these patterns.
Changes in the levels and slopes of the main outcome variables (mean HAZ and WHZ) were assessed using the Stata ITSA command, using OLS regression with Newey-West standard errors and a lag of 1 (to adjust for potential autocorrelation between concurrent time points).38 This allowed a comparison of the change in levels and slopes before the intervention and during the postintervention period between the two age groups. Data missing for the 2 years (2012 and 2014) were imputed using linear interpolation for each camp, in order to run the Stata ITSA command. In the pooled analysis, camps were treated as weighted equally, regardless of population size, since this analysis is concerned more with the evaluation of the ration change itself in the context it occurred rather than generalisability.

(A) Level change; (B) Slope change; (C) Level and slope change; (D) Slope change following a lag; (E) Temporary level change; (F) Temporary slope change leading to a level change.
Patient and public involvement
Due to the nature of this secondary research, patients or the public were not involved in the design, conduct, reporting or dissemination plans of our research.
Results
Data were available for 12 refugee camps in eastern Chad over six different years between 2010 and 2017 resulting in a raw dataset with 39 231 records of children 6–59 months (table 1). Just over a third (35.1%) of the sample included children aged 6–23 months and 49.6% were girls. A small number of children with missing data on both height and weight (n=615) were dropped from the analysis. There were 14 children with data missing on weight and 31 with data missing on height. Sixty-seven data points were recorded as missing with non-plausible HAZ and 55 for non-plausible WHZ.
Table 1.
Number of children aged 6–59 months by camp and year in SENS surveys at eastern Chad camps
| Camp | Year | Total | |||||
| 2010 | 2011 | 2013 | 2015 | 2016 | 2017 | ||
| Amnabak | 732 | 504 | 469 | 403 | 371 | 571 | 3050 |
| Bredjing | 618 | 380 | 523 | 505 | 500 | 650 | 3176 |
| Djabal | 512 | 589 | 565 | 465 | 804 | 681 | 3616 |
| Farchana | 665 | 481 | 489 | 524 | 509 | 557 | 3225 |
| Gaga | 648 | 477 | 478 | 548 | 519 | 568 | 3238 |
| Gozamer | 787 | 601 | 549 | 466 | 776 | 645 | 3824 |
| Iridimi | 688 | 478 | 511 | 483 | 606 | 519 | 3285 |
| Kounoungo | 566 | 516 | 582 | 475 | 505 | 584 | 3228 |
| Mile | 641 | 446 | 503 | 438 | 543 | 577 | 3148 |
| Oure Cassoni | 611 | 512 | 524 | 459 | 433 | 533 | 3072 |
| Touloum | 615 | 472 | 525 | 531 | 520 | 569 | 3232 |
| Treguine | 685 | 492 | 472 | 485 | 479 | 524 | 3137 |
| Total | 7768 | 5948 | 6190 | 5782 | 6565 | 6978 | 39 231 |
SENS, Standardised Expanded Nutrition Survey.
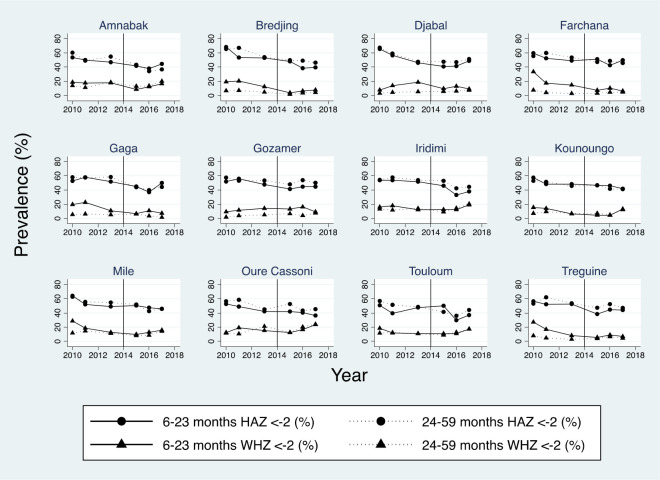
The trends for the prevalence of being stunted and wasted over time by age group and for each camp are shown in figure 1. Nearly all camps showed a significant decrease in stunting and wasting over time. The exceptions being Amnabak and Kounoungo (stunting 6–23 months); Gozamer (stunting 24–59 months); Amnabak, Gozamer, Iridimi and Touloum (wasting 6–23 months) and Djabal (wasting 24–59 months).
Figure 1.
Trend in stunting and wasting prevalence by camp and age group. HAZ, height-for-age z-score; WHZ, weight-for-height z-score
Nearly half of all children (49.8%) in the pooled database were stunted, 10.6% were wasted and 6.0% were both stunted and wasted. The prevalence of children who were stunted was higher in the age group 24–59 months compared with the younger group (50.8% vs 48.2% (p<0.001, χ2=24.0)), the prevalence of children who were wasted was higher in the younger age group: 13.9% vs 8.8% (p<0.001, χ2=241.9).
Overall, the prevalence of children classified as stunted or wasted decreased significantly over time. On average, there was a 13.0 percentage point decrease between 2010 and 2017, from 57.7% to 44.7% (p<0.001, χ2=459.9) which equates to an annual average rate of reduction of 4.1%.32 The prevalence of wasting decreased from 12.3% to 11.8% (p<0.001, χ2=103.8). The odds of being both stunted and wasted was 1.38 higher than not (p<0.001, 95% CI=1.29 to 1.47).
Table 2 illustrates that for each age group the prevalence of being stunted or wasted significantly decreased over time except in the 24–59 month age group which showed a significant 2.8 percentage points increase in the prevalence of being wasted.
Table 2.
Prevalence of stunting and wasting over time by age group for all camps combined
| 2010 | 2011 | 2013 | 2015 | 2016 | 2017 | Total % (n) | P value* | |
| 6–23 months (HAZ <−2%) |
57.0 | 52.0 | 48.7 | 45.3 | 40.5 | 43.4 | 48.2 (n=13 752) |
<0.001 |
| 24–59 months (HAZ <−2 %) |
58.1 | 56.5 | 51.8 | 47.6 | 44.8 | 45.4 | 50.8 (n=25 448) |
<0.001 |
| 6–23 months (WHZ <−2 %) |
18.9 | 16.6 | 13.0 | 8.8 | 11.6 | 12.5 | 13.9 (n=13 745) |
<0.001 |
| 24–59 months (WHZ <−2 %) |
8.6 | 8.3 | 8.9 | 7.0 | 8.2 | 11.4 | 8.8 (n=25 441) |
<0.001 |
*P value for χ2 statistic.
HAZ, height-for-age z-score; WHZ, weight-for-height z-score.
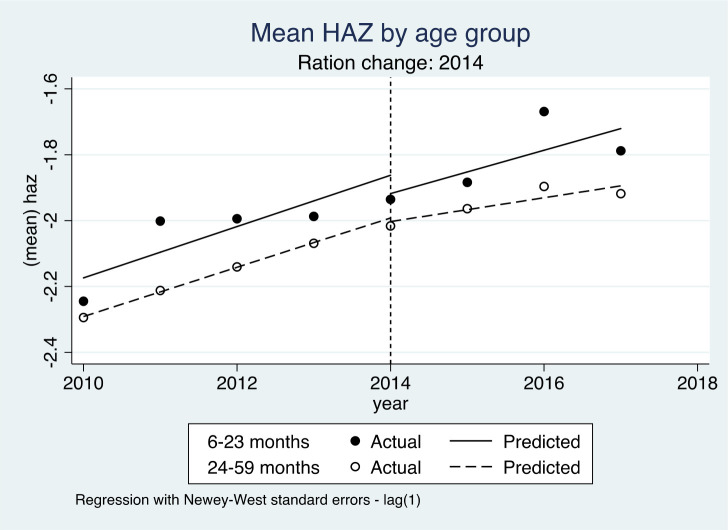
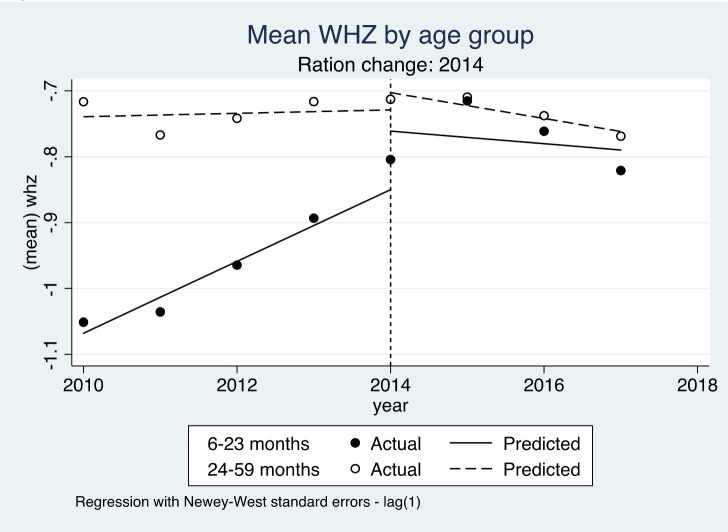
The results for the change in levels and slopes for mean HAZ and WHZ are shown in figures 2 and 3. The solid lines represent the predicted linear trends, or slopes, for children aged 6–23 months and the dashed lines for children aged 24–59 months. The vertical dotted line represents the point in time when the ration change started with segmented predicted linear trends, or slopes, either side representing the periods before and after 2014.
Figure 2.
Interrupted time-series for mean HAZ by age group. HAZ, height-for-age z-score
Figure 3.
Interrupted time-series for mean WHZ by age group references. WHZ, weight-for-height z-score
For HAZ, there were no significant changes in terms of changes in level (both age groups) or slope (younger age group). However, the older age group saw a significant difference in the post-2014 slope compared with the pre-2014 slope with a post-2014 decrease of mean HAZ of 0.04 per year (p=0.02, 95% CI=−0.07 to –0.01) (figure 2).
For the younger age group, figure 3 shows a significant annual WHZ increase of 0.05 (p=0.002, 95% CI=0.03 to 0.08) during the pre-2014 period. However, this was followed by a significant post-2014 decrease in WHZ of 0.06 (p=0.03, 95% CI=−0.12 to –0.01). In fact, both age groups saw a similar negative trend in mean WHZ during the post-2014 period compared with the pre-2014 trend.
Discussion
The overall decline in the prevalence of stunting/improvement in mean HAZ in both age groups and in the prevalence of wasting/improvement in mean WHZ in the younger age group in the camps is encouraging. In light of the ITSA results, however, the 2014 GFD ration change was associated with a decrease in the trend for improvement of stunting in the older age group and of wasting for both age groups. Given that all of the children in the younger age group and some of the children in the older age group would have been affected by the ration change this suggests that the change was not beneficial for growth.
This analysis shows that the dual burden of wasting and stunting is a significant challenge in refugee camp settings. Given the increasing evidence of the higher risk of mortality in children who are both stunted and wasted,33 but also for increasing progress towards the global Sustainable Development Goal (SDG) 2.2, it would make sense to broaden the scope of the interventions aimed at children in camps. Although it is not possible to be more specific here without knowing more about the causes of either, it is likely that, due to the different aetiologies and drivers of both wasting and stunting, multiple approaches would be needed. More evidence is needed to understand the overlaps/common drivers between stunting and wasting in these settings in order to develop a more integrated nutrition service. This is not only applicable here but also for increasing progress towards SDG 2.2 in addressing all forms of malnutrition. Recent efforts have been made to understand multiple approaches for addressing not just different forms of undernutrition but also overnutrition and diet-related non-communicable diseases as in double-duty approaches34 and triple-duty approaches including climate change35 by determining common drivers.
Limitations
Evidence from this study needs to be interpreted carefully since there are a number of limitations. The analyses are relatively simple and do not include a range of factors known or suspected to be associated with wasting and/or stunting. Causality cannot be inferred. The SENS data come from repeated cross-sectional surveys (ie, the same data but from a different sample of children each time), so without knowing more about the context within which these populations were under at the time of each survey, it is unclear as to whether the changes in growth observed were due to the nutrition supplementation or rather to other external factors.
With repeated cross-sectional surveys it is also not possible to look at individual changes in linear and ponderal growth over time nor to use individuals as their own controls. The lack of a control group questions the validity of the results36 although the ITSA design is considered a good front-runner for further, more robust study designs. Knowledge around intrahousehold sharing of food and rations, including the SQ-LNS, was lacking. Without a full understanding of the context in which the data come from, it is difficult to then make a full interpretation of the results although hypotheses can be drawn.
Conclusion
The cuts to the GFD ration in 2014 may have adversely affected young children’s nutritional status even though SQ-LNS was provided as a supplement. This suggests that SQ-LNS did not sufficiently offset the reduction in the GFD or the amount of it that the child received. In fact, the progress seen before 2014 slowed or even stopped and this questions what role the blanket SQ-LNS distribution had as a preventative intervention. For example, what would have happened to the anthropometric status of these children had there been no blanket distribution of SQ-LNS? Would further declines in anthropometric status, especially stunting, have occurred? Would it have been a better use of resources to support the GFD ration rather than providing the more expensive SQ-LNS? Without the specific data we can only hypothesise what the alternative outcomes may have been. What we may surmise, however, is that a targeted intervention for these young children was clearly insufficient to compensate for the shortfalls of wider food assistance in sustaining the previous progress in nutritional status.
Footnotes
Funding: This study was funded by Irish Aid (HQPU/2019/ENN).
Competing interests: None declared.
Provenance and peer review: Not commissioned; internally peer reviewed.
Data availability statement
Data are available upon reasonable request.
Ethics statements
Patient consent for publication
Not required.
References
- 1. UNHCR . Figures at glance, 2020. Available: https://www.unhcr.org/pages/49c3646c11.html [Accessed 3 Jul 2020].
- 2. Salama P, Spiegel P, Talley L, et al. Lessons learned from complex emergencies over past decade. Lancet 2004;364:1801–13. 10.1016/S0140-6736(04)17405-9 [DOI] [PubMed] [Google Scholar]
- 3. Hynes M, Sakani O, Spiegel P, et al. A study of refugee maternal mortality in 10 countries, 2008-2010. Int Perspect Sex Reprod Health 2012;38:205–13. 10.1363/3820512 [DOI] [PubMed] [Google Scholar]
- 4. Tan TM, Spiegel P, Haskew C, et al. Does spending on refugees make a difference? A cross-sectional study of the association between refugee program spending and health outcomes in 70 sites in 17 countries. Confl Health 2016;10:28. 10.1186/s13031-016-0095-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Hershey CL, Doocy S, Anderson J, et al. Incidence and risk factors for malaria, pneumonia and diarrhea in children under 5 in UNHCR refugee camps: a retrospective study. Confl Health 2011;5:24. 10.1186/1752-1505-5-24 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. 2020 global nutrition report: action on equity to end malnutrition. Bristol, UK: Development Initiatives; 2020.
- 7. Leroy JL, Frongillo EA. Perspective: what does stunting really mean? A critical review of the evidence. Adv Nutr 2019;10:196–204. 10.1093/advances/nmy101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Bhutta ZA, Akseer N, Keats EC, et al. How countries can reduce child stunting at scale: lessons from exemplar countries. Am J Clin Nutr 2020;112:894S–904. 10.1093/ajcn/nqaa153 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. UNICEF, World Health Organization, International Bank for Reconstruction and Development/The World Bank . Levels and trends in child malnutrition: key findings of the 2020 edition of the Joint Child Malnutrition Estimates. Geneva: World Health Organization, 2020. [Google Scholar]
- 10. OECD . States of fragility, 2018. Available: https://www.oecd.org/dac/conflict-fragility-resilience/listofstateoffragilityreports.htm [Accessed 28 Sep 2020].
- 11. Briend A, Khara T, Dolan C. Wasting and stunting--similarities and differences: policy and programmatic implications. Food Nutr Bull 2015;36:S15–23. 10.1177/15648265150361S103 [DOI] [PubMed] [Google Scholar]
- 12. Martorell R, Young MF. Patterns of stunting and wasting: potential explanatory factors. Adv Nutr 2012;3:227–33. 10.3945/an.111.001107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Angood C, Khara T, Dolan C, et al. Research priorities on the relationship between wasting and stunting. PLoS One 2016;11:e0153221. 10.1371/journal.pone.0153221 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Global Nutrition Report: Shining a light to spur action on nutrition. Development Initiatives, Chapter 2, ‘The burden of malnutrition’, 2018. Available: https://globalnutritionreport.org/reports/global-nutrition-report-2018/burden-malnutrition [Accessed 3 Jul 2020].
- 15. Schoenbuchner SM, Dolan C, Mwangome M, et al. The relationship between wasting and stunting: a retrospective cohort analysis of longitudinal data in Gambian children from 1976 to 2016. Am J Clin Nutr 2019;110:498–507. 10.1093/ajcn/nqy326 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Victora CG, Christian P, Vidaletti LP, et al. Revisiting maternal and child undernutrition in low-income and middle-income countries: variable progress towards an unfinished agenda. Lancet 2021;397:1388–99. 10.1016/S0140-6736(21)00394-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Bhutta ZA, Das JK, Rizvi A, et al. Evidence-based interventions for improvement of maternal and child nutrition: what can be done and at what cost? Lancet 2013;382:452–77. 10.1016/S0140-6736(13)60996-4 [DOI] [PubMed] [Google Scholar]
- 18. Black RE, Victora CG, Walker SP, et al. Maternal and child undernutrition and overweight in low-income and middle-income countries. Lancet 2013;382:427–51. 10.1016/S0140-6736(13)60937-X [DOI] [PubMed] [Google Scholar]
- 19. Dewey KG, Adu-Afarwuah S. Systematic review of the efficacy and effectiveness of complementary feeding interventions in developing countries. Matern Child Nutr 2008;4(Suppl 1):24–85. 10.1111/j.1740-8709.2007.00124.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Hossain M, Choudhury N, Adib Binte Abdullah K, et al. Evidence-based approaches to childhood stunting in low and middle income countries: a systematic review. Arch Dis Child 2017;102:903–9. 10.1136/archdischild-2016-311050 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Roth DE, Krishna A, Leung M, et al. Early childhood linear growth faltering in low-income and middle-income countries as a whole-population condition: analysis of 179 demographic and health surveys from 64 countries (1993-2015). Lancet Glob Health 2017;5:e1249–57. 10.1016/S2214-109X(17)30418-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Bergeron G, Castleman T. Program responses to acute and chronic malnutrition: divergences and convergences. Adv Nutr 2012;3:242–9. 10.3945/an.111.001263 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Alderman HH, Elder LK, Goyal A. Improving nutrition through multisectoral approaches (English). Washington, DC: World Bank Group, 2013. http://documents.worldbank.org/curated/en/625661468329649726/Improving-nutrition-through-multisectoral-approaches [Google Scholar]
- 24. Heidkamp RA, Piwoz E, Gillespie S, et al. Mobilising evidence, data, and resources to achieve global maternal and child undernutrition targets and the sustainable development goals: an agenda for action. Lancet 2021;397:1400–18. 10.1016/S0140-6736(21)00568-7 [DOI] [PubMed] [Google Scholar]
- 25. UNHCR standardised expanded nutrition survey (SENS) guidelines for refugee populations, version 3. office of the United nations high commissioner for refugees, Geneva, Switzerland, 2019. Available: http://sens.unhcr.org/ [Accessed 5 Jul 2020].
- 26. Stein AD, Wang M, Martorell R, et al. Growth patterns in early childhood and final attained stature: data from five birth cohorts from low- and middle-income countries. Am J Hum Biol 2010;22:353–9. 10.1002/ajhb.20998 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. WHO Technical Report Series 854 . Physical status: the use and interpretation of anthropometry. Report of a WHO expert Committee. Geneva: World Health Organisation, 1995. [PubMed] [Google Scholar]
- 28. StataCorp LLC, College Station, TX, USA.
- 29. WHO . Child growth standards: length/height-for-age, weight-for-age, weight-for-length, weight-for-height and body mass index-for-age: methods and development. Geneva: WHO, 2006. [Google Scholar]
- 30. Perumal N, Bassani DG, Roth DE. Use and misuse of stunting as a measure of child health. J Nutr 2018;148:311–5. 10.1093/jn/nxx064 [DOI] [PubMed] [Google Scholar]
- 31. Rose G, Day S. The population mean predicts the number of deviant individuals. BMJ 1990;301:1031–4. 10.1136/bmj.301.6759.1031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. UNICEF . Technical note: how to calculate average annual rate of reduction (AARR) of underweight prevalence, 2007. Available: https://data.unicef.org/resources/technical-note-calculate-average-annual-rate-reduction-aarr-underweight-prevalence/ [Accessed 3 Jul 2020].
- 33. Myatt M, Khara T, Schoenbuchner S, et al. Children who are both wasted and stunted are also underweight and have a high risk of death: a descriptive epidemiology of multiple anthropometric deficits using data from 51 countries. Arch Public Health 2018;76:1–11. 10.1186/s13690-018-0277-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Hawkes C, Ruel MT, Salm L, et al. Double-duty actions: seizing programme and policy opportunities to address malnutrition in all its forms. Lancet 2020;395:10218:142–55. Erratum in: Lancet 2020;395(10221):338. 10.1016/S0140-6736(19)32506-1 [DOI] [PubMed] [Google Scholar]
- 35. Swinburn BA, Kraak VI, Allender S, et al. The global Syndemic of obesity, undernutrition, and climate change: the Lancet Commission report. Lancet 2019;393:791–846. Erratum in: Lancet 2019: 393(10173):746. 10.1016/S0140-6736(18)32822-8 [DOI] [PubMed] [Google Scholar]
- 36. Linden A. Challenges to validity in single-group interrupted time series analysis. J Eval Clin Pract 2017;23:413–8. 10.1111/jep.12638 [DOI] [PubMed] [Google Scholar]
- 37. Bernal JL, Cummins S, Gasparrini A. Interrupted time series regression for the evaluation of public health interventions: a tutorial. Int J Epidemiol 2017;46:348–55. 10.1093/ije/dyw098 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Linden A. Conducting interrupted time-series analysis for single- and multiple-group comparisons. The Stata Journal 2015;15:480–500. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data are available upon reasonable request.