PURPOSE:
The presence of caregivers or companions during clinical encounters influences the dynamics and outcomes of the encounters. Most prior studies of companions in clinical encounters focus on non-Hispanic White patients. However, there is generally lower-quality patient-physician communication during encounters with Black patients; these communication differences may contribute to racial health disparities. The purpose of the present study was to examine effects of the presence and active participation of companions on encounters between Black patients with cancer and non-Black oncologists.
METHODS:
This was a secondary analysis of data collected during a larger intervention study. Participants were Black patients with breast, colon, or lung cancer who had a treatment-discussion encounter with a participating non-Black medical oncologist. Video recordings of encounters were coded for patient, companion, and oncologist communication. After the encounter, patients reported perceptions of the recommended treatment; patients and oncologists reported perceptions of each other.
RESULTS:
Data from 114 patients and 19 oncologists were included in analyses. Only 47% of patients brought a companion to the encounter. Oncologists spent more time with accompanied Black patients, used more patient-centered communication with them, and perceived them as having more social support compared with unaccompanied Black patients. Oncologists reported that accompanied patients asked more questions. When companions participated more actively in the encounter, oncologists used more patient-centered communication.
DISCUSSION:
Bringing a companion to oncology appointments may be beneficial to Black patients because oncologists spend more time with patients, use more patient-centered communication, and perceive patients more positively, all of which may ultimately improve patient health and well-being outcomes.
INTRODUCTION
Although about 13% of the population of the United States identifies as Black or African American, only about 5% of practicing physicians are Black.1 The percentage of Black oncologists is even lower,2 and underrepresentation is likely to be an issue in oncology for the foreseeable future.2 Although patients generally prefer to see providers of similar racial and ethnic backgrounds,3 because of the shortage of Black oncologists, the vast majority of oncology encounters for Black patients with cancer are with a non-Black oncologist.
There tends to be lower-quality patient-physician communication in Black patients' clinical encounters, especially when the physician is not Black.4,5 Black patients tend to ask fewer questions6 and participate less actively in decision making7; physicians engage in less patient-centered communication8 and convey less information during encounters with Black patients.5 Black patients also tend to have less positive views of their non-Black physicians, and non-Black physicians tend to have less positive views of their Black patients.4,9
These differences in communication may be an important contributing factor in racial health disparities.10 Street et al's Ecological Theory of Patient-Centered Communication11 (ETPCC) posits that communication between providers, patients, and family members impacts important proximal and intermediate outcomes, such as patient understanding of and commitment to treatment. This communication ultimately impacts patient health outcomes—such as emotional well-being, pain control, and functional ability—both indirectly, through these proximal and intermediate outcomes, and directly.11,12
Importantly, Hoerger et al12 state that the ETPCC “...suggests that clinical communication research should address multiple levels, namely the mutual interactions between physicians and patients as well as the social and clinical contexts…” (p. 3). One key contextual factor is who is present during the encounter beyond the patient and provider: Many patients with cancer bring a family caregiver or other companion to their oncology appointments,13,14 and companions' presence can influence the dynamics and outcomes of an encounter. Companions serve a variety of helpful functions. They may help provide history and other information to providers,15 ask questions and express concerns,16 help patients make decisions,17 provide emotional support to patients,18 and help patients remember information and instructions given during the encounter.18 Conversely, companions may also have their own informational and psychosocial needs and thus divide the provider's attention, and companions may even impede patient care in some cases.16,19
Past work has found that patients are more satisfied with clinical encounters and their medical care when a companion is present.13,20 However, few studies have examined other effects of bringing a companion to clinical encounters.14 Findings of the few existing studies are mixed, with several reporting negative outcomes associated with accompanied encounters, such as decreased patient understanding of their medical problems21 or less positive talk and partnership building from providers.22 Overall, however, research supports the idea that bringing a companion to clinical encounters is beneficial to patients.14,23 For example, when a patient is accompanied, the provider tends to be more satisfied with the encounter,24 provide more information,5,25 and better understand the patient's concerns26; accompanied patients report better understanding of the information they are given,26 and the encounter is longer.25
Even fewer studies have specifically focused on the impact of companions on oncology encounters. It is particularly important to understand this impact in an oncology setting because patients with cancer are more frequently accompanied to encounters compared with patients in other settings, and several of the reported negative effects of bringing a companion are not consistently observed in oncology encounters.14
Furthermore, most prior studies examining companions' influence on encounters have focused on non-Hispanic White patients. This lack of research on Black patients' encounters is an important gap in the literature. As noted earlier, patient-provider interactions are affected by race, with lower-quality communication in interactions between Black patients and their providers. Additionally, Black patients are significantly less likely than White patients to bring a companion to oncology encounters—notably, one study found that 40% of Black patients with cancer were accompanied, compared with 86% of White patients.6
The present study aimed to examine the effects of the presence and active participation of a companion on encounters between Black patients with cancer and their oncologists, guided by key components of the ETPCC. Specifically, we examined the effect of companions on patient and oncologist communication behaviors and on key intermediate outcomes from Street et al's ETPCC,11 including patient perceptions of treatment and oncologist perceptions of the patient. We hypothesized that, when patients were accompanied, they would participate more actively during the encounter; oncologists would exhibit more patient-centered communication and spend more time in the encounter; patients would have greater confidence in the recommended treatment; and oncologists would anticipate better patient adherence and perceive patients to have more social support. For accompanied patients, we expected to see parallel effects when companions participated more actively in the encounter—that is, more patient active participation, more patient-centered communication, longer encounters, greater confidence in treatment, better anticipated adherence, and more perceived social support.
METHODS
The present study is a secondary, cross-sectional analysis of data from a larger randomized controlled trial.27 The parent trial tested the effects of a question prompt list intervention on patient active participation and other communication outcomes during encounters of Black patients with cancer with their oncologists. See Eggly et al27 for additional details and the CONSORT diagram.
Participants
Participants were patients with cancer and their medical oncologists at two cancer hospitals in Detroit, MI, USA. Inclusion criteria for patients included: (1) self-identified as Black, African American, or Afro-Caribbean; (2) diagnosis of breast, colon, or lung cancer; (3) age 30-85 years; and (4) had an upcoming appointment with a participating oncologist for an initial discussion of cancer treatment. Medical oncologists were eligible to participate if they treated patients with breast, colon, or lung cancer at one of the data collection sites. Although oncologist race was not an exclusion criterion, no participating oncologists self-identified as Black; therefore, all encounters in the present study were between Black patients and non-Black oncologists.
Procedure
Study procedures were approved by Institutional Review Boards at Wayne State University and both cancer hospitals where participants were recruited (protocol No. 1112010429); all participants provided informed consent. Patients were approached up to 2 weeks before a scheduled treatment-discussion appointment with a participating oncologist. Enrolled patients were randomly assigned to a control group or one of two intervention groups (one group received a question prompt list booklet, and the other received a question prompt list booklet plus a communication coach). Those assigned to either intervention group received the intervention on the same day, immediately following random assignment. Fifteen patients were not randomly assigned because of an error in the random assignment software (n = 2) or because the patient's diagnosis indicated that the oncologist was unlikely to discuss medical treatment during the encounter (eg, ductal carcinoma in situ; n = 13). These patients were assigned to the control group.
The oncology encounter occurred within 2 weeks of patient enrollment. Encounters were video recorded, and recordings were coded by trained observers. See Eggly et al27 for additional details about coding procedures and inter-rater reliability. Immediately after the encounter, patients and oncologists each completed self-report questionnaires about their perceptions of the encounter and of each other.
Measures
Observed communication behaviors.
Oncologist patient-centered communication (observer-coded).
Using a Likert-type scale ranging from 1 (strongly disagree) to 5 (strongly agree), trained observers rated their global agreement with 12 statements related to the oncologist's communication during the encounter in three areas9: informativeness (eg, The doctor thoroughly explained everything to the patient), supportiveness (eg, The doctor tried to reassure and comfort the patient), and partnership building (eg, The doctor asked for the patient's opinion about what to do about their condition). Ratings were averaged to create a single variable, oncologist patient-centered communication (observer-coded), with higher scores representing more patient-centered communication.
Patient active participation (observer-coded).
Using a Likert-type scale ranging from 1 (strongly disagree) to 5 (strongly agree), trained observers rated their global agreement with seven statements related to the patient's behavior during the encounter9: (1) The patient asked for greater detail; (2) The patient asked for treatment recommendations; (3) The patient asked questions; (4) The patient offered their opinion of the treatment; (5) The patient stated their preferences; (6) The patient expressed concerns; and (7) The patient expressed opinions. Ratings were averaged to create a single variable, patient active participation (observer-coded), with higher scores representing more patient active participation.
Companion active participation (observer-coded).
The same coding system used for patient active participation9 was applied to companion active participation, with companion being substituted for patient in the seven statements rated by coders. Ratings were averaged to create a single variable, companion active participation (observer-coded), with higher scores representing higher levels of companion active participation.
Oncologist time spent with the patient (observer-coded).
Trained observers recorded the number of minutes that the oncologist spent in the consult room with the patient.
Postencounter perceptions.
Oncologist patient-centered communication (patient-reported).
Immediately after the encounter, patients reported their perceptions of how patient-centered the oncologist's communication was using a 14-item measure developed and validated in previous work.28 Example items include How well do you think your doctor understood you today? and To what extent did the doctor ask about your goals for treatment? Responses were given a Likert-type scale ranging from 1 (not at all) to 4 (completely) and then averaged to create a single variable, oncologist patient-centered communication (patient-reported), with higher scores representing more perceived patient-centered communication.
Patient active participation (oncologist-reported).
Immediately after the encounter, oncologist perceptions of one element of patient active participation, question asking, were assessed with a single item: The patient asked few questions. Oncologists rated their agreement on a Likert-type scale ranging from 1 (strongly disagree) to 5 (strongly agree). This item was reverse-scored so that higher scores represented more perceived patient active participation.
Confidence in the recommended treatment (patient-reported).
The patient's confidence in the recommended treatment was assessed with a single item: How sure or unsure are you that this treatment is the best treatment for your cancer? Patients responded on a scale of 1 (extremely unsure) to 6 (extremely sure), with higher scores representing greater confidence that the recommended treatment was the best treatment for them.
Anticipated patient adherence (oncologist-reported).
Oncologist perceptions of how likely the patient was to follow treatment recommendations were assessed with two items: The patient is likely to follow the medical advice given and The patient is likely to follow the treatment regimen. Oncologists rated their agreement on a Likert-type scale ranging from 1 (strongly disagree) to 5 (strongly agree). Responses were averaged to create a single variable, anticipated patient adherence (oncologist-reported), with higher scores indicating that the oncologist anticipated better adherence from the patient.
Perceptions of patient social support (oncologist-reported).
Oncologist perceptions of patient social support were assessed with a single item: The patient lacks social support. Oncologists rated their agreement on a Likert-type scale ranging from 1 (strongly disagree) to 5 (strongly agree). This item was reverse-scored so that higher scores represented higher perceived levels of patient social support.
Statistical Methods
To account for the nested nature of the data (patients within oncologists), a series of multilevel models were conducted: First, the presence or absence of a companion was modeled as a predictor of patient and oncologist outcome variables—specifically, patient and oncologist communication behavior, oncologist time spent with the patient, patient confidence in the recommended treatment, and oncologist perceptions of patient adherence and social support. Second, for accompanied patients, companions' active participation was modeled as a predictor of the same patient and oncologist outcome variables. Maximum likelihood estimation was used to handle missing data, which allows the use of all available data from all variables in a model and produces unbiased parameter estimates under the missing-at-random assumption.29 To control for any effects of the intervention that was evaluated in the parent study, all models included intervention group as a control variable. Analyses were conducted using Mplus version 7.30
RESULTS
Descriptive Statistics
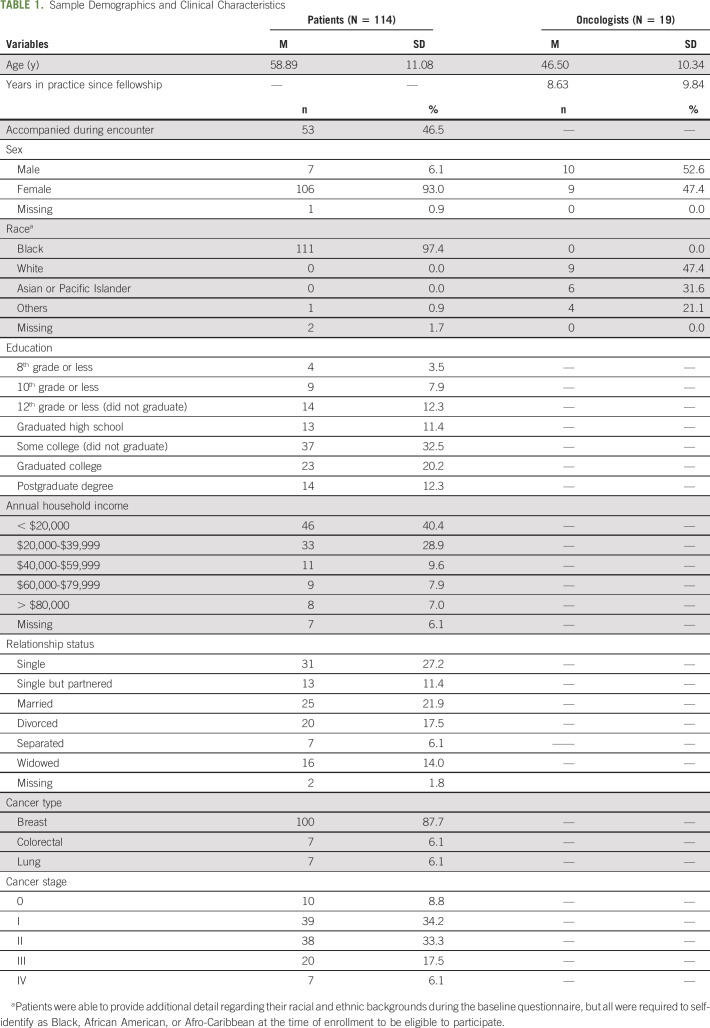
A total of 137 Black patients with cancer and 21 non-Black medical oncologists were enrolled in the parent study and provided at least some data. Of these, 114 patients and 19 oncologists provided data during the encounter and in postencounter questionnaires and were included in analyses. Only 53 patients (46.5%) brought a companion to the encounter; this is roughly in line with findings in the previous work6 that about 40% of Black patients (v 86% of White patients) are accompanied to oncology encounters. Of these 53 accompanied patients, data on companion active participation were only available for 48 patients. On average, patients were 59 years old and the vast majority were female (93.0%). Most had breast cancer (87.7%), with the remainder having colorectal or lung cancer (6.1% each). Most oncologists self-identified as White (47.4%) or Asian or Pacific Islander (31.6%), and 47.4% were female. Table 1 shows additional demographic information of patients and oncologists and patient clinical characteristics. Table 2 shows descriptive statistics for key predictor and outcome variables.
TABLE 1.
Sample Demographics and Clinical Characteristics
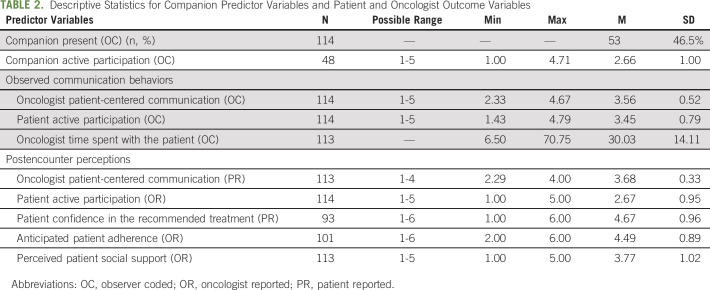
TABLE 2.
Descriptive Statistics for Companion Predictor Variables and Patient and Oncologist Outcome Variables
Effects of Companions on Encounters.
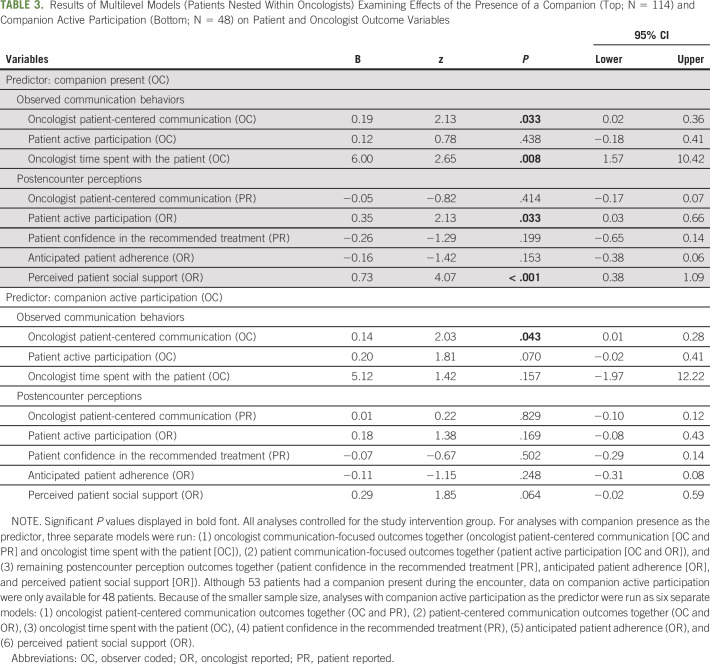
Table 3 shows the results of the multilevel models.
TABLE 3.
Results of Multilevel Models (Patients Nested Within Oncologists) Examining Effects of the Presence of a Companion (Top; N = 114) and Companion Active Participation (Bottom; N = 48) on Patient and Oncologist Outcome Variables
Effects of companion presence.
Observers did not rate accompanied patients as participating more actively during the encounter, but oncologists perceived accompanied patients as participating more actively—that is, asking more questions—than unaccompanied patients. There were no differences between accompanied and unaccompanied patients in how patient-centered they perceived the oncologist's communication to be; however, oncologists were rated by observers as engaging in significantly more patient-centered communication with accompanied patients. Finally, oncologists spent significantly more time—six additional minutes on average—with patients when a companion was present.
There were no differences between accompanied and unaccompanied patients in their confidence in the recommended treatment or level of patient adherence anticipated by oncologists. However, unsurprisingly, providers perceived accompanied patients to have significantly greater social support.
Effects of companion active participation.
When observers rated companions as participating more actively in the encounter, they also rated oncologists' communication as more patient centered. No other statistically significant effects of companion active participation were observed on communication behaviors or postencounter perceptions; however, a trend was seen for observer-coded patient active participation and oncologist perceptions of patient social support.
DISCUSSION
Past research has demonstrated that there tends to be lower-quality patient-physician communication during clinical encounters with Black patients,4,5 and these communication differences can contribute to racial health disparities.10 One important factor influencing the dynamics and outcomes of these encounters is whether the patient brings a companion. However, most prior studies of the impact of a companion on clinical encounters were conducted in samples of non-Hispanic White patients. The present study examined the effects of the presence and active participation of companions on treatment-planning encounters between Black patients with cancer and their non-Black oncologists.
Overall, findings suggest that, for Black patients, having a companion present positively impacts some aspects of non-Black oncologists' behavior during the encounter and their perceptions of the patient. Specifically, when a companion was present, oncologists were observed to engage in more patient-centered communication; oncologists were also observed to engage in more patient-centered communication when companions participated more actively in the encounters. These findings are particularly important, as patient-centered communication has been linked with improved outcomes, such as patient satisfaction and emotional well-being,31,32 improved medical outcomes,33 and reductions in certain types of medical expenditures.34 Although companions' presence and active participation were associated with observed patient-centered communication, they were not associated with patient report of patient-centered communication. However, some previous work35 has found weak correlations between observer coding and patient report, and that observer coding of patient-centered communication was associated with important outcomes (eg, patient trust in the provider) that were not associated with patient report of patient-centered communication.
The results also revealed that oncologists spent more time with accompanied Black patients—six additional minutes, which represents about a 20% increase in the average encounter length. Although longer encounters may present logistical challenges for providers and clinics, they present an opportunity for more information to be exchanged, and they are associated with many positive outcomes, including more patient-centered communication36 and attention to patients' behavioral and psychosocial issues,37 as well as increased patient satisfaction38 and participation in medical decision making.39
Of particular interest are results related to non-Black oncologists' perceptions of Black patients. Oncologists reported that accompanied patients participated more actively in the encounter and had more social support compared with unaccompanied patients. These findings are particularly noteworthy because research on implicit bias has shown that healthcare providers tend to have more negative perceptions of Black patients40; these negative perceptions are related to worse outcomes, including lower-quality communication and more negative patient perceptions of the provider and treatment recommendations.40 The results of the present study present a potential avenue for improving non-Black oncologist perceptions of Black patients—that is, encouraging patients to bring companions to appointments.
Oncologist perceptions of patients are also important because they may have clinical implications, such as influencing treatment recommendations or the way treatment options are presented to patients. For example, if a particular treatment being considered would require substantial support or caregiving for the patient, an oncologist may (intentionally or unintentionally) spend less time discussing that treatment option or not recommend it as strongly to a patient whom the oncologist perceives as having low levels of social support. However, more research in this area is needed to better understand the relationship between oncologist perceptions and treatment recommendations—and ultimately their impact on racial health disparities—as well as the role that companions may play in this relationship.
Study Limitations
This study had several strengths, most notably the use of observed behavioral data from clinical encounters between Black patients, non-Black oncologists, and companions. However, this was a secondary analysis of existing data; no data were available on the type of patient-companion relationship (eg, spouse, child, and friend), on companion demographics, or on companion-specific outcomes (eg, companion perceptions of oncologists and oncologist perceptions of companions). Another notable limitation was that patient active participation was measured differently in observers versus oncologists: Observers rated multiple aspects of patient participation, including asking questions, making assertions, and expressing concerns, while oncologist report of patient participation was limited to a single item that assessed only one aspect of this construct (asking questions). Future research would benefit from evaluating specific companion communication behaviors, as well as assessing patient and companion well-being outcomes and longer-term patient clinical outcomes of the effects observed in the present study.
Clinical Implications
The results of this study suggest that there are several benefits to Black patients bringing a companion to oncology encounters with non-Black oncologists, such as the oncologist exhibiting more patient-centered communication and having more positive perceptions of the patient. Thus, it may be advisable for oncology practices to encourage and facilitate the inclusion of companions specifically in the care of their Black patients.
In conclusion, given that Black patients are much less likely than White patients to bring a companion to clinical encounters in the first place,6 the results of this study suggest that additional work is needed to understand the reasons for this difference and to identify strategies to facilitate companion involvement in Black patients' care; for example, including companions in clinical encounters via telephone or video calls may enable companions to accompany patients virtually, which might yield similar benefits as when companions attend in-person. Additional research on the clinical encounters of Black patients—particularly research that considers the patient's social context and support network—is vital to developing interventions to facilitate patient- and family-centered communication for Black patients, improving clinical outcomes and, ultimately, racial health disparities.
SUPPORT
Grants from the National Cancer Institute generously supported the parent project of this study (1U54CA153606-01, PI: T. L. Albrecht; P30CA022453, PI: G. Bepler), as well as the first author's time on the present study (5T32CA090314-16, PIs: T. H. Brandon and S. T. Vadaparampil).
AUTHORS' DISCLOSURES OF POTENTIAL CONFLICTS OF INTEREST
Disclosures provided by the authors are available with this article at DOI https://doi.org/10.1200/OP.20.00820.
AUTHOR CONTRIBUTIONS
Conception and design: Amy K. Otto, Lauren M. Hamel, Susan Eggly
Provision of study materials or patients: Susan Eggly
Collection and assembly of data: Tanina F. Moore, Susan Eggly
Data analysis and interpretation: All authors
Manuscript writing: All authors
Final approval of manuscript: All authors
Accountable for all aspects of the work: All authors
AUTHORS' DISCLOSURES OF POTENTIAL CONFLICTS OF INTEREST
Impact of Patients' Companions on Clinical Encounters Between Black Patients and Their Non-Black Oncologists
The following represents disclosure information provided by authors of this manuscript. All relationships are considered compensated unless otherwise noted. Relationships are self-held unless noted. I =Immediate Family Member, Inst = My Institution. Relationships may not relate to the subject matter of this manuscript. For more information about ASCO’s conflict of interest policy, please refer to www.asco.org/rwc or ascopubs.org/op/authors/author-center.
Open Payments is a public database containing information reported by companies about payments made to US-licensed physicians (Open Payments).
No potential conflicts of interest were reported.
REFERENCES
- 1.Association of American Medical Colleges : Diversity in Medicine: Facts and Figures 2019, 2019 [Google Scholar]
- 2.American Society of Clinical Oncology : Key Trends in Tracking Supply of and Demand for Oncologists, 2018 [Google Scholar]
- 3.Saha S, Taggart SH, Komaromy M, et al. : Do patients choose physicians of their own race? Health Aff (Millwood) 19:76-83, 2000 [DOI] [PubMed] [Google Scholar]
- 4.Shen MJ, Peterson EB, Costas-Muniz R, et al. : The effects of race and racial concordance on patient-physician communication: A systematic review of the literature. J Racial Ethn Health Disparities 5:117-140, 2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gordon HS, Street RL, Jr, Sharf BF, et al. : Racial differences in doctors' information-giving and patients' participation. Cancer 107:1313-1320, 2006 [DOI] [PubMed] [Google Scholar]
- 6.Eggly S, Harper FW, Penner LA, et al. : Variation in question asking during cancer clinical interactions: A potential source of disparities in access to information. Patient Educ Couns 82:63-68, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cooper-Patrick L, Gallo JJ, Gonzales JJ, et al. : Race, gender, and partnership in the patient-physician relationship. JAMA 282:583-589, 1999 [DOI] [PubMed] [Google Scholar]
- 8.Cooper LA, Roter DL, Johnson RL, et al. : Patient-centered communication, ratings of care, and concordance of patient and physician race. Ann Intern Med 139:907-915, 2003 [DOI] [PubMed] [Google Scholar]
- 9.Street RL, Jr, Gordon H, Haidet P: Physicians' communication and perceptions of patients: Is it how they look, how they talk, or is it just the doctor? Soc Sci Med 65:586-598, 2007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Diette GB, Rand C: The contributing role of health-care communication to health disparities for minority patients with asthma. Chest 132:802S-809S, 2007(suppl 5) [DOI] [PubMed] [Google Scholar]
- 11.Street RL, Jr, Makoul G, Arora NK, et al. : How does communication heal? Pathways linking clinician-patient communication to health outcomes. Patient Educ Couns 74:295-301, 2009 [DOI] [PubMed] [Google Scholar]
- 12.Hoerger M, Epstein RM, Winters PC, et al. : Values and options in cancer care (VOICE): Study design and rationale for a patient-centered communication and decision-making intervention for physicians, patients with advanced cancer, and their caregivers. BMC Cancer 13:188, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Street RL, Gordon HS: Companion participation in cancer consultations. Psychooncology 17:244-251, 2008 [DOI] [PubMed] [Google Scholar]
- 14.Laidsaar-Powell RC, Butow PN, Bu S, et al. : Physician-patient-companion communication and decision-making: A systematic review of triadic medical consultations. Patient Educ Couns 91:3-13, 2013 [DOI] [PubMed] [Google Scholar]
- 15.Clayman ML, Roter D, Wissow LS, et al. : Autonomy-related behaviors of patient companions and their effect on decision-making activity in geriatric primary care visits. Soc Sci Med 60:1583-1591, 2005 [DOI] [PubMed] [Google Scholar]
- 16.Ishikawa H, Hashimoto H, Roter DL, et al. : Patient contribution to the medical dialogue and perceived patient-centeredness. An observational study in Japanese geriatric consultations. J Gen Intern Med 20:906-910, 2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bracher M, Stewart S, Reidy C, et al. : Partner involvement in treatment-related decision making in triadic clinical consultations–A systematic review of qualitative and quantitative studies. Patient Educ Couns 103:245-253, 2019 [DOI] [PubMed] [Google Scholar]
- 18.Schilling LM, Scatena L, Steiner JF, et al. : The third person in the room: Frequency, role, and influence of companions during primary care medical encounters. J Fam Pract 51:685-690, 2002 [PubMed] [Google Scholar]
- 19.Greene MG, Majerovitz SD, Adelman RD, et al. : The effects of the presence of a third person on the physician-older patient medical interview. J Am Geriatr Soc 42:413-419, 1994 [DOI] [PubMed] [Google Scholar]
- 20.Wolff JL, Roter DL: Hidden in plain sight: Medical visit companions as a resource for vulnerable older adults. Arch Intern Med 168:1409-1415, 2008 [DOI] [PubMed] [Google Scholar]
- 21.Prohaska TR, Glasser M: Patients' views of family involvement in medical care decisions and encounters. Res Aging 18:52-69, 1996 [Google Scholar]
- 22.Ishikawa H, Roter DL, Yamazaki Y, et al. : Physician-elderly patient-companion communication and roles of companions in Japanese geriatric encounters. Soc Sci Med 60:2307-2320, 2005 [DOI] [PubMed] [Google Scholar]
- 23.Clayman ML, Morris MA: Patients in context: Recognizing the companion as part of a patient-centered team. Patient Educ Couns 91:1-2, 2013 [DOI] [PubMed] [Google Scholar]
- 24.Cene CW, Haymore B, Laux JP, et al. : Family presence and participation during medical visits of heart failure patients: An analysis of survey and audiotaped communication data. Patient Educ Couns 100:250-258, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Labrecque MS, Blanchard CG, Ruckdeschel JC, et al. : The impact of family presence on the physician-cancer patient interaction. Soc Sci Med 33:1253-1261, 1991 [DOI] [PubMed] [Google Scholar]
- 26.Rosland AM, Piette JD, Choi H, et al. : Family and friend participation in primary care visits of patients with diabetes or heart failure: Patient and physician determinants and experiences. Med Care 49:37-45, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Eggly S, Hamel LM, Foster TS, et al. : Randomized trial of a question prompt list to increase patient active participation during interactions with black patients and their oncologists. Patient Educ Couns 100:818-826, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Stewart M, Brown JB, Donner A, et al. : The impact of patient-centered care on outcomes. J Fam Pract 49:796-804, 2000 [PubMed] [Google Scholar]
- 29.Enders CK: Applied Missing Data Analysis, in Kenny DA, Little TD. (ed): New York, NY, The Guilford Press, 2010 [Google Scholar]
- 30.Muthén LK, Muthén BO: Mplus User's Guide (7th ed). Los Angeles, CA, Muthén & Muthén, 1998-2012 [Google Scholar]
- 31.Jiang S: Pathway linking patient-centered communication to emotional well-being: Taking into account patient satisfaction and emotion management. J Health Commun 22:234-242, 2017 [DOI] [PubMed] [Google Scholar]
- 32.Venetis MK, Robinson JD, Turkiewicz KL, et al. : An evidence base for patient-centered cancer care: A meta-analysis of studies of observed communication between cancer specialists and their patients. Patient Educ Couns 77:379-383, 2009 [DOI] [PubMed] [Google Scholar]
- 33.Kaplan SH, Greenfield S, Ware JE, Jr: Assessing the effects of physician-patient interactions on the outcomes of chronic disease. Med Care 27:S110-S127, 1989(suppl 3) [DOI] [PubMed] [Google Scholar]
- 34.Epstein RM, Franks P, Shields CG, et al. : Patient-centered communication and diagnostic testing. Ann Fam Med 3:415-421, 2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Dong S, Butow PN, Costa DS, et al. : The influence of patient-centered communication during radiotherapy education sessions on post-consultation patient outcomes. Patient Educ Couns 95:305-312, 2014 [DOI] [PubMed] [Google Scholar]
- 36.Laws MB, Epstein L, Lee Y, et al. : The association of visit length and measures of patient-centered communication in HIV care: A mixed methods study. Patient Educ Couns 85:e183-e188, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Wilson A, Childs S: The relationship between consultation length, process and outcomes in general practice: A systematic review. Brit J Gen Pract 52:1012-1020, 2002 [PMC free article] [PubMed] [Google Scholar]
- 38.Comstock LM, Hooper EM, Goodwin JM, et al. : Physician behaviors that correlate with patient satisfaction. J Med Educ 57:105-112, 1982 [DOI] [PubMed] [Google Scholar]
- 39.Kaplan SH, Gandek B, Greenfield S, et al. : Patient and visit characteristics related to physicians participatory decision-making style results from the medical outcomes study. Med Care 33:1176-1187, 1995 [DOI] [PubMed] [Google Scholar]
- 40.Penner LA, Dovidio JF, Gonzalez R, et al. : The effects of oncologist implicit racial bias in racially discordant oncology interactions. J Clin Oncol 34:2874-2880, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]