Abstract
The objective of this placebo-controlled, double-blind, randomized study (designed according to evidence-based medicine standards) was to determine the effect of 30-day administration of powdered brown algae, Ascophyllum nodosum (ProDen PlaqueOff, SwedenCare AB, Sweden), on saliva metabolomes in dogs. Sixty client-owned dogs underwent professional dental cleaning and were randomly subdivided into two groups receiving daily powdered brown algae A. nodosum, or a placebo (microcrystalline cellulose in powder), adjusted to their bodyweight. After a comprehensive oral health assessment and professional dental cleaning, which were both performed under general anesthesia, clinical assessments for gingivitis, plaque, and calculus were conducted. Saliva samples were collected at Day 0 and Day 30 of supplementation. Whole saliva is a mixed fluid that is derived predominantly from the major salivary glands but it also contains numerous other constituents. Additionally, its composition varies on whether salivary secretion is basal or stimulated. Authors put efforts to avoid contamination of saliva by other constituents and character of saliva was basal. Quadrupole time-of-flight (QTOF) mass spectrometer was used to conduct analysis of the saliva samples. Metabolomic analyses identified clear changes after 30 days of supplementation, and the direction of these changes was completely different than in dogs that received a placebo treatment during the same period. The positive clinical effect of 30 days of A. nodosum supplementation on oral health status in dogs described in previous publication combined with the absence of some metabolites in the saliva of dogs on day 30 of supplementation suggest that brown algae inhibit or turn off some pathways that could enhance plaque or calculus development. The exact mechanism of A. nodosum is still unclear and warrants further study.
Keywords: ascophyllum, dogs, metabolomics, metabolites, oral health, saliva
Introduction
Periodontal disease is one of the most common conditions in dogs. It has a prevalence ranging from 44 to 100% in adult dogs, and its incidence and severity increase with age (1). It is initiated by plaque formation and calculus deposition on the tooth enamel, which leads to gingivitis, periodontitis, and tooth loss (2). The majority of cases are irreversible but often controllable (1). There are many different approaches to periodontal disease prevention, the majority of which involve oral care and the elimination of plaque and calculus.
One approach to periodontal disease prevention in dogs is the use of powdered Ascophyllum nodosum seaweed as a food additive (3). These brown algae can be administered to dogs directly as a food additive or indirectly as an ingredient of pet food, treats, or other nutritional products. In a previous study, treatment of adult dogs with edible treats containing A. nodosum for 90 days reduced plaque deposition by 40% and calculus formation by 20% compared to a control group (3). A formula containing the active agent as a powder has also been evaluated in dogs and received the Veterinary Oral Health Council Seal of Acceptance (www.vohc.org). Additional studies are currently being conducted in cats. In humans ingesting the algae significantly reduced the formation of supragingival calculus and plaque, and the occurrence of gingival bleeding (4).
The composition of saliva and identification of saliva metabolites which play a role in oral health and disease are the subject of intense research. In humans, due to deficiency of periodontal screening procedures the use of metabolomic tools has led to identification of metabolites associated with periodontal variables linked with tissue destruction, host defense mechanisms and bacterial metabolism (5). Quantitatively, production of saliva or flow rates are either considered basal or surge. Salivary composition varies, depending on whether salivary secretion is basal or stimulated (6). Whole saliva is a mixed fluid that is derived predominantly from the major salivary glands. However, whole saliva also contains constituents that do not originate in the salivary gland, including gingival crevicular fluid (GCF), serum transudate from the mucosa and sites of inflammation, expectorated bronchial and nasal secretions, microorganisms and products, viruses, fungi, desquamated epithelial cells, and food and debris. Depending on their size and charge, molecules from blood enter into saliva (7).
Despite evidenced effectiveness of brown algae administration for the reduction of plaque and calculus deposition, the exact mechanisms of its action are currently unknown. One suggested mechanism is based on our hypothesis that some of the seaweed's active ingredients are absorbed in the small intestine and then secreted into the oral cavity via saliva. That is why to investigate our hypothesis, in the study presented here, the metabolomes of non-stimulated, whole saliva were investigated in dogs that received powdered A. nodosum in their food for 30 days.
Materials and Methods
Dogs
The dogs included in the study were client-owned. All procedures performed during the study were conducted in accordance with standard veterinary care protocols and relevant Polish regulations (Art.1 ust.2 pkt1 Dz. U.2015 poz. 266), so the study did not require ethics committee approval. All dog owners provided written informed consent for the participation of their dogs in the study. The study adhered to VOHC requirements to assess the efficacy of an oral supplement containing A. nodosum.
Inclusion/Exclusion Criteria
None of the dogs included in the study had received any anti-inflammatory drugs, or antibiotics within the 30 days prior to the initiation of the treatment. All dogs were required to have most of their teeth, but the teeth specifically required for the assessment were bilateral maxillary I3, C, P3, P4, and M1 and mandibular C, P3, P4, and M1. Oral health status was required to be no worse than PD2 as determined via American Veterinary Dental College stage (www.avdc.org). The parameters assessed to determine the general health status of the dogs included urinalysis, complete blood count (CBC), thyroxine, selected serum tests (urea, total protein, albumin, glucose, alanine transaminase, alkaline phosphatase), and a clinical assessment (see section Dental procedures and oral health assessment for further details). Pregnant dogs, and any dogs with non-gingival inflammation oral ulceration or laceration as well as with systemic disease or increased levels of thyroxine were excluded. The latter was due to increased amount of iodine in supplement (the seaweed) and this information is included in manufacturer's description.
The randomization lists for each trial and group were generated using the Research Randomizer (8) randomization program. The numbers of dogs receiving the active substance or a placebo were equal (n = 30 per group). The clients were blinded to group assignment, as were the personnel conducting the clinical study and the statistician. None of the dogs received any form of oral hygiene treatment during the study other than the study preparation or the corresponding placebo.
Products
During the study, all dogs received the supplement in powder form prepared by the manufacturer (Swedencare AB, Sweden). One group received powder containing the brown algae A.N. ProDen™ (ProDen PlaqueOff®), and the other group received a microcrystalline cellulose powder. One measuring scoop included 330 mg of product, and the recommended daily doses were 0.5 of a scoop for dogs weighing 2.0–4.9 kg, 1.0 scoop for dogs weighing 5.0–9.9 kg, and 1.5 scoops for dogs weighing 10.0–14.9 kg. This results in a dose of product in the range of 33.2–82.5 mg/kg. The two products (active and placebo) were packed into a neutral non-transparent container that included a measuring scoop. The containers were labeled with the study details and the date, but not with an overt indication of whether the container contained the experimental preparation or the placebo. During the study period all dogs were fed dry kibble (Hill's SP Canine Adult Chicken) and tap water was provided ad libitum. Information about food intake and any variations were recorded by the dog owners.
Dental Procedures and Oral Health Assessment
On the first day of the study (T0) all participating dogs were treated at the dental facility of Arka Veterinary Clinic in Krakow, Poland, which is a referral clinic with a hospital, training facility, and dental/surgery profile (www.arka-vet.pl). The study procedures conducted at T30 were performed under sedation at the same facility. The study was conducted between May 2018 and August 2018.
Animals qualified for anesthesia on T0 if they had an anesthesia risk of ≤ 1 (9). All dogs were first evaluated via a general physical examination that included visual assessment, heart and lung auscultation, capillary refill time assessment, and body weight and body temperature measurements. All parameters and remarks were recorded on an anesthesia chart. Intravenous catheters were placed and blood was collected for immediate laboratory work. Urine samples were collected via cystocentesis and immediately evaluated using a UA analyzer to measure pH and specific gravity, and test for protein, glucose, ketones, and blood. The Oral Health Index (OHI) of each dog was evaluated before sedation in accordance with published protocols, and was defined as the sum of scores obtained for three parameters; lymphadenopathy, dental deposits, and periodontal disease, with 0 points indicating optimal oral health, and 6 points indicating the poorest oral health (10).
Sedation was performed using recommended doses of medetomidine (Sedator, Eurovet Animal Health B.V.) and butorphanol (Torbugesic, Zoetis, Poland Sp. z o.o.). Preoxygenation was then performed using a mask for the delivery of medical oxygen. After sedation was achieved, each dog was administered the recommended dose of propofol (Scanofol, ScanVet, Poland Sp. z o.o.) to induce general anesthesia. An endotracheal tube was placed, the cuff was filled, cardio monitor peripheral probes were attached to the dog's body, and a temperature maintenance system was installed. General anesthesia was maintained via isoflurane and oxygen for the duration of dental procedures, which included comprehensive oral health assessment with periodontal probing, dental charting, and full mouth radiography.
The oral assessment methods for gingivitis, plaque, and calculus were applied to 9 (5 + 4) target teeth on each side; maxillary 13, C, P3, P4, and M1, and mandibular C, P3, P4, and M1. Every dog had 18 teeth assessed. The buccal surfaces of the target teeth on both sides of the mouth were scored by an experienced assessor who evaluated gingival bleeding index, plaque, and calculus in that order.
Saliva Sampling
All dogs were fasted and were not engaged in any activities for at least 12 h prior to awake examination, during which a saliva sample was collected. According to the VOHC requirements, scoring episode was performed within +/−3 h of when the next treatment would have been given if the trial had continued. The dogs were given the Ascophyllum product in the afternoon, the rechecks and thus the saliva collection was approximately 3 h prior to normal feeding time so the sampling was 21 h prior to the next food or supplement administration.
A sterile size 80 paper point ISO was introduced into the oral vestibulum space via dental forceps and kept there until it was completely soaked with saliva. The average time of soaking was 15 s and approximately amount of saliva that made complete soaking was 25 μl. At a time of collection samples, the completion of soaking was based on time and visual assessment. It then was placed into a labeled sterile Eppendorf tube and frozen at −20°C. If required, this process was also performed on the contralateral side. The tubes were then packaged with ice and transported to the laboratory. Saliva samples were taken from all dogs at two timepoints; prior to professional dental cleaning (T0), and at least 12 h after the last of 30 days of administration of the experimental product or placebo (T30). Saliva collection was performed before sedation and prior to the assessment of dental indices.
Metabolomic Analyses
Equipment
Metabolomic analyses were performed using a high-pressure liquid chromatography Symbiosis Pico UhPLC system. The detector used was a SCIEX TripleTOF 5600+ DuoSpray Source for SCIEX TripleTOF 5600+ (TurboIonSpray and APCI). Data were analyzed using SCIEX MarkerView™, XCMSplus, and MetaboAnalyst 4.0 software.
Sample Preparation
Filters with samples were placed into 1.5-mL tubes, and then, 800 μL of a 1:1 mixture of acetonitrile and methanol was added. Vials were vortexed (2,000 rotations for 15 min) and centrifuged for 15 min at 13,000 rpm. Supernatant was transferred to glass autosampler vials, which were then placed in an autosampler at 4°C. Saliva samples (8.0 μL) were injected directly into a Spark Holland Symbiosis™ Pico. Chromatographic separation was performed on Hypersil chromatographic column, BDS C18, 150 × 4.6 mm, 5 mm with a Hypersil C18 guard column (10 × 2.1 mm, size 5 μm). The mobile phase consists of methanol: formic acid (99:1, v/v) A and water: formic acid (99:1, v/v) B, the flow rate was constant 500 μLmin−1. Gradient elution of mobile phase 100% A was started, 1.1–40 min linear gradient to 100% B, 40.1–55 min 100% B, 55.1–60 min linear gradient to 100% A. The runtime of the method was 60 min.
MS Parameters: The optimized detection conditions included curtain gas (N2) 25 psi, nebulizer gas (N2) 20 psi, heater gas (N2) 50 psi, ion source voltage floating 5,500 V, and source temperature 500°C. Samples with a heated electrospray ionization probe measured in positive ionization (H-ESI+). Every third analyzed saliva sample using the Calibrant Delivery System (SCIEX) MS sytem was auto-calibrated using original calibrators (SCIEX).
Calculations and Metabolites Identification
Metabolomic comparisons were performed within each experimental group between T0 and T30. Metabolite profiles obtained in the 100–1100 Da range with 5 cps sensitivity were analyzed using MarkerView™ software to compare the groups, including Student's t-tests and principal component analysis (PCA). The generated metabolomics profiling data sets were processed by the control software of the Analyst® mass spectrometer and saved in a specific data format (*raw). The first step was to convert data from Excalibur-specific raw files to open format files (*mzXML) using MS Convertor software (MSConvert). Subsequently, metabolomics data were processed using the XCMSplus platform. Additionally, principal component analysis (PCA) resulted in comparative profiles of metabolomes of specific groups were analyzed by MarkerView™ software. The classification of identified metabolites in particular metabolic pathways was conducted using the XCMSplus platform and MetaboAnalyst 4.0 software with a probability threshold of p < 0.0001. The identification of metabolites was carried out on the basis of the ChemSpider database (access via PeakView™) indications above 80% probability of confirming a given structure - these data were compared with the indications of metabolites from the MetaboAnalyst 4.0 database.
Results
After 30 days of product administration there were significant changes in dog saliva metabolomes (Figures 1, 2). In the untreated control group 4,347 metabolites exhibited levels that differed on day 30 compared to day 0. Of these, 962 differed significantly (p > 0.05) (data not shown). Using specialized software, 68 different molecules were identified based on their molecular weights. Based on a list of known metabolites included in software database, no significantly altered metabolic pathways were identified after 30 days of placebo treatment (Table 1). Analyses performed on individual metabolites revealed three groups; metabolites elevated after 30 days of administration, metabolites decreased after 30 days of administration, and metabolites absent after 30 days of administration (Table 2). The absent metabolites included molecules involved in metabolism of vitamin A, as well as metabolites of some drugs (tamoxifen). Metabolites that had increased after 30 days of placebo administration included molecules involved in arachidonic acid metabolism, leukotriene metabolism, and prostaglandin formation from arachidonate.
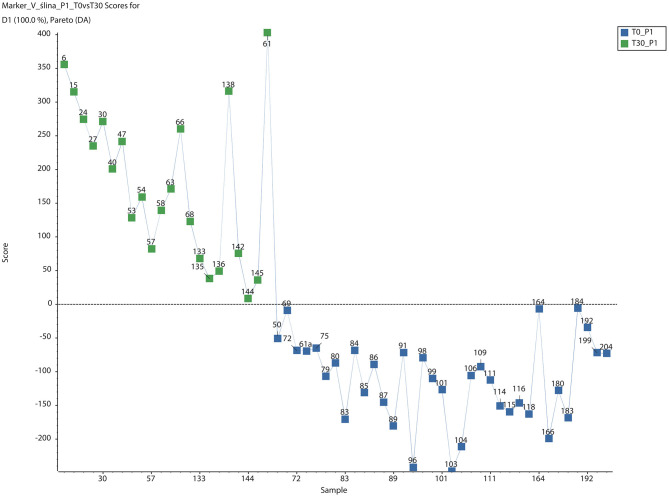
Figure 1.
PCA-DA Score plots for saliva of dogs after 30-day-long period of placebo administration. Green boxes and blue boxes represent metabolome of sample from dogs in day 0 and day 30 after placebo administration, respectively (PCA-DA, Scaling PARETO, SCIEX MarkerView™).
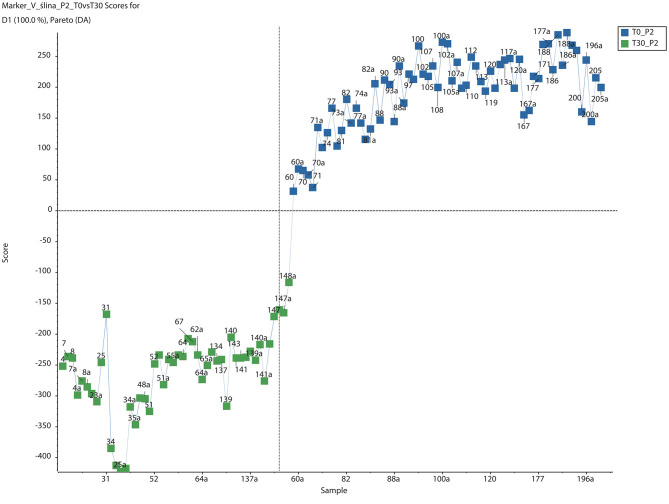
Figure 2.
PCA-DA Score plots for saliva of dogs after 30-day-long period of Ascophyllum nodosum administration. Green boxes and blue boxes represent metabolome of sample from dogs in day 0 and day 30 after Ascophyllum nodosum administration, respectively (PCA-DA, Scaling PARETO, SCIEX MarkerView™).
Table 1.
List of metabolic pathways identified in dog saliva after 30 days of placebo administration.
| Pathway | Total | Hits (all) | Hits (sig.) | p-value | Gamma P |
|---|---|---|---|---|---|
| Drug metabolism - cytochrome P450 | 53 | 20 | 3 | 0.489 | 0.120 |
| De novo fatty acid biosynthesis | 106 | 21 | 3 | 0.524 | 0.125 |
| Purine metabolism | 80 | 13 | 2 | 0.516 | 0.139 |
| Glycerophospholipid metabolism | 156 | 24 | 3 | 0.619 | 0.139 |
| Tyrosine metabolism | 160 | 20 | 2 | 0.754 | 0.181 |
| Vitamin A (retinol) metabolism | 67 | 33 | 3 | 0.823 | 0.183 |
| C21-steroid hormone biosynthesis and metabolism | 112 | 60 | 5 | 0.910 | 0.203 |
| Leukotriene metabolism | 92 | 41 | 3 | 0.919 | 0.223 |
| Prostaglandin formation from arachidonate | 78 | 50 | 2 | 0.993 | 0.347 |
| Arachidonic acid metabolism | 95 | 65 | 2 | 0.999 | 0.420 |
Table 2.
List of significantly (p < 0.05) regulated metabolites in dog saliva after 30 days of placebo administration.
| No. | Metabolite | Metabolic pathway | KEGG ID | Molecular weight | p-value | Fold Change (FC) | logFC | Remarks |
|---|---|---|---|---|---|---|---|---|
| 1 | (4Z,7Z,10Z,13Z,16Z,19Z)-docosahexaenoic acid | De novo fatty acid biosynthesis | C06429 | 328.4,880 | 0.014 | 57.703 | 1.761 | |
| 2 | N(omega)-(ADP-D-ribosyl)-L-arginine | Vitamin B3 (nicotinate and nicotinamide) metabolism | C01201 | 715.5,014 | <0.001 | 3.714 | 0.570 | |
| 3 | 1-(1-alkenyl)-sn-glycero-3-phosphate | Glycerophospholipid metabolism | C15646 | 197.1,030 | 0.001 | 3.603 | 0.557 | |
| 4 | S-succinyldihydrolipoamide | TCA cycle | C01169 | 307.4,294 | 0.031 | 298.063 | 2.474 | |
| 5 | 7-methyluric acid | Caffeine metabolism | C16355 | 182.1,368 | <0.001 | 2.777 | 0.444 | |
| 6 | 1-methyluric acid | Caffeine metabolism | C16359 | 474.6,511 | <0.001 | 2.777 | 0.444 | |
| 7 | (9E)-octadecenoic acid | Fatty acid activation | C01712 | 282.2,559 | 0.001 | 2.037 | 0.309 | |
| 8 | (9Z)-octadecenoic acid | De novo fatty acid biosynthesis | C00712 | 282.4,614 | 0.001 | 2.037 | 0.309 | |
| 9 | Hypoxanthine | Purine metabolism | C00262 | 136.1,115 | 0.034 | 2.028 | 0.307 | |
| 10 | (5Z,8Z,11Z,14Z,17Z)-eicosapentaenoic acid | De novo fatty acid biosynthesis | C06428 | 302.4,510 | <0.001 | 1.594 | 0.202 | |
| 11 | Homovanillic acid | Tyrosine metabolism | C05582 | 182.1,733 | 0.005 | 1.543 | 0.188 | |
| 12 | 16-glucuronide-estriol | Androgen and estrogen biosynthesis and metabolism | C05504 | 464.5,055 | 0.005 | 1.543 | 0.188 | |
| 13 | L-fucose 1-phosphate | Fructose and mannose metabolism | C02985 | 244.1,364 | 0.316 | 1.541 | 0.188 | |
| 14 | Pregnanolone | C21-steroid hormone biosynthesis and metabolism | C05480 | 318.4,935 | 0.316 | 1.541 | 0.188 | |
| 15 | 1,2-naphthoquinone | Xenobiotics metabolism | C14783 | 158.1,534 | 0.006 | 1.457 | 0.163 | |
| 16 | 11-cis-retinal | Vitamin A (retinol) metabolism | C02110 | 284.4,357 | 0.006 | 1.457 | 0.163 | |
| 17 | N6,N6,N6-trimethyl-L-lysine | Lysine metabolism | C03793 | 188.2,673 | 0.006 | 1.457 | 0.163 | |
| 18 | Leukotriene E4 | Leukotriene metabolism | C05952 | 439.6,086 | 0.006 | 1.457 | 0.163 | |
| 19 | 1-(5′-phosphoribosyl)-5-amino-4-(N-succinocarboxamide)-imidazole | Purine metabolism | C04823 | 454.2,833 | 0.006 | 1.457 | 0.163 | |
| 20 | Hydroxytamoxifen | Drug metabolism - cytochrome P450 | C05011 | 387.5,140 | 0.006 | 1.457 | 0.163 | |
| 21 | Phenylacetic acid | Tyrosine metabolism | C07086 | 136.1,479 | 0.004 | 1.445 | 0.160 | |
| 22 | Sterol | Glycerophospholipid metabolism | C00370 | 248.4,036 | 0.193 | 0.838 | −0.077 | Negative value of logFC = lower metabolite content at T30 |
| 23 | (2R,3S)-2,3,4-trihydroxybutanoic acid | Ascorbate (vitamin C) and aldarate metabolism | C01620 | 136.1,033 | 0.001 | 0.480 | −0.318 | Negative value of logFC = lower metabolite content at T30 |
| 24 | Sterol | C21-steroid hormone biosynthesis and metabolism | C00370 | 284.4,036 | 0.001 | 0.408 | −0.389 | Negative value of logFC = lower metabolite content at T30 |
| 25 | Lidocaine | Drug metabolism - cytochrome P450 | C07073 | 234.3,373 | <0.001 | 0.120 | −0.922 | Negative value of logFC = lower metabolite content at T30 |
| 26 | Dechloroethylcyclo-phosphamide | Drug metabolism - cytochrome P450 | C16550 | 198.5,877 | <0.001 | 0.058 | −1.237 | Negative value of logFC = lower metabolite content at T30 |
| 27 | 6-mercaptopurine | Drug metabolism - other enzymes | C02380 | 152.1,771 | <0.001 | 0.020 | −1.695 | Negative value of logFC = lower metabolite content at T30 |
| 28 | Retinyl ester | Vitamin A (retinol) metabolism | C02075 | 313.4,538 | <0.001 | Metabolite is absent at T30 | ||
| 29 | 11beta-hydroxyprogesterone | C21-steroid hormone biosynthesis and metabolism | C05498 | 330.4,611 | 0.014 | Metabolite is absent at T30 | ||
| 30 | 16(R)-HETE | Arachidonic acid metabolism | C14778 | 320.4,663 | 0.006 | 1.457 | 0.163 | |
| 11,12-EET | Arachidonic acid metabolism | C14770 | 320.4,663 | 0.004 | 1.445 | 0.160 | ||
| 14,15-EET | Arachidonic acid metabolism | C14771 | 320.4,663 | 0.004 | 1.445 | 0.160 | ||
| 19(S)-HETE | Arachidonic acid metabolism | C14749 | 320.4,663 | 0.004 | 1.445 | 0.160 | ||
| 20-HETE | Arachidonic acid metabolism | C14748 | 320.4,663 | 0.004 | 1.445 | 0.160 | ||
| 20-hydroxy arachidonic acid | Glycerophospholipid metabolism | C14748 | 320.4,663 | 0.004 | 1.445 | 0.160 | ||
| 5,6-EET | Arachidonic acid metabolism | C14768 | 320.4,663 | 0.004 | 1.445 | 0.160 | ||
| 8,9-EET | Arachidonic acid metabolism | C14769 | 320.4,663 | 0.004 | 1.445 | 0.160 | ||
| 31 | 17alpha-hydroxyprogesterone | C21-steroid hormone biosynthesis and metabolism | C01176 | 330.4,611 | 0.316 | 1.541 | 0.188 | |
| 11-deoxycorticosterone; | C21-steroid hormone biosynthesis and metabolism | C03205 | 330.4,611 | <0.001 | 0.120 | −0.922 | Negative value of logFC = lower metabolite content at T30 | |
| 32 | 5(S)-HETE | Arachidonic acid metabolism | C04805 | 336.4,657 | <0.001 | 10.476 | 1.020 | |
| 5(S)-HPETE | Leukotriene metabolism | C05356 | 336.4,657 | 0.006 | 1.457 | 0.163 | ||
| Leukotriene B4 | Leukotriene metabolism | C02165 | 336.4,657 | 0.006 | 1.457 | 0.163 | ||
| Prostaglandin A1 | Prostaglandin formation from arachidonate | C04685 | 336.4,657 | 0.006 | 1.457 | 0.163 | ||
| Prostaglandin B1 | Prostaglandin formation from arachidonate | C00959 | 336.4,657 | 0.006 | 1.457 | 0.163 | ||
| 15(S)-HETE | Arachidonic acid metabolism | C05966 | 336.4,657 | 0.004 | 1.445 | 0.160 | ||
| Prostaglandin C1 | Prostaglandin formation from arachidonate | C04686 | 336.4,657 | 0.004 | 1.445 | 0.160 | ||
| 15H-11,12-EETA; | Arachidonic acid metabolism | C14781 | 336.4,657 | <0.001 | 0.020 | −1.695 | Negative value of logFC = lower metabolite content at T30 |
The identification of metabolites was carried out on the basis of the ChemSpider database (access via PeakView™) indications above 80% probability of confirming a given structure so the table contains also the names of isomers or molecules with the same molecular weight with the same p-values and FC.
In the group treated with the A. nodosum preparation 4,213 metabolites exhibited levels that differed on day 30 compared to day 0. Of these, 1,570 metabolites differed significantly (p < 0.05) (data not shown). Using specialized software 61 different molecules were identified based on their molecular weights. Based on a list of known metabolites, no significantly altered metabolic pathways were identified after 30 days of A. nodosum treatment (Table 3), although the significance of changes within the selenoamino acid metabolism pathway was considerably high (p = 0.063). The number of metabolites absent in dog saliva after 30 days of A. nodosum administration was higher than that in the control group (Table 4). The administration of A. nodosum was associated with a complete absence of 27/61 identified metabolites in the dog saliva. These absent metabolites included molecules involved in androgen and estrogen biosynthesis and metabolism (dehydroepiandrosterone), and prostaglandin synthesis from arachidonate and fatty acid metabolism (linoleic acid). Metabolites increased in dog saliva after A. nodosum administration included molecules involved in selenoamino acid metabolism (selenomethionine Se-oxide; tetrahydrofolate), linoleate metabolism, and squalene and cholesterol biosynthesis.
Table 3.
List of metabolic pathways identified in dog saliva after 30 days of Ascophyllum nodosum administration.
| No. | Pathway Name | Total | Hits (all) | Hits (sig.) | p-value | Gamma P |
|---|---|---|---|---|---|---|
| 1 | Selenoamino acid metabolism | 35 | 6 | 3 | 0.067 | 0.0,489 |
| 2 | Tyrosine metabolism | 160 | 28 | 6 | 0.350 | 0.068 |
| 3 | Fatty acid metabolism | 63 | 19 | 4 | 0.421 | 0.081 |
| 4 | Drug metabolism - other enzymes | 31 | 6 | 2 | 0.277 | 0.084 |
| 5 | Vitamin E metabolism | 54 | 21 | 4 | 0.504 | 0.091 |
| 6 | Fatty acid activation | 74 | 35 | 6 | 0.580 | 0.094 |
| 7 | Porphyrin metabolism | 43 | 15 | 3 | 0.494 | 0.097 |
| 8 | Methionine and cysteine metabolism | 94 | 9 | 2 | 0.478 | 0.110 |
| 9 | Purine metabolism | 80 | 17 | 3 | 0.584 | 0.110 |
| 10 | Squalene and cholesterol biosynthesis | 55 | 27 | 4 | 0.714 | 0.125 |
| 11 | Pyrimidine metabolism | 70 | 11 | 2 | 0.592 | 0.128 |
| 12 | Urea cycle/amino group metabolism | 85 | 12 | 2 | 0.641 | 0.136 |
| 13 | Aspartate and asparagine metabolism | 114 | 12 | 2 | 0.641 | 0.136 |
| 14 | Vitamin A (retinol) metabolism | 67 | 29 | 4 | 0.767 | 0.138 |
| 15 | Linoleate metabolism | 46 | 23 | 3 | 0.789 | 0.152 |
| 16 | Drug metabolism - cytochrome P450 | 53 | 15 | 2 | 0.762 | 0.163 |
| 17 | Xenobiotics metabolism | 110 | 15 | 2 | 0.762 | 0.163 |
| 18 | De novo fatty acid biosynthesis | 106 | 34 | 4 | 0.867 | 0.170 |
| 19 | Glycosphingolipid metabolism | 67 | 17 | 2 | 0.822 | 0.181 |
| 20 | Carnitine shuttle | 72 | 21 | 2 | 0.902 | 0.215 |
| 21 | Bile acid biosynthesis | 82 | 23 | 2 | 0.929 | 0.232 |
| 22 | Androgen and estrogen biosynthesis and metabolism | 95 | 45 | 4 | 0.968 | 0.243 |
| 23 | Glycerophospholipid metabolism | 156 | 29 | 2 | 0.973 | 0.281 |
| 24 | D4 & E4-neuroprostane formation | 37 | 32 | 2 | 0.984 | 0.305 |
| 25 | Leukotriene metabolism | 92 | 44 | 3 | 0.989 | 0.305 |
| 26 | C21-steroid hormone biosynthesis and metabolism | 112 | 60 | 4 | 0.996 | 0.347 |
| 27 | Prostaglandin formation from arachidonate | 78 | 50 | 3 | 0.996 | 0.347 |
Table 4.
List of significantly (p < 0.05) regulated metabolites in dog saliva after 30 days of Ascophyllum nodosum administration.
| No. | Metabolite | Metabolic pathway | KEGG ID | Molecular weight | p value | Fold Change (FC) | logFC | Remarks |
|---|---|---|---|---|---|---|---|---|
| 1 | L-palmitoylcarnitine | Carnitine shuttle | C02990 | 399.6,077 | <0.001 | 9.073 | 0.958 | |
| 2 | 7-alpha-Hydroxy-3-oxo-4-cholestenoate | Bile acid biosynthesis | C17337 | 430.6,200 | <0.001 | 817.951 | 2.912 | |
| 3 | 2-(S-glutathionyl)acetyl glutathione | Xenobiotics metabolism | C14863 | 654.6,678 | 0.005 | 4.411 | 0.655 | |
| 4 | alpha-tocopherol | Vitamin E metabolism; Ascorbate (Vitamin C) and aldarate metabolism | C02477 | 430.7,061 | 0.004 | 4.402 | 0.644 | |
| 5 | N6,N6,N6-trimethyl-L-lysine | Lysine metabolism | C03793 | 188.2,673 | 0.004 | 39.033 | 1.591 | |
| 6 | 2′-deoxyadenosine 5′-diphosphate | Purine metabolism; Pyrimidine metabolism; Hexose metabolism | C00206 | 411.2,017 | 0.030 | 2.529 | 0.403 | |
| 7 | Docosahexaenoic acid | De novo fatty acid biosynthesis | C06429 | 328.4,883 | <0.001 | 2.122 | 0.327 | |
| 8 | N1-acetylspermine | Aspartate and asparagine metabolism | C16681 | 244.3,769 | <0.001 | 18.137 | 1.259 | |
| 9 | N-carbamoyl-L-aspartate | Pyrimidine metabolism | C00438 | 176.1,274 | <0.001 | 16.801 | 1.225 | |
| 10 | N(omega)-(ADP-D-ribosyl)-L-arginine | Vitamin B3 (nicotinate and nicotinamide) metabolism | C01201 | 715.5,014 | <0.001 | 11.332 | 1.054 | |
| 11 | Glycochenodeoxycholate | Bile acid biosynthesis | C05466 | 449.6,233 | <0.001 | 1.896 | 0.278 | |
| 12 | Selenomethionine Se-oxide | Selenoamino acid metabolism | C05708 | 212.1,057 | 0.001 | 1.873 | 0.273 | |
| 13 | Geranylgeranyl diphosphate | Squalene and cholesterol biosynthesis | C00353 | 450.4,432 | 0.008 | 1.636 | 0.214 | |
| 14 | 20-hydroxyleukotriene E4 | Leukotriene metabolism | C03577 | 455.6,080 | 0.177 | 1.293 | 0.112 | |
| 15 | Lithocholic acid | Bile acid biosynthesis | C03990 | 376.5,726 | 0.030 | 1.289 | 0.110 | |
| 16 | 3′-phosphoadenylylselenate; | Selenoamino acid metabolism | C05696 | 554.1,593 | 0.036 | 1.168 | 0.067 | |
| 17 | 2′-deoxyinosine 5′-phosphate | Purine metabolism | C06196 | 332.2,066 | 0.188 | 0.629 | −0.201 | Negative value of logFC = lower metabolite content at T30 |
| 18 | Codeine-6-glucuronide | Drug metabolism - cytochrome P450 | C16577 | 475.4,884 | 0.002 | 0.344 | −0.463 | Negative value of logFC = lower metabolite content at T30 |
| 19 | SN38 glucuronide | Drug metabolism - other enzymes | C11376 | 568.5,287 | 0.003 | 0.030 | −1.527 | Negative value of logFC = lower metabolite content at T30 |
| 20 | Protoporphyrinogen IX | Porphyrin metabolism | C01079 | 568.7,058 | 0.003 | 0.030 | −1.527 | Negative value of logFC = lower metabolite content at T30 |
| 21 | 5-acetylamino-6-formylamino-3-methyluracil | Caffeine metabolism | C16365 | 226.1,894 | 0.001 | Metabolite is absent at T30 | ||
| 22 | (9Z,11E,15Z)-(13S)-hydroperoxyoctadeca-9,11,15-trienoate | Omega-3 fatty acid metabolism | C04785 | 310.4,284 | <0.001 | Metabolite is absent at T30 | ||
| 23 | Levomethadyl acetate | Drug metabolism - cytochrome P450 | C08012 | 353.4,977 | <0.001 | Metabolite is absent at T30 | ||
| 24 | 7-dehydrodesmosterol | Squalene and cholesterol biosynthesis | C05107 | 382.6,218 | <0.001 | Metabolite is absent at T30 | ||
| 25 | (R)-4′-phosphopantothenoyl-L-cysteine | Vitamin B5 - CoA biosynthesis from pantothenate | C04352 | 402.3,578 | 0.004 | Metabolite is absent at T30 | ||
| 26 | Squalene | Squalene and cholesterol biosynthesis | C00751 | 410.7,180 | 0.001 | Metabolite is absent at T30 | ||
| 27 | Diacetylchitobiose (chitobiose) | Sialic acid metabolism | C01674 | 424.4,003 | <0.001 | Metabolite is absent at T30 | ||
| 28 | 6-mercaptopurine | Drug metabolism - other enzymes | C02380 | 152.1,771 | <0.001 | Metabolite is absent at T30 | ||
| Thiopurine | Urea cycle/amino group metabolism | C01756 | 152.1,771 | <0.001 | Metabolite is absent at T30 | |||
| 29 | Phenylacetylglutamine | Tyrosine metabolism | C04148 | 264.2,771 | 0.076 | 1.688 | 0.227 | |
| Formyl-N-acetyl-5-methoxykynurenamine | Tryptophan metabolism | C05642 | 264.2,771 | 0.076 | 1.688 | 0.227 | ||
| 30 | Linoleic acid | Glycerophospholipid metabolism; Di-unsaturated fatty acid beta-oxidation | C01595 | 280.4,455 | <0.001 | Metabolite is absent at T30 | ||
| 9-cis,12-cis-octadecadienoic acid | Fatty acid metabolism; Linoleate metabolism | C01595 | 280.4,455 | <0.001 | Metabolite is absent at T30 | |||
| Linoleic acid; | Fatty acid activation; de novo fatty acid biosynthesis | C01595 | 280.4,455 | <0.001 | Metabolite is absent at T30 | |||
| 31 | 9-cis-retinal | Vitamin A (retinol) metabolism | C02110 | 284.4,357 | <0.001 | Metabolite is absent at T30 | ||
| retinal-11-cis | Vitamin A (retinol) metabolism | C16681 | 284.4,357 | <0.001 | Metabolite is absent at T30 | |||
| 32 | Dehydroepiandrosterone | C21-steroid hormone biosynthesis and metabolism | C01227 | 288.4,244 | <0.001 | Metabolite is absent at T30 | ||
| 17-beta-hydroxy-4-androsten-3-one | Prostaglandin formation from arachidonate | C00535 | 288.4,244 | <0.001 | Metabolite is absent at T30 | |||
| 5beta-androstane-3,17-dione | Prostaglandin formation from arachidonate | C03772 | 288.4,244 | <0.001 | Metabolite is absent at T30 | |||
| Dehydroepiandrosterone | Androgen and estrogen biosynthesis and metabolism | C01227 | 288.4,244 | <0.001 | Metabolite is absent at T30 | |||
| 17-beta-hydroxy-4-androsten-3-one | Androgen and estrogen biosynthesis and metabolism | C00535 | 288.4,244 | <0.001 | Metabolite is absent at T30 | |||
| 5-beta-androstane-3,17-dione | Androgen and estrogen biosynthesis and metabolism | C03772 | 288.4,244 | <0.001 | Metabolite is absent at T30 | |||
| 5-alpha-androstane-3,17-dione | Androgen and estrogen biosynthesis and metabolism | C00674 | 288.4,244 | <0.001 | Metabolite is absent at T30 | |||
| 33 | (9R,10S)-(12Z)-9,10-epoxyoctadecenoic acid | Linoleate metabolism | C14825 | 296.4,449 | <0.001 | 49.832 | 1.698 | |
| (12R,13S)-(9Z)-12,13-epoxyoctadecenoic acid | Linoleate metabolism | C14826 | 296.4,449 | <0.001 | 49.832 | 1.698 | ||
| (9Z,11E)-(13S)-13-hydroxyoctadeca-9,11-dienoic acid | Linoleate metabolism | C14762 | 296.4,449 | <0.001 | 49.832 | 1.698 | ||
| 34 | 5-pregnen-3beta-ol-20-one | Androgen and estrogen biosynthesis and metabolism | C01953 | 316.4,776 | <0.001 | Metabolite is absent at T30 | ||
| 5-beta-pregnane-3,20-dione | Prostaglandin formation from arachidonate | C00054 | 316.4,776 | <0.001 | Metabolite is absent at T30 | |||
| 5-pregnen-3beta-ol-20-one | Prostaglandin formation from arachidonate | C01953 | 316.4,776 | Metabolite is absent at T30 | ||||
| 20-alpha-hydroxy-4-pregnen-3-one | Prostaglandin formation from arachidonate | C04042 | 316.4,776 | <0.001 | Metabolite is absent at T30 | |||
| 35 | Sphinganine 1-phosphate | Glycerophospholipid metabolism | C01120 | 381.4,877 | <0.001 | Metabolite is absent at T30 | ||
| Sphinganine 1-phosphate | Glycosphingolipid metabolism | C01120 | 381.4,877 | <0.001 | Metabolite is absent at T30 | |||
| 36 | 14-demethyllanosterol | Squalene and cholesterol biosynthesis | C05108 | 412.6,908 | 0.041 | 2.065 | 0.315 | |
| Isofucosterol | Squalene and cholesterol biosynthesis | C08821 | 412.6,908 | 0.041 | 2.065 | 0.315 | ||
| 7-dehydroavenasterol | Squalene and cholesterol biosynthesis | C15782 | 412.6,908 | 0.041 | 2.065 | 0.315 | ||
| 37 | Adenosine 3′,5′-bisphosphate | Tyrosine metabolism; Methionine and cysteine metabolism; Xenobiotics metabolism; Glycosphingolipid metabolism; Prostaglandin formation from arachidonate; Glycosphingolipid biosynthesis - ganglioseries; Keratan sulfate biosynthesis; Proteoglycan biosynthesis | C00054 | 427.2,011 | 0.012 | 1.852 | 0.268 | |
| 2′-deoxyguanosine 5′-diphosphate | Purine metabolism; Pyrimidine metabolism; | C00361 | 427.2,011 | 0.012 | 1.852 | 0.268 | ||
| 38 | Tetrahydrofolic acid | Selenoamino acid metabolism | C00101 | 445.4,292 | 0.004 | 2.827 | 0.451 | |
| Tetrahydrofolate | Methionine and cysteine metabolism; Urea cycle/amino group metabolism; Histidine metabolism; Glycine, serine, alanine and threonine metabolism; Vitamin B9 (folate) metabolism | C00101 | 445.4,292 | 0.004 | 2.827 | 0.451 | ||
| 39 | Uroporphyrin I | Porphyrin metabolism | C05767 | 830.7,469 | <0.001 | 0.109 | −0.962 | Negative value of logFC = lower metabolite content at T30 |
| Uroporphyrin III | Porphyrin metabolism | C02469 | 830.7,469 | <0.001 | 49.832 | 1.698 |
The identification of metabolites was carried out on the basis of the ChemSpider database (access via PeakView™) indications above 80% probability of confirming a given structure so the table contains also the names of isomers or molecules with the same molecular weight with the same p-values and FC.
Discussion
The sum of the small molecules present in a biological sample, known as the “metabolome” has become an area of interest to many researchers in recent years. A consequence of this is the development of metabolomics, which can be described as untargeted measurement of the metabolome. The results of metabolomic analyses are influenced by genetics, environmental factors, and different clinical conditions that affect animals. This technology can be applied to human and animal clinical diagnostics, as well as nutrition, exercise, physiology, agriculture/plant biochemistry, and toxicology. One of the key factors supporting the metabolomics development is the possibility of identifying new potential biomarkers that could become standard diagnostic components in human and animal health screenings (11).
A metabolomic diagnostic approach has previously been applied in many different clinical contexts (12), and saliva as one of numerous body fluids is an obvious area of interest. In humans the composition of the saliva metabolome is a promising diagnostic tool for systemic diseases as well as oral problems, and investigation of the saliva metabolome has even resulted in the development of a specific field known as salivaomics (13). Studies in this area have yielded important information about caries, oral cancer, and systemic conditions (14–16). Due to the ease of sample collection the metabolomic study of saliva may become an important diagnostic tool in the future (17).
To the best of the authors' knowledge, the current study is one of the first to evaluate canine saliva with respect to metabolomics, particularly with regard to oral health. The reason for undertaking the study was to investigate the influence of supplementation of dogs' diets with A. nodosum algae on oral health status, which has been described in our previous studies (3). Clinical effects of supplementation were evident, but the mechanisms of A. nodosum's action are still unclear. Because the available laboratory modalities (complete blood count, serum studies) did not reveal any significant changes in dogs receiving A. nodosum, we assumed that it may influence the composition of dog saliva.
To identify changes in dog saliva composition it was necessary to evaluate the whole saliva metabolome. Protocol for collection, storage, and transportation was designed based on a protocol used for nuclear magnetic resonance-based oral biofluid samples (18). The method used in the current study differed from that recently described by (19), but it facilitated the acquisition of informative samples. Comparative studies are necessary however, to identify the best method of saliva sampling from dogs for metabolomic analyses.
The analyses conducted in the present study yielded some important conclusions. First, in placebo group there were changes in saliva metabolome composition of saliva (Figure 1). Analysis of a list of differentially regulated metabolites revealed increasing levels of proinflammatory leukotrienes, and many different metabolites of arachidonic acid or prostaglandins formed from arachidonate (Table 1). Conversely, many metabolites involved in the metabolism of vitamin A had disappeared from dog saliva after 30 days of treatment. The exact meaning of these changes is unclear however the authors presume that it was oral prophylactic procedure that influenced the composition of saliva.
Secondly in the current study changes in the saliva metabolome were clearly evident in dogs after 30 days of A. nodosum administration (Figure 2), but the directions of these changes differed. An ingredient derived from algae, known as isofucosterol, was detected after 30 days of A. nodosum supplementation. It is one of the sterols produced solely by algae so its presence almost certainly resulted from the algae supplementation (20). The supplementation of dogs' diets with A. nodosum also resulted in upregulation of the selenoamino acid metabolism pathway, which was probably associated with the observed significant change in selenomethionine Se-oxide level. The numbers of metabolites belonging to androgen and estrogen biosynthesis and metabolism pathways were also of interest, as was the disappearance of prostaglandin formation from the arachidonate pathway after 30 days of A. nodosum supplementation. The lack of dehydroepiandrosterone and testosterone was of particular interest. In humans increased dehydroepiandrosterone is correlated with periodontitis level (21), so in the current study the lack of dehydroepiandrosterone in the saliva of dogs administered A. nodosum could be a reflection of improved oral health status; but this is highly speculative.
There are almost no data about saliva composition in healthy or ill dogs. In a recent study, dog saliva metabolomes were compared to human saliva metabolomes (19). The unique canine metabolites identified in that study were mostly lipids and lipid-like molecules (i.e., carnitines). In the current study the presence of L-palmitoylcarnitine was detected in the A. nodosum-treated group. Turunen et al. (19) detected sphinganine in dog saliva but not human saliva, and in the present study, sphinganine-1-phosphate was detected in the A. nodosum-treated group. These are two examples of possible concordance between the results of the two studies, but what must be noted—and was also pointed out by (19)—is that thousands of molecules detected results in hundreds of identifications. Thus, specific conclusions are not justified based on currently identified molecules.
The Authors of the current study are also aware of its limitations, especially in the field of metabolites identification. The identification of metabolites was carried out on the basis of the database indications above 80% probability of confirming a given structure. Molecules were identified only based on their molecular weight. Our metabolomic analysis used the MetaboAnalyst software to assign metabolites important in our analysis to well-described metabolic pathways. This analysis identified potential metabolites in a given metabolic pathway. Repetitions of m/z may be due to the involvement of metabolites with the same m/z in two different metabolic pathways. However, our studies were rather focused on showing the differences between the T0 vs. T30 groups and certainly the results of these analyses would require further confirmation of the validity of the data indicated. That is why in the Supplementary Table 1 we included all the raw data from the experiment which could help the readers to validate the results obtained.
In conclusion, the positive clinical effect of 30 days of A. nodosum supplementation on oral health status in dogs combined with the absence of many metabolites in the saliva of dogs on day 30 of supplementation suggest that brown algae inhibit or turn off some pathways that could lead to plaque or calculus development. Notably however, it cannot be determined whether these absences are a direct consequence of A. nodosum action or the influence of the extract on associated processes in the oral cavity. Metabolomic analyses identified clear changes after 30 days of supplementation, and the direction of these changes was completely different than in dogs that received a placebo treatment during the same period. The exact mechanism of A. nodosum is still unclear and warrants further study, but such studies must include analysis of dog saliva composition.
Data Availability Statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding authors.
Ethics Statement
All procedures performed during the study were conducted in accordance with standard veterinary care protocols and relevant Polish regulations (Art.1 ust.2 pkt1 Dz. U.2015 poz. 266), so the study did not require ethics committee approval. All dog owners provided written informed consent for the participation of their dogs in the study. Written informed consent was obtained from the owners for the participation of their animals in this study.
Author Contributions
JG, MJ, and US designed the scientific project. JW performed metabolomic tests and contributed in analyze of the results. JG performed research in animals. MJ made statistics. US helped editing. All authors contributed to the article and approved the submitted version.
Conflict of Interest
US is employed as a consultant and CEO at the company UKS Life Science AB. The remaining authors declare that the research was conducted in the absence of any commercial or financial relationship that could be construed as a potential conflict of interest.
Footnotes
Funding. This study was sponsored by Swedencare AB, Sweden. The funder covered costs of veterinary medical services, metabolomic studies, statistical analyze and publication fee. The funder was not involved in the study design, collection, analysis, interpretation of data, the writing of this article or the decision to submit it for publication.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fvets.2021.681951/full#supplementary-material
References
- 1.Wallis C, Pesci I, Colyer A, Milella L, Southerden P, Holcombe LJ, et al. A longitudinal assessment of periodontal disease in Yorkshire terriers. BMC Vet Res. (2019) 15:20. 10.1186/s12917-019-1923-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Harvey CE. Management of periodontal disease: understanding the options. Vet Clin North Am Small Anim Pract. (2005) 35:819–36. 10.1016/j.cvsm.2005.03.002 [DOI] [PubMed] [Google Scholar]
- 3.Gawor J, Jank M, Jodkowska K, Klim E, Svensson UK. Effects of edible treats containing Ascophyllum nodosum on the oral health of dogs: a double-blind, randomized, placebo-controlled single-center study. Front Vet Sci. (2018) 5:168. 10.3389/fvets.2018.00168 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.van Dijken JW, Koistinen S, Ramberg P. A randomized controlled clinical study of the effect of daily intake of Ascophyllum nodosum alga on calculus, plaque, and gingivitis. Clin Oral Investig. (2015) 19:1507–18. 10.1007/s00784-014-1383-2 [DOI] [PubMed] [Google Scholar]
- 5.Liebsch C, Pitchika V, Pink C, Samietz S, Kastenmüller G, Artati A, et al. The saliva metabolome in association to oral health status. J Dent Res. (2019) 98:642–51. 10.1177/0022034519842853 [DOI] [PubMed] [Google Scholar]
- 6.Eubanks DL, Woodruff KA. The Basics of Saliva. J Vet Dentistry. (2010) 27:266–7. 10.1177/089875641002700413 [DOI] [PubMed] [Google Scholar]
- 7.Furman RB, Niemiec BA. Salivation. In: Washabau RJ, Day MJ. editors. Canine and Feline Gastroenterology. London: Elsevier; (2013). p. 162–66. [Google Scholar]
- 8.Urbaniak GC, Plous S. Research Randomizer (Version 4.0). (2013). Available online at: http://www.randomizer.org (accessed April 23, 2018).
- 9.Muir WW. Considerations for general anesthesia. In: Tranquilli WJ, Thurmon JC, Grimm KG. editors. Lumb and Jones' Veterinary Anesthesia and Analgesia. 4th ed. St. Ames: Blackwell; (2007). p. 17–30. [Google Scholar]
- 10.Gawor J, Reiter AM, Jodkowska K. Influence of diet on oral health in cats and dogs. J Nutrition. (2006) 136:2021S−3S. 10.1093/jn/136.7.2021S [DOI] [PubMed] [Google Scholar]
- 11.Kennedy AD, Wittmann BM, Evans AM, Miller LAD, Toal DR, Lonergan S, et al. Metabolomics in the clinic: A review of the shared and unique features of untargeted metabolomics for clinical research and clinical testing. J Mass Spectrom. (2018) 53:1143–54. 10.1002/jms.4292 [DOI] [PubMed] [Google Scholar]
- 12.Gibney MJ, Walsh M, Brennan L, Roche HM, German B, van Ommen B. Metabolomics in human nutrition: opportunities and challenges. Am J Clin Nutr. (2005) 82:497–503. 10.1093/ajcn/82.3.497 [DOI] [PubMed] [Google Scholar]
- 13.Shah S. Salivaomics: the current scenario. J Oral Maxillofac Pathol. (2018) 22:375–81. 10.4103/jomfp.JOMFP_171_18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Pereira JL, Duarte D, Carneiro TJ, Ferreira S, Cunha B, Soares D, et al. Saliva NMR metabolomics: Analytical issues in pediatric oral health research. Oral Dis. (2019) 25:1545–54. 10.1111/odi.13117 [DOI] [PubMed] [Google Scholar]
- 15.Agatonovic-Kustrin S, Morton DW, Smirnov V, Petukhov A, Gegechkori V, Kuzina V, et al. Analytical strategies in lipidomics for discovery of functional biomarkers from human saliva. Dis Markers. (2019) 4:6741518. 10.1155/2019/6741518 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Assad DX, Mascarenhas ECP, de Lima CL, de Toledo IP, Chardin H, Combes A, et al. Salivary metabolites to detect patients with cancer: a systematic review. Int J Clin Oncol. (2020) 25:1016–36. 10.1007/s10147-020-01660-7 [DOI] [PubMed] [Google Scholar]
- 17.Gardner A, Carpenter G, So PW. Salivary metabolomics: from diagnostic biomarker discovery to investigating biological function. Metabolites. (2020) 10:47. 10.3390/metabo10020047 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Schirra HJ, Ford PJ. NMR-based metabolomics of oral biofluids. Methods Mol Biol. (2017) 1537:79–105. 10.1007/978-1-4939-6685-1_5 [DOI] [PubMed] [Google Scholar]
- 19.Turunen S, Puurunen J, Auriola S, Kullaa AM, Karkkainen O, Lohi H, et al. Metabolome of canine and human saliva: a non-targeted metabolomics study. Metabolomics. (2020) 16:90. 10.1007/s11306-020-01711-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lopes G, Sousa C, Valentao P, Andrade PB. Sterols in algae and health. In: Hernandez-Ledesma B, Herrero M, edited. Bioactive Compounds from Marine Foods: Plant and Animal Sources. Chapter: John Wiley & Sons, Ltd; (2013). p. 174–91. [Google Scholar]
- 21.Mudrika S, Muthukumar S, Suresh R. Correlation between salivary levels of stress related hormones and chronic periodontitis. J Int Clin Dental Res Org. (2014) 6:92–7. 10.4103/2231-0754.143488 [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding authors.