Abstract
Objectives
The Coronavirus Disease 2019 pandemic has affected the health care system significantly. We compare 2019 to 2020 to evaluate how trauma encounters has changed during the pandemic.
Methods
Retrospective analysis using a large US health care system to compare trauma demographics, volumes, mechanisms of injury, and outcomes. Statistical analysis was used to evaluate for significant differences comparing 2019 to 2020.
Results
Data was collected from 88 hospitals across 18 states. 169 892 patients were included in the study. There were 6.3% fewer trauma patient encounters in 2020 compared to 2019. Mechanism of injury was significantly different between 2019 and 2020 with less blunt injuries (89.64% vs. 88.39%, P < .001), more burn injuries (1.84% vs. 2.00%, P = .021), and more penetrating injuries (8.58% vs. 9.75%, P < .001). Compared to 2019, patients in 2020 had higher mortality (2.62% vs. 2.88%, P < .001), and longer hospital LOS (3.92 ± 6.90 vs. 4.06 ± 6.56, P < .001).
Conclusion
The COVID-19 pandemic has significantly affected trauma patient demographics, LOS, mechanism of injury, and mortality.
Keywords: special topics, trauma, trauma acute care
Introduction
The Coronavirus Disease 2019 (COVID-19) pandemic has significantly affected the United States health care system including trauma centers and patients.1-3 During the initial months of the pandemic, domestic violence calls have increased by 25% while traffic congestion has diminished accompanying a >60% decrease in local travel in the United States.4-6 While some areas were seeing decreases in motor vehicle accidents, motor vehicle fatalities were increasing likely from the public driving faster on highways.7,8 A pandemic of this magnitude is rare and provides a critical and unique time to evaluate trends in trauma. Previous studies have shown decreases in trauma admissions and increases in penetrating and violence related trauma.9-16 Evaluation of the United States traumatic injuries during 2020 is warranted to evaluate how fluctuations has changed during a unique period in history and help anticipate future trends during similar situations.
Methods
Monthly trauma volumes from 88 hospitals in 18 states were queried from a large US health care system database from January 2019 to December 2020 identifying 172,061 patients. Patients with missing data on gender (n = 371), Injury Severity Score (ISS) (n = 202), not having admission dates from January 2019 to December 2020 (n = 21), and missing ICD-10 codes on mechanism of injury (n = 1575) were excluded. A total of 169 892 patients with 173 936 trauma encounters were included to compare monthly trauma volumes in the pre-pandemic period (January to December 2019) to the pandemic period (January to December 2020). Data on age, sex, race/ethnicity, hospital length of stay (LOS), ISS, and discharge description were extracted. Mechanism of injury was classified based on the ICD-10 codes. Categorical variables were reported as percentages and continuous variables reported as means. Chi-square tests were used to compare categorical variables and two-sample t-test was used to compare continuous variables. P-value threshold of P < .05 was used for 2-tailed tests. The study was approved by the hospitals Institutional Review Board. Data analysis was performed using SAS 9.4 and R version 4.0.2.
Results
Data was collected from 88 hospitals across 18 states (CA, CO, FL, GA, ID, IN, KS, KY, LA, MO, MS, NH, NV, SC, TN, TX, UT, VA). 169 892 trauma patients were included in the study. There were 89 813 patients in 2019 and 84 123 patients in 2020 (Table 1). Trauma patients in 2020 were more likely to be male (56.60% vs. 57.44%, P < .001), African American or other race (10.45% vs. 10.96%, P < .001; 5.15% vs. 5.70% P < .001), more severely injured by ISS >12 (17.25% vs. 19.53% P < .001), have a higher mortality (2.62% vs. 2.88%, P < .001), and longer hospital LOS (3.92 ± 6.90 vs. 4.06 ± 6.56, P < .001).
Table 1.
Trauma Characteristics Comparing 2019 to 2020.
| Trauma patient characteristics | 2019 | 2020 | P value |
|---|---|---|---|
| Mean ± SD/n (%) | Mean ± SD/n (%) | ||
| No of encounters | 89 813 | 84 123 | |
| No of patients | 87 007 | 82 885 | |
| Age (mean) | 53.87 ± 24.01 | 53.87 ± 23.84 | .985 |
| Male (%) | 49 243 (56.60%) | 47 606 (57.44%) | <.001 |
| Race | |||
| White | 64 394 (74.01%) | 60 665 (73.19%) | .010 |
| African American | 9094 (10.45%) | 9084 (10.96%) | <.001 |
| Asian | 1601 (1.84%) | 1469 (1.77%) | .356 |
| Hispanic | 7436 (8.55%) | 6942 (8.38%) | .309 |
| Other | 4482 (5.15%) | 4725 (5.70%) | <.001 |
| ISS (mean) | 8.17 ± 7.50 | 8.72 ± 7.63 | <.001 |
| ISS ≤ 12 | 71 998 (82.75%) | 66 697 (80.47%) | <.001 |
| ISS > 12 | 15 009 (17.25%) | 16 188 (19.53%) | <.001 |
| Mechanism of injury | |||
| Blunt | 77 992 (89.64%) | 73 258 (88.39%) | <.001 |
| Burn | 1603 (1.84%) | 1655 (2.00%) | .021 |
| Penetrating | 7469 (8.58%) | 8081 (9.75%) | <.001 |
| LOS (mean) | 3.92 ± 6.90 | 4.06 ± 6.56 | <.001 |
| Discharge information | |||
| Mortality | 2279 (2.62%) | 2383 (2.88%) | .001 |
| Home | 52 974 (60.88%) | 50 462 (60.88%) | .994 |
| Hospice | 1290 (1.48%) | 1495 (1.80%) | <.001 |
| Facility/other hospitals | 5307 (6.10%) | 5640 (6.80%) | <.001 |
| Rehab | 21 209 (24.38%) | 19 366 (23.36%) | <.001 |
| Others | 3948 (4.54%) | 3539 (4.27%) | .007 |
Significant P-values bolded (P < .05).
Abbreviations: ISS, injury severity score; LOS, length of stay.
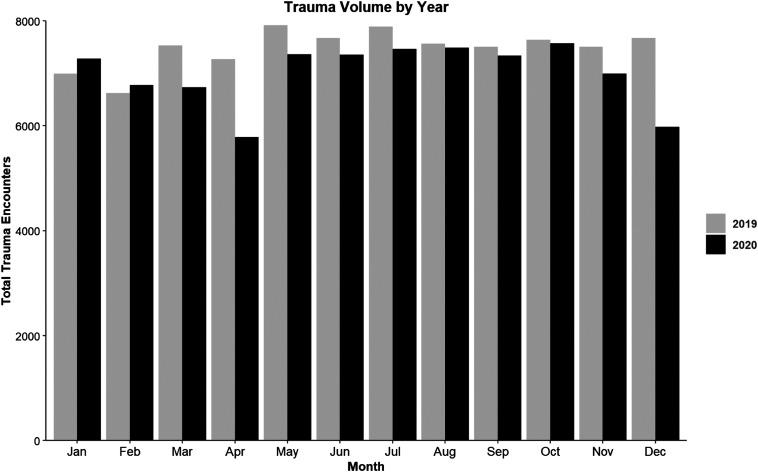
Compared to 2019, there was a 6.3% decrease in volume in 2020 with a decrease in volume beginning in March of 2020 that persisted the remainder of the year with a gradual increase to pre-COVID volumes (Figure 1). The initial 20.5% decrease in trauma volumes occurred in April 2020. A second decrease in trauma volume occurs in November 2020 with a nadir 22.1% decrease in trauma volume in December 2020.
Figure 1.
Trauma volume by month comparing 2019 to 2020.
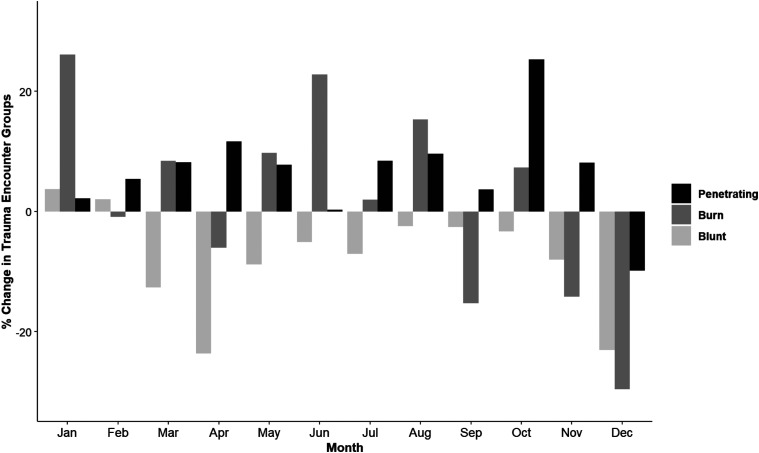
Significant changes in mechanism of injury and ISS begin in March (Table 2). Mechanism of injury are significantly different between 2019 and 2020 with less blunt injuries (89.64% vs. 88.39%, P < .001), more burn injuries (1.84% vs. 2.00%, P = .021), and more penetrating injuries (8.58% vs. 9.75%, P < .001). Penetrating trauma remains increased for 2020 compared to 2019 until December where there is a percentage decrease in all mechanisms of injury (Figure 2).
Table 2.
Trauma Characteristics by Month in 2019 and 2020.
| January | Feb | March | April | May | June | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 2019 | 2020 | P | 2019 | 2020 | P | 2019 | 2020 | P | 2019 | 2020 | P | 2019 | 2020 | P | 2019 | 2020 | P | |
| Mean ± SD/n (%) | Mean ± SD/n (%) | Mean ± SD/n (%) | Mean ± SD/n (%) | Mean ± SD/n (%) | Mean ± SD/n (%) | Mean ± SD/n (%) | Mean ± SD/n (%) | Mean ± SD/n (%) | Mean ± SD/n (%) | Mean ± SD/n (%) | Mean ± SD/n (%) | |||||||
| Total encounters | 6995 | 7276 | 6624 | 6772 | 7534 | 6735 | 7272 | 5784 | 7920 | 7364 | 7674 | 7356 | ||||||
| No of patients | 6704 | 7116 | 6358 | 6633 | 7285 | 6585 | 7006 | 5657 | 7672 | 7229 | 7454 | 7239 | ||||||
| Age (mean) | 56.54 ± 23.81 | 55.89 ± 23.98 | .105 | 56.16 ± 23.63 | 56.44 ± 23.68 | .488 | 54.52 ± 23.87 | 54.80 ± 23.83 | .481 | 54.06 ± 24.42 | 53.80 ± 24.04 | .552 | 53.31 ± 24.16 | 53.36 ± 23.79 | .896 | 53.36 ± 23.82 | 52.68 ± 23.81 | .079 |
| Male (%) | 3858 (55.15%) | 934 (54.07%) | .199 | 3598 (54.32%) | 3648 (53.87%) | .614 | 4272 (56.70%) | 3840 (57.02%) | .719 | 4083 (56.15%) | 3402 (58.82%) | .002 | 4527 (57.16%) | 4306 (58.47%) | .104 | 4351 (56.70%) | 4309 (58.58%) | .021 |
| ISS (mean) | 8.30 ± 7.67 | 8.38 ± 7.41 | .557 | 8.35 ± 7.70 | 8.42 ± 7.11 | .550 | 8.33 ± 7.69 | 8.81 ± 7.60 | <.001 | 8.27 ± 7.57 | 9.00 ± 7.82 | <.001 | 8.28 ± 7.76 | 8.74 ± 7.80 | <.001 | 8.24 ± 7.56 | 8.85 ± 8.02 | <.001 |
| ISS > 12 | 1271 (18.17%) | 1287 (17.69%) | .466 | 1180 (17.81%) | 1220 (18.02%) | .778 | 1382 (18.34%) | 1344 (19.96%) | .015 | 1253 (17.23%) | 1203 (20.80%) | <.001 | 1402 (17.70%) | 1443 (19.60%) | .003 | 1374 (17.90%) | 1488 (20.23%) | <.001 |
| LOS (mean) | 4.08 ± 6.15 | 4.17 ± 7.52 | .417 | 4.11 ± 7.59 | 4.23 ± 6.77 | .342 | 4.03 ± 7.26 | 3.93 ± 6.57 | .403 | 3.81 ± 7.62 | 3.89 ± 6.66 | .531 | 3.80 ± 6.38 | 3.90 ± 6.53 | .353 | 3.78 ± 6.59 | 4.05 ± 6.44 | .011 |
| Mortality | 181 (2.59%) | 178 (2.45%) | .628 | 188 (2.84%) | 146 (2.16%) | .013 | 199 (2.64%) | 206 (3.06%) | .148 | 186 (2.56%) | 180 (3.11%) | .064 | 203 (2.56%) | 181 (2.46%) | .716 | 169 (2.20%) | 214 (2.91%) | .007 |
| Mechanism of injury | ||||||||||||||||||
| Blunt | 6276 (89.72%) | 6509 (89.46%) | .627 | 6016 (90.82%) | 6138 (90.64%) | .737 | 6805 (90.32%) | 5946 (88.29%) | <.001 | 6557 (90.17%) | 5006 (86.55%) | <.001 | 7068 (89.24%) | 6443 (87.49%) | .001 | 6843 (89.17%) | 6494 (88.28%) | .089 |
| Burn | 134 (1.92%) | 169 (2.32%) | .103 | 111 (1.68%) | 110 (1.62%) | .868 | 131 (1.74%) | 142 (2.11%) | .122 | 116 (1.60%) | 109 (1.88%) | .232 | 144 (1.82%) | 158 (2.15%) | .163 | 127 (1.65%) | 156 (2.12%) | .041 |
| Penetrating | 585 (8.36%) | 598 (8.22%) | .778 | 497 (7.50%) | 524 (7.74%) | .632 | 598 (7.94%) | 647 (9.61%) | <.001 | 599 (8.24%) | 669 (11.57%) | <.001 | 708 (8.94%) | 763 (10.36%) | .003 | 704 (9.17%) | 706 (9.60%) | .388 |
| Race | ||||||||||||||||||
| White | 5368 (76.74%) | 5450 (74.90%) | .028 | 5030 (75.94%) | 5064 (74.78%) | .200 | 5588 (74.17%) | 4960 (73.65%) | .932 | 5412 (74.42%) | 4226 (73.06%) | .233 | 5845 (73.80%) | 5422 (73.63%) | .798 | 5708 (74.38%) | 5323 (72.36%) | .008 |
| African American | 687 (9.82%) | 722 (9.92%) | .801 | 613 (9.25%) | 630 (9.30%) | .904 | 799 (10.85%) | 717 (10.96%) | .859 | 738 (10.36%) | 641 (11.38%) | .069 | 829 (10.72%) | 768 (10.73%) | 1.000 | 816 (10.88%) | 863 (12.03%) | .031 |
| Asian | 121 (1.73%) | 150 (2.06%) | .155 | 105 (1.59%) | 131 (1.93%) | .135 | 162 (2.20%) | 115 (1.76%) | .071 | 106 (1.46%) | 78 (1.35%) | .682 | 148 (1.91%) | 113 (1.58%) | .136 | 120 (1.60%) | 120 (1.67%) | .778 |
| Hispanic | 522 (7.46%) | 620 (8.52%) | .018 | 543 (8.20%) | 585 (8.64%) | .347 | 598 (8.12%) | 564 (8.62%) | .302 | 648 (9.10%) | 490 (8.70%) | .455 | 685 (8.86%) | 610 (8.52%) | .490 | 635 (8.47%) | 627 (8.74%) | .575 |
| Others | 297 (4.25%) | 334 (4.59%) | .337 | 333 (5.03%) | 362 (5.35%) | .429 | 387 (5.14%) | 379 (5.63%) | .207 | 368 (5.06%) | 349 (6.03%) | .017 | 413 (5.21%) | 451 (6.12%) | .016 | 395 (5.15%) | 423 (5.75%) | .111 |
Significant P-values bolded (P < .05).
Abbreviations: ISS, injury severity score; LOS, length of stay.
Figure 2.
Trauma mechanism comparing 2019 to 2020.
Patients in 2020 had a longer hospital LOS in days (3.92 ± 6.90 vs. 4.06 ± 6.56, P < .001). This significant difference appeared from June to September. There was a higher percentage mortality (2.62% vs. 2.88%, P = .001) and patients discharged to hospice (1.48% vs. 1.80%, P < .001) in 2020 compared to 2019.
Discussion
Since the COVID-19 pandemic, trauma volumes of hospitals have substantially decreased. This is suspected to be largely due to the regulations and behavioral changes among the public. Our study showed that within the 2020 COVID-19 pandemic, an approximately 6% cumulative decrease in trauma volume has occurred with the largest decreases occurring in April and December 2020. This decrease begins in March, possibly corresponding with stay-at-home orders. This mirrors other studies showing decreased trauma volumes across the United States and among other countries. Kamine et al17 showed that trauma volumes decreased 57.4% during February to April 2020 in comparison to previous years in their Level II trauma hospital in New Hampshire. Sherman et al showed decreased trauma volumes by 70% at a Level I trauma center in Louisiana during the pandemic during March to May 2020.18 Qasim et al found a 20.3% decrease in trauma volume in Philadelphia during March to May 2020.19 Matthay et al16 found a 50% decrease in trauma volume after the stay-at-home order from March to June 2020 in comparison to the previous months in San Francisco. Similar drops in trauma volume occurred in Los Angeles CA during January to June 2020 while a return to pre pandemic volumes occur.20 While most studies evaluate the early pandemic up to the first 6 months, our study evaluates the entirety of 2020 as the decrease in trauma volume becomes less significant as the year progresses. A second inflection in trauma volume occurs in November 2020, likely corresponding to the third and largest wave of COVID-19 positivity.21 Past epidemics have seen similar changes. In the previous 2003 SARS epidemic in Taiwan, emergency departments visits decreased by 51% and trauma visits decreased by 57.6% but recovered to pre-epidemic numbers in July, the same month that the World Health Organization removed Taiwan from the list of SARS epidemic countries.22,23
This study found an increase percentage of penetrating trauma that persisted for the pandemic. Many other studies regarding trauma have found similar increases in penetrating trauma. Southern California24 penetrating trauma increased from 10.3% to 13.0%, A Los Angeles County study20 separately identified increase in penetrating trauma 15.4% to 15.7%, Philadelphia19 penetrating trauma increased 17.5% to 23.7%, and San Francisco16 violence related injuries increased 17% to 46%. This study identified a concurrent decrease in blunt trauma accompanying the increased proportions of penetrating trauma which is similar to previous studies. This may suggest that while stay at home orders may affect blunt trauma such as motor vehicle accidents, violence related injuries continue and may be exacerbated by socioeconomic stressors inflicted by the pandemic. A second inflection in trauma volumes and mechanism of injury occurs in November 2020 during the height of the third wave of positive COVID-19 cases. This decrease in volume by 22.1% in December accompanies a decrease in all mechanisms of injury; 23.1% blunt, 29.6% in burns, and 9.8% penetrating. This is the first month during the pandemic where penetrating trauma has decreased. Changes in trauma volume and mechanism during the beginning of 2020 may be attributed to stay-at-home orders while the second decrease may be from other causes and require further investigation.
There were significant changes in hospital LOS and mortality in 2020. The difference in hospital LOS is relatively small and coincides with no difference in ICU LOS found in previous reports.20 While mortality differences fluctuated throughout the year, the greatest mortality among trauma patients in 2020 occurred in March (3.06%) and April (3.11%), then again in November (3.10%) and December (3.56%). The peaks in mortality occur during the initial stay-at-home orders and the third peak of COVID-19 positivity yet the explanation for this change in mortality is difficult to ascertain. Kaufman et al25 found that 2.6% of trauma patients tested positive for COVID-19 and had an increased risk of death (OR 6.05, 95% CI 2.29, 15.99) when matched with COVID-19 negative trauma patients. Conversely, Ghafil et al20 found no difference in mortality during the COVID-19 pandemic. Further studies regarding the change in outcomes during the COVID-19 pandemic are warranted as patient and health care system factors may help explain these differences.
Limitations present in this study include the granularity and inability to identify more specific mechanisms of injury such as motor vehicle crashes, gunshot wounds, or knife wounds. While most previous studies are focused in highly populated cities, this study involves multiple hospitals spread among multiple states therefore the distribution of the collected data may affect results. Additionally, hospitals may not have equal experiences as state and local responses to the COVID-19 pandemic have varied.
Conclusion
Trauma volumes have dramatically changed during the COVID-19 pandemic with an initial decrease in March and a second decrease in November. Mechanism of injury has also seen dramatic changes with increases in penetrating trauma. Lastly, trauma mortality appears to have fluctuated with the COVID-19 pandemic. Further studies detailing these unique inflection points may help describe how human behavior affects trauma patients.
Footnotes
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1.Ashford RU, Nichols JS, Mangwani J. Annotation: The COVID-19 pandemic and clinical orthopaedic and trauma surgery. J Clin Orthop Trauma. 2020;11(3):504-505. doi: 10.1016/j.jcot.2020.04.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Khazaei M, Asgari R, Zarei E, Moharramzad Y, Haghighatkhah H, Sanei Taheri M. Incidentally diagnosed COVID-19 infection in trauma patients; a clinical experience. Arch Acad Emerg Med. 2020;8(1):e31. [PMC free article] [PubMed] [Google Scholar]
- 3.De Vitis R, Passiatore M, Perna A, Proietti L, Taccardo G. COVID-19 contagion and contamination through hands of trauma patients: what risks and what precautions?. J Hosp Infect. 2020;105(2):354-355. doi: 10.1016/j.jhin.2020.03.037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pamer M, Wolfe C. Violence inside the home becomes a concern in O.C. as ‘adverse effect’ of stay-at-home order. In: KCBS TV in Los Angeles (KTLA5). 2020. https://ktla.com [Google Scholar]
- 5.Reed T. COVID-19 Eliminates Congestion in American Cities. INRIX. 2020. https://inrix.com [Google Scholar]
- 6.Shilling F. Special Report 3: Impact of COVID19 Mitigation on Traffic, Fuel Use and Climate Change. [Internet]. Davis: University of California; 2020. [cited 2021 January 1]. https://roadecology.ucdavis.edu [Google Scholar]
- 7.Kopf D. Traffic Collisions Are Plummeting in Several US Cities. [Internet]. New York, NY: Quartz. 2020. [cited 2021 January 2]. https://qz.com/1822492/traffic-accidents-are-plummeting-because-of-the-pandemic [Google Scholar]
- 8.Feese J. Absent Traffic Jams, Many Drivers Getting More Reckless. GHSA. 2020. https://www.ghsa.org [Google Scholar]
- 9.DiFazio LT, Curran T, Bilaniuk JW, et al. The Impact of the COVID-19 pandemic on hospital admissions for trauma and acute care surgery. Am Surg. 2020;86(8):901-903. doi: 10.1177/0003134820939904 [DOI] [PubMed] [Google Scholar]
- 10.Aljuboori Z, Sieg E. The early effects of social distancing resultant from COVID-19 on admissions to a level I trauma center. Injury. 2020;51(10):2332. doi: 10.1016/j.injury.2020.06.036 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Jain A, Goyal V, Varma C. Reflection of epidemiological impact on burden of injury in tertiary care centre, pre-COVID and COVID Era: “lockdown, a good fortune for saving life and limb”. Indian J Surg. 2020:1-5. doi: 10.1007/s12262-020-02640-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Harris D, Ellis DY, Gorman D, Foo N, Haustead D. Impact of COVID-19 social restrictions on trauma presentations in South Australia. Emerg Med Australasia (EMA). 2021;33(1):152-154. doi: 10.1111/1742-6723.13680 [DOI] [PubMed] [Google Scholar]
- 13.Christey G, Amey J, Campbell A, Smith A. Variation in volumes and characteristics of trauma patients admitted to a level one trauma centre during national level 4 lockdown for COVID-19 in New Zealand. N Z Med J. 2020;133(1513):81-88. [PubMed] [Google Scholar]
- 14.MacDonald DRW, Neilly DW, et al. Effects of the COVID-19 lockdown on orthopaedic trauma: a multicentre study across Scotland. Bone Jt Open. 2020;1(9):541-548. doi: 10.1302/2633-1462.19.BJO-2020-0114.R1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Fahy S, Moore J, Kelly M, Flannery O, Kenny P. Analysing the variation in volume and nature of trauma presentations during COVID-19 lockdown in Ireland. Bone Jt Open. 2020;1(6):261-266. doi: 10.1302/2046-3758.16.BJO-2020-0040.R1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Matthay ZA, Kornblith AE, Matthay EC, et al. The distance study: determining the impact of social distancing on trauma epidemiology during the COVID-19 epidemic-an interrupted time-series analysis. J Trauma Acute Care Surg. 2021;90(4):700-707. doi: 10.1097/TA.0000000000003044 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kamine TH, Rembisz A, Barron RJ, Baldwin C, Kromer M. Decrease in trauma admissions with COVID-19 pandemic. West J Emerg Med. 2020;21(4):819-822. doi: 10.5811/westjem.2020.5.47780 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sherman WF, Khadra HS, Kale NN, Wu VJ, Gladden PB, Lee OC. How did the number and type of injuries in patients presenting to a regional level i trauma center change during the COVID-19 pandemic with a stay-at-home order?. Clin Orthop Relat Res. 2021;479(2):266-275. doi: 10.1097/CORR.0000000000001484 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Qasim Z, Sjoholm LO, Volgraf J, et al. Trauma center activity and surge response during the early phase of the COVID-19 pandemic-the Philadelphia story. J Trauma Acute Care Surg. 2020;89(4):821-828. doi: 10.1097/TA.0000000000002859 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ghafil C, Matsushima K, Ding L, Henry R, Inaba K. Trends in trauma admissions during the COVID-19 pandemic in Los Angeles county, California. JAMA Netw Open. 2021;4(2):e211320. doi: 10.1001/jamanetworkopen.2021.1320 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.“COVID Data Tracker” . Center for Disease Control and Prevention. 2021. https://covid.cdc.gov/covid-data-tracker/#datatracker-home [Google Scholar]
- 22.Huang HH, Yen DH, Kao WF, Wang LM, Huang CI, Lee CH. Declining emergency department visits and costs during the severe acute respiratory syndrome (SARS) outbreak. J Formos Med Assoc. 2006;105(1):31-37. doi: 10.1016/S0929-6646(09)60106-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Huang CC, Yen DH, Huang HH, et al. Impact of severe acute respiratory syndrome (SARS) outbreaks on the use of emergency department medical resources. J Chin Med Assoc. 2005;68(6):254-259. doi: 10.1016/S1726-4901(09)70146-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Yeates EO, Grigorian A, Barrios C, et al. Changes in traumatic mechanisms of injury in Southern California related to COVID-19: penetrating trauma as a second pandemic. J Trauma Acute Care Surg. 2021;90(4):714-721. doi: 10.1097/TA.0000000000003068 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kaufman EJ, Ong AW, Cipolle MD, et al. The Impact of COVID-19 infection on outcomes after injury in a state Trauma system. J Trauma Acute Care Surg. 2021. doi: 10.1097/TA.0000000000003310 [DOI] [PubMed] [Google Scholar]