Abstract
The endocrine hospitalist and inpatient diabetes management team increases access to endocrinology consultations and improves glycemic control and quality metrics such as length of stay and hospital readmission. Enhanced glycemic care is needed in both academic and community hospital settings. Endocrine fellowship programs should implement endocrine hospitalist rotations with emphasis on training endocrine fellows to deliver fast-paced inpatient endocrine care. Entrepreneurship, innovation, and a “start-up” culture within the field of Endocrinology should be encouraged and supported by healthcare systems.
Keywords: endocrine, hospitalist, endocrinology, diabetes, quality
Diabetes Care in the Hospital Setting
Diabetes in hospitalized patients is associated with increased length of stay and readmission, resulting in increased costs to the healthcare system.1-5 In 2017, the last year for which such information is available, the total estimated cost of diabetes care in the United States exceeded $327 billion, $97 billion of which was spent in an inpatient setting.6,7 Care for people diagnosed with diabetes accounts for 1 in 4 healthcare dollars spent.7 The rate of hyperglycemic emergencies has been increasing this past decade.8 In 2013 Draznin and the Planning Research in Inpatient Diabetes consortium outlined the key aspects of inpatient glucose management and called to action leading endocrine societies, urging further progress in the science of inpatient diabetes management.9 The American Diabetes Association has been recommending for several years to “consult with specialized diabetes or glucose management teams” when caring for hospitalized patients with diabetes.10-13 Despite numerous efforts by the endocrine and diabetes community to improve diabetes care for hospitalized patients, care remains suboptimal. Many hospitals still rely mostly on correctional/sliding scale rapid-acting insulin, a potentially harmful “reflexive behavior” which compares unfavorably to physiologically scheduled insulin.9,14,15 Academic and community centers are both still lacking in optimized diabetes management.16,17 While some academic institutions may have additional resources for diabetes, most patients do not have access to these resources and are cared for at community hospitals (5198 out of a total of 6146 hospitals in the United States).18
What Is the Fastest-Growing Medical Specialty in the United States?
During the mid-90s, hospitals were encouraged to enhance efficiency without sacrificing the quality of care. The role of hospitalist emerged as an elegant response to this challenge. Hospitalists emphasize the improvement of systems of care, with the anticipated benefits of reduced cost, shortened length of stay, and enhanced quality of care and patient satisfaction.19,20 Most of my internal medicine residency colleagues became hospitalists. Their jobs vary considerably. They may have a shift-based “7-day on and 7-day off” schedule model21 with a high earnings potential. A growing number of fellowships help to infuse academic spirit and scholarship into daily hospitalist routine.22 During the latter part of my endocrinology fellowship, I was moonlighting as a hospitalist on weekends at Suburban Hospital, a member of Johns Hopkins Medicine. This 240-bed community hospital is conveniently located across the street from the National Institutes of Health (NIH) Clinical Center in Bethesda, Maryland. Every fourth patient who came to the hospital for any reason presented with diabetes. My hospitalist colleagues knew that I was a budding endocrinologist, and they kept asking me questions, such as: “How do I manage this patient on an insulin pump?” “How do I transition this patient from intravenous to subcutaneous insulin?” or “What do you think about this elevated TSH?”
I enjoyed my time as a hospitalist but wanted to focus on innovative endocrine issues. In August 2014, I met with the hospital leaders and discussed a potential opportunity to join the team as a hospitalist. I asked if I could alternate between 7 days of hospitalist work and 7 days of endocrinology work. In response, I was asked to consider a “different role which would enable me to do endocrinology work while at the hospital.” I was advised to create a business proposal for this initiative. I was immediately confronted with the most important question: How many patients would I see per day [ie, how many relative value units could I generate to offset the expense of my salary and benefits]? Fortunately, I received incredible support from the Division of Endocrinology, Diabetes and Metabolism at Johns Hopkins University School of Medicine and the Johns Hopkins Community Physicians (JHCP), who helped me refine the business proposal ideas while augmenting and strengthening the academic aspects of the initiative. My mentors from the NIH provided invaluable support for my “clinical start-up” and encouraged me to think outside of the box.
Branding of the Endocrine Hospitalist Program
I needed a branding strategy. I decided to focus on inpatient diabetes first. Multiple successful models have described the inpatient diabetes management team approach1,23-34 (Figure 1). I initially used a model from the Johns Hopkins Hospital with which I was most familiar.29,34. Briefly, this model engages the staff and hospital leadership in the importance of inpatient glycemic management and focuses on educating staff involved in the care of patients with diabetes through structured knowledge dissemination.29 The core diabetes team consists of advanced practice providers who deliver diabetes consultations and a supervising endocrinologist.29 However, I quickly realized that being the only endocrinologist in the community hospital, one is obliged to become something more than a diabetologist. I often think of myself as a “handyman.” I can work up and manage hyponatremia, abnormal TSH levels, adrenal masses, and extreme hyper- and hypoglycemia. The head of business operations assisted me in creating a billing area code. I was trying to explain to her that I will be “doing Endocrine consultations while working as a Hospitalist.” She first proposed the title of “Endocrine Hospitalist.”
Figure 1.
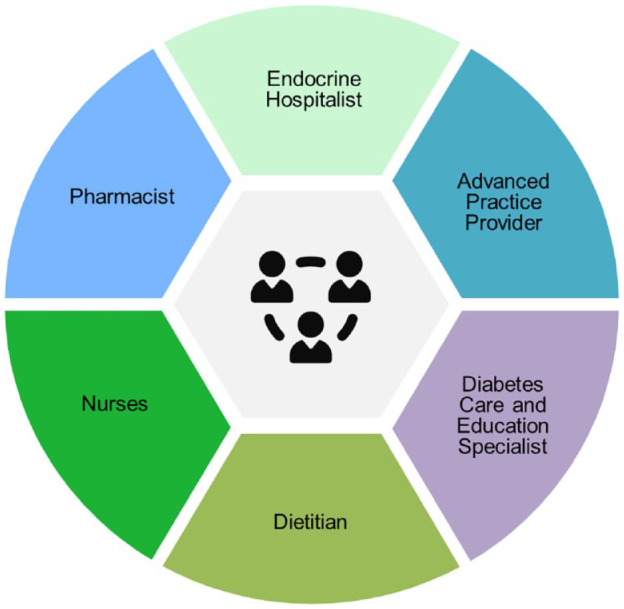
Simplified structure of the endocrine hospitalist/inpatient diabetes management team (Adapted by permission from Springer Nature Customer Service Centre GmbH: Springer Nature [Current Diabetes Reports] [The Financial Impact of an Inpatient Diabetes Management Service]. Haque WZ, Demidowich AP, Sidhaye A, Golden SH, Zilbermint M. [COPYRIGHT] (2021).
What Is an Endocrine Hospitalist?
The definition of an endocrine hospitalist is an endocrinology-trained physician (or advanced practice provider) whose subspecialty interest is in the management of inpatients with diabetes and various endocrine disorders, without having major outpatient responsibilities. Endocrine hospitalists provide consultations for patients in the emergency department, ward floors, and intensive care units. Endocrine hospitalist’s tasks are summarized in Figure 1.
Building the Endocrine Hospitalist Program from Scratch
Using my expertise and skills as a community organizer and hospitalist, I built the program, which relied heavily on volunteer work provided by my hospital colleagues. I organized a multidisciplinary Glucose Steering Committee. Briefly, this is an interdisciplinary team consisting of an endocrinologist, pharmacist, nurse educators, transition guide nurses, community health and wellness nurses, dietitian, information technology specialist, patient and family advisor, and quality improvement representative.1,35
The committee developed and implemented hospital-wide glucose policies and initiatives, providing targeted education and support to facilitate policy acceptance.1,29,31,34-36 While the Endocrine Hospitalist program was heavily focused on diabetes (Figure 2), I also took the time to develop a relationship with cardiothoracic surgeons, neurosurgeons, and ear, nose, throat (ENT) specialists. Additionally, I continued my close collaboration with the endocrine surgery teams at the NIH Clinical Center and Johns Hopkins Hospital.
Figure 2.

Endocrine hospitalist’s tasks.
I used to wake up early in order to be at the hospital by 6:45 am to join the “nursing change of shift report” and educate nurses on the evidence-based hypoglycemia protocol,35 how to use an insulin pen, the purpose of basal-bolus insulin therapy,36 and dynamic endocrine tests. The education of my peers was important as well. I organized “lunch and learns” for hospitalists and advanced nurse practitioners: gathering in groups of 5 to discuss diabetes discharge planning, insulin pumps, and new antidiabetes medications. Very practical information was shared, such as the necessity of ordering insulin pen needles together with insulin pens. This took some of my hospitalist colleagues by surprise. Finally, my team organized multiple half-day diabetes symposia for primary care physicians in the community.1
Discharge Planning for Hospitalized Patients with Diabetes
Initiating a long-term management plan for diabetes during the transition to outpatient for the patient living with diabetes is one of the key features of the Endocrine Hospitalist program. My team had complete responsibility for discharge planning, addressing all of the patient’s diabetes needs.1 We placed all the diabetes-related orders: pen needles, lancets, glucometer strips, glucometers. The team counseled patients about insulin therapy and the use of the newer classes of antidiabetes medications, prescribed for the management of diabetes comorbidities. We especially ensured that patients got the type of insulin that was covered by their insurance plan once they were discharged from the hospital. We arranged an endocrinology follow-up for most patients with complex cases and met with many community endocrinologists and their medical practice administrators in the area. We made “handshake” agreements to make sure that all recently discharged patients had an appropriate follow-up within 1-3 weeks. After 2 years, JHCP expanded the local endocrine practice and added a nurse practitioner who now sees most of our discharged patients with diabetes.
No Margin, No Mission?
Did the Endocrine Hospitalist program have an impact on the length of stay and 30-day readmission rates of patients who were comanaged by our specialized diabetes team? During the first 17 months of our program, we had a total of 4654 admitted patients with diabetes, while endocrine hospitalists comanaged 18.3% of the patients.1 We found that the 30-day readmission of patients comanaged by our team decreased by 10.7% for the patients comanaged by the diabetes team.1 The length of stay decreased by 27%.1 We calculated a cost savings of $953 000 associated with this outcome.1 Glycemic control may have improved as well. Carter et al. reported the frequency of hypoglycemia significantly decreased at Suburban Hospital from 7.5% in January 2016 to 3.9% in September 2019 (P = .001) with an estimated cost of care savings of $98 635.35 After the expansion and replication of the program to Howard County General Hospital, another community hospital within the Johns Hopkins Health System, Demidowich and colleagues reported that hyperglycemia at this institution decreased among patients comanaged by endocrine hospitalists (53.8%-42.5%, P < .0001), though no change in length of stay or readmission was noted.32 The authors speculated that other issues such as barriers to care, medical literacy, and/or lack of health insurance may have contributed to a lack of reduction in the length of stay in that study. Overall, our findings were consistent with other studies on trends in patients with diabetes and the impact on quality metrics.31,33,37,38
The Maryland Hospital System and the Importance of Program Expansion
The Maryland Hospital system operates somewhat differently than the rest of the country. In 2014, the state of Maryland started a new “all-payer model” in collaboration with the Centers for Medicare and Medicaid services.39,40 The model limits all-payer per capita hospital growth, including inpatient and outpatient care, focused on readmission reductions and incentives to limit overall hospital expenditures.40 Another Maryland initiative started in 2014, called a “global budget,” gives each hospital an annual global budget for inpatient, outpatient, and emergency department care. This initiative incentivizes each hospital in Maryland to reduce readmissions and hospital utilization.39,40 The rest of the United States is following the Hospital Readmissions Reduction Program, a Medicare value-based purchasing program (ie, paying for value, defined as the health outcomes or quality achieved in relation to the costs of the care provided) that encourages hospitals to improve care coordination and reduce avoidable readmissions.41-43 Since the expansion of our initiative to Howard County General Hospital,32 we have initiated talks with other institutions in Maryland and beyond about expanding our model.
Endocrine Hospitalists During the COVID-19 Pandemic
In response to the exigencies imposed on our team by the COVID-19 pandemic, we were able to successfully deploy an inpatient endocrine telemedicine service. Patients were provided with a tablet computer and we connected with them via Zoom.44 Instructions and infographics on how to connect with patients via the telemedicine platform have been provided to the nursing and medical staff. However, due to a surge in patients, technical challenges, inadequate training, and limited computer literacy, this pilot project was set aside. The same technology is now being used occasionally for late-evening consultations in the emergency departments, as well as interhospital cross-coverage. We offer (and bill for) virtual inpatient consultations, eliminating the need to go to the hospital in-person.
Advantages of Being an Endocrine Hospitalist
My schedule is usually flexible, although I prefer to start early, at around 7 am. Most discharge decisions are made by 11 am, and hence my team has to prepare a comprehensive discharge diabetes plan by that time. Our overhead is modest: we do not need an extra nurse to check vital signs since every inpatient has a nurse and we have no medical assistants. We do not require major medical supplies. The number of patient phone calls and prior authorizations is limited and we handle these ourselves. Importantly, there are endless opportunities for quality improvement research and teaching, especially the teaching of nurses and advanced practice practitioners.
Challenges
As with any other initiative, endocrine hospitalists have experienced challenges. It has not been easy to obtain data on key quality and financial metrics. Case volumes are frequently unknown; fee-for-service/per encounter dollar amounts had to be estimated for the first 2 years until the program had matured. Finally, this initiative requires an upfront investment, like any other healthcare “start-up,” and continued support. Why are other community hospitals reluctant to implement similar programs? Could it be that endocrinology is considered an “outpatient” specialty? Or perhaps, endocrinologists may not have enough business/financial skills to put together a business plan?34,45 Could there be a financial explanation? Endocrine hospitalists may not be able to generate enough revenue through billings to cover the entire cost of salaries and benefits, even if the impact on quality metrics is significant.
The Future of the Endocrine Hospitalist Program
This commentary is the first detailed description of the Endocrine Hospitalist program setup and experience. I hope that other institutions will use this as a blueprint in setting up their programs.
The Endocrine Hospitalist program and diabetes management teams are the “new standard” and represent the future in our field. The “old model,” where an outpatient endocrinologist would come in after a full clinic day to see the inpatient consults, is likely to wane. Enhanced glycemic management is needed both in academic and community settings. Endocrine fellowship programs may consider implementing endocrine hospitalist rotations, with the focus on training the future generation of endocrine fellows who are particularly concentrated on delivering inpatient endocrine care. I anticipate that many other subspecialists will become hospitalists as well. While most of the endocrinology jobs in the United States are employment based, entrepreneurship, innovation, and “start-up” culture within the healthcare systems should be encouraged.
Acknowledgments
The author thanks David C. Klonoff for the invitation to write the commentary and for guidance through this topic and manuscript preparation; Andrew P. Demidowich for the friendship, inspiration, development, and growth of the Endocrine Hospitalist model at Howard County General Hospital and beyond; Mahsa Motevalli and Kristine Batty for infusing nursing philosophy and enhancing the model of care delivery; Atul Rohatgi and Eric Park for assistance and support in developing the Endocrine Hospitalist initiative; Sherita H. Golden, Paul W. Ladenson, Rexford S. Ahima, and Nestoras N. Mathioudakis for providing a successful inpatient diabetes management model and the support from the Johns Hopkins University School of Medicine; Constantine A. Stratakis and Maya B. Lodish for mentorship and friendship; Jacky Schultz, LeighAnn Sidone, Mohammed Shafeeq Ahmed, Eric Dobkin, Sunil Vasudevan, Thomas Stewart, Joseph Linstrom, Eric E. Howell, Leo Rotello, and Patricia Wachter for providing endless support for the Endocrine Hospitalist initiative; Robert Rothstein for providing continuous support and sharing his vision for the program; endocrine moonlighters and members of Glucose Steering Committees at Suburban and Howard County General Hospitals; Maya Nadison for the assistance with figures.
Footnotes
Declaration of Conflicting Interests: The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: The author declares consulting for the Guidepoint and G.L.G.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Mihail Zilbermint  https://orcid.org/0000-0003-4047-7260
https://orcid.org/0000-0003-4047-7260
References
- 1. Mandel SR, Langan S, Mathioudakis NN, et al. Retrospective study of inpatient diabetes management service, length of stay and 30-day readmission rate of patients with diabetes at a community hospital. J Community Hosp Intern Med Perspect. 2019;9(2):64-73. doi: 10.1080/20009666.2019.1593782 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Levetan CS, Passaro M, Jablonski K, Kass M, Ratner RE. Unrecognized diabetes among hospitalized patients. Diabetes Care. 1998;21(2):246-249. [DOI] [PubMed] [Google Scholar]
- 3. Gaines M, Pratley RE. Impact of Hyperglycemia on 30-Day Readmission Rates. American Diabetes Association; 2018. [Google Scholar]
- 4. Seringa J, Marques AP, Moita B, Gaspar C, Raposo JF, Santana R. The impact of diabetes on multiple avoidable admissions: a cross-sectional study. BMC Health Serv Res. 2019;19(1):1002. doi: 10.1186/s12913-019-4840-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Comino EJ, Harris MF, Islam MD, et al. Impact of diabetes on hospital admission and length of stay among a general population aged 45 year or more: a record linkage study. BMC Health Serv Res. 2015;15:12. doi: 10.1186/s12913-014-0666-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Riddle MC, Herman WH. The cost of diabetes care-an elephant in the room. Diabetes Care. 2018;41(5):929-932. doi: 10.2337/dci18-0012 [DOI] [PubMed] [Google Scholar]
- 7. American Diabetes Association. Economic costs of diabetes in the U.S. in 2017. Diabetes Care. 2018;41(5):917-928. doi: 10.2337/dci18-0007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Benoit SR, Hora I, Pasquel FJ, Gregg EW, Albright AL, Imperatore G. Trends in emergency department visits and inpatient admissions for hyperglycemic crises in adults with diabetes in the U.S., 2006-2015. Diabetes Care. 2020;43(5):1057-1064. doi: 10.2337/dc19-2449 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Draznin B, Gilden J, Golden SH, Inzucchi SE. Pathways to quality inpatient management of hyperglycemia and diabetes: a call to action. Diabetes Care. 2013;36(7):1807-1814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. American Diabetes Association. 14. Diabetes care in the hospital: standards of medical care in diabetes-2018. Diabetes Care. 2018;41(suppl 1):S144-S151. doi: 10.2337/dc18-S014 [DOI] [PubMed] [Google Scholar]
- 11. American Diabetes Association. 15. Diabetes care in the hospital: standards of medical care in diabetes-2019. Diabetes Care. 2019;42(suppl 1):S173-S181. doi: 10.2337/dc19-S015 [DOI] [PubMed] [Google Scholar]
- 12. American Diabetes Association. 15. Diabetes care in the hospital: standards of medical care in diabetes-2020. Diabetes Care. 2020;43(suppl 1):S193-S202. doi: 10.2337/dc20-S015 [DOI] [PubMed] [Google Scholar]
- 13. American Diabetes Association. 15. Diabetes care in the hospital: standards of medical care in diabetes-2021. Diabetes Care. 2021;44(suppl 1):S211-S220. doi: 10.2337/dc21-S015 [DOI] [PubMed] [Google Scholar]
- 14. Golden SH, Maruthur N, Mathioudakis N, et al. The case for diabetes population health improvement: evidence-based programming for population outcomes in diabetes. Curr Diab Rep. 2017;17(7):51. doi: 10.1007/s11892-017-0875-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Hirsch IB. Sliding scale insulin–time to stop sliding. JAMA. 2009;301(2):213-214. doi: 10.1001/jama.2008.943 [DOI] [PubMed] [Google Scholar]
- 16. Schnipper JL, Barsky EE, Shaykevich S, Fitzmaurice G, Pendergrass ML. Inpatient management of diabetes and hyperglycemia among general medicine patients at a large teaching hospital. J Hosp Med. 2006;1(3):145-150. doi: 10.1002/jhm.96 [DOI] [PubMed] [Google Scholar]
- 17. Boord JB, Greevy RA, Braithwaite SS, et al. Evaluation of hospital glycemic control at US academic medical centers. J Hosp Med. 2009;4(1):35-44. doi: 10.1002/jhm.390 [DOI] [PubMed] [Google Scholar]
- 18. American Hospital Association. Fast Facts on US Hospitals, 2020. Chicago, IL: American Hospital Association; 2020. [Google Scholar]
- 19. Wachter RM, Goldman L. Zero to 50,000 - the 20th anniversary of the hospitalist. N Engl J Med. 2016;375(11):1009-1011. doi: 10.1056/NEJMp1607958 [DOI] [PubMed] [Google Scholar]
- 20. Dressler DD, Pistoria MJ, Budnitz TL, McKean SC, Amin AN. Core competencies in hospital medicine: development and methodology. J Hosp Med. 2006;1(1):48-56. [DOI] [PubMed] [Google Scholar]
- 21. O’Donnell CM, Stern M, Leong T, Molitch-Hou E, Mitchell B. Incorporating continuity in a 7-on 7-off hospitalist model and the correlation with patient handoffs and length of stay. Am J Med Qual. 2019;34(6):553-560. doi: 10.1177/1062860618818355 [DOI] [PubMed] [Google Scholar]
- 22. Howell E, Kravet S, Kisuule F, Wright SM. An innovative approach to supporting hospitalist physicians towards academic success. J Hosp Med. 2008;3(4):314-318. doi: 10.1002/jhm.327 [DOI] [PubMed] [Google Scholar]
- 23. Drincic AT, Akkireddy P, Knezevich JT. Common models used for inpatient diabetes management. Curr Diab Rep. 2018;18(3):10. doi: 10.1007/s11892-018-0972-x [DOI] [PubMed] [Google Scholar]
- 24. Levetan CS, Salas JR, Wilets IF, Zumoff B. Impact of endocrine and diabetes team consultation on hospital length of stay for patients with diabetes. Am J Med. 1995;99(1):22-28. doi: 10.1016/s0002-9343(99)80100-4 [DOI] [PubMed] [Google Scholar]
- 25. Koproski J, Pretto Z, Poretsky L. Effects of an intervention by a diabetes team in hospitalized patients with diabetes. Diabetes Care. 1997;20(10):1553-1555. doi: 10.2337/diacare.20.10.1553 [DOI] [PubMed] [Google Scholar]
- 26. Puig J, Supervia A, Marquez MA, Flores J, Cano JF, Gutierrez J. Diabetes team consultation: impact on length of stay of diabetic patients admitted to a short-stay unit. Diabetes Res Clin Pract. 2007;78(2):211-216. doi: 10.1016/j.diabres.2007.03.010 [DOI] [PubMed] [Google Scholar]
- 27. Korytkowski M, Dinardo M, Donihi AC, Bigi L, Devita M. Evolution of a diabetes inpatient safety committee. Endocr Pract. 2006;12(suppl 3):91-99. doi: 10.4158/EP.12.S3.91 [DOI] [PubMed] [Google Scholar]
- 28. Pietras SM, Hanrahan P, Arnold LM, Sternthal E, McDonnell ME. State-of-the-art inpatient diabetes care: the evolution of an academic hospital. Endocr Pract. 2010;16(3):512-521. doi: 10.4158/EP09319.CO [DOI] [PubMed] [Google Scholar]
- 29. Munoz M, Pronovost P, Dintzis J, et al. Implementing and evaluating a multicomponent inpatient diabetes management program: putting research into practice. Jt Comm J Qual Saf. 2012;38(5):195-206. doi: 10.1016/s1553-7250(12)38025-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Rushakoff RJ, Sullivan MM, MacMaster HW, et al. Association between a virtual glucose management service and glycemic control in hospitalized adult patients: an observational study. Ann Intern Med. 2017;166(9):621-627. doi: 10.7326/M16-1413 [DOI] [PubMed] [Google Scholar]
- 31. Haque WZ, Demidowich AP, Sidhaye A, Golden SH, Zilbermint M. The financial impact of an inpatient diabetes management service. Curr Diab Rep. 2021;21(2):5. doi: 10.1007/s11892-020-01374-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Demidowich AP, Batty K, Love T, et al. Effects of a dedicated inpatient diabetes management service on glycemic control in a community hospital setting. J Diabetes Sci Technol. 2021. doi: 10.1177/1932296821993198 (in press). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Newton CA, Young S. Financial implications of glycemic control: results of an inpatient diabetes management program. Endocr Pract. 2006;12(suppl 3):43-48. doi: 10.4158/EP.12.S3.43 [DOI] [PubMed] [Google Scholar]
- 34. Sidhaye AR, Mathioudakis N, Bashura H, Sarkar S, Zilbermint M, Golden SH. Building a business case for inpatient diabetes management teams: lessons from our center. Endocr Pract. 2019;25(6):612-615. doi: 10.4158/EP-2018-0471 [DOI] [PubMed] [Google Scholar]
- 35. Shelton C, Demidowich A, Motevalli M, et al. Retrospective quality improvement study of insulin-induced hypoglycemia and implementation of hospital-wide initiatives. J Diabetes Sci Technol. 2021. (in press). DOI: 10.1177/19322968211008513 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Najmi U, Haque W, Ansari U, et al. Inpatient insulin pen implementation, waste, and potential cost savings: a community hospital experience. J Diabetes Sci Technol. 2021. (under review). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Healy SJ, Black D, Harris C, Lorenz A, Dungan KM. Inpatient diabetes education is associated with less frequent hospital readmission among patients with poor glycemic control. Diabetes Care. 2013;36(10):2960-2967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Bansal V, Mottalib A, Pawar TK, et al. Inpatient diabetes management by specialized diabetes team versus primary service team in non-critical care units: impact on 30-day readmission rate and hospital cost. BMJ Open Diabetes Res Care. 2018;6(1):e000460. doi: 10.1136/bmjdrc-2017-000460 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Patel A, Rajkumar R, Colmers JM, Kinzer D, Conway PH, Sharfstein JM. Maryland’s global hospital budgets–preliminary results from an all-payer model. N Engl J Med. 2015;373(20):1899-1901. doi: 10.1056/NEJMp1508037 [DOI] [PubMed] [Google Scholar]
- 40. Sharfstein JM, Stuart EA, Antos J. Maryland’s all-payer health reform-a promising work in progress. JAMA Intern Med. 2018;178(2):269-270. doi: 10.1001/jamainternmed.2017.7709 [DOI] [PubMed] [Google Scholar]
- 41. McIlvennan CK, Eapen ZJ, Allen LA. Hospital readmissions reduction program. Circulation. 2015;131(20):1796-1803. doi: 10.1161/CIRCULATIONAHA.114.010270 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Porter ME. What is value in health care? N Engl J Med. 2010;363(26):2477-2481. doi: 10.1056/NEJMp1011024 [DOI] [PubMed] [Google Scholar]
- 43. Chee TT, Ryan AM, Wasfy JH, Borden WB. Current state of value-based purchasing programs. Circulation. 2016;133(22):2197-2205. doi: 10.1161/CIRCULATIONAHA.115.010268 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Shelton C, Demidowich AP, Zilbermint M. Inpatient diabetes management during the COVID-19 crisis: experiences from two community hospitals. J Diabetes Sci Technol. 2020;14(4):780-782. doi: 10.1177/1932296820930268 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Umpierrez G, Rushakoff R, Seley JJ, et al. Hospital diabetes meeting 2020. J Diabetes Sci Technol. 2020;14(5):928-944. doi: 10.1177/1932296820939626 [DOI] [PMC free article] [PubMed] [Google Scholar]


