Abstract
Background and Aims:
Acute mesenteric venous thrombosis accounts for up to 20% of all patients with acute mesenteric ischemia in high-income countries. Acute mesenteric venous thrombosis is nowadays relatively more often diagnosed with intravenous contrast-enhanced computed tomography in the portal phase than at explorative laparotomy No high-quality comparative studies between anticoagulation alone, endovascular therapy, or surgery exists. The aim of the present systematic review was to offer a contemporary overview on management.
Materials and Methods:
Eleven relevant published original studies with series of at least ten patients were retrieved from a Pub Med search between 2015 and 2020 using the Medical Subject Heading term “mesenteric venous thrombosis.”
Results:
When MVT is diagnosed early, immediate anticoagulation with either unfractionated heparin or subcutaneous low-molecular-weight heparin should commence. Surgeons need to be aware of the importance to scrutinize the computed tomography images themselves for assessment of secondary intestinal abnormalities to mesenteric venous thrombosis and the risk of bowel resection and worse prognosis. Progression toward peritonitis is an indication for explorative laparotomy and assessment of bowel viability. Frank transmural small bowel necrosis should be resected and bowel anastomosis may be delayed for several days until second look. Meanwhile, intravenous full-dose unfractionated heparin should be given at the end of the first operation. Postoperative major intra-abdominal or gastrointestinal bleeding occurs rarely, but the heparin effect can instantaneously be reversed by protamine sulfate. Patients who do not improve during conservative therapy with anticoagulation alone but without developing peritonitis may be subjected to endovascular therapy in expert centers. When the patient’s intestinal function has recovered, with or without bowel resection, switch from parenteral unfractionated heparin or low-molecular-weight heparin therapy to oral anticoagulation can be performed. There is a trend that direct oral anticoagulants are increasingly used instead of vitamin K antagonists. Up to now, direct oral anticoagulants have been shown to be equally effective with the same rate of bleeding complications. Patients with no strong permanent trigger factor for mesenteric venous thrombosis such as intra-abdominal cancer should undergo blood screening for inherited and acquired thrombophilia.
Conclusion:
Early diagnosis with emergency computed tomography with intravenous contrast-enhancement and imaging in the portal phase and anticoagulation therapy is necessary to be able to have a succesful non-operative succesful course.
Keywords: Acute care surgery and trauma, vascular surgery, mesenteric venous thrombosis, intestinal ischemia, management, anticoagulation
Introduction
Epidemiology of Mesenteric Venous Thrombosis
Mesenteric venous thrombosis (MVT) accounted for 16% of all acute mesenteric ischemia, also including arterial embolism, arterial thrombosis, and non-occlusive mesenteric ischemia, in a population-based study in the city of Malmö, Sweden, including 402 patients with an autopsy rate of 87% (1). The estimated overall incidence of MVT was 2.7/100,000 person-years with equal incidences in both genders.
Pathogenesis of Mvt
There are three major pathways for the pathogenesis of MVT (2):
Direct injury. Inflammatory process around the vein due to acute pancreatitis or inflammatory bowel disease. Surgical trauma such as splenectomy or abdominal trauma.
Local venous congestion due to portal hypertension/liver cirrhosis, or stasis due to severe congestive heart failure.
Thrombophilia. Acquired thrombophilia such as pancreatic cancer, myeloproliferative cancer disease, or oral contraceptive use. Inherited thrombophilia such as Factor V Leiden mutation.
Clinical Presentation
Patients with acute MVT usually present themselves within 24–72 h of symptoms (3). The predominant symptom is mid abdominal pain. Fever and signs of peritonitis suggest progression of ischemia to intestinal infarction (4). There are no accurate plasma biomarkers for MVT.
Diagnostic Computed Tomography
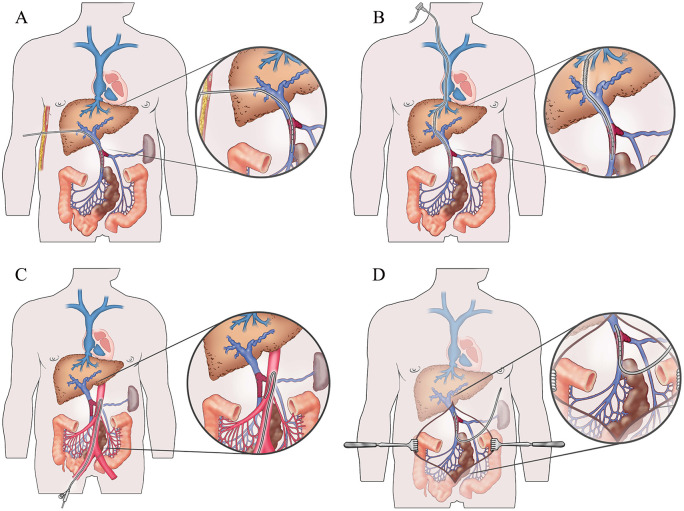
Diagnosis of MVT is almost exclusively dependent on computed tomography (CT) of the abdomen with intravenous contrast enhancement in the portal phase (5). CT is highly sensitive to diagnose MVT (6, 7) and can accurately visualize both the extent of thrombosis within the portomesenteric venous system and secondary abnormal intestinal findings (Fig. 1). The inter-reader agreement on CT for secondary intestinal abnormalities is slightly lower than for diagnosing MVT (8).
Fig. 1.
A CT with intravenous contrast enhancement in the portal phase showed MVT (two thin arrows). Note the secondary intestinal abnormalities such as dilated small bowel loops (thick arrow), mesenteric edema (dashed line), and ascites (dotted line).
Color Doppler ultrasound alone is not sufficient to evaluate the extent of portomesenteric thrombosis, and cannot evaluate secondary intestinal abnormalities, and needs to be complemented by CT.
Non-Operative Therapy
The treatment depends on stage of the disease. Non-operative approach with bowel rest and full anticoagulation using unfractionated heparin intravenously is initiated in patients diagnosed early without development of peritonitis. Low-molecular-weight heparin (LMWH) administered subcutaneously twice daily may be used in patients with milder symptoms. When symptoms have declined, most patients can switch to direct oral anticoagulants (DOACs) or vitamin K antagonists (VKA) (9). Anticoagulation is given for 6 months in the presence of an identifiable transient risk factor, whereas patients with underlying thrombophilia or idiopathic MVT may be considered for lifelong anticoagulation (10) since recurrence of MVT is highly fatal (11).
Surgery
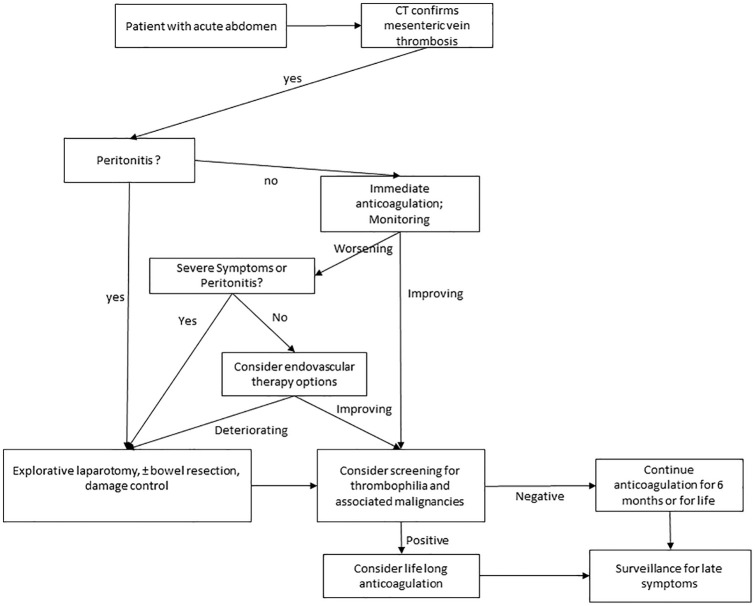
Although availability of CT scanners has improved, exploratory laparotomy will remain the leading mode of diagnosing MVT worldwide in the foreseeable future. Explorative laparotomy is safer than laparoscopy. Transmural bowel infarction should be resected. Antibiotics are indicated in patients in need of bowel resection (12). The distinction between irreversible and reversible intestinal ischemia may be very difficult in MVT, probably more difficult than in acute mesenteric arterial occlusion. The border between irreversible and reversible intestinal ischemia may also be diffuse (13) (Fig. 2) and sometimes it may be wiser to resect the infarcted bowel at primary laparotomy, leave the abdomen open with a temporary abdominal dressing, and perform bowel anastomosis at planned second look laparotomy. These patients should receive full dose of intravenous heparin from the start of the explorative laparotomy, at latest, until the bowel function has normalized.
Fig. 2.
Explorative laparotomy in a patient with MVT. At laparotomy, 0.4 m of the most reddish and severely ischemic segment (thin arrow) was resected and anastomosed. Note the distended small bowel loops (thick black arrows) and the edema in the adjacent mesentery (dashed line). Histopathology of the resected bowel did not show transmural infarction but did show infarcted mucosa and venous thrombosis. It is uncertain whether bowel resection really was necessary or if the ischemic bowel would have recovered without bowel resection and anticoagulation therapy alone.
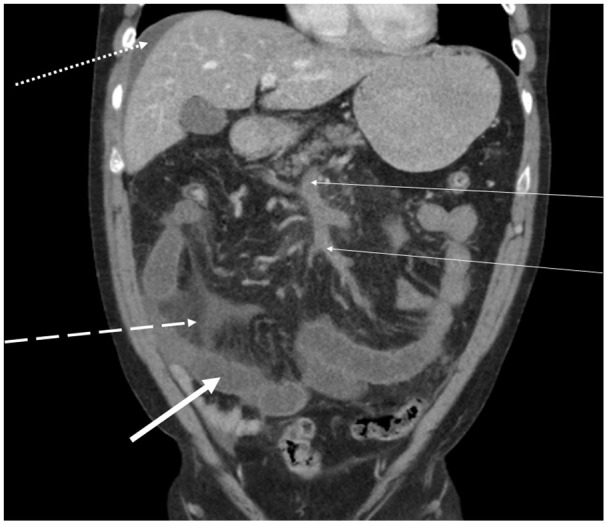
Endovascular, Hybrid, and Open Vascular Surgery
There are no high-quality studies suggesting that endovascular therapy has an established role in the treatment of MVT, but may be an option in selected patients not responding satisfactorily to anticoagulation therapy. A number of endovascular therapy options have developed for MVT (Fig. 3A to D). These techniques can provide rapid thrombus dissolution and removal. Thrombolysis via the Superior Mesenteric Artery (SMA) may be the least effective since it requires long infusion times with thrombolytic agents, which has been found to be associated with an increased risk of bleeding (14) (Fig. 3c). Combining endovascular therapy with open surgery (hybrid approach) has been described in a modern series of nine patients (15), where bowel resection was followed by fluoroscopic-guided balloon thrombectomy after surgical exposure of the superior mesenteric vein, ending up with completion control venography. In a reported series of 31 surgically treated patients in 1997, 11 underwent open surgical thrombectomy, of which 5 received additional treatment with continuous local thrombolysis with high-dose recombinant tissue plasminogen activator for 2–3 days (16) (Fig. 3D). The catheter was removed after thrombolytic therapy without complications. In-hospital mortality of these 11 patients was 27% (3/11), and none of the five selected patients receiving thrombolysis died in hospital. Since then, no series with open surgical thrombectomy of the portomesenteric venous system has been published. Therefore, the role of open surgical thrombectomy in modern practice is uncertain.
Fig. 3.
A–D) Schematic drawings of various ways of local delivery of thrombolysis for MVT. Usually a special catheter with multiple side holes will be placed directly in the thrombus (A, B, D). An occluding ball wire at the catheter tip end hole (not shown) will allow for even pressure distribution of lytic agent at the side holes. Typically, an intestinal segment of the jejunum and/or ileum will be swollen and ischemic. A) Percutaneous hepatic access. B) Percutaneous transjugular intrahepatic portosystemic shunt including stent graft placement in the shunt. C) Percutaneous transfemoral access and indirect thrombolysis by an endhole catheter placed in the superior mesenteric artery. D) Intra-operatively placed catheter in the superior mesenteric vein at laparotomy.
Source: Salim S. On Acute Mesenteric Venous Thrombosis. Lund: Lund University, 2020. Figures reused by permission from Robin Tran.
Aim of This Systematic Review
Because of the rarity of the diagnosis, high-level evidence is lacking and optimal management remains uncertain. The aim of this systematic review is to review recently published series on MVT and to provide the basis of contemporary management of MVT.
Methods
Original articles were searched for in PubMed on 15 February 2020. Medical Subject Heading (MeSH) term was “Mesenteric venous thrombosis” and articles between 2015 and 2020 were included. In total, 1703 abstracts were checked. Articles in English language were selected. Only original reports with ⩾10 patients with MVT with or without extension to the portal or splenic vein were considered. Reports on portomesenteric venous thrombosis or splanchnic vein thrombosis without further specification on location of thrombosis or no reported patient characteristics or outcome data separately for patients with MVT were excluded (n = 20). Unvalidated larger (nation- or statewide) cohort or register-studies on mesenteric ischemia were excluded. The search protocol and article selection (Fig. 4) was completed by one author (S.A.).
Fig. 4.

Preferred Reporting Items for Systematic Reviews and Meta-analysis (PRISMA) flowchart describing the literature search.
Data quality was assessed by the European Society of Cardiology system (17): Level of evidence A reflects data derived from multiple clinical trials or meta-analyses; B reflects data derived from a single randomized clinical trial or large non-randomized studies; C consensus of opinion of the experts and/or small studies, retrospective studies, and registries.
Statistics
Data pooling was performed, whenever possible. Proportion of sex after data pooling was expressed in percentage with 95% confidence intervals (CIs). Data management and statistical analysis were performed using the SPSS for Windows program package (SPSS version 25.0, Chicago, IL, USA). Quantitative differences between groups were assessed with the Mann–Whitney U test. The Pearson correlation test was used for calculating correlations. A p-value < 0.05 was considered significant.
Results
Patient Characteristics
Eleven studies (evidence level C) were retrieved (18–28), of which seven were from East Asian countries (Table 1). The total number of patients was 604, 207 females and 397 males. The pooled estimate of proportion of female sex was 34.3% (95% CI = 30.5%–38.5%).
Table 1.
Contemporary published series on acute MVT.
| First author (publication year) | Population, country | Number of patients | Mean or median age | Female sex (%) | Study period | Frequency of bowel resection (%) | Frequency of endovascular procedure (%) | 30-day or in-hospital mortality rate (%) | Diagnostic autopsy (%) |
|---|---|---|---|---|---|---|---|---|---|
| Al-Thani (18) (2015) | Qatar | 35 | 45 | 12 (34.3) | 2005–2012 | 28/35 (80) | 0 (0) | 6/35 (17.1) | 0 (0) |
| Cho (19) (2018) a | Korea | 41 | 62 | 10 (24.4) | 2000–2017 | 4/41 (9.8) | 0 (0) | 2/41 (4.9) | 0 (0) |
| Kim (20) (2017) a | South Korea | 66 | 50 | 20 (30.3) | 2002–2016 | 15/66 (22.7) | 0 (0) | 3/66 (4.5) | 0 (0) |
| Liu (21) (2019) a | China | 68 | 45 | 18 (26.5) | 2009–2014 | 44/68 (64.7) | 49/68 (72.1) | 2/68 (2.9) | 0 (0) |
| Maldonado (22) (2016) a | USA | 80 | 58 | 34 (42.5) | 1999–2015 | 4/75 b (5.3) | 4/75 b (5.3) | 1/80 (1.2) | 0 (0) |
| Matthaei (23) (2019) | Germany | 10 | 50 | 5 (50) | 2005–2015 | 8/10 (80) | 0 (0) | 0/10 (0) | 0 (0) |
| Nagaraja (24) (2015) | India | 56 | 50 | 13 (23.2) | 1997–2012 | 51/56 (91.1) | 0 (0) | 15/56 (26.8) | 0 (0) |
| Salim (25) (2018) | Sweden | 120 | 58 | 53 (44.2) | 2000–2015 | 24/120 (20) | 8/120 (6.7) | 13/120 (10.8) | 6/120 (5) |
| Wang (26) (2019) | China | 78 | 61 | 24 (30.8) | 2014–2018 | 58/78 (74.4) | 0 (0) | Not reported | 0 (0) |
| Yang (27) (2016) | China | 32 | 45 | 12 (37.5) | 2012–2014 | 25/32 (78.1) | 15/32 (46.9) | 8/32 (25) | 0 (0) |
| Zeng (28) (2017) | China | 18 | 51 | 6 (33.3) | 2013–2014 | 2/18 (11.1) | 0 (0) | 0/18 (0) | 0 (0) |
| Pooled data | – | 604 | – | 207 (34.3) | – | 263/599 (43.9) | 76/599 (12.7) | 50/526 (9.5) | 6/604 (0.1) |
MVT: mesenteric venous thrombosis; CT: computed tomography.
All selected by diagnosis on CT/initial imaging.
Five patients had no available data on treatment.
Outcomes
The pooled bowel resection, endovascular procedure, and 30-day mortality rate were 43.9%, 12.7%, and 9.5%, respectively (Table 1). Four series (21, 22, 25, 27) reported endovascular procedures, ranging from 6.7% to 72.1% of the included number of patients in respective study. The four series (19–22) that diagnosed all patients by CT/initial imaging had all a low 30-day mortality rate, ranging from 1.2% to 4.9%. One series included 15 asymptomatic and 65 symptomatic MVT patients, and demographic and outcome data were presented on all MVT patients with available data (22). Only one series (25) included individuals diagnosed primarily at autopsy. There was no difference in bowel resection (p = 0.43) or 30-day mortality (p = 0.61) rate between study populations from high-income (18–20, 22, 23, 25) and low- and middle-income (21, 24, 26–28) countries. There was a trend that higher bowel resection rate was correlated (r = 0.62; p = 0.055) with higher 30-day mortality rate in the studies.
Discussion
Epidemiology
The proportion of MVT as an etiology in the city of Mansoura, Egypt, was found to be remarkably high, 77% (78 patients) (29). This discrepancy was perhaps mostly attributed to the high prevalence of chronic liver disease secondary to endemic hepatitis C virus infection in Egypt (30).
Nagaraja et al. (24) found that MVT was seen in 56 (48%) out of 117 Indian patients with acute mesenteric ischemia. The reasons behind this high proportion of MVT may be attributed to a more rapid progression of illness in patients with mesenteric arterial occlusive disease and deaths outside the study hospital.
The mean or median age of MVT patients at presentation in contemporary series (18–28) was reported to be between 45 and 62 years. The results on gender distribution (18–28) support that MVT is slightly more common in males compared to females.
The Importance To Scrutinize The Ct Images
It is very important that the responsible physicians taking care of the patient scrutinizes the CT images together with the radiologist in charge. Secondary intestinal abnormalities to MVT such as small bowel wall edema have been found to be associated with bowel resection after multi-variable adjustment (5). In another recent report performing adjustment for confounders, CT-verified dilated small bowel loops, defined as ⩾2.0 cm, were associated with intestinal necrosis and bowel resection (26). Patients with thrombosis extending into the portal vein or complete thrombosis of the superior mesenteric vein were also found to have an increased risk of bowel resection (20). Moreover, less extensive thrombosis is associated with less risk of long-term sequelae of portal venous hypertension (22).
The Place of Endovascular Therapy
In modern series (18–28), endovascular therapy was not at all performed in the majority of centers, whereas two centers performed endovascular therapy in 47% (27) and 72% (21) of the patients, respectively.
Nevertheless, the bowel resection rate was very high in these series, 64.7% (21) and 78.1% (27), respectively, which simply may be related to too late diagnosis.
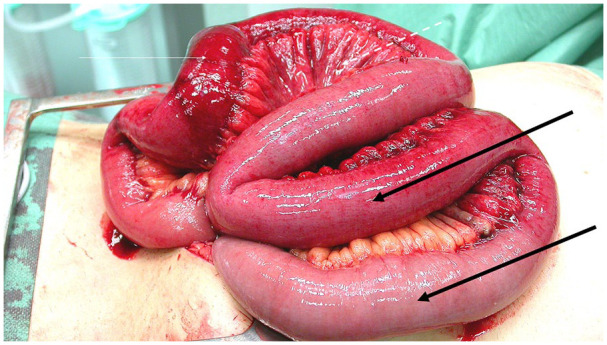
Until further evidence is available, endovascular therapy should be performed in experienced centers in patients that clinically deteriorate during anticoagulation therapy (25) in order to avoid explorative laparotomy and bowel resection. In this series, endovascular therapy reduced the need of bowel resection in five out of eight patients (25). Suggested management algorithm of patients with acute MVT is presented in Fig. 5.
Fig. 5.
Suggested algorithm for management of acute MVT.
Late Bowel Complications
The reported frequencies of small bowel stricture were 3.0% (20), 5.6% (28), and 9.4% (27) in modern series. The ischemic insult heals by ending up with a tight clinically relevant fibrotic stricture of the small bowel wall, resulting in a mechanical ileus. This condition requires an operation, usually after a few months (25), to relieve the ileus.
The reported frequencies of short bowel syndrome were 5.9% (21), 25% (27), 31% (18), and 40% (23) in modern series. If possible, take down of ileostomies and re-anastomosis should be performed whenever possible to avoid further complications from long-term parenteral nutritional support and to relief the short bowel syndrome (25). Indeed, short bowel syndrome has been found to be associated with mortality (27).
The Place of Ct Follow-Up
In 70 patients with a follow-up CT at a median follow-up time of 6 months, 46 (66%) patients had either complete or partial regression of thrombotic status within the portomesenteric venous system (5). No clinical variable was found to be associated with successful thrombus recanalization. There is currently no data to recommend a routine CT follow-up for evaluation of changes in thrombotic status. The indication for discontinuation of anticoagulation therapy is based on whether there is an identifiable transient risk factor or not.
Bowel Resection and Mortality
Early diagnosis of MVT is the key to lower mortality. The pooled data on patients diagnosed using CT only/initial imaging only (19–22) had a comparably low 30-day mortality rate, ranging from 1.2% to 4.9%. There was a trend that bowel resection at initial surgery was correlated with increased 30-day mortality among the modern series (18–28). The reported contemporary 30-day mortality rate is underestimated, since only one (25) out of the eleven (18–28) series reported findings at autopsy. In addition, it should be acknowledged that the pooled results of outcome in this review are prone to publication bias. The clinical data of this study stems from different study populations worldwide where availability of health care and CT scanners around the clock vary greatly. However, when comparing the contemporary series from high-income versus low- to middle-income countries, there was no difference in bowel resection and 30-day mortality rate. Regarding long-term mortality, there was no difference between patients with MVT and systemic venous thromboembolism in a population-based study from Sweden (31).
Areas of Uncertainties
The shift from VKA to DOACs in the medical long-term treatment of MVT has not been proven to be better (9). Therefore, the setup of a multi-center randomized controlled trial (RCT) between LMWH followed by VKA versus LMWH followed by DOACs is warranted. Patients planned for anticoagulation-first strategy after diagnosis at CT are suitable candidates. Endpoints would be traditional outcome data such as bowel resection, mortality, and major bleeding, but also quality of life. There should be a plan for a cost-effective analysis at the planning stages.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: S. Acosta  https://orcid.org/0000-0002-3225-0798
https://orcid.org/0000-0002-3225-0798
References
- 1. Acosta S: Epidemiology of mesenteric vascular disease: Clinical implications. Semin Vasc Surg 2010;23:4–8. [DOI] [PubMed] [Google Scholar]
- 2. Zarrouk M, Salim S, Elf J, et al. : Testing for thrombophilia in mesenteric venous thrombosis: Retrospective original study and systematic review. Best Pract Res Clin Gastroenterol 2017;31:39–48. [DOI] [PubMed] [Google Scholar]
- 3. McKinsey JF, Gewertz BL: Acute mesenteric ischemia. Surg Clin North Am 1997;77:307–318. [DOI] [PubMed] [Google Scholar]
- 4. Hmoud B, Singal AK, Kamath PS: Mesenteric venous thrombosis. J Clin Exp Hepatol 2014;4:257–263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Salim S, Ekberg O, Elf J, et al. : Clinical implications of CT findings in mesenteric venous thrombosis at admission. Emerg Radiol 2018;25:407–413. [DOI] [PubMed] [Google Scholar]
- 6. Henes FO, Pickhardt PJ, Herzyk A, et al. : CT angiography in the setting of suspected acute mesenteric ischemia: Prevalence of ischemic and alternative diagnoses. Abdom Radiol 2017;42:1152–1161. [DOI] [PubMed] [Google Scholar]
- 7. Lehtimäki TT, Kärkkäinen JM, Saari P, et al. : Detecting acute mesenteric ischemia in CT of the acute abdomen is dependent on clinical suspicion: Review of 95 consecutive patients. Eur J Radiol 2015;84:2444–2453. [DOI] [PubMed] [Google Scholar]
- 8. Copin P, Ronot M, Nuzzo A, et al. : Inter-reader agreement of CT features of acute mesenteric ischemia. Eur J Radiol 2018;105:87–95. [DOI] [PubMed] [Google Scholar]
- 9. Salim S, Ekberg O, Elf J, et al. : Evaluation of direct oral anticoagulants and vitamin K antagonists in mesenteric venous thrombosis. Phlebology 2019;34:171–178. [DOI] [PubMed] [Google Scholar]
- 10. Björck M, Koelemay M, Acosta S, et al. : Editor’s choice—Management of the diseases of mesenteric arteries and veins: Clinical practice guidelines of the European Society of Vascular Surgery (ESVS). Eur J Vasc Endovasc Surg 2017;53:460–510. [DOI] [PubMed] [Google Scholar]
- 11. Brandt LJ, Boley SJ: AGA technical review on intestinal ischemia: American Gastrointestinal Association. Gastroenterology 2000;118:954–968. [DOI] [PubMed] [Google Scholar]
- 12. Grisham A, Lohr J, Guenther JM, et al. : Deciphering mesenteric venous thrombosis: Imaging and treatment. Vasc Endovasc Surg 2005;39:473–479. [DOI] [PubMed] [Google Scholar]
- 13. Levy PJ, Krausz MM, Manny J: The role of second-look procedure in improving survival time for patients with mesenteric venous thrombosis. Surg Gynecol Obstet 1990;170:287–291. [PubMed] [Google Scholar]
- 14. Hollingshead M, Burke CT, Mauro MA, et al. : Transcatheter thrombolytic therapy for acute mesenteric and portal vein thrombosis. J Vasc Interv Radiol 2005;16:651–661. [DOI] [PubMed] [Google Scholar]
- 15. Xu R, Tang L, Wang X, et al. : Hybrid therapy consisting of bowel resection and fluoroscopic-assisted balloon thrombectomy for small bowel infarction caused by acute mesenteric venous thrombosis. Ann Vasc Surg 2019;59:202–207. [DOI] [PubMed] [Google Scholar]
- 16. Klempnauer J, Grothues F, Bektas H, et al. : Results of portal thrombectomy and splanchnic thrombolysis for the management of acute mesentericoportal thrombosis. Br J Surg 1997;84:129–132. [PubMed] [Google Scholar]
- 17. Hamm CW, Bassand JP, Agewall S, et al. : ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation. Eur Heart J 2011;32:2999–3054. [DOI] [PubMed] [Google Scholar]
- 18. Al-Thani H, El-Mabrok J, El-Menyar A, et al. : Clinical presentation and outcome of mesenteric vein thrombosis: A single-center experience. Angiology 2015;66:249–256. [DOI] [PubMed] [Google Scholar]
- 19. Cho JW, Choi JJ, Um E, et al. : Clinical manifestations of superior mesenteric venous thrombosis in the era of computed tomography. Vasc Specialist Int 2018;34(4):83–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Kim HK, Hwang D, Park S, et al. : Treatment outcomes and risk factors for bowel infarction in patients with acute superior mesenteric venous thrombosis. J Vasc Surg Venous Lymphat Disord 2017;5(5):638–646. [DOI] [PubMed] [Google Scholar]
- 21. Liu K, Liu S, Li L, et al. : Evaluation of endovascular therapy combined with bowel resection treatment on patients with acute mesenteric venous thrombosis. Ann Vasc Surg 2020;65:72–81. [DOI] [PubMed] [Google Scholar]
- 22. Maldonado TS, Blumberg SN, Sheth SU, et al. : Mesenteric vein thrombosis can be safely treated with anticoagulation but is associated with significant sequelae of portal hypertension. J Vasc Surg Venous Lymphat Disord 2016;4(4):400–406. [DOI] [PubMed] [Google Scholar]
- 23. Matthaei H, Klein A, Branchi V, et al. : Acute mesenteric ischemia (AMI): Absence of renal insufficiency and performance of early bowel resection may indicate improved outcomes. Int J Colorectal Dis 2019;34(10):1781–1790. [DOI] [PubMed] [Google Scholar]
- 24. Nagaraja R, Rao P, Kumaran V, et al. : Acute mesenteric ischaemia: An Indian perspective. Indian J Surg 2015;77(Suppl. 3):843–849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Salim S, Zarrouk M, Elf J, et al. : Improved prognosis and low failure rate with anticoagulation as first line therapy in mesenteric venous thrombosis. World J Surg 2018;42:3803–3811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Wang Y, Zhao R, Xia L, et al. : Predictive risk factors of intestinal necrosis in patients with mesenteric venous thrombosis: Retrospective study from a single center. Can J Gastroenterol Hepatol 2019;2019:8906803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Yang S, Zhang L, Liu K, et al. : Postoperative catheter-directed thrombolysis versus systemic anticoagulation for acute superior mesenteric venous thrombosis. Ann Vasc Surg 2016;35:88–97. [DOI] [PubMed] [Google Scholar]
- 28. Zeng Q, Fu QN, Li FH, et al. : Early initiation of argatroban therapy in the management of acute superior mesenteric venous thrombosis. Exp Ther Med 2017;13:1526–1534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Sameh EH: Predictive factors intestinal transmural necrosis in patients in patients with acute mesenteric ischemia. World J Surg 2018;42:2364–2372. [DOI] [PubMed] [Google Scholar]
- 30. Kandeel A, Genedy M, El-Refai S, et al. : The prevalence of hepatitis C virus infection in Egypt 2015: Implications for future policy on prevention and treatment. Liver Int 2017;37:45–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Salim S, Zarrouk M, Elf J, et al. : Clinical implications of different risk factor profiles in patients with mesenteric venous thrombosis and systemic venous thromboembolism: A population-based study. J Thromb Thrombolysis 2019;47:572–577. [DOI] [PMC free article] [PubMed] [Google Scholar]