Abstract
The high technical success rate of transjugular intrahepatic portosystemic shunt (TIPS) placement makes the procedure a popular treatment option for symptomatic portal hypertension. Among the major drawbacks of the procedure — hepatic encephalopathy, acute hepatic failure, hemorrhage, biliary injury — TIPS dysfunction is one of the most prevalent, often requiring endovascular reintervention. Conventional techniques for shunt revision rely on transjugular access to the stent; but in technically difficult cases of abnormal angulation or severe stenosis, transhepatic access may also be required. The pull-through method utilizes both transjugular and transhepatic access to achieve stable through-and-through access in order to advance a sheath into the stent and recannulate the shunt. In the case of TIPS foreshortening, however, the distal end of the stent may abut the wall of the hepatic vein, jailing it off and obviating the advancement of a wire out of that end. We present here a case of a modified pull-through method for TIPS revision whereby a transhepatic wire is passed through the interstices of the stent at the distal end to enter into the hepatic vein and IVC. Subsequent snaring of the wire at the transjugular end establishes through-and-through access, and balloon dilation through the interstices allows for insertion of a transjugular sheath into the TIPS stent for recanalization. Our case highlights how the modified pull-through method, using trans-stent access, can be safely performed in patients with a foreshortened TIPS that abuts against the hepatic and portal vessel walls.
Keywords: TIPS Revision, Trans-Stent Access, Portal Hypertension
Introduction
Transjugular intrahepatic portosystemic shunt (TIPS) placement is often indicated for symptomatic portal hypertension refractory to medical and endoscopic treatment. The procedure achieves successful portal venous decompression and clinical resolution of symptoms in about 90% of cases [1,2]. One major drawback, however, is the frequent need for endovascular reintervention due to stent occlusion [2,3]. Shunt dysfunction occurs in approximately 15% of covered stents and 44% of bare metal stents [4,5]. Loss of shunt patency is an urgent indication for TIPS revision due to the consequent rise in risk of variceal bleeding.
The conventional technique for shunt revision relies on catheterizing the TIPS from a transjugular approach before utilizing a combination of angioplasty, stent relining, or stent extension to reduce the portosystemic pressure gradient. In technically difficult cases where a conventional approach is not feasible, as in severe hepatic ostial stenosis or thrombosis, several techniques have been described to establish access. The pull-through method is a popular option with successful outcomes. For example, Chen et al. report a 92% primary patency rate 12 months after TIPS revision with the pull-through method [6]. This technique requires percutaneous transhepatic access to the occluded stent under fluoroscopic guidance. A guidewire is then passed through the occlusion and into the systemic circulation where a snare from a transjugular approach captures the wire and pulls it through. With stable through-and-through access, a sheath is subsequently introduced into the occluded TIPS and a catheter and glidewire are used the recannulate the proximal stent and select the portal vein. Other techniques reported in the literature for TIPS recanalization inaccessible to conventional transvenous approaches include using the back end of a stiff guidewire fixed in the liver parenchyma to secure the sheath or gaining transvenous access with support from a metal cannula or Colapinto needle [7,8].
Severe TIPS malpositioning, however, may pose a different challenge for recanalization other than the occlusion itself. In these cases, the pull-through method may be adjusted to accommodate the specific architecture of the TIPS. We report here a case of a 53-year-old male with a history of NASH cirrhosis, symptomatic portal hypertension, and hepatocellular carcinoma who presented for revision of a thrombosed TIPS that was originally placed at an outside hospital. Upon review, the TIPS had been created from two uncovered stents, for which the proximal and distal ends were foreshortened. The proximal and distal ends of the stent abutted the walls of the right portal vein and right hepatic vein, respectively, effectively jailing off both ends. We describe the first reported case of successful revision of an occluded TIPS with through-and-through access established directly through the interstices of the stent.
Case report
The patient was a 53-year-old male with a history of NASH cirrhosis complicated by hepatocellular carcinoma, portal hypertension, and esophageal variceal bleeding status post-TIPS placement at an outside hospital 13 months prior. Two months after TIPS placement, the stent was noted to be occluded and latter attempts at recannulation and revision of the TIPS were unsuccessful (Fig. 1). The patient was referred to our practice for management of thrombosed TIPS stent associated with portal vein thrombosis.
Fig. 1 –
Pre-Procedure Lateral CT with IV Contrast
Caption: Lateral CT with IV contrast demonstrates shrunken and nodular liver with left lobe hypertrophy and a chronically occluded TIPS stent (arrow)
Internal jugular venous access was achieved, and a 10 French, 45 cm vascular sheath (Cook Group, Bloomington, Indiana, USA) was positioned with the tip in the right atrium. Right atrial pressure was obtained through the sheath (3 mmHg). Ultrasound was then used to evaluate the liver, which demonstrated an occluded TIPS stent (Fig. 2). Under direct sonographic visualization, the stent was accessed using a 21-gauge 15 cm percutaneous entry needle (Cook Group, Bloomington, Indiana, USA).
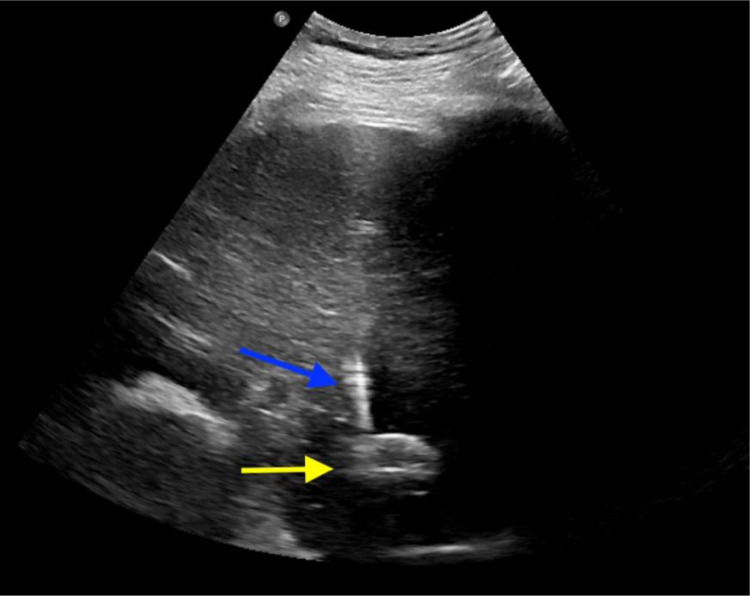
Fig. 2 –
Ultrasound-Guided Transhepatic Access
Caption: Ultrasound is used to evaluate the liver, which demonstrates occluded TIPS stent (yellow arrow). Under sonographic visualization, the TIPS stent is accessed using a 21-gauge 15 cm percutaneous entry needle (blue arrow). (Color version of the figure is available online.)
Needle tip location within the stent was confirmed fluoroscopically, and a 0.018 nitinol wire (EV3, Plymouth, Minnesota, USA) was advanced through the needle into the stent (Fig. 3).
Fig. 3 –
Fluoroscopic Confirmation of Transhepatic Access
Caption: Fluoroscopy confirms needle tip location within the stent. A 0.018 nitinol wire (arrow) is then advanced into the stent
The needle was exchanged over the wire for a 5 French AccuStick transitional dilator (Boston Scientific, Galway, Ireland). The AccuStick sheath was unable to be fully advanced through the stent, so the wire and inner stiffeners were removed and a 4 French angled glide catheter (Cook Group, Bloomington, Indiana, USA) was advanced over the nitinol wire into the stent. The nitinol wire was exchanged for a Glidewire Advantage (Terumo, Somerset, New Jersey, USA), which was guided through the stent and into the inferior vena cava. Notably, the wire crossed through the interstices of the stent in the hepatic vein, but this could not be avoided due to original stent foreshortening.
An Ensnare (Merrit Medical, South Jordan, Utah, USA) was advanced through the transjugular sheath, and the wire was snared to achieve through-and-through access (Fig. 4).
Fig. 4 –
Trans-Stent Advancement to Achieve Through-And-Through Access with Transjugular Snare
Caption: A Glidewire Advantage wire is advanced via a transhepatic approach (yellow arrow), notably crossing through the interstices of the stent into the hepatic vein. An Ensnare from the transjugular end is used to snare the Glidewire to achieve stable body-floss access (blue arrow). (Color version of the figure is available online.)
With this more stable access, the Accustick sheath was able to be advanced into the stent. A 6 mm Mustang balloon (Boston Scientific, Galway, Ireland) was advanced over the wire and used to dilate the interstices of the stent (Fig. 5).
Fig. 5 –
Balloon Dilatation of Stent Interstices
Caption: Balloon dilatation of distal stent interstices with 10 mm Mustang balloon (arrow)
We used the sheath to swallow the balloon, as it was deflated, in order to advance the transjugular sheath into the TIPS. A venogram through the sheath demonstrated appropriate positioning with tip inside the stent. The stent was again noted to be occluded. A Kumpe catheter (Cook Group, Bloomington, Indiana, USA) was advanced through the transjugular sheath into the TIPS, and a J-wire was advanced through the catheter into the splenic vein. The wire was exchanged for a marker pigtail catheter, and a portal venogram was performed. This demonstrated severe stenosis of the portal venous end of the TIPS, which was T-boned on the back wall of the right portal vein (Fig. 6). The left portal vein and main portal vein were patent. The portal pressure was measured (19 mmHg) for a portosystemic gradient of 16 mmHg prior to revision.
Fig. 6 –
Portal Venogram Post Dilatation of Distal TIPS Stent
Caption: Portal venogram demonstrates thrombosis of portal vein and TIPS stents following dilatation of distal TIPS stent. Proximal stent is noted to be T-boned on the back wall of the right portal vein (arrow)
We then used a 10 mm Mustang balloon (Boston Scientific, Galway, Ireland) to dilate the entirety of the TIPS as well as the clot within the right portal vein. The sheath was advanced over the deflating balloon into the splenic vein and the Glidewire Advantage wire was replaced. A new 10 mm x 10 cm (8 cm covered + 2 cm uncovered) Viatorr stent graft (GORE, Flagstaff, Arizona, USA) was advanced over the wire and deployed to achieve smoother course in the hepatic vein. Additionally, this provided a longer covered portion at the junction of the parenchymal tract and the right portal vein. We then dilated the Viatorr stent to 10 mm.
Given stenosis at the junction of the right and left portal veins with thrombus formation, we then extended the portal venous end of the TIPS using a 10 mm x 6 cm Venovo uncovered stent (BD, Franklin Lakes, New Jersey, USA). The marker pigtail catheter was replaced, and a portal venogram was performed. This demonstrated patent TIPS with decreased filling of portal collaterals. Due to angle of the distal hepatic venous outflow, we then elected to extend the distal stent with a 10 mm x 6 cm Venovo stent. A final portal venogram was performed, and pressures were measured (Fig. 7). Right atrial pressure was 6 mmHg, and portal venous pressure was 14 mmHg for a final portosystemic gradient of 8 mmHg.
Fig. 7 –
Portal Venogram Post Dilatation of Distal TIPS Stent and Extension of Proximal and Distal Stents
Caption: Venography shows widely patent TIPS stent post distal dilatation of stent, relining, and extension of proximal and distal ends
The transjugular sheath was removed, and hemostasis was achieved with manual compression. The AccuStick sheath in the liver was retracted into the parenchymal tract. The hepatic parenchymal tract was then coiled using 4 mm 0.035 Nester coils (Cook Group, Bloomington, Indiana, USA) to provide hemostasis.
The patient was discharged later that evening and continues to be managed by Interventional Radiology for locoregional treatment of hepatocellular carcinoma.
Discussion
Transjugular intrahepatic portosystemic shunt (TIPS) is a popular option for managing the sequelae of portal hypertension. However, the high incidence of TIPS dysfunction due to stent stenosis or thrombosis calls for frequent endovascular reintervention. Periodic Doppler ultrasound examinations can detect significant changes in flow velocity within the stent, portal veins, or hepatic veins, indicating the need for TIPS revision [2,9]. In this case, follow-up imaging two months after TIPS demonstrated thrombosis of the stent which eventually extended into the portal vein.
The conventional technique for TIPS revision entails accessing the stent via a transjugular approach and using a combination of balloon angioplasty, shunt relining, and shunt extension to restore flow and reduce the portosystemic pressure gradient [8]. Angioplasty is an effective method for maintaining patency in cases of intimal hyperplasia or thrombosis. Additionally, relining a TIPS with covered stent grafts can treat in-stent and venous end stenoses. Because abnormal angulation can disturb normal flow and promote thrombosis, shunt extension can alleviate any acute angulation of a stent at the distal ends.
Accessing a shunt via a transvenous approach can be technically challenging, particularly with hepatic ostial stenosis or thrombosis, small caliber hepatic veins, or hepatic veins with anterior origins. Several techniques have been described to overcome this, but the pull-through method is one of the most frequently referenced. The pull-through method relies on percutaneous transhepatic access into the TIPS to circumvent the occlusion. From there, a guidewire can be passed through the superior end of the stent and captured by a snare placed at the transjugular end. With stable through-and-through access, a sheath can be introduced into the stent and a guidewire advanced into the portal vein for portal pressure measurement, portal venography, and recanalization through the three techniques mentioned above.
The novelty of our case stems from the foreshortened orientation of the stent, which was T-boned against the vessel walls of the right hepatic and right portal veins. This precluded advancement of a wire in or out of the superior end of the stent even with percutaneous transhepatic access. We demonstrate that TIPS revision can still be achieved by passing a guidewire through the interstices of the stent, establishing through-and-through access, and dilating the interstices with an Accustick sheath set and a balloon dilator. The shunt can then be extended at the venous end to achieve a smoother course and allow for easier access in the future if necessary.
An alternative solution to revision is placing a parallel TIPS. This procedure is done for patients with a non-salvageable primary TIPS or with symptom persistence despite a functioning primary TIPS. The literature suggests that a second TIPS procedure carries a technical success rate of nearly 100% [10,11]. However, a parallel TIPS carries the same risk of complications as a primary procedure, including hepatic encephalopathy, acute hepatic failure, hemorrhage, biliary injury, and TIPS dysfunction [12]. Hepatic encephalopathy is a major complication of TIPS with an incidence around 5-35% [13]. In about 95% of cases, hepatic encephalopathy can be managed conservatively with lactulose, a protein-restricted diet, and branched chain amino acids. In refractory cases, TIPS occlusion via a balloon or reduction in stent diameter may be warranted [13]. Acute hepatic failure secondary to TIPS placement carries a very poor prognosis. This complication stems from some degree of hepatic ischemia due to consequent changes in portal flow dynamics through the shunt [12]. Chung et al. advocate for maintaining a portosystemic pressure gradient greater than 5 mmHg in patients with marginal hepatic functional status to minimize the risk of hepatic failure [14]. In addition, through parenchymal tract formation using a TIPS needle, arterial and biliary injury may occur, including pseudoaneurysm formation or transection [12]. He et al. suggest that the placement of a parallel TIPS takes less procedure time and may be associated with a reduced risk of hemorrhage and biliary injury given that the primary TIPS can be used as a marker for the portal vein [10]. Therefore, portal vein angiography can be omitted, and the difficulty of creating a tract between the hepatic and portal vein is theoretically reduced. Still, given the significant risk associated with any TIPS procedure, additional investigation on the complications of a parallel TIPS compared to TIPS recanalization is required.
In summary, we report here a unique variation of the pull-through method for TIPS recanalization in technically difficult cases where transjugular access to the stent cannot be achieved. This method is useful specifically for stents that directly abut the vessel walls at the aditus, preventing passage of a guidewire out the superior end. We assert that this method is effective and feasible with limited complication risks compared to placement of an additional parallel TIPS.
Funding
The authors have no outside funding sources to disclose.
Informed consent
The authors obtained written and informed consent from the patient for submission of this manuscript for publication.
Footnotes
Acknowledgements: The authors have no acknowledgements to disclose.
Competing Interest: The authors certify that they have NO affiliations with or involvement in any organization or entity with any financial interest (such as honoraria; educational grants; participation in speakers’ bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements), or non-financial interest (such as personal or professional relationships, affiliations, knowledge or beliefs) in the subject matter or materials discussed in this manuscript.
References
- 1.Boyer T.D., Haskal Z.J. The role of transjugular intrahepatic portosystemic shunt in the management of portal hypertension. Hepatol. 2005;41(2):386–400. doi: 10.1002/hep.20559. [DOI] [PubMed] [Google Scholar]
- 2.Colombato L. The Role of Transjugular Intrahepatic Portosystemic Shunt (TIPS) in the Management of Portal Hypertension. J. Clin. Gastroenterol. 2007;41:S344–S351. doi: 10.1097/MCG.0b013e318157e500. Suppl 3(Supplement 3) [DOI] [PubMed] [Google Scholar]
- 3.Sommer C.M., Gockner T.L., Stampfl U. Technical and clinical outcome of transjugular intrahepatic portosystemic stent shunt: bare metal stents (BMS) versus viatorr stent-grafts (VSG) Eur J Radiol. 2012;81(9):2273–2280. doi: 10.1016/j.ejrad.2011.06.037. [DOI] [PubMed] [Google Scholar]
- 4.Bureau C., Pagan J.C.G., Layrargues G.P. Patency of stents covered with polytetrafluoroethylene in patients treated by transjugular intrahepatic portosystemic shunts: long-term results of a randomized multicentre study. Liver international. 2007;27(6):742–747. doi: 10.1111/j.1478-3231.2007.01522.x. [DOI] [PubMed] [Google Scholar]
- 5.Fidelman N., Kwan S.W., LaBerge J.M. The transjugular intrahepatic portosystemic shunt: an update. Am J Roentgenol (1976) 2012;199(4):746–755. doi: 10.2214/AJR.12.9101. [DOI] [PubMed] [Google Scholar]
- 6.Chen S.-l., Xiao C.-j., Wang S. The Pull-Through Technique for Recanalization of Transjugular Intrahepatic Portosystemic Shunt Dysfunction. Gastroenterology Research and Practice. 2020;2020 doi: 10.1155/2020/9150173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Miraglia R., Maruzzelli L., Luca A. Recanalization of occlusive transjugular intrahepatic portosystemic shunts inaccessible to the standard transvenous approach. Diagnostic and interventional radiology (Ankara, Turkey) 2013;19(1):61–65. doi: 10.4261/1305-3825.DIR.5541-12.1. [DOI] [PubMed] [Google Scholar]
- 8.Parvinian A., Omene B.O., Bui J.T. Angiographic patterns of transjugular intrahepatic portosystemic shunt dysfunction and interventional approaches to shunt revision. J Clin Imaging Sci. 2013;3(1):19. doi: 10.4103/2156-7514.111237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Longo J.M., Bilbao J.I., Rousseau H.P. Transjugular intrahepatic portosystemic shunt: evaluation with Doppler sonography. Radiology. 1993;186(2):529–534. doi: 10.1148/radiology.186.2.8421760. [DOI] [PubMed] [Google Scholar]
- 10.He F.L., Wang L., Yue Z.D. Parallel transjugular intrahepatic portosystemic shunt for controlling portal hypertension complications in cirrhotic patients. World J Gastroenterol. 2014;20(33):11835–11839. doi: 10.3748/wjg.v20.i33.11835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Raissi D., Yu Q., Nisiewicz M. Parallel transjugular intrahepatic portosystemic shunt with Viatorr stents for primary TIPS insufficiency: Case series and review of literature. World J. Hepatol. 2019;11(2):217–225. doi: 10.4254/wjh.v11.i2.217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Suhocki P.V., Lungren M.P., Kapoor B. Transjugular intrahepatic portosystemic shunt complications: prevention and management. Semin Intervent Radiol. 2015;32(2):123–132. doi: 10.1055/s-0035-1549376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Madoff D.C., Wallace M.J., Ahrar K. TIPS-related Hepatic Encephalopathy: Management Options with Novel Endovascular Techniques. RadioGraphics. 2004;24(1):21–36. doi: 10.1148/rg.241035028. [DOI] [PubMed] [Google Scholar]
- 14.Chung H.H., Razavi M.K., Sze D.Y. Portosystemic pressure gradient during transjugular intrahepatic portosystemic shunt with Viatorr stent graft: what is the critical low threshold to avoid medically uncontrolled low pressure gradient related complications? J Gastroenterol Hepatol. 2008;23(1):95–101. doi: 10.1111/j.1440-1746.2006.04697.x. [DOI] [PubMed] [Google Scholar]