Abstract
African American women report low participation in physical activity and are disproportionately burdened by related conditions (obesity, breast and colon cancer). Physical activity interventions have shown promising results among African American women, but most studies in this area have focused on short-term increases. More enduring changes in health behavior will be needed to eliminate existing health disparities. Thus, the current study examined 12-month physical activity and psychosocial outcomes from a pilot randomized controlled trial (N=84) of a Home-based Individually-tailored Physical activity Print (HIPP) intervention for African American women in the Deep South. Retention was 77.4% at 12 months. HIPP participants increased self-reported MVPA from 35.1 minutes/week (SD= 47.8) at baseline to 124 minutes/week (SD=95.5) at 12 months, compared to the wellness contact control participants who reported increases from 48.2 minutes/week (SD= 51.3) to 102.5 minutes/week (SD=94.5) over 12 months (between group p>0.05). Results indicate that modest improvements in MVPA and related psychosocial variables occurred during the active intervention phase (months 0–6) and were sustained during the tapered maintenance period (months 6–12). Low cost, high reach, home-based strategies have great potential for supporting sustained participation in physical activity and achieving long-term health benefits among African American women in the Deep South.
Introduction
Physical activity is an established modifiable risk factor for several cancers (e.g., breast, colon) (Kushi et al., 2006). Accordingly, the American Cancer Society recommends ≥150 minutes/week of moderate-intensity aerobic physical activity for cancer risk reduction. However, most Americans are insufficiently active, especially in the South, where cancer incidence and mortality rates are generally higher (U.S. Department of Health and Human Services, 2017). Census data indicates that 55% of African Americans, the largest racial minority group in the US, live in the South, and 105 Southern counties have an African American population of 50% or higher (United States Census Bureau, 2011). African American women report particularly low activity levels (36% meet national physical activity guidelines vs. 49% of White women) (Centers for Disease Control and Prevention, 2015) and suffer disproportionately from related conditions (obesity, breast/colon cancer)(American Cancer Society, 2016). In fact, breast cancer incidence rates have risen among African American women and now exceed rates found among White women in seven southern US states (including Alabama) (American Cancer Society, 2016). Moreover, breast cancer mortality is 42% higher in African American vs. White women (American Cancer Society, 2016). Colon cancer statistics are even more concerning, with African American women having a 17.9% higher incidence rate and a 29.4% higher mortality rate than White women (American Cancer Society, 2016). Effective physical activity interventions are needed to help address these health disparities.
A recent review of physical activity interventions for African American women published from 2009–2015 (Bland & Sharma, 2017) found 13 interventions, seven of which produced increases in physical activity. While these findings are promising, studies in this area have primarily focused on short-term changes in physical activity. Healthy lifestyle behaviors will need to be maintained over time to achieve enduring health benefits and meaningfully address health disparities. In fact, all interventions in the previously mentioned review lasted 6 months or less (except one study with a qualitative exploratory research design). Similar issues were noted in earlier reviews on physical activity interventions among African American adults (Whitt-Glover et al., 2014) (D Pekmezi & Jennings, 2009) and authors called for an examination of the long-term impact of physical activity interventions, typically defined as at least 6 months after cessation of active intervention (Marcus et al., 2000), in this target population.
Thus, to help fill gaps in the literature on physical activity maintenance in underserved populations, the current study examines 12-month physical activity and related psychosocial outcomes from a Home-based Individually-tailored Physical activity Print (HIPP) intervention for African American women in the Deep South (N=84). In the first 6 month active intervention period, HIPP intervention participants reported larger increases (M= +73.9 minutes/week, SD=90.9) in moderate-intensity or greater physical activity than the wait list control group (M=+41.5 minutes/week, SD=64.4, P = 0.22) and significantly greater improvements in physical activity goal setting and enjoyment(D. Pekmezi et al., 2017). We hypothesize that these improvements will be maintained at 12 months, after the tapered intervention phase (months 6–12).
Methods
Design
The current study examines 12-month physical activity and related psychosocial outcomes from a pilot randomized controlled trial (N=84) of the Home-based Individually-tailored Physical activity Print (HIPP) intervention for African American women in the Deep South vs. a wellness contact control condition. The primary outcome variable for this study was minutes per week of MVPA as measured by the 7-Day Physical Activity Recall interview (7-Day PAR) at 12 months. Other physical activity and performance and related psychosocial outcomes were also assessed at this time point.
Setting and sample
Data were collected at the University of Alabama at Birmingham between 2014 and 2016 and analyzed in 2017–2018. The study protocol was approved by the UAB Institutional Review Board and registered with ClinicalTrials.gov (NCT02574689).
Eligible participants were underactive (<60 minutes/week of MVPA at point of screening) women who self-identified as African American and/or Black and had no contraindications for unsupervised physical activity (e.g., a history of heart disease, myocardial infarction, angina, stroke, Body mass index (BMI) over 45 kg/m2, orthopedic conditions). Eligibility criteria also included: 50–69 years of age; stable residence and not planning to move; and scoring ≥19 on the Rapid Estimate of Adult Literacy in Medicine (Davis et al., 1993), as the intervention materials were written at a 4th grade reading level (Marcus, Banspach, et al., 1992).
Protocol
Participants were recruited via face-to-face activities and flyers on campus and in local municipal buildings (city hall, county health department), community centers, and libraries. Further detail on recruitment is available in a prior report (D. Pekmezi et al., 2017). Interested individuals were screened for eligibility via telephone interview, which included items from the Physical Activity Readiness Questionnaire to assess cardiovascular/musculoskeletal risk factors (Canadian Society for Exercise Physiology, 1994). Then, participants attended an orientation session to learn more about the study, complete the informed consent process, and receive accelerometers, with instructions to wear the devices for seven days.
Participants returned the accelerometers to the research center at the baseline physical activity and psychosocial assessment and were randomly assigned to one of the two interventions: the HIPP intervention or wellness contact control conditions. Randomization was stratified by BMI category (BMI < 30 kg/m2 and BMI ≥ 30 kg/m2). Randomization lists were pre-prepared by the study statistician and participants received their group assignment in a sealed envelope.
All participants completed update surveys (at 6 weeks, 10 weeks, 4 months, 5 months; see measures) and received regular group-appropriate cancer prevention print materials by mail for 6 months during the intensive intervention period (three intervention mailings in month 1, two intervention mailings in months 2–3, and one mailing in months 4–6). In the tapered maintenance period (months 6–12), participants completed update surveys and received intervention mailings at months 8 and 10.
Physical activity and psychosocial assessments were completed again at 6 and 12 months, along with accelerometer wear protocols. To encourage retention, participants received reimbursement for travel and childcare expenses and incentives for completing the baseline, 6 month, and 12 month assessments ($25) and the monthly update surveys ($10).
HIPP Intervention
The HIPP intervention encouraged participants to incrementally increase their physical activity until national recommendations were met. The two main intervention components included 1) motivation-matched physical activity manuals (with targeted advice based on the individual participant’s current level of motivational readiness, or stage of change) and 2) individually tailored feedback reports. Implementation involved mail delivery and using a computer expert system to generate feedback based on participant responses to monthly update surveys on Social Cognitive Theory (SCT) (Bandura, 1986) and Transtheoretical Model (TTM) (Prochaska & DiClemente, 1983) constructs, such as i) stages of change (precontemplation, contemplation, preparation, action, maintenance), ii) processes of change (cognitive and behavioral stategies used to advance through the stages of change), iii) self-efficacy (confidence in one’s ability to be active, despite barriers), iv) decisional balance (weighing the pros and cons of participating in physical activity), v) social support from friends and family for physical activity, vi) outcome expectations (anticipated consequences of physical activity), vii) perceived enjoyment of physical activity, and viii) self-regulation (physical activity goal setting and planning).
Participants were also given Accusplit AE120XLv3-xBX pedometers and activity logs to encourage self-monitoring, as well as tip sheets addressing barriers to physical activity identified during 11 focus groups with African American women in Alabama (e.g. time, negative outcome expectations, safety, costs, enjoyment, social support, fear of injury). The motivation-matched manuals, computer expert-tailored feedback reports, tip sheets were all designed/developed in past studies conducted by the team and adapted for the current study(D. Pekmezi et al., 2017). Further details on efforts to address the intervention needs and preferences of our target population, formative research, and resulting HIPP intervention are available in prior reports (D. Pekmezi et al., 2017).
Wellness contact control condition
These participants were mailed cancer prevention information from the ACS website (www.cancer.org) on topics other than physical activity at the same time points as HIPP participants.
Measures
Physical activity and performance
The main outcome measure was the 7-Day Physical Activity Recall (PAR) (Blair et al., 1985), which estimates minutes per week of physical activity. This protocol has previously demonstrated reliability, internal consistency, and congruent validity with objective physical activity measures (Pereira et al., 1997) and was administered at baseline, 6 months, and 12 months.
Participants also wore ActiGraph GT3X accelerometers for 7 days at each timepoint, which measures both movement and intensity of activity and have been validated with heart rate telemetry (Janz, 1994) and total energy expenditure (Melanson & Freedson, 1995). ActiLife software version 6.1 was used to validate and analyze bouts of activity, with a cut point of 1952 counts/minute selected as the minimum threshold for moderate-intensity activity (Freedson, Melanson, & Sirard, 1998). Moreover, minimum valid wear time was set at four days of at least 600 minutes of wear. Consistent with the physical activity data collected by the PAR (i.e., physical activity bouts of 10 minutes or more) and the focus of the national guidelines, only activity bouts ≥10 minutes were included in the estimation of total minutes/week of activity.
Time spent in strength and flexibility exercises was assessed with three items (“Do you regularly do strength and flexibility exercises like sit-ups, push-ups, yoga, or stretching?”, “How many days per week do you do these exercises?”, and “On the days that you do strength and flexibility exercises, how many minutes do you spend doing them?”) used in several similar past studies (Marcus et al., 2015; Marcus et al., 2007). Weight was measured on Scaletronix digital scale to nearest 1/10th kg.
To gain an understanding of whether the physical activity intervention improved physical functioning, participants completed the 6-Minute Walk Test at the research center at baseline, 6 months and 12 months. This test determines the distance that can be walked on a flat, hard surface in 6 minutes and has wide-spread use in both clinic and field testing (Butland, Pang, Gross, Woodcock, & Geddes, 1982).
Psychosocial Variables
Demographic information was collected at baseline. Transtheoretical Model and Social Cognitive Theory constructs were measured at the research center at baseline, 6 months, and 12 months and then via mailed update surveys at 6 weeks, 10 weeks, 4 months, 5 months, 8 months, and 10 months for intervention tailoring. Participants’ stage of change for physical activity was determined by four items, with previously demonstrated reliability (kappa = 0.78; intraclass correlation, r = 0.84) and concurrent validity with measures of self-efficacy and physical activity (Marcus, Selby, Nlaura, & Rossi, 1992). Reliable and valid measures were also used for assessing physical activity processes of change (40 items, 10 subscales, alphas= 0.62–0.96) (Marcus, Rossi, Selby, Niaura, & Abrams, 1992), decisional balance (16 items; alphas: Cons = 0.79 and Pros = 0.95) (Marcus, Rakowski, & Rossi, 1992), social support from family and friends (13 items; alphas = 0.61–0.91) (Sallis, Grossman, Pinski, Patterson, & Nader, 1987), outcome expectations (9 items; alpha = 0.89) (Resnick, Zimmerman, Orwig, Furstenberg, & Magaziner, 2000), enjoyment (18 items; alpha = 0.96) (Kendzierski & DeCarlo, 1991), self-regulation ( 20 items; alphas=.87-.89) (Rovniak, Anderson, Winett, & Stephens, 2002), and self- efficacy ( 5 items; alpha = 0.82) (Marcus, Selby, et al., 1992).
Data Analysis
Differences between the intervention and control group in physical activity and related psychosocial variables at 12 months were examined with a generalized linear model controlling for values at six months. Data were analyzed as intent-to-treat using complete case analysis and mixed models with the assumption that data were missing at random. Results were similar, so the p values for complete case analysis are presented. Within-group differences between six and 12 months were analyzed with paired t-tests. For categorical data, Fisher’s exact test was used for between-group comparisons. The proportion of participants meeting physical activity guidelines at 12 months was compared between groups by Fisher’s exact test and expressed as an odds ratio and 95% confidence interval. In secondary analyses, minutes of MVPA was compared by employment status (full time vs. other), age (< 60 vs. ≥60) and education (college vs. other) by t-tests. For all analyses, a p of < 0.05 was deemed statistically significant and were performed with SAS® version 9.4.
Results
Demographic Characteristics
Of the 84 participants randomized, 65 (77.4%) provided primary outcome data at 12 months. Participants were African American women living in Birmingham, Alabama. The mean BMI was 32.1 kg/m2 (SD=5.16) and the average age was 57 years old. Most reported full-time employment (60.7%) and at least a college level degree (56%). See previously published report for more detail on demographic characteristics (D. Pekmezi et al., 2017).
Changes in physical activity and performance at 12 months
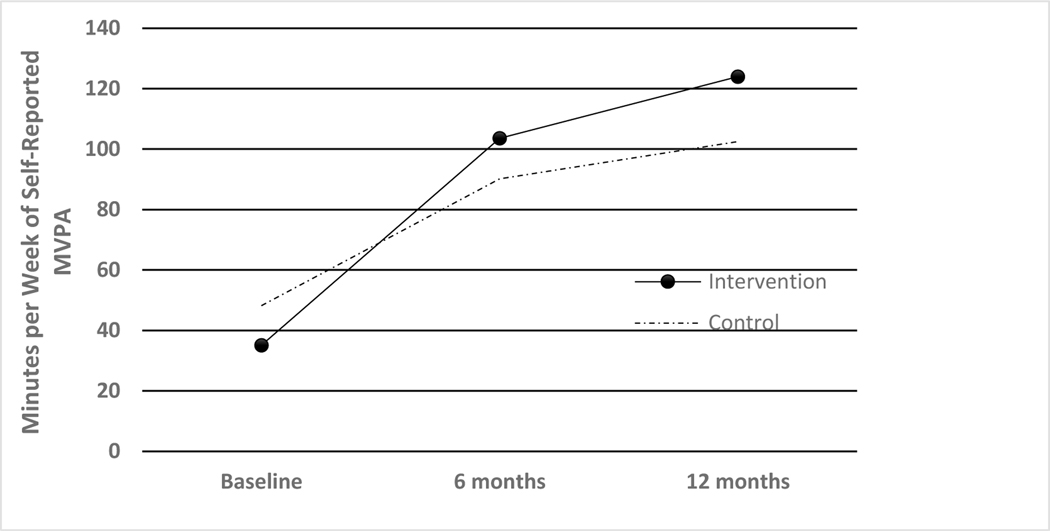
Unadjusted means of weekly minutes of self-reported MVPA over time are presented in Fig. 1. Participants in the HIPP intervention arm increased their self-reported MVPA from 35.1 minutes/week (SD= 47.8) at baseline to 124 minutes/week (SD=95.5) at 12 months, compared to the control participants who reported increases from 48.2 minutes/week (SD= 51.3) to 102.5 minutes/week (SD=94.5) over 12 months (between group p>0.05). The largest gains in MVPA occurred during the active intervention phase, with the HIPP arm reporting an approximate 33 min/week greater increase in physical activity from baseline to 6 months than the wellness contact control arm (between group p>0.05) (D. Pekmezi et al., 2017).
Figure 1.
Changes in self-reported moderate-to-vigorous physical activity over time.
MVPA gains during the first 6 months were mostly sustained during the maintenance period. Between months 6 and 12, the intervention participants increased their self-report physical activity by 12.1 minutes/week, whereas the control arm reported increases of 5 minutes/week. There were no significant within- or between-group changes in self-report MVPA from 6 months to 12 months; however, the HIPP arm continued to report greater physical activity (almost 22 more minutes/week) than control at conclusion of the maintenance period.
Accelerometer data also indicated no significant within- or between-group changes in MVPA from 6–12 months and provided lower estimates of MVPA at 12 months than self-report findings (Spearmann correlation r=0.40).
Some subgroups of participants found the intervention particularly beneficial to physical activity maintenance. HIPP participants with higher levels of education (college degree, N=19) reported significantly greater physical activity (M=156.5 minutes/week of MVPA, SD= 96.9) at 12 months than less-educated HIPP participants (no college degree, N=15; M=83 minutes/week of MVPA, SD=77.6), p= 0.02. No such trends were found for age and employment status, despite a priori hypotheses that older and/or less employed participants might have more time available to participate in intervention-related activities than younger and/or more employed participants.
At 12 months, 44.1% of Intervention participants met ACSM guidelines for physical activity (self-reported MVPA ≥ 150 min per week), which was higher, but not statistically different, than the 6 month percentage (25.6 %). The number meeting guidelines in the control group changed from 21.6 % at 6 months to 25.8 % at 12 months. The odds of meeting guidelines did not significantly differ between the groups at 12 months (OR 2.27, 95% CI 0.79– 6.49, p = 0.19).
There were no significant between-group differences in changes in strength and flexibility exercises or weight from 6–12 months (see Table 1); however, the intervention arm reported almost twice as much time spent participating in strength and flexibility exercises at 12 months (37 minutes/week), compared to the control arm (20 minutes/week). Moreover, the control group reported a significant decrease in 6 minute walk distance from 6 to 12 months (Mean change= −40.9 meters, SD= 61.3), unlike the small reduction observed in the intervention arm. These differences approached significance (p=0.059).
Table 1.
Changes in physical activity from 6 months to 12 months
| Intervention | Control | ||||||
|---|---|---|---|---|---|---|---|
| Variables | 6 Month Mean (SD) | 12 Month Mean (SD) | Change (SD) | 6 Month Mean (SD) | 12 Month Mean (SD) | Change (SD) | P |
| Self report MVPA (min/week, 10 minute bouts) | 103.6 (86.5) | 124.0 (95.1) | 12.1 (94.9) | 90.2 (71.6) | 102.5 (94.5) | 5.0 (92.9) | 0.45 |
| Accelerometer MVPA (min/week, 10 minute bouts) | 31.5 (58.9) | 17.7 (40.6) | −17.1 (65.5) | 20.8 (38.2) | 12.4 (31.9) | 1.6 (50.2) | 0.80 |
| Self report strength and flexibility exercise (min/week) | 25.1 (67.5) | 37.0 (69.0) | 9.8 (63.9) | 20.7 (39.8) | 20.0 (31.7) | 0.6 (21.9) | 0.31 |
| 6MWD (meters) | 364.8 (54.7) | 353.9 (52.0) | −10.7 (53.1) | 367.4 (48.8) | 330.5 (48.8) | −40.9 (61.3)* | 0.059 |
| Weight (kg) | 85.6 (13.9) | 85.4 (14.0) | −0.4 (3.4) | 87.4 (14.0) | 89.7 (13.3) | −0.6 (2.9) | 0.91 |
p < 0.05 for within group change, paired t-test
SD=standard deviation
Changes in physical activity related psychosocial variables at 12 months
The HIPP arm reported significantly greater improvements in physical activity related psychosocial variables, such as physical activity goal setting (P = 0.02) and enjoyment (P = 0.04), compared with the control group, after the 6-month active intervention (D. Pekmezi et al., 2017). There were no significant between group differences in changes in any psychosocial variables over the maintenance period, yet the HIPP arm still continued to report higher scores on physical activity goal setting (M=2.88, SD= 0.98 vs. M= 2.37, SD=1.02) and enjoyment (M=100.89, SD=21.23, vs. M=84.7, SD=29.2) than the control arm at 12 months. Moreover, motivational readiness for physical activity appeared higher in the intervention arm, with 66.7% of the intervention arm vs. 44% of the control arm reporting maintenance as their stage of change for physical activity at 12 months. There were no within group differences in changes in any psychosocial variables from 6 to 12 months, with one exception. The control arm reported significant increases in decisional balance scores (Mean change= 0.29, SD= 0.65) over the maintenance period, yet their mean decisional balance score was still lower at 12 months (M=1.84, SD=1.13) than the intervention arm (M=1.95, SD=1.14).
Discussion
Findings indicate that improvements in self-reported physical activity and related psychosocial variables among African American women in the Deep South after 6 months active participation in the Home-based Individually-tailored Physical activity Print (HIPP) intervention (D. Pekmezi et al., 2017) were maintained at 12 months. More importantly, this improvement was achieved with a tapered intervention, consisting of only two maintenance dose mailings over the maintenance period, from months 6 to 12. This study fills an important gap in the literature as few physical activity intervention studies conducted among African American women have followed participants past 6 months (Bland & Sharma, 2017).
We were able to compare our results with similar past physical activity print intervention studies conducted among other minority women (Latinas) (Marcus et al., 2015) and mostly White adults (Marcus et al., 2007). Retention rates at 12 months of 77.4% for African American women in the current study were equivalent to other studies, i.e., 80.8% for Latinas, and 80.25% in the mostly White adult sample. As for physical activity outcomes, HIPP intervention participants on average reported less physical activity at 12 months (124 minutes/week MVPA) than the mostly White participants (M=162.37 minutes/week MVPA), yet more than the Latina participants (M=95.78 minutes/week) at 12 months. Similarly, 44.1% of HIPP intervention participants met national guidelines for physical activity (self-reported MVPA ≥ 150 min per week) at 12 months, whereas almost 50% of mostly White participants and only 16.7% of Latina participants in other studies met guidelines at the same time point. Physical activity-related psychosocial outcomes at 12 months in the current study were analogous to findings from the past physical activity print intervention study among mostly White participants, in that gains in behavioral and cognitive processes of change, self-efficacy, and decisional balance were maintained from 6 to 12 months. Psychosocial data on the Latina participants were not available at this time point.
Strengths of the current study include the use of a theoretical framework and randomized controlled design. Only six of the studies in the previously mentioned review of physical activity interventions for African American women (Bland & Sharma, 2017) were randomized controlled trials. Most of the evidence base in this area rely on quasi-experimental designs and small pilot studies. Moreover, the intervention was grounded in strong behavioral theory, unlike seven of the 13 interventions in the recent review (Bland & Sharma, 2017), which called for more incorporation of theory. The main limitation of the current study is the use of a small sample of community volunteers, which may reduce the generalizability of findings to the overall target population.
Participants also were generally well-educated and findings suggested that participants with higher education levels benefited more from the HIPP intervention, as they reported greater physical activity (almost 74 additional minutes/week of MVPA) at 12 months than those with lower education levels. This contrasts with past findings of King and colleagues, in which less-educated participants were more likely to maintain exercise gains at 2-year assessment (King et al., 1997). These discrepancies in results may be attributed to differences in the literacy requirements of the intervention delivery channels, as HIPP relied on print materials and the SSHIP trial of King et al. involved group-based exercise and/or telephone-based counseling. Regardless, future directions in this area should incorporate lower literacy intervention approaches (telephone counseling, DVDs, etc.). Such strategies will enhance the inclusivity of the HIPP intervention, as well as its effectiveness and relevance for less-educated individuals. This represents a critical next step, as education levels in this region are below the national average (United States Department of Commerce, 2012).
Moreover, participants described interest in strength and flexibility exercise at 6 months (D. Pekmezi et al., 2017)and the substantial participation in such activities at 12 months further confirms the relevance of this topic for African American women in the Deep South. While HIPP currently focuses on aerobic physical activity, strength and flexibility exercises are now emphasized in the national physical activity guidelines and will need to be incorporated in future iterations of this program.
Conclusion
Home-based print physical activity intervention approaches are relatively low cost, bypass frequently cited barriers to participation (transportation, time, childcare), and require minimal effort from research staff. Such maintenance strategies have great potential for scale-up and may represent a promising tool for supporting sustained lifestyle behavior change among African American women in the Deep South, which will be essential to achieving long-term health benefits and eliminating existing cancer disparities in this at-risk target population.
Table 2.
Changes in psychosocial variables from 6 months to 12 months
| Intervention | Control | ||||||
|---|---|---|---|---|---|---|---|
| Variables | 6 Month Mean (SD) | 12 Month Mean (SD) | Change (SD) | 6 Month Mean (SD) | 12 Month Mean (SD) | Change (SD) | Across group p 12 months |
| Pros (range =1–5) | 4.06 (0.84) | 4.00 (0.83) | −0.07 (0.55) | 3.78 (0.88) | 3.88 (0.75) | 0.23 (0.51) | 0.19 |
| Cons (range =1–5) | 2.09 (0.98) | 2.05 (0.97) | 0.01 (0.61) | 2.05 (0.71) | 2.04 (0.78) | −0.06 (0.65) | 0.76 |
| Decisional balance* | 1.95 (1.13) | 1.95 (1.14) | −0.07 (0.62) | 1.75 (0.90) | 1.84 (1.13) | 0.29 (0.65)* | 0.07 |
| Cognitive processes (range =1–5) | 3.45 (0.89) | 3.54 (0.81) | 0.04 (0.60) | 3.24 (0.83) | 3.23 (0.65) | 0.02 (0.47) | 0.48 |
| Behavioral processes (range =1–5) | 3.34 90.69) | 3.56 (0.71) | 0.10 (0.49) | 3.01 (0.73) | 2.99 (0.67) | 0.00 (0.62) | 0.16 |
| Self-Efficacy (range =1–5) | 3.18 (0.88) | 3.07 (0.76) | −0.19 (0.72). | 2.73 (0.81) | 2.84 (0.88) | 0.19 (0.73) | 0.46 |
| Goal setting (range =1–5) | 2.85 (0.83) | 2.88 (0.98) | 0.01 (0.76) | 2.50 (0.96) | 2.37 (1.02) | −0.05 (0.84) | 0.41 |
| Planning (range =1–5) | 2.82 (0.70) | 2.85 (0.80) | −0.05 (0.50) | 2.63 (0.60) | 2.52 (0.77) | 0.01 (0.70) | 0.89 |
| Outcome expectations (range =1–5) | 4.39 (0.81) | 4.49 (0.54) | 0.05 (0.71) | 4.16 (0.62) | 4.20 (0.70) | −0.01 (0.56) | 0.19 |
| Enjoyment (range=18–126) | 101.05 (24.76) | 100.89 (21.23) | −5.04 (17.05) | 91.23 (22.71) | 84.7 (29.2) | −1.26 (27.4) | 0.76 |
| Family support (range=10–50) | 25.94 (10.74) | 26.9 (12.8) | −0.07 (7.59) | 23.81 (9.63) | 24.2 (11.7) | 0.96 (10.44) | 0.89 |
| Friend support (range=10–50) | 22.67 (11.21) | 22.8 (12.5) | 0.56 (8.48) | 19.49 (7.92) | 20.5 (11.3) | 1.58 (9.31) | 0.59 |
| Stages of change | N (%) | N (%) | N (%) | N (%) | 0.09 | ||
| Precontemplation | 0 (0.0) | 2 (7.4) | 0 (0.0) | 0 (0.0) | |||
| Contemplation | 6 (16.47) | 5 (18.5) | 11 (29.33) | 9 (36.0) | |||
| Preparation | 8 (22.22) | 2 (7.4) | 6 (16.22) | 2 (8.0) | |||
| Action | 5 (13.29) | 0 (0.0) | 7 (18.92) | 3 (12.0) | |||
| Maintenance | 17(47.22) | 18 (66.7) | 13 (35.14) | 11 (44.0) | |||
for decisional balance, scores greater than 0 indicate more pros than cons for physical activity and scores less than 0 indicate more cons than pros.
SD=standard deviation
Acknowledgments
This research was supported by the American Cancer Society (MRSG-13–156-01-CPPB), the National Center for Advancing Translational Sciences (UL1TR001417), and National Heart, Lung, And Blood Institute of the National Institutes of Health (T32HL105349). Drs. David Allison, Mona Fouad, and Molly Bray provided substantial earlier contributions to the development of this study. Michelle Constant-Jones, Claudia Hardy, Tara Bowman, Jolene Lewis, and the staff at the Clinical Research Unit of the University of Alabama at Birmingham, as well as Rachelle Edgar of the University of California, San Diego, provided valuable research assistance on this project. We also thank our research participants for their time. This work is dedicated to our beloved colleague and co-author, Dr. Karen Meneses. She was a constant source of knowledge and inspiration and will be deeply missed.
Contributor Information
D. Pekmezi, Department of Health Behavior, School of Public Health, University of Alabama at Birmingham..
M.C. Ainsworth, Department of Health Behavior, School of Public Health, University of Alabama at Birmingham..
R. Desmond, Division of Preventive Medicine, University of Alabama at Birmingham..
M. Pisu, Division of Preventive Medicine, University of Alabama at Birmingham..
V. Williams, Department of Health Behavior, School of Public Health, University of Alabama at Birmingham..
K. Wang, Department of Health Behavior, School of Public Health, University of Alabama at Birmingham..
T. Holly, Department of Epidemiology, School of Public Health, University of Alabama at Birmingham..
K. Meneses, Research in the School of Nursing at the University of Alabama at Birmingham..
B.H. Marcus, Brown University in Providence, Rhode Island..
W. Demark-Wahnefried, University of Alabama at Birmingham..
References
- American Cancer Society. (2016). Cancer Facts & Figures for African Americans 2016–2018. Retrieved from Atlanta: [Google Scholar]
- Bandura A. (1986). Social foundations of thought and action: A social cognitive theory: Prentice-Hall, Inc. [Google Scholar]
- Blair SN, Haskell WL, Ho P, Paffenbarger RS, Vranizan KM, Farquhar JW, & Wood PD (1985). Assessment of habitual physical activity by a sevenday recall in a community survey and controlled experiments. American Journal of Epidemiology, 122(5), 794–804. Retrieved from https://www.scopus.com/inward/record.uri?eid=2-s2.0-0022412672&partnerID=40&md5=087265cef6ec7ca8a0b8bd5215668a85 [DOI] [PubMed] [Google Scholar]
- Bland V, & Sharma M. (2017). Physical activity interventions in African American women: A systematic review. Health Promot Perspect, 7(2), 52–59. doi: 10.15171/hpp.2017.11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Butland RJA, Pang J, Gross ER, Woodcock AA, & Geddes DM (1982). Two-, six-, and 12-minute walking tests in respiratory disease. British Medical Journal, 284(6329), 1607–1608. Retrieved from https://www.scopus.com/inward/record.uri?eid=2-s2.0-0020057635&partnerID=40&md5=e771f567b3a6300001a676939f7dd068 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Canadian Society for Exercise Physiology. (1994). PAR-Q and You. Gloucester, Ontario: Canadian Society for Exercise Physiology. [Google Scholar]
- Centers for Disease Control and Prevention. (2015). National Center for Health Statistics, Health Data Interactive. [Google Scholar]
- Davis TC, Long SW, Jackson RH, Mayeaux EJ, George RB, Murphy PW, & Crouch MA (1993). Rapid estimate of adult literacy in medicine: a shortened screening instrument. Fam Med, 25(6), 391–395. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/8349060 [PubMed] [Google Scholar]
- Freedson PS, Melanson E, & Sirard J. (1998). Calibration of the Computer Science and Applications, Inc. accelerometer. Med Sci Sports Exerc, 30(5), 777–781. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/9588623 [DOI] [PubMed] [Google Scholar]
- Janz KF (1994). Validation of the CSA accelerometer for assessing children’s physical activity. Med Sci Sports Exerc, 26(3), 369–375. [PubMed] [Google Scholar]
- Kendzierski D, & DeCarlo KJ (1991). Physical Activity Enjoyment Scale: Two Validation Studies. Journal of Sport and Exercise Psychology, 13(1), 50–64. doi: 10.1123/jsep.13.1.50 [DOI] [Google Scholar]
- King AC, Kiernan M, Oman RF, Kraemer HC, Hull M, & Ahn D. (1997). Can we identify who will adhere to long-term physical activity? Signal detection methodology as a potential aid to clinical decision making. Health Psychol, 16(4), 380–389. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/9237091 [DOI] [PubMed] [Google Scholar]
- Kushi LH, Byers T, Doyle C, Bandera EV, McCullough M, McTiernan A, . . . Thun MJ (2006). American Cancer Society Guidelines on Nutrition and Physical Activity for cancer prevention: reducing the risk of cancer with healthy food choices and physical activity. CA Cancer J Clin, 56(5), 254–281; quiz 313–254. [DOI] [PubMed] [Google Scholar]
- Marcus BH, Banspach SW, Lefebvre RC, Rossi JS, Carleton RA, & Abrams DB (1992). Using the stages of change model to increase the adoption of physical activity among community participants. Am J Health Promot, 6(6), 424–429. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/10146803 [DOI] [PubMed] [Google Scholar]
- Marcus BH, Dubbert PM, Forsyth LH, McKenzie TL, Stone EJ, Dunn AL, & Blair SN (2000). Physical activity behavior change: issues in adoption and maintenance. Health Psychol, 19(1S), 32–41. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/10709946 [DOI] [PubMed] [Google Scholar]
- Marcus BH, Dunsiger SI, Pekmezi D, Larsen BA, Marquez B, Bock BC, . . . Tilkemeier P. (2015). Twelve-month physical activity outcomes in Latinas in the Seamos Saludables trial. American Journal of Preventive Medicine, 48(2), 179–182. doi: 10.1016/j.amepre.2014.08.032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marcus BH, Napolitano MA, King AC, Lewis BA, Whiteley JA, Albrecht A, . . . Papandonatos GD (2007). Telephone versus print delivery of an individualized motivationally tailored physical activity intervention: Project STRIDE. Health Psychol, 26(4), 401–409. doi: 10.1037/0278-6133.26.4.401 [DOI] [PubMed] [Google Scholar]
- Marcus BH, Rakowski W, & Rossi JS (1992). Assessing motivational readiness and decision making for exercise. Health Psychology, 11(4), 257–261. doi: 10.1037//0278-6133.11.4.257 [DOI] [PubMed] [Google Scholar]
- Marcus BH, Rossi JS, Selby VC, Niaura RS, & Abrams DB (1992). The stages and processes of exercise adoption and maintenance in a worksite sample. Health Psychology, 11(6), 386–395. doi: 10.1037//0278-6133.11.6.386 [DOI] [PubMed] [Google Scholar]
- Marcus BH, Selby VC, Nlaura RS, & Rossi JS (1992). Self-efficacy and the stages of exercise behavior change. Research Quarterly for Exercise and Sport, 63(1), 60–66. doi: 10.1080/02701367.1992.10607557 [DOI] [PubMed] [Google Scholar]
- Melanson EL Jr., & Freedson PS (1995). Validity of the Computer Science and Applications, Inc. (CSA) activity monitor. Med Sci Sports Exerc, 27(6), 934–940. [PubMed] [Google Scholar]
- Pekmezi D, Ainsworth C, Joseph RP, Williams V, Desmond R, Meneses K, . . . Demark-Wahnefried W. (2017). Pilot Trial of a Home-based Physical Activity Program for African American Women. Med Sci Sports Exerc, 49(12), 2528–2536. doi: 10.1249/MSS.0000000000001370 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pekmezi D, & Jennings E. (2009). Interventions to Promote Physical Activity Among African Americans. American Journal of Lifestyle Medicine, 3(3), 173–184. [Google Scholar]
- Pereira MA, FitzerGerald SJ, Gregg EW, Joswiak ML, Ryan WJ, Suminski RR, . . . Zmuda JM (1997). A collection of Physical Activity Questionnaires for health-related research. Medicine and science in sports and exercise, 29(6 Suppl), S1–205. Retrieved from https://www.scopus.com/inward/record.uri?eid=2-s2.0-0031155915&partnerID=40&md5=521c926c6b4868ebc97a6aacbb9241e0 [PubMed] [Google Scholar]
- Prochaska JO, & DiClemente CC (1983). Stages and processes of self-change of smoking: Toward an integrative model of change. Journal of Consulting and Clinical Psychology, 51(3), 390–395. doi: 10.1037/0022-006X.51.3.390 [DOI] [PubMed] [Google Scholar]
- Resnick B, Zimmerman SI, Orwig D, Furstenberg A-L, & Magaziner J. (2000). Outcome Expectations for Exercise Scale: Utility and Psychometrics. The Journals of Gerontology Series B: Psychological Sciences and Social Sciences, 55(6), S352–S356. doi: 10.1093/geronb/55.6.S352 [DOI] [PubMed] [Google Scholar]
- Rovniak LS, Anderson ES, Winett RA, & Stephens RS (2002). Social cognitive determinants of physical activity in young adults: a prospective structural equation analysis. Ann Behav Med, 24(2), 149–156. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/12054320 [DOI] [PubMed] [Google Scholar]
- Sallis JF, Grossman RM, Pinski RB, Patterson TL, & Nader PR (1987). The development of scales to measure social support for diet and exercise behaviors. Preventive Medicine, 16(6), 825–836. doi: 10.1016/0091-7435(87)90022-3 [DOI] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services. (2017). United States Cancer Statistics: 1999–2014 Incidence and Mortality Web-based Report. Retrieved from www.cdc.gov/uscs
- United States Census Bureau. (2011). 2010 Census Shows Black Population has Highest Concentration in the South. Retrieved from https://www.census.gov/newsroom/releases/archives/2010_census/cb11-cn185.html
- United States Department of Commerce. (2012). 2010 Census Population and Housing Tables. [Google Scholar]
- Whitt-Glover MC, Keith NR, Ceaser TG, Virgil K, Ledford L, & Hasson RE (2014). A systematic review of physical activity interventions among African American adults: evidence from 2009 to 2013. Obes Rev, 15 Suppl 4, 125–145. doi: 10.1111/obr.12205 [DOI] [PubMed] [Google Scholar]