Abstract
Study Design:
Systematic review.
Objective:
Spinal orthoses have been generally used in the management of osteoporotic vertebral fractures in the elderly population with purported positive biomechanical and functional effects. To our knowledge, this is the first systematic review of the literature examining the role of spinal orthoses in osteoporotic elderly patients who sustain low energy trauma vertebral fractures.
Methods:
A systematic literature review adherent to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines was conducted. Methodical searches utilizing MEDLINE, EMBASE, Google Scholar, and Cochrane Databases was performed.
Results:
Of the 2019 articles initially retrieved, 7 published articles (4 randomized controlled trials and 3 prospective cohort studies) satisfied the inclusion criteria. Five studies reported improvement in quantitative measurements of spinal column stability when either a rigid or semirigid orthosis was used, while 1 study was equivocal. The studies also showed the translation of biomechanical benefit into significant functional improvement as manifested by improved postural stability and reduced body sway. Subjective improvement in pain scores and quality of life was also noted with bracing.
Conclusion:
The use of spinal orthoses in neurologically intact elderly patients aged 60 years and older with osteoporotic compression vertebral fractures results in improved biomechanical vertebral stability, reduced kyphotic deformity, enhanced postural stability, greater muscular strength and superior functional outcomes.
Keywords: braces, osteoporotic fractures, spinal fractures, orthotic devices
Introduction
Low-energy traumatic osteoporotic vertebral fractures (OVFs) are the archetypal manifestation of osteoporosis; a systemic disequilibrium between bone modeling and remodeling leading to reduced bone mineral density and increased bone fragility. 1 The incidence of OVFs is estimated to be 5% to 10% in women in their fifth and sixth decades of life, and more than 30% in those aged 80 years or older. 2,3 In the setting of an aging population, a rise in the incidence of OVFs is anticipated. 4,5 Vertebral fractures not only predict future osteoporotic fractures, either of the spine or the hip but also carry an overall increase in mortality up to 15%. 6 –9 Despite their high prevalence and potential significance in relation to mortality and morbidity, only one-third are symptomatic. 10,11 This may explain why, despite escalating prevalence, the implementation of medical and adjunct therapies has not seen a corresponding rise. 1
Management options for OVFs include analgesia, physiotherapy, a rigid or semirigid orthosis, lumbosacral orthosis, garment orthoses, or surgical intervention such as percutaneous kyphoplasty or vertebroplasty with or without instrumentation. The supporting role of an orthosis is to limit the range of motion and promote neutral vertebral alignment as the fracture heals, minimize secondary traumatic injury, improve posture, alleviate pain, and allow time for antiresorptive treatments to take effect. 3 However, it has been contended that orthosis use results in weakening of paraspinal musculature bulk with subsequent increased fragility, as well as complications such as pressure ulcerations. 12
Utilization of bracing has at times caused angst in the medical community as there is a paucity of literature. Concepts of the weakening of skeletal mechanical and postural musculature and reduced proprioceptive ability leading to debility, and psychosocial deterioration are a few reasons a proportion of rehabilitative, geriatric, family care practitioners and allied health members shun bracing as a valid option for this complex condition.
The goal of this study is to evaluate the role of spinal orthoses with regard to vertebral stability, muscular strength, and functional outcome in OVFs in the elderly. For the purpose of this study, we have defined elderly as an age of ≥60 years. 13 This is the first systematic review evaluating the role of spinal braces in the elderly population who have sustained an OVF.
Methods
Eligibility Criteria
The Population, Intervention, Comparison, and Outcome (PICO) question for this systematic review was: “In the elderly population, considered as aged 60 years or older (P), does the use of a spinal orthosis or brace (I) of any type such as rigid, semirigid, or elastic (C) result in improved biomechanical or functional outcomes (O)?”
Information Sources and Search
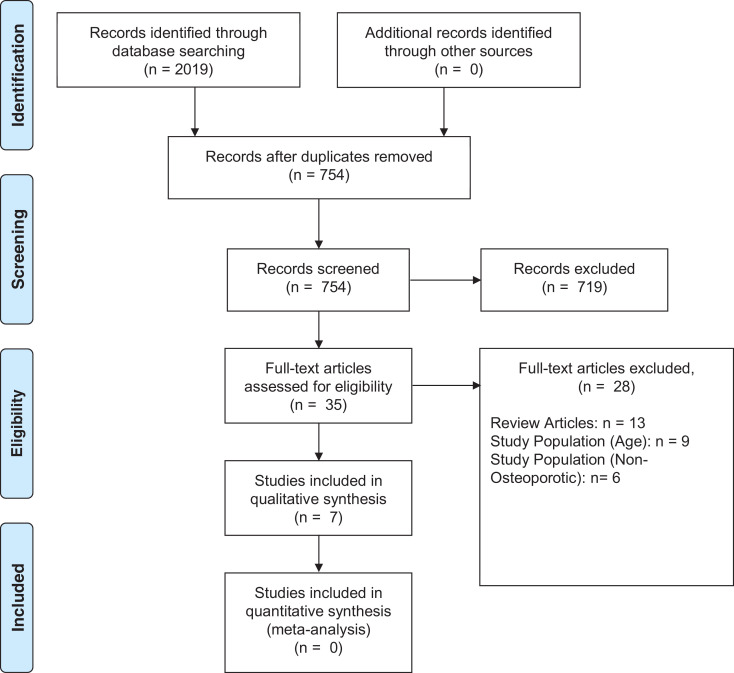
In accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines, we performed a systematic electronic search of Medline, EMBASE, Google Scholar, and Cochrane Database of Systematic Reviews from their date of inception to December 2019 (Figure 1). 14 A broad search strategy was favored with the keywords in order to capture as many potentially relevant articles as possible. For example, the Medline database was queried with the following search terms in various Boolean combinations: “Spine,” “Vertebral,” “Thoracic Vertebra*,” “Lumbar Vertebra*,” “Fracture,” “Spinal Fractures,” “Compression Fracture,” “Osteoporotic Fracture,” “Orthosis,” “Brace.” Only studies in the English language evaluating humans were included. Notably, we deliberately excluded the restrictive term of “elderly” in the search to retrieve as many potentially relevant studies as possible, which may yet still have salvageable and applicable subgroup analyses of interest.
Figure 1.
Search strategy flow diagram in accordance with the Preferred Reporting Itemsfor Systematic Reviews and Meta-Analyses (PRISMA) protocol. 14
Study Selection
Two reviewers (BK and JT) independently screened the titles and abstracts of all returned search results. Following this, full-text articles of the retrieved studies were assessed for suitability of inclusion. The bibliography and citing articles of all included studies were also screened to identify additional eligible articles. Discrepancies were discussed until consensus attained. Inclusion criteria were defined as (1) randomized or nonrandomized controlled trials, any cohort study examining the role of a form of spinal orthosis in patients aged 60 years or older who sustained an OVF of the thoracolumbar spine without high-energy trauma; (2) any follow-up time acceptable with immediate or delayed assessment of the effect of a brace being of interest; and (3) human studies. If 2 studies were encountered with shared data, the study with the largest dataset was to be preferred.
Data Collection Process and Data Items
Data from all eligible studies was independently extracted into a preformatted form by one author (BK) and cross-checked by another (JT) in accordance with the Cochrane Handbook for Systematic Reviews. 15 No authors were contacted for further unpublished data.
All quantitative data was to be collected to facilitate a meta-analysis where possible. Outcome variables of interest included vertebral body height progress or indirect measurements of vertebral body union such as Cobb’s angle or kyphosis angle, quality of life scores, lower back pain scores, functional outcomes measurements such as muscular strength, body sway and postural balance markers, and respiratory function.
Risk of Bias
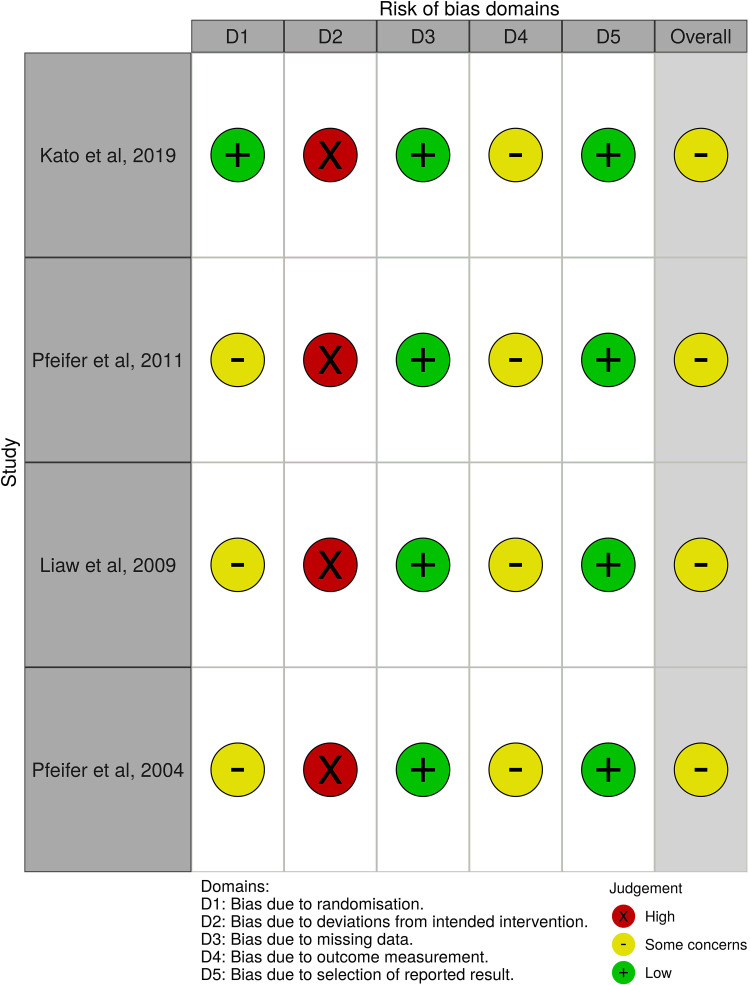
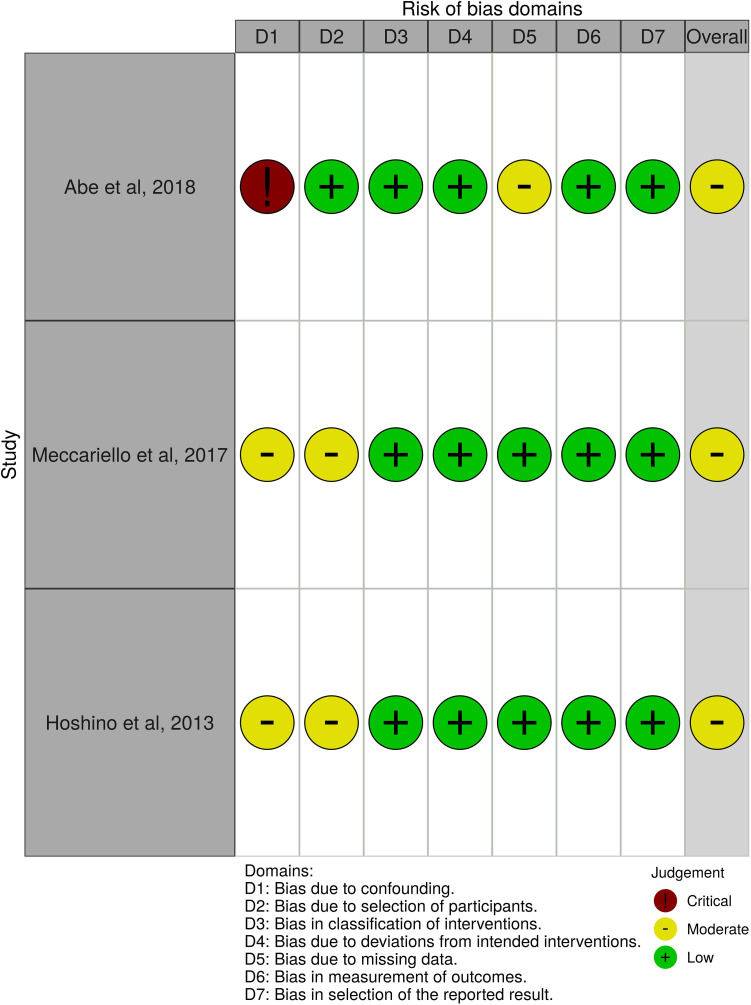
Risk of bias in individual studies was assessed in accordance with Cochrane recommendations. 15 The Risk of Bias of Randomized Controlled Trials 2 (RoB 2) and the Risk Of Bias In Non-Randomized Studies of Interventions (ROBINS-I) tool was applied for the included randomized and nonrandomized studies, respectively. 16,17 Study quality was independently assessed by 2 authors (BK and JT) with consensus attained following discussion. The “Robvis” tool was utilized to generate the traffic light plot in accordance with Cochrane recommendation. 18
Synthesis of Results
A meta-analysis is to be performed where possible regarding the above outcomes.
Results
Study Selection
The initial search yielded 2019 articles, which were distilled to 754 after removal of duplicates. Abstracts were screened leading to 35 studies warranting full-text assessment for eligibility. This eventually yielded 7 articles, comprising 4 randomized controlled trials and 3 prospective cohort studies, with the reasons for the exclusion of assessed full-text articles displayed in Table 1. Common reasons for exclusion were review articles retrieved without original datasets, inappropriate study population age group with patients less than 60 years old, or inclusion of patients without osteoporosis.
Table 1.
Complete List of 28 Full-Text Articles Assessed and Reason for Exclusion.
| Reason for exclusion | Type of orthosis | ||||
|---|---|---|---|---|---|
| Rigid | Semirigid | Flexible or elastic | Mixed orthoses | ||
| Thoracolumbosacral orthosis (TLSO): Taylor brace, Knight-Taylor brace |
Thoracolumbar orthosis (TLO): Jewett, cruciform anterior spinal hypertension (CASH) orthoses |
Thoracolumbar Backpack (TLO): Spinomed | Garment: Spinomed active, Osteomed orthosis |
||
| Age group | Murata et al, 201 2 19 | Shariatzadeh et al, 201 6 20 | Jacobs et al, 201 9
21
Li et al, 201 5 22 Valentin et al, 201 3 23 |
Vogt et al, 200 8 24 | Dionyssiotis et al, 201 5
25
Kim et al, 201 4 26 Talic et al, 201 2 27 |
| Non–osteoporotic vertebral fractures | Urquuhart et al, 201 6
28
van Leeuwen et al, 200 0 29 Jones et al, 198 7 30 |
Alin et al, 201 9 31 | Stadhouder et al, 200 9 32 | Chiba et al, 201 1 33 | |
| Review article | Ameis et al, 201 8
34
Muratore et al, 201 8 35 Rajasekaran et al, 201 7 36 Goodwin et al, 201 6 37 Jin et al, 201 6 38 McCarthy et al, 201 6 39 Newman et al, 201 6 40 |
Karimi et al, 201 5
41
Rzewuska et al, 201 5 42 Chang et al, 201 4 43 Longo et al, 201 1 44 Lin et al, 200 8 45 Bonaiuti et al,200 5 46 |
|||
Study Characteristics
The 7 included studies examined rigid, semirigid, and elastic orthotic devices in 1157 participants with a mean age of 77.2 years (Table 2). All studies examined osteoporotic compression vertebral fractures in elderly patients without any evidence of neurological compromise. The majority of the studied population was female (78.3%). Trials were performed in Germany, Italy, Japan, and Taiwan. The type of orthosis studied and further characteristics are summarized in Table 3.
Table 2.
Study Design and Patient Demographics of the 4 Randomized Controlled Trials (RCTs) and 3 Prospective Cohort Studies Which Were Included.
| Study | Study design | Indication for orthosis | Participant source | Sample size | Female gender (%) | Mean age intervention group (range), years | Average age comparison group (range), years |
|---|---|---|---|---|---|---|---|
| Kato et al, 201 9 47 | RCT | Osteoporotic females with acute single-level vertebral compression fracture | Hospital | 284 | 100 | 76.0 (70.8-81.2) | 75.5 (70.1-80.9) |
| Abe et al, 201 8 48 | Prospective cohort | Osteoporotic patients with single-level vertebral fracture | Hospital | 154 | 85.7 | 81.2 (60-98) | |
| Meccarielloet al, 201 7 49 | Prospective cohort study | Osteoporotic patients with acute single-level vertebral compression fracture | Hospital | 140 | 71.4 | 81.9 (65-90) | 82.8 (65-93) |
| Hoshino et al, 201 3 50 | Prospective cohort | Osteoporotic patients with acute vertebral fracture | Hospital | 362 | 83.7 | 76.2 (NR) | 77.0 (NR) |
| Pfeifer et al, 201 1 51 | RCT | Osteoporotic women with vertebral fracture | Community | 108 | 100 | Group 1 (Spinomed): 72.8 (65.7-79.9) Group 2 (Spinomed active): 72.3 (65.6-79.0) |
69.7 (60.8-78.6) |
| Liaw et al, 200 9 52 | Cross RCT | Osteoporotic patients with vertebral compression fracture | Hospital | 47 | 78.7 | 68.2 (59.6-76.8) | |
| Pfeifer et al, 200 4 53 | RCT | Osteoporotic women with subacute vertebral fracture | Community | 62 | 100 | 72.8 (65.7-79.9) | 72.3 (65.6-79.0) |
Abbreviations: RCT, randomized controlled trial; NR, not reported.
Table 3.
Intervention Characteristics of Included Studies.
| Study | Intervention group | No. of participants: intervention | Comparison group | No. of participants: comparison | Phase of fracture | Level of fracture | Duration of orthosis use | Follow-up |
|---|---|---|---|---|---|---|---|---|
| Kato et al, 201 9 47 | Rigid TLSO | 141 | Soft TLSO | 143 | Acute | T10-L2 | 12 weeks | 4, 8, 12, 24, and 48 weeks |
| Abe et al, 201 8 48 | Rigid TLO (Jewett brace) proceeding 2 weeks of bed rest | 154 | Nil | Not applicable | Acute | T4-L5 | 12-24 weeks | 6-8, and 24 weeks |
| Meccariello et al, 201 7 49 | Three-point orthosis (3PO) | 72 | TLO Backpack (Spinomed) | 68 | Acute | T6-L3 | 10 weeks | 1, 3, and 6 months |
| Hoshino et al, 201 3 50 | Brace Tailor-made hard Tailor-made elastic Ready-made elastic |
327 | No brace | 35 | Acute | T5-L5 | 4.1 months (2.2-6.0) | 6 months |
| Pfeifer et al, 201 1 51 | Group 1: Spinomed orthosis Group 2: Spinomed active orthosis |
Group 1: 36 Group 2: 36 |
No brace | 36 | Subacute | NR | 6 months | 6 months |
| Liawet al, 200 9 52 | Rigid TLSO (Knight-Taylor orthosis) | 47 | No brace | 47 | NR | NR | Immediate | Immediate |
| Pfeifer et al, 200 4 53 | Spinomed orthosis | 31 | No brace | 31 | Subacute | NR | 6 months | 6 months |
Abbreviations: TLSO, thoracolumbosacral orthosis; TLO, thoracolumbar orthosis; NR, not reported.
Study Quality
Risk of bias assessment was evaluated for included randomized and nonrandomized controlled trials with the RoB 2 and ROBINS-I tools, respectively, in a Cochrane-endorsed fashion (Figures 2 and 3). 16,17 The inability to effectively blind participants to the use of an orthosis resulted in an inherent performance bias in all included studies.
Figure 2.
Risk of bias as assessed by the Risk of Bias of Randomized Controlled Trials (RoB 2) tool based on the Cochrane Handbook for Systematic Reviews of Interventions. 16
Figure 3.
Risk of bias as assessed by the Risk Of Bias In Non-Randomized Studies of Interventions (ROBINS-I) tool as recommended by the Cochrane Handbook for Systematic Reviews of Intervention. 17
Results of Individual Studies
Both the heterogeneity of outcomes and type of spinal orthosis investigated precluded an effective meta-analysis from being conducted. Instead, we present a tabulated summary of the trials and their relevant results (Table 4). This is followed by a comprehensive narrative review.
Table 4.
Primary and Secondary Outcomes of Included Studies.
| Study | Outcomes | Conclusion |
|---|---|---|
| Kato et al, 201 9 47 | Primary outcome: Anterior vertebral body compression percentage (AVBCP) at 48 weeks. Secondary outcomes: European Quality of Life-5 Dimensions, 3-Level Questionnaire (EQ-5D-3L) Visual analogue scale (VAS) for lower back pain Japanese Orthopedic Association Back Pain Evaluation Questionnaire (JOQBPEQ) |
Primary outcome: No significant difference in AVBCP Secondary outcomes All scores (EQ-5D-3L), VAS, JOQBPEQ significantly improved after application of either brace No significant differences between 2 groups |
| Abe et al, 201 8 48 | Primary outcome: Average vertebral instability: absolute difference of the vertebral wedging angle between standing and supine position Secondary outcomes: Average vertebral instability stratified in union versus delayed union groups (delayed union defined as greater than 5 degrees of wedging angle at 24 weeks) Length of hospital stay between union and delayed union groups |
Primary outcome: Average vertebral instability 4.9° ± 4.8° at 3 weeks, 2.9° ± 3.5° at 6-8 weeks, and 1.8° ± 3.0° at 24 weeks Secondary outcomes: Vertebral instability at 3 weeks, 6-8 weeks, and 24 weeks higher in delayed union group than union group No statistically significant difference in length of hospital stay between union and delayed union groups |
| Meccariello et al, 201 7 49 | Primary outcomes—functional recovery: Visual analogue scale (VAS) for pain Oswestry Low Back Pain Disability Questionnaire (OLBPDQ) Measurement of forced expiratory volume in first second (FEV1) Secondary outcomes—radiological: Union rate Regional kyphosis angle (RKA) Height of fractured vertebral body on full-spine X-ray Cobb’s angle Delmas Index |
Primary outcomes (statistically significant) Decreased VAS pain scores, reduced OLBPDQ disability scores, and improved FEV1 volumes in Spinomed group at 3 and 6 months compared with 3PO group Secondary outcomes: No statistically significant difference in union rate, RKA, or mean vertebral body height No statistically significant difference of Cobb’s angle or Delmas Index Complications: Lower rate of complications in Spinomed than 3PO group (11.7% vs 38.8%, P < .05) |
| Hoshino et al, 201 3 50 | Primary outcomes: Quality of life by the Short-Form-36 (SF-36) Physical Component Summary (PCS) Activities of Daily Living (ADLs) by the Japanese Long-Term Care Insurance System Visual analogue scale (VAS) for Back Pain Cognitive status by the Mini-Mental State Examination (MMSE) Secondary outcome: Vertebral collapse ratio—anterior body height of the fractured vertebral body divided by those of adjacent intact vertebral bodies |
Primary outcomes: Intervention factors of brace type demonstrated no significant differences in SF-36 PCS, ADLs, VAS, or cognitive scores Middle-column injuries were found to be a significant risk factor for reduced SF-36 and ADL scores, prolonged back pain, and vertebral collapse |
| Pfeifer et al, 201 1 51 | Primary outcomes: Back extensor strength Abdominal flexor strength Degree in angle of kyphosis Body sway Vital capacity Average pain with Miltner’s Rating Scale Well-being with Hobi’s Scale Limitations of daily living with Leidig-Bruckner Questionnaire |
Primary outcomes: Favoring group 1 (Spinomed) and group 2 (Spinomed active) group: Back extensor strength—72% and 64% increase Abdominal flexor strength—44% and 56% increase Degree in angle of kyphosis—11% and 11% decrease Body sway—23% and 20% decrease Vital capacity—19% and 18% increase Average pain—41% and 47% decrease Well-being—18% and 18% increase Limitations of daily living—49% and 54% decrease |
| Liaw et al, 200 9 52 | Primary outcomes (assessed by computerized dynamic posturography): Sensory organization test (SOT) Limit of stability (LOS) Rhythmic weight shift test (RWS) |
Primary outcomes: Knight-Taylor brace resulted in greater average stability, greater average maximal stability under swayed vision and decreased average velocity of sway with reduced frequency of falls However, brace also resulted in significant decrease in overall percentage of directional control |
| Pfeifer et al, 200 4 53 | Primary outcomes: Back extensor strength Abdominal flexor strength Degree in angle of kyphosis Body sway Vital capacity Average pain with Miltner’s Rating Scale Well-being with Hobi’s Scale Limitations of daily living with Leidig-Bruckner Questionnaire |
Primary outcomes. All in favor of Spinomed orthosis group: Back extensor strength—73% increase Abdominal flexor strength—58% increase Degree in angle of kyphosis—11% decrease Body sway—25% decrease Vital capacity—7% increase Average pain—38% decrease Well-being—15% increase Limitations of daily living—27% decrease |
Vertebral Stability
Six studies examined the mechanical effects of orthoses on the vertebral column. Kato et al 47 defined the anterior vertebral body compression percentage (AVBCP) as the ratio between the vertical height of the compressed anterior section to the posterior section at the same level. The mean AVBCP favored the rigid brace treatment group at 12 weeks (58.5% vs 54.6%, P = .04), 24 weeks (56.6% vs 52.7%, P = .07), and 48 weeks (55.5% vs 53.0%, P = .20), but notably only attained statistical significance following 12 weeks of orthosis use. 47
Conversely, Meccariello et al 49 demonstrated that average height loss was less in the dynamic corset Spinomed (SDO) group than in the rigid 3-point orthosis (3PO) group (4.9 vs 5.3 cm, P > .05) after 6 months but was not adequately powered to achieve statistical significance. At this time, the Cobb’s angle was also similar in both groups (27.1° in 3PO and 27.3° in SDO), as was the Delmas index (92.5 in 3PO, 93.6 in SDO) and union rate (93% in 3PO and 94% in SDO). 49 This is consistent with the findings of Pfeifer et al 51,53 who found that vertebral body height increased when wearing either the Spinomed brace (+5.3 ± 6.3, P < .01) or the Spinomed active brace (+6.1 ± 5.0, P < .01). This correlated with a decrease in the angle of kyphosis at −7.9 ± 4.9 (P < .01) and −8.1 ± 10.5 (P < .01), respectively. 51,53
In a similar manner, Abe et al 23 examined the utility of 2 weeks of rigorous bedrest either in the lateral position or semi-Fowler position at 20° to 30° followed by implementation of the rigid Jewett brace. Vertebral instability showed a progressive decline at 3 weeks (4.9° ± 4.8°), 6 to 8 weeks (2.9° ± 3.5°), and finally at 24 weeks (1.8° ± 3.0°). 48 The prospective cohort study by Hoshino et al 50 found that there was no statistically significant difference in the odds ratio of sustaining vertebral collapse between tailor-made hard brace compared with tailor-made elastic (0.42, 0.23-1.19), ready-made elastic (0.57, 0.26-1.22) or no brace (0.43, 0.16-1.19).
Postural Stability
Three studies supported the positive impact of a brace on balance and functional stability. Liaw et al 52 utilized computed posturography to examine the effect of wearing the rigid Knight-Taylor brace, discovering that orthosis use resulted in improved average stability (68.3% ± 8.5% vs 63.6% ± 10.5%, P < .001), superior average maximal stability under swayed vision (87.0% ± 4.2% vs 84.6% ± 7.1%, P = .012), greater average percentage of ankle strategy (83.7% ± 5.7% vs 82.0% ± 6.1%, P = .013) and decreased average velocity of center of gravity target sway (0.85 ± 0.24 vs 0.92 ± 0.31 deg/s, P = .0001). This translated to a lower frequency of falls in all subtests, despite the Knight-Taylor brace resulting in a decrease in overall directional control. 52
Pfeifer et al 51,53 similarly determined an improvement in body sway at 6 months with the Spinomed brace showing a decrease in sway of 5.9 ± 7.2 mm/s (P = .03), and the Spinomed active orthosis a decrease by 6.2 ± 7.4 mm/s (P = .02).
Muscular Strength
Three studies investigated orthosis effect on muscular strength both directly with pressure gauge measurement and indirectly with respiratory function as a surrogate. Pfeifer et al 51,53 showed that back extensor strength, quantitatively measured in newtons, was improved by both the Spinomed orthosis (189 ± 141, 95% CI 125.1-238.9, P < .01) and Spinomed active orthoses (+166 ± 120, 95% CI 137.4-212.3, P < .01). An increase in abdominal flexor strength was also observed in both orthoses groups (+94 ± 71, 95% CI 41.2-100.8, P < .01 and +135 ± 83, 95% CI 63.4-115.7, P < .01). 51,53
Meccariello et al 49 examined forced expiratory volume in 1 second (FEV1) and found that there was no difference in average FEV1 between a rigid 3PO and Spinomed at 1 week or 1 month, but improvement at 6 months in the Spinomed group 77.3% (67%-93%) compared with the 3PO group 65.8% (54%-84%). In concordance with this finding, Pfeifer et al 51,53 also determined that the Spinomed brace resulted in an increase in FEV1 of 2.9% ± 13.5% (P = .04) at 6 months, and the Spinomed active orthosis an increase by 3.1% ± 17.3% (P = .04). In addition, vital capacity in both the Spinomed (6.1% ± 20.5%, P < .01) and Spinomed active (5.5% ± 13.1%, P = .03) groups. 51,53 Significantly, the FEV1 decreased in the control group (3.8% ± 16.1%). 51,53
There is therefore statistically significant moderate quality evidence that orthosis use, whether rigid or semirigid, improves abdominal and paraspinal muscle strength. Additionally, semirigid orthosis use improves respiratory function.
Pain
Five studies assessed the effect of orthoses on pain. Kato et al 47 reported that the mean visual analogue score (VAS) of both rigid brace (28.2) and soft brace (26.3) treatment was lower at 48 weeks compared with commencement. The soft brace was favored by participants (difference −1.9, 95% CI −8.7 to 5.1, P = .43), but this did not reach statistical significance to demonstrate superiority to the rigid brace. 47
Another study compared VAS scores following use of the 3PO or the Spinomed brace. There was no difference at 1 month, but lower scores were detected in the Spinomed group of 4.3 (3-6) and 3.9 (1-4) at 3 and 6 months while the 3PO group scores remained constant at 5.6 (4-8) and 5.6 (3-8). 49 This is contradicted by Hoshino et al 50 who found no difference in prolonged back pain, defined in this study as a VAS greater than 5 out of 10 at 6-month follow-up, between the tailor-made hard brace, tailor-made elastic brace, ready-made elastic brace, or no brace.
When pain was assessed with an alternative score such as the Japanese Orthopedic Association Back Pain Evaluation Questionnaire (JOQBPEQ) score, participants also favored soft braces (60.6) over rigid braces (57.3) at 48 weeks (difference 3.3, 95% CI −4.4 to 11.0, P = .43). 47 However, the study was not sufficiently powered to achieve statistical significance. 47 The Oswestry Lower Back Pain Disability Questionnaire (OLBPDQ) showed long-term improvement in scores of 76.5 (68-100) in the 3PO group and 75.9 (68-100) at 1 month with no significant difference, but fell at 3 months (63.6 vs 57.3) and 6 months (43.6 vs 37.5) with a statistically significant difference. 49
Pfeifer et al 51,53 supported these findings determining that average pain on Miltner’s Rating Scale decreased in either the Spinomed (−1.5 ± 1.2, P < .01) or the Spinomed active group (−1.4 ± 1.1, P < .01) with an increased in the control (+0.1 ± 0.9). The disability score also decreased in both groups at −2.1 ± 1.6 (P < .01) and −2.0 ± 1.5 (P < .01) in the Spinomed and Spinomed active groups, respectively. 51,53
Quality of Life
Four studies examined longitudinal quality of life changes following implementation of a spinal orthosis. Kato et al 47 elected to employ the European Quality of Life-5 Dimensions, 3-Level Questionnaire, which demonstrated an improvement in both rigid and soft brace treatment groups (0.74 vs 0.74, P = .67) without adequate power to reach statistical significance. This was similar to the result of another prospective cohort study comparing SF-36 scores when using the tailor-made hard brace compared with tailor-made elastic braces (1.39, 0.73-2.65 and 1.10, 0.55-2.21), ready-made elastic braces (1.01, 0.45-2.27 and 0.99, 0.42-2.36), or no brace (1.14, 0.43-2.98 and 1.04, 0.35-3.09). 50 There seemed to be a slight favoring of the ready-made elastic brace with less reduction in activities of daily living at 0.60 (0.22-1.65) compared to the tailor-made elastic brace (1.03, 0.50-2.15) and no brace (1.68, 0.56-5.10) but was not of statistical significance. 50
Pfeifer et al 51,53 determined that wearing either the Spinomed or Spinomed active brace improved well-being on Hobi’s Scale at an increase in +10.3 ± 7.9 (P < .01) and +10.7 ± 8.2 (P < .01) respectively, compared with a negative outcome in the control group without orthosis of −2.3 ± 3.0.
Cognitive Status
Two studies evaluated mental health following orthosis use. Kato et al 47 included a subgroup breakdown of mental health assessment, with scores improving at 48 weeks with both rigid brace (55.9 vs 52.1)and soft brace treatment (55.6 vs 54.5) without a statistically significant difference between the 2 groups. Similarly, Hoshino et al 50 could not separate the tailor-made hard brace from the odds ratio of cognitive impairment on the Mini-Mental State Examination from the tailor-made elastic brace (1.55 041-5.00) or the ready-made elastic brace (0.91, 0.13-6.21).
Complications
Two studies recorded complications of orthosis use. Kato et al 47 reported 7 patients in the rigid brace group and nine in the soft brace developed new vertebral fractures, without any significant difference between the groups (OR 0.78, 95% CI 0.23-2.42). On the other hand, Meccariello et al 49 favored the Spinomed group with a lower complication rate (11.7%) compared with the rigid 3PO group (38.8%, P < .05). The majority of the complications involved gastric ulcers, decubitus ulcers, inguinal hernias, or refracture. 49
Discussion
This is the first systematic review to investigate the role of spinal orthoses on biomechanical and functional outcomes following osteoporotic compression vertebral fractures in the elderly cohort aged 60 years or greater. The fundamental role of an orthosis is to promote vertebral fracture healing and stability, encourage anatomical posture, minimise post-traumatic kyphotic deformity and improve quality of life. 54 Although there still exists a lack of international consensus regarding classification of OVFs, the German Society for Orthopaedics and Trauma (DGOU) have proposed 5 subtypes based on degree of vertebral deformity. 55 This classification can be used in conjunction with the DGOU recommendations (which also takes into consideration neurological status, visual analogue pain score, and bone mineral density) to guide clinicians as to whether fractures can be conservatively managed or may require surgical fixation. 56 All elderly patients included in our study sustained osteoporotic vertebral compression fractures without neurological compromise (not DGOU types 4 or 5), which were deemed suitable by the authors for conservative management with bracing. However, we have determined through an exhaustive literature search that despite the vast array of orthoses available, ranging from rigid to semirigid dynamic braces such as Spinomed or the more flexible Spinomed active, there is a scarcity of high-quality evidence to guide clinicians on the indications or duration regarding implementation of these useful adjuncts. Consequently, this has led to previous meta-analyses, in the general rather than elderly population, of equivocal nature without clear recommendations concerning their use. 37,38,40
It has been previously posited that immobilization with orthoses leads to muscle atrophy and is therefore paradoxically detrimental to vertebral healing and posture. Indeed, one survey demonstrated that a similar belief was held by up to 50% of clinicians. 12 As such, the dynamic semi-rigid Spinomed brace was developed with the theoretical advantage of providing not only stability at rest, but also generating tactile feedback to the wearer. 51 This served as a reminder for the user to activate their own musculature and minimize a kyphotic posture through a biomechanical feedback loop. What this review elucidates is that, in the elderly population, there is actually low to moderate quality evidence from 5 studies, which suggests a brace is likely to facilitate vertebral healing as evidenced by multiple outcome measures. 47 –49,51,53 Vertebral height and kyphotic angle are also improved with orthosis use for 12 weeks or more. 48,49,51,53 Ambiguity remains regarding the superiority of one form of orthosis over another. 47 Nonetheless, it is striking that there was no evidence in any of the included studies that orthosis use had negative biomechanical consequences in the elderly population. 47 –49,51
This biomechanical benefit of spinal orthoses translated into functional improvement in three of the studies. 51 –53 Immobilization with spinal orthoses has previously been theorized to lead to disuse muscle atrophy following muscle unloading and therefore attenuation of protein synthesis via the Akt-mTOR pathway and alterations in the myonuclear domain. 57,58 However, Fayolle-Minon et al 59 demonstrated that there was no statistically significant change in isometric strength after 21 days of lumbar orthosis use. Furthermore, Pfeifer et al 51,53 in 2 separate studies found marked improvements in extensor and flexor strength following orthosis use. As such, disuse atrophy may be a consequence of ageing but this systematic review demonstrates there is both immediate benefit to postural stability and delayed benefit to muscle strength with orthosis use. 51 –53,60
These findings are in alignment with the electrophysiological literature investigating the effects of spinal orthoses on muscle strength. Cholewicki et al 61 performed electromyographic studies which reported no evidence of detrimental effect on neuromuscular function in subjects who wore a lumbosacral orthosis. Furthermore, Kawaguchi et al 62 concluded that an orthosis increases the strength of musculature with reduced electromyographic muscle activity. This is consistent with orthoses reducing axial load during performance. 62 In a systematic review of 35 studies examining lumbosacral supports, Azadinia et al 63 determined that the majority of studies showed either no change or an improvement in muscle strength. The exception uncovered was a single study which found a reduced cross-sectional area of the abdominal and para-spinal musculature on ultrasonography following the use of lumbar belts rather than true spinal orthoses. 64 Therefore, evidence from the neurosurgical and electrophysiological literature advocates for the use of spinal orthosis use from a functional perspective.
Additionally, there is moderate quality evidence that spinal orthosis use in OVFs reduces pain and improves quality of life. 47,49 –51,53 The adverse effects of pain on recovery are intuitive. For example, Knopp-Sihota et al 65 demonstrated that pain was inversely related to degree of mobility. In turn, mobility is inextricably linked to functional improvement. 25 Furthermore, pain may impair respiratory function which is of particular importance given Chen et al 6 emphasized that chest infection is the leading cause of death in OVFs. This review uncovered moderate-quality evidence that both FEV1 and vital capacity is likely to be improved by wearing a spinal orthosis, further advocating for spinal orthosis use. 49,51,53 An important consideration regarding quality of life is that the compliance rate with orthosis use has been noted by Kato et al 47 to be lower with rigid compared to semirigid braces due to wearer discomfort. This poor compliance rate was remedied by Pfeifer et al 51 by using a semirigid orthosis with excellent effect: 105 of their 108 patient cohort completed 6 months of the intervention, and 100 subjects were still utilizing the orthosis after 12 months. As such, concerns regarding orthosis compliance should not dissuade clinicians from their use.
Common complications of spinal orthoses include decubitus ulcers and soft tissue infections, which are more likely in the elderly cohort. 43 Only 2 studies in this review compared complication rates between brace types with conflicting conclusions. 47 –49 What can be deduced is that braces should be implemented for a finite time period rather than indefinitely given the potential for complications. This tenet is supported by Meccariello et al 49 who intriguingly found that participants who wore the Spinomed orthosis for 10 weeks continued to demonstrate biomechanical and functional improvement at 3- and 6-month follow-up despite brace removal. The significance of this lies in the fact that this period of time should be used to commence osteoporotic antiresorptive medical therapy (at the least) or osteoblast inductive medical therapy (with contraindications excluded) to restore or accelerate bone healing and subsequently decrease overall morbidity and mortality related to OVF. 66 –68 Thus, spinal orthoses may simultaneously serve as an effective adjunct and bridging tool while systemic therapies take effect to maintain post traumatic spinal alignment.
It is also telling that alternative therapies for OVFs are still being investigated. Indeed, Barker et al 69 determined that intensive physiotherapy therapy likely only has short-term benefits compared with physiotherapy education of patients. This theme was reiterated by Caitriona et al 70 who highlighted there still exists uncertainty and a lack of evidence as to the exact role of physiotherapy and to what degree it should be incorporated into a standardized rehabilitation regime. There also exists conflicting evidence regarding the role of vertebroplasty, with the American Society for Bone and Mineral Research Task Force concluding that there is still no demonstrable clinical benefit of this intervention. 71 In a climate where such ambivalence surrounds alternative interventions, our systematic review provides urgent clarification on the biomechanical and functional benefits of the readily available adjunct of spinal orthoses in the management of elderly patients who have sustained OVFs.
This systematic review unfortunately was limited by the heterogeneity and quality of available evidence. A broad spectrum of orthoses was studied with variable direct and indirect measures of their mechanical and functional benefits or reported risks. This thereby precludes effective extraction of data and the performance of a meta-analysis. The included studies were susceptible to performance bias given the difficulty inherent in blinding participants to the intervention. We also accept that potential confounders such as concurrent physiotherapy or implementation of medical therapy are not separable from a research question like this due to them being mainstream treatment of OVF. On the other hand, the studies were undertaken in a variety of international centers with rigorous and well-defined protocols, suggesting appropriate internal and external validity.
Conclusion
Our novel systematic review provides pooled evidence for the first time that there is moderate-quality evidence to support the use of spinal orthoses in the management of acute osteoporotic vertebral compression fractures in elderly patients aged 60 years and older who are neurologically intact. Bracing of these patients results in improved biomechanical vertebral stability, reduced kyphotic deformity, enhanced postural stability, greater muscular strength, and superior functional outcomes.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iDs: Barry Ting Sheen Kweh, MBBS  https://orcid.org/0000-0001-9130-1543
https://orcid.org/0000-0001-9130-1543
Terence Tan, MBBS  https://orcid.org/0000-0003-2145-0214
https://orcid.org/0000-0003-2145-0214
Joost Rutges, MD, PhD  https://orcid.org/0000-0002-9452-415X
https://orcid.org/0000-0002-9452-415X
References
- 1. Compston J, McClung MR, Leslie WD. Osteoporosis. Lancet. 2019;393:364–376. [DOI] [PubMed] [Google Scholar]
- 2. Ballane G, Cauley JA, Luckey MM, Fuleihan GEH. Worldwide prevalence and incidence of osteoporotic vertebral fractures. Osteoporos Int. 2017;28:1531–1542. [DOI] [PubMed] [Google Scholar]
- 3. Wong CC, McGirt MJ. Vertebral compression fractures: a review of current management and multimodal therapy. J Multidiscip Healthc. 2013;6:205–214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Kim TY, Jang S, Park CM, et al. Trends of incidence, mortality, and future projection of spinal fractures in Korea using nationwide claims data. J Korean Med Sci. 2016;31:801–805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Nazrun AS, Tzar MN, Mokhtar SA, Mohamed IN. A systematic review of the outcomes of osteoporotic fracture patients after hospital discharge: morbidity, subsequent fractures, and mortality. Ther Clin Risk Manag. 2014;10:937–948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Chen YC, Lin WC. Risk of long-term infection-related death in clinical osteoporotic vertebral fractures: a hospital-based analysis. PLoS One. 2017;12:e0182614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Hasserius R, Karlsson MK, Jónsson B, Redlund-Johnell I, Johnell O. Long-term morbidity and mortality after a clinically diagnosed vertebral fracture in the elderly—a 12-and 22-year follow-up of 257 patients. Calcif Tissue Int. 2005;76:235–242. [DOI] [PubMed] [Google Scholar]
- 8. Kado DM, Browner WS, Palermo L, Nevitt MC, Genant HK, Cummings SR. Vertebral fractures and mortality in older women: a prospective study. Arch Intern Med. 1999;159:1215–1220. [DOI] [PubMed] [Google Scholar]
- 9. Black DM, Arden NK, Palermo L, Pearson J, Cummings SR. Prevalent vertebral deformities predict hip fractures and new vertebral deformities but not wrist fractures. J Bone Miner Res. 1999;14:821–828. [DOI] [PubMed] [Google Scholar]
- 10. Schousboe JT. Epidemiology of vertebral fractures. J Clin Densitom. 2016;19:8–22. [DOI] [PubMed] [Google Scholar]
- 11. Longo UG, Loppini M, Denaro L, Maffulli N, Denaro V. Conservative management of patients with an osteoporotic vertebral fracture: a review of the literature. J Bone Joint Surg Br. 2012;94:152–157. [DOI] [PubMed] [Google Scholar]
- 12. Kawchuk GN, Edgecombe TL, Wong AYL, Cojocaru A, Prasad N. A non-randomized clinical trial to assess the impact of nonrigid, inelastic corsets on spine function in low back pain participants and asymptomatic controls. Spine J. 2015;15:2222–2227. [DOI] [PubMed] [Google Scholar]
- 13. Dugarova E. Ageing, Older Persons And The 2030 Agenda For Sustainable Development. United Nations Development Programme; 2017. [Google Scholar]
- 14. Moher D, Liberati A, Tetzlaff J, Altman DG; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med. 2009;151:264–269. [DOI] [PubMed] [Google Scholar]
- 15. Higgins JP, Green S. Cochrane Handbook for Systematic Reviews of Interventions. Cochrane Collaboration/Wiley; 2011. [Google Scholar]
- 16. Sterne JAC, Savović J, Page MJ, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. 2019;366:l4898. [DOI] [PubMed] [Google Scholar]
- 17. Sterne JA, Hernán MA, Reeves BC, et al. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ. 2016;355:i4919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. McGuinness LA. Robvis: an R package and web application for visualising risk-of-bias assessments. Published 2019. Accessed September 15, 2020. https://github.com/mcguinlu/robvis [DOI] [PubMed]
- 19. Murata K, Watanabe G, Kawaguchi S, et al. Union rates and prognostic variables of osteoporotic vertebral fractures treated with a rigid external support. J Neurosurg Spine. 2012;17:469–475. [DOI] [PubMed] [Google Scholar]
- 20. Shariatzadeh H, Modaghegh BS, Mirzaei A. The effect of dynamic hyperextension brace on osteoporosis and hyperkyphosis reduction in postmenopausal osteoporotic women. Arch Bone Jt Surg. 2017;5:181–185. [PMC free article] [PubMed] [Google Scholar]
- 21. Jacobs E, Senden R, McCrum C, van Rhijn LW, Meijer K, Willems PC. Effect of a semirigid thoracolumbar orthosis on gait and sagittal alignment in patients with an osteoporotic vertebral compression fracture. Clin Interv Aging. 2019;14:671–680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Li M, Law SW, Cheng J, Kee HM, Wong MS. A comparison study on the efficacy of SpinoMedÒ and soft lumbar orthosis for osteoporotic vertebral fracture. Prosthet Orthot Int. 2015;39:270–276. [DOI] [PubMed] [Google Scholar]
- 23. Valentin GH, Pedersen LN, Maribo T. Wearing an active spinal orthosis improves back extensor strength in women with osteoporotic vertebral fractures. Prosthet Orthot Int. 2014;38:232–238. [DOI] [PubMed] [Google Scholar]
- 24. Vogt L, Hübscher M, Brettmann K, Banzer W, Fink M. Postural correction by osteoporosis orthosis (Osteo-med): a randomized, placebo-controlled trial. Prosthet Orthot Int. 2008;32:103–110. [DOI] [PubMed] [Google Scholar]
- 25. Dionyssiotis Y, Trovas G, Thoma S, Lyritis G, Papaioannou N. Prospective study of spinal orthoses in women. Prosthet Orthot Int. 2015;39:487–495. [DOI] [PubMed] [Google Scholar]
- 26. Kim HJ, Yi JM, Cho HG, et al. Comparative study of the treatment outcomes of osteoporotic compression fractures without neurologic injury using a rigid brace, a soft brace, and no brace: a prospective randomized controlled non-inferiority trial. J Bone Joint Surg Am. 2014;96:1959–1966. [DOI] [PubMed] [Google Scholar]
- 27. Talic A, Kapetanovic J, Dizdar A. Effects of conservative treatment for osteoporotic thoracolumbal spine fractures. Mater Sociomed. 2012;24:16–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Urquhart JC, Alrehaili OA, Fisher CG, et al. Treatment of thoracolumbar burst fractures: extended follow-up of a randomized clinical trial comparing orthosis versus no orthosis. J Neurosurg Spine. 2017;27:42–47. [DOI] [PubMed] [Google Scholar]
- 29. van Leeuwen PJ, Bos RP, Derksen JC, de Vries J. Assessment of spinal movement reduction by thoraco-lumbar-sacral orthoses. J Rehabil Res Dev. 2000;37:395–403. [PubMed] [Google Scholar]
- 30. Jones RF, Snowdon E, Coan J, King L, Engel S. Bracing of thoracic and lumbar spine fractures. Paraplegia. 1987;25:386–393. [DOI] [PubMed] [Google Scholar]
- 31. Alin CK, Uzunel E, Kronhed ACG, Alinaghizadeh H, Salminen H. Effect of treatment on back pain and back extensor strength with a spinal orthosis in older women with osteoporosis: a randomized controlled trial. Arch Osteoporos. 2019;14:5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Stadhouder A, Buskens E, Vergroesen DA, Fidler MW, de Nies F, Oner FC. Nonoperative treatment of thoracic and lumbar spine fractures: a prospective randomized study of different treatment options. J Orthop Trauma. 2009;23:588–594. [DOI] [PubMed] [Google Scholar]
- 33. Chiba K, Yoshida M, Shinomiya K, Satomi K, Nagata K. Conservative managements for osteoporotic thoracolumbar vertebral compression fractures—a multi-centre prospective RCT. Spine Journal Meeting Abstracts. October 2011. P63. [Google Scholar]
- 34. Ameis A, Randhawa K, Yu H, et al. The Global Spine Care Initiative: a review of reviews and recommendations for the non-invasive management of acute osteoporotic vertebral compression fracture pain in low- and middle-income communities. Eur Spine J. 2018;27(suppl 6):861–869. [DOI] [PubMed] [Google Scholar]
- 35. Muratore M, Ferrera A, Masse A, Bistolfi A. Osteoporotic vertebral fractures: predictive factors for conservative treatment failure. A systematic review. Eur Spine J. 2018;27:2565–2576. [DOI] [PubMed] [Google Scholar]
- 36. Rajasekaran S, Kanna RM, Schnake KJ, et al. Osteoporotic thoracolumbar fractures—how are they different? Classification and treatment algorithm. J Orthop Trauma. 2017;31(suppl 4):S49–S56. [DOI] [PubMed] [Google Scholar]
- 37. Goodwin VA, Hall AJ, Rogers E, Bethel A. Orthotics and taping in the management of vertebral fractures in people with osteoporosis: a systematic review. BMJ Open. 2016;6:e010657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Jin YZ, Lee JH. Effect of brace to osteoporotic vertebral fracture: a meta-analysis. J Korean Med Sci. 2016;31:1641–1649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. McCarthy J, Davis A. Diagnosis and management of vertebral compression fractures. Am Fam Physician. 2016;94:44–50. [PubMed] [Google Scholar]
- 40. Newman M, Lowe CM, Barker K. Spinal orthoses for vertebral osteoporosis and osteoporotic vertebral fracture: a systematic review. Arch Phys Med Rehabil. 2016;97:1013–1025. [DOI] [PubMed] [Google Scholar]
- 41. Karimi M. The effects of orthosis on thoracolumbar fracture healing: a review of the literature. J Orthop. 2015;12(suppl 2):S230–S237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Rzewuska M, Ferreira M, McLachlan AJ, Machado GC, Maher CG. The efficacy of conservative treatment of osteoporotic compression fractures on acute pain relief: a systematic review with meta-analysis. Eur Spine J. 2015;24:702–714. [DOI] [PubMed] [Google Scholar]
- 43. Chang V, Holly LT. Bracing for thoracolumbar fractures. Neurosurg Focus. 2014;37:E3. [DOI] [PubMed] [Google Scholar]
- 44. Longo UG, Loppini M, Denaro L, Maffulli N, Denaro V. Osteoporotic vertebral fractures: current concepts of conservative care. Br Med Bull. 2012;102:171–189. [DOI] [PubMed] [Google Scholar]
- 45. Lin JT, Lane JM. Nonpharmacologic management of osteoporosis to minimize fracture risk. Nat Clin Pract Rheumatol. 2008;4:20–25. [DOI] [PubMed] [Google Scholar]
- 46. Bonaiuti D, Arioli G, Diana G, et al. SIMFER rehabilitation treatment guidelines in postmenopausal and senile osteoporosis. Eur Medicophys. 2005;41:315–337. [PubMed] [Google Scholar]
- 47. Kato T, Inose H, Ichimurs S, et al. Comparison of rigid and soft-brace treatments for acute osteoporotic vertebral compression fracture: a prospective, randomized, multicenter study. J Clin Med. 2019;8:198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Abe T, Shibao Y, Takeuchi Y, et al. Initial hospitalization with rigorous bed rest followed by bracing and rehabilitation as an option of conservative treatment for osteoporotic vertebral fractures in elderly patients: a pilot one arm safety and feasibility study. Arch Osteoporos. 2018;13:134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Meccariello L, Muzii VF, Falzarano G, et al. Dynamic corset versus three-point brace in the treatment of osteoporotic compression fractures of the thoracic and lumbar spine: a prospective, comparative study. Aging Clin Exp Res. 2017;29:443–449. [DOI] [PubMed] [Google Scholar]
- 50. Hoshino M, Tsujio T, Terai H, et al. Impact of initial conservative treatment interventions on the outcomes of patients with osteoporotic vertebral fractures. Spine (Phila Pa 1976). 2013;38:E641–E648. [DOI] [PubMed] [Google Scholar]
- 51. Pfeifer M, Kohlwey L, Begerow L, Minne HW. Effects of two newly developed spinal orthoses on trunk muscle strength, posture, and quality-of-life in women with postmenopausal osteoporosis: a randomized trial. Am J Phys Med Rehabil. 2011;90:805–815. [DOI] [PubMed] [Google Scholar]
- 52. Liaw MY, Chen CL, Chen JF, Tang FT, Wong AMK, Ho HH. Effects of Knight-Taylor brace on balance performance in osteoporotic patients with vertebral compression fracture. J Back Musculoskelet Rehabil. 2009;22:75–81. [DOI] [PubMed] [Google Scholar]
- 53. Pfeifer M, Begerow B, Minne HW. Effects of a new spinal orthosis on posture, trunk strength, and quality of life in women with postmenopausal osteoporosis: a randomized trial. Am J Phys Med Rehabil. 2004;83:177–186. [DOI] [PubMed] [Google Scholar]
- 54. van Poppel MN, de Looze MP, Koes BW, Smid T, Bouter LM. Mechanisms of action of lumbar supports: a systematic review. Spine (Phila Pa 1976). 2000;25:2103–2113. [DOI] [PubMed] [Google Scholar]
- 55. Schnake KJ, Blattert TR, Hahn P, et al. Classification of osteoporotic thoracolumbar spine fractures: recommendations of the Spine Section of the German Society for Orthopaedics and Trauma (DGOU). Global Spine J. 2018;8(2 suppl):46S–49S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Blattert TR, Schnake KJ, Gonschorek O, et al. Nonsurgical and surgical management of osteoporotic vertebral body fractures: recommendations of the spine section of the German Society for Orthopaedics and Trauma (DGOU). Global Spine J. 2018;8(2 suppl):50S–55S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Gao Y, Arfat Y, Wang H, Goswami N. Muscle atrophy induced by mechanical unloading: mechanisms and potential countermeasures. Front Physiol. 2018;9:235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Brooks NE, Myburgh KH. Skeletal muscle wasting with disuse atrophy is multi-dimensional: the response and interaction of myonuclei, satellite cells and signaling pathways. Front Physiol. 2014;5:99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Fayolle-Minon I, Calmels P. Effect of wearing a lumbar orthosis on trunk muscles: study of the muscle strength after 21 days of use on healthy subjects. Joint Bone Spine. 2008;75:58–63. [DOI] [PubMed] [Google Scholar]
- 60. Seene T, Kaasik P. Muscle weakness in the elderly: role of sarcopenia, dynapenia, and possibilities for rehabilitation. Eur Rev Aging Phys Act. 2012;9:109–117. [Google Scholar]
- 61. Cholewicki J, McGill KC, Shah KR, Lee AS. The effects of a three-week use of lumbosacral orthoses on trunk muscle activity and on the muscular response to trunk perturbations. BMC Musculoskelet Disord. 2010;11:154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Kawaguchi Y, Gejo R, Kanamori M, Kimura T. Quantitative analysis of the effect of lumbar orthosis on trunk muscle strength and muscle activity in normal subjects. J Orthop Sci. 2002;7:483–489. [DOI] [PubMed] [Google Scholar]
- 63. Azadinia F, Takamjani EE, Kamyab M, Parnianpour M, Cholewicki J, Maroufi N. Can lumbosacral orthoses cause trunk muscle weakness? A systematic review of literature. Spine J. 2017;17:589–602. [DOI] [PubMed] [Google Scholar]
- 64. Rostami M, Noormohammadpour P, Sadeghian AH, Mansournia MA, Kordi R. The effect of lumbar support on the ultrasound measurements of trunk muscles: a single-blinded randomized controlled trial. PM R. 2014;6:302–308. [DOI] [PubMed] [Google Scholar]
- 65. Knopp-Sihota JA, Newburn-Cook CV, Homik J, Cummings GG, Voaklander D. Calcitonin for treating acute and chronic pain of recent and remote osteoporotic vertebral compression fractures: a systematic review and meta-analysis. Osteoporos Int. 2012;23:17–38. [DOI] [PubMed] [Google Scholar]
- 66. Sattui SE, Saag KG. Fracture mortality: associations with epidemiology and osteoporosis treatment. Nat Rev Endocrinol. 2014;10:592–602. [DOI] [PubMed] [Google Scholar]
- 67. Genev IK, Tobin MK, Zaidi SP, Khan SR, Amirouche FML, Mehta AI. Spinal compression fracture management: a review of current treatment strategies and possible future avenues. Global Spine J. 2017;7:71–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Shigenobu K, Hashimoto T, Kanayama M, Ohha H, Yamane S. The efficacy of osteoporotic treatment in patients with new spinal vertebral compression fracture pain, ADL, QOL, bone metabolism and fracture-healing—in comparison with weekly teriparatide with bisphosphonate. Bone Rep. 2019;11:100217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Barker K, Newman M, Stallard N, et al. Physiotherapy rehabilitation for osteoporotic vertebral fracture—a randomised controlled trial and economic evaluation (PROVE trial). Osteoporos Int. 2020;31:277–289. [DOI] [PubMed] [Google Scholar]
- 70. Caitriona C, Mark MG, Elaine H, et al. Management of hospitalised osteoporotic vertebral fractures. Arch Osteoporos. 2020;15:14. [DOI] [PubMed] [Google Scholar]
- 71. Ebeling PR, Akesson K, Bauer DC, et al. The efficacy and safety of vertebral augmentation: a second ASBMR Task Force Report. J Bone Miner Res. 2019;34:3–21. [DOI] [PubMed] [Google Scholar]