Abstract
Study Design:
Age- and sex-matched cohort study.
Objectives:
To compare outcomes after open versus minimally invasive transforaminal lumbar interbody fusion (MIS-TLIF) with bilateral facetectomies.
Methods:
We retrospectively compared patients who underwent single- or 2-level MIS-TLIF with an age- and sex-matched open-TLIF cohort. Surgical data was collected for operative time, estimated blood loss (EBL), and drain use. Clinical outcomes included the Visual Analog Scale (VAS), Oswestry Disability Index (ODI), length of stay (LOS), complications, and reoperations. Lumbar radiographs were measured for changes in global lumbar lordosis (LL) and segmental lordosis (SL).
Results:
Between 2016 and 2020, 38 MIS-TLIF patients were compared with 38 open-TLIF patients. No subfascial drain was used in the MIS-TLIF group (P < .001). The MIS-TLIF group had longer operative time (310.8 vs 276.5 minutes; P = .046) but less EBL (282.4 vs 420.8 mL; P = .007). LOS (P = .15), complication rates (P = .50), and revision rates (P = .17) were equivalent. VAS and ODI improved but did not differ between groups. In the open-TLIF group, LL and SL were restored or improved in 81.6% and 86.9% of cases, respectively. In the MIS-TLIF group, LL and SL were restored or improved in 86.8% and 97.4% of cases, respectively. There were no differences in changes in LL and SL between groups.
Conclusions:
Compared with the age- and sex-matched open-TLIF cohort, patients undergoing MIS-TLIF had reduced EBL and subfascial drain use but increased operative time. There were no differences in complications, reoperations, or LOS. Both groups demonstrated improvement in VAS and ODI. MIS-TLIF with bilateral facetectomies provided equivalent improvements in global and segmental LL.
Keywords: spinal fusion, lordosis, minimally invasive surgery, lumbar interbody fusion, spondylosis, spondylolisthesis
Introduction
Transforaminal lumbar interbody fusion (TLIF) was first introduced by Harms and Rolinger in 1982 as a modification of the posterior lumbar interbody fusion (PLIF) technique. 1 Because the corridor to the disc space is more lateral, less dural retraction is required. Therefore, TLIF offers the theoretical advantage of fewer nerve root injuries in comparison to PLIF. 2 Today, TLIF is often utilized in conjunction with posterolateral lumbar instrumented fusion procedures to facilitate arthrodesis. The addition of TLIF has been shown to increase the rates of radiographic fusion compared with posterolateral fusion alone. 3 TLIF can be performed via an open or minimally invasive surgery (MIS) approach. The proposed advantages of MIS TLIF include less estimated blood loss (EBL), less postoperative pain, and shorter length of stay (LOS). 4,5 However, as with any minimally invasive spine procedure, MIS TLIF has a steep learning curve 6 and its own unique sets of challenges and complications. 5
One of the technical challenges of both open and MIS TLIF is optimal placement of the interbody cage to preserve or improve postoperative lumbar lordosis (LL). In a retrospective study by Madhavan et al, 7 the authors reported that 57% of patients with normal preoperative LL developed postoperative kyphosis. Other studies have also documented kyphogenic effects of MIS TLIF. 8 -11 Lee et al 8 reported an initial increase in the segmental lordotic angle after MIS TLIF, but this angle decreased significantly with time when compared with the preoperative segmental lordosis (SL). Vaishnav et al 11 observed a decrease in segmental and regional lordosis after MIS TLIF with the use of static interbody cages in patients with high preoperative LL.
The aforementioned studies by Lee et al 8 and Vaishnav et al 11 involved MIS TLIF cases in which only unilateral facetectomy was performed (ie, unilateral MIS TLIF). 8,11 In our experience, we always take down both facets (bilateral MIS TLIF) in order to compress across the fused segments after insertion of the interbody device. The present study evaluates the radiographic and clinical outcomes after bilateral MIS TLIF in comparison to an age- and sex-matched cohort of patients undergoing open TLIF with bilateral facetectomies. We hypothesize equivalent improvements in global and segmental LL after MIS TLIF compared to open TLIF with bilateral facetectomies.
Materials and Methods
This study was approved by our institutional review board. It was a retrospective cohort study comparing patients undergoing single- or 2-level TLIF with bilateral facetectomies via open versus MIS approaches at a single academic center. The 2 cohorts were matched by sex and age. Inclusion criteria were adult patients >18 years old who had 1- or 2-level TLIF. Patients were excluded if they had prior lumbar fusion surgeries or if they had 3 or more levels of interbody fusion.
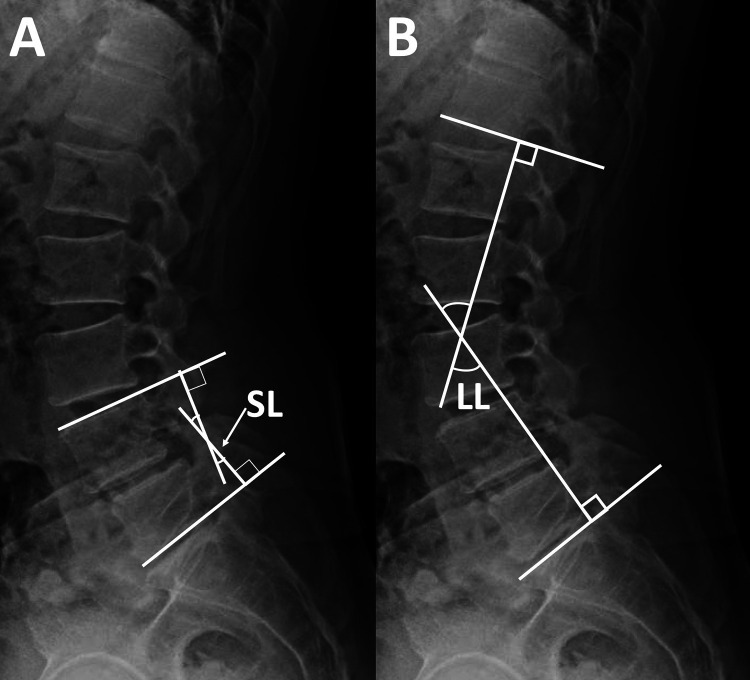
The electronic medical records were reviewed to obtain basic demographic, clinical, and operative data. Standing neutral lumbar radiographs preoperatively and at final follow-up were reviewed for the following radiographic parameters: global LL and SL (Figure 1). LL was defined as the angle subtended by the inferior endplate line of T12 and the superior endplate line of S1. SL was defined as the angle subtended by the superior endplate line of the upper instrumented vertebra and the inferior endplate line of the lower instrumented vertebra. Taking the SEM previously reported for the Cobb method into consideration, 12 only a change in LL or SL of ≥3° was considered significant. Clinical outcomes were assessed via the Visual Analog Scale (VAS) pain score and Oswestry Disability Index (ODI). The t-test and χ2 test were used to compare continuous and categorical variables, respectively. A probability of type I error <0.05 was utilized to assess statistical significance.
Figure 1.
Overview of the radiographic parameters of interest. This is an example for L4-5 transforaminal lumbar interbody fusion: A. Segmental lordosis (SL) is defined as the angle subtended by the superior endplate line of the upper instrumented vertebra and the inferior endplate line of the lower instrumented vertebra. B. Global lumbar lordosis (LL) is defined as the angle subtended by the inferior endplate line of T12 and the superior endplate line of S1.
Bilateral MIS TLIF Technique
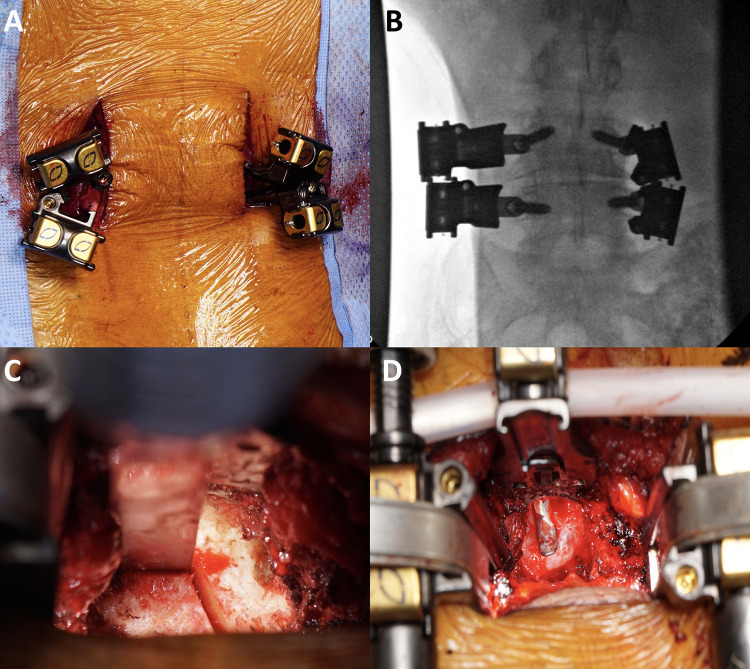
Bilateral mini-open paramedian incisions were utilized in patients undergoing MIS TLIF, consistent with the Wiltse approach (Figure 2). Pedicle screws were placed with the assistance of an O-arm and surgical navigation. A screw shank/blade assembly was inserted at each level, and the blades were then attached to a retractor body. Light cables were subsequently placed into the retractor blades to improve visualization. With the retractor system assembled, bilateral complete facetectomies were performed, removing the entire superior articular process to clearly expose the disc space for the discectomy and interbody fusion. The pars was kept intact to protect the exiting nerve root. Adequate lateral recess decompression was ensured by visualizing the traversing nerve root on each side. In addition, we ensured adequate central decompression by removing the entire ligamentum flavum and undersurface of the lamina to allow for passage of a curved freer across the midline. Discectomy and interbody fusion were then performed from the most symptomatic side. Finally, rods were placed and compressed to restore lordosis. Of note, bilateral facetectomies were also performed for the open TLIF. The goal of the facetectomies in both groups was to access the disc space for interbody fusion and to facilitate restoration of LL with compression after the interbody fusion procedure was completed.
Figure 2.
Intraoperative images of minimally invasive transforaminal lumbar interbody fusion: A. Bilateral mini-open paramedian incisions are made. Pedicle screws are placed under image guidance. A screw shank/blade assembly is inserted at each level. B. Intraoperative posteroanterior fluoroscopic X-ray demonstrating the screw shank/blade assembly. C. Complete facetectomy is performed on each side using an osteotome and Kerrison rongeur. D. Central decompression is achieved by removing the ligamentum flavum and undersurface of the lamina to allow for passage of a curved freer across the midline.
Results
A total of 38 consecutive patients who underwent MIS TLIF between 2016 and 2020 (25 single level, 13 two level) were compared with a matched cohort of 38 patients who underwent open TLIF (25 single level, 13 two level). The mean age (62.1 vs 61.4 years; P = .75) and gender distributions (23 female and 15 male patients) were expectedly similar between the 2 cohorts. The BMIs were also comparable (32.3 vs 32.2 kg/m2; P = .95). The mean follow-up periods for the MIS and open cohorts were 350 and 393 days, respectively (P = .55). In each cohort, the surgical diagnosis was lumbar spondylosis alone (n = 16, 42.1%) or lumbar spondylosis with degenerative spondylolisthesis (n = 22, 57.9%; Table 1). Both groups had the same distribution of primary (n = 35, 92.1%) and revision (n = 3, 7.9%) lumbar spine surgeries.
Table 1.
Demographic Comparison Between the 2 Groups.
| Characteristic | Open TLIF | MIS TLIF | Significance |
|---|---|---|---|
| Cases | 38 | 38 | |
| Age | 61.4 | 62.1 | P = .75 |
| Sex | 23 F:15 M | 23 F:15 M | |
| BMI | 32.2 | 32.3 | P = .95 |
| Diagnosis | Spondylosis alone: 16 With spondylolisthesis: 22 |
Spondylosis alone: 16 With spondylolisthesis: 22 |
|
| Case type | Primary: 35 Revision: 3 |
Primary: 35 Revision: 3 |
|
| Length of stay | 3.6 | 3.1 | P = .15 |
| Follow-up | 392.7 | 350.7 | P = .55 |
| Change in VAS | 3.2 | 3.5 | P = .68 |
| Change in ODI | 9.3 | 7.0 | P = .47 |
| Complication | 6 | 4 | P = .50 |
| Reoperation | 4 | 1 | P = .17 |
Abbreviations: BMI, body mass index; F, female; M, male; MIS, minimally invasive surgery; ODI, Oswestry Disability Index; TLIF, transforaminal lumbar interbody fusion; VAS, Visual Analog Scale.
No suprafascial or subfascial drain was used in the MIS group, compared with 97.4% (37 of 38 cases) in the open group (P < .001). The operative time was shorter in the open group (276.5 vs 310.8 minutes; P = .046), whereas the EBL was less in the MIS group (282.4 vs 420.8 mL; P = .007). However, there was an equal rate of intraoperative transfusion of packed red blood cells (pRBCs; 3 cases per group, 7.9%). The early surgical complication rates for the MIS and open cohorts were 10.5% versus 15.8% (P = .50). The revision rates for the MIS and open cohorts were 2.6% versus 10.5% (P = .17; Table 2).
Table 2.
Operative Comparison Between the 2 Groups.
| Characteristic | Open TLIF | MIS TLIF | Significance |
|---|---|---|---|
| Cases | 38 | 38 | |
| Single level | 25 | 25 | |
| Two level | 13 | 13 | |
| Drain | 37 | 0 | P < .001 |
| Estimated blood loss | 420.8 | 282.4 | P = .007 |
| Intraoperative transfusion | 3 | 3 | |
| Operative time | 276.5 | 310.8 | P = .046 |
Abbreviations: MIS, minimally invasive surgery; TLIF, transforaminal lumbar interbody fusion.
Clinically, there were statistically significant improvements in VAS in the MIS (6.1 to 2.5; P < .001) and open (5.9 to 2.7; P < .001) cohorts. However, VAS improvement did not differ between groups (3.5 vs 3.2; P = .68). Likewise, there were statistically significant improvements in ODI in the MIS (23.0 to 14.8; P = .004) and open (25.2 to 17.1; P < .001) cohorts that did not differ between groups (7.0 vs 9.25, P = .47; Table 1). The LOS was also similar (3.6 vs 3.1 days; P = .15). However, 23.7% of MIS patients were discharged on postoperative day 1, compared with 2.6% in the open cohort.
The changes in LL and SL are summarized in Table 3. Radiographically, in the open group, the LL was restored or improved in 81.6% of the cases and SL in 86.9% of the cases. Likewise, in the MIS group, the LL and SL were restored or improved in 86.8% and 97.4% of the cases, respectively (Table 4). There were no differences in the changes in LL and SL between groups. Subgroup analysis did not demonstrate any statistically significant differences in the change in LL and SL for diagnosis (spondylosis alone vs spondylosis with spondylolisthesis) or TLIF level (single- vs 2-level; Table 5).
Table 3.
Radiographic Comparison Between the 2 Groups.
| Parameter | Open TLIF | MIS TLIF | Significance |
|---|---|---|---|
| Preoperative LL | 50.9 ± 11.9 | 53.8 ± 10.7 | P = .26 |
| Postoperative LL | 54.2 ± 11.9 | 58.2 ± 10.5 | P = .13 |
| Change in LL | 3.4 ± 6.0 | 4.4 ± 5.8 | P = .47 |
| Preoperative SL | 24.1 ± 7.5 | 21.4 ± 8.6 | P = .14 |
| Postoperative SL | 27.1 ± 6.8 | 25.3 ± 8.9 | P = .32 |
| Change in SL | 3.0 ± 6.2 | 3.9 ± 3.9 | P = .46 |
Abbreviations: MIS, minimally invasive surgery; LL, global lumbar lordosis; SL, segmental lordosis; TLIF, transforaminal lumbar interbody fusion.
Table 4.
Changes in Global LL and SL With Surgery.a
| Parameter | Open TLIF | MIS TLIF |
|---|---|---|
| Lumbar lordosis (LL) | ||
| Increased | 23 (60.5%) | 23 (60.5%) |
| Unchanged | 8 (21.1%) | 10 (26.3%) |
| Decreased | 7 (18.4%) | 5 (13.2%) |
| Segmental lordosis (SL) | ||
| Increased | 21 (55.3%) | 25 (65.8%) |
| Unchanged | 12 (31.6%) | 12 (31.6%) |
| Decreased | 5 (13.2%) | 1 (2.6%) |
Abbreviations: MIS, minimally invasive surgery; TLIF, transforaminal lumbar interbody fusion.
a After surgery, an increase or decrease in LL or SL is defined as a change in measurement of ≥3° or ≤3° from preoperative, respectively.
Table 5.
Comparison in the Change in Global LL and SL by Diagnosis (Spondylosis Alone vs Spondylosis With Spondylolisthesis) and TLIF Levels (Single- vs 2-Level).
| Parameter | Open TLIF | MIS TLIF | Significance |
|---|---|---|---|
| Spondylosis | n = 16 | n = 16 | |
| Change in LL | 2.0 ± 6.3 | 1.9 ± 5.3 | P = .98 |
| Change in SL | 1.0 ± 6.1 | 2.8 ± 3.7 | P = .32 |
| Spondylolisthesis | n = 22 | n = 22 | |
| Change in LL | 4.4 ± 5.9 | 6.1 ± 5.7 | P = .32 |
| Change in SL | 4.5 ± 6.1 | 4.7 ± 4.0 | P = .89 |
| Single level | n = 25 | n = 25 | |
| Change in LL | 3.1 ± 6.0 | 3.7 ± 6.0 | P = .73 |
| Change in SL | 2.2 ± 6.5 | 3.2 ± 3.5 | P = .50 |
| Two level | n = 13 | n = 13 | |
| Change in LL | 3.9 ± 6.4 | 5.7 ± 5.5 | P = .46 |
| Change in SL | 4.5 ± 5.7 | 5.2 ± 4.6 | P = .74 |
Abbreviations: LL, lumbar lordosis; MIS, minimally invasive surgery; SL, segmental lordosis; TLIF, transforaminal lumbar interbody fusion.
Discussion
The results from this study highlight several key differences between MIS and open TLIF. Consistent with previously published studies, one of the main advantages of MIS TLIF is the decrease in blood loss. 4,5,13 The MIS group in our study had significantly less blood loss compared with the open cohort. However, the intraoperative transfusion rates were similar between groups. At our institution, we administer systemic tranexamic acid prior to making an incision for both MIS and open TLIF procedures and have noticed a decrease in the need for intraoperative pRBC transfusions. In addition, we routinely use cell saver for autotransfusion to avoid allogeneic blood transfusions. 14 Because of the decrease in blood loss, no suprafascial or subfascial drain was used in the MIS cohort. A prospective randomized clinical study by Hung et al 15 demonstrated no significant differences in perioperative outcomes (eg, operative time, EBL, LOS, and complications) in MIS TLIF cases with and without closed suction wound drainage. In fact, on average, patients without drains ambulated a day earlier than patients with drains after MIS TLIF. 15 Interestingly, the operative time in the MIS group was significantly higher than the open group. In the literature, there are published studies in support of MIS TLIF 4 or open TLIF 16 in terms of surgical duration. In our experience, MIS TLIF takes longer because we are performing bilateral facetectomies rather than unilateral facetectomies. Furthermore, our study included the first 38 consecutive MIS TLIF patients operated on by 1 provider, and 1 study suggests that it takes roughly that many number of cases to improve operative time and proficiency. 17 Although not directly addressed in this study, MIS TLIF certainly increases the ionizing radiation exposure for both surgeons and patients. 18 Therefore, this should be carefully discussed when counseling patients regarding the risks and benefits between open versus MIS TLIF.
In the age- and sex-matched MIS and open cohorts, the early surgical complication rates and revision rates were comparable. However, the types of complications were notably different. Specifically, there were more incidental durotomies in the MIS group (3 of 4 complications, 75%), whereas there were more deep wound infections and seromas in the open group (5 of 6 complications, 83.3%). Specifically, in the open cohort, 3 patients had surgical site infection, and 2 patients developed symptomatic seroma; all these patients had subfascial drains during their index surgery and required formal irrigation and debridement to treat their complication. There was 1 MIS TLIF patient without a subfascial drain who developed a large seroma causing lumbar radiculopathy requiring irrigation and debridement. We believe that the use of a subfascial drain should be considered on a case-by-case basis, irrespective of whether the TLIF procedure is performed open or MIS.
Previously published studies have shown that MIS TLIF is associated with lower complication rates than open surgery; however, the difference is not statistically significant. 5,16 Studies comparing open versus MIS lumbar discectomy have reported higher rates of durotomy and lower rates of wound infection. 19 A systematic review by Parker et al 20 concluded that there was a significant decrease in the incidence of surgical site infection after MIS compared with open TLIF. Thus, MIS TLIF may be a better option in patients with high risks for perioperative wound complications, such as obese patients. 21 In our study, there was 1 reoperation in the MIS cohort for adjacent segment disease (ASD), compared with 4 reoperations in the open cohort for ASD (1 case) and pseudarthrosis (3 cases). MIS techniques have also been shown to decrease the incidence of ASD following lumbar spine surgeries compared with open approaches because of less soft-tissue disruption, 22 although this conclusion was not observed in our study. During MIS TLIF, when pedicle screws are placed percutaneously, careful attention needs to be paid to avoid iatrogenic superior facet joint violation, which is a known risk factor for ASD. 23 Whereas revision for pseudarthrosis was only seen in the open cohort in our study, pseudarthrosis is also a potential long-term complication of MIS TLIF. 17,24
In our study, there were statistically significant improvements in VAS and ODI after MIS and open TLIF. However, the changes in VAS and ODI were comparable between groups, suggesting equivalent outcomes between MIS and open TLIF procedures. This finding of comparable clinical outcomes has been published in multiple studies. 4,5 Interestingly, although the change in VAS did not differ between groups, Cheng et al 4 showed that the total administration of morphine-equivalent pain medication in the hospital tended to be lower in the MIS group. Another interesting finding in our study is the equivalent LOS between the 2 groups, although more MIS patients were discharged on postoperative day 1. However, the majority of publications have favored a lower LOS after MIS TLIF when compared with open procedures. 4,5 Eckman et al 25 published a same-day discharge rate of 73% (808 of 1114 patients) after single- or 2-level MIS TLIF. Siemionow et al 26 identified several predictors of LOS greater than 24 hours after MIS TLIF, including higher VAS, higher total fluids at the end of the case, lower preoperative hemoglobin, and lower mean percentage of fraction of inspired oxygen. 26 Thus, optimization of certain modifiable factors could potentially optimize time to discharge. Other noted benefits of MIS TLIF are earlier mobilization, quicker return to work, and reduced costs. 4,27 -30
As previously discussed, TLIF can potentially be kyphogenic, with one study concluding that 57% of patients with normal LL preoperatively developed kyphosis postoperatively. 7 Dorward et al 31 observed that patients who had TLIF performed in the L3-S1 region actually lost lordosis postoperatively. This is a problem also observed in MIS TLIF, 8 -11 leading some to believe “TLIF is kyphosing.” 32 However, open TLIF with bilateral facetectomies, when done appropriately, is a common way of restoring LL and sagittal balance. 33,34 We have applied this to our MIS TLIF technique and perform bilateral facetectomies in all MIS TLIF cases. In our study, we found that MIS TLIF with bilateral facetectomies preserved or improved LL in 86.8% of cases and SL in 97.4% of cases, similar in comparison to open TLIF with bilateral facetectomies (Figure 3). Thus, one strategy during open or MIS TLIF to restore LL and SL is to perform bilateral facetectomies. This, in our experience, allows for greater compression across the instrumented vertebrae to create a more favorable LL postoperatively. Although this study demonstrates the similarities and differences between MIS and open TLIF, it does not directly compare MIS TLIF with unilateral versus bilateral facetectomies. In fact, other factors may influence the change in lordosis after TLIF, including the type of cage used 11 and where the cage is placed. 35 Future studies should focus on directly comparing unilateral versus bilateral MIS TLIF to determine the significance of bilateral facetectomies on clinical and radiographic outcomes. Another limitation of this study is that although we matched for sex and age, there could be other potential confounding factors that might be unevenly distributed between the 2 groups being compared.
Figure 3.
Standing neutral lumbar radiographs of patients who underwent open and minimally invasive transforaminal lumbar interbody fusion (MIS TLIF) demonstrating improvement in global and segmental lordosis postoperatively. Preoperative (A) and postoperative (B) lateral radiographs of a patient who had L4-5 open TLIF. Preoperative (C) and postoperative (D) lateral radiographs of a patient who had L3-5 MIS TLIF.
In summary, in comparison to an age- and sex-matched open TLIF cohort, patients undergoing single- or 2-level MIS TLIF had significantly reduced EBL and subfascial drain use but increased operative times. There were no significant differences in transfusion rates, surgical complication rates, revision rates, or LOS. Both groups demonstrated significant improvements in VAS and ODI; however, the changes in VAS and ODI were comparable between groups. Finally, MIS TLIF with bilateral facetectomies provided equivalent improvements in global and segmental LL when compared with open TLIF with bilateral facetectomies.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iDs: Hai Le, MD  https://orcid.org/0000-0002-9111-9060
https://orcid.org/0000-0002-9111-9060
Ryan Anderson, MD  https://orcid.org/0000-0003-4892-0255
https://orcid.org/0000-0003-4892-0255
Eileen Phan, BA  https://orcid.org/0000-0002-3770-2626
https://orcid.org/0000-0002-3770-2626
Joseph Wick, MD  https://orcid.org/0000-0002-0030-0367
https://orcid.org/0000-0002-0030-0367
References
- 1. Harms J, Rolinger H. A one-stager procedure in operative treatment of spondylolistheses: dorsal traction-reposition and anterior fusion. Article in German. Z Orthop Ihre Grenzgeb. 1982;120:343–347. [DOI] [PubMed] [Google Scholar]
- 2. Gum JL, Reddy D, Glassman S. Transforaminal lumbar interbody fusion (TLIF). JBJS Essent Surg Tech. 2016;6:e22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Levin JM, Tanenbaum JE, Steinmetz MP, Morz TE, Overley SC. Posterolateral fusion (PLF) versus transforaminal lumbar interbody fusion (TLIF) for spondylolisthesis: a systematic review and meta-analysis. Spine J. 2018;18:1088–1098. [DOI] [PubMed] [Google Scholar]
- 4. Cheng JS, Park P, Le H, Reisner L, Chou D, Mummaneni PV. Short-term and long-term outcomes of minimally invasive and open transforaminal lumbar interbody fusions: is there a difference? Neurosurg Focus. 2013;35:E6. [DOI] [PubMed] [Google Scholar]
- 5. Hammad A, Wirries A, Ardeshiri A, Nikiforov O, Geiger F. Open versus minimally invasive TLIF: literature review and meta-analysis. J Orthop Surg Res. 2019;14:229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Lee KH, Yeo W, Soeharno H, Yue WM. Learning curve of a complex surgical technique: minimally invasive transforaminal lumbar interbody fusion (MIS TLIF). J Spinal Disord Tech. 2014;27:E234–E240. [DOI] [PubMed] [Google Scholar]
- 7. Madhavan K, Shamrock AG, Chieng LO, et al. Assessment of sagittal balance post TLIF—are we kyphosing the lumbar spine? Paper presented at: 2017 AANS/CNS Joint Section on Disorders of the Spine and Peripheral Nerves; March 8-11, 2017; Las Vegas, NV. [Google Scholar]
- 8. Lee HJ, Kim JS, Ryu KS. Minimally invasive TLIF using unilateral approach and single cage at single level in patients over 65. Biomed Res Int. 2016;2016:4679865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Shen X, Wang L, Zhang H, Gu X, Gu G, He S. Radiographic analysis of one-level minimally invasive transforaminal lumbar interbody fusion (MI-TLIF) with unilateral pedicle screw fixation for lumbar degenerative diseases. Clin Spine Surg. 2016;29:E1–E8. [DOI] [PubMed] [Google Scholar]
- 10. Uribe JS, Myhre SL, Youssef JA. Preservation or restoration of segmental and regional spinal lordosis using minimally invasive interbody fusion techniques in degenerative lumbar conditions: a literature review. Spine (Phila Pa 1976). 2016;41(suppl 8):S50–S58. [DOI] [PubMed] [Google Scholar]
- 11. Vaishnav AS, Saville P, McAnany S, et al. Retrospective review of immediate restoration of lordosis in single-level minimally invasive transforaminal lumbar interbody fusion: a comparison of static and expandable interbody cages. Oper Neurosurg (Hagerstown). 2020;18:518–523. [DOI] [PubMed] [Google Scholar]
- 12. Hwang JH, Modi HN, Suh SW, et al. Reliability of lumbar lordosis measurement in patients with spondylolisthesis: a case-control study comparing the Cobb, centroid, and posterior tangent methods. Spine (Phila Pa 1976). 2010;35:1691–1700. [DOI] [PubMed] [Google Scholar]
- 13. Patel AA, Zfass-Mendez M, Lebwohl NH, et al. Minimally invasive versus open lumbar fusion: a comparison of blood loss, surgical complications, and hospital course. Iowa Orthop J. 2015;35:130–134. [PMC free article] [PubMed] [Google Scholar]
- 14. Djurasovic M, McGraw KE, Bratcher K, et al. Randomized trial of cell saver in 2- to 3-level lumbar instrumented posterior fusions. J Neurosurg Spine. 2018;29:582–587. [DOI] [PubMed] [Google Scholar]
- 15. Hung PI, Chang MC, Chou PH, Lin HH, Wang ST, Liu CL. Is a drain tube necessary for minimally invasive lumbar spine fusion surgery? Eur Spine J. 2017;26:733–737. [DOI] [PubMed] [Google Scholar]
- 16. Hey HW, Hee HT. Open and minimally invasive transforaminal lumbar interbody fusion: comparison of intermediate results and complications. Asian Spine J. 2015;9:185–193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Nandyala SV, Fineberg SJ, Pelton M, et al. Minimally invasive transforaminal lumbar interbody fusion: one surgeon’s learning curve. Spine J. 2014;14:1460–1465. [DOI] [PubMed] [Google Scholar]
- 18. Kim CH, Lee CH, Kim KP. How high are radiation-related risks in minimally invasive transforaminal lumbar interbody fusion compared with traditional open surgery? a meta-analysis and dose estimates of ionizing radiation. Clin Spine Surg. 2016;29:52-59. [DOI] [PubMed] [Google Scholar]
- 19. Evaniew N, Khan M, Drew B, Kwok D, Bhandari M, Ghert M. Minimally invasive versus open surgery for cervical and lumbar discectomy: a systematic review and meta-analysis. CMAJ Open. 2014;2:E295–E305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Parker SL, Adogwa O, Witham TF, Aaronson OS, Cheng J, McGirt MJ. Post-operative infection after minimally invasive versus open transforaminal lumbar interbody fusion (TLIF): literature review and cost analysis. Minim Invasive Neurosurg. 2011;54:33–37. [DOI] [PubMed] [Google Scholar]
- 21. Lau D, Khan A, Terman SW, Yee T, Marca FL, Park P. Comparison of perioperative outcomes following open versus minimally invasive transforaminal lumbar interbody fusion in obese patients. Neurosurg Focus. 2013;35:E10. [DOI] [PubMed] [Google Scholar]
- 22. Li XC, Huang CM, Zhong CF, Liang RW, Luo SJ. Minimally invasive procedure reduces adjacent segment degeneration and disease: new benefit-based global meta-analysis. PLoS One. 2017;12:e0171546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Patel JY, Kundnani VG, Merchant ZI, Jain S, Kire N. Superior facet joint violations in single level minimally invasive and open transforaminal lumbar interbody fusion: a comparative study. Asian Spine J. 2020;14:25–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Emami A, Faloon M, Sahai N, et al. Risk factors for pseudarthrosis in minimally-invasive transforaminal lumbar interbody fusion. Asian Spine J. 2018;12:830–838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Eckman WW, Hester L, McMillen M. Same-day discharge after minimally invasive transforaminal lumbar interbody fusion: a series of 808 cases. Clin Orthop Relat Res. 2014;472:1806–1812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Siemionow K, Pelton MA, Hoskins JA, Singh K. Predictive factors of hospital stay in patients undergoing minimally invasive transforaminal lumbar interbody fusion and instrumentation. Spine (Phila Pa 1976). 2012;37:2046–2054. [DOI] [PubMed] [Google Scholar]
- 27. Adogwa O, Parker SL, Bydon A, Cheng J, McGrit J. Comparative effectiveness of minimally invasive versus open transforaminal lumbar interbody fusion: 2-year assessment of narcotic use, return to work, disability, and quality of life. J Spinal Disord Tech. 2011;24:479–484. [DOI] [PubMed] [Google Scholar]
- 28. Parker SL, Lerner J, McGirt MJ. Effect of minimally invasive technique on return to work and narcotic use following transforaminal lumbar inter-body fusion: a review. Prof Case Manag. 2012;17:229–235. [DOI] [PubMed] [Google Scholar]
- 29. Parker SL, Adogwa O, Bydon A, Cheng J, McGrit J. Cost-effectiveness of minimally invasive versus open transforaminal lumbar interbody fusion for degenerative spondylolisthesis associated low-back and leg pain over two years. World Neurosurg. 2012;78:178–184. [DOI] [PubMed] [Google Scholar]
- 30. Parker SL, Mendenhall SK, Shau DN, et al. Minimally invasive versus open transforaminal lumbar interbody fusion for degenerative spondylolisthesis: comparative effectiveness and cost-utility analysis. World Neurosurg. 2014;82:230–238. [DOI] [PubMed] [Google Scholar]
- 31. Dorward IG, Lenke LG, Bridwell KH, et al. Transforaminal versus anterior lumbar interbody fusion in long deformity constructs: a matched cohort analysis. Spine (Phila Pa 1976). 2013;38:E755–E762. [DOI] [PubMed] [Google Scholar]
- 32. Chou D. Commentary: Retrospective review of immediate restoration of lordosis in single-level minimally invasive transforaminal lumbar interbody fusion: a comparison of static and expandable interbody cages. Oper Neurosurg (Hagerstown). 2020;18:E153–E154. [DOI] [PubMed] [Google Scholar]
- 33. Jagannathan J, Sansur CA, Oskouian RJ, Jr, Fu KF, Shaffrey CI. Radiographic restoration of lumbar alignment after transforaminal lumbar interbody fusion. Neurosurgery. 2009;64:955–964. [DOI] [PubMed] [Google Scholar]
- 34. Zhu Y, Wang B, Wang H, Jin Z, Zhu Z, Liu H. Long-term clinical outcomes of selective segmental transforaminal lumbar interbody fusion combined with posterior spinal fusion for degenerative lumbar scoliosis. ANZ J Surg. 2014;84:781–785. [DOI] [PubMed] [Google Scholar]
- 35. Kwon BK, Berta S, Daffner SD, et al. Radiographic analysis of transforaminal lumbar interbody fusion for the treatment of adult isthmic spondylolisthesis. J Spinal Disord Tech. 2003;16:469–476. [DOI] [PubMed] [Google Scholar]