Abstract
Study Design:
Narrative review.
Objectives:
Describe a comprehensive spine telemedicine examination.
Methods:
We discuss telemedicine examination techniques for commonly encountered spine conditions.
Results:
Techniques to evaluate gait, the cervical spine, the lumbar spine, adult spinal deformity patients, and adolescent scoliosis patients via telemedicine are described. We review limitations of the spine telemedicine examination and discuss special considerations such as patient safety and criteria for in-person assessment.
Conclusions:
While there are limitations to the spine telemedicine examination, unique strategies exist to provide important information to the examiner. Efforts have already been undertaken to validate and expand the capabilities of the spine telemedicine examination.
Keywords: telemedicine, virtual spine examination, COVID-19
Introduction
The worldwide spread of COVID-19 has disrupted nearly every facet of routine clinical practice. Orthopedic and spine providers are now providing outpatient care remotely through previously underutilized digital platforms. 1 -7 Telemedicine for outpatient orthopedic care was explored prior to the current pandemic. 8 -14 These studies determined that telemedicine consultation was feasible, 12,14 cost-effective, 8 and associated with high patient satisfaction 9 for this patient population. However, these efforts focused mainly on general orthopedics and trauma populations with little or no focus on patients presenting to spine surgeons. Some authors have questioned the role of telemedicine for patients with “back problems,” but this was a purely anecdotal conclusion based on the treatment of 5 patients in 2 studies. 10,12 Recent efforts to characterize the elements of the orthopedic telemedicine virtual physical exam have focused on the hip, shoulder, knee, and elbow. 15 With the current rapid rise in the use of telemedicine evaluations, there is a need for a spine-focused telemedicine physical exam protocol.
Tanaka et al 15 recently outlined a comprehensive virtual visit protocol for patients prior to their telemedicine examination. This includes a previsit checklist that is sent to patients outlining instructions to optimize the visit—attire, lighting, privacy, video connection, camera position, and so on. We have adopted similar practices with some minor modifications. While orthopedic physical examinations can be more focused to a single body-part in some cases (eg, left elbow), the spine examination often requires the examiner to see a larger area of the body—lower extremities, full body during gait, and so on. As such, patients are advised to wear shorts so that the lower extremities can be assessed and are encouraged to wear clothing that allows for the modest examination of the chest, abdomen, and back.
Prior to the visit, patients are sent instructions to optimize camera position and lighting. We advise patients to position their camera in a space where they will be able to ambulate on camera. The camera should be positioned to allow for full body assessment while standing and ambulating. In some instances, such as tall and/or obese patients, the camera will need to be moved further away to maximize the field. This has not been problematic thus far in our experience. Handheld devices are particularly useful when someone is accompanying the patient. Such devices can be easily moved to change focus and zoom. After making their appointment, patients are contacted by a staff member to assist with platform access and technology troubleshooting. Based on screening questions, patients are instructed to have certain household items present (ie, water bottle or weight) to aid in the examination. In our experience, these steps have reduced connection issues and improved the efficiency of the exam. If previously completed imaging studies are available from outside sources, we encourage them to be delivered and uploaded to our PACS (picture archiving and communication system) system. On the basis of the referral information, further imaging is needed, we may organize for them to be obtained prior to the telemedicine visit. Images and/or diagrams of commonly completed examination maneuvers can be sent to patients ahead of the visit to facilitate the examination. While some patients (and providers) have difficulty with telemedicine and the new technology, our experience has mirrored the literature regarding shorter wait times and reduced time requirements, in particular travel to the office, while maintaining high patient satisfaction. 9,16,17
Prior to initiating the examination, a comprehensive new or interval history should be obtained from the patient. The provider can ascertain information that focuses the examination and differentiates elective issues from urgent and emergent problems—wound drainage, fevers, progressive or severe neurologic deficits, gait disturbances, intractable pain. 1 During the encounter, the provider can often utilize the share screen feature of the telemedicine platform to review the patient’s imaging. Like any medical or surgical visit, it is important to review the risks, benefits, and alternatives of the available treatments with the patient as well as the anticipated outcomes.
Limitations and Special Considerations
Before discussing the elements of the spine telemedicine examination, it is important to review some limitations of the spine telemedicine visit. To our knowledge, the essential elements of a spine telemedicine examination have not yet been validated. Evaluating extremity reflexes and assessing for pathologic reflexes (Hoffman’s, Babinski) are key parts of an in-person spine examination. Unfortunately, this is not possible with a telemedicine visit, unless of course there is an able assistant at the patient’s site. In addition, simple provocatory maneuvers and resistive strength testing may not be assessed. There are techniques to augment testing that can evaluate for myelopathy and provide information beyond antigravity strength. However, one cannot ignore the current limitations of the telemedicine examination regarding differentiating 4/5 strength from 5/5 and detecting subtle sensory deficits. 18 Since telemedicine will remain a part of medical practice after the current 2019/2020 pandemic, further work is needed to address the current limitations of the spine telehealth examination.
Compared with other surgical specialties, triaging spine patients carries a unique set of challenges and higher acuity cases. 1,19 It is imperative to identify patients who may need urgent face-to-face evaluation and possibly emergent surgical intervention. The decision to proceed with emergent in-person evaluation and/or surgery can be made through telemedicine. 18 In general, patients with incontinence, urinary retention, progressive neurological deficits, acute loss of ambulation, and/or signs of infection are advised to present to the Emergency Department for initial evaluation. While some patients may ultimately not need spine surgery, the benefit of urgent evaluation in these instances far outweighs the harm caused by delay. 18
The care and safety of the patient during telemedicine evaluations are paramount. Like others, we remain concerned about patient injury and/or falls during gait and balance testing. 18 Individuals accompanying the patient are instructed to remain vigilant and provide support when able. However, when the patient is alone, the provider must determine if the patient can safely complete the maneuver. We generally will err on the side of caution and have been fortunate to not have any patient safety events. To our knowledge, the extent of provider liability should a patient become injured during a telemedicine has not been established. The same principles apply to patients who rely on walking aids or use wheelchairs for transportation. In these cases, certain components of the examination are amended or avoided to ensure the safety of the patient. When available, individuals accompanying the patient can provide safety support and be of assistance to the examiner. A sudden reliance on such aids may be indicative of acute neurologic decline and warrants immediate investigation. If concerns regarding safety render the examination incomplete, then the patient will need an in-person visit.
Some patients require additional support to prepare for and complete a telemedicine spine visit. However, in our experience, the additional support is no different than what is required for an in-person visit. In general, when a patient with a cognitive deficit presents for an in-person visit they are accompanied by a caregiver or aid. Similar support is needed for the proper setup and execution of telemedicine visits and examinations. Patients with more severe deficits often live in facilities with on-site physicians and clinical staff members. Telemedicine enables the on-site clinician to communicate directly with the spine provider, which is generally does not occur during in-person visits. Prior studies have demonstrated that telemedicine visits are well tolerated by pediatric spine patients and their parents. 17 Visit scheduling and consent are completed in the same manner as an in-person visit. Parental involvement in visit preparation (camera positioning, portal access, etc), intake paperwork and the examination depends on the patient’s age and maturity level.
Virtual Examination
Gait
Gait evaluation is frequently utilized during in-person patient visits because it provides useful diagnostic information and functional assessment. Under most circumstances, it can be incorporated into the telemedicine spine consult in a safe and reasonable manner. The patient is instructed to position the camera such that their full body is able to be visualized through the gait cycle (Figure 1). Different abnormal gait patterns are well described and, in our experience, can be recognized via telemedicine. While specific gait disturbances can have multiple different etiologies, recognition of abnormal pattern can influence the remainder of the exam and treatment plan.
Figure 1.
Gait examination. After repositioning their camera, the patient is instructed to ambulate. Ideally, the patient’s entire body will be visualized and allow for assessment of balance, posture, and gait pattern.
Many patients with myelopathy have a spastic paretic gait characterized by stiff legs, a wide base, and jerky movements. 20 The patients also move slowly and have reduced toe clearance during swing phase. This gait pattern should raise concern for cervical and/or thoracic cord compression. Recognition of this pattern during a telemedicine exam is even more important due to the inability to assess reflexes via telemedicine. Patients with lumbar stenosis exhibit a different pattern of altered gait. 21 The hallmark of neurogenic claudication is the worsening of lower extremity symptoms with standing and ambulation. These patients adopt a compensatory stooped forward posture during ambulation to reduce epidural pressure. Patients with significant ankle dorsiflexor weakness (foot drop) exhibit a steppage gait. These patients either drag the affected foot or compensate with exaggerated hip and knee flexion. There is often a slapping sound as the toes of the affected foot contact the ground. Unilateral foot drop can be caused by a number of different conditions, including compression of the L4 and L5 nerve roots. In some instances, coronal deformity, leg length inequality, and coronal imbalance may become more apparent with ambulation. 22
Cervical Spine
The nature of the telemedicine exam facilitates inspection of the ventral neck. The dorsal skin is inspected when relevant to the patient’s history and complaints. Surgical incisions are evaluated for healing and infection. Posterior incisions should be assessed for muscle atrophy and appropriate healing. Head and neck posture are assessed passively during the encounter. The patient’s head should be midline, with the chin above the manubrium. The patient should be able to maintain upright head posture and gaze into the camera. After having the patient turn their chair or adjust the camera, one can assess the sagittal alignment of the cervical spine.
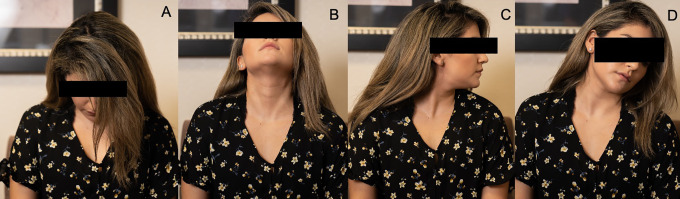
Active cervical range of motion (ROM) can be assessed while the patient remains seated. Limitations due to stiffness and/or pain are carefully noted. The patient is instructed to complete flexion (normal 80°-90°), extension (normal 70°), left and right rotation (normal 70°-90°), and lateral flexion maneuvers (20°-45°) (Figure 2). These ROM maneuvers may provide additional information regarding the patient’s clinical status. For example, patients with spinal cord demyelination can experience an electric shock sensation down the spine into the trunk and extremities with flexion of the cervical spine (Lhermitte’s sign). 23 Patients with suspected cervical radiculopathy are instructed to complete neck extension with lateral bending (Spurling test) (Figure 2). This maneuver, even without axial compression, is a reliable provocative test in the diagnosis of cervical radiculopathy. 24 The shoulder abduction test for cervical radiculopathy is well-suited for telemedicine. 25 Patients are instructed to abduct their shoulder and hold their arm above their head. Subsequent relief of upper extremity pain is indicative of a cervical nerve root compression. This test is useful to distinguish cervical radiculopathy from peripheral nerve lesions and shoulder dysfunction.
Figure 2.
The nature of the telemedicine exam facilitates evaluation of head and neck motion. The patient is instructed to complete neck flexion (A), extension (B), and left and right rotation (C). The patient is instructed to complete an extension with lateral bending maneuver (D) if there is concern for an ipsilateral cervical radiculopathy.
A thorough in-person cervical spine examination determines the extent of motor and sensory derangements and evaluates for signs of spinal cord compression and myelopathy. Despite limitations inherent to the telemedicine exam, careful assessment of upper extremity function can take place via this method. Upper extremity sensation defects are assessed during the history. When clarification is needed, the patient is instructed to pinpoint the precise location of their sensory symptoms via touch. Upper extremity myotomes (C5-T1) are assessed for strength against gravity. Significant motor deficits can be identified in upper extremity muscle groups (0-2/5 strength). Ability to perform range of motion against gravity can be scored as “muscle strength of at least 3/5.” When subtle weakness is suspected, common household objects can be utilized in the exam. For example, patients can hold bottles of water (1 lb) or gallon milk (8 lbs) containers to add resistive force. 15 The patient is instructed to “curl” the object with both the right and left arm to assess strength and stamina differences of the biceps (Figure 3). This same type of maneuver can be used for deltoid and triceps function. To assess grip strength the patient can be instructed to squeeze a tennis ball or any available squishy object repeatedly. Standing single-arm push-ups against a wall can also be performed to assess biceps (lower) and triceps (raise) strength. Buckling or failure to complete the maneuver indicates weakness.
Figure 3.

Upper extremity strength can be assessed beyond gravity using simple household objects. The patient is instructed to “curl” the object with both the right and left arm to assess strength and stamina differences of the biceps.
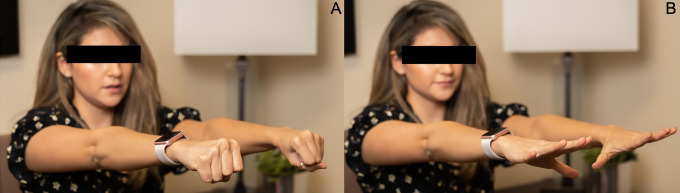
Patients with myelopathy (cervical and thoracic) will have alterations to their gait. As a result, we recommend assessing gait when deemed safe and feasible. We will also perform a Romberg test if the patient is accompanied by someone, as impaired dorsal column function may result in swaying or falling while standing with closed eyes and extended arms. A positive Romberg test can occur in a variety of a proprioceptive disorders, including cervical myelopathy. Finger escape sign and grip and release test are useful tools to assesses for myelopathy with telemedicine. 26 In the finger escape test, patients are instructed to hold their fingers extended and adducted. A positive finger escape test can be seen in myelopathy and occurs when the little finger spontaneously abducts and flexes. A positive grip-and-release test occurs when a patient is unable to make a tight grip and release it 20 times in 10 seconds (Figure 4) Myelopathic patients are unable to complete these fast, repetitive motions.
Figure 4.
The grip-and-release test is a quantifiable test for myelopathy. Myelopathic patients are unable to make a fist (A) and release it (B) 20 times in 10 seconds.
Lumbar Spine
Examination of the lumbar spine usually begins with inspection of the overlying dorsal skin. This necessitates having the patient stand and face away from the camera. Evaluation of the ventral skin is at the discretion of the provider; prior ventral incision, consideration of anterior retroperitoneal surgery. Surgical sites can be evaluated for stage of healing and/or presence of infection. If the patient has focal pain, the location can be identified by the patient. The examiner can assess for obvious scoliosis, flatback deformity, and leg-length discrepancy. Having the patient place their hands on their iliac crests is useful technique to further estimate the level of their pain; lumbar spine versus sacrum/sacroiliac joint (SIJ).
Patients with SIJ dysfunction will localize their pain off the midline and below the lumbar spine (Fortin’s finger test). 27 Multiple clinical pain provocation tests for the SIJ have been described and validated. 28 Patients with SIJ pain will often lean on the unaffected side while seated. Any alteration in posture while seated can be seen on camera while taking a history and investigated. With the patient seated, the examiner can ask the patient to flex, abduct and externally rotate (FABER) the hip on the affected side (Figure 5). Reproduction of pain with this maneuver is indicative of SIJ pain. Seated hip range of motion (flexion, extension, internal rotation, external rotation) testing is utilized to evaluate for hip osteoarthritis. The drop test is a reliable provocative test for the SIJ that does not require the examiner to directly interact with the patient. 29,30 While standing and bracing the wall, the patient is instructed to raise the heel on the affected side bearing near fully body weight. Next, the patient forcefully drops their heel to the floor while keeping the knee extended (Figure 6). Alternatively, the patient can initiate a small hop on the affected side again landing on the heal with the knee extended. These maneuvers produce a shear force cranially through the ipsilateral SIJ that produces pain in individuals with joint dysfunction. 30
Figure 5.

Seated FABER examination for sacroiliac joint (SIJ) pain. The patient is instructed to flex, abduct, and externally (FABER) rotate the hip on the affected side.
Figure 6.
Drop test for sacroiliac joint (SIJ) pain. While standing and bracing the wall, the patient is instructed to raise the heel on the affected side bearing near fully body weight (A). Next, the patient forcefully drops their heel to the floor while keeping the knee extended (B).
In our experience, active lumbar ROM can be readily assessed via telemedicine. The patient can be asked to reproduce movements that either produce or alleviate pain. While standing, the patient can perform flexion (normal 80°-90°), extension (normal 20°-30°), side bending (normal 15°-30°), and rotation (normal 30°-40°) maneuvers. Differences in ROM and ability to perform movements due to pain can be observed and aid in diagnosis. For example, discogenic symptoms are frequently exacerbated with flexion and relieved with extension. The opposite can occur in patients with spinal stenosis. Pain with combined extension and rotation can indicate facetogenic pain. In patients with suspected lumbar radiculopathy, seated straight leg raise (SLR) can be performed (Figure 7). It is equivalent to a traditional supine SLR and is practical for telemedicine assessment. 31 While seated the patient is instructed to actively extend the knee with the hip in a flexed position. Lower extremity radicular pain with knee straightening, or the patient leaning back to avoid pain indicates sciatic nerve tension.
Figure 7.

Seated straight leg raise (SLR) can be performed in patients with suspected lumbar radiculopathy. While seated, the patient is instructed to extend their knee joint.
A key feature of a comprehensive lumbar spine examination includes the assessment of lower extremity motor and sensory function. Patients can describe and localize specific areas of altered sensation and numbness. The lack of physician directed resistance with routine testing makes it difficult to detail anything beyond 3/5 strength. Despite these limitations, all lumbosacral (L1-S3) myotomes are assessed against gravity. A significant loss of strength can be identified. A number of patient-directed maneuvers are helpful to test beyond antigravity strength in frequently affected muscle groups. First, the examiner should instruct the patient to properly position their camera to capture the relevant body part/movement. Safety should also be assessed prior to attempting these tests as patients may have altered strength and balance. When the patient is alone, we recommend making sure a stable surface (counter, table, etc) is available. Squats, heel-walking, and toe-walking can be used to further test quadricep (L3/4), ankle dorsiflexor/tibialis anterior/extensor hallicus longus (L4/5) and calf/plantar flexors (S1) strength, respectively (Figure 8). Single leg squats, toe-rises, and heel rises can further distinguish a strength deficit relative to the contralateral limb. The hip abductors (L5) can be evaluated with a modified Trendelenburg test by asking the patient to support themselves perpendicular to a table or chair back and then lift their inside leg while observing if the pelvis dips (Figure 9).
Figure 8.

Squats (A), heel-walking (B), and toe-walking (C) can be used to further test lower extremity myotomes.
Figure 9.
Modified Trendelenburg test for hip abductor strength. The patient stands perpendicular to a table or chair for support. The inside leg is lifted to test the outside hip abductors. Patients with normal hip abductor strength will be able to support the inside hemipelvis (A). Abnormal hip abductor strength will result in contralateral (inside) hemipelvis dipping (B).
Adult Spinal Deformity
Adult spinal deformity (ASD) refers to a diverse collection of spinal conditions that occur throughout adulthood. These patients experience a constellation of neurological and functional symptoms that are distinct from adolescent patients. The goal of the telemedicine exam for ASD patients is to evaluate and characterize their global deformity while identifying acute changes in neurological status or function.
The telemedicine exam for ASD begins with an assessment of global posture. Standing helps elucidate coronal and sagittal deformities. 22 With the patient standing and facing the camera, one can inspect the patient for coronal trunk shift. The patient’s head should be balanced above the pelvis. The patient can then turn away from the camera. Many of these patients have had prior surgery. Surgical scars should be inspected for signs of infection, hardware prominence or failure. One can also evaluate for asymmetry of the trunk, shoulders, and pelvis. An important part of the exam is examining the sagittal profile of the patient. The camera is positioned to see the patient from head to toe and the patient is instructed to turn to the side. This can be difficult to do with a personal computer that is relatively fixed. An accompanying person with a smart phone or tablet camera can position themselves to capture the full patient. The patient is evaluated for positive sagittal imbalance and associated compensatory mechanisms—hip extension, knee flexion, pelvic retroversion, posterior tilt of the head.
Following assessment of coronal and sagittal deformity, we analyze their gait. Patients with ASD often assume a decompensated posture due to the fatigue of inefficient ambulation. This dynamic sagittal imbalance can provide additional information regarding their deformity. As previously discussed, gait can provide clues regarding nerve root compression and myelopathy. This is especially important since we are not able to test reflexes. Some patients experience camptocormia, a nonfixed and involuntary flexion of their lumbar spine, after initiating ambulation. 22,32 It is related to Parkinson’s disease and other neuromuscular disorders and should be distinguished from structural spinal deformity.
Lower extremity myotomes and dermatomes are evaluated as detailed above. If there is any concern for cervical compression, the upper extremities are evaluated as well. Concerning findings may prompt urgent imaging or in-person evaluation.
Adolescent Scoliosis
Evaluations of new and established adolescent spine patients have continued throughout the COVID-19 pandemic. A thorough assessment of gait and lower extremity motor/sensory function should take place as previously detailed. However, there are additional aspects of the telemedicine exam unique to this patient population. In particular, the examiner should be wary of conditions that are important to distinguish from idiopathic scoliosis. Facial asymmetry and cranial nerve dysfunction can point to brain and brainstem abnormalities. If there is concern, hypermobility can be evaluated using the Beighton-Horan criteria; elbow extension, knee extension, little finger extension, thumb to forearm, and forward bending. 33 Hypermobility and arachnodactyly are associated with connective tissue disorders.
Careful examination of the ventral and dorsal aspects of the trunk takes place with the patient standing. Skin markings can be indicative of other underlying conditions; tuft of hair in spinal dysraphism and café au spots in Neurofibromatosis. 34 The patient’s feet should be examined for signs of underlying neurological disorders; toe clawing, cavus deformity, contractures. Asymmetry of the torso, pelvis and shoulders can be assessed with patient standing and facing away from the video camera. Pelvic obliquity can occur in the setting of limb-length inequality. An unidentified limb-length inequality may be the source of a functional scoliosis. 35
A key component of the adolescent spine examination is evaluation of coronal and sagittal alignment. Deviation to one side (coronal decompensation) should be documented. Increased kyphosis or any sharp change in sagittal alignment should be noted. The rotation of thoracic vertebrae produces a rib hump on the convexity of the deformity. The flexibility and morphology of the coronal curve can be assessed with the Adams forward bend test. The patient is instructed to turn away from the camera and bend at the waist until their trunk is in the horizontal plane. The rib hump can be viewed and compared with the lower side to estimate the degree of deformity and flexibility. The patient then can be instructed to bed to each side to further assess coronal flexibility of both the thoracic and lumbar components of their curves.
Future Directions
Future work is needed to assess the quality and validity of the spine telemedicine examination. Given the likelihood that telemedicine will persist and grow even after the restrictions of the pandemic, it will be important to assess patient satisfaction with the experience. Perhaps certain patients or visit types are best suited to this medium. Tanaka et al 15 reviewed some of the potential technological advances related to motion-capture imaging and remote dynamic testing. 15 With regard to spine surgery, efforts have already been taken to develop a self-administered neurological examination for telemedicine that utilizes TheraBands and Semmes-Weinstein monofilaments. 36 Future work will no doubt expand on these efforts and increase the reliability and reproducibility of the spine telemedicine examination.
Acknowledgments
The authors would like to acknowledge and thank Phillip Slaughter and Ally Parish for their help with the figures in the article.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Alexander M. Satin  https://orcid.org/0000-0001-9181-7494
https://orcid.org/0000-0001-9181-7494
References
- 1. Jain NS, Alluri RK, Schopler SS, Hah R, Wang JC. COVID-19 and spine surgery: a review and evolving recommendations. Global Spine J. 2020;10:528–533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Sarpong NO, Forrester LA, Levine WN. What’s important: redeployment of the orthopaedic surgeon during the COVID-19 pandemic: perspectives from the trenches. J Bone Joint Surg Am. 2020;102:1019–1021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Vannabouathong C, Devji T, Ekhtiari S, et al. Novel coronavirus COVID-19: current evidence and evolving strategies. J Bone Joint Surg Am. 2020;102:734–744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Liang ZC, Wang W, Murphy D, Hui JHP. Novel coronavirus and orthopaedic surgery: early experiences from Singapore. J Bone Joint Surg Am. 2020;102:745–749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Halawi MJ, Wang DD, Hunt TR, 3rd. What’s important: weathering the COVID-19 crisis: time for leadership, vigilance, and unity. J Bone Joint Surg Am. 2020;102:759–760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Haleem A, Javaid M, Vaishya R, Vaish A. Effects of COVID-19 pandemic in the field of orthopaedics. J Clin Orthop Trauma. 2020;11:498–499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Parisien RL, Shin M, Constant M, et al. Telehealth utilization in response to the novel coronavirus (COVID-19) pandemic in orthopaedic surgery. J Am Acad Orthop Surg. 2020;28:e487–e492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Buvik A, Bergmo TS, Bugge E, Smaabrekke A, Wilsgaard T, Olsen JA. Cost-effectiveness of telemedicine in remote orthopedic consultations: randomized controlled trial. J Med Internet Res. 2019;21:e11330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Buvik A, Bugge E, Knutsen G, Småbrekke A, Wilsgaard T. Patient reported outcomes with remote orthopaedic consultations by telemedicine: a randomised controlled trial. J Telemed Telecare. 2019;25:451–459. [DOI] [PubMed] [Google Scholar]
- 10. Buvik A, Bugge E, Knutsen G, Småbrekke A, Wilsgaard T. Quality of care for remote orthopaedic consultations using telemedicine: a randomised controlled trial. BMC Health Serv Res. 2016;16:483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Aarnio P, Lamminen H, Lepistö J, Alho A. A prospective study of teleconferencing for orthopaedic consultations. J Telemed Telecare. 1999;5:62–66. [DOI] [PubMed] [Google Scholar]
- 12. Haukipuro K, Ohinmaa A, Winblad I, Linden T, Vuolio S. The feasibility of telemedicine for orthopaedic outpatient clinics—a randomized controlled trial. J Telemed Telecare. 2000;6:193–198. [DOI] [PubMed] [Google Scholar]
- 13. Sathiyakumar V, Apfeld JC, Obremskey WT, Thakore RV, Sethi MK. Prospective randomized controlled trial using telemedicine for follow-ups in an orthopedic trauma population: a pilot study. J Orthop Trauma. 2015;29:e139–e145. [DOI] [PubMed] [Google Scholar]
- 14. Vuolio S, Winblad I, Ohinmaa A, Haukipuro K. Videoconferencing for orthopaedic outpatients: one-year follow-up. J Telemed Telecare. 2003;9:8–11. [DOI] [PubMed] [Google Scholar]
- 15. Tanaka MJ, Oh LS, Martin SD, Berkson EM. Telemedicine in the era of COVID-19: the virtual orthopaedic examination. J Bone Joint Surg Am. 2020;102:e57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Sharareh B, Schwarzkopf R. Effectiveness of telemedical applications in postoperative follow-up after total joint arthroplasty. J Arthroplasty. 2014;29:918–922.e1. [DOI] [PubMed] [Google Scholar]
- 17. Sultan AA, Acuña AJ, Samuel LT, et al. Utilization of telemedicine virtual visits in pediatric spinal deformity patients: a comparison of feasibility and patient satisfaction at a large academic center. J Pediatr Orthop. Published online March 31, 2020. doi:10.1097/BPO.0000000000001553 [DOI] [PubMed] [Google Scholar]
- 18. Donnally CJ, 3rd, Vaccaro AR, Schroeder GD, Divi SN. Is evaluation with telemedicine sufficient before spine surgery? Clin Spine Surg. Published online June 2, 2020. doi:10.1097/BSD.0000000000001027 [DOI] [PubMed] [Google Scholar]
- 19. Donnally CJ, 3rd, Shenoy K, Vaccaro AR, Schroeder GD, Kepler CK. Triaging spine surgery in the COVID-19 era. Clin Spine Surg. 2020;33:129–130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Lim MR, Huang RC, Wu A, Girardi FP, Cammisa FP, Jr. Evaluation of the elderly patient with an abnormal gait. J Am Acad Orthop Surg. 2007;15:107–117. [DOI] [PubMed] [Google Scholar]
- 21. Suda Y, Saitou M, Shibasaki K, Yamazaki N, Chiba K, Toyama Y. Gait analysis of patients with neurogenic intermittent claudication. Spine (Phila Pa 1976). 2002;27:2509–2513. [DOI] [PubMed] [Google Scholar]
- 22. Smith JS, Shaffrey CI, Fu KMG, et al. Clinical and radiographic evaluation of the adult spinal deformity patient. Neurosurg Clin N Am. 2013;24:143–156. [DOI] [PubMed] [Google Scholar]
- 23. Kempster PA, Rollinson RD. The Lhermitte phenomenon: variant forms and their significance. J Clin Neurosci. 2008;15:379–381. [DOI] [PubMed] [Google Scholar]
- 24. Anekstein Y, Blecher R, Smorgick Y, Mirovsky Y. What is the best way to apply the Spurling test for cervical radiculopathy? Clin Orthop Relat Res. 2012;470:2566–2572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Davidson RI, Dunn EJ, Metzmaker JN. The shoulder abduction test in the diagnosis of radicular pain in cervical extradural compressive monoradiculopathies. Spine (Phila Pa 1976). 1981;6:441–446. [DOI] [PubMed] [Google Scholar]
- 26. Cook CE, Wilhelm M, Cook AE, Petrosino C, Isaacs R. Clinical tests for screening and diagnosis of cervical spine myelopathy: a systematic review. J Manipulative Physiol Ther. 2011;34:539–546. [DOI] [PubMed] [Google Scholar]
- 27. Fortin JD, Falco FJ. The Fortin finger test: an indicator of sacroiliac pain. Am J Orthop (Belle Mead NJ). 1997;26:477–480. [PubMed] [Google Scholar]
- 28. Laslett M, Aprill CN, McDonald B, Young SB. Diagnosis of sacroiliac joint pain: validity of individual provocation tests and composites of tests. Man Ther. 2005;10:207–218. [DOI] [PubMed] [Google Scholar]
- 29. Robinson HS, Brox JI, Robinson R, Bjelland E, Solem S, Telje T. The reliability of selected motion-and pain provocation tests for the sacroiliac joint. Man Ther. 2007;12:72–79. [DOI] [PubMed] [Google Scholar]
- 30. Laslett M. Evidence-based diagnosis and treatment of the painful sacroiliac joint. J Man Manip Ther. 2008;16:142–152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Fajolu OK, Pencle FJ, Rosas S, Chin KR. A prospective analysis of the supine and sitting straight-leg raise test and its performance in litigation patients. Int J Spine Surg. 2018;12:58–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Margraf N, Wrede A, Deuschl G, Schulz-Schaeffer W. Pathophysiological concepts and treatment of camptocormia. J Parkinsons Dis. 2016;6:485–501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Wolf JM, Cameron KL, Owens BD. Impact of joint laxity and hypermobility on the musculoskeletal system. J Am Acad Orthop Surg. 2011;19:463–471. [DOI] [PubMed] [Google Scholar]
- 34. Magee DJ. Orthopedic Physical Assessment. 6th ed. Elsevier Health Sciences; 2014. [Google Scholar]
- 35. Raczkowski JW, Daniszewska B, Zolynski K. Functional scoliosis caused by leg length discrepancy. Arch Med Sci. 2010;6:393–398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Goyal DK, Divi SN, Bowles DR, et al. Telemedicine neurological exam: a pilot trial. Paper presented at: 47th Annual CSRS Meeting; November 21-23, 2019; New York, NY. [Google Scholar]