Editor—Sleep plays an essential role in homeostasis of multiple organ systems and cognitive function.1,2 It is commonly disrupted in the perioperative period.3 The lack of large-scale pragmatic trials investigating the relationship between perioperative sleep and clinical outcomes can be attributed to logistics of labour-intensive clinical polysomnography. As an alternative to polysomnography, lightweight wireless wearable devices may provide high-quality sleep data for in-home studies.4,5 However, it is unclear whether these technological advances can potentially translate into larger clinical investigations on the putative relationships between sleep and perioperative outcomes.
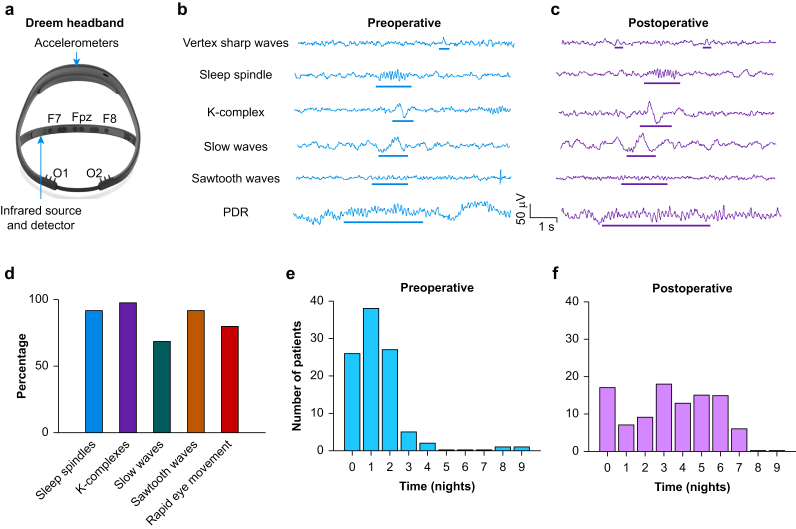
Here, we evaluate the feasibility of using a wireless EEG headband for characterising perioperative sleep structure (Fig. 1a). The Dreem headband (Dreem, New York, NY, USA), previously validated against polysomnography for a broad age demographic,5 has EEG dry electrodes, including frontal (F7, F8, and Fpz) and occipital (O1 and O2) sensors. An infrared light source–detector pair allows pulse plethysmography whilst accelerometers track respiratory effort. We hypothesised that (i) wireless wearable headbands would allow acquisition of perioperative EEG sleep markers suitable for sleep staging and quantitative analyses, (ii) one night of preoperative sleep is sufficient for establishing baseline sleep structure, and (iii) sleep would be disrupted in the postoperative period.
Fig 1.
Electroencephalogram (EEG) waveforms recorded by the Dreem device allowed sleep staging in the pre- and postoperative settings. (a) The Dreem device is a portable, wireless headband used to continuously monitor EEG data, pulse plethysmography, and accelerometry data during sleep. The Dreem device contains five dry EEG electrodes for recording at three frontal locations (F7, F8, and Fpz) and two occipital locations (O1 and O2) in addition to sensors for obtaining plethysmography and accelerometry data. Example EEG waveforms from one patient are shown (b) before and (c) after surgery (postoperative Day 3). These EEG signals were recorded from channel Fpz–F7. The EEG microstructural elements that allow sleep staging include vertex sharp waves, sleep spindles, K-complexes, slow waves, and sawtooth waves. The posterior dominant rhythm (PDR) assists in the detection of wakefulness (recorded in channel Fpz–O1). (d) Percentage of detectable EEG microstructural elements in preoperative records. Frequency of the device utilisation for all patients in (e) pre- and (f) postoperative settings. The Dreem device was utilised with a median (inter-quartile range) of 1 (1) and 3 (2) nights in the pre- and postoperative periods, respectively.
We recruited 100 geriatric cardiac surgical patients at Barnes-Jewish Hospital for this pilot study as part of the prospective observational investigation, Prognosticating Delirium Recovery Outcomes Using Wakefulness and Sleep Electroencephalography (ClinicalTrials.gov NCT03291626).6 These cardiac surgical patients are at risk for poor clinical outcomes related to disruption of perioperative sleep.7 Human studies approval was obtained from the institutional review board. The following inclusion criteria were used: English speaking, 60 yr of age or greater, and scheduled for elective cardiac surgery requiring cardiopulmonary bypass. Participants were excluded for deep hypothermic circulatory arrest, preoperative delirium at enrolment, and deafness or blindness. Patients were offered remuneration for up to two preoperative and seven postoperative recordings.
The Dreem was used to record nocturnal sleep data preoperatively and from postoperative night 0 to 7. Each record underwent scoring in 30 s epochs by registered polysomnographic technologists. The modified American Academy of Sleep Medicine criteria for scoring single-channel frontal EEG4 were further amended to include occipital EEG, closely spaced frontal EEG electrodes, and respiratory effort.6 Epochs were non-scorable if they did not fulfil staging criteria for wakefulness (W), non-rapid eye movement (N1–N3), and rapid eye movement (REM) sleep. Records were excluded as non-scorable if <60 min of sleep was present.
Dreem provided adequate EEG microstructural elements required for staging sleep macrostructure.8 Figure 1b and c illustrates EEG motifs used in sleep staging, using exemplary recordings obtained on a preoperative (Fig. 1b) and a postoperative (Fig. 1c) night for the same patient (EEG channel Fpz–F7). Amongst the 74 patients who provided preoperative data, 80% (106/132) of records were scorable. Of these scorable data sets, 92% had sleep spindles, 98% had K-complexes, 69% had slow waves, 92% had sawtooth waves, and 80% had REM (Fig. 1d). Total sleep time (TST; median of 209.8 min) was distributed as 8.3% N1, 70.6% N2, 2.1% N3, and 19% REM (Supplementary Fig. 1a), consistent with expected sleep structure in geriatric populations.9 Overall, Dreem afforded sufficient EEG quality in providing scorable preoperative sleep data.
Tolerability of Dreem was acceptable for recording nocturnal preoperative sleep. Of the 90 patients approached for preoperative recordings, 74 (82%) recorded at least one preoperative night. The yield of overnight preoperative sleep records was reasonable given a multistate referral base and patient engagement days before surgery, with a median (inter-quartile range [IQR]) of 1 (1) night (Fig. 1e).
We observed minimal intra-subject variance in preoperative sleep structure. Amongst 26 patients with two preoperative nocturnal recordings, paired Wilcoxon signed-rank tests revealed no significant intra-subject differences in the fraction of TST for REM (median difference: 5.6%; P=0.12), N1 (median difference: 0.17%; P=0.58), N2 (median difference: 6.06%; P=0.18), or N3 (median difference: 0.03%; P=0.99).
We had 83 patients (94%) complete at least one postoperative night of recording. An example set of hypnograms is included (Supplementary Fig. 1c). We excluded 69 records because of mechanical ventilation and concurrent sedation (propofol, dexmedetomidine, fentanyl, or midazolam). Of the remaining 270 postoperative nocturnal recordings, 189 (70%) were scorable. The recording time median (IQR) was 796 (275) min with corresponding TST of 178 (140) min (Supplementary Fig. 1b). N1 and N2 sleep accounted for 93.5% of TST, with median (IQR) durations of 24 (23) min for N1 and 137 (123) min for N2. Median (IQR) durations of N3 and REM were 0 (0) and 0 (13) min, respectively. Non-scorable epochs were attributed to movement or inadequacy for satisfying staging criteria because of atypical morphology.10 Contamination of these epochs could arise from effects of analgesics, sedatives, or noise arising from temporary external pacemakers. Non-scorable epochs accounted for 16.4% of total epochs between the first stage of sleep onset and the last epoch with a median (IQR) of 17 (112) min in postoperative recordings. Overall, patients wore Dreem with a median (IQR) of 3 (2) postoperative nights (Fig. 1f). Mann–Whitney U-tests with Benjamini–Hochberg adjustment showed significant differences in TST proportions for all sleep stages across pre- and postoperative sleep records. Overall, N1 and N2 were augmented in the postoperative period at the expense of REM and N3 (Supplementary Table 1).
In summary, we evaluated the perioperative use of a headband equipped with EEG dry electrodes, built-in amplifiers, and a design for consumer comfort. We reported disruption of sleep structure in postoperative setting consistent with previous investigations.7 A single night, rather than multiple nights, may suffice in establishing preoperative sleep macrostructure during Dreem wear. We avoided the time and labour required for repeated placement of gel/paste-based electrodes normally utilised for polysomnography. Thus, despite the caveats for gauging duration of TST and sleep stages, Dreem is a feasible alternative to polysomnography for serial evaluation of sleep in the perioperative period, particularly for EEG microstructural elements. This approach will be useful for large-scale investigations on the epidemiology, clinical impact, and treatment of perioperative sleep disturbances.
Acknowledgements
The authors would like to thank additional members of the Prognosticating Delirium Recovery Outcomes Using Wakefulness and Sleep Electroencephalography study group, including Jacob D. Bolzenius, Emma R. Huels, Brian Hickman, Jordan Oberhaus, Hersh Maniar, Daniel Park, Katie Dalton, Paul Galgani, Paul Krucylak, Spencer Melby, Troy Wildes, Michael Avidan, and ShiNung Ching.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.bja.2021.02.018.
Declarations of interest
The authors declare that they have no conflicts of interest.
Funding
US National Institute on Aging (National Institutes of Health R01AG057901) to BJAP.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Cirelli C., Tononi G. Is sleep essential? PLoS Biol. 2008;6 doi: 10.1371/journal.pbio.0060216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Irwin M.R. Sleep and inflammation: partners in sickness and in health. Nat Rev Immunol. 2019;19:702–715. doi: 10.1038/s41577-019-0190-z. [DOI] [PubMed] [Google Scholar]
- 3.Chung F., Liao P., Yegneswaran B., Shapiro C.M., Kang W. Postoperative changes in sleep-disordered breathing and sleep architecture in patients with obstructive sleep apnea. Anesthesiology. 2014;120:287–298. doi: 10.1097/ALN.0000000000000040. [DOI] [PubMed] [Google Scholar]
- 4.Lucey B.P., McLeland J.S., Toedebusch C.D. Comparison of a single-channel EEG sleep study to polysomnography. J Sleep Res. 2016;25:625–635. doi: 10.1111/jsr.12417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Arnal P.J., Thorey V., Debellemaniere E. The Dreem headband compared to polysomnography for EEG signal acquisition and sleep staging. Sleep. 2020;43:zsaa097. doi: 10.1093/sleep/zsaa097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Smith S.K., Nguyen T., Labonte A.K. Protocol for the Prognosticating Delirium Recovery Outcomes Using Wakefulness and Sleep Electroencephalography (P-DROWS-E) study: a prospective observational study of delirium in elderly cardiac surgical patients. BMJ Open. 2020;10 doi: 10.1136/bmjopen-2020-044295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Liao W.C., Huang C.Y., Huang T.Y., Hwang S.L. A systematic review of sleep patterns and factors that disturb sleep after heart surgery. J Nurs Res. 2011;19:275–288. doi: 10.1097/JNR.0b013e318236cf68. [DOI] [PubMed] [Google Scholar]
- 8.Berry R.B.B., Gamaldo C.E., Harding S.M., Lloyd R.M., Marcus C.L., Vaughn B.V. American Academy of Sleep Medicine; Darien, IL: 2015. The AASM manual for scoring of sleep and associated events: rules, terminology and technical specifications, version 2.3. [Google Scholar]
- 9.Van Cauter E., Leproult R., Plat L. Age-related changes in slow wave sleep and REM sleep and relationship with growth hormone and cortisol levels in healthy men. JAMA. 2000;284:861–868. doi: 10.1001/jama.284.7.861. [DOI] [PubMed] [Google Scholar]
- 10.Watson P.L., Pandharipande P., Gehlbach B.K. Atypical sleep in ventilated patients: empirical electroencephalography findings and the path toward revised ICU sleep scoring criteria. Crit Care Med. 2013;41:1958–1967. doi: 10.1097/CCM.0b013e31828a3f75. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.