Abstract
The anatomy of the elbow joint had been studied extensively over the last 2 decades. The increased understanding of the anatomy and contribution of the anatomical structures to the elbow biomechanics had enabled surgeons to improve the results of surgical reconstruction and fracture fixation. This review articles intend to summarise the salient functional and clinical anatomical and relevant biomechanical data that had been published recently.
Keywords: Anatomy, Biomechanics, Elbow
Introduction
The elbow joint is one of the most complex joints in the human body as it incorporates 3 articulations within its joint capsule, namely the ulno-humeral joint, radio-capitellar joint and the proximal radio-ulnar joint. The ulno-humeral and radio-capitellar joint allows sagittal plane flexion and extension movement whereas the radio-capitellar joint and the proximal radio-ulnar joint provides the rotation of the forearm in the coronal plane. The intricate interplay between the 3 articulations and the collateral ligaments provides the stable functional elbow which connects the shoulder to the hand and positions the hand in space by changing the length of the upper limb with flexion-extension and altering the position of the hand with rotation of the forearm The aim of this review is to outline the updated salient surgical anatomy and biomechanical features of these anatomical structures to aid surgical management of the elbow joint pathology especially during trauma surgery.
Anatomy of the distal humerus
The humerus is relatively straight in the coronal plane but it has an apex posterior bow of approximately 10° at the junction of approximately middle and distal one third in the sagittal plane.1 (Fig. 1). The canal of the distal humerus changes from being circular in proximal humerus to being triangular in distal humerus.2,3 The distal humerus flattens and widens into medial and lateral columns. The lateral column, which give rises to the capitellum diverges away from the humeral shaft more than the medial column which give rise to the trochlea. Hence, the spool-shaped trochlea is centred over the distal humerus in line with the long axis of the humeral shaft.4 The capitellum is not spherical but ellipsoidal with a greater radius of curvature in the medial-lateral direction.5 The trochlea contains two well-marked borders, i.e., the prominent medial and the smaller lateral ridge, which are divided by a centre sulcus called the trochlear groove. The depth of the trochlear sulcus and the two ridges form an average 142°6 open angle (trochlear notch angle, Fig. 2) downwards on the coronal plane. The apex of the medial and lateral faces of the coronoid keys into this notch. The medial ridge of the trochlea is more prominent than the lateral ridge, which causes 6°–8° of valgus tilt at its articulation with the ulna.7 (Fig. 2) This contributed to the carrying angle of the elbow, which is defined by the angle formed between the long axis of the humerus with the long axis of the ulna. The capitellum on the other hand is flexed forward in the sagittal plane by an average on approximately 40°.8 As such the flexion extension axis of the elbow is not parallel to the coronal plane but is internal rotated by approximately 14°.9 (Fig. 3) This has resulted in the difference in the carrying angle when the elbow moves from flexion to extension.10,11 The carrying angle is approximately 10–15° in male and 15–20° in female.6 The flexion extension axis of the humerus has been defined to pass from the geometric centres of the trochlea and the capitellum.12 Clinically the trans-epicondylar axis approximates the actual flexion extension axis of the elbow and can be used as a guide.13
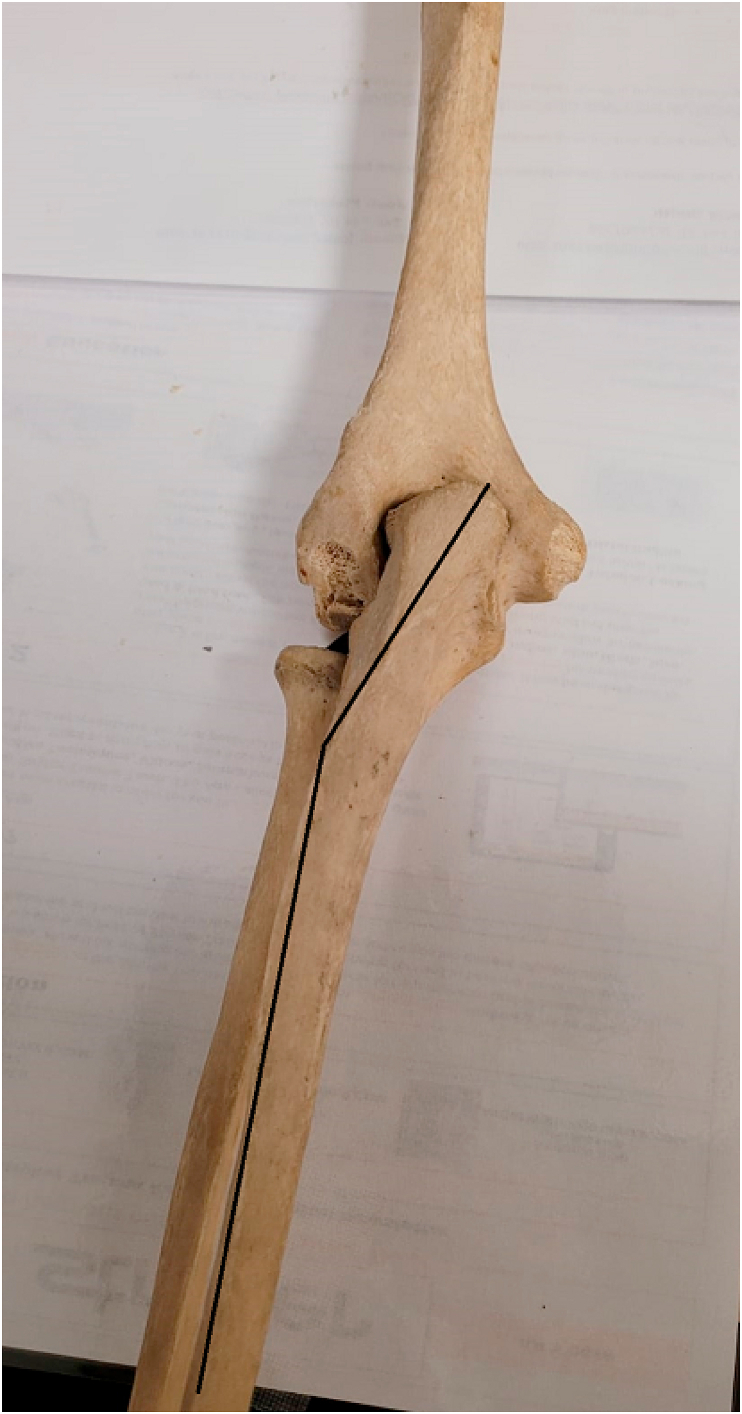
Fig. 1.
Showing apex posterior, anterior angulated distal humerus on sagittal plane with the capitellum flexed anteriorly by approximately 30–40°. Centre drill hole on the capitellum is the site of origin of the lateral collateral ligament complex.
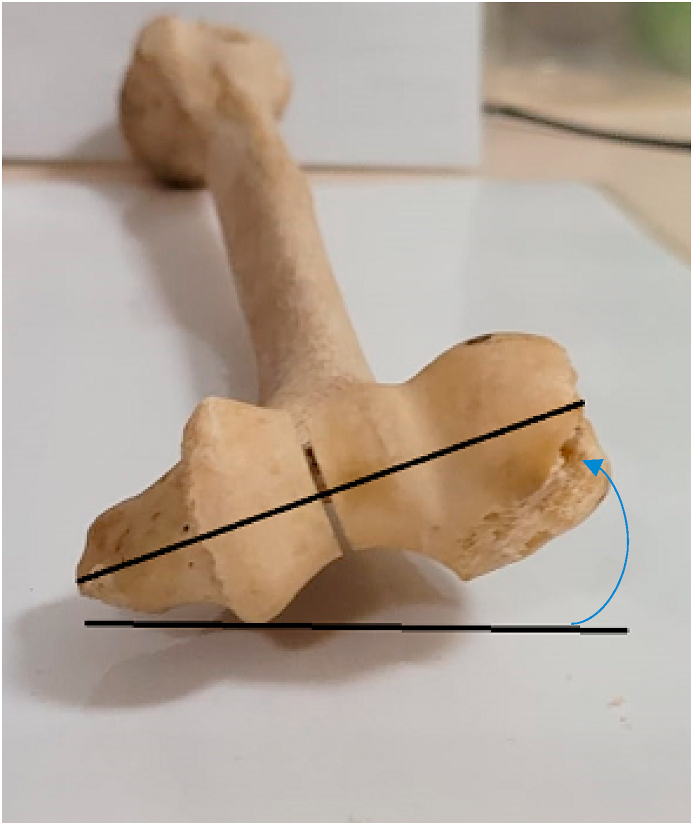
Fig. 2.
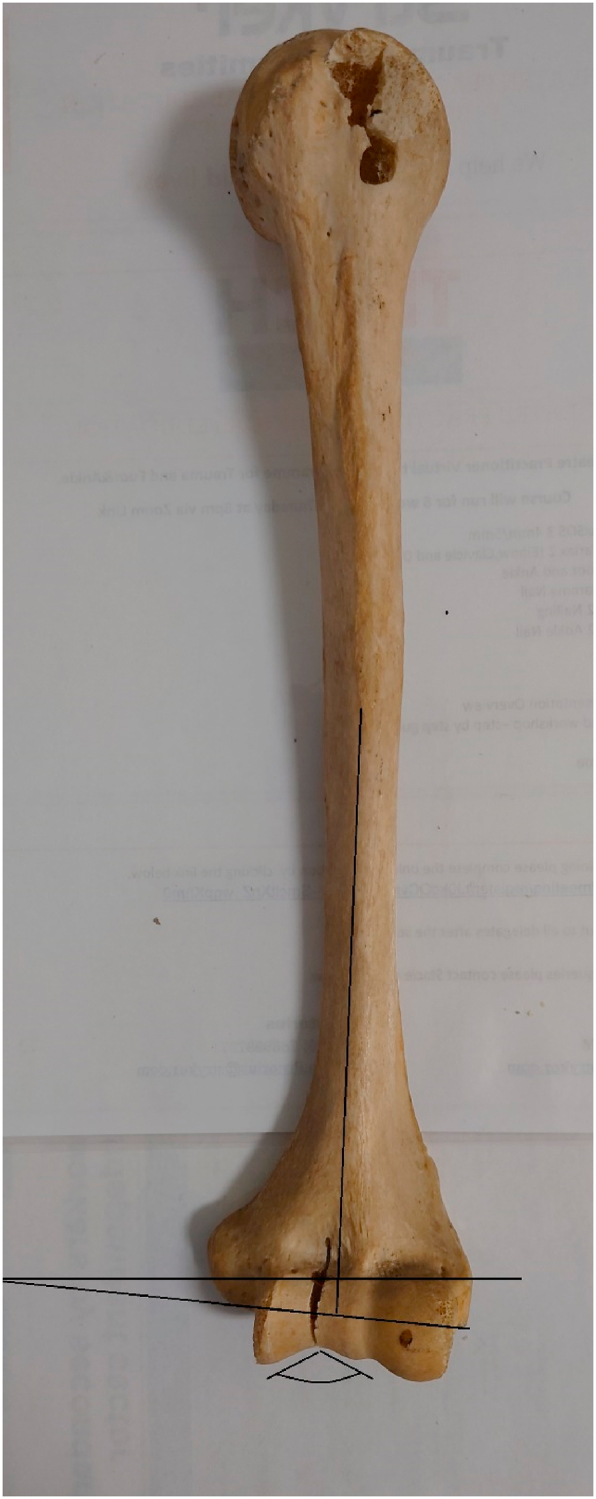
Showing the valgus angulation of articular segment relative to the shaft and the trochlear notch angle (angulated line), of average 142°.
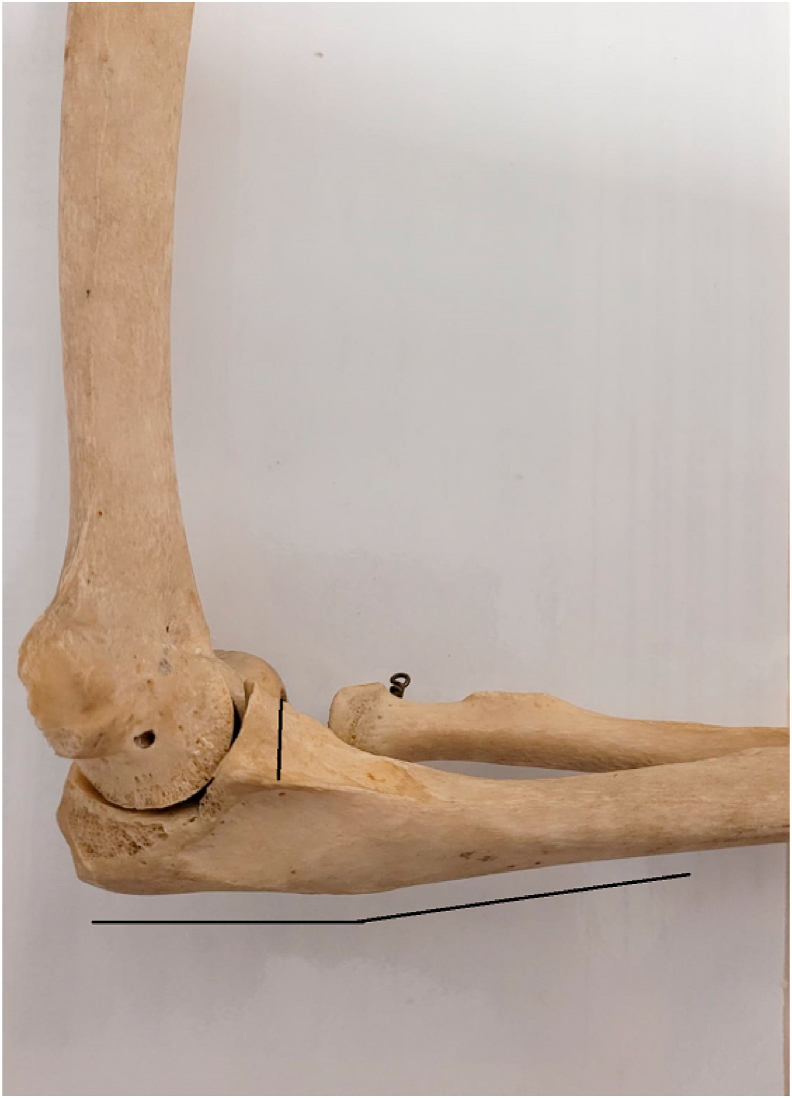
Fig. 3.
The distal humeral articular segment and the trans-epicondylar line (oblique line) are internally rotated (arrow) relative to the posterior flat surface of the humeral shaft (horizontal line).
The capsule and collateral ligaments
The elbow capsule extends from proximal to the radial and coronoid fossa anteriorly and olecranon fossa posteriorly and attach to the anterior margin of the coronoid and to the annular ligaments and articular margin of the sigmoid notch posteriorly. The fibre of anterior elbow capsule had been shown14 to run in 3 distinct pattern and hence described as 3 bands, namely the anterolateral band originating from the lateral supracondylar ridge to the annular ligament; the anteromedial band from superior medial trochlear ridge to the annular ligament and the anterior transverse band crossing the elbow in a medial to lateral direction from the central and inferior-anterior trochlear ridge to the anteromedial annular ligament and the coronoid tip. Similar pattern of distinct bands was also observed in the posterior capsule. The facts that these bands showed different fibre orientations suggested that they play an important but undefined role in elbow joint strain and stability. In fact, a consistent distribution pattern of articular sensory receptors was observed in the anterior elbow capsule.15
The medial and lateral collateral ligament of the elbows had been classified as the primary stabiliser of the elbow. These ligaments are thickened capsule and appeared as a more distinctive structure from the adjacent capsular structure. The medial collateral ligament (MCL) has been described as consisting of three components: the anterior bundle, the posterior bundle, and the transverse ligament.16 The most important component, the anterior bundle of MCL, originates from the anteroinferior surface of the medial epicondyle and inserts onto the anteromedial aspect of the coronoid process, the sublime tubercle (Fig. 4).
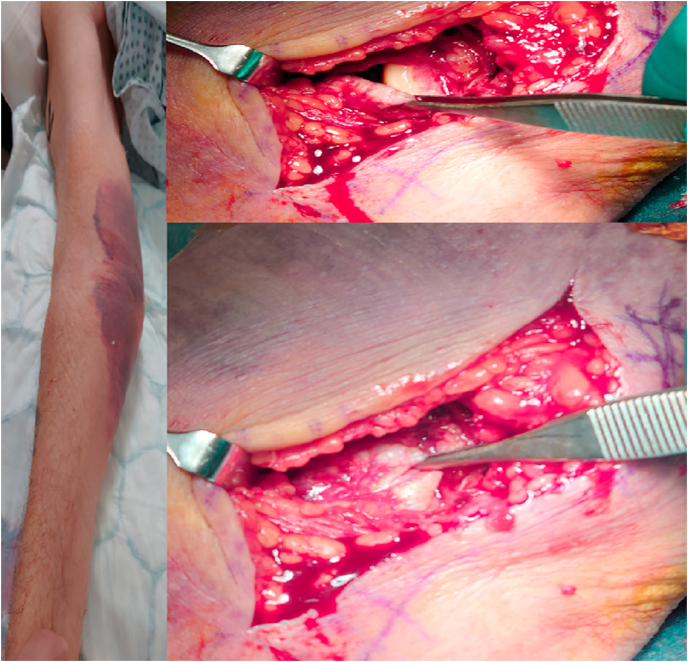
Fig. 4.
Showing MCL rupture from its attachment at the inferior medial epicondyle in a patient with posteromedial elbow dislocation. The forceps is holding the ruptured ligament exposing the origin in top right photo and opposition of the ligament back to the origin in the bottom right photo.
The lateral collateral ligament (LCL) complex consists of four components, namely the radial collateral ligament, the lateral ulnar collateral ligament, the annular ligament, and the accessory collateral ligament. The annular ligament attaches to the anterior and posterior margins of the lesser sigmoid notch. The remaining LCL complex collectively originates along the inferior surface of the lateral epicondyle (Fig. 5). The lateral ulnar collateral ligament inserted into the supinator crest and form a hammock behind the radial head to prevent varus and posterolateral instability.17 The radial and accessory collateral ligaments insert into the annular ligament and helps to stabilizes the radial head.
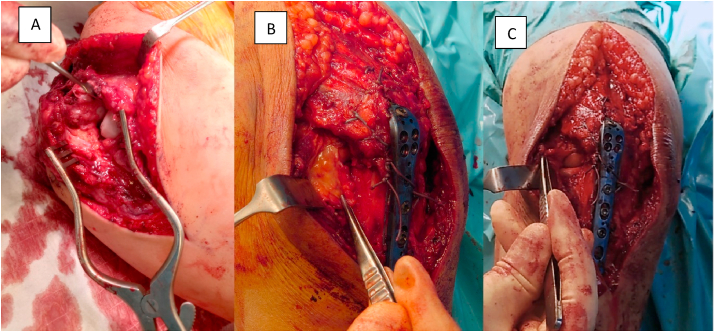
Fig. 5.
Showing rare rupture of the LUCL from its attachment to the supinator crest(A). forceps holding the ruptured ligament(B), reflected ligament revealing the radial head and capitellum (C).
The anatomy of proximal ulna
The proximal ulna has a complex anatomy. It has been shown to have a dorsal angulation in sagittal plane (PUDA),18 a varus angulation in coronal plane and a torsional angulation in the axial plane. Restoring the anatomy of this complex 3-dimensional angulation of the ulna is important especially in fixation of Monteggia or transolecranon fracture dislocation.18
Rouleau et al.2 showed that the PUDA (Fig. 6) was present in 96% of the radiographs of Caucasian cadavers (n = 50). The average PUDA was reported as 5.7° (range, 0.2°–11.8°; SD, 2.4°) and was located at an average of 47 mm distal to the olecranon tip. Although some interobserver variation and methodological difference may account for the reported difference, different range of PUDA for different population had been reported in the literature.18, 19, 20 The distances from the tip of olecranon to the apex of the PUDA had been reported to range between 45.2 mm and 86.3 mm.2,7
Fig. 6.
Showing the PUDA (horizontal lines); vertical line showing the coronoid height with the sublime tubercle at the bottom of the line.
The PUDA was shown to correlated to the range of motion of the elbow.21 Elbows with a smaller PUDA (<4.9°) had been shown to have significantly greater terminal extension (mean of 4.2°) but similar terminal flexion compared with elbow with larger PUDA.
The proximal ulna has varus angulation (tip of the apex pointing radially) (Fig. 7). The point of angulation from the tip of olecranon ranges from 73.7 to 85.4 mm .3,10,22 In a Turkish cohort, the varus angulation was found 9.3° ± 2.2° (range 4°–15°) and the varus angulation point was 73.7 ± 6.8 mm (range 59.9–91 mm) from the tip of olecranon.,3 Slight variation in varus angulation has been reported by various authors using the slightly different methodology and different ethnic cohort. The average value ranges from 8.48° to 17.7°.3,5,6,23,24 Mark Morrey of the Mayo Clinic, USA has described it as the “rule of 8” meaning 8° radial bow approximately 8 cm from the tip of the olecranon (personal communication). The apex of varus angulation and the dorsal angulation expressed as distance from the tip of olecranon can only be served as a reference. It would be more useful to express this as a ratio to the total length of ulna. Yong et al. reported the average length ratio of the dorsal and varus angulation apex to the total ulnar length was 26.4% (range 19.8–30.7%) and 32.7% (range 27.5–37.5%), respectively5 whilst Hopf et al. reported these ratio as 23.2% (PUDA) and 18.9% (VA).6 Wang et al. reported the tip-apex ratio for PUDA was 0.29 (range, 0.23–0.33).12 These apices of angulation were all situated distal to the lesser sigmoid notch. This location of the varus angulation may have an impact on the biomechanics of tension band wiring. The line of pull of the tensile triceps force will not be straight if the distal osseous hole for passing the tension band wire is distal to the apex of angulation and potentially creating a displacing sliding force: implying that the distal osseous hole should not be more than 7–8 cm from the tip of the olecranon.
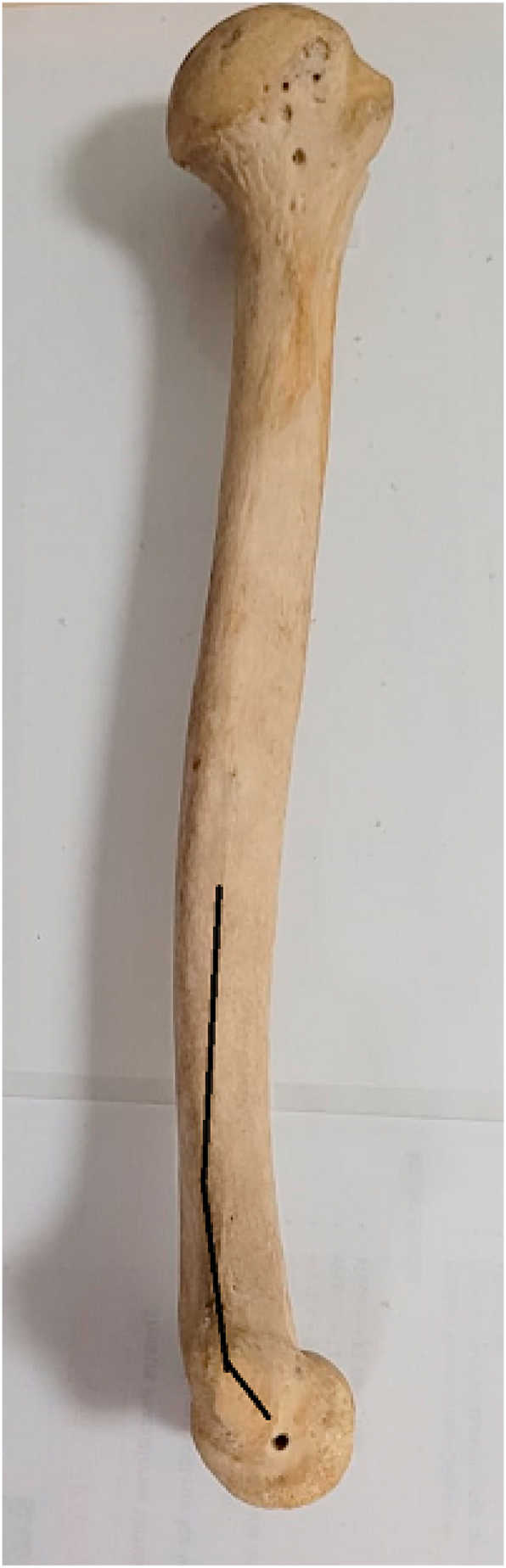
Fig. 7.
Showing varus angulation of the proximal ulna.
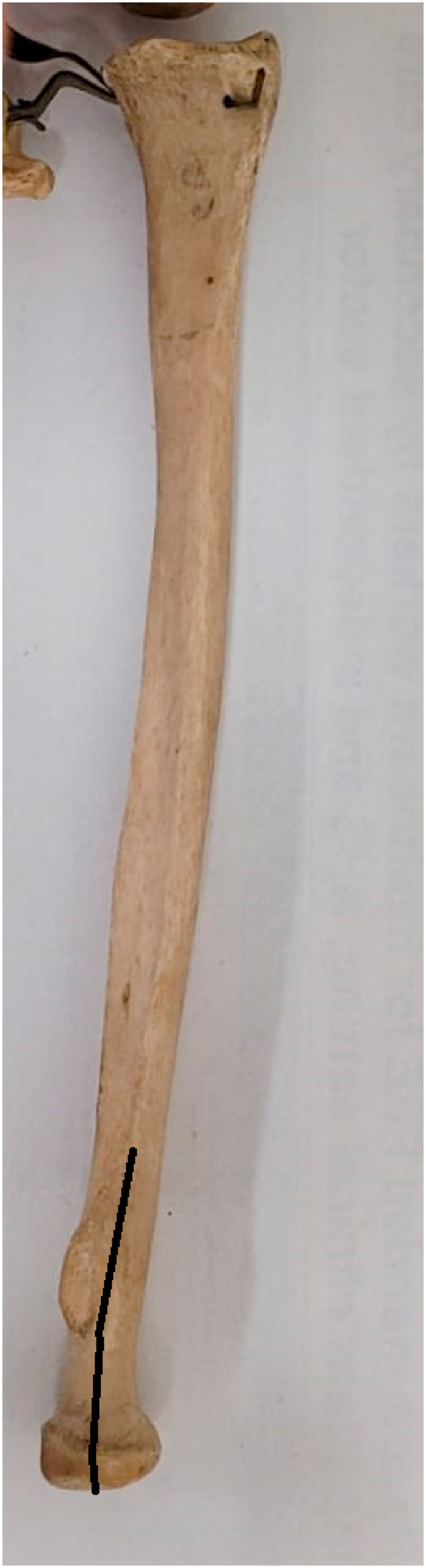
The olecranon of the proximal ulna is also rotated externally relative to the distal ulnar shaft and this pertained to the proximal ulna torsional angle (Fig. 8). Yong at el7 described that the flat posterior surface of the olecranon is rotated externally towards the radius relative to the flat subcutaneous border of the distal ulna. Depending on the method of measurement, the torsional angle varies from a mean of 11.1°–22.5°.4,7
Fig. 8.
Showing torsional angle of the olecranon relative to the coronoid.
The mean width of the olecranon bare area (lacking articular cartilage) was 0.53 cm (range, 0.13–0.97 cm), and the mean distance from the triceps insertion to the corresponding area of the bare spot on the dorsal cortex was 2.1 cm (range, 1.4–2.5 cm).25 Over-compression of the olecranon bare area during fracture reduction to obtain articular cartilage reduction can result in a narrowed trochlear fossa and incongruent radius of curvature.
The medullary canal diameter of ulna tapers to its narrowest diameter at approximately just after mid shaft and then widen again. In a CT study of the proximal ulna, Hopf et al. reported the smallest diameter of the medullary canal was 4.2 mm (SD 1.1 mm) which was located at 141.3 mm (SD 19.7 mm) from the olecranon tip in a German cohort with an average ulna length of 253.6 mm (SD 19.9 mm).8
On the other hand, Wang et al. reported that the medullary canal is not circular but elliptical with the mean inner diameters of the medullary canal at the apex of the varus angulation 0.71 cm (range, 0.42–1.25 cm) for medial-lateral and 0.74 cm (range, 0.50–1.24 cm) for antero-posterior dimension (10).
Functional anatomy of the proximal ulna in relationship to elbow stability
The proximal ulna has a few important osseous structures which play important roles in elbow stability. The olecranon and coronoid processes comprise the greater sigmoid notch of the ulna, which articulates with the trochlea of the distal humerus. The olecranon blocks the anterior translation of the ulna with respect to the distal humerus, whereas an intact coronoid process resists posterior translation of the proximal ulna in extension beyond 30° or greater. The posterior olecranon height measured from the posterior cortex of the olecranon to the tip was reported to be 24.6 ± 2.6 mm (range 19.4–29 mm) in a Turkish study.4 An et al. showed that removal of more than 25% of the proximal olecranon resulted in increased instability during varus rotational stress whereas removal of 50% of the olecranon can result in significant loss of stability in anterior or volar displacement of the ulna.26
The coronoid is a triangular bone arising from the anterior proximal ulna. The coronoid process is an interesting osseous structure as it is intimately related to 3 important anatomical structures. On the medial side, the sublime tubercle arises from the medal coronoid whereas on the lateral side, the coronoid hosts the lesser sigmoid notch and the supinator crest, which arises immediately inferior and distal to the lesser sigmoid notch. The sublime tubercle and the supinator crest are the sites of attachment of the medial and lateral collateral ligament complexes, respectively. Hence the coronoid plays an important role in the stability of the elbow. Bernard Morrey of the Mayo Clinic, USA describes it as ‘the most valuable piece of real estate in the elbow’ (personal communication). The coronoid process has been divided into anteromedial facet, anterolateral facet and the base. The “tip” of the coronoid, which is intra-articular in location, is the apex of the process where the anteromedial and anterolateral facet meets. Understanding the anatomy of the coronoid is important to appreciate various classification and management of coronoid fractures. Doornberg and Ring had described the involvement of different anatomical area of the coronoid with different mechanism of injury.27 The large fractures of the coronoid process are associated with anterior and posterior olecranon fracture–dislocations, small transverse fractures are associated with terrible-triad injuries, and anteromedial facet fractures are associated with varus posteromedial rotational instability pattern injuries.
The coronoid process height, with its base defined by the trough of the trochlear notch and the slope change of the distal coronoid process, is about 15 mm and was 42% of the ulnar height.28 The olecranon-coronoid angle ranged between 33° and 38°. The capsule of the elbow joint inserts approximately 1.9 mm distal to the osseous edge of the tip of coronoid. The total cartilage and bone thickness proximal to the capsule was 4.7–5.9 mm.29,30 The anterior capsule of the elbow joint had a substantial attachment at the radial side (11.9 ± 2.2 mm) of the coronoid compared to that at the ulnar side (6.1 ± 1 mm).16 The O'Driscoll classification of coronoid tip fracture divide the tip fracture into subtype 1 of tip fractures involving ≤2 mm of the coronoid, and subtype 2 of tip fractures involving >2 mm.31 This subtype classification essentially distinguish the inclusion of capsular attachment in the fracture. The basilar fracture on the other hand was classified as including at least 50% of the coronoid height which would include the broad attachment of the capsule and thus adequately repaired basilar fracture would add to stability of the elbow. In fact, histological studies had shown that dense slow adapting Ruffini corpuscles and fast acting Pacinian corpuscles are found mainly in the anterior elbow capsule.32,33 These mechanoreceptors detect changes in joint pressure, regulate muscle reflexes and control acceleration and joint motion which in combination play an important role in neuromodulation of the elbow joint stability. 34 Adams et al.35 identified an oblique ‘‘anterolateral’’ type fractures involving the anterolateral portion of the coronoid and the lesser sigmoid notch. This type of fracture usually occurs with posterolateral valgus instability and elbow dislocation, sometimes associated with a radial head fracture and/or “terrible triad” injury. The anterolateral oblique fracture may represent the more severe spectrum of the tip fracture and Adams et al. recommended fixation of the anterolateral facet if the fragment is more than 5 mm.36 A modified Regan-Morrey classification was introduced based on the study from Adams et al.,30,37 a separate oblique subtype which involve either the anterolateral facet with the lesser sigmoid (type IV-L) or anteromedial facet with the sublime tubercle (type-M).
Using 3D CT to compare articular facet configuration, Kataoka et al. showed that the tip of olecranon mimics 89.2 ± 6.9% of the articular surface of the coronoid whereas the proximal and lateral radial head covers 80.3% ± 11.2% and 81.5% ± 11.0% of the coronoid articular surface, respectively.38 Hence these are potential source for the autograft reconstruction of comminuted coronoid fracture. Alolabi et al. showed that reconstruction of the coronoid using the tip of the ipsilateral olecranon was an effective method for restoring normal kinematics over a range of elbow motion from 20° to 120° in a cadaveric model of an elbow with a 40% coronoid deficiency.39
Anatomy of the proximal radius
The radial head has complex anatomy, and it has been described as circular or ellipsoidal with a 1–2 mm depression in the mid portion defined as the dish or the fovea radialis.40,41 The radial head articulates with the capitellum proximally and the lesser sigmoid notch of the ulna medially.
Two third of circumference of the radial head has thickened articular cartilage42 as compared to non-articulating one third of the rim (113°) which has thin cartilage. With the radius in neutral position, the cartilage is thickest in the posteromedial region43 although the variation within the rim is small (range, 0.76–1.73 mm The area bounded by the radial styloid and Lister tubercle correspond to the non-articular portion of the radial head. Another useful anatomical landmark is the bicipital tuberosity which is offset from the radial head and is situated opposite the non-articular portion of radial head.44
The concave surface of the radial head articulates with the convex surface of the humeral capitellum acting as a buttress, providing stability by the concavity compression mechanism and tensioning of the lateral collateral ligament complex, and resisting external rotation at the ulnohumeral joint.45 The concave proximal surface of the radial head has been described to have 3 diameters: namely the maximum, minimum and dish diameter (Fig. 9). The maximum and minimum diameters pertained to the ellipsoidal shape of the radial head. However, the difference in the diameter is only in the range of 1–2 mm43,46 and the mean diameter had been reported to be approximately between 20 and 29 mm.43,46, 47, 48 The difference is probably due to a combination of difference methodology in measurement and ethnic or gender difference. The dish diameter pertained to the deepened dish on the concave surface. The dish is circular whereas the whole radial head circumference is elliptical. Hence the fovea radialis (the centre of the dish) which articulates with the capitellum is not in the centre of the radial head circumference but is offset.43 The axial view revealed that the fovea radialis was backward eccentric in full supination and forward eccentric in full pronation. In an elliptical radial head, the orientation of the long axis is perpendicular to the radial notch with the forearm in neutral rotation.49 The radial head does not rotate precisely around a specific centre in full pronation and supination due to this “non-circular shape”.48,50 With pronation the radial head translates anteriorly, placing the posterior annular ligament under tension while in supination the radial head translates posteriorly, placing the anterior portion of the annular ligament under tension. Altering this offset with a circular radial head replacement has a significant effect on the axial rotation of the ulna during flexion-extension and rotation of the ulna during gravity valgus stress were altered.51
Fig. 9.
Showing maximum and minimum diameter of the elliptical radial head.
The mean radial head height is approximately 9.8–11.89 mm.44,48,51,52 Although there is slight difference in radial head height in the anterior, posterior, radial, and ulnar aspects of the radial head, contributed by the cartilage thickness, the difference is insignificant.51 Van Riet et al. showed that the length of the lesser sigmoid notch is a reliable predictor of radial head height.53 The radial neck height measured from the radial tuberosity is around 13 mm.54
The angle between the neck and the diaphysis is around 152–178°48,55,56; slight difference reported in angle for circular and elliptical head is due to the shape of the radial head.48 (Fig. 10) The radial head is also inclined by an average of 2.5° relative to the neck.50 Finally, the ulnar notch of the proximal radius internally rotates relative to the radial notch of the proximal ulna with the forearm in neutral rotation. This forms a torsional angle with an average value of 53.5°.
Fig. 10.
Showing the neck-shaft and neck-head angles.
Conclusion
The anatomy of the elbow joint had been studied extensively over the last 2 decades. The increased understanding of the anatomy and contribution of the anatomical structures to the elbow biomechanics had enabled surgeons to improve the results of surgical reconstruction and fracture fixation.
References
- 1.Schwarz G.M., Zak L., Hirtler L., Wozasek G.E. Anatomical considerations of intramedullary humeral nailing and lengthening. J Clin Med. 2020 Mar 16;9(3):806. doi: 10.3390/jcm9030806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Brownhill J.R., King G.J., Johnson J.A. Morphologic analysis of the distal humerus with special interest in elbow implant sizing and alignment. J Shoulder Elbow Surg. 2007;16(3 Suppl):S126–S132. doi: 10.1016/j.jse.2006.01.018. [DOI] [PubMed] [Google Scholar]
- 3.Goldberg S.H., Omid R., Nassr A.N., Beck R., Cohen M.S. Osseous anatomy of the distal humerus and proximal ulna: implications for total elbow arthroplasty. J Shoulder Elbow Surg. 2007;16(3 Suppl):S39–S46. doi: 10.1016/j.jse.2006.01.011. [DOI] [PubMed] [Google Scholar]
- 4.Miyasaka K.C. Anatomy of the elbow. Orthop Clin N Am. 1999;30(1):1–13. doi: 10.1016/s0030-5898(05)70057-2. [DOI] [PubMed] [Google Scholar]
- 5.Sabo M.T., McDonald C.P., Ng J., Ferreira L.M., Johnson J.A., King G.J. A morphological analysis of the humeral capitellum with an interest in prosthesis design. J Shoulder Elbow Surg. 2011;20(6):880–884. doi: 10.1016/j.jse.2011.01.007. [DOI] [PubMed] [Google Scholar]
- 6.Giannicola G., Scacchi M., Sedati P., Gumina S. Anatomical variations of the trochlear notch angle: MRI analysis of 78 elbows. Musculoskelet Surg. 2016;100(Suppl 1):89–95. doi: 10.1007/s12306-016-0407-2. [DOI] [PubMed] [Google Scholar]
- 7.Goldfarb C.A., Patterson J.M., Sutter M., Krauss M., Steffen J.A., Galatz L. Elbow radiographic anatomy: measurement techniques and normative data. J Shoulder Elbow Surg. 2012;21(9):1236–1246. doi: 10.1016/j.jse.2011.10.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Simanovsky N., Lamdan R., Hiller N., Simanovsky N. The measurements and standardization of humerocondylar angle in children. J Pediatr Orthop. 2008;28(4):463–465. doi: 10.1097/BPO.0b013e31817445ff. [DOI] [PubMed] [Google Scholar]
- 9.Sabo M.T., Athwal G.S., King G.J. Landmarks for rotational alignment of the humeral component during elbow arthroplasty. J Bone Joint Surg Am. 2012 Oct 3;94(19):1794–1800. doi: 10.2106/JBJS.J.01740. [DOI] [PubMed] [Google Scholar]
- 10.Golden D.W., Jhee J.T., Gilpin S.P., Sawyer J.R. Elbow range of motion and clinical carrying angle in a healthy pediatric population. J Pediatr Orthop B. 2007;16(2):144–149. doi: 10.1097/BPB.0b013e328010fcf2. [DOI] [PubMed] [Google Scholar]
- 11.An K.N., Morrey B.F., Chao E.Y. Carrying angle of the human elbow joint. J Orthop Res. 1984;1(4):369–378. doi: 10.1002/jor.1100010405. [DOI] [PubMed] [Google Scholar]
- 12.Bottlang M., O'Rourke M.R., Madey S.M., Steyers C.M., Marsh J.L., Brown T.D. Radiographic determinants of the elbow rotation axis: experimental identification and quantitative validation. J Orthop Res. 2000;18:821–828. doi: 10.1002/jor.1100180521. [DOI] [PubMed] [Google Scholar]
- 13.Tan Z., Ng Y., Yew A., Morrey B., Sen H.T. Geometric accuracy of elbow flexion extension(F-E) axis based on approximation to the epicondylar axis. Orthopaed Proc. 2014;99B Suppl 8. [Google Scholar]
- 14.Reichel L.M., Morales O.A. Gross anatomy of the elbow capsule: a cadaveric study. J Hand Surg Am. 2013;38:110–116. doi: 10.1016/j.jhsa.2012.09.031. [DOI] [PubMed] [Google Scholar]
- 15.Kholinne E., Lee H.J., Deslivia M.F. Neuroanatomical distribution of sensory receptors in the human elbow joint capsule. Shoulder Elbow. 2019;11(4):300–304. doi: 10.1177/1758573218760245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Floris S., Olsen B.S., Dalstra M., Søjbjerg J.O., Sneppen O. The medial collateral ligament of the elbow joint: anatomy and kinematics. J Shoulder Elbow Surg. 1998;7(4):345–351. doi: 10.1016/s1058-2746(98)90021-0. [DOI] [PubMed] [Google Scholar]
- 17.O'Driscoll S.W., Bell D.F., Morrey B.F. Posterolateral rotatory instability of the elbow. J Bone Joint Surg Am. 1991;73(3):440–446. [PubMed] [Google Scholar]
- 18.Totlis T., Anastasopoulos N., Apostolidis S., Paraskevas G., Terzidis I., Natsis K. Proximal ulna morphometry: which are the "true" anatomical preshaped olecranon plates? Surg Radiol Anat. 2014;36(10):1015–1022. doi: 10.1007/s00276-014-1287-5. [DOI] [PubMed] [Google Scholar]
- 19.Beşer C.G., Demiryürek D., Özsoy H. Redefining the proximal ulna anatomy. Surg Radiol Anat. 2014;36(10):1023–1031. doi: 10.1007/s00276-014-1340-4. [DOI] [PubMed] [Google Scholar]
- 20.Puchwein P., Schildhauer T.A., Schöffmann S., Heidari N., Windisch G., Pichler W. Three-dimensional morphometry of the proximal ulna: a comparison to currently used anatomically preshaped ulna plates. J Shoulder Elbow Surg. 2012;21(8):1018–1023. doi: 10.1016/j.jse.2011.07.004. [DOI] [PubMed] [Google Scholar]
- 21.Rouleau D.M., Canet F., Chapleau J. The influence of proximal ulnar morphology on elbow range of motion. J Shoulder Elbow Surg. 2012;21(3):384–388. doi: 10.1016/j.jse.2011.10.008. [DOI] [PubMed] [Google Scholar]
- 22.Wang A.A., Mara M., Hutchinson D.T. The proximal ulna: an anatomic study with relevance to olecranon osteotomy and fracture fixation. J Shoulder Elbow Surg. 2003;12(3):293–296. doi: 10.1016/s1058-2746(02)86803-3. [DOI] [PubMed] [Google Scholar]
- 23.Shi X., Pan T., Wu D., Chen R., Lin Z., Pan J. The impact of varus angulation on proximal fractures of the ulna. BMC Muscoskel Disord. 2018;19(1):103. doi: 10.1186/s12891-018-2012-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Windisch G., Clement H., Grechenig W., Tesch N.P., Pichler W. The anatomy of the proximal ulna. J Shoulder Elbow Surg. 2007;16(5):661–666. doi: 10.1016/j.jse.2006.12.008. [DOI] [PubMed] [Google Scholar]
- 25.Wang A.A., Mara M., Hutchinson D.T. The proximal ulna: an anatomic study with relevance to olecranon osteotomy and fracture fixation. J Shoulder Elbow Surg. 2003;12(3):293–296. doi: 10.1016/s1058-2746(02)86803-3. [DOI] [PubMed] [Google Scholar]
- 26.An K.N., Morrey B.F., Chao E.Y. The effect of partial removal of proximal ulna on elbow constraint. Clin Orthop Relat Res. 1986;209:270–279. [PubMed] [Google Scholar]
- 27.Doornberg J.N., Ring D. Coronoid fracture patterns. J Hand Surg Am. 2006;31(1):45–52. doi: 10.1016/j.jhsa.2005.08.014. [DOI] [PubMed] [Google Scholar]
- 28.Matzon J.L., Widmer B.J., Draganich L.F., Mass D.P., Phillips C.S. Anatomy of the coronoid process. J Hand Surg Am. 2006;31(8):1272–1278. doi: 10.1016/j.jhsa.2006.05.010. [DOI] [PubMed] [Google Scholar]
- 29.Shimura H., Nimura A., Nasu H. Joint capsule attachment to the coronoid process of the ulna: an anatomic study with implications regarding the type 1 fractures of the coronoid process of the O'Driscoll classification. J Shoulder Elbow Surg. 2016;25(9):1517–1522. doi: 10.1016/j.jse.2016.01.024. [DOI] [PubMed] [Google Scholar]
- 30.Weber M.F.V.d.L., Barbosa D.M., Belentani C. Coronoid process of the ulna: paleopathologic and anatomic study with imaging correlation. Emphasis on the anteromedial “facet”. Skeletal Radiol. 2009;38:61–67. doi: 10.1007/s00256-008-0556-y. [DOI] [PubMed] [Google Scholar]
- 31.O'Driscoll S.W., Jupiter J.B., Cohen M.S., Ring D., McKee M.D. Difficult elbow fractures: pearls and pitfalls. Instr Course Lect. 2003;52 [PubMed] [Google Scholar]
- 32.Kholinne E., Lee H.J., Deslivia M.F. Neuroanatomical distribution of sensory receptors in the human elbow joint capsule. Shoulder Elbow. 2019;11(4):300–304. doi: 10.1177/1758573218760245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Phillips D., Petrie S., Solomonow M., Zhou B.H., Guanche C., D'Ambrosia R. Ligamentomuscular protective reflex in the elbow. J Hand Surg Am. 1997;22(3):473–478. doi: 10.1016/S0363-5023(97)80015-9. [DOI] [PubMed] [Google Scholar]
- 34.Garrigues G.E., Wray W.H., III, Lindenhovius A.L., Ring D.C., Ruch D.S. Fixation of the coronoid process in elbow fracture-dislocations. J Bone Joint Surg Am. 2011;93(20):1873–1881. doi: 10.2106/JBJS.I.01673. [DOI] [PubMed] [Google Scholar]
- 35.Adams J.E., Sanchez-Sotelo J., Kallina C.F., 4th, Morrey B.F., Steinmann S.P. Fractures of the coronoid: morphology based upon computer tomography scanning. J Shoulder Elbow Surg. 2012;21(6):782–788. doi: 10.1016/j.jse.2012.01.008. [DOI] [PubMed] [Google Scholar]
- 36.Adams J.E., Steinmann S.P. Coronoid fractures: evaluation and treatment. Orthop Traumatol. 2013;27(4):250–253. [Google Scholar]
- 37.Morrey B., Sanchez Sotelo J., Morrey M. Morrey's the Elbow and its Disorders. fifth ed. Elsevier Science; 2017. Coronoid fractures; pp. 428–439. [Google Scholar]
- 38.Kataoka T., Moritomo H., Miyake J., Murase T., Sugamoto K. Three-dimensional suitability assessment of three types of osteochondral autograft for ulnar coronoid process reconstruction. J Shoulder Elbow Surg. 2014;23(2):143–150. doi: 10.1016/j.jse.2013.10.004. [DOI] [PubMed] [Google Scholar]
- 39.Alolabi B., Gray A., Ferreira L.M., Johnson J.A., Athwal G.S., King G.J. Reconstruction of the coronoid process using the tip of the ipsilateral olecranon. J Bone Joint Surg Am. 2014;96(7):590–596. doi: 10.2106/JBJS.L.00698. [DOI] [PubMed] [Google Scholar]
- 40.Captier G., Canovas F., Mercier N., Thomas E., Bonnel F. Biometry of the radial head: biomechanical implications in pronation and supination. Surg Radiol Anat. 2002;24(5):295–301. doi: 10.1007/s00276-002-0059-9. [DOI] [PubMed] [Google Scholar]
- 41.Giannicola G., Sedati P., Polimanti D., Cinotti G., Bullitta G. Contribution of cartilage to size and shape of radial head circumference: magnetic resonance imaging analysis of 78 elbows. J Shoulder Elbow Surg. 2016;25(1):120–126. doi: 10.1016/j.jse.2015.07.003. [DOI] [PubMed] [Google Scholar]
- 42.Caputo A.E., Mazzocca A.D., Santoro V.M. The nonarticulating portion of the radial head: anatomic and clinical correlations for internal fixation. J Hand Surg Am. 1998;23(6):1082–1090. doi: 10.1016/S0363-5023(98)80020-8. [DOI] [PubMed] [Google Scholar]
- 43.Yeung C., Deluce S., Willing R., Johnson M., King G.J., Athwal G.S. Regional variations in cartilage thickness of the radial head: implications for prosthesis design. J Hand Surg Am. 2015;40(12) doi: 10.1016/j.jhsa.2015.09.005. 2364-23671.e1. [DOI] [PubMed] [Google Scholar]
- 44..
- 45.Weiss A.P., Hastings H., 2nd The anatomy of the proximal radioulnar joint. J Shoulder Elbow Surg. 1992;1(4):193–199. doi: 10.1016/1058-2746(92)90013-S. Epub 2009 Feb 25. PMID: 22971623. [DOI] [PubMed] [Google Scholar]
- 46.Jensen S.L., Olsen B.S., Søjbjerg J.O. Elbow joint kinematics after excision of the radial head. J Shoulder Elbow Surg. 1999;8(3):238–241. doi: 10.1016/s1058-2746(99)90135-0. [DOI] [PubMed] [Google Scholar]
- 47.Swieszkowski W., Skalski K., Pomianowski S., Kedzior K. The anatomic features of the radial head and their implication for prosthesis design. Clin Biomech. 2001;16(10):880–887. doi: 10.1016/s0268-0033(01)00075-4. [DOI] [PubMed] [Google Scholar]
- 48.Puchwein P., Heidari N., Dorr K., Struger L., Pichler W. Computer-aided analysis of radial head morphometry. Orthopedics. 2013;36(1):e51–e57. doi: 10.3928/01477447-20121217-18. [DOI] [PubMed] [Google Scholar]
- 49.Beredjiklian P.K., Nalbantoglu U., Potter H.G., Hotchkiss R.N. Prosthetic radial head components and proximal radial morphology: a mismatch. J Shoulder Elbow Surg. 1998;(8):471–475. doi: 10.1016/s1058-2746(99)90079-4. [DOI] [PubMed] [Google Scholar]
- 50.van Riet R.P., Van Glabbeek F., Neale P.G., Bortier H., An K.N., O'Driscoll S.W. The noncircular shape of the radial head. J Hand Surg Am. 2003;28(6):972–978. doi: 10.1016/s0363-5023(03)00426-x. [DOI] [PubMed] [Google Scholar]
- 51.Shannon H.L., Deluce S.R., Giles J.W., Johnson J.A., King G.J. The effect of radial head implant shape on radiocapitellar kinematics during in vitro forearm rotation. J Shoulder Elbow Surg. 2015;24(2):258–264. doi: 10.1016/j.jse.2014.09.019. [DOI] [PubMed] [Google Scholar]
- 52.van Riet R.P., Van Glabbeek F., Baumfeld J.A. The effect of the orientation of the noncircular radial head on elbow kinematics. Clin Biomech. 2004;19(6):595–599. doi: 10.1016/j.clinbiomech.2004.03.002. [DOI] [PubMed] [Google Scholar]
- 53.Itamura J.M., Roidis N.T., Chong A.K., Vaishnav S., Papadakis S.A., Zalavras C. Computed tomography study of radial head morphology. J Shoulder Elbow Surg. 2008;17(2):347–354. doi: 10.1016/j.jse.2007.07.019. [DOI] [PubMed] [Google Scholar]
- 54.van Riet R.P., van Glabbeek F., de Weerdt W., Oemar J., Bortier H. Validation of the lesser sigmoid notch of the ulna as a reference point for accurate placement of a prosthesis for the head of the radius: a cadaver study. J Bone Joint Surg Br. 2007;89(3):413–416. doi: 10.1302/0301-620X.89B3.18099. [DOI] [PubMed] [Google Scholar]
- 55.Van Riet R.P., Van Glabbeek F., Neale P.G. Anatomical considerations of the radius. Clin Anat. 2004;17(7):564–569. doi: 10.1002/ca.10256. [DOI] [PubMed] [Google Scholar]
- 56.Koslowsky T.C., Beyer F., Germund I., Mader K., Jergas M., Koebke J. Morphometric parameters of the radial neck: an anatomical study. Surg Radiol Anat. 2007;29(4):279–284. doi: 10.1007/s00276-007-0206-4. [DOI] [PubMed] [Google Scholar]