Abstract
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), which causes COVID-19, has spread around the globe with remarkable consequences for the health of millions of people. Despite the approval of mRNA vaccines to prevent the spread of infection, long-term immunity must still be monitored. Targeting and modifying virus receptor binding regions to activate B cell receptors (BCRs) is a promising way to develop long-term immunity against SARS-CoV-2. After the interaction of antigens, BCRs undergo series of signal transduction events through phosphorylation of immune receptor tyrosine activation motifs (ITAMs) to produce neutralizing antibodies against pathogens. BCRs intricate entity displays remarkable capability to translate the external mechanosensing cues to reshape the immune mechanism. However, potential investigations suggesting how SARS-CoV-2 specific B cells respond to mechanosensing cues remain obscure. This study proposes a sophisticated hypothesis explaining how B cells isolated from the CP of SARS-CoV-2 infected patients may undergo a triggered series of B cell activation, BCR dynamics, proximal signalling, and antibody production on PDMS-embedded in-vitro antigen-presenting structures (APCs). These studies could provide detailed insights in the future for the development of structural and therapeutic entanglements to fight against pathogens.
Keywords: BCR, Mechanotransduction, SARS-CoV-2, Vaccine entanglements, Antibody production, BCR dynamics, BCR spatiotemporal dynamics
Introduction
The novel coronavirus severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) is a positive-sense single-stranded RNA virus identified as the causative agent of COVID-19 [1]. Similar to the other viruses of the coronaviridae family, the virus principally infects respiratory airways, exhibiting symptoms ranging from mild respiratory infections to severe acute respiratory syndrome [2], [3]. Long-term effects of the virus may result in organ failure in some patients, ultimately leading to death [4]. Long incubation periods and the asymptomatic nature of SARS-CoV-2 make the diagnosis of infection challenging and may contribute to transmission [5], [6]. The approval of anti-viral drugs such as remdesivir, monoclonal antibodies against S protein, and Pfizer and BioNTech's mRNA vaccines provide a pathway to mitigate the spread and disease severity [7]. However, long-term immunity is still essential to prevent the continued spread of COVID-19 infection and re-establish normal socio-economic activities [8], [9], [10].
During SARS-CoV-2 infection, B cells may contribute significantly to producing antibodies through delicate interactions of BCRs with antigens [11]. Following exposure of SARS-CoV-2 antigens through natural infection or with the vaccine, intricate BCR-antigen interactions at B cell membrane results in phosphorylation of immune receptor tyrosine activation motifs (ITAM) interlinked (Igα, β) domains [12], carried through underlying kinases (pLyn, pSyk) [12]. These activities result in the onset of series of events, including cellular proliferation [13], [14], differentiation of B cells into plasma and memory B cells [15], [16], isotype antibody switching, maturation, and production of antibodies to combat infection [14]. Consequently, mechanosensing transduced through BCRs could be used as an alternative strategy to induce long-term immunity against COVID-19.
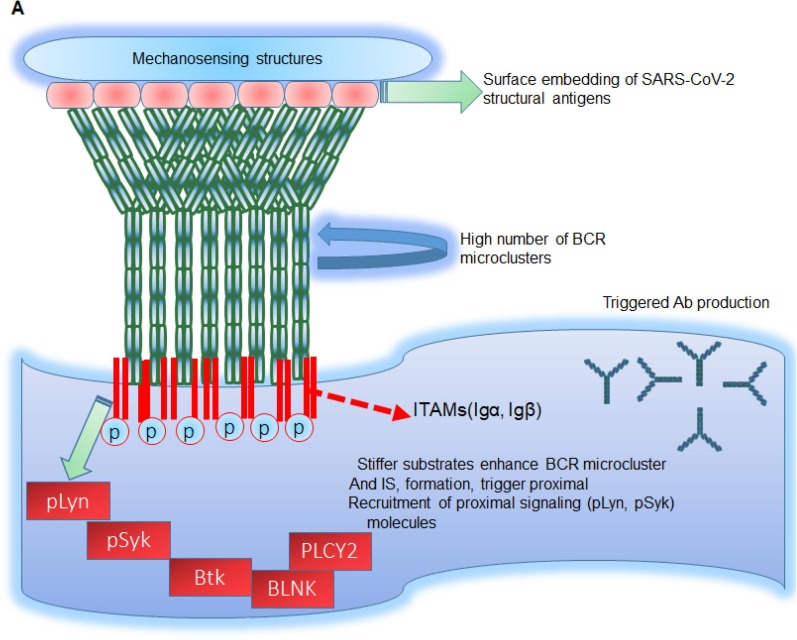
Although, potential investigations regarding B cells and subset (Follicular, marginal zone B cells) counts during SARS-CoV-2 infection have been illustrated [16]. However, studies to better decipher the mechanism of how B BCRs of SARS-CoV-2 specific patient's B cells respond to SARS-CoV-2 antigens and proximal signaling has attained limited attention. This study proposes a novel role for SARS-CoV-2 specific B cells in investigating BCR signaling, mechanoresponsiveness, spatiotemporal dynamics, and underlying signaling cascade events on antigen embedded mechanosensing APCs. Interestingly, these coherent investigations could trigger antibody production events in the future that may be helpful in the production of vaccines providing long-term immunity. Additionally, in the future, these mechanosensing entanglements may be used in conjunction with direct structural therapeutics. This study also highlights a sequential methodology to translate the proposed hypothesis into reality (Fig. 1 ).
Fig. 1.
BCRs surface interaction with SARS-CoV-2 glycoproteins triggers the humoral immune response. BCRs microcluster and immunological synapse (IS) formation are two critical events in the initiation of B cell activation. Following the interaction of BCRs with SARS-CoV-2 structural antigens (RBD, envelope proteins) embedded on PDMS mechanosensing structures, dramatic crosslinking of BCRs occurs, resulting in phosphorylation of immune receptor tyrosine activation motifs (ITAMS) flanked (Igα, Igβ) domains via underlying enzymes pLyn. These proximal sites are followed by phosphorylated spleen tyrosine kinas (pSyk), which provides a docking site for Burton tyrosine kinase (Btk), resulting in site-specific aggregation of adaptor proteins including BLNK and PLCγ-2 to trigger NAbs production to combat infection.
Theory and background
B cell activation and BCR-mediated signalling have been investigated using elastomers fabricated from polydimethylsiloxane (PDMS) with varying rigidity properties. [17], [18], [19]. Innate and adaptive immune cells retain a sophisticated mechanism to sense the minute external mechanosensing features [20], [21], and in response, generate efficient chemical signals to reshape downstream series of events [12]. Interestingly, PDMS and PA moulded in-vitro fabrications have been used in various studies to capture cellular properties such as activation [12], [22], cytoskeleton dynamics [23], and membrane-proximal recruitment of signalling molecules in B cells immunological synapse (IS) [17], [24], [25], [26]. On exterior micropillar topographies, similar speculations have been used to explore perforin and granzyme secretion as well as TCR activation at the Ag-TCR contact interface periphery [27] (Table 1 ) [27]. Similar mechanistic perturbations have been employed previously to investigate cellular locomotion of innate and adaptive immune cells [28], their polarity and differentiation, and cellular survival events [29], [30], [31]. Nevertheless, using the strategies mentioned earlier, a triggered level of NAbs could be achieved by instructing B cells on mechanosensing featured topographies.
Table 1.
Several PDMS/PA fabricated elastomers have been implemented to unravel BCR signalling, antibody production, proximal signalling, cellular proliferation, class switching, TCR immunological synapse (IS) formation, and other pathways such as perforin and granzyme secretion at TCR-APCs contact interface junctional periphery.
| Mechanosensing structure | Type of cells | Principle and mode of investigations | References |
|---|---|---|---|
| PDMS/PA elastomers | B and T cells | To investigate B cell receptor signalling, antibody production, and underlying pathways | [22], [25], [37] |
| Thick and thin micropillars | T cells | To dissect TCR formation, perforin, and granzyme secretion at TCR-APCs contact interface junction | [27] |
| PDMS coated beads | B cells | To investigate traction force generation and to dissect signalling studies | [38], [39] |
| Subcellular nano ridges | B cells | To analyze BCR signalling, F-actin dynamics, and calcium influx response in B cells | [23] |
| Ligands presenting PA gels | B and T cells | To analyze physiological events including cytokine secretion through naïve T cells at TCR-APCs contact interface junction | [40] |
The sophisticated mechanism through which vaccines work reflects proximal correlation with B cells and suggests potential mechanistic capability describing how BCR undergoes signal transduction events to balance the immune mechanism [32]. Refashioned in-vitro APCs to achieve specific efficacious properties could be fundamental in reshaping the immune system [31]. Interestingly, following the prescribed methodologies, B cells through delicate interactions with SARS-CoV-2 structural catalogs could achieve specific mechanisms, including (1) intricate triggered production of SARS-CoV-2 specific neutralizing antibodies (nAbs), (2) BCR activation, (3) BCR dynamics on mechanistic invitro APCs, (4) triggered SARS-CoV-2 specific immune responses, (5) enhanced humoral immune responses (6). Thus, a repertoire of such mechanosensing-guided BCR signalling will not only boosts up an immune mechanism for SARS-CoV-2 but also for dengue and other pool of viruses.
Physiologically, through delicate interactions of in-vivo APCS, vaccine entanglements urge B cells to produce specific antibodies against spike protein (S), in the case of SARS-CoV-2 [33], [34]. VDJ rejoining events prompt B cells to produce neutralizing antibody repertoire [14], [35]. One of the several reasons to trigger SARS-CoV-2 specific antibody response is the onset of early diminished serum antibody titers [36]. This is an additional reason to engineer and instruct B-cells to keep on producing the required antibodies perpetually as and when they are needed.
Proposed hypothesis
There are several SARS-CoV-2 vaccines currently undergoing clinical trials, but there are few reports on how BCR recognizes SARS-CoV-2 antigens to trigger immune cascade events and antibody production. Thus, there is a dire need to conduct an in-depth investigation of the proposed issue to provide a theoretical and experimental basis for understanding how the immune system recognizes SARS-CoV-2 structural antigens and subsequent vaccine development. Indeed, a series of dynamic, transient, but well-ordered molecular events happening on the plasma membrane of the BCR membrane; however, due to these events' dynamic and transient nature, they are complicated to be studied by conventional biochemical and immunological approaches. Additionally, it is vital to generate an entire library of SARS-CoV-2 envelope protein-specific BCRs and express them on the plasma membrane of model B cell lines. Next, they must be used to study the dynamic recognition of SARS-CoV-2 specific antigen by B cells via cutting-edge, high-resolution, high-speed live-cell and single-molecule imaging techniques. Likewise, to investigate the correlation between B cell activation intensity and antibody neutralizing ability. Finally, we proposed that how the density, arrangement, and Young's modulus features of presenting matrix of the SARS-CoV-2 protein antigens affect the efficiency of B cell immune activation
How to test the hypothesis?
Using CP of SARS-CoV-2 B-cells we could could prove the proposed hypothesis in-vitro. In contrast, B cells could be isolated from healthy individuals to control and compare differences in BCR signalling, dynamics, mechanoresponsiveness, and antibody production. Moreover, BCRs from SARS-CoV-2 infected B cells can be engineered on model cell lines using the CRISPR/Cas9 system [41]. Briefly, Primary B cells from SARS-CoV-2 infected and healthy individuals could be isolated, maintained, and harvested. SARS-CoV-2 specific structural antigens could be purified and embedded on PDMS elastomers showing uniform distribution, accessibility, and modulus features. BCRs can be stained with Alexa-Flour 546 conjugated goat anti-mouse IgM Fab fragment [25]. The elastic modulus and other properties may be studied using atomic force microscopic (AFM) techniques on PDMS-mediated gels. BCRs of SARS-CoV-2 infected patients will be constructed on model cell lines like A-20 and CH-27 utilizing the CRISPR/Cas9 technology. Then, for 10–15 min, BCR-labeled primary B cells could be loaded onto PDMS in-vitro topographies. Images of B cells demonstrating contact interface will be acquired using confocal or TIRFM microscopy. Mean fluorescence intensity (MFI) and total fluorescence intensity (TFI) profile measurement will be employed to determine the threshold level of B cell activation [22], [24], [25].
Similarly, the spatiotemporal dynamics of BCRs can be captured in live-cell imaging studies using confocal flourescence microscopy and interpreted using Image-J software. Additionally, B cells could be cultured and maintained on PDMS elastomers in the presence of SARS-CoV-2 specific antigens. By cultivating and stimulating cells on PDMS-embedded elastomers, it is possible to quantify the production of antibodies specific to SARS-CoV-2 antigens.
Practical considerations
Mechanosensing in-vitro APCs [25], topographically implanted with SARS-CoV-2 structural antigens on PDMS elastomers, can be used to culture, harvest, and instruct B cells. Following BCR's interactions with SARS-CoV-2 antigens on in-vitro APCs, signal transduction events emerged through phosphorylation of BCRs interlinked ITAMs flanked Igα, Igβ domains [42], [43]. These events led to the subsequent recruitment and site specif membrane-proximal accumulation of signalling subunits and adaptor proteins to intensify the immune cascade events [12]. A mixture of several B cells and cell lines (A-20, CH-27, J55L) could be employed to teach immune responses using the methodologies as mentioned above. In this case, purified SARS-CoV-2 structural antigens could be implanted on PDMS gel initially fixed with 5% BSA material. This approach can be successfully used against SARS-CoV-2 and other pools of viruses, including Epstein Bar virus (EBV), Ebola virus, dengue virus, MERS and SARS-CoV.
It should not escape our notice that altered stiffness and rigidity features of PDMS elastomer gels, and uneven surface embedding of SARS-CoV-2, structural antigens could interfere with BCR signalling magnitude and the ultimate fate of immune cascade events [24], [25]. Although, such a scenario might create obstacles in acquiring the precise conclusion. For that reason, initially, SARS-CoV-2 developed surface density features, and comparable accessibility to antibodies should be confirmed through quantifying the mean fluorescence intensity (MFI) and total fluorescence intensity (TFI) profile. Another feature could be differential surface rigidity features of PDMS in-vitro topographies; thus, comparative stiffness evaluation could be analyzed through electro force nanoindenter.
Furthermore, in-vitro culture and maintenance of splenic primary B cells are complex. However, B cells could be stimulated with lipopolysaccharide (LPS) or SARS-CoV-2 structural antigens and subjected to in-vitro culture to decipher the antibody production aptitude better. In this case, B cells could be manipulated to investigate antibody production using SARS-CoV-2 antigens. By using the technique mentioned above, such cells would be accessible and viable enough to produce antibodies.
Another fundamental aspect to note is an antibody-dependent enhancement (ADE), which should be well considered during anti-SARS-CoV-2 antibody production using BCRs transduced mechanotransduction pathways. ADE phenomenon has been observed in SARS-CoV-2 and some other viral infections, including dengue and respiratory syncytial virus (RSV) [44]. Although the ADE mechanism can render SARS-CoV-2 antibodies ineffective [39], it is imperative to address ADE in the context of efforts to create countermeasures against SARS-CoV-2 via the mechanotransduction pathway. Primary B cells isolated from the CP of infected individuals should be used as a model to assess the ADE phenomenon of antibodies produced. It has been investigated that people infected with SARS-CoV-2 exhibit enhanced antibody responses for a long time. Therefore, it is advisable to construct a library of SARS-CoV-2 antigens-specific BCRs from CP of infected people and fully express model B cell lines to interact with epitope-directed in-vitro mechanical perturbations. Such so produced antibodies may be competent enough.
An additional critical feature to examine is an assessment of neutralizing potential of anti-SARS-CoV-2 antibodies. Neutralizing antibodies (NAbs) block viral entry and interfere binding with their receptors (hACE-2) and thus provides protective immunity [45]. In that case, it's plausible to assess neutralizing potential of anti-SARS-CoV-2 antibodies through in-vitro neutralization tests. Furthermore, prescribed investigations would be reasonable to analyze the correlation between BCR activation intensity profile measured through calculating mean fluorescence intensity (MFI), and total fluorescence intensity (TFI) profile and neutralizing ability
Conclusion
Given advances in cutting-edge biophysical imaging tools, such as confocal and total internal reflection fluorescence microscope (TIRFM), as well as genetic and pharmacological approaches, it can be concluded that intricate BCR signalling of B cells isolated from the CP of SARS-CoV-2 infected patients could be instructed on mechanosensing featured PDMS in-vitro elastomers, externally embedding. Despite certain financial obstacles, prescribed mechanistic entanglements could be an excellent way to increase humoral immune responses not just for SARS-CoV-2 but also for MERS, SARS-CoV.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- 1.Wang X., Guo X., Xin Q., Pan Y., Hu Y., Li J., et al. Neutralizing antibody responses to severe acute respiratory syndrome coronavirus 2 in coronavirus disease 2019 inpatients and convalescent patients. Clin Infect Dis. 2020:1–7. doi: 10.1093/cid/ciaa721. Xx. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Galluccio F., Ergonenc T., Garcia Martos A., Allam A.-S., Pérez-Herrero M., Aguilar R., et al. Treatment algorithm for COVID-19: a multidisciplinary point of view. Clin Rheumatol. 2020;39:2077–2084. doi: 10.1007/s10067-020-05179-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Keam S., Megawati D., Patel S.K., Tiwari R., Dhama K., Harapan H. Immunopathology and immunotherapeutic strategies in severe acute respiratory syndrome coronavirus 2 infection. Rev Med Virol [Internet] 2020;30(5):e2123. doi: 10.1002/rmv.2123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Datta P.K., Liu F., Fischer T., Rappaport J., Qin X. SARS-CoV-2 pandemic and research gaps: Understanding SARS-CoV-2 interaction with the ACE2 receptor and implications for therapy. Theranostics. 2020;10(16):7448–7464. doi: 10.7150/thno.48076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tian Y., Rong L., Nian W., He Y. Review article: gastrointestinal features in COVID-19 and the possibility of faecal transmission. Aliment Pharmacol Ther [Internet] 2020;51(9):843–851. doi: 10.1111/apt.15731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Guo Y.-R., Cao Q.-D., Hong Z.-S., Tan Y.-Y., Chen S.-D., Jin H.-J., et al. The origin, transmission and clinical therapies on coronavirus disease 2019 (COVID-19) outbreak- A n update on the status. Mil Med Res. 2020;7(1):1–10. doi: 10.1186/s40779-020-00240-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Noor R. Developmental Status of the Potential Vaccines for the Mitigation of the COVID-19 Pandemic and a Focus on the Effectiveness of the Pfizer-BioNTech and Moderna mRNA Vaccines. Curr Clin Microbiol Rep. 2021;2 doi: 10.1007/s40588-021-00162-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bharadwaj A., Wahi N., Saxena A., Chaudhary D. Proteome organization of COVID-19: Illustrating targets for vaccine development. J Pure Appl Microbiol. 2020;14(1):831–840. [Google Scholar]
- 9.Lu L, Zhang H, Zhan M, Jiang J, Yin H, Dauphars DJ, et al. Antibody Response and Therapy in COVID-19 Patients: Significance in Vaccine Development. 2020;(August):1–20. Available from: www.preprints.org. [DOI] [PMC free article] [PubMed]
- 10.Kalita P, Padhi AK, Zhang KYJ, Tripathi T. Design of a peptide-based subunit vaccine against novel coronavirus SARS-CoV-2. Microb Pathog [Internet]. 2020;145:104236. Available from: http://www.sciencedirect.com/science/article/pii/S0882401020305234. [DOI] [PMC free article] [PubMed]
- 11.Faiq MA. B-cell engineering: A promising approach towards vaccine development for COVID-19. Med Hypotheses [Internet]. 2020;144(April):109948. Available from: https://doi.org/10.1016/j.mehy.2020.109948. [DOI] [PMC free article] [PubMed]
- 12.Feng Y, Wang Y, Zhang S, Haneef K, Liu W. Structural and immunogenomic insights into B-cell receptor activation. J Genet Genomics [Internet]. 2020 Jan 20 [cited 2020 May 1];47(1):27–35. Available from: https://www.sciencedirect.com/science/article/pii/S1673852720300072. [DOI] [PubMed]
- 13.Li J, Yin W, Jing Y, Kang D, Yang L, Cheng J, et al. The coordination between B cell receptor signaling and the actin cytoskeleton during B cell activation. Front Immunol. 2019;10(JAN):1–13. [DOI] [PMC free article] [PubMed]
- 14.Lebien T.W., Tedder T.F. B lymphocytes: How they develop and function. Blood. 2008;112(5):1570–1580. doi: 10.1182/blood-2008-02-078071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.De Biasi S, Lo Tartaro D, Meschiari M, Gibellini L, Bellinazzi C, Borella R, et al. Expansion of plasmablasts and loss of memory B cells in peripheral blood from COVID-19 patients with pneumonia. Eur J Immunol [Internet]. 2020;50(9):1283–94. Available from: https://doi.org/10.1002/eji.202048838. [DOI] [PubMed]
- 16.Quast I, Tarlinton D. B cell memory: understanding COVID-19. Immunity [Internet]. 2021;54(2):205–10. Available from: https://doi.org/10.1016/j.immuni.2021.01.014. [DOI] [PMC free article] [PubMed]
- 17.Wan Z., Liu W. The growth of B cell receptor microcluster is a universal response of B cells encountering antigens with different motion features. Protein Cell. 2012;3(7):545–558. doi: 10.1007/s13238-012-2054-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wan Z, Zhang S, Fan Y, Liu K, Du F, Davey AM, et al. B Cell Activation Is Regulated by the Stiffness Properties of the Substrate Presenting the Antigens. J Immunol [Internet]. 2013 May 1;190(9):4661 LP – 4675. Available from: http://www.jimmunol.org/content/190/9/4661.abstract. [DOI] [PubMed]
- 19.Wan Z, Chen X, Chen H, Ji Q, Chen Y, Wang J, et al. The activation of IgM- or isotype-switched IgG- and IgE-BCR exhibits distinct mechanical force sensitivity and threshold. Elife. 2015;4(AUGUST2015):1–24. [DOI] [PMC free article] [PubMed]
- 20.Zhu C, Chen W, Lou J, Rittase W, Li K. Mechanosensing through immunoreceptors. Nat Immunol [Internet]. 2019;20(10):1269–78. Available from: https://doi.org/10.1038/s41590-019-0491-1. [DOI] [PMC free article] [PubMed]
- 21.Rushdi M., Li K., Yuan Z., Travaglino S., Grakoui A., Zhu C. Mechanotransduction in T cell development, differentiation and function. Cells. 2020;9(2):364. doi: 10.3390/cells9020364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Shaheen S, Wan Z, Haneef K, Zeng Y, Jing W, Liu W. B cell mechanosensing: A mechanistic overview. Adv Immunol [Internet]. 2019 [cited 2020 May 1];144:23–63. Available from: https://www.sciencedirect.com/science/article/pii/S0065277619300306. [DOI] [PubMed]
- 23.Ketchum CM, Sun X, Suberi A, Fourkas JT, Song W, Upadhyaya A. Subcellular topography modulates actin dynamics and signaling in B-cells. Mol Biol Cell [Internet]. 2018;29(14):1732–42. Available from: https://doi.org/10.1091/mbc.E17-06-0422. [DOI] [PMC free article] [PubMed]
- 24.Wan Z., Zhang S., Fan Y., Liu K., Du F., Davey A.M., et al. B cell activation is regulated by the stiffness properties of the substrate presenting the antigens. J Immunol. 2013;190(9):4661–4675. doi: 10.4049/jimmunol.1202976. [DOI] [PubMed] [Google Scholar]
- 25.Shaheen S, Wan Z, Li Z, Chau A, Li X, Zhang S, et al. Substrate stiffness governs the initiation of b cell activation by the concerted signaling of PKCβ and focal adhesion kinase. Elife. 2017;6:1–29. [DOI] [PMC free article] [PubMed]
- 26.Tang S., Wan Z., Gao Y., Zheng J.-S., Wang J., Si Y.-Y., et al. Total chemical synthesis of photoactivatable proteins for light-controlled manipulation of antigen-antibody interactions. Chem Sci. 2016;7(3):1891–1895. doi: 10.1039/c5sc03404c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Tamzalit F, Wang MS, Jin W, Tello-Lafoz M, Boyko V, Heddleston JM, et al. Interfacial actin protrusions mechanically enhance killing by cytotoxic T cells. Sci Immunol [Internet]. 2019;4(33):eaav5445. Available from: http://immunology.sciencemag.org/content/4/33/eaav5445.abstract. [DOI] [PMC free article] [PubMed]
- 28.Haase K., Pelling A.E. Investigating cell mechanics with atomic force microscopy. J R Soc Interface. 2015;12(104):20140970. doi: 10.1098/rsif.2014.0970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Chen W, Villa-Diaz LG, Sun Y, Weng S, Kim JK, Lam RHW, et al. Nanotopography influences adhesion, spreading, and self-renewal of human embryonic stem cells. ACS Nano [Internet]. 2012;6(5):4094–103. Available from: https://doi.org/10.1021/nn3004923. [DOI] [PMC free article] [PubMed]
- 30.Bettinger CJ, Langer R, Borenstein JT. Engineering substrate topography at the micro- and nanoscale to control cell function. Angew Chem Int Ed [Internet]. 2009;48(30):5406–15. Available from: https://doi.org/10.1002/anie.200805179. [DOI] [PMC free article] [PubMed]
- 31.Rahmati M., Silva E.A., Reseland J.E., A. Heyward C., Haugen H.J. Biological responses to physicochemical properties of biomaterial surface. Chem Soc Rev. 2020;49(15):5178–5224. doi: 10.1039/d0cs00103a. [DOI] [PubMed] [Google Scholar]
- 32.Jardine J, Julien J-P, Menis S, Ota T, Kalyuzhniy O, McGuire A, et al. Rational HIV immunogen design to target specific germline B cell receptors. Science (80-) [Internet]. 2013;340(6133):711 LP – 716. Available from: http://science.sciencemag.org/content/340/6133/711.abstract. [DOI] [PMC free article] [PubMed]
- 33.Ni L, Ye F, Cheng ML, Feng Y, Deng YQ, Zhao H, et al. Detection of SARS-CoV-2-specific humoral and cellular immunity in COVID-19 convalescent individuals. Immunity [Internet]. 2020;52(6):971-977.e3. Available from: https://doi.org/10.1016/j.immuni.2020.04.023. [DOI] [PMC free article] [PubMed]
- 34.Chatterjee S.K., Saha S., Munoz M.N.M. Molecular pathogenesis, immunopathogenesis and novel therapeutic strategy against COVID-19. Front Mol Biosci. 2020;7(August):1–11. doi: 10.3389/fmolb.2020.00196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Shinohara H., Kurosaki T. Genetic analysis of B cell signaling. Subcell Biochem. 2006;40(3):145–187. doi: 10.1007/978-1-4020-4896-8_10. [DOI] [PubMed] [Google Scholar]
- 36.Supasa P., Zhou D., Dejnirattisai W., Liu C., Mentzer A.J., Ginn H.M., et al. Reduced neutralization of SARS-CoV-2 B.1.1.7 variant by convalescent and vaccine sera. Cell. 2021;184(8):2201–2211.e7. doi: 10.1016/j.cell.2021.02.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Zeng Y., Yi J., Wan Z., Liu K., Song P., Chau A., et al. Substrate stiffness regulates B-cell activation, proliferation, class switch, and T-cell-independent antibody responses in vivo. Eur J Immunol. 2015;45(6):1621–1634. doi: 10.1002/eji.201444777. [DOI] [PubMed] [Google Scholar]
- 38.Wang J, Lin F, Wan Z, Sun X, Lu Y, Huang J, et al. Profiling the origin, dynamics, and function of traction force in B cell activation. Sci Signal [Internet]. 2018;11(542):eaai9192. Available from: http://stke.sciencemag.org/content/11/542/eaai9192.abstract. [DOI] [PubMed]
- 39.Dubin-Thaler BJ, Hofman JM, Cai Y, Xenias H, Spielman I, Shneidman A V., et al. Quantification of cell edge velocities and traction forces reveals distinct motility modules during cell spreading. PLoS One. 2008;3(11). [DOI] [PMC free article] [PubMed]
- 40.Judokusumo E, Tabdanov E, Kumari S, Dustin ML, Kam LC. Mechanosensing in T Lymphocyte Activation. Biophys J [Internet]. 2012;102(2):L5–7. Available from: http://www.sciencedirect.com/science/article/pii/S0006349511054087. [DOI] [PMC free article] [PubMed]
- 41.Quijada-Álamo M, Hernández-Sánchez M, Alonso-Pérez V, Rodríguez-Vicente AE, García-Tuñón I, Martín-Izquierdo M, et al. CRISPR/Cas9-generated models uncover therapeutic vulnerabilities of del(11q) CLL cells to dual BCR and PARP inhibition. Leukemia [Internet]. 2020;34(6):1599–612. Available from: http://dx.doi.org/10.1038/s41375-020-0714-3. [DOI] [PMC free article] [PubMed]
- 42.Johnson SA, Pleiman CM, Pao L, Schneringer J, Hippen K, Cambier JC. Phosphorylated immunoreceptor signaling motifs (ITAMs) exhibit unique abilities to bind and activate Lyn and Syk tyrosine kinases. J Immunol [Internet]. 1995;155(10):4596 LP – 4603. Available from: http://www.jimmunol.org/content/155/10/4596.abstract. [PubMed]
- 43.Gold MR, Reth MG. Antigen Receptor Function in the Context of the Nanoscale Organization of the B Cell Membrane. Annu Rev Immunol [Internet]. 2019 Apr 26 [cited 2020 May 1];37(1):97–123. Available from: https://www.annualreviews.org/doi/10.1146/annurev-immunol-042718-041704. [DOI] [PubMed]
- 44.Lee WS, Wheatley AK, Kent SJ, DeKosky BJ. Antibody-dependent enhancement and SARS-CoV-2 vaccines and therapies. Nat Microbiol [Internet]. 2020;5(10):1185–91. Available from: http://dx.doi.org/10.1038/s41564-020-00789-5. [DOI] [PubMed]
- 45.Plotkin SA. Correlates of protection induced by vaccination. Clin Vaccine Immunol [Internet]. 2010;17(7):1055 LP – 1065. Available from: http://cvi.asm.org/content/17/7/1055.abstract. [DOI] [PMC free article] [PubMed]