Abstract
Background: Telecommunication models promise to improve access to cancer genetic counseling. Little is known about their impact among the geographically underserved. This work examined knowledge and emotional outcomes and attitudes/beliefs regarding cancer telegenetic services (via live-interactive videoconferencing) in Maine.
Materials and Methods: Cancer telegenetic patients seen at two remote sites and control (in-person) patients responded to pre-/postsurveys assessing care impact on hereditary breast and ovarian cancer (HBOC) knowledge and emotional health, ease of access to services, and telegenetics satisfaction/acceptability.
Results: 158/174 (90%) participants returned pre- and immediate postcounseling surveys (90 remote and 68 in-person). Fewer returned 1-month postsurveys. Remote patients were older with lower education levels, more likely to live in rural counties and to have cancer histories. The two groups were matched relative to gender, race, and health insurance status. HBOC knowledge improved equally in both groups pre- versus immediately postcounseling and was maintained at 1 month in both groups. Decreased anxiety was evident postcounseling with no significant difference between groups. Depression improved significantly in remote patients immediately postcounseling; 1-month depression measures were lower in both groups. The availability of telegenetics eased transportation needs/work absences, and patients reported satisfaction with telecommunication quality. Despite overall acceptance of telegenetics, 32% of remote patients noted preference for in-person care.
Conclusions: There were few differences in HBOC knowledge and emotional outcomes comparing traditional in-person cancer genetic services with telegenetics, and satisfaction with/acceptance of this model was high. These data relate to scalability of cancer telegenetics in rural regions regionally and nationally.
Keywords: : e-Health, m-Health, telehealth, telemedicine, cancer genetic counseling
Introduction
Basic scientific and clinical discoveries in hereditary cancer susceptibility risk assessment, counseling, and testing are advancing cancer control and prevention efforts nationally, resulting in increasing demand for cancer genetic counseling services. Acknowledged by leaders of the United States Precision Medicine Initiative, a rapidly evolving research agenda promises to place additional demands on those with cancer genetic expertise due to accelerated progress toward genome-directed diagnostic, prognostic, and treatment decision-making.1 Despite the promise of precision cancer medicine, access by patients in rural communities to credentialed cancer genetic professionals has been limited because traditional (i.e., in-person) services are largely concentrated in tertiary medical settings.2–6 The need for alternative models of cancer genetic care has been acknowledged as a means to meet growing demands.6,7
The impact of telemedicine has been evaluated as a model to provide genetic counseling to geographically underserved patients.8 Studies show that telemedicine via live-interactive videoconferencing in genetics (telegenetics) (1) increases access to care for those facing geographic barriers, (2) improves cost efficiency, and (3) meets growing demands.9 However, there has been incomplete study of ease-of-use and satisfaction/comfort with this model of care among rural American patients. Furthermore, although studies outside the United States have been done, there are only limited data on the impact of cancer telegenetics on patient knowledge and emotional outcomes compared with the impact of traditional in-person services in underpopulated regions of the United States.6,7,10–13 To scale cancer telegenetic services nationally, improved awareness of the impact of this model of care on patient outcomes is essential. Moreover, an understanding of patients' attitudes regarding their satisfaction with/acceptability of this technology is critical to widespread adoption and sustainability.
By comparing pre-/postsurvey results from patients seen via telegenetics with those from patients seen in-person, this study examined the outcomes of cancer genetic counseling on the following: (1) hereditary breast and ovarian cancer (HBOC) knowledge, (2) emotional health, (3) differences in knowledge and emotional outcomes based on care model, (4) impact of telegenetics on access to care, (5) satisfaction with telegenetic technology, and (6) telegenetics acceptability.
Materials and Methods
Participants
This study was implemented at the Maine Medical Center (MMC) Cancer Risk and Prevention Clinic (CRPC) in Scarborough, Maine. CRPC staff provides in-person care in Scarborough and telegenetic services via live-interactive videoconferencing in two remote clinics, described more fully below. At study initiation in 2013, the CRPC was Maine's only institution-based, genetic counselor-supported cancer genetic program. Potential participants included all new patients seen (remote or in-person) with personal and/or family histories suggestive of hereditary cancer susceptibility. All counseling sessions (both remote and in-person) were staffed by a board-certified cancer genetic counselor and a medical oncologist experienced in cancer genetic counseling. Remote and in-person visits were standardized relative to visit length and educational and counseling content. All patients undergoing genetic testing returned to clinic (via telegenetics or in-person) for results disclosure.
The control group included patients seen in-person. The remote group included patients counseled by the same staff via telegenetics at two distant hospital-based clinics. Remote sites had institution-based clinical staff who assisted the patients in appointment scheduling, telegenetic visits (e.g., support of equipment, provision of educational resources matching those offered to in-person patients, genetic testing paperwork, and blood draws), and postvisit care. Both in-person counseling sessions and remote sessions were conducted in dedicated clinic examination rooms with closed doors to ensure privacy. In general, referrals to each of the clinical sites were based on geographic proximity to that site. Referrals were from a range of clinicians, including primary care clinicians and cancer specialists. One site is located in Belfast, Maine, ∼110 miles from MMC. The second site is located in Augusta, Maine, ∼70 miles from MMC. All sites serve rural patients.14
Procedures
The MMC Institutional Review Board exempted this work from review because of the low risk, and the completed surveys were deidentified. Participant recruitment occurred between 2013 and 2015. Patients were invited to participate at the time of their initial visit and were made aware that participation was voluntary. Recruitment continued until at least 50 in-person and 100 remote patients responded to one or more survey instruments. Participants were surveyed precounseling, immediately postcounseling on site, and 1-month postcounseling via U.S. mail. One-month postcounseling surveys were distributed 4 weeks after results disclosure among those undergoing genetic testing. Surveys were coded for pre-/postcounseling data analysis; otherwise, they did not include identifying information. Patients were informed that response to individual survey items was voluntary. A research team member who was not involved in participants' clinical care entered data into a password-protected database. A second nonclinical team member performed a database audit of 40% of participants to confirm validity of entered data.
Instrumentation
An assessment of cancer genetic knowledge and scales to measure depression and anxiety were included in each of the surveys. All participants responded to a total of 13 true/false knowledge questions, including 4 items focused on hereditary colorectal cancer and 9 items related to HBOC. The four items reflecting hereditary colorectal cancer knowledge were excluded from reporting in this study because they were developed by the study team and considered exploratory. The nine HBOC-related knowledge questions were adapted from a National Human Genome Research Institute Cancer Genetics Studies Consortium tool, used in a number of previous studies focused on assessing HBOC knowledge.15–18 Study participants responded to all knowledge items; however, data analysis for HBOC knowledge was predicated on participants' reported personal and family history of cancer. Specifically, HBOC knowledge was assessed and reported only among participants having a personal and/or family history of breast and/or ovarian cancer. “Don't know” responses were considered incorrect.
Depression and anxiety were assessed through the Patient Health Questionnaire for Depression and Anxiety (PHQ-4), validated in healthcare and community settings,19–21 as well as in the cancer setting.21,22 This 4-item instrument asked respondents to report (on a scale of 0–3) their feelings relative to anxiety (two items: “Feeling nervous, anxious, or on edge”; “Not being able to stop or control worrying”) and depression (two items: “Feeling down, depressed, or hopeless”; “Little interest or pleasure in doing things”) with a response of zero reflecting no symptoms, and a response of three reflecting symptoms nearly every day.
PHQ-4 results analysis includes assessment of anxiety and depression subscales (score range for each totaling 0–6) such that a total score of three or more in each of the two subscales is considered positive. It also includes evaluation of the total score of both subscales (score range from 0 to 12). Categories of psychological distress are as follows: None 0–2; Mild 3–5; Moderate 6–8; and Severe 9–12.19
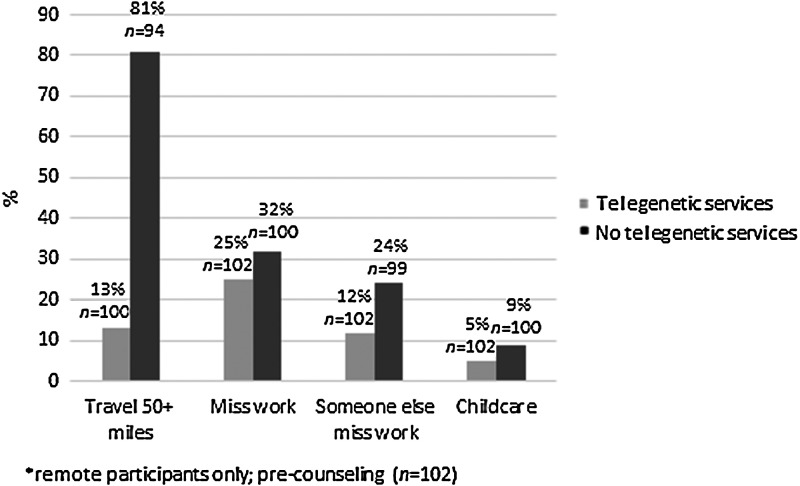
Presurvey
The presurvey for both control and remote sites included five questions focused on ease-of-access to clinical services, including distance traveled, mode of transportation, and economic burden (e.g., missed work for self and/or other(s) childcare needs). Remote participants were asked to answer these same questions as if telegenetic services were unavailable. Access-to-care questions were adapted from a MMC survey instrument used to assess ongoing general (noncancer) telegenetic care. Access-related data presented in this study reflect responses from remote participants only. All respondents were queried about basic demographic/medical characteristics.
Immediate postsurvey
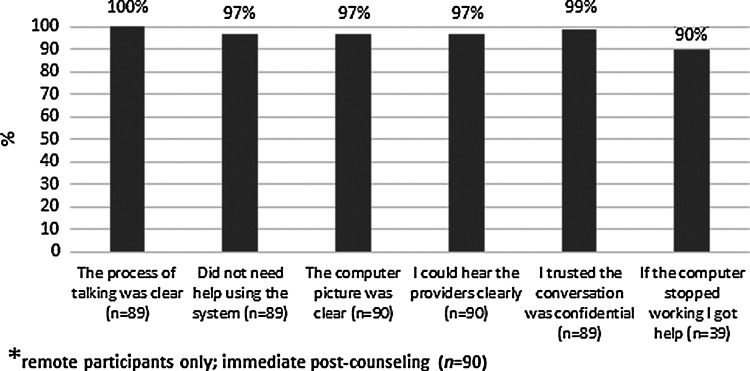
For remote sites, there were seven questions assessing satisfaction with the telecommunication technology, including ease-of-use of equipment, sound and picture quality, access to technical help if needed, and trust in confidentiality of the information discussed. Five of these items were adapted from a previously validated telehealth satisfaction survey instrument.23 The confidentiality question was adapted from a similar item in the Utah Telehealth Network's patient satisfaction survey.24 The first six items included responses on a 4-point Likert scale from strongly agree to strongly disagree. The seventh item was an open-ended question asking the participant to explain how the equipment had stopped working, if it had malfunctioned.
One-month postcounseling survey
For all sites, the 1-month mailed postcounseling survey included 11 items assessing participants' satisfaction with clinical services using a 4-point Likert scale from strongly agree to strongly disagree. Participants were also asked if they would recommend this service to others, and to rate their visit on a scale of 0 (worst possible) to 10 (best possible). These items were adapted from the Patient Satisfaction Survey developed by National Research Corporation, the Consumer Assessment of Healthcare Providers and Systems (CAHPS) vendor for the health system (acocahps.cms.gov).25 All participants were asked for any additional feedback in an open-ended format relative to the services received.
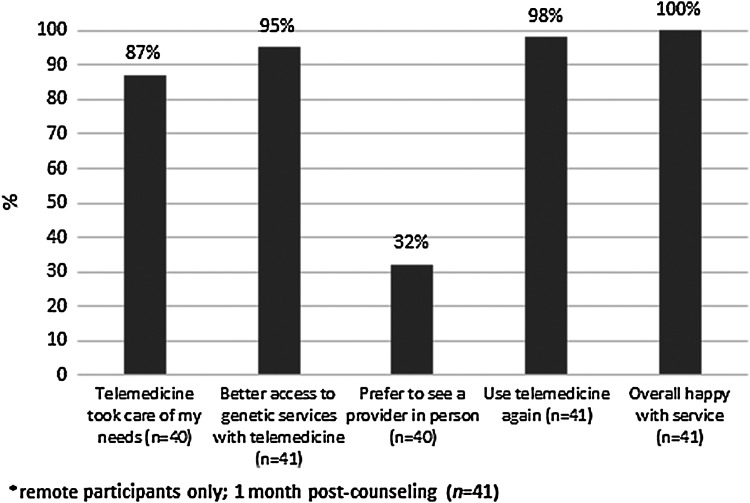
Remote participants were asked to answer five additional questions regarding telegenetics acceptability, assessed through a 4-point Likert scale from strongly agree to strongly disagree. Four of these were adapted from the previously validated Telemedicine Satisfaction Questionnaire;23 one question (“I would prefer to see the genetic providers in-person”) was adapted from an existing MMC survey instrument used to assess general (noncancer) telegenetic care in Northern Maine. In this study, we report on 1-month responses by remote participants to the five telegenetics acceptability items.
Data analyses
Statistical analyses were performed using SAS Enterprise Guide version 5.1 (Cary, NC). Between-group differences for categorical data were calculated using chi-square statistics. Within-group differences for noncategorical data were calculated using paired t-tests, whereas between-group differences were calculated using independent t-tests. Participants' responses to two survey items reflecting anxiety were summed, as were two items reflecting depression. Emotional data presented in Table 2 represent the mean of anxiety sums and depression sums among participants from each of the two study groups. Responses (4-point Likert scale) to questions relative to satisfaction with and acceptability of telegenetic services were dichotomized such that strongly agree and agree responses were combined and classified as agree; whereas disagree and strongly disagree responses were combined and classified as disagree (Figs. 2, 3).
Table 2.
Change in Knowledge and Emotional Status Pre- Versus Postcounseling
| STUDY POPULATION | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| REMOTE (n = 106) | IN-PERSON (n = 68) | REMOTE VERSUS IN-PERSON | |||||||||
| Precounseling | Immediate postcounseling | Change | Precounseling | Immediate postcounseling | Change | Pre- versus immediate postchange difference | |||||
| Variablea | n | Mean (SD) | n | Mean (SD) | p value | n | Mean (SD) | n | Mean (SD) | p value | p valueb |
| HBOC knowledge | 83 | 3.7 (2.25) | 66 | 6.6 (1.54) | <.0001 | 50 | 4.1 (2.18) | 50 | 6.9 (1.63) | <.0001 | .85 |
| Anxiety | 98 | 1.42 (1.84) | 89 | 1.2 (1.54) | .07 | 66 | 1 (1.25) | 68 | 0.8 (1.14) | .004 | .59 |
| Depression | 99 | 0.90 (1.53) | 89 | 0.67 (1.31) | .02 | 66 | 0.42 (0.96) | 68 | 0.35 (0.84) | .13 | .09 |
| ONE-MONTH POSTCOUNSELING | ||||
|---|---|---|---|---|
| REMOTE (n = 41) | IN-PERSON (n = 24) | |||
| Variablea | n | Mean (SD) | n | Mean (SD) |
| HBOC knowledge | 31 | 5.9 (2.08) | 18 | 6.9 (1.51) |
| Anxiety | 40 | 0.82 (1.37) | 24 | 0.58 (0.77) |
| Depression | 40 | 0.35 (0.73) | 24 | 0.29 (0.69) |
n's vary for individual measures as not all participants responded to all survey items.
Breast cancer knowledge measure depicts mean number of correct responses out of a maximum of 9 possible correct responses among participants with a personal or family history of breast/ovarian cancer; Anxiety and Depression items depict mean sum of two items reflecting anxiety and two items reflecting depression (range 0–6).
p value depicts the difference (if any) in degree of measure change pre- versus immediately postcounseling comparing remote versus in-person participants.
HBOC, hereditary breast and ovarian cancer.
Fig. 2.
Satisfaction with telegenetic technology*.
Fig. 3.
Acceptability of telegenetic services*.
Results
Participants
A total of 174 patients participated in this study (106 remote; 68 in-person). Of these, 158 (90%) returned both pre- and immediate postcounseling surveys, including 90/106 remote patients (85%) and 68 in-person patients (100%). A total of 41/90 remote patients (46%) and 24/68 in-person patients (35%) returned 1-month postcounseling surveys. Response to individual survey items varied.
Table 1 summarizes basic demographic and medical/family history characteristics of all 174 respondents. Comparing groups, remote patients were older (p = .02), less likely to have a 4-year college education (p = .006), more likely to live in a rural county (p < .0001), and more likely to have a personal history of cancer (p = .005). Group demographic characteristics were similar with regards to gender, race, and perception of health insurance coverage adequacy.
Table 1.
Differences in Demographic Characteristics Remote Versus In-Person Participants
| CHARACTERISTIC | REMOTE n = 106 | IN-PERSON n = 68 | p |
|---|---|---|---|
| Age in years, mean (SD) | 55 (15.5) | 49 (13.5) | .02 |
| Female gender, n (%) | 88 (83) | 57 (84) | .55 |
| Race, n (%) | .58 | ||
| White | 95 (90) | 62 (91) | |
| Black or African American | 2 (2) | 0 (0) | |
| Native American | 2 (2) | 0 (0) | |
| Other | 7 (7) | 6 (9) | |
| Insurance status, n (%) | .81 | ||
| Adequately insured | 90 (85) | 58 (85) | |
| Under or uninsured | 7 (7) | 3 (4) | |
| Prefer not to answer | 1 (1) | 0 (0) | |
| Do not know | 4 (4) | 5 (7) | |
| No response | 4 (4) | 2 (3) | |
| Education level, n (%) | .006 | ||
| Less than high school graduate | 1 (1) | 1 (1) | |
| High school graduate | 27 (25) | 5 (7) | |
| Some college or 2-year degree | 38 (36) | 23 (34) | |
| Four-year college or greater | 35 (33) | 37 (54) | |
| No response | 5 (5) | 2 (3) | |
| County of residence, n (%) | <.0001 | ||
| Rural | 95 (90) | 27 (40) | |
| Urban | 11 (10) | 41 (60) | |
| No personal history of cancer, n (%) | 42 (40) | 38 (56) | |
| Personal cancer history, n (%) | 60 (57) | 29 (43) | .005 |
| Breast cancer | 30 (50) | 6 (21) | |
| Ovarian cancer | 1 (2) | 4 (14) | |
| Colorectal cancer | 6 (10) | 4 (14) | |
| Uterine cancer | 1 (2) | 3 (10) | |
| Other | 9 (15) | 8 (28) | |
| More than one | 11 (18) | 3 (10) | |
| No response | 2 (3) | 1 (3) | |
| Family history of cancer, n (%) | 98 (92) | 64 (94) | .56 |
SD, standard deviation.
Knowledge gain
A total of 41/174 participants (18 in-person and 23 remote) were excluded from knowledge analysis because they did not report a personal and/or family history of breast/ovarian cancer. Table 2 shows that among those reporting a personal and/or family history of breast/ovarian cancer, there was a statistically significant increase in HBOC knowledge pre- versus immediately postcounseling in both groups with no difference in the degree of knowledge gained comparing groups. Importantly, gain in knowledge persisted when data were analyzed only among those participants responding to HBOC knowledge items in both pre- and immediate postcounseling survey instruments (data not shown). Table 2 also shows that gain in HBOC knowledge over precounseling baseline persisted in both groups at 1 month following counseling.
Emotional outcomes
Comparing the two study populations' precounseling, remote patients had higher levels of anxiety and depression (Table 2). As shown, there was a statistically significant reduction in anxiety pre- versus immediately postcounseling within the in-person group and a trend toward reduced anxiety pre- versus immediately postcounseling within the remote group. The degree of change in anxiety comparing groups was not statistically significant. Relative to depression, there was a reduction in depression measures comparing pre- versus immediately postcounseling within the remote group in contrast to no significant change within the in-person group. Although there was a trend toward a greater reduction in depression among those seen remotely compared with the in-person group, pre- versus immediately postcounseling, this did not meet statistical significance (p = .09). Table 2 shows that at 1-month postcounseling, both study populations reported reduced anxiety and depression compared with measures collected immediately postcounseling.
Ease of access
Figure 1 depicts that among the remote patients responding to ease-of-access questions, 13% reported traveling 50 miles or more to their telegenetics appointment; whereas 81% would have traveled more than 50 miles to access in-person services. Likewise, due to availability of telegenetic services, fewer patients and/or others supporting their attendance were required to miss work, and childcare needs were eased slightly by telegenetics.
Fig. 1.
Impact of telegenetics on care access*.
Satisfaction with telegenetic technology
There was general satisfaction with the telecommunication technology used (Fig. 2). A minority reported equipment problems requiring assistance, including the picture freezing (n = 10) and/or loss of internet connection (n = 6). Ninety percent of the patients reporting technical problems noted that they were adequately addressed. All but one remote participant trusted that their conversation was confidential.
Acceptability of telegenetic services
Remote patients were surveyed 1 month after genetic counseling to assess acceptability of cancer telegenetics as a care model. Among the 41 respondents, there was overall acceptance of this care model as reflected in reports of better access to genetic services, willingness to use telemedicine again, and happiness with the services; however, 13% (n = 5) reported that telemedicine did not address their healthcare needs, and 32% (n = 13) of remote patients would have preferred seeing the provider in-person (Fig. 3).
Discussion
We examined HBOC knowledge and emotional outcomes among those counseled remotely versus those receiving traditional in-person cancer genetic counseling services at a tertiary care center in Maine. This work also examined the impact of telegenetics on ease-of-access to cancer genetic services, as well as satisfaction with the technology used and acceptability of the services rendered.
Sociodemographic factors that create persistent health and healthcare inequities are major challenges in Maine, ranking 32nd (high to low) in per capita income.26 It is among 19 American states failing to adopt Medicaid Expansion under the Affordable Care Act, limiting health insurance access among its lowest income adults.27 Just over 60% of Maine's 1.3 million residents live in rural areas, compared with 19% in the United States as a whole, impacting provision of specialty care services, including cancer genetic counseling.28,29 The data reported in this study may be generalizable to other geographically underserved areas and may support expanded access to care in rural communities nationally.
Relative to cancer genetic knowledge gained, we show an increase in HBOC knowledge pre- versus immediately postcounseling in both study groups, with similar levels of increase comparing groups, and persistent knowledge gains 1 month postcounseling. The work reported in this study extends findings from United Kingdom, Australian, and U.S. studies and reinforces the benefit of cancer telegenetics as a means to expand rural access to high-quality genetic counseling services.10–13
We show a decline in measures of anxiety and depression in both groups postcounseling with minor differences in short-term emotional outcomes comparing the telegenetic care model with traditional in-person cancer genetic counseling. These findings are similar to results of earlier studies from non-U.S. countries and more densely populated American States.11–13 This is significant because assessment and supportive management of patients' emotional signs and symptoms are essential components of the genetic counseling process. The ability of the counselor to play a central role in the emotional health of her/his patient is presumably based on her/his success in building rapport and conveying empathy—both factors that could be negatively impacted by telehealth technology. Combined with previous data, our work supports telegenetics as a means to provide effective and supportive cancer genetic counseling services to geographically isolated patients.
Significantly, there was a higher level of baseline emotional distress among remote patients. We cannot determine from this work the cause for this difference. It is possible that it reflected medical and sociodemographic factors. Remote patients had higher personal rates of cancer compared with in-person patients. Furthermore, remote patients had lower education levels, and most (90%) were from rural counties, in comparison with in-person patients (40%). There is a dearth of literature examining the influence of geographic place of residence (rural vs. urban) on emotional disorders.30 There is need for further study regarding the emotional support needs of geographically underserved individuals accessing telegenetic services (and other cancer care services) at state and national levels.
We show the influence of telegenetic technology on ease-of-access to specialty cancer genetic services. The majority of remote respondents would have traveled at least 50 miles one-way if telegenetic services were unavailable. Relative to economic impact, more respondents and/or others supporting the visits would have missed work and would have spent money on transportation and childcare had they traveled for these services. Transportation costs and other economic burdens are significant issues relative to promoting equitable access to cancer genetic counseling services in rural areas nationally.31
The results reported in this study reveal that there was general satisfaction with telegenetic technology among remote participants. This included ease-of-use of the equipment and participants' ability to communicate clearly. There was little concern about confidentiality of the information discussed. In most circumstances, technical issues were overcome in a timely manner. We show that acceptability of the telegenetic care model was high, including addressing healthcare needs, improved access, willingness to use technology again, and overall happiness with the services rendered. However, 13/40 (32%) remote respondents reported preference for in-person services. This is not an unexpected finding because in-person counseling represents the standard model of care nationally. Previous work in a postoperative study population from Scotland revealed similar findings relative to preference for usual (in-person care) over telemedicine services.32 Furthermore, older patients are less likely to feel comfortable with technology overall, although they may rate specific experiences high.33
Dedicated information technology (IT) specialists support all MMC telegenetic services. Furthermore, local IT specialists and healthcare professionals provided support throughout the remote patient's care. These labor-intensive resources likely influenced study results relative to both satisfaction with/acceptability of telegenetics; that is, 90% of participants who experience technical problems reported that these issues were addressed in a timely manner. It is important to take these resources into account in considering telegenetics scalability.
Study limitations
Although this work advances understanding of the impact of cancer telegenetic services via live-interactive videoconferencing on HBOC knowledge and emotional outcomes among rural patients and provides valuable insight relative to satisfaction with/acceptability of telegenetic services, there are several important limitations to this study that influence the data's generalizability. First, this work involved a limited number of patients of one Maine clinical service. This affects the transferability of this work to services staffed by multiple clinical teams or alternating staff members. Second, as measures of knowledge gained were HBOC focused, we did not examine change in knowledge among those facing risk for other hereditary cancer susceptibility disorders, limiting the generalizability of reported findings. Third, responses to questions reflecting satisfaction with both the technology and the clinical services rendered may have reflected respondents' desire to please the clinical team, not their attitudes regarding telegenetics. Fourth, study results are reflective of both the clinical services offered to study participants, and the IT and other clinical support resources likely unique to MMC cancer genetic services. Fifth, as this was a nonrandomized study, between-group knowledge and emotional health comparisons should be viewed with caution.
This work adds to a growing body of literature addressing the increasing demands for high-quality cancer genetic counseling and novel means to address these demands, especially among those facing geographic barriers to care. Results reported in this study should be confirmed among a broader population of patients from other rural regions nationally and among patients served by clinical teams with more limited levels of technical support. Finally, studies should be extended to other telegenetic care models, including telecommunication services provided to patients within their homes via teleconferencing or phone.
Conclusion
This work reveals that there were few differences in HBOC knowledge and emotional outcomes between traditional in-person cancer genetic counseling services and telegenetic services via live-interactive videoconferencing. As expected, the availability of telegenetics eased transportation needs and work absences. Remote study participants were satisfied with the quality of the technology used. Although there was overall acceptance of telegenetics, nearly a third of remote patients noted preference for in-person care. These data relate directly to the scalability of telegenetics as a means to extend access to cancer genetic counseling to rural populations regionally and nationally.
Acknowledgments
We thank Erica Jackson CRA, Katherine A. Lafferty CGC, Kristen Langlois RN, and Kim Lenfestey LCSW for their assistance in this work, Norma Albrecht for article preparation, and Michael Erard for editorial assistance.
This study was partially supported by the Maine Cancer Foundation grant in 2014 entitled: Expanding Cancer Telegenetics to Serve Five Maine Counties.
Disclosure Statement
No competing financial interests exist.
References
- 1.Collins FS, Varmus H. A new initiative on precision medicine. N Engl J Med 2015;372:793–795 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Epplein M, Koon KP, Ramsey SD, Potter JD. Genetic services for familial cancer patients: A follow-up survey of National Cancer Institute Cancer Centers. J Clin Oncol 2005;23:4713–4718 [DOI] [PubMed] [Google Scholar]
- 3.Friedman LC, Cooper HP, Webb JA, et al. . Primary care physicians' attitudes and practices regarding cancer genetics: A comparison of 2001 with 1996 survey results. J Cancer Educ 2003;18:91–94 [DOI] [PubMed] [Google Scholar]
- 4.Garber JE, Offit K. Hereditary cancer predisposition syndromes. J Clin Oncol 2005;23:276–292 [DOI] [PubMed] [Google Scholar]
- 5.Vig HS, Armstrong J, Egleston BL, et al. . Cancer genetic risk assessment and referral patterns in primary care. Genet Test Mol Biomarkers 2009;13:735–741 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Buchanan AH, Rahm AK, Williams JL. Alternate service delivery models in cancer genetic counseling: A mini-review. Front Oncol 2016;6:120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Vrecar I, Hristovski D, Peterlin B. Telegenetics: An update on availability and use of telemedicine in clinical genetics service. J Med Syst 2017;41:21. [DOI] [PubMed] [Google Scholar]
- 8.Committee on Evaluating Clinical Applications of Telemedicine. A Guide to Assessing Telecommunications for Health Care: Washington, DC: The National Academies Press, National Academy of Sciences, 1996 [PubMed] [Google Scholar]
- 9.Hilgart JS, Hayward JA, Coles B, Iredale R. Telegenetics: A systematic review of telemedicine in genetics services. Genet Med 2012 [DOI] [PubMed]
- 10.Buchanan AH, Datta SK, Skinner CS, et al. . Randomized trial of telegenetics vs. in-person cancer genetic counseling: Cost, patient satisfaction and attendance. J Genet Couns 2015;24:961–970 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Coelho JJ, Arnold A, Nayler J, et al. . An assessment of the efficacy of cancer genetic counselling using real-time videoconferencing technology (telemedicine) compared to face-to-face consultations. Eur J Cancer 2005;41:2257–2261 [DOI] [PubMed] [Google Scholar]
- 12.Zilliacus EM, Meiser B, Lobb EA, et al. . Are videoconferenced consultations as effective as face-to-face consultations for hereditary breast and ovarian cancer genetic counseling? Genet Med 2011;13:933–941 [DOI] [PubMed] [Google Scholar]
- 13.Bradbury A, Patrick-Miller L, Harris D, et al. . Utilizing remote real-time videoconferencing to expand access to cancer genetic services in community practices: A multicenter feasibility study. J Med Internet Res 2016;18:e23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Office of Management and Budget. List of Rural Counties And Designated Eligible Census Tracts in Metropolitan Counties. Available at ftp://ftp.hrsa.gov/ruralhealth/eligibility2005.pdf (last accessed June17, 2016)
- 15.Bluman LG, Rimer BK, Berry DA, et al. . Attitudes, knowledge, and risk perceptions of women with breast and/or ovarian cancer considering testing for BRCA1 and BRCA2. J Clin Oncol 1999;17:1040–1046 [DOI] [PubMed] [Google Scholar]
- 16.Lerman C, Biesecker B, Benkendorf JL, et al. . Controlled trial of pretest education approaches to enhance informed decision-making for BRCA1 gene testing. J Natl Cancer Inst 1997;89:148–157 [DOI] [PubMed] [Google Scholar]
- 17.Calzone KA, Prindiville SA, Jourkiv O, et al. . Randomized comparison of group versus individual genetic education and counseling for familial breast and/or ovarian cancer. J Clin Oncol 2005;23:3455–3464 [DOI] [PubMed] [Google Scholar]
- 18.Hughes C, Gomez-Caminero A, Benkendorf J, et al. . Ethnic differences in knowledge and attitudes about BRCA1 testing in women at increased risk. Patient Educ Couns 1997;32:51–62 [DOI] [PubMed] [Google Scholar]
- 19.Kroenke K, Spitzer RL, Williams JB, Lowe B. An ultra-brief screening scale for anxiety and depression: The PHQ-4. Psychosomatics 2009;50:613–621 [DOI] [PubMed] [Google Scholar]
- 20.Kroenke K, Spitzer RL, Williams JB, Lowe B. The patient health questionnaire somatic, anxiety, and depressive symptom scales: A systematic review. Gen Hosp Psychiatry 2010;32:345–359 [DOI] [PubMed] [Google Scholar]
- 21.MacDonald DJ, Blazer KR, Weitzel JN. Extending comprehensive cancer center expertise in clinical cancer genetics and genomics to diverse communities: The power of partnership. J Natl Compr Canc Netw 2010;8:615–624 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Polidoro Lima M, Osorio FL. Indicators of psychiatric disorders in different oncology specialties: A prevalence study. J Oncol 2014;2014:350262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Yip MP, Chang AM, Chan J, MacKenzie AE. Development of the Telemedicine Satisfaction Questionnaire to evaluate patient satisfaction with telemedicine: A preliminary study. J Telemed Telecare 2003;9:46–50 [DOI] [PubMed] [Google Scholar]
- 24.Utah Telehealth Network. Telehealth Patient Satisfaction Survey. 2016. Available at https://healthit.ahrq.gov/health-it-tools-and-resources/health-it-survey-compendium/utah-telehealth-network-telehealth-patient (last accessed June20, 2016)
- 25.Centers for Medicare & Medicaid Services. Consumer assessment of healthcare providers and systems. Baltimore, MD. Available at http://acocahps.cms.gov/globalassets/aco---epi-2-new-site/pdfs-for-aco/survey-instruments/2016-aco-survey/english/2016_aco-9_mail_survey_english.pdf (last accessed June21, 2017) [Google Scholar]
- 26.Bureau of Economic Analysis. State personal income 2011 (released March 28, 2012). Available at www.bea.gov/newsreleases/regional/spi/2012/spi0312.htm (last accessed July16, 2012)
- 27.Henry J. Kaiser Family Foundation. Status of state action on the Medicaid expansion decision. Available at http://kff.org/health-reform/state-indicator/state-activity-around-expanding-medicaid-under-the-affordable-care-act (last accessed June15, 2016)
- 28.U.S. Census Bureau. Census 2000 Summary File 1, Matrices H1 and H3. Available at http://factfinder2.census.gov/faces/tableservices/jsf/pages/productview.xhtml?pid=DEC_00_SF1_GCTH1.ST93&prodType=table (last accessed August9, 2012)
- 29.U.S. Department of Commerce. Growth in urban population outpaces rest of nation, Census Bureau Reports. In: U.S. Census Bureau, ed. U.S. Federal Government; Washington, DC, 2012 [Google Scholar]
- 30.Breslau J, Marshall GN, Pincus HA, Brown RA. Are mental disorders more common in urban than rural areas of the United States? J Psychiatr Res 2014;56:50–55 [DOI] [PubMed] [Google Scholar]
- 31.Ambroggi M, Biasini C, Del Giovane C, et al. . Distance as a barrier to cancer diagnosis and treatment: Review of the literature. Oncologist 2015;20:1378–1385 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Marsh J, Bryant D, MacDonald SJ, et al. . Are patients satisfied with a web-based followup after total joint arthroplasty? Clin Orthop Relat Res 2014;472:1972–1981 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Gordon NP, Hornbrook MC. Differences in access to and preferences for using patient portals and other eHealth technologies based on race, ethnicity, and age: A database and survey study of seniors in a large health plan. J Med Internet Res 2016;18:e50. [DOI] [PMC free article] [PubMed] [Google Scholar]