Abstract
Background:
Weightbearing computed tomography (WBCT) is a reliable and precise modality for the measurement and analysis of bone position in the foot and ankle, as well as associated deformities. WBCT to assess three dimensional relationships among bones allowed the development of new measurements, as the Foot and Ankle Offset (FAO), which has high inter and intra-rater reliability. This study reports the University of Iowa’s experience utilizing WBCT for the care of foot and ankle patients by describing its utility across different orthopedic diseases in improving diagnostic assessment, aiding surgical planning, and expanding the use for objective clinical follow-up.
Methods:
The medical records of consecutive patients with various foot and ankle disorders that underwent WBCT examination as part of the standard of care at a single institution between November 2014 and August 2020 were retrospectively reviewed. Patient factors, including body mass index (BMI), sex, and patient comorbidities were collected. 3D coordinates for calculation of FAO were harvested using the Multiplanar Reconstruction (MPR) views were calculated from the obtained exams. Descriptive statistics were performed with Shapiro-Wilk test and the Anderson-Darling tests.
Results:
1175 feet and ankles (820 patients) had a WBCT performed over the studied 68 months. 53% of the subjects were male and 47% female. 588 of the acquisitions were from the right side (50.04%) and 587 from the left side (49.96%). Diabetes was present in 15.47% of, Rheumatic diagnoses in 4.52% and smoking habits in 44.10% of patients. Mean BMI of the sample was found to be 32.47 (32.03-32.90, 95% CI). The mean Foot and Ankle Offset (FAO) encountered in the study’s population was 2.43 (2.05-2.82, 95% CI; min -30.8, max 37.65; median 2.39).
Conclusion:
This study contains the largest cohort of WBCTs with accompanied FAO measurements to date, which can aid with establishing a new baseline FAO measurement for multiple pathological conditions. Acquiring WBCTs resulted in a variety of more specific diagnoses for patient with foot and ankle complaints. The ability to utilize WBCT for presurgical planning, the capability to provide a 3D reconstruction of patient anatomy, and its use for assessment of advanced relational foot and ankle measurements, such as FAO, demonstrate how WBCT may serve as a remarkable utility in clinical practice and has become a standard of care in our practice at the University of Iowa.
Level of Evidence: IV
Keywords: weight-bearing ct, foot ankle offset
Introduction
Previous studies have identified the weightbearing computed tomography (WBCT) is a reliable and precise modality for the measurement and analysis of bone position in the foot and ankle, as well as associated deformities.1-4 WBCT offers assessment and visualization of the true relative positioning between bones of joints under loading conditions, which cannot be assessed by standard CT scans.4 Traditional weight bearing radiographs for assessment of bone orientation under loading are more susceptible to technological errors, such as rotational malalignment, which leads clinicians to obtain inaccurate measurements of pathological deformities.5 Moreover, WBCT has already demonstrated high utility for various foot and ankle deformities ranging from Progressive Collapsing Foot Deformity (PCFD) and Hallux Valgus (HV) to Periprosthetic Cysts and Ankle Osteoarthritis (AO).6-10 This imaging modality allows for a more accurate three-dimensional deformity assessment and a higher spatial resolution, providing the physician with a more complete armamentarium for treatment planning.1,2 The evaluation of measurements and signs extracted from WBCTs demonstrate both high intra-rater reliability and inter-rater reliability among varying levels of clinicians and for different conditions.2,11,12
The capability in the WBCT to assess three dimensional relationships among bones allowed the development of new measurements, as the Foot and Ankle Offset (FAO).13-15 This assessment describes the relationship between the relative position of the ankle joint’s mechanical axis (center of the talus) and the foot tripod (first metatarsal, fifth metatarsal and calcaneus).1,13,14 It is a semiautomatic three-dimensional assessment tool, providing a percentage of ankle deviation from the foot vector. In other words, it corresponds to the level arm of the torque produced in the ankle by bodyweight and ground reaction forces during physiological weight bearing ambulation.1,13,14 Previous studies showed a value of 2.3% (+-2.9) in normal patients, -11.6% (+-6.9) in varus and 11.4% (+-5.7) in valgus alignment.14 Moreover, the use of the FAO has validated in the assessment of PCFD, Cavovarus Deformities and Ankle Arthritis, providing a reliable value for diagnosis and deformity prognosis.10,16,17
New indications and clinical utilities are being described for WBCT over the last decade.18,19 Syndesmotic instability, lateral ligament instability, Lisfranc ligament injury, hallux rigidus and post-traumatic conditions are gaining attention from the scientific community as the WBCT portrays a natural and physiological stress to the evaluated region.20-23 Research focusing in WBCT applicability in knee and hip disorders are also increasing while new devices gain the capability of a more proximal evaluation.24,25 As such, this study aims to report the University of Iowa’s experience utilizing WBCT for the care of a large cohort of foot and ankle patients. We intend to show its utility across different orthopedic diseases as an instrument that improves diagnostic assessment, aids knowledge to surgical planning, and expands the use for objective clinical follow-up, as well as describe the overall foot alignment of the patients assessed, by measuring FAO
Methods
Study Design
This is a retrospective epidemiological observational IRB-approved study that complied with the Declaration of Helsinki and the Health Insurance Portability and Accountability Act (HIPAA) and it reviewed medical records of consecutive patients with various foot and ankle disorders that underwent WBCT examination as part of the standard of care at a single institution between November 2014 and August 2020.
Sample
The University of Iowa Department of Orthopaedics and Rehabilitation introduced a WBCT scanner in November 2014 for use by the foot and ankle clinicians. All patient WBCTs obtained from activation of the WBCT scanner in November of 2014 until August of 2020 were collected. For the purposes of this report, each WBCT is defined as a single foot/ ankle CT with unique laterally, left or right, obtained with the patient bearing weight through the imaged extremity. Any bilateral WBCTs obtained were split into individual scans to maintain consistent reporting. Patient data and their associated WBCT scans were compiled into a single study database under the supervision of the principal investigator.
Retrospective chart review was utilized to collect all patient demographics including age, body mass index (BMI), sex, and patient comorbidities (diabetes, rheumatoid diseases, and smoking status). The main diagnosis related to the need for WBCT imaging was also evaluated.
All the patients had their diagnoses reviewed and the WBCT images were assessed for measurement of the Foot and Ankle Offset (FAO).
WBCT Imaging
WBCT studies were completed with a cone-beam CT extremity scanner (PedCAT™, CurveBeam LLC, Warrington, PA, USA). Participants were instructed to bear weight in a normal and physiological standing upright position, dispensing the body weight uniformly between the lower limbs and with the feet set at shoulder width and measurements.
The raw 3D data was converted to sagittal, coronal, and axial image slices that were then transferred digitally into dedicated software (CubeVue™, CurveBeam, LLC, Warrington, PA, USA). Image marks were removed, and studies were given a unique and random number. One fellowship-trained foot and ankle surgeons independently and blindly assessed FAO.
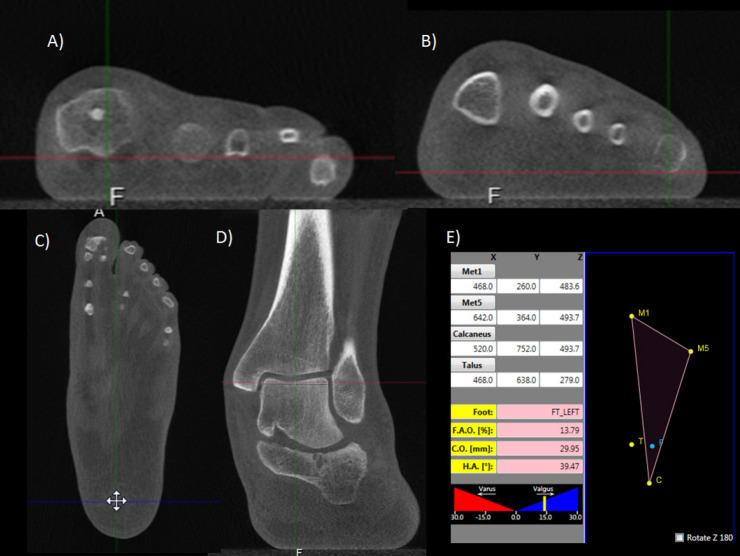
The 3D coordinates for calculation of FAO were harvested using the Multiplanar Reconstruction (MPR) views. The first point marked is the most distal voxel of the first metatarsal head, followed by the most distal voxel of the fifth metatarsal head and most distal voxel of the calcaneal tuberosity. Finally, the most central and proximal aspect of the talar dome was marked, and the automatic calculation of the FAO was given by the software (Figure 1).
Fig 1.
Foot and Ankle Offset (FAO) semiautomatic measurement. Using the three planes (x; y; z), the most plantar voxel of the first metatarsal is found (A) in the three planes, followed by the most plantar voxel of the fifth metatarsal (B), the most plantar voxel of the calcaneus (C) and the most proximal and central voxel of the talus (D). The software calculates (E) positioning of the foot tripod (M1-M5-C) and the expect position of the ankle joint center (F). The percentage of displacement in subject’s talus position (T) in relation to this axis (M1-M5-C-F) is determined as the FAO.
Statistical Analysis
The variables were initially evaluated for normality using the Shapiro-Wilk test and the Anderson-Darling test. Mean, median, interquartile range (IQR), and 95% confidence interval (CI) values for each measurement were reported.
Demographic data and diagnoses were assessed by frequencies distributions and quantile plots. P values of less than 0.05 were considered significant. Estimate of the likelihood of the model to estimate future was performed by Akaike information criterion (AIC) and Bayesian information criterion (BIC).
Results
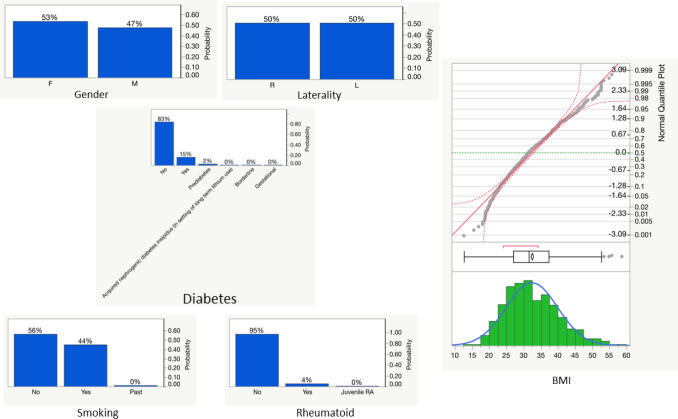
A total of 1175 feet and ankles (820 patients) had a WBCT performed over the studied 68 months. 53% of the subjects were male and 47% female. 588 of the acquisitions were from the right side (50.04%) and 587 from the left side (49.96%). Diabetes was present in 15.47% of patients, Rheumatic diagnoses in 4.52%, and smoking habits in 44.10% of patients included. Mean BMI of the sample was found to be 32.47 (32.03-32.90, 95% CI). A summary of demographics findings can be found in Figure 2.
Figure 2.
Demographic distribution for gender, laterality, comorbidities, and body mass index (BMI).
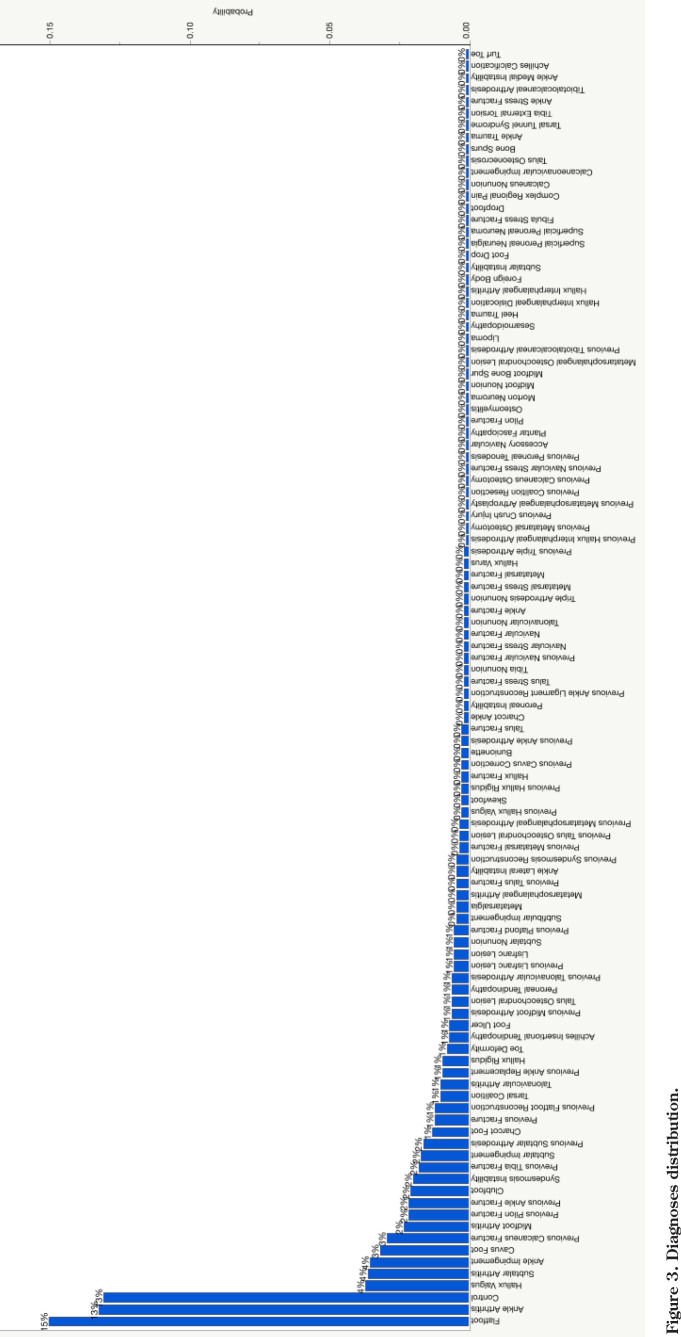
The main obtained diagnoses were PCFD (Flatfoot) with 15.01% of occurrences and Ankle Arthritis with 13.21%. A considerable number of controls (13.04%) was shown, mainly the contralateral side of affected limb. Hallux valgus (C 3.7%), subtalar arthritis (3.6%), ankle impingement (3.5%), Cavovarus (3.1%), previous calcaneus fracture (2.9%), midfoot arthritis (2.3%), previous pilon fracture (2,1%), previous ankle fracture (2.1%), clubfoot (2%) and syndesmosis instability (1.9%) follow the sample incidence. A complete list of diagnoses may be found on Table 1 and Figure 3.
Table 1.
Summary of the Most Common Foot and Ankle Disorders that Underwent a WBCT Over the Studied Period
| Diagnosis | Count | Prob |
|---|---|---|
| Flatfoot | 175 | 0.15009 |
| Ankle Arthritis | 154 | 0.13208 |
| Control | 152 | 0.13036 |
| Hallux Valgus | 43 | 0.03688 |
| Subtalar Arthritis | 42 | 0.03602 |
| Ankle Impingement | 41 | 0.03516 |
| Cavus Foot | 37 | 0.03173 |
| Previous Calcaneus Fracture | 34 | 0.02916 |
| Midfoot Arthritis | 27 | 0.02316 |
| A Previous Pilon Fracture | 25 | 0.02144 |
| Previous Ankle Fracture | 25 | 0.02144 |
| Clubfoot | 24 | 0.02058 |
| Syndesmosis Instability | 23 | 0.01973 |
| Previous Tibia Fracture | 21 | 0.01801 |
| Subtalar Impingement | 20 | 0.01715 |
| Previous Subtalar Arthrodesis | 19 | 0.01630 |
| Charcot Foot | 15 | 0.01286 |
| Previous Fracture | 14 | 0.01201 |
| Previous Flatfoot Reconstruction | 14 | 0.01201 |
| Tarsal Coalition | 12 | 0.01029 |
| Talonavicular Arthritis | 12 | 0.01029 |
| Previous Ankle Replacement | 11 | 0.00943 |
| Hallux Rigidus | 11 | 0.00943 |
| Toe Deformity | 9 | 0.00772 |
| Achilles Insertional Tendinopathy | 8 | 0.00686 |
| Foot Ulcer | 8 | 0.00686 |
| Previous Midfoot Arthrodesis | 7 | 0.00600 |
| Talus Osteochondral Lesion | 7 | 0.00600 |
| Peroneal Tendinopathy | 7 | 0.00600 |
| Previous Talonavicular Arthrodesis | 7 | 0.00600 |
| Previous Lisfranc Lesion | 6 | 0.00515 |
| Lisfranc Lesion | 6 | 0.00515 |
| Subtalar Nonunion | 6 | 0.00515 |
Figure 3.
Diagnoses distribution.
The mean Foot and Ankle Offset (FAO) encountered in the study’s population was 2.43 (2.05-2.82, 95% CI; min -30.8, max 37.65; median 2.39). Figure 4 and Table 2 displays FAO distribution.
Figure 4.
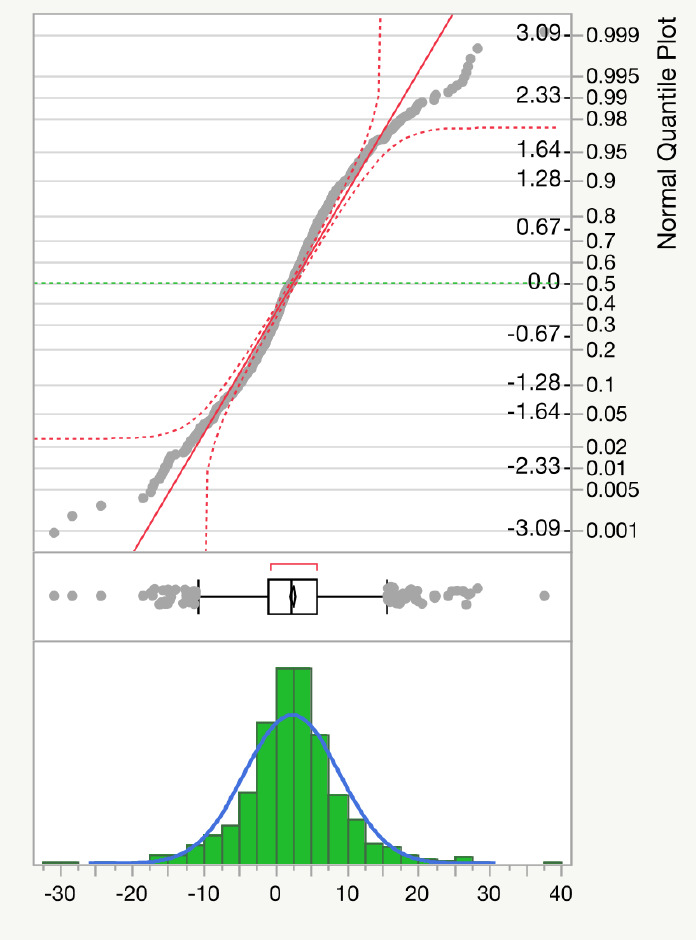
Foot and Ankle Offset (FAO) distribution over the analyzed population.
Table 2.
Fitted Normal Distribution to Foot and Ankle Offset Readings
| Parameter | Estimate | Std Error | Lower 95% | Upper 95% | |
|---|---|---|---|---|---|
| Location | μ | 2.4391278 | 0.1975659 | 2.0519056 | 2.8263499 |
| Dispersion | σ | 6.6559495 | 0.054185 | 6.5505916 | 6.6672228 |
| Measures | |||||
| -2*LogLikelihood | 7522.8007 | ||||
| AICc | 7526.8113 | ||||
| BIC | 7536.8695 | ||||
Discussion
Weight-bearing computed tomography (WBCT) is a reality in current orthopedic care and become a standard study in the assessment of foot and ankle patients at the University of Iowa. The use of this method is helping physicians and orthopedic surgeons to better diagnose, assess and treat patients. To the author’s knowledge, this is the first study to portray a substantial population of individuals that received a WBCT as standard clinical care, specifying diagnoses and demographics. Additionally, we demonstrated the largest collection of FAO in the literature across multiple diagnoses, and with accompanied control measurements that previous prospective investigations have utilized to establish possible patterns for symptomatic foot and ankle injuries.17 Within the study a total of 23 diagnoses had a sample size greater than 10, and 11 diagnoses had sample sizes of at least 25, which provided a greater diversity in clinical data than many of the prospective studies analyzing FAO for various pathological conditions.15,26 The calculated mean FAO of 2.43 (2.05-2.82, 95% CI) within our large, diverse population based on diagnoses, may represent a more accurate or true baseline measurement than what has been previously reported. Along the same lines, the present work provides diagnoses that are specific to each individual imaging study obtained. This is particularly important as previous epidemiological studies of this kind have limited their data to anatomical location of disease (ankle, midfoot, hindfoot, etc), which provides low granularity for applying clinical data to individualized patient care.27,28
Moreover, previous epidemiological studies utilizing large datasets of foot and ankle WBCTs have emphasized financial efficacy and radiation exposure relative to traditional weight bearing radiographs and standard CTs.27,28 A prior investigation by Richter et al. has demonstrated the superiority of WBCTs in comparison to traditional radiographs in the angle measures of the 1st – 2nd intermetatarsa, talo-metatarsal 1 (TMT) dorsoplantar and lateral projection, hindfoot angle, calcaneal pitch angle.29 Improvements in angle measurements utilizing WBCT were due to the function of weight-bearing’s effect on alignment for imaging and subsequent three-dimensional reconstruction to eliminate many of the technical difficulties present with capturing high quality traditional radiographs.29 The present work utilized WBCT for providing an accurate, reproducible measurement in FAO, across multiple pathologies as part of standard patient care. FAO has been previously utilized as a standard measure in multiple prospective studies and correlation with disease severity have been assessed.10,16,17 These measurements may aid in the establishment of anatomical variants for predisposition to various foot and ankle pathologies that can be accurately utilized by clinicians with various degrees of experience as previous studies have already demonstrated high intra-rater and inter-rater reliability.2,11,12
Likewise, the aim to establishing these type of measurements may also provide clinicians with the information necessary to accurately assess disease progression and need for surgical intervention by determining if patients demonstrate greater deviation from control measurement ranges, as previously presented for patients with syndesmotic injuries.21,30 Furthermore, the capability to utilize WBCT to demonstrate assess the three-dimensional relationship within the foot and ankle by calculating FAO cannot be understated. This measurement provides an accurate and readily reproducible biomechanical axis that can be correlated with severity of diseases in many instances and is highly reliable among different observers.1,13,14 For example, previous investigation on PCFD demonstrated a preoperative FAO of 9.8% (8.0-11.5, 95% CI) and FAO of 1.3% (-0.42.9, 95% CI) following surgical correction.31 This finding in small cohort of 19 patients (20 feet) was consistent with previous non-pathological values of an FAO of 2.3% (+-2.9) in normal patients, -11.6% (+-6.9) in varus and 11.4% (+-5.7) in valgus alignment.14,15 More importantly, these corrections demonstrated statistically significant correlation with positive clinical outcomes as assessed by patient reported outcome measures (PROs) postoperatively, which have gained greater emphasis recently as healthcare systems seek to reimburse patient care based on PROs.15,32
There are several limitations present withing this work. First, the study was retrospective in nature and data was acquired from a single institution in the Midwest region of the United States. The single center aspect of data collection and possible lack of diversity in patient demographics may limit the generalizability of the findings from the assimilated dataset. Moreover, there was no standardization in the methodology for the time periods that the WBCTs were obtained that limits the reproducibility of building a database for comparison. Further, the study is descriptive and provides an epidemiological dataset that cannot directly compare different interventions or pathologies no protocol was established indicating the rationale for WBCT acquisition, follow-up studies, or intended utilization of the study. Additionally, no comparisons between the different conditions identified within the study were performed, which could have demonstrated that other factors within the study population, including specific patient demographics, could have influence on FAO measurements. Moreover, no clinical evolution and outcomes measures were studied, which might have supported WBCT capability in changing the course and care of diseases, however other works have established relationships between WBCT measures and PROs.15,26 Finally, the dataset utilized a single observer for assessment and measurement of FAO that could theoretically skew the results and introduce bias. However, previous works have already demonstrated that intra and inter-rater reliability for this measure is high and is sustained across varying levels of experience.11
Conclusions
WBCTs from a total of 1175 feet and 820 unique patients were obtained over the study period. This study contains the largest cohort of WBCTs with accompanied FAO measurements to date, which can aid with establishing a new baseline FAO measurement for multiple pathological conditions. Acquiring WBCTs resulted in a variety of more specific diagnoses for patient with foot and ankle complaints. The ability to utilize WBCT for presurgical planning, the capability to provide a 3D reconstruction of patient anatomy, and its use for assessment of advanced relational foot and ankle measurements, such as FAO, demonstrate how WBCT may serve as a remarkable utility in clinical practice.
References
- 1.Barg A, Bailey T, Richter M, de Cesar Netto C, Lintz F, Burssens A, et al. Weightbearing Computed Tomography of the Foot and Ankle: Emerging Technology Topical Review. Foot Ankle Int. 2018;39(3):376–86. doi: 10.1177/1071100717740330. . PubMed PMID: 29171283. [DOI] [PubMed] [Google Scholar]
- 2.Bernasconi A, Cooper L, Lyle S, Patel S, Cullen N, Singh D, et al. Intraobserver and interobserver reliability of cone beam weightbearing semi-automatic three-dimensional measurements in symptomatic pes cavovarus. Foot Ankle Surg. 2020;26(5):564–72. doi: 10.1016/j.fas.2019.07.005. . PubMed PMID: 31378592. [DOI] [PubMed] [Google Scholar]
- 3.Cheung ZB, Myerson MS, Tracey J, Vulcano E. Weightbearing CT Scan Assessment of Foot Alignment in Patients With Hallux Rigidus. Foot Ankle Int. 2018;39(1):67–74. doi: 10.1177/1071100717732549. . PubMed PMID: 28971698. [DOI] [PubMed] [Google Scholar]
- 4.Conti MS, Ellis SJ. Weight-bearing CT Scans in Foot and Ankle Surgery. J Am Acad Orthop Surg. 2020;28(14):e595–e603. doi: 10.1177/1071100717732549. . PubMed PMID: 32692095. [DOI] [PubMed] [Google Scholar]
- 5.Barg A, Amendola RL, Henninger HB, Kapron AL, Saltzman CL, Anderson AE. Influence of Ankle Position and Radiographic Projection Angle on Measurement of Supramalleolar Alignment on the Anteroposterior and Hindfoot Alignment Views. Foot Ankle Int. 2015;36(11):1352–61. doi: 10.1177/1071100715591091. . PubMed PMID: 26116431. [DOI] [PubMed] [Google Scholar]
- 6.Kim JB, Yi Y, Kim JY, Cho JH, Kwon MS, Choi SH, et al. Weight-bearing computed tomography findings in varus ankle osteoarthritis: abnormal internal rotation of the talus in the axial plane. Skeletal Radiol. 2017;46(8):1071–80. doi: 10.1007/s00256-017-2655-0. . PubMed PMID: 28432396. [DOI] [PubMed] [Google Scholar]
- 7.Ferri M, Scharfenberger AV, Goplen G, Daniels TR, Pearce D. Weightbearing CT scan of severe flexible pes planus deformities. Foot Ankle Int. 2008;29(2):199–204. doi: 10.3113/FAI.2008.0199. Epub 2008/03/05. doi: 10.3113/ fai.2008.0199. PubMed PMID: 18315976. [DOI] [PubMed] [Google Scholar]
- 8.Mahmoud K, Metikala S, Mehta SD, Fryhofer GW, Farber DC, Prat D. The Role of Weightbearing Computed Tomography Scan in Hallux Valgus. Foot Ankle Int. 2020. . PubMed PMID: 33148045. [DOI] [PubMed]
- 9.de Cesar Netto C, Richter M. Use of Advanced Weightbearing Imaging in Evaluation of Hallux Valgus. Foot and ankle clinics. 2020;25(1):31–45. doi: 10.1016/j.fcl.2019.10.001. . PubMed PMID: 31997745. [DOI] [PubMed] [Google Scholar]
- 10.Lintz F, Mast J, Bernasconi A, Mehdi N, de Cesar Netto C, Fernando C, et al. 3D, Weight-bearing Topographical Study of Periprosthetic Cysts and Alignment in Total Ankle Replacement. Foot Ankle Int. 2020;41(1):1–9. doi: 10.1177/1071100719891411. . PubMed PMID: 31779466. [DOI] [PubMed] [Google Scholar]
- 11.de Cesar Netto C, Shakoor D, Dein EJ, Zhang H, Thawait GK, Richter M, et al. Influence of investigator experience on reliability of adult acquired flatfoot deformity measurements using weight-bearing computed tomography. Foot Ankle Surg. 2019;25(4):495–502. doi: 10.1016/j.fas.2018.03.001. . PubMed PMID: 30321961. [DOI] [PubMed] [Google Scholar]
- 12.Krähenbühl N, Tschuck M, Bolliger L, Hintermann B, Knupp M. Orientation of the Subtalar Joint: Measurement and Reliability Using Weight-bearing CT Scans. Foot Ankle Int. 2016;37(1):109–14. doi: 10.1177/1071100715600823. . PubMed PMID: 26293157. [DOI] [PubMed] [Google Scholar]
- 13.Zhang JZ, Lintz F, Bernasconi A, Zhang S. 3D Biometrics for Hindfoot Alignment Using Weightbearing Computed Tomography. Foot Ankle Int. 2019;40(6):720–6. doi: 10.1177/1071100719835492. . PubMed PMID: 30854889. [DOI] [PubMed] [Google Scholar]
- 14.Lintz F, Welck M, Bernasconi A, Thornton J, Cullen NP, Singh D, et al. 3D Biometrics for Hindfoot Alignment Using Weightbearing CT. Foot Ankle Int. 2017;38(6):684–9. doi: 10.1177/1071100717690806. . PubMed PMID: 28183212. [DOI] [PubMed] [Google Scholar]
- 15.Day J, de Cesar Netto C, Nishikawa DRC, Garfinkel J, Roney A, JOM M, et al. Three-Dimensional Biometric Weightbearing CT Evaluation of the Operative Treatment of Adult-Acquired Flatfoot Deformity. Foot Ankle Int. 2020;41(8):930–6. doi: 10.1177/1071100720925423. . PubMed PMID: 32506953. [DOI] [PubMed] [Google Scholar]
- 16.de Cesar Netto C, Myerson MS, Day J, Ellis SJ, Hintermann B, Johnson JE, et al. Consensus for the Use of Weightbearing CT in the Assessment of Progressive Collapsing Foot Deformity. Foot Ankle Int. 2020;41(10):1277–82. doi: 10.1177/1071100720950734. . PubMed PMID: 32851880. [DOI] [PubMed] [Google Scholar]
- 17.de Cesar Netto C, Bernasconi A, Roberts L, Pontin PA, Lintz F, Saito GH, et al. Foot Alignment in Symptomatic National Basketball Association Players Using Weightbearing Cone Beam Computed Tomography. Orthopaedic journal of sports medicine. 2019;7(2):2325967119826081. doi: 10.1177/2325967119826081. . PubMed PMID: 30815498; PubMed Central PMCID: PMCPMC6385333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lintz F, Beaudet P, Richardi G, Brilhault J. Weight-bearing CT in foot and ankle pathology. Orthopaedics & Traumatology: Surgery & Research. 2020. p. 102772. [DOI] [PubMed]
- 19.Conti MS, Ellis SJ. Weight-bearing CT Scans in Foot and Ankle Surgery. JAAOS - Journal of the American Academy of Orthopaedic Surgeons. 2020;28(14):e595–e603. doi: 10.5435/jaaos-d-19-00700. . PubMed PMID: 00124635-202007150-00005. [DOI] [PubMed] [Google Scholar]
- 20.Willey MC, Compton JT, Marsh JL, Kleweno CP, Agel J, Scott EJ, et al. Weight-Bearing CT Scan After Tibial Pilon Fracture Demonstrates Significant Early Joint-Space Narrowing. J Bone Joint Surg Am. 2020;102(9):796–803. doi: 10.2106/jbjs.19.00816. . PubMed PMID: 32379120. [DOI] [PubMed] [Google Scholar]
- 21.Hagemeijer NC, Chang SH, Abdelaziz ME, Casey JC, Waryasz GR, Guss D, et al. Range of Normal and Abnormal Syndesmotic Measurements Using Weightbearing CT. Foot Ankle Int. 2019;40(12):1430–7. doi: 10.1177/1071100719866831. . PubMed PMID: 31442094. [DOI] [PubMed] [Google Scholar]
- 22.Lintz F, Bernasconi A, Baschet L, Fernando C, Mehdi N, De Cesar Netto C. Relationship Between Chronic Lateral Ankle Instability Hindfoot Varus Using Weight-Bearing Cone Beam Computed Tomography. Foot & Ankle International. 2019;40(10):1175–81. doi: 10.1177/1071100719858309. [DOI] [PubMed] [Google Scholar]
- 23.Welck MJ, Myerson MS. The value of Weight-Bearing CT scan in the evaluation of subtalar distraction bone block arthrodesis: Case report. Foot Ankle Surg. 2015;21(4):e55–9. doi: 10.1016/j.fas.2015.08.002. . PubMed PMID: 26564734. [DOI] [PubMed] [Google Scholar]
- 24.Hirschmann A, Buck FM, Fucentese SF, Pfirrmann CWA. Upright CT of the knee: the effect of weight-bearing on joint alignment. European Radiology. 2015;25(11):3398–404. doi: 10.1007/s00330-015-3756-6. [DOI] [PubMed] [Google Scholar]
- 25.Hirschmann A, Buck FM, Herschel R, Pfirrmann CWA, Fucentese SF. Upright weight-bearing CT of the knee during flexion: changes of the patellofemoral and tibiofemoral articulations between 0° and 120°. Knee Surgery, Sports Traumatology, Arthroscopy. 2017;25(3):853–62. doi: 10.1007/s00167-015-3853-8. [DOI] [PubMed] [Google Scholar]
- 26.Day MA, Ho M, Dibbern K, Rao K, An Q, Anderson DD, et al. Correlation of 3D Joint Space Width From Weightbearing CT With Outcomes After Intra-articular Calcaneal Fracture. Foot Ankle Int. 2020;41(9):1106–16. doi: 10.1177/1071100720933891. . PubMed PMID: 32648780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Richter M, Lintz F, de Cesar Netto C, Barg A, Burssens A, Ellis S. Results from more than 13,000 Weight-Bearing CT scans over 6.8 years. Impact on costs, radiation exposure and time spent. Fuß & Sprunggelenk. 2020.
- 28.Richter M, Lintz F, de Cesar Netto C, Barg A, Burssens A. Results of more than 11,000 scans with weightbearing CT - Impact on costs, radiation exposure, and procedure time. Foot Ankle Surg. 2020;26(5):518–22. doi: 10.1016/j.fas.2019.05.019. . PubMed PMID: 31239196. [DOI] [PubMed] [Google Scholar]
- 29.Richter M, Seidl B, Zech S, Hahn S. PedCAT for 3D-imaging in standing position allows for more accurate bone position (angle) measurement than radiographs or CT. Foot Ankle Surg. 2014;20(3):201–7. doi: 10.1016/j.fas.2014.04.004. [DOI] [PubMed] [Google Scholar]
- 30.Hamard M, Neroladaki A, Bagetakos I, Dubois-Ferrière V, Montet X, Boudabbous S. Accuracy of cone-beam computed tomography for syndesmosis injury diagnosis compared to conventional computed tomography. Foot Ankle Surg. 2020;26(3):265–72. doi: 10.1016/j.fas.2019.03.006. . PubMed PMID: 30992183. [DOI] [PubMed] [Google Scholar]
- 31.Dagneaux L, Dufrenot M, Bernasconi A, Bedard NA, de Cesar Netto C, Lintz F. Three-Dimensional Biometrics to Correlate Hindfoot and Knee Coronal Alignments Using Modern Weightbearing Imaging. Foot Ankle Int. 2020;41(11):1411–8. doi: 10.1177/1071100720938333. . PubMed PMID: 32698631. [DOI] [PubMed] [Google Scholar]
- 32.Squitieri L, Bozic KJ, Pusic AL. The Role of Patient-Reported Outcome Measures in Value-Based Payment Reform. Value Health. 2017;20(6):834–6. doi: 10.1016/j.jval.2017.02.003. . PubMed PMID: 28577702; PubMed Central PMCID: PMCPMC5735998. [DOI] [PMC free article] [PubMed] [Google Scholar]