Abstract
Background:
Inaccuracy of ankle syndesmotic repair via reduction and trans-syndesmotic fixation can occur during ankle fracture repair. The goal of this study was to determine whether reduction and fixation of the posterior malleolar fracture (PM) fragment in rotational ankle fractures reduces the need for independent syndesmotic screw fixation.
Methods:
A retrospective study was conducted using a consecutive series of patients treated operatively for a rotationally unstable ankle fracture with a PM fragment between 2011-2017. All ankle fractures underwent open reduction and internal fixation and divided into two groups: PM fixed or not fixed. An intraoperative stress evaluation of the ankle following bony fixation was performed in all cases to evaluate syndesmotic instability. Patient and fracture characteristics, and intraoperative instability and trans-syndesmotic fixation were compared between both groups.
Results:
Eighty-five unstable ankle fractures that had a PM fragment were identified. Forty-three fractures underwent PM fixation and 42 did not. There were no differences between the PM fixation groups with regard to age, gender, body mass index or fracture pattern (p>0.183 for all). On average, PM fragments in the fixed group were larger than those not fixed (p<0.001). There were significantly lower odds of needing syndesmotic fixation if the PM fragment was reduced and fixed (p<0.001). Only 2 out of 43 ankles with a fixed PM fragment underwent syndesmotic fixation compared with 34 out of 42 non-fixed PM fragments.
Conclusion:
Posterior malleolar fixation imparts syndesmotic stability and may obviate the need for trans-syndesmotic fixation for restoring dynamic ankle mortise congruence.
Level of Evidence: III
Keywords: ankle fractures, posterior malleolus, operative treatment
Introduction
Posterior malleolar (PM) fractures are a common component in rotational ankle fractures and occur in up to 44-46% of all ankle fractures.1,2 The presence of a PM fragment in ankle fracture is likely indicative of worse clinical outcomes.3 When planning for open reduction and internal fixation (ORIF) of a rotational ankle fracture, the decision to fix the PM fragment is highly variable among surgeons.4 Fragment size (percentage distal tibial articular surface), which is implicated in long-term arthritic changes,5 has been the main determining factor for most surgeons, with 25-33% of the articular surface as the cited threshold for fixation.6 However, there is generally no consensus on whether or not to fix smaller PM fragments.
The anatomic relationship between the PM fragment of the distal tibia and the ankle syndesmosis through the posteroinferior tibiofibular ligament (PITFL) is well established. Anatomic reduction and stable fixation of this fragment is technically feasible through the posterolateral approach7 and can restore the previously disrupted PITFL complex in addition to restoring the tibiotalar articular surface and contact area.8,9 Restoring the PITFL along with fibular fixation should confer stability to the syndesmosis, and may potentially limit the need for trans-syndesmotic reduction and screw fixation.
Trans-syndesmotic reduction and direct fixation of an unstable syndesmosis has been demonstrated to have a high rate of malreduction (30-40%) on computed tomography (CT) imaging.10,11 Furthermore, malreduction of the syndesmosis can alter ankle kinematics and has been associated with poorer functional outcomes.11-13 Recent evidence suggests that syndesmotic stabilization through PM fixation has outcomes that are at least equivalent to syndesmotic screw fixation on follow-up.14 These findings merit further investigation to determine whether surgeons should be more aggressive about fixing PM fragments.
The primary aim of this study is to determine whether PM reduction and internal fixation reduces the need for trans-syndesmotic fixation in rotational ankle fractures. As a secondary aim, the effect of fragment size on this relationship will be examined. We hypothesize that fixation of the PM fragment, regardless of size, confers stability to the syndesmosis and obviates the need for trans-syndesmotic fixation.
Methods
Study Design and Patient Population
A retrospective review was performed on an institutional review board-approved database of subjects who underwent ankle ORIF by any of 4 orthopedic trauma surgeons at one urban, academic institution from 2011-2017. Three hundred and sixty patients were identified. Patients 18 and older, with rotational ankle fracture patterns involving a posterior malleolar fragment were included in this study. Subjects with non-rotational ankle and distal tibia fractures, or fracture patterns without a posterior malleolar fragment, and subjects with incomplete pre-operative and fluoroscopic imaging were excluded. Using these criteria, 85 patients (23.6%) with 85 bi- or trimalleolar fractures make up our study cohort (Figure 1). The posterior malleolus fragment was reduced and fixed in 43 and not fixed in 42 subjects forming the two comparison groups in this study.
Figure 1.
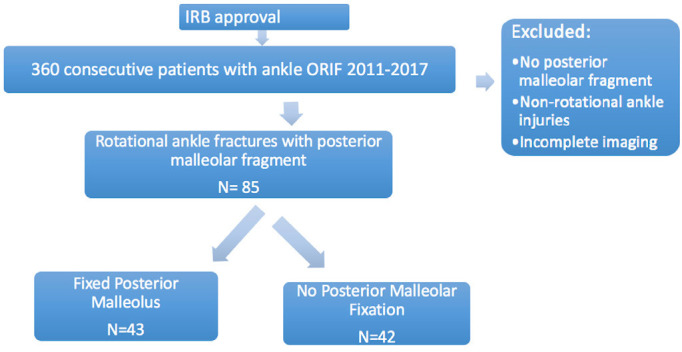
Flow Diagram illustrating the retrospective study sampling method and subject inclusion for analysis.
Surgical Technique
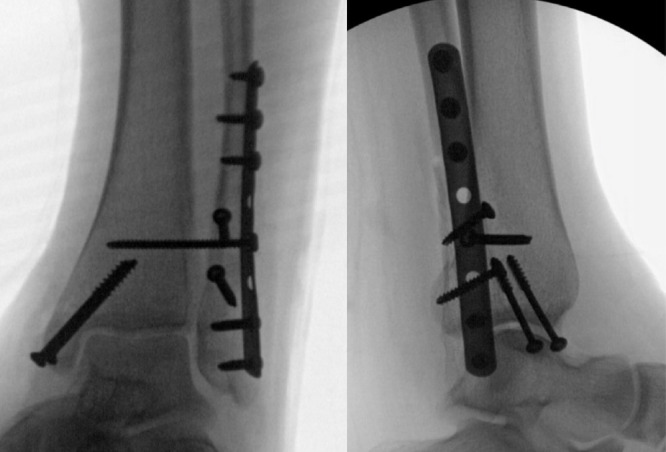
In either case, all fractures underwent open reduction and internal fixation using standard fixation principles with small fragment plates and screws. In cases in which the posterior malleolus was not fixed the patient was positioned supine. The decision on whether or not to fix the fragment was surgeon-dependent, but mainly predicated on fragment size and articular involvement. If the decision to fix the posterior malleolus was made it was done with an open approach if the fragment was displaced. In two cases where the fragment was not displaced, fixation in situ was performed with anteroposterior partially threaded cannulated screws. The patient was positioned depending on the pre-operative plan decided by the surgeon. A posterolateral approach between the flexor hallucis longus and the peroneal tendons was typically performed in the lateral or prone position. In this setting, the fibula was typically fixed first with a posteriorly placed anti-glide plate, followed by reduction of the posterior malleolar fragment and fixation with a plate and screws (Figure 2) or lag screws alone. Medial malleolar fixation was performed last, and done either in the prone position or after switching to supine position depending on surgeon preference.
Figure 2.

Post-operative images of a trimalleolar ankle fracture (a) AP, (b) lateral with a posterior malleolar fragment that was fixed with a posterior antiglide plate through a posterolateral approach.
It was our standard protocol to perform an external rotation stress test following fibular, posterior and medial malleolar fixation, to determine stability of the syndesmosis under fluoroscopy. Loss of tibiofibular overlap (<1mm) or increase in tibiofibular clear space (>5mm) on the stress view indicated syndesmotic instability, which was typically addressed using transsyndesmotic fully-threaded cortical screws (Figure 3) or TightRope®(Arthrex, Naples Fla) transosseous suture and endo-button fixation. If trans-syndesmotic screw fixation was elected, the number of screws, and cortices of purchase varied depending on surgeon preference, and patient factors (diabetes, obesity). Reduction of the syndesmosis by anatomically aligning the fibula to the tibial incisura with or without the use of clamps was performed if needed depending on the extent of syndesmotic widening and disruption. All syndesmotic reductions were assessed on biplanar fluoroscopic imaging and accepted if adequate. Post-operatively all patients in this study were treated with a standardized protocol that included, non-weight bearing for a period of 6 weeks, and started early ankle range of motion with physical therapy. Venous thromboembolic disease prophylaxis was maintained in all cases with either low molecular weight heparin or an aspirin daily for 4 weeks.
Figure 3.
Post-operative images of a trimalleolar ankle fracture (a) AP, (b) lateral with a posterior malleolar fragment that was not directly fixed, and trans-syndesmotic fixation with one fully threaded tri-cortical screw used to stabilize the syndesmosis.
Radiographic Review
Complete pre-operative radiographic imaging as well as intra-operative fluoroscopy were reviewed by two authors (OB, RN) to determine radiographic parameters such as posterior malleolar fragment size, as well as whether the syndesmosis was unstable to intra-operative external rotation stress examination. In patients requiring syndesmotic screw fixation, the reduction was assessed intra-operatively and judged to be adequate. based upon standard image intensification views. On pre-operative radiographs, the ankle fracture pattern was classified as bi- or tri-malleolar, as well as the presence of medial clear space widening, and loss of tibiofibular overlap. The size of the posterior malleolar fragment as a percentage of the distal tibial articular surface was measured on the lateral view as historically described by Hartford8 utilizing the ruler function on the digital x-ray system (PACS, Siemens, Ehrlanger Germany). Despite the underestimate of fragment size on lateral x-ray views given the posterolateral orientation of the fragment, all measurements were performed with the same standard using x-ray imaging, as not all subjects had computed tomography imaging pre-operatively.
Statistical Analysis
Baseline patient demographics and characteristics were compared between the two groups of posterior malleolus fixation using independent samples t-test or Fisher’s exact test as appropriate. To address the primary hypothesis, Fisher’s exact test was used to compare both groups of posterior malleolar fixation on the proportions of syndesmotic instability requiring trans-syndesmotic fixation. This relationship was also tested using a binary logistic regression model controlling for posterior malleolar fragment size. All statistical analysis was performed using Statistical Package for Social Sciences (SPSS Version 23).
Results
With the numbers available, there were no statistical differences in age, gender, body mass index (BMI) or fracture pattern (bi or trimalleolar) between both groups of PM fixation (p>0.183 for all) (Table 1). The average age of patients in this study sample was 51 years and 62% were female. The mean BMI was 28, and the majority of ankle fractures in this sample were tri-malleolar (86%). The average size of the PM in the fixed group was 27% ± 9% of the articular surface, whereas the size among those not fixed was 19% ± 8% (p<0.001).
Table 1.
Baseline Patient Demographics and Ankle Fracture Characteristics by Group of Posterior Malleolar Fixation
| Group of Posterior Malleolar Fixation | ||||
|---|---|---|---|---|
| Fixed (n=43) | Not fixed (n=42) | P-value | ||
| Baseline Characteristic | Age (years) | 50 ± 17 | 51 ± 18 | 0.756 |
| Gender (M / F) | Females = 30 Males = 13 |
Females = 23 Male = 19 |
0.183 | |
| Body Mass Index (kg/m2) | 28 ± 5 | 28 ± 7 | 0.641 | |
| Bi- or Trimalleolar | Bi = 7 Tri = 36 |
Bi = 5 Tri = 37 |
0.757 | |
| Posterior Malleolar Fragment (% of articular surface) | 27% ± 9% | 19% ± 8% | <0.001 * | |
Among all fixed PM fragments that were fixed, 39 (91%) were fixed with plates (T or 1/3 tubular plates) and 4 (9%) were fixed with anteroposterior partially-threaded screws. Thirty-four (94%) of all trans-syndesmotic fixations were performed using one or two fully threaded screws drilled and placed in a holding position, and 2 (6%) were performed using a suture over a button device (TightRope®, Arthex).
Only 2 (4.6%) syndesmotic complexes were found to be unstable following PM fixation, both requiring syndesmotic screw fixation, compared with 34 (80.9%) unstable syndesmotic complexes when the PM was not fixed (Figure 4) (Figure 2) (p<0.001). The odds ratio of requiring syndesmotic fixation if the PM was fixed was 0.011 (95% CI: 0.002-0.058). The association between persistent syndesmotic instability and PM fixation remained significant in a binary logistic regression model controlling for PM fragment size (p<0.001). Finally, when comparing posterolateral incisions and dissection for PM fixation (n=39) to direct lateral fibular approaches in cases with percutaneous or without PM fixation (n=46), there were only two cases of post-operative wound complications, one in either group (p=1.000).
Figure 4.
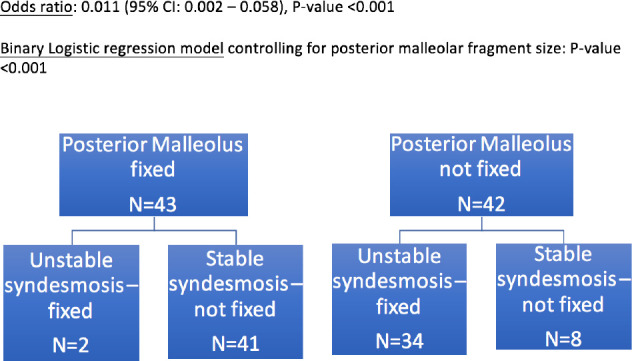
Flow Diagram demonstrating the number of cases which required trans-syndesmotic fixation secondary to syndesmotic instability between the two groups.
Discussion
This clinical study confirms our belief that PM fixation increases syndesmotic complex stability and may reduce the need for independent trans-syndesmotic fixation. Reduction and fixation of the PM fragment anatomically restores the syndesmosis and may be anatomically and biomechanically more superior to trans-syndesmotic fixation. This explains why 95% of all of the fixed PM ankles in this study did not demonstrate residual instability on stress exam following PM fixation. A study of postoperative CT scans comparing ankles in which PM was fixed regardless of fragment size to those with syndesmotic screws only, demonstrated improved reduction of the syndesmotic articulation with PM fixation, than with direct trans-syndesmotic screw fixation.15 Furthermore, PM fixation has been demonstrated to restore 70% of syndesmotic stiffness compared with 40% with syndesmotic screws, in a cadaver study.16 This is concordant with other evidence demonstrating that PITFL injury has the highest predictive value for syndesmotic instability compared with the other syndesmotic ligaments.17 Moreover, PM fixation through an open, posterolateral approach was not associated with any increased risk of wound complications compared with a direct lateral fibular incision.
It is unclear why in 2 cases out of 43, the syndesmosis was found to be unstable after PM fixation, requiring separate trans-syndesmotic screws. One hypothesis is that there may have been significant stripping of the PITFL iatrogenically during the identification of the fragment, such that restoring the PM fragment no longer restored the PITFL function.
Apart from restoring syndesmotic stability, PM fixation restores the distal tibial articular surface, which holds important implications for tibiotalar contact area and pressures. Size of the PM fragment has been inversely correlated with tibiotalar contact area,8,18 which forms the basis of using fragment size for surgical indication of fixation. Moreover, PM fragment size >5% of the articular surface, and residual articular step off of >=1mm have been correlated with development of tibiotalar arthritis.5 These findings are suggestive that PM fixation, even in small fragments, may impede degenerative changes of the tibiotalar joint. More long-term evidence is needed to investigate this relationship.
Trans-syndesmotic fixation, although widely used, is associated with high rates of malreduction which is associated with poorer functional outcomes. Davidovitch et al., found a 30-38% rate of syndesmotic malreduction whether standard fluoroscopy or intraoperative CT scan were used.10 Another study by Sagi et al., demonstrated a 44% rate of malreduction with closed reduction of the syndesmosis intraoperatively, compared with 15% malreduction rate with open reduction of the syndesmosis.11 This high rate of malreduction is not inconsequential, and is associated with worse functional outcome scores.11,12 Direct comparisons between the clinical outcomes of trans-syndesmotic fixation and PM fixation are limited in the existing literature. Miller et al., found equivalent outcomes scores between both methods in 1 year follow-up.14 Another study demonstrated worse clinical outcomes at 1 year in subjects who had syndesmotic fixation in addition to malleolar fixation, compared with malleolar fixation alone, but this included lateral and medial malleoli.13 Given the well-studied biomechanical and anatomic advantages of PM fixation compared with trans-syndesmotic fixation, more evidence is needed on the clinical outcomes between both, over long-term follow-up, to better guide surgical indications.
One limitation of this study is the lack of postoperative assessment of syndesmotic reduction for all treated ankles because post-operative CT scans were not obtained. Plain films have been shown to be significantly less accurate than CT at assessing syndesmotic reduction.19 Other limitations of this study include its retrospective nature, and therefore inherently prone to selection bias with case selection. Furthermore, the sample size was too limited to allow for further multi-variable control of other potentially confounding variables including patient demographics and ankle fracture characteristics. Finally, there are other potentially confounding variables that were not captured in this database including the surgeon’s indication to fix the PM fragment, PM reduction and fixation technique and energy and mechanism of injury, which may be related to syndesmotic stability after PM fixation. Finally, we have no patient reported outcomes to determine whether this approach to syndesmotic fixation makes difference in clinical outcomes.
Conclusion
The results of this study suggest that posterior malleolar fixation may be an alternative to trans-syndesmotic fixation for restoring ankle stability while potentially avoiding the risks of tibiofibular malreduction and compromised functional outcomes that result from direct trans-syndesmotic fixation. Further study is needed to validate these findings and compare the accuracy of syndesmotic reduction as well as clinical outcomes.
Acknowledgements
The authors would like to recognize the efforts of Abdullah Qatu, BSE in preparing the database that was ultimately used in this study.
References
- 1.Court-Brown CM, McBirnie J, Wilson G. Adult ankle fractures--an increasing problem? Acta orthopaedica Scandinavica. 1998;69:43–47. doi: 10.3109/17453679809002355. [DOI] [PubMed] [Google Scholar]
- 2.Jehlicka D, Bartonicek J, Svatos F, et al. [Fracture-dislocations of the ankle joint in adults. Part I: epidemiologic evaluation of patients during a 1-year period] Acta chirurgiae orthopaedicae et traumatologiae Cechoslovaca. 2002;69:243–247. [PubMed] [Google Scholar]
- 3.Tejwani NC, Pahk B, Egol KA. Effect of posterior malleolus fracture on outcome after unstable ankle fracture. The Journal of trauma. 2010;69:666–669. doi: 10.1097/TA.0b013e3181e4f81e. [DOI] [PubMed] [Google Scholar]
- 4.Irwin TA, Lien J, Kadakia AR. Posterior malleolus fracture. The Journal of the American Academy of Orthopaedic Surgeons. 2013;21:32–40. doi: 10.5435/JAAOS-21-01-32. [DOI] [PubMed] [Google Scholar]
- 5.Drijfhout van Hooff CC, Verhage SM, Hoogendoorn JM. Influence of fragment size and postoperative joint congruency on long-term outcome of posterior malleolar fractures. Foot & ankle international / American Orthopaedic Foot and Ankle Society [and] Swiss Foot and Ankle Society. 2015;36:673–678. doi: 10.1177/1071100715570895. [DOI] [PubMed] [Google Scholar]
- 6.De Vries JS, Wijgman AJ, Sierevelt IN, et al. Long-term results of ankle fractures with a posterior malleolar fragment. The Journal of foot and ankle surgery: official publication of the American College of Foot and Ankle Surgeons. 2005;44:211–217. doi: 10.1053/j.jfas.2005.02.002. [DOI] [PubMed] [Google Scholar]
- 7.Verhage SM, Boot F, Schipper IB, et al. Open reduction and internal fixation of posterior malleolar fractures using the posterolateral approach. The bone & joint journal. 2016;98B:812–817. doi: 10.1302/0301-620X.98B6.36497. [DOI] [PubMed] [Google Scholar]
- 8.Hartford JM, Gorczyca JT, McNamara JL, et al. Tibiotalar contact area. Contribution of posterior malleolus and deltoid ligament. Clinical orthopaedics and related research. 1995. pp. 182–187. [PubMed]
- 9.Solan MC, Sakellariou A. Posterior malleolus fractures: worth fixing. The bone & joint journal. 2017;99B:1413–1419. doi: 10.1302/0301-620X.99B11.BJJ-2017-1072. [DOI] [PubMed] [Google Scholar]
- 10.Davidovitch RI, Weil Y, Karia R, et al. Intraoperative syndesmotic reduction: three-dimensional versus standard fluoroscopic imaging. The Journal of bone and joint surgery American volume. 2013;95:1838–1843. doi: 10.2106/JBJS.L.00382. [DOI] [PubMed] [Google Scholar]
- 11.Sagi HC, Shah AR, Sanders RW. The functional consequence of syndesmotic joint malreduction at a minimum 2-year follow-up. Journal of orthopaedic trauma. 2012;26:439–443. doi: 10.1097/BOT.0b013e31822a526a. [DOI] [PubMed] [Google Scholar]
- 12.Chen DW, Li B, Yu GR. Functional. consequence of syndesmotic malreduction. Journal of orthopaedic trauma. 2013;27:e247. doi: 10.1097/BOT.0b013e3182a7020b. [DOI] [PubMed] [Google Scholar]
- 13.Egol KA, Pahk B, Walsh M, et al. Outcome after unstable ankle fracture: effect of syndesmotic stabilization. Journal of orthopaedic trauma. 2010;24:7–11. doi: 10.1097/BOT.0b013e3181b1542c. [DOI] [PubMed] [Google Scholar]
- 14.Miller AN, Carroll EA, Parker RJ, et al. Posterior malleolar stabilization of syndesmotic injuries is equivalent to screw fixation. Clinical orthopaedics and related research. 2010;468:1129–1135. doi: 10.1007/s11999-009-1111-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Miller AN, Carroll EA, Parker RJ, et al. Direct visualization for syndesmotic stabilization of ankle fractures. Foot & ankle international / American Orthopaedic Foot and Ankle Society [and] Swiss Foot and Ankle Society. 2009;30:419–426. doi: 10.3113/FAI-2009-0419. [DOI] [PubMed] [Google Scholar]
- 16.Gardner MJ, Brodsky A, Briggs SM, et al. Fixation of posterior malleolar fractures provides greater syndesmotic stability. Clinical orthopaedics and related research. 2006;447:165–171. doi: 10.1097/01.blo.0000203489.21206.a9. [DOI] [PubMed] [Google Scholar]
- 17.Park YH, Yoon MA, Choi WS, et al. The predictive value of MRI in the syndesmotic instability of ankle fracture. Skeletal radiology. 2017. [DOI] [PubMed]
- 18.Macko VW, Matthews LS, Zwirkoski P, et al. The joint-contact area of the ankle. The contribution of the posterior malleolus. The Journal of bone and joint surgery American volume. 1991;73:347–351. [PubMed] [Google Scholar]
- 19.Gardner MJ, Demetrakopoulos D, Briggs SM, et al. Malreduction of the tibiofibular syndesmosis in ankle fractures. Foot & ankle international / American Orthopaedic Foot and Ankle Society [and] Swiss Foot and Ankle Society. 2006;27:788–792. doi: 10.1177/107110070602701005. [DOI] [PubMed] [Google Scholar]


