Abstract
Chronic lymphocytic inflammation with pontine perivascular enhancement responsive to steroids (CLIPPERS) is a rare and poorly understood pathology. In this case report we present a 51-year-old male that presented with neurological deficits with recent hypersensitivity pneumonitis. Imaging studies showed multiple punctate enhancing lesions involving the brainstem. After initiation of corticosteroids his symptoms improved, with a decrease in size of his lesions 6-months after his initial presentation. Due to its misdiagnosis, we propose the use of diagnostic criteria, described on this case report, for prompt treatment to avoid neurological sequelae.
Keywords: CLIPPERS, Pons, Hypersensitivity pneumonitis, Brain MRI
Introduction
Chronic lymphocytic inflammation with pontine perivascular enhancement responsive to steroids (CLIPPERS) is a rare pathology [1]. CLIPPERS prevalence is still unknown, recently found to have a male predilection with a mean age onset at 50 years [2]. It has been described with a subacute clinical presentation involving predominantly the brainstem and cranial nerves, symptoms can include ataxia, dysarthria or oculomotor abnormalities [3]. On Magnetic Resonance Imaging (MRI) it is characterized as multiple punctate and curvilinear perivascular enhancements peppering the pons [4] with a good response to steroid treatment [5]. Response to immunosuppressive agents suggests an immune-mediated pathology [3]. We present a case of CLIPPERS in a patient with recent hypersensitivity pneumonitis.
Case report
A 51-year-old man admitted to the hospital referring a one-week sudden onset of right-sided extremity weakness which was subsequently followed with development of diplopia. Pertinent previous medical history included recent hypersensitivity pneumonitis diagnosed 5 months ago, with a relapse one month prior to presentation (Fig. 1). Neurological examination was remarkable for left facial nerve palsy, right extremity weakness and right-sided gaze evoked horizontal nystagmus.
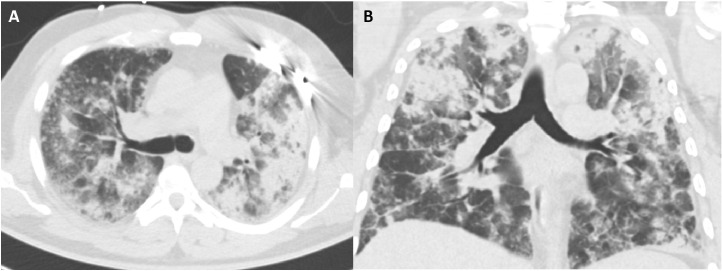
Fig. 1.
Axial (A) and coronal (B) non-contrast high-resolution CT chest in lung window at the level of the carina, performed 1 month prior to presentation. Demonstrates diffuse bilateral groundglass densities with peribronchial thickening, predominantly in the upper lobes, as well as scattered perilymphatic nodules.
Unenhanced head computed tomography scan performed to evaluate for stroke was unremarkable for acute intracranial process. Subsequently a brain MRI was performed, which revealed numerous punctate enhancing lesions involving the pons, middle cerebellar peduncle, medial cerebellar lobes, middle frontal gyrus, cingulate gyrus and corona radiata (Fig. 2). Initial differential considerations were broad including but not limited to CLIPPERS, neuro-Behçet, neurosarcoidosis, lymphoma, demyelinating lesions, and Bickerstaff brainstem encephalitis. In view of these abnormal findings, he underwent an extensive laboratory workup; as well as started on high dose prednisone.
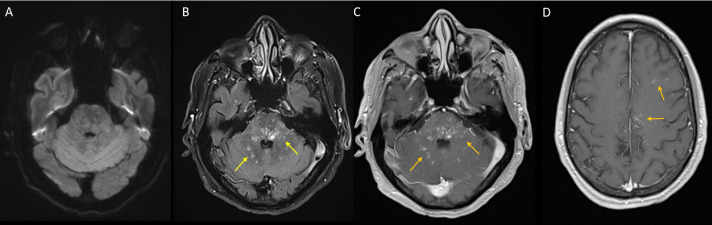
Fig. 2.
Initial brain MRI. Axial DWI (A) is negative for restricted diffusion. Axial FLAIR at the level of the middle cerebellar peduncles shows multiple punctate foci of increased signal intensity within the pons, middle cerebellar peduncles and medial cerebellar lobes (B, yellow arrows). Post-gadolinium enhanced non-fat saturated axial T1WI at the level of the middle cerebellar peduncles (C) and at the level of the corona radiata (D) demonstrates multiple punctate enhancing foci within the pons, middle cerebellar peduncles and medial cerebellar lobes (C, orange arrows), middle frontal gyrus and cingulate gyrus (D, orange arrows). (Color version of figure is available online.)
Blood cell count and biochemical parameters were within normal range, and serum analysis was negative for multiple infections (including toxoplasmosis, herpes, Epstein-Barr virus, west Nile virus, cytomegalovirus, histoplasma, varicella zoster) as well as angiotensin converting enzyme (ACE).
Cerebral spinal fluid (CSF) obtained by lumbar puncture was negative for any significant abnormality. Blood count and antigen/antibody testing for infectious agents were negative.
After an exhaustive negative clinical workup, review of the imaging differentials left CLIPPERS as a possible diagnosis of exclusion. The patient underwent treatment with high dose intravenous methylprednisolone 1 g/day over 5 days, followed by a maintenance dose of prednisone 40 mg/day which resulted in significant clinical improvement just after 4 days of treatment. The follow-up contrast enhanced brain MRI performed 10 days after presentation revealed a significant improvement of the number and enhancement of previously noted punctate enhancing lesions (Fig. 3). Upon discharge he was continued on low dose prednisone 40 mg/day and mycophenolate total of 1000 mg/day. On 2 month follow-up brain MRI, there were persistent multiple small hyperintense lesions involving the pons, middle cerebellar peduncles and medial cerebellar lobes, with interval development of new lesions in the superior frontal gyrus (Fig. 4). At the time of this follow-up his prednisone dose was decreased to 20 mg/day and mycophenolate to a total of 750 mg/day. Because of relapse state, corticosteroids, as well as immunosuppressant doses were again increased. Upon 6-month follow up brain MRI, there were considerable improvement of size and number of previously noted lesions (Fig. 5).
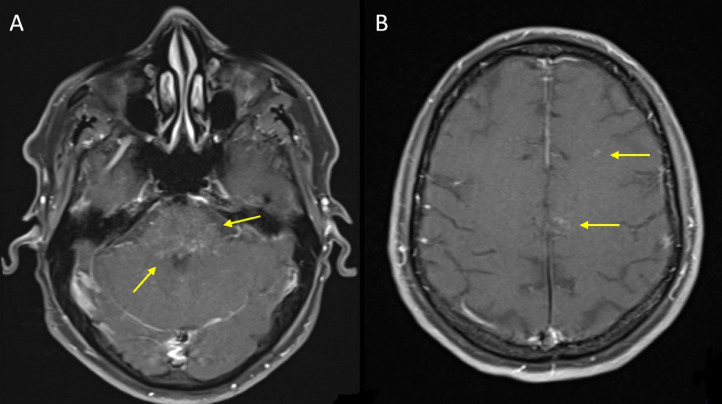
Fig. 3.
Follow-up brain MRI at day 10 after initial presentation. Post-gadolinium enhanced fat saturated axial T1WI at the level of the middle cerebellar peduncles (A) and corona radiata (B), demonstrating interval decrease in number and intensity of previously noted enhancing foci within the pons, middle cerebellar peduncles and medial cerebellar lobes (A, yellow arrows), middle frontal gyrus and cingulate gyrus (B, yellow arrows). (Color version of figure is available online.)
Fig 4.
Follow-up brain MRI at 2 months after initial presentation. Post-gadolinium enhanced fat saturated axial T1WI at the level of the middle cerebellar peduncles (A) and vertex (B), demonstrates interval increase in number and intensity of previously noted enhancing foci within the pons, middle cerebellar peduncles and medial cerebellar lobes (A, yellow arrows), new punctate enhancing foci involving the superior frontal gyrus (B) (yellow arrows). (Color version of figure is available online.)
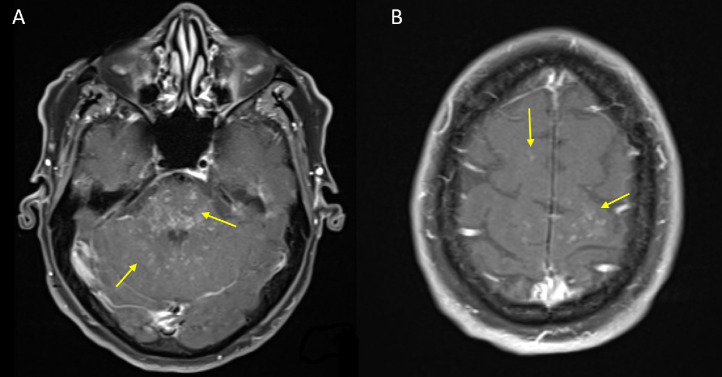
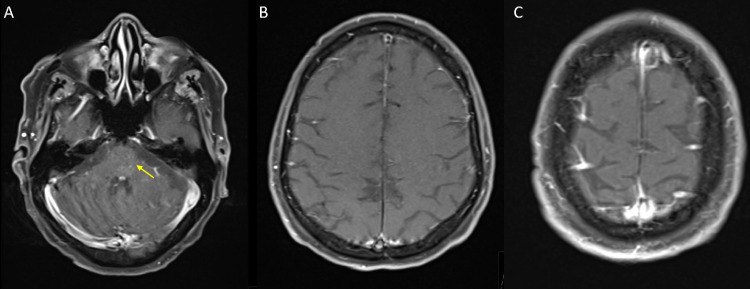
Fig 5.
Follow-up brain MRI at 6 months after initial presentation. Contrast enhanced fat saturated axial T1WI at the level of the middle cerebellar peduncles (A), corona radiata (B) and vertex (C), demonstrate substantial decrease in number and intensity of previously noted multiple punctate enhancing foci within the pons, middle cerebellar peduncles and medial cerebellar lobes (A, yellow arrow) and almost complete resolution of previously noted punctate enhancing foci involving the bilateral superior frontal gyri, left middle frontal gyrus and left cingulate gyrus (B,C). (Color version of figure is available online.)
Discussion
CLIPPERS syndrome is a relatively newly described pathology; it was first described in 2010 by Pittock et al. on 8 cases that showed a characteristic MRI pattern of punctate and curvilinear enhancements peppering the pons [1].
The pathogenesis of CLIPPERS is poorly understood. Multiple hypotheses have been proposed regarding the exact etiology of this disorder as well as to its predilection to affect specific parts of the brain. The most accepted hypothesis is one explaining this disease as an autoimmune disorder, with a specific immune-mediated response against antigens in the perivascular regions adjacent to the pons [3]. An interesting feature of our patient is his recent history of hypersensitivity pneumonitis, this raises the possibility of a triggering event. Only a handful of cases have been found with predisposing pathologies seen after influenza vaccine, herpes zoster infection and prior history of allergies [6], [7], [8]. Hypersensitivity pneumonitis is also an immune-mediated disease [9]. One possibility is that antibodies created for this pathology might have precipitated an additional immune reaction for specific antigens located in the perivascular regions adjacent to the pons.
Because of a small amount of reported cases, prevalence is unknown, but it has been found to affect predominantly males around age 50 [2]2. A clinical characteristic is its subacute course with most common symptoms related to brainstem, cranial nerve and cerebellar dysfunction, including ataxia, dysarthria, motor weakness and cranial nerve palsy [4].
It has a broad clinical presentation with multiple mimickers, an extensive laboratory and CSF workup is suggested. Nonspecific markers have been found including an elevated antinuclear antibody, ACE, hypercalcemia and elevated IgE [3]. However, while CLIPPERS remains a diagnosis of exclusion, characteristic imaging features on MRI should raise the possibility of this disease process as a differential diagnosis.
Multiple studies have confirmed the MRI characteristics described by Pittock et al. These include bilateral and symmetrical punctate and curvilinear contrast enhanced lesions, without adjacent soft tissue edema or mass effect. The most common location for these lesions include the middle cerebellar peduncles, pons and can extend into the cerebellar hemispheres and spinal cord [4], [10]. Lesions seem to be more apparent on contrast-enhanced studies and less conspicuous on T2 and fluid-attenuated inversion recovery (FLAIR) [3]. A recent proposed diagnostic criterion by Tobin et al. take into account clinical, imaging and neuropathological findings. The proposed MRI criteria include homogenous, enhancing lesions predominantly in the pons and cerebellum that measure < 3 mm with marked improvement once treatment is started, including as well, spinal cord lesions [5].
Diagnosis is difficult as it is based on clinical, radiological, laboratory and CSF sampling, and in some rare cases, biopsies are needed [3]. Treatment consists of high dose corticosteroids [3]. Improvement has been seen within 2 to 4 days after the initiation of treatment [4]. However, some patients with CLIPPERS-like lesions have ultimately been found to have other pathologies including malignancy or vasculitis [11]. Thus, failure of durable response to steroids may necessitate biopsy [4]. It is well-known that a fast withdrawal or taper of corticosteroids can provoke recurrence with a relapse in symptoms and MRI findings, for which immunosuppressive agents have been used to avoid relapses [3].
Conclusion
CLIPPERS is a relatively newly described pathology with characteristic MRI findings. Prompt recognition can assist with diagnosis and initiate treatment with corticosteroids which can help avoid neurological sequelae. Because it is a rare and poorly described pathology, it can be misdiagnosed; therefore, we propose the universal use of the diagnostic criteria described by Tobin et al. to avoid overlooking this treatable condition. Further research is needed to identify causal factors, as well as description of histological findings, and patient demographics.
Footnotes
Consent Statement: All patient identifying information has been stripped from the images, as well as no patient identifying information is used in the case report
Competing Interest: None
References
- 1.Pittock SJ, Debruyne J, Krecke KN, Giannini C, van den Ameele J, De Herdt V. Chronic lymphocytic inflammation with pontine perivascular enhancement responsive to steroids (CLIPPERS) Brain. 2010;133(9):2626–2634. doi: 10.1093/brain/awq164. [DOI] [PubMed] [Google Scholar]
- 2.Taieb G, Allou T, Labauge P. Therapeutic approaches in CLIPPERS. Curr Treat Options Neurol. 2017;19(5):17. doi: 10.1007/s11940-017-0455-4. [DOI] [PubMed] [Google Scholar]
- 3.Dudesek A, Rimmele F, Tesar S, Kolbaske S, Rommer PS, Benecke R. CLIPPERS: chronic lymphocytic inflammation with pontine perivascular enhancement responsive to steroids. Review of an increasingly recognized entity within the spectrum of inflammatory central nervous system disorders. Clin Exp Immunol. 2014;175(3):388–396. doi: 10.1111/cei.12204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bag A, Davenport J, Hackney J, Roy R, Fathallah-Shaykh HM. Case 212: Chronic lymphocytic inflammation with pontine perivascular enhancement responsive to steroids. Radiology. 2014;273:94–947. doi: 10.1148/radiol.14131355. [DOI] [PubMed] [Google Scholar]
- 5.Tobin WO, Guo Y, Krecke KN, Parisi JE, Lucchinetti CF, Pittock SJ. Diagnostic criteria for chronic lymphocytic inflammation with pontine perivascular enhancement responsive to steroids (CLIPPERS) Brain. 2017;140(9):2415–2425. doi: 10.1093/brain/awx200. [DOI] [PubMed] [Google Scholar]
- 6.Wang L, Holthaus EA, Jimenez XF, Tavee J, Li Y. MRI evolution of CLIPPERS syndrome following herpes zoster infection. J Neurol Sci. 2015;348(1–2):277–278. doi: 10.1016/j.jns.2014.11.022. [DOI] [PubMed] [Google Scholar]
- 7.Hillesheim PB, Parker JR, Parker JC, Escott E, Berger JR. Chronic lymphocytic inflammation with pontine perivascular enhancement responsive to steroids following influenza vaccination. Arch Pathol Lab Med. 2012;136(6):681–685. doi: 10.5858/arpa.2011-0428-CR. [DOI] [PubMed] [Google Scholar]
- 8.Tohge R, Nagao M, Yagishita A, Matsubara S. A case of chronic lymphocytic inflammation with pontine perivascular enhancement responsive to steroids (CLIPPERS) in East Asia. Intern Med. 2012;19:1115–1119. doi: 10.5858/arpa.2011-0428-CR. [DOI] [PubMed] [Google Scholar]
- 9.Spagnolo P, Rossi G, Cavazza A, Bonifazi M, Paladini I, Bonella F. Hypersensitivity pneumonitis: a comprehensive review. J Investig Allergol Clin Immunol. 2015;25(4):237–250. [PubMed] [Google Scholar]
- 10.Vola E, Russo C, Macera A, Del Vecchio W, Puoti G, Caranci F. Unusual CLIPPERS presentation and role of MRI examination in the proper diagnostic assessment: a case report. Eur J Radiol Open. 2019;6:212–214. doi: 10.1016/j.ejro.2019.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zalewski NL, Tobin WO. CLIPPERS. Curr Neurol Neurosci Rep. 2017;17(9):65. doi: 10.1007/s11910-017-0773-7. [DOI] [PubMed] [Google Scholar]