Abstract
Process-of-care quality measure research can be used to identify gaps in the delivery of dental services to pregnant patients. The aim of this study was to evaluate the types of dental services that pregnant patients received in four dental clinics over five years as documented in the electronic health record (EHR). To accomplish this objective, the authors modified and validated a previously published claims-based dental quality measure for EHR use. After the electronic dental quality measure specifications were defined, the number of pregnant patients was calculated at three academic dental institutions and one large accountable care organization, and the types of dental care services they received over a five-year period (2013-17) were determined. Calibrated reviewers at each institution independently reviewed a sub-sample of patient charts to validate the information obtained from EHR queries, and the concordance between manual chart reviews and EHR query reports was analyzed. Of the 335,078 women aged 15-44 years who received care at the four clinics for the five reporting years, 3.9% (n=13,026) were pregnant. Among these pregnant patients, 48.9% (n=6,366) received a periodic dental examination; 30.0% (n=3,909) received a comprehensive dental exam; and 21.5% (n=2,799) received additional dental services, irrespective of comprehensive or periodic oral evaluations. Overall, the mean proportion of pregnant patients seeking care in these academic dental and group practice clinics was low, but 78.9% of them received either a periodic or comprehensive oral evaluation. Given the importance of oral health care during pregnancy, these findings suggest a need for curriculum development to incorporate prenatal oral health education in the training of dental students.
Keywords: dental care, dental patients, dentistry, pregnancy, pregnant patients, quality improvement, dental quality measure, dental education
The integration of oral and general health care services is progressing quite slowly,1,2 and the interprofessional model of care delivery that promotes patient-centered care is yet to become mainstream in dentistry.3 This limited integration especially affects pregnant women who have elevated risks of oral diseases, especially gingivitis and periodontitis.4,5 The two most common oral health diseases—caries and periodontal disease—are mostly preventable through good oral hygiene habits, healthy nutrition, and regular dental visits. Despite scientific evidence regarding the safety of receiving dental treatments during pregnancy,6 according to the Pregnancy Risk Assessment Monitoring System, only 49% of pregnant women reported visiting a dentist in the U.S. in 2011,7,8 with similar levels in Australia9,10 and the United Kingdom.11 Because all pregnant women should be visiting the dentist in order to maintain good oral health during pregnancy, the low number of women receiving care indicates a gap in oral health.
The American Dental Education Association (ADEA) Competencies for the New General Dentist emphasize the need for “graduates to be competent to manage the oral health care of … adults, as well as the unique needs of women.”12 Similarly, the Commission on Dental Accreditation (CODA) Standard 2-23 states that “graduates must be competent in providing oral health care within the scope of general dentistry to patients in all stages of life.”13 Despite these training standards, most dentists in one study reported that they did not feel adequately equipped to deliver care to pregnant women.10 Some documented determinants of dental visits during pregnancy are a combination of few physician-initiated referrals to dental care, lack of insurance coverage, limited oral health knowledge, including a lack of understanding of the safety of dental procedures, and hesitancy by dental professionals to treat pregnant patients.6,14 We theorized that the identification of pregnant patients and the types of dental services received would be useful to identify gaps in the delivery of dental services. Furthermore, it will provide helpful information to dentists, faculty, and administrators on measures to improve patient care.
The aim of this study was therefore to evaluate the types of dental services that pregnant patients received in four dental clinics over five years as documented in the electronic health record (EHR). To accomplish this objective, we modified the specifications of “Pregnant Women: Oral Evaluation,” a program level quality measure proposed by the Dental Quality Alliance (DQA),15 developed an electronic measure, and implemented the e-measure at four dental clinics.
Methods
The Institutional Review Boards at all participating dental institutions (The University of Texas School of Dentistry at Houston, University of California, San Francisco School of Dentistry, Harvard School of Dental Medicine, and Skourtes Institute) approved this study. We conducted a retrospective cohort study at three academic dental institutions and one large dental accountable care organization to assess the proportion of pregnant patients who received any dental services and the types of dental services received over a five-year period (2013-17). All four sites use axiUm (Exan Group, Henry Schein, Melville, NY, USA) as their EHR platform.
Using a previously described methodology,16,17 we modified the “Pregnant Women: Oral Evaluation” claims-based measure15 using a three-step process: 1) adapt the claims-based process of care pregnancy dental qualify measure (DQM) developed by the DQA for EHR use; 2) establish the validity of the electronic measure (eMeasure); and 3) implement the eMeasure and assess the proportion of pregnant women who received any dental services and the types of dental services from the Code on Dental Procedures and Nomenclature18 received for the calendar year of 2015 and longitudinally over four years (2013, 2014, 2016, and 2017).
The process was as follows. In step 1, we revised the DQA measure for administrative-claims data. Table 1 shows the numerator and denominator specifications for the modified dental quality eMeasure. Following the age classification from the National Health Statistics,19 we limited the age of pregnant patients to 15-44 years. Since all institutions use the same EHR platform, we developed a Structured Query Language (SQL) script for data extraction and generation of a report in a standard format. At all four institutions, information on pregnancy condition was available as self-reported data in a structured format from the medical history forms. Before we generated the final script, each study site validated the script with a manual review of 20 randomly selected charts to verify that the script extracted accurate information as documented in patients’ charts. In step 2, at each institution, two calibrated reviewers independently reviewed an initial set of 50 randomly selected charts for interrater reliability calculations using Cohen’s kappa (κ).20 Chart reviewers discussed and resolved any discrepancies before a single reviewer completed the manual reviews. We compared the performance of the automated query reports with the manual chart reviews, considered the gold standard. As previously described,16,17 we determined validity using a five-step methodology consisting of automated EHR queries and sample size determination, manual chart reviews, assessment of concordance between automated EHR queries and manual reviews, measure score calculation for the reporting year, and longitudinal measure score calculation. In step 3, we implemented the eMeasures (Primary Measure and Sub-eMeasures) as specified in Table 1 for the reporting year of 2015. After establishing the validity of the Primary eMeasure, we extended the implementation for an additional period of four years (2013, 2014, 2016, and 2017), except for Site 2 where data for 2013 were not available to evaluate longitudinal trends.
Table 1.
Original and modified process of care pregnancy dental quality measures
| Measure | ||
|---|---|---|
| Measure Description | Numerator | Denominator |
| Original DQA measure (claims data) Pregnant women: oral evaluation | Unduplicated number of all enrolled women identified as pregnant who received a comprehensive (D0150) or periodic (D0120) oral evaluation. | a) Unduplicated number of all enrolled women identified as pregnant. b) Unduplicated number of all enrolled women identified as pregnant who received at least one dental service. |
| Revised primary eMeasure Evaluating the number of pregnant women as patients of record |
Women patients aged 15 to 44 years included in the denominator who reported being pregnant in the reporting year of 2015. | All women patients aged 15 to 44 years who had a completed dental procedurea (D0100-D9999) in the reporting year of 2015. |
| Sub eMeasure A Evaluating the proportion of pregnant patients who received an oral evaluation |
Pregnant patients included in the denominator who received a comprehensiveb (D0150) and/or periodic (D0120) oral evaluationb in the reporting year of 2015. | All pregnant patients who had a completed dental procedurea (D0100-D9999) in the reporting year of 2015. |
| Sub eMeasure B Evaluating the proportion of pregnant patients who received any additional dental services irrespective of comprehensive (D0150) or periodic dental evaluations (D0120) |
Pregnant patients who received a dental procedureb categorized into diagnostic (D0100-D0999), preventive (D1000-D1999), restorative (D2000-D2999), endodontics (D3000-D3999), periodontics (D4000-D4999), prosthodontics (D5000-D6999), oral and maxillofacial surgery (D7000-D7999), orthodontics (D8000-D8999), and/or adjunctive general services (D9000-D9999) in the same reporting vear as the denominator. |
Note: Denominator excludes patient charts created for virtual patient exercises, inactive patients, manikins, and examination board.
In process or completed dental procedure codes
Dental procedure codes
Results
In the first step of the process (adaptation of the claims-based process of care pregnancy DQM for EHR use), we identified demographic characteristics of our study population as available in our EHRs (Table 2). A total of 335,078 women aged 15-44 years visited the four clinics for any dental service over the five-year study period. Of these women patients, 3.9% (n=13,026; 95% CI: 3.82,3.95) reported being pregnant (Primary eMeasure). Most pregnant patients were aged 26 to 35 years, white, and non-Hispanic. It is important to note that a large proportion of race/ethnicity data was missing across all study sites.
Table 2.
Demographic characteristics of pregnant patients aged 15-44 years for 2013-17 by site
| Characteristic | Site 1 N (%) |
Site 2 N (%) |
Site 3 N (%) |
Site 4 N (%) |
|---|---|---|---|---|
| Number of women patients aged 15-44 (denominator) | 17,822 | 9,122 | 19,185 | 288,949 |
| Pregnant women (numerator) | 297 (1.7%) | 398 (4.4%) | 291 (1.5%) | 12,040 (4.2%) |
| Age group | ||||
| 15-20 years | 23 (7.7%) | 1 (0.3%) | 27 (9.3%) | 705 (5.9%) |
| 21-25 years | 65 (21.9%) | 11 (2.8%) | 39 (13.4%) | 2,433 (20.2%) |
| 26-30 years | 81 (27.3%) | 46 (11.6%) | 67 (23.0%) | 3,724 (31.0%) |
| 31-35 years | 79 (26.6%) | 173 (43.5%) | 84 (28.9%) | 3,480 (29.0%) |
| 36-40 years | 34 (11.4%) | 132 (33.2%) | 62 (21.3%) | 1,468 (12.2%) |
| 41-45 years | 15 (5.1%) | 35 (8.8%) | 17 (5.8%) | 230 (2.0%) |
| Race | ||||
| White | 60 (20.2%) | 162 (40.7%) | 15 (5.2%) | 5,841 (48.5%) |
| African American | 42 (14.1%) | 14 (3.5%) | 13 (4.5%) | 323 (2.7%) |
| Asian | 13 (4.4%) | 67 (16.8%) | 17 (5.8%) | 388 (3.2%) |
| Native American | 19 (6.4%) | 0 | 0 | 66 (0.5%) |
| Pacific Islander | 0 | 0 | 2 (0.7%) | 64 (0.5%) |
| Other | 40 (13.5%) | 54 (13.6%) | 32 (11.0%) | 894 (7.4%) |
| Unknown | 123 (41.4%) | 100 (25.1%) | 212 (72.9%) | 4,464 (37.1%) |
| Ethnicity | ||||
| Hispanic | 42 (14.1%) | 18 (4.5%) | 30 (10.3%) | 36 (0.3%) |
| Non-Hispanic | 0 | 213 (53.5%) | 25 (8.6%) | 0 |
| Other | 25 (8.4%) | 133 (33.4%) | 0 | 265 (2.2%) |
| Unknown | 190 (64%) | 34 (8.5%) | 236 (81.1%) | 11,739 (97.5%) |
Note: The data for site 2 were available for only 2014-17. “Unknown” in the Race and Ethnicity categories refers to data that were not available.
In the second step (eMeasure query validation), we performed a validity analysis of the Revised Primary eMeasure for the reporting year of 2015 (Table 3). When comparing the manual and query measure scores, we found no differences, indicating that the query performed well and measured as determined in the specifications document (p=0.05, 0.43, 0.72, and 0.49 for sites 1, 2, 3, and 4, respectively). We calculated sensitivity, specificity, and positive and negative predictive values (PPV, NPV) to evaluate the concordance between manual and query scores. These calculations showed at least 90% concordance, except for a PPV of 74.47% due to inconsistencies in dates recorded in the medical history form of 12 patient charts at site 4; hence, the query was not able to correctly extract the information if the patient was or was not pregnant in 2015.
Table 3.
Query and manual reviews measure scores (revised primary eMeasure) for each site for reporting year of 2015
| Site |
Query |
Manual |
p-value (95% CI) |
||||
|---|---|---|---|---|---|---|---|
| Site 1 | Num | 105 | MS: 2.9% (95% CI 2.4, 3.4) | Num | 2 | MS: 0.8% (95% CI 0.09, 2.8) | p=0.05 (−0.033, −0.009) |
| Den | 3649 | Den | 252 | ||||
| Site 2 | Num | 78 | MS: 3.6% (95% CI 2.8, 4.4) | Num | 14 | MS: 4.5% (95% CI 2.5, 7.4) | p=0.43 (−0.015, 0.033) |
| Den | 2150 | Den | 311 | ||||
| Site 3 | Num | 58 | MS: 1.5% (95% CI 1.1, 1.9) | Num | 4 | MS: 1.8% (95% CI 0.05, 4.5) | p=0.72 (−0.015, 0.021) |
| Den | 3749 | Den | 221 | ||||
| Site 4 | Num | 2157 | MS: 3.8% (95% CI 3.6, 4.0) | Num | 16 | MS: 4.5% (95% CI 2.6, 7.2) | p=0.49 (−0.015, 0.03) |
| Den | 56749 | Den | 352 | ||||
| Sensitivity | 97.22% (95% CI 85.4, 99.9) | ||||||
| Specificity | 98.91% (95% CI 98.1, 99.4) | ||||||
| Positive predictive value | 74.47% (95% CI 59.6, 86.1) | ||||||
| Negative predictive value | 99.91% (95% CI 99.5, 99.9) | ||||||
Num=numerator; Den=denominator; MS=measure score; CI=confidence interval
Note: Under Manual reviews, denominator is minimum number of charts for manual review at each institution for reporting year (2015): 252, 311, 221, and 352 charts at sites 1-4, respectively. Sample size was determined using proportions (p) −0.029, 0.045, 0.015, and 0.040 for sites 1, 2, 3, and 4. Margins of error and significance levels at each site were set at a standard 0.02 (d=0.02, α=0.05). The p-values are relationship between manual and automated queries calculated with two-sample test of proportions.
In the third step (implementation of eMeasure and assessment of measure scores), we found that, for the five reporting years and four sites, the total proportion of pregnant patients was 3.9%. Of these, the percentage of patients who received either a periodic (D0120) or comprehensive oral evaluation (D0150) was 48.9% (95% CI: 48.1, 49.7) and 30% (95% CI, 29.2, 30.8), respectively (Table 4). Overall, across all four sites, the number of pregnant patients receiving a periodic (D0120) or comprehensive oral evaluation (D0150) was 78.9% (95% CI: 77.8, 79.2).
Table 4.
Percentage of pregnant patients aged 15-44 years at each site who received comprehensive (D0150) or periodic (D0120) oral evaluations for 2013-17 (sub-eMeasure A)
| Site | D0120 |
Percentage (95% CI) |
D0150 |
Percentage (95% CI) |
Pregnant Patients Who Received D0120 or D0150 |
Percentage (95% CI) |
|||
|---|---|---|---|---|---|---|---|---|---|
| Site 1 | Num | 60 | 20.2% | Num | 125 | 42.1% | Num | 192 | 64.6% |
| Den | 297 | (15.78, 25.22) | Den | 297 | (36.4, 47.92) | Den | 297 | (58.9, 70.0) | |
| Site 2 | Num | 176 | 44.2% | Num | 39 | 9.8% | Num | 211 | 53.0% |
| Den | 398 | (39.27, 49.25) | Den | 398 | (7.06, 13.15) | Den | 398 | (47.97, 58.0) | |
| Site 3 | Num | 67 | 23.0% | Num | 160 | 55.0% | Num | 220 | 75.6% |
| Den | 291 | (18.31, 28.29) | Den | 291 | (49.06, 60.79) | Den | 291 | (70.24, 80.42) | |
| Site 4 | Num | 6,063 | 50.4% | Num | 3,585 | 29.8% | Num | 9,604 | 79.8% |
| Den | 12,040 | (49.45, 51.25) | Den | 12,040 | (28.95, 30.60) | Den | 12,040 | (79.0, 80.48) | |
| Total | Num | 6,366 | 48.9% | Num | 3,909 | 30.0% | Num | 10,227 | 78.9% |
| Den | 13,026 | (48.1, 49.73) | Den | 13,026 | (29.22, 30.80) | Den | 13,026 | (77.79, 79.21) | |
D0120=periodic oral evaluation, established patient; D0150=comprehensive oral evaluation, new or established patient; Num=numerator (number of pregnant patients who received D0120 and/or D0150 procedures); Den=denominator (total number of pregnant patients included in denominator)
Note: The data for site 2 were available for only 2014-17.
We also evaluated the types of dental procedures pregnant patients received irrespective of periodic and comprehensive oral evaluations (Sub-eMeasure B). Overall, 21.5% (n=2,799) of pregnant patients received any other dental services. Figure 1 shows the types of dental procedures received by pregnant patients over the five-year study period. The most frequently received procedures by pregnant patients were for diagnostic services (e.g., examinations) (42.7% to 87.7%) and preventive services (e.g., oral prophylaxis) (65% to 87%). The pregnant patients also received restorative (e.g., composite restorations) and adjunctive general services (including palliative treatment for dental pain). Periodontal and oral surgical procedures were the least received dental services by pregnant patients, and less than 1% received orthodontic treatment.
Figure 1. Percentage of dental procedures received by pregnant patients over five reporting years (2013-17) by site (sub-eMeasure B).
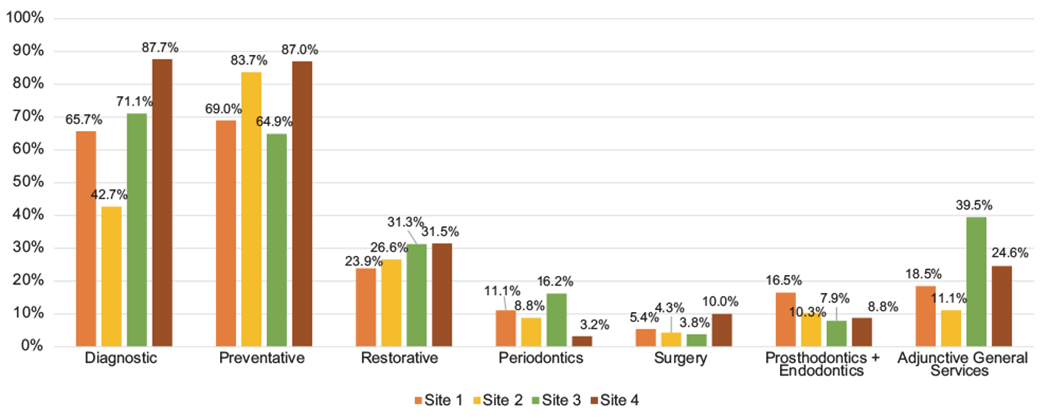
Note: The data for site 2 were available for only 2014-17. A total of 2,799 pregnant patients received dental procedures irrespective of periodic or comprehensive oral evaluations.
Discussion
In this study, we evaluated the number of pregnant women who visited four dental clinics over a five-year study period and the type of dental services they received using a modified Dental Quality eMeasure. Nationally, the pregnancy rate for women aged 15-44 years is 102.1 per 1,000 (10.2%).21 Our study mirrors the small number of pregnant women seeking dental care found in a survey of 31 U.S. dental schools published in 2013.22 In that study, Curtis et al. discussed the need for health professionals to recognize the importance of prenatal oral health programs; however, they also found that less than 50% of dental students in the study were exposed to evidence-based guidelines on the treatment of pregnant women. With 6.2 million pregnancies in the U.S. in 2010, the limited use of dental services by pregnant women is a public health problem because of the increased risk for periodontal conditions during pregnancy23 and the potential transmission of cariogenic bacteria present in the mother’s mouth to the newborn via sharing utensils.24 The inadequate prenatal oral health training received in dental school does little to address the oral health disparities of this vulnerable population.22
Across all four sites, the majority of pregnant women who came in for a dental visit underwent mainly preventive procedures, primarily oral prophylaxis. It is unlikely that this population did not have additional dental care needs, given that, of all patients who visited the dental office in one study, an estimated 25% had unmet dental needs.25 It is possible that these women decided to postpone additional dental care needs because of their pregnant state, that their providers suggested postponing dental care beyond basic prophylaxis, and/or that their providers did not discuss additional care options with these patients. However, it is beyond the scope of this process-of-care quality measure to evaluate if dental procedures beyond oral prophylaxis and examinations (D120, D150, D180) were avoided because of pregnancy.
Due to the paucity of specific dental educational standards and competencies for treating pregnant women,5,12 the uptake of formal academic maternal and child health programs in dental education has been found to be slow.26 Maternal and child health government-led initiatives, including Women and Child Infant Health Programs, exist in every state,27,28 but we have observed that only in recent years have academic institutions begun to embrace interprofessional maternal health programs that train both dental and medical students simultaneously. Jackson et al. described implementation of a pioneer maternal oral health program at the University of North Carolina at Chapel Hill School of Medicine and School of Dentistry, with the objective of providing training to medical and dental students on prenatal oral health.26 For such programs to be implemented, critical factors in academic institutions needed to be in place including leadership support and buy-in, seamless communication and referral pathways between medical residents and dental clinics, and delivering pertinent insurance information, e.g., Medicaid coverage and eligibility, to women patients. The latter is particularly relevant as Medicaid covers nearly 45% of all births in the U.S.29 Unfortunately, Medicaid does not require states to offer comprehensive dental coverage to adult pregnant women,30 which has led to a wide variation in dental services covered from state to state, ranging from emergency services only to oral exams and preventive services to comprehensive care.31 Healthy People 2020 has a generic objective to “increase the proportion of children, adolescents, and adults who used the oral health care system in the previous year.”32 Augmenting the level of dental service utilization among pregnant women should be part of this overall objective through integrated prenatal policies that promote oral and general health, especially among populations that are underserved with limited access dental services.28,33
Patient-centered care, interprofessional practice, and integration of oral and general health will all be better served with medical and dental electronic health records that are seamlessly connected with each other. Dental and medical EHR connectivity would facilitate the implementation of evidence- based patient-centered care and enable the development of additional meaningful dental and medical quality measures to evaluate a range of quality measures, including prenatal oral and general health care.34 Dental institutions, specifically academic dental institutions, are uniquely positioned to implement innovative strategies, including updates and adaptation of clinical practice and educational curricula, to provide dental and dental hygiene students the necessary training required for dental professionals to deliver high-quality care to pregnant patients.
Our study had some limitations. The study focused on a process-of-care DQM that by definition has as its primary objective to provide information that can help identify gaps and guide quality improvement decisions.35 It was beyond its scope to evaluate if specific determinants of dental visits, including insurance type and Medicaid coverage, contributed to the low number of pregnant women among our patient population. As our study was conducted in three academic dental clinics and a large accountable care organization, the generalizability of our results to different types of dental clinics including private clinics and hospital-based practices is limited. Patients’ self-reported pregnancy status may be another limitation because we were not able to verily pregnancy status with information from the patients’ medical records. Therefore, there may have been an underreporting of pregnancy status, especially for patients who did not know they were pregnant at the time of the dental appointment, and that would result in a smaller denominator. Finally, race and ethnicity information was missing for nearly half of our patients. Despite all these deficiencies, patient documentation in EHRs is the most accurate and complete source of information available for dental providers to help manage care and provide data for quality and clinical research.
Conclusion
This study demonstrated the feasibility of using patient-level, electronic health record data to implement a revised process-of-care dental quality measure to assess the type of dental care services pregnant women received across three academic institutions and one large accountable dental care organization over five years. Overall, our findings indicated that very few dental patients sought dental care during pregnancy in either the educational institutions or private clinic. There is a need for action to improve access to dental care for pregnant patients, to promote curriculum redesign, and to incorporate prenatal oral health programs in the clinical training of dental and dental hygiene students. In the future, implementation of interprofessional models between dentistry and primary care can help advance oral and general health care for our pregnant patients.
Acknowledgments
Research reported in this article was supported in part by award R01DE024166 from the National Institute of Dental and Craniofacial Research, National Institutes of Health. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Disclosure
The authors reported no conflicts of interest.
Contributor Information
Ana Neumann, The University of Texas School of Dentistry at Houston.
Enihomo Obadan-Udoh, School of Dentistry, University of California, San Francisco.
Suhasini Bangar, The University of Texas School of Dentistry at Houston.
Shwetha V. Kumar, The University of Texas School of Dentistry at Houston.
Oluwabunmi Tokede, Harvard School of Dental Medicine.
Aram Kim, Harvard School of Dental Medicine.
Alfa Yansane, School of Dentistry, University of California, San Francisco.
Elizabeth Mertz, School of Dentistry, University of California, San Francisco.
Sapna Panwar, School of Dentistry, University of California, San Francisco.
Arti Gharpure, School of Dentistry, University of California, San Francisco.
Krisha Kumar Kookal, The University of Texas School of Dentistry at Houston.
Joanna Mullins, Skourtes Institute, Hillsboro, OR.
Joshua B. Even, Skourtes Institute, Hillsboro, OR.
Kristen Simmons, Skourtes Institute, Hillsboro, OR.
Joel M. White, School of Dentistry, University of California, San Francisco.
Muhammad F. Walji, The University of Texas School of Dentistry at Houston.
Elsbeth Kalenderian, Department Chair, School of Dentistry, University of California, San Francisco.
REFERENCES
- 1.Lamster IB, Myers-Wright N. Oral health care in the future: expansion of the scope of dental practice to improve health. J Dent Educ 2017;81(9 Suppl):eS83–90. [DOI] [PubMed] [Google Scholar]
- 2.Oral health in America: a report of the surgeon general. Rockville, MD: U.S. Public Health Service, Department of Health and Human Services, National Institute of Dental and Craniofacial Research, 2000. [Google Scholar]
- 3.Marchi KS, Fisher-Owens SA, Weintraub JA, et al. Most pregnant women in California do not receive dental care: findings from a population-based study. Public Health Rep 2010;125(6):831–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Brailer C, Robison V, Barone L. Protect tiny teeth toolkit: an oral health communications resource for providers of pregnant women and new mothers. J Womens Health (Larchmt) 2019;28(5):568–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Oral Health Care During Pregnancy Expert Workgroup. Oral health care during pregnancy: a national consensus statement. Washington, DC: National Maternal and Child Oral Health Resource Center, 2012. [Google Scholar]
- 6.Michalowicz BS, DiAngelis AJ, Novak MJ, et al. Examining the safety of dental treatment in pregnant women. J Am Dent Assoc 2008; 139(6): 685–95. [DOI] [PubMed] [Google Scholar]
- 7.Shulman HB, D’Angelo DV, Harrison L, et al. The pregnancy risk assessment monitoring system (PRAMS): overview of design and methodology. Am J Public Health 2018; 108(10):1305–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Centers for Disease Control and Prevention. Pregnancy risk assessment monitoring system. Atlanta: Centers for Disease Control and Prevention, 2018. [Google Scholar]
- 9.George A, Ajwani S, Bhole S, et al. Knowledge, attitudes, and practices of dentists towards oral health care during pregnancy: a cross sectional survey in New South Wales, Australia. Aust Dent J 2017;62(3):301–10. [DOI] [PubMed] [Google Scholar]
- 10.Riggs E, Yelland J, Shankumar R,Kilpatrick N. “We are all scared for the baby”: promoting access to dental services for refugee background women during pregnancy. BMC Pregnancy Childbirth 2016; 16:12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hullah E, Turok Y, Nauta M, Yoong W. Self-reported oral hygiene habits, dental attendance, and attitudes to dentistry during pregnancy in a sample of immigrant women in North London. Arch Gynecol Obstet 2008;277(5):405–9. [DOI] [PubMed] [Google Scholar]
- 12.American Dental Education Association. ADEA competencies for the new general dentist. J Dent Educ 2017;81(7):844–7. [DOI] [PubMed] [Google Scholar]
- 13.Commission on Dental Accreditation. Accreditation standards for dental education programs. Chicago: American Dental Association, 2018. [Google Scholar]
- 14.Rocha JS, Arima LY, Werneck RI, et al. Determinants of dental care attendance during pregnancy: a systematic review. Caries Res 2018;52(1-2): 139–52. [DOI] [PubMed] [Google Scholar]
- 15.Dental Quality Alliance. Adult measures under consideration. 2013. At: www.ada.org/en/science-research/dental-quality-alliance/dqa-measure-activities. Accessed 22 Apr. 2019.
- 16.Bhardwaj A, Ramoni R, Kalenderian E, et al. Measuring up: implementing a dental quality measure in the electronic health record context. J Am Dent Assoc 2016; 147(1):35–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Neumann A, Kalenderian E, Ramoni R, et al. Evaluating quality of dental care among patients with diabetes: adaptation and testing of a dental quality measure in electronic health records. J Am Dent Assoc 2017; 148(9):634–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.CDT 2018: dental procedure codes. 8th ed. Chicago: American Dental Association, 2017. [Google Scholar]
- 19.Martin JA, Hamilton BE, Osterman MJK. Births in the United States, 2017. NCHS Data Brief 2018;318:1–8. [PubMed] [Google Scholar]
- 20.Cohen J. A coefficient of agreement for nominal scales. Educ Psychol Meas 1960;20(1): 37–46. [Google Scholar]
- 21.Curtin SC, Abma JC, Ventura SJ, Henshaw SK. Pregnancy rates for U.S. women continue to drop. NCHS Data Brief 2013;136:1–8. [PubMed] [Google Scholar]
- 22.Curtis M, Silk HJ, Savageau JA. Prenatal oral health education in U.S. dental schools and obstetrics and gynecology residencies. J Dent Educ 2013;77(11): 1461–8. [PubMed] [Google Scholar]
- 23.Iheozor-Ejiofor Z, Middleton P, Esposito M, Glenny AM. Treating periodontal disease for preventing adverse birth outcomes in pregnant women. Cochrane Database Syst Rev 2017;6:CD005297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.American College of Obstetricians, Gynecologists, Women’s Health Care Physicians Committee on Health Care for Underserved Women. Committee opinion no. 569: oral health care during pregnancy and through the lifespan. Obstet Gynecol 2013;122(2 Pt 1):417–22. [DOI] [PubMed] [Google Scholar]
- 25.Singhal A, Chattopadhyay A, Garcia AI, et al. Disparities in unmet dental need and dental care received by pregnant women in Maryland. Matern Child Health J 2014;18(7): 1658–66. [DOI] [PubMed] [Google Scholar]
- 26.Jackson JT, Quinonez RB, Kerns AK, et al. Implementing a prenatal oral health program through interprofessional collaboration. J Dent Educ 2015;79(3):241–8. [PubMed] [Google Scholar]
- 27.City of Houston Health Department. Houston Health Department women, infants, and children program. 2019. At: www.houstontx.gov/health/WIC/index.html. Accessed 22 Apr. 2019.
- 28.Milgrom P, Ludwig S, Shirtcliff RM, et al. Providing a dental home for pregnant women: a community program to address dental care access—a brief communication. J Public Health Dent 2008;68(3): 170–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Markus AR, Andres E, West KD, et al. Medicaid covered births, 2008 through 2010, in the context of the implementation of health reform. Womens Health Iss 2013;23(5):e273–80. [DOI] [PubMed] [Google Scholar]
- 30.Center for Health Care Strategies. Fact sheet: Medicaid adult dental benefits—an overview. Hamilton, NJ: Center for Health Care Strategies, 2018. [Google Scholar]
- 31.Centers for Medicare & Medicaid Services. Dental benefits for adults in Medicaid. 2018. At: www.medicaid.gov/medicaid/benefits/dental/index.html. Accessed 22 Apr. 2019.
- 32.Healthy People 2020. Oral health objectives. 2018. At: www.healthypeople.gov/2020/topics-objectives/topic/oral-health/objectives. Accessed 19 Apr. 2019.
- 33.Azofeifa A, Yeung LF, Alverson CJ, Beltran-Aguilar E. Oral health conditions and dental visits among pregnant and nonpregnant women of childbearing age in the United States, National Health and Nutrition Examination Survey, 1999-2004. Prev Chronic Dis 2014; 11 :E163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Acharya A, Mahnke A, Chyou PH, et al. Medical providers’ dental information needs: a baseline survey. Stud Health Technol Inform 2011; 169:387–91. [PMC free article] [PubMed] [Google Scholar]
- 35.Kalenderian E, Ramoni R, Spallek H, et al. Quality measures everywhere: the case for parsimony. J Am Dent Assoc 2018; 149(4):322–6. [DOI] [PMC free article] [PubMed] [Google Scholar]


