Abstract
Mass disasters result in extensive health problems and make health care delivery problematic, as has been the case during the COVID-19 pandemic. Although COVID-19 was initially considered a pulmonary problem, it soon became clear that various other organs were involved. Thus, many care providers, including kidney health personnel, were overwhelmed or developed burnout. This review aims to describe the spectrum of burnout in mass disasters and suggests solutions specifically for nephrology personnel by extending previous experience to the COVID-19 pandemic. Burnout (a psychologic response to work-related stress) is already a frequent part of routine nephrology practice and, not surprisingly, is even more common during mass disasters due to increased workload and specific conditions, in addition to individual factors. Avoiding burnout is essential to prevent psychologic and somatic health problems in personnel as well as malpractice, understaffing, and inadequate health care delivery, all of which increase the health care burden of disasters. Burnout may be prevented by predisaster organizational measures, which include developing an overarching plan and optimizing health care infrastructure, and ad hoc disaster-specific measures that encompass both organizational and individual measures. Organizational measures include increasing safety, decreasing workload and fear of malpractice, optimizing medical staffing and material supplies, motivating personnel, providing mental health support, and enabling flexibility in working circumstances. Individual measures include training on coping with stress and problematic conditions, minimizing the stigma of emotional distress, and maintaining physical health. If these measures fall short, asking for external help is mandatory to avoid an inefficient disaster health care response. Minimizing burnout by applying these measures will improve health care provision, thus saving as many lives as possible.
Keywords: burnout, massive disaster, earthquake, hurricane, COVID-19, pandemic, nephrology
Mass Disasters and the COVID-19 Pandemic
Disasters result in a “serious disruption of the functioning of a society causing widespread human, material, economic or environmental losses” (1); in the case of mass disasters, the number of victims overwhelms the local system. Disasters are classified as either natural (e.g., epidemics, earthquakes, storms, floods) or man-made (e.g., wars, terrorist attacks) (2). During mass disasters, the health care workload increases, while the number of operational health care personnel decreases. The same concerns are also applicable to nephrology (3). In fact, nephrology personnel are prone to burnout and depressive symptoms even in routine practice (4). Therefore, there is a need to describe the spectrum of burnout in mass disasters and suggest solutions on the basis of previous experience to have an efficient health care response to help as many people as possible.
The COVID-19 biologic disaster is a typical example of a “disaster without borders.” As of November 6, 2020, SARS-CoV-2 had infected 48,534,508 people and killed 1,231,017 around the globe (5), and resulted in extreme health-related, social, and economic problems, all of which contribute to burnout. Because COVID-19 is a disaster with significant effect on nephrology, a team of clinicians, all coming from highly affected COVID-19 areas, such as North Italy, Madrid, Flanders, and Istanbul, wrote this review, extending previous experience from earthquakes to the COVID-19 crisis.
The Concept of Burnout
Burnout is a psychologic syndrome characterized by a “prolonged response to chronic interpersonal stressors on the job” or “psychological response to work-related stress” (6). Burnout prevalence is up to 78% in health workers (7,8) and affects almost all specialties (8), with risks of irreversible harm toward self, patients, institutions, and even society (8,9).
There are three major features of burnout: (1) exhaustion, (2) feelings of cynicism, and (3) professional inefficacy (6). These are associated with psychologic and psychiatric problems (e.g., anxiety, increased depression, and suicidal tendency); somatic signs (e.g., gastrointestinal and cardiovascular complaints); social problems (e.g., loss of empathy, social isolation, and marital conflicts) (10); and health problems, which again contribute to the burnout (6). Burnout may also affect team spirit, creating disorganization. Importantly, treatment by burned-out professionals generates patient dissatisfaction, unfavorable outcomes, medical errors, and malpractice (9 –11), and malpractice also causes burnout (12).
Situational conditions such as heavy workloads, excessive bureaucracy and computerization, long working hours, and chronic staff shortages (6,8) and individual factors such as younger age, female sex, problematic family situations, and job dissatisfaction are associated with burnout and subsequent depression (9,10,13), and burnout and depression often intensify each other (10,14).
Health Problems after Mass Disasters
Health care provision is problematic due to patient overflow and logistic difficulties, including damage to health care facilities, mental problems due to uncertainty about the future, and shortages of materials and personnel, amplifying ineffective health care risks (Figure 1). Because these factors predispose people to burnout (15), a vicious circle may ensue. Early in the COVID-19 pandemic, the shortage of tests, inadequate detection, lack of personal protective equipment (PPE), inaccurate and improvised management, and insufficient capacity resulted in suboptimal health care. Of note, attention often focused on hospitals and intensive care units (16), and immense problems in nursing homes went unnoticed (17).
Figure 1.
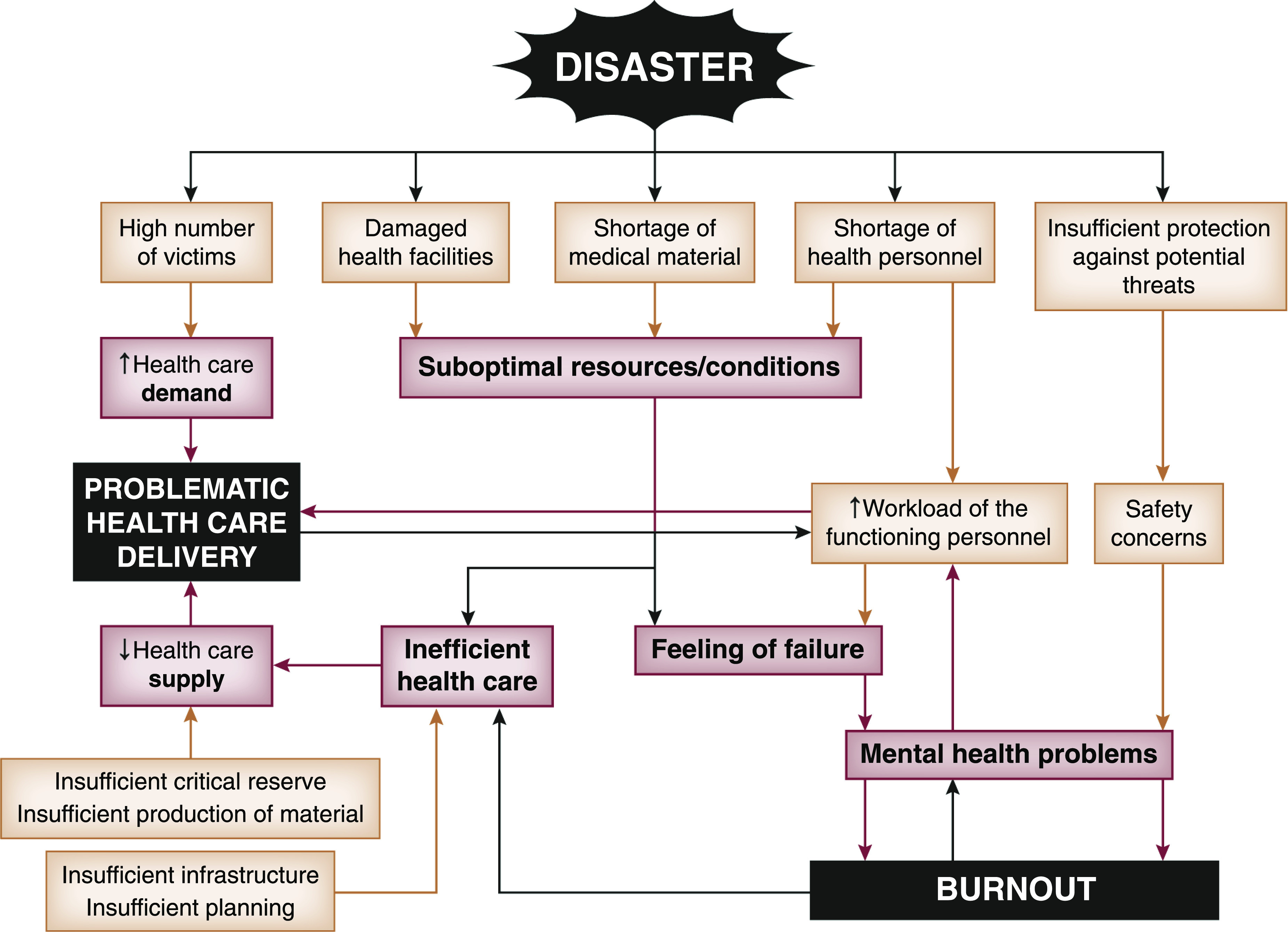
Role of burnout in health care provision after mass disasters. Overall, there is an increased demand for health care, while there is a decreased supply. Various factors play an important role in ineffective health care provision, which differ depending on the type of disaster (e.g., damaged health care facilities are very frequent after earthquakes, tsunamis, hurricanes, and wars, whereas a shortage of medical material is common after pandemics, and insufficient planning is an almost consistent part of all mass disasters). These factors and safety concerns form the basis of burnout, which further negatively affects health care services, and differ depending on the disaster (e.g., shotgun wounds or bombing injuries during wars, being crushed under collapsed buildings during earthquakes, or being infected during pandemics).
Kidney problems during disasters are associated with multiple comorbidities, and treatment heavily depends on operational or functioning infrastructure. So far, crush-related AKI after earthquakes and maintenance dialysis delivery problems after hurricanes are most frequently reported (18 –21). Although COVID-19 initially seemed a pulmonary problem, soon cardiovascular, central nervous, and kidney problems (AKI, high susceptibility in patients with CKD who have had transplants, dialysis delivery problems, and outbreaks in hemodialysis centers) became apparent (22 –35). Indeed, CKD has emerged as the most common comorbid risk factor for severe COVID-19 (36,37).
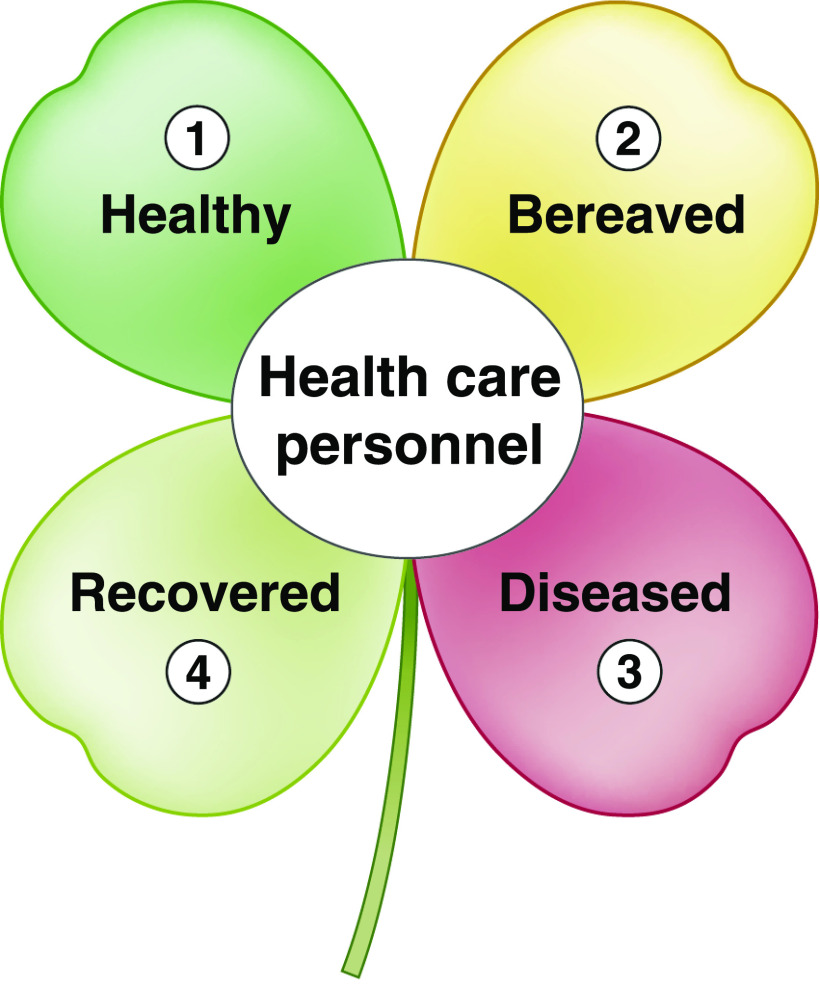
During a pandemic, health care personnel may be juggling several roles sequentially or simultaneously (Figure 2), making them subject to additional risks. Personal experience by the authors and extrapolation from other specialties indicate that burnout risk among nephrology personnel is high during disasters. This has also occurred with COVID-19 due to the overlapping effect of threats to self-safety, increased workload, PPE requirements, medical supply shortages, sudden changes in work schedules, concerns about health and safety of family members, and continuing everyday family responsibilities irrespective of the high workload (16,38,39).
Figure 2.
Variations in mental and physical health status of health care personnel during mass pandemic disasters. Very different, sometimes sequential or even simultaneous conditions may occur and occasionally oblige the personnel to continue working, at the expense of neglecting their own health. Risky working practice may be due to underdiagnoses due to lack of diagnostic or protective resources or simply because of dedication. (1) In ideal conditions, healthy personnel provide health care. (2) Affected family members or colleagues may result in a bereaved health care worker, decreasing efficacy. (3) They may continue to work willingly or unwillingly, even if they are diseased (or affected) by the disaster. (4) The personnel may recover; however, sometimes they may go back to work without adequate rehabilitation. Of note, for nonpandemic disasters such a earthquakes, hurricanes, etc., a similar condition may occur where the terms “healthy” and “diseased” may be replaced by “unaffected” and “affected.”
This review describes several features of burnout in disaster circumstances and suggests measures for prevention, which is far more effective in preventing long-term consequences than post-hoc treatment.
Burnout after Mass Disasters
Mass disasters are characterized by extreme numbers of victims; there were 225,000, 173,000, and 500,000 casualties after the Indian Ocean tsunami (40), Pakistan-Kashmir (41), and Haiti earthquakes (42), respectively. In these cases, health care supplies became deficient because of health facility destruction and shortages of medical materials and personnel (3,43), all of which can predispose people to burnout (Figure 1, Table 1). During the COVID-19 pandemic, there has been no structural damage, but health care personnel have had similar problems of burnout and depression. Main causes were fear of, or actual, personal health problems, worry about the future, deficiency in providing appropriate health services due to extreme patient numbers, shortage of diagnostic tools, shortage of materials, and dropout of personnel because of infection or psychologic problems (44).
Table 1.
Problems in providing health care after mass disasters, which may predispose health care personnel to burnout
| Workload | Infrastructural | Emotional | Organizational |
|---|---|---|---|
| High number of victims | Damaged health facilities | Worries about self-safety | Chaos and panic |
| Shortage of personnel | Shortage of medical material | Worries about relatives’ health | Inadequate preparedness |
| Overwhelming workload | Problems in transportation | Loss of relatives | Working in suboptimal conditions |
| Unfavorable outcome of victims | Problems in communication | Loss of property | Inexperience |
| Loss of self-esteem | Lack of instructions | ||
| Feelings of incapability |
Nephrology Personnel at Risk of Burnout during Disasters
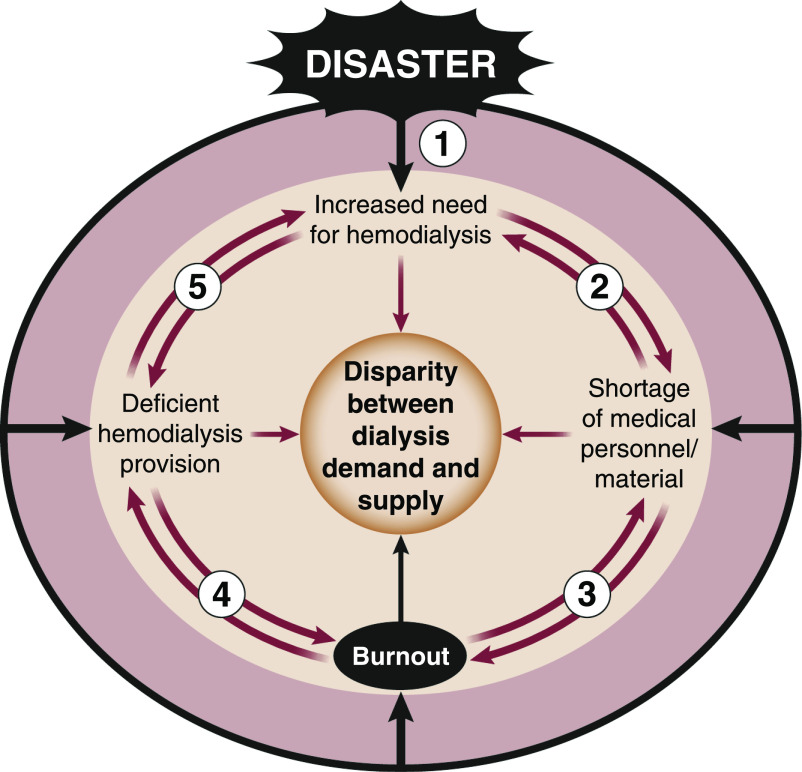
After disasters, nephrology personnel are faced with large numbers of victims. After earthquakes, 2%–3% of all injured people suffer from crush syndrome, a potentially fatal condition if not treated properly (45,46). After COVID-19, AKI occurred in more than 30% of hospitalized patients, among whom 25%–30% needed dialysis support (24,47). Increased demand with a necessity to continue routine care and shortage of dialysis material may cause additional stress (Figure 3) (28,32,48,49). Nephrology personnel exerting various functions during disasters are prone to burnout, through mechanisms that differ by disaster.
Figure 3.
Complex interaction between disasters and hemodialysis delivery. (1) Dialysis demand increases after disasters because of new AKI cases. (2) Due to various reasons, there is a shortage of dialysis supply. Thus, number of dialysis sessions decreases, and even daily routine demand may not be met, which in turn exaggerates the increased need for hemodialysis. (3) Health care personnel’s burnout contributes to shortage of personnel, and this factor is a trigger for increasing risk of burnout. (4) Burned-out personnel may not work efficiently, causing deficient dialysis provision. (5) Deficient service supply contributes to increased need for hemodialysis, while dialysis shortage increases the extent of deficiency. Disaster circumstances are the main driving force for each of these components.
Disaster Relief Coordinators
Generating action plans before disasters and managing interventions in disaster conditions is associated with an overwhelming feeling of responsibility and sometimes inability. Assigning appropriate personnel to appropriate positions, providing medical devices, and assuring security of personnel at any moment in suboptimal conditions predisposes the nephrology leadership to burnout (50–53).
Nephrologists on the Front Line
Nephrologists are prone to burnout under everyday conditions in the case of demanding and depressing working conditions. In a survey of 347 US nephrology fellows undertaken before the COVID-19 breakout, about one third reported experiencing burnout and depressive symptoms (4). Female physicians and those experiencing poor work-life balance or a disruptive work environment were at especially high risk. The risk is highest in front-line doctors due to austere conditions (54), and is even more prominent during pandemics because of the threat of contracting the disease (16) and having to make triage decisions, such as allocating care unequally due to supply or capacity shortages.
Nurses and Nursing Assistants
Hemodialysis nurses have a high risk of burnout, even in day-to-day practice (55,56). This risk is increased by heavy and stressful work after mass disasters, such as working in close contact with patients who are infected during pandemics, connecting and disconnecting them from equipment (57), or performing acts demanding high levels of concentration, such as parenteral treatment. As hemodialysis nurses are dealing with intradialytic complications in different patients, frequent changing of PPE can be emotionally and physically taxing. Shortage of PPE generates extra burden.
Because many kidney health care personnel lose efficacy due to the high risk of physical or psychologic dysfunction, those remaining active may have to take over their commitments, which increases workload and contributes to novel cases of burnout (3). The problem is compounded by the need to provide support to patients who were non-nephrological and had COVID-19. At some points during the pandemic, 90% of inpatients in large hospitals from severely affected areas were patients with COVID-19, and 70%–80% of nephrologists were reassigned to general COVID-19 care (58).
Nevertheless, apart from scarce media coverage (48), little attention has been paid to this problem in kidney health personnel, although this matter has been stressed for many other specialties, such as intensive care (16), oncology (59), allergy/immunology (38), and radiology (39).
Prevention of Burnout after Disasters
Nephrologists, like all medical personnel, can mitigate health problems due to disasters if they are well prepared. For example, studies on patients undergoing maintenance hemodialysis after the landfall of Hurricane Sandy in 2012 revealed that several factors contributed to fewer missed sessions and hospitalizations and lower mortality: early dialysis before the event, strong cultural or social support, dialysis-specific preparedness, evacuation to other dialysis centers, and communication and information sharing among dialysis facilities (60,61).
Prevention or treatment of burnout is mandatory, not only for a person’s own health, but also to keep manpower effective and prevent malpractice. Mental health care plans such as those developed by Médecins Sans Frontières (MSF; Doctors Without Borders) are essential in crisis situations (62).
Frequent causes, preventive strategies, and management of existing burnout have been the topic of a number of general reviews (6,8,63,64). However, what is described in these publications may not always apply to disasters, and thus, we describe an array of measures to minimize the extent of burnout that are specifically adapted to predisaster and ad hoc disaster circumstances.
Predisaster Organizational Measures
Developing an Overarching Plan.
Most health personnel desire to start working immediately after mass disasters, driven by dedication and selflessness. However, this instantaneous full engagement of many carries a risk that they will also experience burnout almost simultaneously, generating a shortage of personnel at a later stage. Therefore, efficient predisaster personnel planning and postdisaster assignment of personnel is a must to control workloads (3,52,65). For pragmatic reasons, instantaneous involvement driven by heroism and altruism of enthusiastic or excited personnel should be discouraged to reserve effective manpower for the later stages of disaster response. Also, rotating workers from higher-stress to lower-stress functions and vice versa may be helpful to prevent burnout, which was also recommended by World Health Organization during the COVID-19 pandemic (53). However, to avoid transmission of infections by health care personnel, rotations should be organized separately in COVID-positive and COVID-free zones. Nonstop activity of personnel to compensate for missing or inefficient colleagues should be avoided as much as possible. A supervisor should be assigned to evaluate personnel for exhaustion and decide when they should take a break, prepare all staff for a sustained effort, and establish a suitable relay and backup schedule.
Optimizing Health Care Infrastructure.
Medical problems are complex in the vast majority of disaster victims, which necessitate functioning and well-developed general and specialized health care infrastructure, for example, surgical theaters, dialysis units, intensive care units, imaging facilities, microbiology, and, especially in epidemics, molecular diagnostic laboratories (52). A deficient professional environment is associated with poor performance and reduced satisfaction, which trigger burnout (16,63). Although measures can be taken by health policy makers for predictable disasters, they may be impossible for unpredictable calamities (16), stressing the importance of maintaining sufficient infrastructure with enough critical reserve in less problematic periods.
Nephrology units in and around disaster-prone areas, or those faced with disaster threat, should develop their own disaster scenarios to cope with sudden influxes of patients (3). This preparation may decrease stress for the disaster relief coordinators and is one of the options allowing a more efficient assignment of nephrology personnel.
The exact need for medical consumables to treat patients should be defined well in advance to allow adequate stockpiling of supplies and PPE, and for organizing acute help from outside the damaged area (3).
Ad Hoc Disaster-Specific Measures.
Organizational Measures
Decreasing the Workload of Health Care Personnel
This can only be made possible by increasing efficiently functioning personnel, for example, moving personnel from less-involved departments, facilities, or geographic areas to the more severely affected ones (3,53). Telemedicine may also decrease the workload of front-line health care personnel (66,67). Specific to dialysis, switching from thrice-weekly to twice-weekly dialysis for patients on maintenance may be useful to decrease workload when resource constraints prevail (3), as twice-weekly dialysis has been suggested to offer noninferior survival rates compared with thrice-weekly therapy and may be beneficial (68). Specific to COVID-19, twice-weekly hemodialysis results in less exposure to infected patients, while also reducing dialysis staff work and the need for transportation and PPE (69). However, underdialysis, especially hyperkalemia, should be avoided (70).
Decreasing Concerns about Safety
To allow efficient work, health care personnel should be able to work in secure conditions (52). The measures to be taken obviously differ among disasters. Thus, working in earthquake-resistant buildings, staying away from the battlefield, and working some distance from coastal areas are needed after earthquakes, wars, and tsunamis, respectively. Considering epidemics and pandemics, PPE (masks, gowns, gloves, protective clothing) should be stockpiled in advance. Shortage of such material has been a major drawback during the COVID-19 pandemic, although it could have been avoided (52).
Maintaining Stock of Medical Consumables and Medications
Consumables used in high quantities during disasters should be delivered regularly for uninterrupted health care. Extensive problems in obtaining laboratory chemicals, test kits, antivirals, antibiotics, immunomodulating medications, dialysis machines, and consumables have been major drawbacks for provision of an effective health care during the COVID-19 pandemic, especially in the early period (16,48).
Reducing Fear of Malpractice
In disaster circumstances, physicians may be allotted to unfamiliar tasks, for example, gynecologists, orthopedists, or ophthalmologists become emergency room physicians, increasing stress and burnout risk. The most effective way for preventing errors and reducing pressure is preparing clear and pragmatic guidelines and recommendations for management of medical and logistic problems, on the basis of experience (3,43,52), and developing online platforms with medical advice by relevant and respected experts. The legal framework may be adapted to avoid unjustified malpractice claims (43).
Motivating and Appreciating Achievements
For caregivers, the improvement of patients should be associated with feelings of self-esteem and satisfaction. In a study on oncology physicians and nurses during the COVID-19 epidemic, medical staff working in the front lines experienced less burnout than those working in usual wards; this was explained by a deeper sense of personal achievement as they saw the direct results of their efforts (59). Similarly, after the 2010 Haiti earthquake, burnout was low among mental health workers, which was attributed to satisfaction associated with helping others (71). Rewarding the successful achievements of personnel financially, institutionally, and in public will improve their performance (6,16,52).
Providing Professional Support
If the level of burnout interferes with efficiency or creates a risk of harm to patients, professional support is needed, which can be accomplished by psychiatry clinics organizing “psychological intervention teams” or “burnout clinics,” as applied during the COVID-19 pandemic (53,72).
Asking for Help from Outside
By definition, it may be impossible to cope with medical problems locally, and outside help may be needed. After many kidney disasters, such as the Armenian (73), Marmara (19), Kashmir (41), and Haiti (42) earthquakes, material and personnel support was instrumental in delivering life-saving dialysis services. Similarly, during the COVID-19 pandemic, there was material and personnel support among some countries (74). Collaboration with nongovernmental organizations such as MSF may be helpful (19,75). MSF provided, and still provides, COVID-19–related support in several countries worldwide to the most vulnerable, such as homeless people, migrants, and the elderly, in precarious circumstances (76). However, during the pandemic many countries closed their borders and tackled COVID-19 at a local scale. Notably, the European Union initially had difficulties in creating solidarity among its member states. This was mainly because of its limited competence in health, although it was subsequently followed by many coordinating activities (77).
Modifying Current Care Paradigms
COVID-19 revealed the weaknesses of the present hospital-centered therapeutic model, including maintenance dialysis, making a move to home dialysis (peritoneal dialysis and home hemodialysis) as the preferred track, rather than focusing on in-center hemodialysis as a general policy (78 –80). Acute peritoneal dialysis may offer both medical and logistic advantages, but also drawbacks, in resource-constrained conditions (3). Advantages include no need for vascular access, lower risk of disequilibrium syndrome, simpler techniques, less hemodynamic instability, and no need for water and electricity. However, these benefits are counterbalanced by a low clearance of small molecules, difficult application if the patient cannot lie down, and high risk of bacterial peritonitis in austere and chaotic circumstances (81), which are frequent in disasters.
In the case of an outbreak in a hemodialysis center, trajectories of infected and noninfected patients should completely be separated to attain cohort isolation and avoid viral transmission.
Paying Attention for Correct Information for All Personnel
Timely, accurate, and unambiguous communication with the teams without over-reporting as well as organizing brief update sessions with an established periodicity significantly affect team spirit. Use of virtual meetings can facilitate access for everyone.
Promoting a Healthy Work Environment
Several strategies such as creating good team spirit, establishing shorter work shifts, maintaining the balance between private and professional life, and making breaks possible for relaxation and rest may prevent burnout (6,82), but are not specific to disasters. Particularly at the start of the COVID-19 crisis, the shortage of PPE necessitated rationing, although personnel had to keep working for longer periods without replacing PPE, precluding essential rest breaks. This problem has largely been neutralized by better advance planning and delivery.
Personal (Individual) Measures
Only some of these measures will be practical in disasters, but nevertheless all options should be explored.
Training on Coping with Stress and Problematic Conditions
Special learning techniques such as cognitive restructuring of irrational thoughts, mindfulness, stress management training, conflict resolution, and resilience promotion vis-à-vis colleagues may help in coping with excessive workload, stress, and burnout (63,83). Special techniques such as yoga or meditation may be of help for relaxation (8). Again, these measures are also instrumental for quality of care because psychologic well-being has an important influence on provided health care (82). However, they should optimally be initiated before, and not during, disasters.
Minimizing the Stigma of Emotional Distress
Professionals should be aware that they are at greater risk of being emotionally affected by the crisis than the rest of the population. The feeling of being forced to function optimally but not reaching this goal may be amplified by the message of heroism transmitted and emphasized by the press, government, and population. With a proper culture of support, seeking help when feeling overwhelmed can be considered a professional strength, not a weakness.
Maintaining Physical Health
Healthy nutrition, avoiding smoking and alcohol, exercise, and adequate sleep are essential to cope with the exhaustion component of burnout (53), but these may not always be possible during disasters due to demanding circumstances, or policy measures such as strict lockdowns precluding exercise.
Burnout symptoms can persist years after an event or recur; hence, long-term psychologic support may be necessary for disaster caregivers (84).
Conclusions
Mass disasters are characterized by increased kidney health care demand, whereas medical and logistic drawbacks limit adequate response. So far, large-scale infrastructural problems have been generated mainly by earthquakes causing AKI and hurricanes adversely affecting dialysis patients. Our experience with COVID-19 was that adequate provision of life-saving medical care, such as dialysis, artificial ventilation, and extracorporeal machine oxygenation, was a central problem affecting personnel on the front lines. This pandemic also emphasized the role of burnout, as another major drawback for providing health care. Kidney health care personnel frequently suffer from burnout due to heavy workloads, a shortage of personnel and material, perceived loss of efficacy, and concerns for personal safety. Preventing burnout is vital to avoid personal health problems, malpractice, lack of manpower, team inefficiency, and unsatisfactory health care delivery at large. Hopefully, lessons learned during the COVID-19 pandemic will be helpful for investigating the reasons and predictors of burnout during mass disasters and how to avoid this problem in future disasters to save as many lives as possible.
Disclosures
M. Sever reports receiving personal fees from Fresenius Medical Care, Turkey, for serving as an advisor, and receiving honorarium from Nobel Pharmaceuticals, Turkey, outside the submitted work. All remaining authors have nothing to disclose.
Funding
None.
Footnotes
Published online ahead of print. Publication date available at www.cjasn.org.
References
- 1. World Health Organization (WHO) : Glossary of humanitarian terms. Available at: https://www.who.int/hac/about/reliefweb-aug2008.pdf. Accessed November 6, 2020
- 2. Guha-Sapir D, Hoyois P; EM-DAT: The International Disaster database, general classification of disasters. Available at: https://www.emdat.be/classification/. Accessed November 6, 2020
- 3. Sever MS, Vanholder R; RDRTF of ISN Work Group on Recommendations for the Management of Crush Victims in Mass Disasters: Recommendation for the management of crush victims in mass disasters. Nephrol Dial Transplant 27[Suppl 1]: i1–i67, 2012. [DOI] [PubMed] [Google Scholar]
- 4. Agrawal V, Plantinga L, Abdel-Kader K, Pivert K, Provenzano A, Soman S, Choi MJ, Jaar BG: Burnout and emotional well-being among nephrology fellows: A national online survey. J Am Soc Nephrol 31: 675–685, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. World Health Organization : Coronavirus disease (COVID-2019) situation reports. Available at: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports/. Accessed November 6, 2020
- 6. Maslach C, Leiter MP: Understanding the burnout experience: Recent research and its implications for psychiatry. World Psychiatry 15: 103–111, 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Doolittle BR, Windish DM, Seelig CB: Burnout, coping, and spirituality among internal medicine resident physicians. J Grad Med Educ 5: 257–261, 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Yates SW: Physician stress and burnout. Am J Med 133: 160–164, 2020. [DOI] [PubMed] [Google Scholar]
- 9. Hall LH, Johnson J, Watt I, Tsipa A, O’Connor DB: Healthcare staff wellbeing, burnout, and patient safety: A systematic review. PLoS One 11: e0159015, 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Williams ES, Rathert C, Buttigieg SC: The personal and professional consequences of physician burnout: A systematic review of the literature. Med Care Res Rev 77: 371–386, 2020. [DOI] [PubMed] [Google Scholar]
- 11. Rathert C, Williams ES, Linhart H: Evidence for the quadruple aim: A systematic review of the literature on physician burnout and patient outcomes. Med Care 56: 976–984, 2018. [DOI] [PubMed] [Google Scholar]
- 12. Balch CM, Oreskovich MR, Dyrbye LN, Colaiano JM, Satele DV, Sloan JA, Shanafelt TD: Personal consequences of malpractice lawsuits on American surgeons. J Am Coll Surg 213: 657–667, 2011. [DOI] [PubMed] [Google Scholar]
- 13. Amoafo E, Hanbali N, Patel A, Singh P: What are the significant factors associated with burnout in doctors? Occup Med (Lond) 65: 117–121, 2015. [DOI] [PubMed] [Google Scholar]
- 14. Bianchi R, Schonfeld IS, Laurent E: Burnout-depression overlap: A review. Clin Psychol Rev 36: 28–41, 2015. [DOI] [PubMed] [Google Scholar]
- 15. Suzuki Y, Fukasawa M, Obara A, Kim Y: Burnout among public servants after the Great East Japan Earthquake: Decomposing the construct aftermath of disaster. J Occup Health 59: 156–164, 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Sasangohar F, Jones SL, Masud FN, Vahidy FS, Kash BA: Provider burnout and fatigue during the COVID-19 pandemic: Lessons learned from a high-volume intensive care unit. Anesth Analg 131: 106–111, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Trabucchi M, De Leo D: Nursing homes or besieged castles: COVID-19 in northern Italy. Lancet Psychiatry 7: 387–388, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Sever MS, Vanholder R: Management of crush victims in mass disasters: Highlights from recently published recommendations. Clin J Am Soc Nephrol 8: 328–335, 2013. [DOI] [PubMed] [Google Scholar]
- 19. Vanholder R, Sever MS, De Smet M, Erek E, Lameire N: Intervention of the renal disaster relief task force in the 1999 Marmara, Turkey earthquake. Kidney Int 59: 783–791, 2001. [DOI] [PubMed] [Google Scholar]
- 20. Kopp JB, Ball LK, Cohen A, Kenney RJ, Lempert KD, Miller PE, Muntner P, Qureshi N, Yelton SA: Kidney patient care in disasters: Lessons from the hurricanes and earthquake of 2005. Clin J Am Soc Nephrol 2: 814–824, 2007. [DOI] [PubMed] [Google Scholar]
- 21. Sever MS, Erek E, Vanholder R, Yurugen B, Kantarci G, Yavuz M, Ergin H, Bozfakioglu S, Dalmak S, Tulbek MY, Kiper H, Lameire N: Renal replacement therapies in the aftermath of the catastrophic Marmara earthquake. Kidney Int 62: 2264–2271, 2002. [DOI] [PubMed] [Google Scholar]
- 22. Perico L, Benigni A, Remuzzi G: Should COVID-19 concern nephrologists? Why and to what extent? The emerging impasse of angiotensin blockade. Nephron 144: 213–221, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Chen T, Wu D, Chen H, Yan W, Yang D, Chen G, Ma K, Xu D, Yu H, Wang H, Wang T, Guo W, Chen J, Ding C, Zhang X, Huang J, Han M, Li S, Luo X, Zhao J, Ning Q: Clinical characteristics of 113 deceased patients with coronavirus disease 2019: Retrospective study [published correction appears in BMJ 368: m1295, 2020 10.1136/bmj.m1295]. BMJ 368: m1091, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Wendling P: Medscape medical news: Kidney complications in COVID-19 send hospitals scrambling, 2020. Available at: https://www.medscape.com/viewarticle/929073#vp_3. Accessed November 6, 2020
- 25. Yang X, Yu Y, Xu J, Shu H, Xia J, Liu H, Wu Y, Zhang L, Yu Z, Fang M, Yu T, Wang Y, Pan S, Zou X, Yuan S, Shang Y: Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: A single-centered, retrospective, observational study [published correction appears in Lancet Respir Med 8: e26, 2020 10.1016/S2213-2600(20)30103-X]. Lancet Respir Med 8: 475–481, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Pei G, Zhang Z, Peng J, Liu L, Zhang C, Yu C, Ma Z, Huang Y, Liu W, Yao Y, Zeng R, Xu G: Renal involvement and early prognosis in patients with COVID-19 pneumonia. J Am Soc Nephrol 31: 1157–1165, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Cheng Y, Luo R, Wang K, Zhang M, Wang Z, Dong L, Li J, Yao Y, Ge S, Xu G: Kidney disease is associated with in-hospital death of patients with COVID-19. Kidney Int 97: 829–838, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Agarwal A, Zoccali C, Jha V: Ensuring optimal care for people with kidney diseases during the COVID-19 pandemic, 2020. Available at: https://www.theisn.org/images/Statement_ASN_ERA-EDTA_ISN.pdf. Accessed November 6, 2020
- 29. Goldfarb DS, Benstein JA, Zhdanova O, Hammer E, Block CA, Caplin NJ, Thompson N, Charytan DM: Impending shortages of kidney replacement therapy for COVID-19 patients. Clin J Am Soc Nephrol 15: 880–882, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Fishman JA, Grossi PA: Novel Coronavirus-19 (COVID-19) in the immunocompromised transplant recipient: #Flatteningthecurve. Am J Transplant 20: 1765–1767, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. British Transplantation Society : Guidance on the management of transplant recipients diagnosed with or suspected of having COVID19. Available at: https://bts.org.uk/wp-content/uploads/2020/03/Clinical_management_transplant_recipients.pdf. Accessed November 6, 2020
- 32. ERA-EDTA Working Group EUDIAL : ERA-EDTA information for nephrologists and other professionals on prevention and treatment of covid-19 infections in kidney patients, 2020. Available at: https://www.era-edta.org/en/covid-19-news-and-information/#toggle-id-2. Accessed November 6, 2020
- 33. Watnick S, McNamara E: On the frontline of the COVID-19 outbreak: Keeping patients on long-term dialysis safe. Clin J Am Soc Nephrol 15: 710–713, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Maggiore U, Abramowicz D, Crespo M, Mariat C, Mjoen G, Peruzzi L, Sever MS, Oniscu GC, Hilbrands L, Watschinger B: How should I manage immunosuppression in a kidney transplant patient with COVID-19? An ERA-EDTA DESCARTES expert opinion. Nephrol Dial Transplant 35: 899–904, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Nadim MK, Forni LG, Mehta RL, Connor MJ Jr, Liu KD, Ostermann M, Rimmele T, Zarbock A, Bell S, Bihorac A, Cantaluppi V, Hoste E, Husain-Syed F, Germain MJ, Goldstein SL, Gupta S, Joannidis M, Kashani K, Koyner JL, Legrand M, Lumlertgul N, Mohan S, Pannu N, Peng Z, Perez-Fernandez XL, Pickkers P, Prowle J, Reis T, Srisawat N, Tolwani A, Vijayan A, Villa G, Yang L, Ronco C, Kellum JA: COVID-19-associated acute kidney injury: Consensus report of the 25th Acute Disease Quality Initiative (ADQI) Workgroup [published correction appears in Nat Rev Nephrol 16: 765, 2020 10.1038/s41581-020-00372-5]. Nat Rev Nephrol 16: 747–764, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Williamson EJ, Walker AJ, Bhaskaran K, Bacon S, Bates C, Morton CE, Curtis HJ, Mehrkar A, Evans D, Inglesby P, Cockburn J, McDonald HI, MacKenna B, Tomlinson L, Douglas IJ, Rentsch CT, Mathur R, Wong AYS, Grieve R, Harrison D, Forbes H, Schultze A, Croker R, Parry J, Hester F, Harper S, Perera R, Evans SJW, Smeeth L, Goldacre B: Factors associated with COVID-19-related death using OpenSAFELY. Nature 584: 430–436, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Clark A, Jit M, Warren-Gash C, Guthrie B, Wang HHX, Mercer SW, Sanderson C, McKee M, Troeger C, Ong KL, Checchi F, Perel P, Joseph S, Gibbs HP, Banerjee A, Eggo RM; Centre for the Mathematical Modelling of Infectious Diseases COVID-19 working group: Global, regional, and national estimates of the population at increased risk of severe COVID-19 due to underlying health conditions in 2020: A modelling study. Lancet Glob Health 8: e1003–e1017, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Bansal P, Bingemann TA, Greenhawt M, Mosnaim G, Nanda A, Oppenheimer J, Sharma H, Stukus D, Shaker M: Clinician wellness during the COVID-19 pandemic: Extraordinary times and unusual challenges for the allergist/immunologist. J Allergy Clin Immunol Pract 8: 1781–1790.e3, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Fessell D, Cherniss C: Coronavirus Disease 2019 (COVID-19) and beyond: Micropractices for burnout prevention and emotional wellness. J Am Coll Radiol 17: 746–748, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. The Editors of Encyclopaedia Britannica : Indian Ocean tsunami of 2004. Available at https://www.britannica.com/event/Indian-Ocean-tsunami-of-2004. Accessed November 6, 2020
- 41. Vanholder R, van der Tol A, De Smet M, Hoste E, Koç M, Hussain A, Khan S, Sever MS: Earthquakes and crush syndrome casualties: Lessons learned from the Kashmir disaster. Kidney Int 71: 17–23, 2007. [DOI] [PubMed] [Google Scholar]
- 42. Vanholder R, Gibney N, Luyckx VA, Sever MS; Renal Disaster Relief Task Force: Renal disaster relief task force in Haiti earthquake. Lancet 375: 1162–1163, 2010. [DOI] [PubMed] [Google Scholar]
- 43. Sever MS, Remuzzi G, Vanholder R: Disaster medicine and response: Optimizing life-saving potential. Am J Disaster Med 13: 253–264, 2018. [DOI] [PubMed] [Google Scholar]
- 44. The Lancet: COVID-19: Protecting health-care workers. Lancet 395: 922, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Sever MS, Vanholder R, Lameire N: Management of crush-related injuries after disasters. N Engl J Med 354: 1052–1063, 2006. [DOI] [PubMed] [Google Scholar]
- 46. Sever MS, Erek E, Vanholder R, Koc M, Yavuz M, Ergin H, Kazancioglu R, Serdengecti K, Okumus G, Ozdemir N, Schindler R, Lameire N; Marmara Earthquake Study Group: Treatment modalities and outcome of the renal victims of the Marmara earthquake. Nephron 92: 64–71, 2002. [DOI] [PubMed] [Google Scholar]
- 47. Hirsch JS, Ng JH, Ross DW, Sharma P, Shah HH, Barnett RL, Hazzan AD, Fishbane S, Jhaveri KD; Northwell COVID-19 Research Consortium; Northwell Nephrology COVID-19 Research Consortium: Acute kidney injury in patients hospitalized with COVID-19. Kidney Int 98: 209–218, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Abelson R, Fink S, Kulish N, Thomas K: An overlooked, possibly fatal coronavirus crisis: A dire need for kidney dialysis, 2020. Available at: https://www.nytimes.com/2020/04/18/health/kidney-dialysis-coronavirus.html?auth=link-dismiss-google1tap. Accessed November 6, 2020
- 49. Sise ME, Baggett MV, Shepard JO, Stevens JS, Rhee EP: Case 17-2020: A 68-year-old man with covid-19 and acute kidney injury. N Engl J Med 382: 2147–2156, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Vanholder R, Van Biesen W, Lameire N, Sever MS; International Society of Nephrology/Renal Disaster Relief Task Force: The role of the international society of nephrology/renal disaster relief task force in the rescue of renal disaster victims. Contrib Nephrol 156: 325–332, 2007. [DOI] [PubMed] [Google Scholar]
- 51. Lameire N, Mehta R, Vanholder R, Sever M: The organization and interventions of the ISN Renal Disaster Relief Task Force. Adv Ren Replace Ther 10: 93–99, 2003. [DOI] [PubMed] [Google Scholar]
- 52. Dewey C, Hingle S, Goelz E, Linzer M: Supporting clinicians during the COVID-19 pandemic. Ann Intern Med 172: 752–753, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. World Health Organization (WHO) : Mental health and psychosocial considerations during the COVID-19 outbreak, 2020. Available at: https://www.who.int/docs/default-source/coronaviruse/mental-health-considerations.pdf?sfvrsn=6d3578af_2. Accessed November 6, 2020
- 54. Waeckerle JF: Disaster planning and response. N Engl J Med 324: 815–821, 1991. [DOI] [PubMed] [Google Scholar]
- 55. Ling K, Xianxiu W, Xiaowei Z: Analysis of nurses’ job burnout and coping strategies in hemodialysis centers. Medicine (Baltimore) 99: e19951, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Karakoc A, Yilmaz M, Alcalar N, Esen B, Kayabasi H, Sit D: Burnout syndrome among hemodialysis and peritoneal dialysis nurses. Iran J Kidney Dis 10: 395–404, 2016. [PubMed] [Google Scholar]
- 57. Choi KR, Skrine Jeffers K, Cynthia Logsdon M: Nursing and the novel coronavirus: Risks and responsibilities in a global outbreak. J Adv Nurs 76: 1486–1487, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Abril GEP: La paz: A Madrid hospital at war against Covid-19, 2020. Available at: https://english.elpais.com/eps/2020-04-24/la-paz-a-madrid-hospital-at-war-against-covid-19.htm. Accessed November 6, 2020
- 59. Wu Y, Wang J, Luo C, Hu S, Lin X, Anderson AE, Bruera E, Yang X, Wei S, Qian Y: A comparison of burnout frequency among oncology physicians and nurses working on the front lines and usual wards during the COVID-19 epidemic in Wuhan, China. J Pain Symptom Manage 60: e60–e65, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Murakami N, Siktel HB, Lucido D, Winchester JF, Harbord NB: Disaster preparedness and awareness of patients on hemodialysis after Hurricane Sandy. Clin J Am Soc Nephrol 10: 1389–1396, 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Kelman J, Finne K, Bogdanov A, Worrall C, Margolis G, Rising K, MaCurdy TE, Lurie N: Dialysis care and death following Hurricane Sandy. Am J Kidney Dis 65: 109–115, 2015. [DOI] [PubMed] [Google Scholar]
- 62. Frontières Médecins Sans (MSF): Clinical guidelines - Diagnosis and treatment manual, 2019. Available at: https://www.medbox.org/preview/5da4706a-4bc4-4a83-a1b6-35c31fcc7b87/doc.pdf. Accessed November 6, 2020
- 63. West CP, Dyrbye LN, Shanafelt TD: Physician burnout: Contributors, consequences and solutions. J Intern Med 283: 516–529, 2018. [DOI] [PubMed] [Google Scholar]
- 64. West CP, Dyrbye LN, Erwin PJ, Shanafelt TD: Interventions to prevent and reduce physician burnout: A systematic review and meta-analysis. Lancet 388: 2272–2281, 2016. [DOI] [PubMed] [Google Scholar]
- 65. Sever MS, Lameire N, Vanholder R: Renal disaster relief: From theory to practice. Nephrol Dial Transplant 24: 1730–1735, 2009. [DOI] [PubMed] [Google Scholar]
- 66. Moazzami B, Razavi-Khorasani N, Dooghaie Moghadam A, Farokhi E, Rezaei N: COVID-19 and telemedicine: Immediate action required for maintaining healthcare providers well-being. J Clin Virol 126: 104345, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. El Shamy O, Tran H, Sharma S, Ronco C, Narayanan M, Uribarri J: Telenephrology with remote peritoneal dialysis monitoring during coronavirus disease 19. Am J Nephrol 51: 480–482, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Savla D, Chertow GM, Meyer T, Anand S: Can twice weekly hemodialysis expand patient access under resource constraints? Hemodial Int 21: 445–452, 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Meyer TW, Hostetter TH, Watnick S: Twice-weekly hemodialysis is an option for many patients in times of dialysis unit stress. J Am Soc Nephrol 31: 1141–1142, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Ma Y, Diao B, Lv X, Zhu J, Liang W, Liu L, Bu W, Cheng H, Zhang S, Yang L, Shi M, Ding G, Shen B, Wang H: 2019 novel coronavirus disease in hemodialysis (HD) patients: Report from one HD center in Wuhan, China, 2020. Available at: https://www.medrxiv.org/content/10.1101/2020.02.24.20027201v2.full.pdf. Accessed November 6, 2020
- 71. James LE, Noel JR, Roche Jean Pierre YM: A mixed-methods assessment of the experiences of lay mental health workers in postearthquake Haiti. Am J Orthopsychiatry 84: 152–163, 2014. [DOI] [PubMed] [Google Scholar]
- 72. Kang L, Li Y, Hu S, Chen M, Yang C, Yang BX, Wang Y, Hu J, Lai J, Ma X, Chen J, Guan L, Wang G, Ma H, Liu Z: The mental health of medical workers in Wuhan, China dealing with the 2019 novel coronavirus. Lancet Psychiatry 7: e14, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Solez K, Bihari D, Collins AJ, Eknoyan G, Eliahou H, Fedorov VD, Kjellstrand C, Lameire N, Letteri J, Nissenson AR, Wauters JP, Yamamoto Y: International dialysis aid in earthquakes and other disasters. Kidney Int 44: 479–483, 1993. [DOI] [PubMed] [Google Scholar]
- 74. Cui M: COVID-19: China steps in to help Italy battle the virus, 2020. Available at https://www.dw.com/en/covid-19-china-steps-in-to-help-italy-battle-the-virus/a-52901560. Accessed November 6, 2020
- 75. Vanholder R, Borniche D, Claus S, Correa-Rotter R, Crestani R, Ferir MC, Gibney N, Hurtado A, Luyckx VA, Portilla D, Rodriguez S, Sever MS, Vanmassenhove J, Wainstein R: When the earth trembles in the Americas: The experience of Haiti and Chile 2010. Nephron Clin Pract 117: c184–c197, 2011. [DOI] [PubMed] [Google Scholar]
- 76. Medecins sans Frontieres (MSF) : Coronavirus COVID-19 pandemic. A race against the pandemic – MSF COVID-19 crisis update, 2020. Available at: https://www.msf.org/msf-covid-19-crisis-update. Accessed November 6, 2020
- 77.The European Union: The common EU response to COVID-19, 2020. Available at: https://europa.eu/european-union/coronavirus-response_en. Accessed November 6, 2020
- 78. Charnow JA: COVID-19 crisis could speed adoption of home dialysis, 2020. Available at: https://www.renalandurologynews.com/home/news/nephrology/hemodialysis/covid-19-crisis-could-speed-adoption-of-home-dialysis/. Accessed November 6, 2020
- 79. Brown EA, Perl J: Increasing peritoneal dialysis use in response to the COVID-19 pandemic: Will it go viral? J Am Soc Nephrol 31: 1928–1930, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80. Quintaliani G, Reboldi G, Di Napoli A, Nordio M, Limido A, Aucella F, Messa P, Brunori G; Italian Society of Nephrology COVID-19 Research Group: Exposure to novel coronavirus in patients on renal replacement therapy during the exponential phase of COVID-19 pandemic: Survey of the Italian Society of Nephrology. J Nephrol 33: 725–736, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. Sever MS, Sever L, Vanholder R: Disasters, children and the kidneys. Pediatr Nephrol 35: 1381–1393, 2020. [DOI] [PubMed] [Google Scholar]
- 82. Mattei A, Fiasca F, Mazzei M, Necozione S, Bianchini V: Stress and burnout in health-care workers after the 2009 L’Aquila earthquake: A cross-sectional observational study. Front Psychiatry 8: 98, 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. Shaw SCK: Hopelessness, helplessness and resilience: The importance of safeguarding our trainees’ mental wellbeing during the COVID-19 pandemic. Nurse Educ Pract 44: 102780, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84. Fujitani K, Carroll M, Yanagisawa R, Katz C: Burnout and psychiatric distress in local caregivers two years after the 2011 Great East Japan earthquake and fukushima nuclear radiation disaster. Community Ment Health J 52: 39–45, 2016. [DOI] [PubMed] [Google Scholar]