Significance Statement
Prior work suggests that uniform access to health insurance coverage and health care services reduces disparities in treatment and outcomes of patients with CKD. This study assessed whether expansions of Medicaid coverage to low-income adults in the United States under the Affordable Care Act (ACA) were associated with changes in the incidence rate of kidney failure. The authors found that, in the entire adult population aged 19–64 years, the ACA’s Medicaid expansions were associated with a statistically significant 3% relative reduction in kidney failure incidence in the early period (years 2 and 3) after expansion. However, this decline was not sustained in the later period (years 4 and 5) after expansion. Further research is needed to understand the relationship between expanding health insurance coverage and the incidence of kidney failure.
Keywords: chronic kidney disease, kidney failure, health insurance, Medicaid, uninsured, epidemiology and outcomes
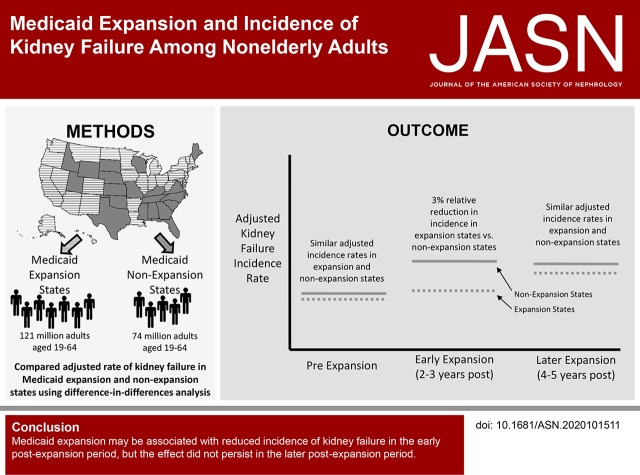
Visual Abstract
Abstract
Background
Low-income individuals without health insurance have limited access to health care. Medicaid expansions may reduce kidney failure incidence by improving access to chronic disease care.
Methods
Using a difference-in-differences analysis, we examined the association between Medicaid expansion status under the Affordable Care Act (ACA) and the kidney failure incidence rate among all nonelderly adults, aged 19–64 years, in the United States, from 2012 through 2018. We compared changes in kidney failure incidence in states that implemented Medicaid expansions with concurrent changes in nonexpansion states during pre-expansion, early postexpansion (years 2 and 3 postexpansion), and later postexpansion (years 4 and 5 postexpansion).
Results
The unadjusted kidney failure incidence rate increased in the early years of the study period in both expansion and nonexpansion states before stabilizing. After adjustment for population sociodemographic characteristics, Medicaid expansion status was associated with 2.20 fewer incident cases of kidney failure per million adults per quarter in the early postexpansion period (95% CI, −3.89 to −0.51) compared with nonexpansion status, a 3.07% relative reduction (95% CI, −5.43% to −0.72%). In the later postexpansion period, Medicaid expansion status was not associated with a statistically significant change in kidney failure incidence (−0.56 cases per million per quarter; 95% CI, −2.71 to 1.58) compared with nonexpansion status and the pre-expansion time period.
Conclusions
The ACA Medicaid expansion was associated with an initial reduction in kidney failure incidence among the entire, nonelderly, adult population in the United States; but the changes did not persist in the later postexpansion period. Further study is needed to determine the long-term association between Medicaid expansion and changes in kidney failure incidence.
Kidney failure, which affects >700,000 Americans, is a serious condition associated with increased morbidity and mortality, lost productivity, high spending, and impaired quality of life.1 In the United States, the burden of kidney failure disproportionately falls on the country’s most disadvantaged communities, with increased incidence rates among persons with lower income and among Black, Hispanic, and Native American persons.1–6
Kidney failure due to diabetes and hypertension, the two leading causes, can be prevented or delayed by control of BP and glucose, through initiation and intensification of appropriate medications, and tailored lifestyle recommendations.1,7–15 However, low-income individuals without health insurance have limited ability to finance health services, are more likely to have undiagnosed hypertension and diabetes, and often forego effective preventive and chronic disease care.16–19 Prior work has found disparities in the treatment and outcomes of patients with CKD are attenuated among populations with uniform health insurance coverage and health care access,20,21 suggesting that expanding health insurance coverage to low-income populations may reduce the incidence of kidney failure.
The Affordable Care Act (ACA) provided states with the option to expand Medicaid coverage to citizens and qualified permanent residents with incomes <138% of the federal poverty level beginning in 2014. Expansions of Medicaid coverage have been associated with improved access to care for chronic diseases, including diabetes and hypertension, and lower 1-year mortality for individuals with kidney failure initiating dialysis.22–26 A total of 25 states, including the District of Columbia, expanded their Medicaid programs on January 1, 2014, and 14 more have since adopted expansions, substantially increasing insurance coverage rates for nonelderly adults in these states.27–30
This study examined the association of the ACA Medicaid expansions with the incidence rate of kidney failure for nonelderly adults aged 19–64.
Methods
Study Design
We used a difference-in-differences approach to examine changes in the quarterly all-cause incidence rate of kidney failure among all nonelderly adults residing in states that expanded Medicaid eligibility under the ACA, relative to concurrent changes in nonexpansion states. The study period spanned from January 1, 2012 through December 31, 2018. The postexpansion period for each state was defined on the basis of its own implementation date (see Supplemental Table 1). Brown University’s Institutional Review Board and the Centers for Medicare and Medicaid Services (CMS) Privacy Board approved the study and waived the requirement for informed consent.
Data Sources and Population
The study population included all persons aged 19–64 years old residing in 2351 Public Use Microdata Areas (PUMAs) in the 50 states and District of Columbia. PUMAs are contiguous geographic areas of at least 100,000 persons nested within states, and are the most detailed level of geography with exact person-counts that are available annually in the American Community Survey (ACS)—an ongoing survey of approximately 3.5 million households per year, designed to be representative of the US population. Using the ACS 1-year Public Use Microdata Sample, we calculated population counts for each age group, sex, and race/ethnicity combination for each PUMA for each year of the study period. Age groups were defined as 19–44 years old and 45–64 years old. Race/ethnicity was categorized as non-Hispanic White, non-Hispanic Black, Hispanic, and other. Other PUMA-level population characteristics were drawn from ACS subject tables. Although Medicaid expansion occurred at the state level, using PUMAs as the unit of analysis allowed us to account for within-state heterogeneity by adjusting for more granular population-level covariates and area-level characteristics.
To identify incident patients with kidney failure, we obtained data from the CMS Renal Management Information System. CMS requires all dialysis facilities and transplant providers that receive Medicare funds to submit the ESRD Medical Evidence Form (CMS 2728) for all incident patients upon treatment initiation; the form includes patient demographic and clinical information, including mailing address.31,32 We geolocated incident patients within PUMAs using ArcGIS spatial mapping software, version 10.5.1 (ESRI). As described in Supplemental Appendix 1 and Supplemental Figure 1, 0.49% of incident patients and 0.21% of the US nonelderly population were excluded from the analysis.
Measures
The primary study outcome was the quarterly all-cause incidence rate of treated kidney failure for each PUMA cell per million population, hereafter referred to simply as the incidence rate, consistent with United States Renal Data System methodology.1 The primary independent variable was an interaction between whether the PUMA was in a state that expanded Medicaid, and whether the time period was after expansion occurred. The postexpansion period was broken into three periods: the first year after expansion (2014 in most states), which was considered a transitional period; the second and third years after expansion (2015–2016 in most states), considered the early postexpansion period; and the fourth and fifth years after expansion (2017–2018 in most states), the later postexpansion period. Each postexpansion period was compared with the baseline pre-expansion period. This specification allowed us to identify any differential effects of Medicaid expansion during the postexpansion period. Because the expansion period for each state was defined by its own implementation date, the later postexpansion period excluded late-expanding states that had not achieved 4 or 5 years postexpansion by the end of the study period. The secondary outcome was the uninsurance rate, evaluated at the person level using ACS Public Use Microdata Sample.33
Covariates for the primary study outcome included age group (19–44 or 45–64 years); sex (male or female); race/ethnicity (non-Hispanic White, non-Hispanic Black, Hispanic, or other); and time-varying, PUMA-level adult population characteristics: the proportion with annual household income below the federal poverty level, the unemployment rate, and the proportion with a high-school degree or equivalency. Covariates for the secondary outcome were the equivalent person-level characteristics.
For incident patients, the dialysis or transplant facility collected and reported information on race/ethnicity using categories available on the CMS 2728 form. PUMA population counts were constructed using the same categories for consistency. Race/ethnicity was included in the study due to well-documented disparities in incidence of kidney failure, and to allow for stratified analyses.1
Statistical Analyses
To model the area-level incidence of kidney failure, we used multivariable linear models with Huber–White robust SEMs clustered at the state level to account for state-level correlation and serial autocorrelation.34 Models for the primary outcome included PUMA fixed effects (to account for underlying area-level factors, such as health system capacity; these fixed effects also capture state-level differences), an indicator for season, and year-quarter fixed effects (to account for any secular trends in the study outcome), and were weighted by the population of each PUMA cell (Supplemental Appendix 2). To model person-level uninsurance rates, we used multivariable linear models with replicate survey weights to account for the ACS sampling design and Huber–White robust SEMs clustered at the state level (Supplemental Appendix 3).33 Models for the secondary outcome included state and year fixed effects.
In exploratory analyses, we stratified our analyses by baseline PUMA socioeconomic characteristics (nonelderly adult poverty and uninsurance rates), PUMA metropolitan status, and demographic characteristics (race/ethnicity, age group, and sex) to quantify changes in incidence across these subpopulations. All analyses were conducted in Stata version 16 (StataCorp) and used two-tailed hypothesis testing with a significance threshold of P<0.05.
Sensitivity Analyses
We conducted a number of sensitivity analyses to assess the validity of the difference-in-differences study design and to test robustness to alternative model specifications, populations, and time periods. First, we confirmed trends in incidence rates were parallel in expansion and nonexpansion states before 2014 by testing the significance of an expansion-by-time indicator using pre-ACA data and by conducting event-study falsification tests during the pre-expansion period. Second, we excluded demographic and time-varying PUMA-level population characteristics from our model, including only time and geographic fixed effects. Third, we excluded time-varying PUMA-level population characteristics from our model, adjusting only for age group, sex, and race/ethnicity. Fourth, we restricted incident patients to those with kidney failure due to diabetes and due to hypertension, the two most common causes of kidney failure. Fifth, we excluded states that expanded their Medicaid programs to many nonelderly adults before 2014, following previous research.35 Sixth, we used states rather than PUMAs as the geographic unit of analysis, using state-level covariates. Seventh, we modeled the entire postexpansion period together and separately estimated difference-in-difference estimates for each year postexpansion. Eighth, we modeled the count of incident patients, rather than the incidence rate, using a generalized linear model with a log link and negative binomial distribution to account for zero inflation of the outcome and including each population cell size as a predictor. Ninth, we restricted our incidence rate calculations to incident patients initiating maintenance dialysis, excluding those who received a preemptive kidney transplant. Prior work has found Medicaid expansion is associated with an increase in Medicaid-covered preemptive transplants,36 so including such patients in incidence-rate calculations may disproportionately increase the incidence rate in Medicaid expansion states in the postexpansion period.
Results
Characteristics of Study Population
The study included 2351 PUMAs (1440 in the 31 states and District of Columbia that expanded Medicaid, 911 in the 19 states that did not). The annual average nonelderly adult population size was 195,090,190. Of this group, an annual average of 120,740,740 resided in expansion states (baseline characteristics: 56.6% aged 19–44, 50.3% female, 64.8% non-Hispanic White, 10.9% non-Hispanic Black, 15.2% Hispanic) and 74,349,449 lived in nonexpansion states (baseline characteristics: 57.6% aged 19–44, 50.5% female, 62.1% non-Hispanic White, 16.4% non-Hispanic Black, 16.1% Hispanic) (Table 1). The baseline uninsurance rate in PUMAs in expansion states was 6 percentage points lower than that in nonexpansion states, whereas differences in the poverty rate, unemployment rate, and proportion of high-school graduates were within 1.2 percentage points.
Table 1.
Characteristics of incident and nonelderly adult populations by state Medicaid expansion status
| Characteristics | Total | Expansion States a | Nonexpansion States | ||
|---|---|---|---|---|---|
| Pre-expansion | Postexpansion | 2012–2013 | 2014–2018 | ||
| Incident patient characteristics | |||||
| Number of patients | 422,526 | 75,891 | 171,442 | 47,210 | 127,983 |
| Age (yr), mean (SD) | 51.3 (10.4) | 51.3 (10.5) | 51.4 (10.4) | 51.2 (10.4) | 51.2 (10.4) |
| Age group, % | |||||
| 19–44 years old | 23.4 | 23.0 | 23.0 | 23.7 | 24.0 |
| 45–64 years old | 76.6 | 77.0 | 77.0 | 76.3 | 76.0 |
| Female, % | 40.4 | 40.0 | 39.2 | 42.2 | 41.7 |
| Race/ethnicity, % | |||||
| Non-Hispanic White | 44.2 | 46.7 | 45.9 | 39.7 | 41.9 |
| Non-Hispanic Black | 31.7 | 29.2 | 25.2 | 41.5 | 38.4 |
| Hispanic | 17.7 | 16.5 | 19.9 | 15.6 | 16.3 |
| Other | 6.4 | 7.6 | 9.0 | 3.2 | 3.4 |
| Insurance coverage type, % | |||||
| Medicaid | 23.6 | 22.5 | 32.4 | 15.3 | 15.5 |
| Uninsured | 10.1 | 10.4 | 3.9 | 17.3 | 15.5 |
| Primary cause of kidney failure, % | |||||
| Diabetes | 48.6 | 47.3 | 49.2 | 48.0 | 48.8 |
| Hypertension | 24.3 | 23.3 | 21.9 | 27.5 | 26.8 |
| Other or uncertain | 27.1 | 29.4 | 28.9 | 24.5 | 24.4% |
| Treatment modality, % | |||||
| Dialysis | 96.9 | 96.3 | 96.5 | 97.3 | 97.6 |
| Preemptive transplant | 3.1 | 3.7 | 3.5 | 2.7 | 2.4 |
| eGFR, mean (SD) b | 9.7 (5.3) | 9.9 (5.6) | 9.6 (5.3) | 9.7 (5.3) | 9.6 (5.2) |
| Nonelderly adult PUMA-level characteristics c | |||||
| Number of states | 51 | 32 | 19 | ||
| Number of PUMAs | 2351 | 1440 | 911 | ||
| Total annual population, mean (SD) | 195,090,190 (1,641,522) | 120,740,740 (528,433) | 74,349,449 (1,183,138) | ||
| Age group, % (SD) | |||||
| 19–44 years old | 57.1 (6.5) | 56.6 (6.5) | 57.0 (6.6) | 57.6 (6.3) | 57.5 (6.3) |
| 45–64 years old | 42.9 (6.5) | 43.4 (6.5) | 43.0 (6.6) | 42.4 (6.3) | 42.5 (6.3) |
| Female, % (SD) | 50.3 (2.2) | 50.3 (2.1) | 50.2 (2.1) | 50.5 (2.2) | 50.5 (2.2) |
| Race/Ethnicity, % (SD) | |||||
| Non-Hispanic White | 61.5 (25.1) | 64.8 (25.6) | 60.8 (26.2) | 62.1 (23.2) | 60.1 (23.4) |
| Non-Hispanic Black | 12.6 (15.8) | 10.9 (15.4) | 10.0 (14.4) | 16.4 (16.6) | 16.6 (16.6) |
| Hispanic | 17.2 (19.1) | 15.2 (17.7) | 18.3 (19.1) | 16.1 (19.3) | 17.3 (19.9) |
| Other | 8.7 (9.5) | 9.1 (10.3) | 10.9 (11.2) | 5.4 (4.9) | 6.1 (5.4) |
| Uninsured, % (SD) | 15.3 (8.8) | 17.9 (8.4) | 10.1 (5.7) | 24.0 (9.3) | 17.9 (8.0) |
| Poverty rate, % (SD) | 13.8 (6.8) | 14.5 (7.3) | 12.9 (6.8) | 15.7 (6.8) | 14.0 (6.3) |
| Unemployment rate, % (SD) | 6.3 (3.1) | 8.4 (3.5) | 5.6 (2.7) | 8.1 (3.3) | 5.3 (2.3) |
| High school graduate, % (SD) | 87.1 (7.8) | 86.8 (8.2) | 87.6 (8.1) | 85.8 (7.4) | 87.0 (7.1) |
| Rural, % | 13.6 | 12.4 | 11.0 | 17.6 | 16.9 |
Percentages may not add precisely to 100% due to rounding.
For incident patient characteristics, the pre- and postexpansion periods for expansion states are determined by the state’s date of expansion and are defined as beginning the first full quarter of expansion (see Supplemental Table 1). For the PUMA characteristics, the postexpansion period begins the first full year a state is expanded for late-expanding states that expanded midyear.
eGFR is calculated using the CKD Epidemiology Collaboration equation from information reported on CMS 2728 and are given in milliliters per minute per 1.73 m2.71
The mean PUMA characteristics are weighted by the PUMA’s population.
Characteristics of Incident Patients with Kidney Failure
From 2012 to 2018, 422,526 individuals developed kidney failure (Supplemental Figure 1, Supplemental Table 2); of this total, 247,333 resided in expansion states (baseline characteristics: mean age, 51.3 years [SD, 10.5]; 40.0% female; 46.7% non-Hispanic White, 29.2% non-Hispanic Black, and 16.5% Hispanic) and 175,193 resided in nonexpansion states (baseline characteristics: mean age, 51.2 years [SD, 10.4]; 42.2% female; 39.7% non-Hispanic White, 41.5% non-Hispanic Black, and 15.6% Hispanic) (Table 1). Incident patients with kidney failure in expansion states were more likely to have Medicaid coverage and less likely to be uninsured than those in nonexpansion states, especially in the postexpansion period. Incident patients in expansion states were more likely to have received a preemptive transplant (baseline, 3.7% versus 2.7%). The share of kidney failure due to diabetes was similar among those residing in expansion and nonexpansion states, although those in expansion states were less likely to have hypertension as the primary cause and more likely to have a different or uncertain cause. The eGFR at incidence, a measure of kidney function, declined modestly among incident patients in both expansion and nonexpansion states over the study period.
Incidence Rates of Kidney Failure
Figure 1 plots trends in the quarterly incidence rate of kidney failure for states that expanded Medicaid on January 1, 2014, and for nonexpansion states after adjustment for population demographics and seasonality.37 Adjusted incidence rates were initially similar between expansion and nonexpansion states, but diverged beginning in 2015, 1 year after expansion states adopted the Medicaid expansion. This divergence became less pronounced in later years postexpansion. Unadjusted incidence rates were higher in nonexpansion than expansion states, and increased over time in both groups before stabilizing in the later postexpansion period (Supplemental Figure 2).
Figure 1.
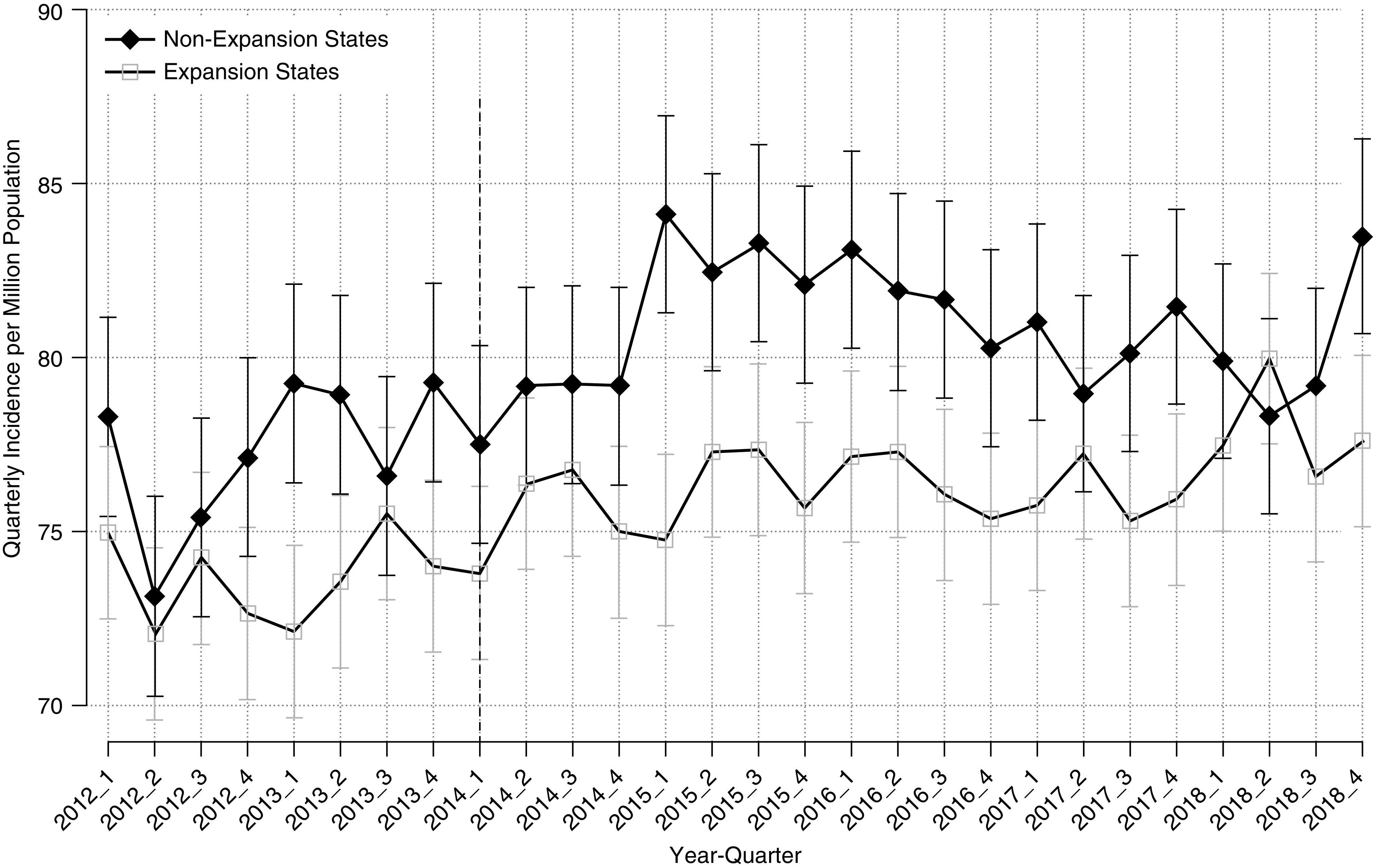
Adjusted quarterly kidney failure incidence per million population, by state Medicaid expansion status; incidence rates were similar in the pre-expansion period before diverging in 2015, one year after expansion occurred. States that expanded their Medicaid programs after January 1, 2014 (time point denoted with a vertical dashed line) are excluded (see Supplemental Table 1). Incidence rates are adjusted for age group, sex, race/ethnicity, and seasonality. Vertical bars provide 95% confidence intervals.
In expansion states, the unadjusted quarterly incidence of kidney failure increased from 71.71 per million population before expansion to 73.89 per million population in the early postexpansion period, and 73.74 per million population in the later postexpansion period (Table 2). In nonexpansion states, the concurrent change was from 80.77 per million to 86.84 per million population in the early postexpansion period, and 85.10 per million population in the later postexpansion period (Table 2). After adjustment for changes in population demographics and other covariates, Medicaid expansion was associated with 2.20 fewer (95% CI, −3.89 to −0.51) incident cases of kidney failure per million adults per quarter in the early postexpansion period, and 0.56 fewer (95% CI, −2.71 to 1.58) cases per million adults per quarter in the later postexpansion period, relative to concurrent trends in nonexpansion states (Table 2). These observed effects represent a 3.07% relative reduction (95% CI, −5.43% to −0.72%) in the early postexpansion period, and a 0.79% relative reduction (95% CI, −3.78% to 2.21%) in the later postexpansion period (Table 2).
Table 2.
Changes in quarterly kidney failure incidence in expansion and nonexpansion states following the ACA Medicaid expansion
| Medicaid Expansion Status | Baseline | Transitional Period | 2 and 3 Years Postexpansion | 4 and 5 Years Postexpansion | Change after Expansion Baseline to 2 and 3 Years Postexpansion (95% CI) | Change after Expansion Baseline to 4 and 5 Years Postexpansion (95% CI) |
|---|---|---|---|---|---|---|
| Expansion states | 71.71 | 72.92 | 73.89 | 73.74 | 2.18 (1.02 to 3.35) | 2.03 (0.85 to 3.21) |
| Nonexpansion states | 80.77 | 82.72 | 86.84 | 85.10 | 6.07 (4.50 to 7.63) | 4.32 (2.76 to 5.89) |
| Unadjusted difference-in-differences estimate | −3.88 (−5.82 to −1.95) | −2.29 (−4.24 to −0.35) | ||||
| Absolute adjusted difference-in-differences estimate | −2.20 (−3.89 to −0.51) | −0.56 (−2.71 to 1.58) | ||||
| Relative adjusted difference-in-differences estimate (%) a | −3.07 (−5.43 to −0.72) | −0.79 (−3.78 to 2.21) | ||||
Incidence rates of kidney failure are per quarter (3 mo) per million population. The transitional period is defined as the first year postexpansion for expansion states, and as 2014 for nonexpansion states. The 2 and 3 year postexpansion period is defined as 2015–2016 for nonexpansion states, and the 4 and 5 year postexpansion period is defined as 2017–2018 for nonexpansion states. Adjusted difference-in-differences model is adjusted for age, sex, and race distribution; poverty rate; unemployment rate; and high-school graduate–attainment rate; in addition to fixed effects for season, year quarter, and PUMA. Estimates and 95% CIs are derived from models weighted by PUMA cell population with Huber–White robust SEMs clustered at the state level.
Difference-in-differences estimate relative to pre-expansion incidence rate in PUMAs in Medicaid expansion states.
Table 3 presents exploratory analyses stratified by population- and area-level characteristics. Quarterly incidence rates varied widely by group; the incidence rate among the non-Hispanic Black population was 3.5 times higher than that of the non-Hispanic White population. Those aged 19–44 years and the non-Hispanic White population experienced the largest relative reductions in kidney failure incidence after Medicaid expansion, compared with nonexpansion states. Although most subgroups experienced an attenuation in the reduction in incidence in the later postexpansion period, the reduction in kidney failure incidence for the non-Hispanic White population was larger in the later postexpansion period than in the earlier postexpansion period (6.35% relative reduction in the early postexpansion period; 9.37% relative reduction in the later postexpansion period), relative to nonexpansion states.
Table 3.
Changes in quarterly kidney failure incidence among nonelderly adults following the ACA Medicaid expansion, stratified analyses
| Characteristic | Mean Adjusted Incidence Rate | Absolute Adjusted Difference-in-Differences Estimate (95% CI) | Relative Adjusted Difference-in-Differences Estimate, % (95% CI) a | ||
|---|---|---|---|---|---|
| 2 and 3 Years Postexpansion | 4 and 5 Years Postexpansion | 2 and 3 Years Postexpansion | 4 and 5 Years Postexpansion | ||
| Age group | |||||
| 19–44 years | 31.56 | −1.44 (−2.61 to −0.27) | −0.51 (−1.92 to 0.91) | −4.95 (−8.97 to −0.94) | −1.73 (−6.60 to 3.13) |
| 45–64 years | 137.83 | −3.51 (−6.58 to −0.45) | −0.85 (−4.64 to 2.94) | −2.76 (−5.17 to −0.35) | −0.67 (−3.64 to 2.30) |
| Sex | |||||
| Male | 92.48 | −2.67 (−4.83 to −0.52) | −1.04 (−3.74 to 1.67) | −3.09 (−5.58 to −0.61) | −1.20 (−4.32 to 1.92) |
| Female | 61.95 | −1.75 (−3.62 to 0.12) | −0.12 (−2.68 to 2.44) | −3.07 (−6.35 to 0.22) | −0.21 (−4.70 to 4.28) |
| Race/Ethnicity | |||||
| Non-Hispanic White | 55.54 | −3.31 (−6.01 to −0.61) | −4.88 (−9.70 to -0.07) | −6.35 (−11.54 to −1.17) | −9.37 (−18.60 to −0.13) |
| Non-Hispanic Black | 193.24 | −2.43 (−9.15 to 4.30) | −1.13 (−8.75 to 6.49) | −1.25 (−4.71 to 2.21) | −0.58 (−4.50 to 3.34) |
| Hispanic | 79.59 | −2.66 (−6.34 to 1.03) | 5.66 (2.39 to 8.92) | −3.50 (−8.36 to 1.36) | 7.46 (3.15 to 11.77) |
| Area-level poverty rate b | |||||
| Below median (14.1%) | 57.46 | −2.10 (−4.19 to −0.01) | −0.80 (−2.88 to 1.29) | −3.84 (−7.66 to −0.02) | −1.46 (−5.26 to 2.35) |
| At or above median | 96.78 | −1.80 (−3.82 to 0.21) | 0.30 (−2.81 to 3.41) | −1.98 (−4.20 to 0.23) | 0.33 (−3.10 to 3.75) |
| Area-level uninsurance rate b | |||||
| Below median (19.6%) | 57.88 | −1.40 (−3.18 to 0.37) | 0.07 (−1.93 to 2.07) | −2.44 (−5.53 to 0.65) | 0.13 (−3.36 to 3.61) |
| At or above median | 96.39 | −1.76 (−4.27 to 0.74) | 1.05 (−2.09 to 4.19) | −1.88 (−4.55 to 0.79) | 1.12 (−2.22 to 4.46) |
| Area-level metropolitan status c | |||||
| Urban | 76.54 | −2.38 (−4.09 to −0.67) | −0.51 (−2.84 to 1.81) | −3.28 (−5.63 to −0.92) | −0.71 (−3.91 to 2.49) |
| Rural | 80.88 | −0.51 (−3.46 to 2.44) | 0.46 (−3.14 to 4.05) | −0.78 (−5.33 to 3.76) | 0.70 (−4.84 to 6.24) |
Incidence rates are per quarter (3 mo) per million population. Models are adjusted for age, sex, and race distribution; poverty rate; unemployment rate; and high-school graduate–attainment rate; in addition to fixed effects for season, year quarter, and PUMA. Stratified analyses for age group, sex, and race/ethnicity do not adjust for the stratified covariate. Estimates and 95% CIs are derived from models weighted by PUMA cell population with Huber–White robust SEMs clustered at the state level.
Difference-in-differences estimate relative to pre-expansion incidence rate in PUMAs in Medicaid expansion states.
Stratification by median PUMA-level poverty and uninsurance rates pre-expansion (2012 and 2013).
Urban-designated PUMAs those with >50% of their 2010 population residing in metropolitan areas.
Uninsurance Rates
Uninsurance rates fell in both expansion and nonexpansion states beginning in 2014, with larger declines in states that expanded their Medicaid programs (Supplemental Figure 3). Before the ACA’s Medicaid expansions, 18.5% of the nonelderly adult population in expansion states lacked health-insurance coverage (Table 4), which fell to 9.9% in the early postexpansion period and 9.4% in the later postexpansion period. The concurrent changes in nonexpansion states were from 24.5% uninsured at baseline, to 17.9% uninsured in the early postexpansion period, and 18.1% in the later postexpansion period. After adjustment for person-level covariates, people living in Medicaid expansion states experienced an additional 2.29 percentage point reduction (95% CI, −2.44 to −2.14) in uninsurance relative to those in nonexpansion states in the early expansion period, and a 2.81 percentage point reduction (95% CI, −2.95 to −2.66) in the later expansion period (Table 4). These observed effects represent 12.39% (95% CI, −13.19% to −11.59%) and 15.20% (95% CI, −15.99% to −14.40%) relative reductions in uninsurance, respectively, compared with preperiod uninsurance rates in Medicaid expansion states. In exploratory analyses stratified by person-level characteristics, baseline uninsurance rates and difference-in-differences estimates were larger for some subgroups, including racial and ethnic minorities and people living in PUMAs with baseline poverty and uninsurance rates above the median (Supplemental Table 3).
Table 4.
Changes in uninsurance rates in expansion and nonexpansion states following the ACA Medicaid expansion
| Medicaid Expansion Status | Baseline | Transitional Period | 2 and 3 Years Postexpansion | 4 and 5 Years Postexpansion | Change after Expansion Baseline to 2 and 3 Years Postexpansion (95% CI) | Change after Expansion Baseline to 4 and 5 Years Postexpansion (95% CI) |
|---|---|---|---|---|---|---|
| Expansion states | 18.48 | 13.44 | 9.92 | 9.44 | −8.55 (−8.65 to −8.46) | −9.03 (−9.13 to −8.94) |
| Nonexpansion states | 24.51 | 20.98 | 17.86 | 18.05 | −6.65 (−6.80 to −6.50) | −6.46 (−6.59 to −6.32) |
| Unadjusted difference-in-differences estimate | −1.90 (−2.09 to −1.71) | −2.57 (−2.74 to -2.41) | ||||
| Absolute adjusted difference-in-differences estimate | −2.29 (−2.44 to −2.14) | −2.81 (−2.95 to −2.66) | ||||
| Relative adjusted difference-in-differences estimate (%) a | −12.39 (−13.19 to −11.59) | −15.20 (−15.99 to −14.40) | ||||
The transitional period is defined as the first year postexpansion for expansion states, and as 2014 for nonexpansion states. The 2 and 3 year postexpansion period is defined as 2015–2016 for nonexpansion states, and the 4 and 5 year postexpansion period is defined as 2017–2018 for nonexpansion states. Adjusted difference-in-difference model is adjusted for age, sex, and race/ethnicity; having household income below the federal poverty level; unemployment status; and high-school graduate–attainment status; in addition to fixed effects for year and state. Estimates and 95% CIs are derived from models with replicate survey weights and Huber–White robust SEMs clustered at the state level.
Difference-in-differences estimate relative to pre-expansion uninsurance rate in Medicaid expansion states.
Sensitivity Analyses
Pre-2014 trends in kidney failure incidence did not differ significantly for expansion and nonexpansion PUMAs (Supplemental Tables 4 and 5). Sensitivity analyses that restricted to incident patients initiating maintenance dialysis or to incidence due to specific causes of kidney failure yielded estimates broadly consistent with the main analysis (Supplemental Table 6), as did analyses that used a negative binomial model, excluded early expansion states, excluded demographic and time-varying PUMA-level covariates, and used states as the geographic unit of analysis (Supplemental Table 7). The sensitivity analysis that modeled the entire postexpansion period together, rather than allowing for a transitional year, attenuated the decline in incidence rates in expansion relative to nonexpansion states, and the sensitivity analysis that modeled each year postexpansion separately observed the largest reduction in the second year postexpansion and gradual attenuation in subsequent years (Supplemental Table 8).
Discussion
In this national study of the entire nonelderly adult population of the United States, the ACA Medicaid expansion was associated with an initial 3.1% relative reduction in the incidence of kidney failure in the early postexpansion period, but this reduction did not persist in the later postexpansion period. The decline in incidence in expansion states relative to nonexpansion states was observed beginning in the second year of expansion and, in the subset of states that expanded in 2014 and 2015, was attenuated in the later postexpansion period, 4 and 5 years after expansion occurred. Our data did not allow us to restrict our analyses to individuals newly eligible for Medicaid or to individuals with CKD; therefore, our study design assessed the effect of expanded health insurance for low-income individuals on a rare condition among the entire nonelderly adult US population.
The progression of CKD is highly variable, and progression from stage 3 CKD to kidney failure can take a decade or longer.38–40 Although our data did not include information on the use of medications and management of chronic conditions, the timing of the declines in incidence aligns with randomized controlled trials that have reported renoprotective benefits of some medication therapies within 1 to 2 years after treatment initiation.12–14,41–44 The attenuation in the observed reduction in the later years postexpansion coincided with erosions in insurance-coverage gains in 2017 and 2018 due to changing federal and state policies, including weakening the health insurance marketplaces and implementation of Medicaid work and other personal-responsibility requirements in certain states.45–48 Additionally, evidence from a randomized policy experiment suggests the mortality declines associated with insurance coverage are largest in the period immediately after people newly gain health insurance, and decay over time with continued maintenance of coverage.49 These dynamics may be similar for kidney failure and explain why the largest reductions in incidence were observed in the early postexpansion period.
This study extends prior evidence demonstrating positive health effects associated with the ACA Medicaid expansions, including improved self-reported health, lower all-cause and cardiovascular death rates for the general population, and lower mortality among incident patients with kidney failure initiating dialysis.22,23,50–52 Notably, several studies have found Medicaid expansion is associated with increased access to diabetes and cardiovascular medications and, among patients in community health centers, improvements in BP control, all of which influence the progression of CKD to kidney failure.26,53–56 Medicaid expansion has been demonstrated to improve state economic conditions and individual household finances, providing another pathway through which population health may improve.57–61 Although self-reported rates of CKD did not increase after Medicaid expansion,62 Medicaid-covered preemptive listing and kidney transplantation increased in expansion states after the ACA.36,63 The findings also extend research from before the ACA that identified an association between more generous Medicaid income-eligibility requirements and lower incidence rates of kidney failure and higher levels of predialysis nephrology care, wait-listing, and transplantation.64
Our findings contrast with the Oregon Health Study, which found no evidence of improved control of diabetes or hypertension among the low-income adults randomly selected as eligible to apply for Medicaid coverage in the state.65 This study’s larger and more representative study population and longer follow-up period may increase its ability to identify small, but meaningful, changes in clinical outcomes, particularly a rare outcome like the onset of kidney failure.
In addition to state Medicaid expansions for nonelderly adults with incomes up to 138% of the federal poverty level, the ACA provided subsidies for individuals in all states with incomes 100%–400% of the federal poverty level to purchase individual marketplace policies. Together, these initiatives reduced uninsurance rates for nonelderly adults, particularly for individuals residing in states that expanded Medicaid, with the greatest absolute gains in insurance coverage observed for racial and ethnic minorities and younger age groups, reducing disparities in uninsurance rates.28–30,66,67 However, consistent with other studies, coverage gains largely stagnated beginning in 2017, and uninsurance rates have subsequently increased for some subgroups.29,46–48,67
These findings have important policy implications. Medicaid expansion may be an important mechanism to reduce incidence of kidney failure, particularly in light of accumulating evidence of kidney-protective benefits of sodium-glucose cotransporter 2 inhibitors, a newer and costly class of medications.42 Our study also suggests loss of Medicaid coverage through repealing the ACA’s Medicaid expansions has the potential to increase the progression to kidney failure among nonelderly adults. Additionally, these findings demonstrate the potential for spending on expansions of Medicaid coverage to reduce costs otherwise borne by the Medicare program, the primary payer for the patients with kidney failure in the United States. Finally, our results are relevant given anticipated severe losses of employer-sponsored health insurance during the coronavirus disease 2019 pandemic and economic crisis, which could threaten access to care, particularly for low-income persons who are ineligible for Medicaid.
This study has several limitations. First, incident patients are only included in the Renal Management Information System if they initiate maintenance dialysis or receive a preemptive kidney transplant, so individuals receiving compassionate or emergency dialysis are not captured in the data. However, more patients seeking treatment or initiating maintenance dialysis as opposed to emergency dialysis in Medicaid expansion states, relative to nonexpansion states, would bias our findings toward the null.68 Second, we were unable to account for the competing risk of death, and death is more common among individuals with CKD than progression to kidney failure.39 Prior studies have found Medicaid expansions are associated with reduced mortality.50–52,69,70 Improved survival of patients with CKD in Medicaid expansion states would bias our findings to the null if more patients with advanced CKD survived and progressed to kidney failure in Medicaid expansion states relative to nonexpansion states. Third, the populations in Medicaid expansion and nonexpansion states could have changed differentially over the study period, although we included a number of time-varying demographic and socioeconomic characteristics in our analyses, and adjustment for these characteristics did not change the main findings. Notably, late-expansion states contributed little to no person-time to the later postexpansion period, and these states (particularly Louisiana and Pennsylvania) are home to an outsized share of the non-Hispanic Black population that resides in Medicaid expansion states. Despite adjusting for race/ethnicity, secular declines in kidney failure incidence for Black Americans, and the different racial/ethnic composition of early- and late-expanding states, may have influenced the attenuation in the longer-term effect of expansion on incidence. Fourth, Medicaid expansion may affect the timing of dialysis initiation or preemptive transplantation for patients with CKD, which could change the composition of the incident population over the course of the study period. However, preemptive transplantation was uncommon in both expansion and nonexpansion states, and changes in the eGFR among incident patients were minimal during the study period and were similar in expansion and nonexpansion states. This suggests the observed reductions in incidence are unlikely to be explained by changes in dialysis initiation to be earlier or later in the course of disease. Fifth, unmeasured factors, such as changes in air pollution in expansion and nonexpansion states, may have influenced the observed association; although the difference-in-differences framework, with geographic and time fixed effects, controls for these kinds of underlying area-level factors. Only time-varying confounders that changed differentially between expansion and nonexpansion states would bias our estimates.
In conclusion, although this study suggests nonelderly adult residents of states that expanded Medicaid under the ACA experienced an initial reduction in the incidence of kidney failure relative to those in nonexpansion states in the early postexpansion period, this effect did not persist in the later postexpansion period for the subset of states that expanded in 2014 and 2015. This mixed pattern of findings suggests expansions of insurance coverage may potentially prevent or delay new cases of kidney failure, but long-term evaluation—particularly for high-risk cohorts—is needed.
Disclosures
R. Mehrotra reports receiving personal honoraria from Baxter Healthcare for serving as an ad hoc consultant outside of the submitted work. R. Mehrotra also reports serving as chair for the Nephrology Longitudinal Assessment Approval Committee of the American Board of Internal Medicine, the editor-in-chief of CJASN, part of the editorial board for Journal of Renal Nutrition and Peritoneal Dialysis International, and as member of the board of trustees of Northwest Kidney Centers. B. Sommers reports having consultancy agreements with Illinois Department of Healthcare and Family Services; and receiving honoraria from JAMA, Urban Institute, and Washington University. All remaining authors have nothing to disclose.
Funding
This work was supported by National Institute of Diabetes and Digestive and Kidney Diseases grant 5R01DK113298.
Supplementary Material
Acknowledgments
This work was conducted under a data-use agreement with the CMS.
The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the Department of Veterans Affairs or the US Government.
B.D. Sommers is currently on leave from Harvard and serving in the US Department of Health and Human Services. However, this article was conceived and drafted while B.D. Sommers was employed at the Harvard School of Public Health, and the findings and views in this article do not reflect the official views or policy of the Department of Health and Human Services.
The sponsor had no role in the design and conduct of the study; in collection, management, analysis, or interpretation of the data; in preparation, review, or approval of the manuscript; or in the decision to submit for publication.
All authors contributed to the conception and design of the study; to the acquisition, analysis, and interpretation of data; in drafting of the manuscript; and in critical revision of the manuscript for important intellectual content. R. Thorsness, S. Swaminathan, B.D. Sommers, and A.N. Trivedi were responsible for statistical analysis; S. Swaminathan and A.N. Trivedi were responsible for obtaining funding; and A.N. Trivedi provided supervision.
Footnotes
Published online ahead of print. Publication date available at www.jasn.org.
Supplemental Material
This article contains the following supplemental material online at http://cjasn.asnjournals.org/lookup/suppl/doi:10.1681/ASN.2020101511/-/DCSupplemental.
Supplemental Appendix 1. Detailed description of kidney failure incidence rate calculations.
Supplemental Appendix 2. Regression equations for analyses: Primary outcome (kidney failure incidence).
Supplemental Appendix 3. Regression equations for analyses: Secondary outcome (uninsurance).
Supplemental Figure 1. Study population flowchart– incident kidney failure cases.
Supplemental Figure 2. Quarterly kidney failure incidence per million population, by state Medicaid expansion status without seasonality adjustment.
Supplemental Figure 3. Annual uninsurance rate, by state Medicaid expansion status.
Supplemental Table 1. Definition of expansion and non-expansion states and post period.
Supplemental Table 2. Sample size for kidney failure incidence rate calculations by years post-expansion and racial/ethnic group.
Supplemental Table 3. Changes in uninsurance among nonelderly adults following the ACA Medicaid expansion, stratified analyses.
Supplemental Table 4. Parallel trends assumption test– time trend.
Supplemental Table 5. Parallel trends assumption test– event study falsification.
Supplemental Table 6. Sensitivity analyses of changes in kidney failure incidence among nonelderly adults following the ACA Medicaid expansion– specific incident patient populations.
Supplemental Table 7. Sensitivity analyses of changes in kidney failure incidence among nonelderly adults following the ACA Medicaid expansion– alternative model specifications.
Supplemental Table 8. Sensitivity analyses of changes in kidney failure incidence among nonelderly adults following the ACA Medicaid expansion– alternative post-period model specifications.
Supplemental Appendix 4. Online-only supplement references.
References
- 1. United States Renal Data System: 2018 USRDS annual data report: Epidemiology of kidney disease in the United States. National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases, 2018. Available at: https://www.usrds.org/2018/view/Default.aspx [Google Scholar]
- 2. Brancati FL, Whittle JC, Whelton PK, Seidler AJ, Klag MJ: The excess incidence of diabetic end-stage renal disease among blacks. A population-based study of potential explanatory factors. JAMA 268: 3079–3084, 1992. 10.1001/jama.1992.03490210061036 [PubMed] [Google Scholar]
- 3. Klag MJ, Whelton PK, Randall BL, Neaton JD, Brancati FL, Stamler J: End-stage renal disease in African-American and white men. 16-year MRFIT findings. JAMA 277: 1293–1298, 1997. 10.1001/jama.1997.03540400043029 [PubMed] [Google Scholar]
- 4. Volkova N, McClellan W, Klein M, Flanders D, Kleinbaum D, Soucie JM, et al.: Neighborhood poverty and racial differences in ESRD incidence. J Am Soc Nephrol 19: 356–364, 2008. 10.1681/ASN.2006080934 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Hall YN, Choi AI, Chertow GM, Bindman AB: Chronic kidney disease in the urban poor. Clin J Am Soc Nephrol 5: 828–835, 2010. 10.2215/CJN.09011209 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Crews DC, Gutiérrez OM, Fedewa SA, Luthi JC, Shoham D, Judd SE, et al.: Low income, community poverty and risk of end stage renal disease. BMC Nephrol 15: 192, 2014. 10.1186/1471-2369-15-192 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. UK Prospective Diabetes Study (UKPDS) Group: Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33) [published correction appears in Lancet 354: 602, 1999]. Lancet 352: 837–853, 1998. 10.1016/S0140-6736(98)07019-6 [PubMed] [Google Scholar]
- 8. Klag MJ, Whelton PK, Randall BL, Neaton JD, Brancati FL, Ford CE, et al.: Blood pressure and end-stage renal disease in men. N Engl J Med 334: 13–18, 1996. 10.1056/NEJM199601043340103 [DOI] [PubMed] [Google Scholar]
- 9. Taal MW, Brenner BM: Renoprotective benefits of RAS inhibition: From ACEI to angiotensin II antagonists. Kidney Int 57: 1803–1817, 2000. 10.1046/j.1523-1755.2000.00031.x [DOI] [PubMed] [Google Scholar]
- 10. Lewis EJ, Hunsicker LG, Bain RP, Rohde RD; The Collaborative Study Group: The effect of angiotensin-converting-enzyme inhibition on diabetic nephropathy [published correction appears in N Engl J Med 330: 152, 1993]. N Engl J Med 329: 1456–1462, 1993. 10.1056/NEJM199311113292004 [DOI] [PubMed] [Google Scholar]
- 11. Parving HH, Lehnert H, Bröchner-Mortensen J, Gomis R, Andersen S, Arner P; Irbesartan in Patients with Type 2 Diabetes and Microalbuminuria Study Group: The effect of irbesartan on the development of diabetic nephropathy in patients with type 2 diabetes. N Engl J Med 345: 870–878, 2001. 10.1056/NEJMoa011489 [DOI] [PubMed] [Google Scholar]
- 12. Jafar TH, Schmid CH, Landa M, Giatras I, Toto R, Remuzzi G, et al.: Angiotensin-converting enzyme inhibitors and progression of nondiabetic renal disease. A meta-analysis of patient-level data. Ann Intern Med 135: 73–87, 2001. 10.7326/0003-4819-135-2-200107170-00007 [DOI] [PubMed] [Google Scholar]
- 13. Lewis EJ, Hunsicker LG, Clarke WR, Berl T, Pohl MA, Lewis JB, et al.; Collaborative Study Group: Renoprotective effect of the angiotensin-receptor antagonist irbesartan in patients with nephropathy due to type 2 diabetes. N Engl J Med 345: 851–860, 2001. 10.1056/NEJMoa011303 [DOI] [PubMed] [Google Scholar]
- 14. Brenner BM, Cooper ME, de Zeeuw D, Keane WF, Mitch WE, Parving HH, et al.; RENAAL Study Investigators: Effects of losartan on renal and cardiovascular outcomes in patients with type 2 diabetes and nephropathy. N Engl J Med 345: 861–869, 2001. 10.1056/NEJMoa011161 [DOI] [PubMed] [Google Scholar]
- 15. Sarnak MJ, Greene T, Wang X, Beck G, Kusek JW, Collins AJ, et al.: The effect of a lower target blood pressure on the progression of kidney disease: Long-term follow-up of the modification of diet in renal disease study. Ann Intern Med 142: 342–351, 2005. 10.7326/0003-4819-142-5-200503010-00009 [DOI] [PubMed] [Google Scholar]
- 16. McWilliams JM: Health consequences of uninsurance among adults in the United States: Recent evidence and implications. Milbank Q 87: 443–494, 2009. 10.1111/j.1468-0009.2009.00564.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Ayanian JZ, Weissman JS, Schneider EC, Ginsburg JA, Zaslavsky AM: Unmet health needs of uninsured adults in the United States. JAMA 284: 2061–2069, 2000. 10.1001/jama.284.16.2061 [DOI] [PubMed] [Google Scholar]
- 18. Institute of Medicine (US) Committee on the Consequences of Uninsurance: Care Without Coverage: Too Little, Too Late. Washington, DC, National Academies Press, 2002. [PubMed] [Google Scholar]
- 19. Wilper AP, Woolhandler S, Lasser KE, McCormick D, Bor DH, Himmelstein DU: Hypertension, diabetes, and elevated cholesterol among insured and uninsured U.S. adults. Health Aff (Millwood) 28: w1151–w1159, 2009. 10.1377/hlthaff.28.6.w1151 [DOI] [PubMed] [Google Scholar]
- 20. Tarver-Carr ME, Powe NR, Eberhardt MS, LaVeist TA, Kington RS, Coresh J, et al.: Excess risk of chronic kidney disease among African-American versus white subjects in the United States: A population-based study of potential explanatory factors. J Am Soc Nephrol 13: 2363–2370, 2002. 10.1097/01.ASN.0000026493.18542.6A [DOI] [PubMed] [Google Scholar]
- 21. Gerber C, Cai X, Lee J, Craven T, Scialla J, Souma N, et al.: Incidence and progression of chronic kidney disease in black and white individuals with type 2 diabetes. Clin J Am Soc Nephrol 13: 884–892, 2018. 10.2215/CJN.11871017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Guth M, Garfield R, Rudowitz R: The effects of Medicaid expansion under the ACA: Updated findings from a literature review. San Francisco, CA, Kaiser Family Foundation, 2020. Available at: https://www.kff.org/report-section/the-effects-of-medicaid-expansion-under-the-aca-updated-findings-from-a-literature-review-report/ [Google Scholar]
- 23. Swaminathan S, Sommers BD, Thorsness R, Mehrotra R, Lee Y, Trivedi AN: Association of Medicaid expansion with 1-year mortality among patients with end-stage renal disease. JAMA 320: 2242–2250, 2018. 10.1001/jama.2018.16504 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Sommers BD, Blendon RJ, Orav EJ, Epstein AM: Changes in utilization and health among low-income adults after Medicaid expansion or expanded private insurance. JAMA Intern Med 176: 1501–1509, 2016. 10.1001/jamainternmed.2016.4419 [DOI] [PubMed] [Google Scholar]
- 25. Allen H, Sommers BD: Medicaid expansion and health: Assessing the evidence after 5 years. JAMA 322: 1253–1254, 2019. 10.1001/jama.2019.12345 [DOI] [PubMed] [Google Scholar]
- 26. Myerson R, Lu T, Tonnu-Mihara I, Huang ES: Medicaid eligibility expansions may address gaps in access to diabetes medications. Health Aff (Millwood) 37: 1200–1207, 2018. 10.1377/hlthaff.2018.0154 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Kaiser Family Foundation: Status of state action on the Medicaid expansion decision. San Francisco, CA, Kaiser Family Foundation, 2020. Available at: https://www.kff.org/health-reform/state-indicator/state-activity-around-expanding-medicaid-under-the-affordable-care-act/. Accessed August 24, 2020 [Google Scholar]
- 28. Wehby GL, Lyu W: The impact of the ACA Medicaid expansions on health insurance coverage through 2015 and coverage disparities by age, race/ethnicity, and gender. Health Serv Res 53: 1248–1271, 2018. 10.1111/1475-6773.12711 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Long SK, Bart L, Karpman M, Shartzer A, Zuckerman S: Sustained gains in coverage, access, and affordability under the ACA: A 2017 update. Health Aff (Millwood) 36: 1656–1662, 2017. 10.1377/hlthaff.2017.0798 [DOI] [PubMed] [Google Scholar]
- 30. Chaudry A, Jackson A, Glied SA: Did the affordable care act reduce racial and ethnic disparities in health insurance coverage? New York, NY, The Commonwealth Fund, 2019. 10.26099/d8hs-cm53 [Google Scholar]
- 31. United States Renal Data System: 2018 researcher’s guide to the USRDS database. National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases, 2018: 76. Available at: https://www.usrds.org/2018/rg/2018_USRDS_Researcher_Guide.pdf [Google Scholar]
- 32. Centers for Medicare & Medicaid Services: End stage renal disease medical evidence report Medicare entitlement and/or patient registration. Woodlawn, MD, Department of Health and Human Services, Centers for Medicare & Medicaid Services, 2006. Available at: https://www.cms.gov/Medicare/CMS-Forms/CMS-Forms/downloads/CMS2728.pdf. Accessed June 14, 2019 [Google Scholar]
- 33. Ruggles S, Flood S, Goeken R, Grover J, Meyer E, Pacas J, et al. IPUMS USA: Version 10.0. Minneapolis, MN, IPUMS, 2020. 10.18128/D010.V10.0 [DOI] [Google Scholar]
- 34. Bertrand M, Duflo E, Mullainathan S: How much should we trust differences-in-differences estimates? Q J Econ 119: 249–275, 2004. 10.1162/003355304772839588 [Google Scholar]
- 35. Miller S, Wherry LR: Health and access to care during the first 2 years of the ACA Medicaid expansions. N Engl J Med 376: 947–956, 2017. 10.1056/NEJMsa1612890 [DOI] [PubMed] [Google Scholar]
- 36. Harhay MN, McKenna RM, Harhay MO: Association between Medicaid expansion under the Affordable Care Act and Medicaid-covered pre-emptive kidney transplantation. J Gen Intern Med 34: 2322–2325, 2019. 10.1007/s11606-019-05279-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Obi Y, Kalantar-Zadeh K, Streja E, Rhee CM, Reddy UG, Soohoo M, et al.: Seasonal variations in transition, mortality and kidney transplantation among patients with end-stage renal disease in the USA. Nephrol Dial Transplant 32[Suppl 2]: ii99–ii105, 2017. 10.1093/ndt/gfw379 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Li L, Astor BC, Lewis J, Hu B, Appel LJ, Lipkowitz MS, et al.: Longitudinal progression trajectory of GFR among patients with CKD. Am J Kidney Dis 59: 504–512, 2012. 10.1053/j.ajkd.2011.12.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Levey AS, Stevens LA, Coresh J: Conceptual model of CKD: Applications and implications. Am J Kidney Dis 53[Suppl 3]: S4–S16, 2009. 10.1053/j.ajkd.2008.07.048 [DOI] [PubMed] [Google Scholar]
- 40. Levin A, Djurdjev O, Beaulieu M, Er L: Variability and risk factors for kidney disease progression and death following attainment of stage 4 CKD in a referred cohort. Am J Kidney Dis 52: 661–671, 2008. 10.1053/j.ajkd.2008.06.023 [DOI] [PubMed] [Google Scholar]
- 41. Hou FF, Zhang X, Zhang GH, Xie D, Chen PY, Zhang WR, et al.: Efficacy and safety of benazepril for advanced chronic renal insufficiency. N Engl J Med 354: 131–140, 2006. 10.1056/NEJMoa053107 [DOI] [PubMed] [Google Scholar]
- 42. Perkovic V, Jardine MJ, Neal B, Bompoint S, Heerspink HJ, Charytan DM, et al.; CREDENCE Trial Investigators: Canagliflozin and renal outcomes in type 2 diabetes and nephropathy. N Engl J Med 380: 2295–2306, 2019. 10.1056/NEJMoa1811744 [DOI] [PubMed] [Google Scholar]
- 43. Maschio G, Alberti D, Janin G, Locatelli F, Mann JF, Motolese M, et al.: Effect of the angiotensin-converting-enzyme inhibitor benazepril on the progression of chronic renal insufficiency. The angiotensin-converting-enzyme inhibition in progressive renal insufficiency study group. N Engl J Med 334: 939–945, 1996. 10.1056/NEJM199604113341502 [DOI] [PubMed] [Google Scholar]
- 44. Bakris GL, Agarwal R, Anker SD, Pitt B, Ruilope LM, Rossing P, et al.; FIDELIO-DKD Investigators: Effect of finerenone on chronic kidney disease outcomes in type 2 diabetes. N Engl J Med 383: 2219–2229, 2020. 10.1056/NEJMoa2025845 [DOI] [PubMed] [Google Scholar]
- 45. Thompson FJ, Gusmano MK, Shinohara S: Trump and the Affordable Care Act: Congressional repeal efforts, executive federalism, and program durability. Publius 48: 396–424, 2018. 10.1093/publius/pjy007 [Google Scholar]
- 46. Chen L, Sommers BD: Work requirements and medicaid disenrollment in Arkansas, Kentucky, Louisiana, and Texas, 2018. Am J Public Health 110: 1208–1210, 2020. 10.2105/AJPH.2020.305697 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Askelson NM, Brady P, Wright B, Bentler S, Momany ET, Damiano P: Purged from the rolls: A study of medicaid disenrollment in Iowa. Health Equity 3: 637–643, 2019. 10.1089/heq.2019.0093 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Bernstein H, Gonzalez D, Karpman M, Zuckerman S: Amid confusion over the public charge rule, immigrant families continued avoiding public benefits in 2019. Washington, DC, Urban Institute, 2020. Available at: https://www.urban.org/sites/default/files/publication/102221/amid-confusion-over-the-public-charge-rule-immigrant-families-continued-avoiding-public-benefits-in-2019_2.pdf [Google Scholar]
- 49. Goldin J, Lurie IZ, McCubbin J: Health insurance and mortality: Experimental evidence from taxpayer outreach. Q J Econ 136: 1–49, 2021. doi:10.1093/qje/qjaa029 [Google Scholar]
- 50. Khatana SAM, Bhatla A, Nathan AS, Giri J, Shen C, Kazi DS, et al.: Association of Medicaid expansion with cardiovascular mortality. JAMA Cardiol 4: 671–679, 2019. 10.1001/jamacardio.2019.1651 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Borgschulte M, Vogler J: Did the ACA Medicaid expansion save lives? J Health Econ 72: 102333, 2020. 10.1016/j.jhealeco.2020.102333 [DOI] [PubMed] [Google Scholar]
- 52. Miller S, Altekruse S, Johnson N, Wherry LR: Medicaid and Mortality: New Evidence from Linked Survey and Administrative Data, Cambridge, MA, National Bureau of Economic Research, 2019, 10.3386/w26081 [Google Scholar]
- 53. Cher BAY, Morden NE, Meara E: Medicaid expansion and prescription trends: Opioids, addiction therapies, and other drugs. Med Care 57: 208–212, 2019. 10.1097/MLR.0000000000001054 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Kim NH, Look KA, Burns ME: Low-income childless adults’ access to antidiabetic drugs in Wisconsin Medicaid after coverage expansion. Health Aff (Millwood) 38: 1145–1152, 2019. 10.1377/hlthaff.2018.05198 [DOI] [PubMed] [Google Scholar]
- 55. Cole MB, Galárraga O, Wilson IB, Wright B, Trivedi AN: At federally funded health centers, Medicaid expansion was associated with improved quality of care. Health Aff (Millwood) 36: 40–48, 2017. 10.1377/hlthaff.2016.0804 [DOI] [PubMed] [Google Scholar]
- 56. Sumarsono A, Lalani H, Segar MW, Rao S, Vaduganathan M, Wadhera RK, et al.: Association of Medicaid expansion with rates of utilization of cardiovascular therapies among Medicaid beneficiaries between 2011 and 2018. Circ Cardiovasc Qual Outcomes 14: e007492, 2021. 10.1161/CIRCOUTCOMES.120.007492 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Zewde N, Eliason E, Allen H, Gross T: The effects of the ACA Medicaid expansion on nationwide home evictions and eviction-court initiations: United States, 2000–2016. Am J Public Health 109: 1379–1383, 2019. 10.2105/AJPH.2019.305230 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Caswell KJ, Waidmann TA: The Affordable Care Act Medicaid expansions and personal finance. Med Care Res Rev 76: 538–571, 2019. 10.1177/1077558717725164 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Ayanian JZ, Ehrlich GM, Grimes DR, Levy H: Economic effects of Medicaid expansion in Michigan. N Engl J Med 376: 407–410, 2017. 10.1056/NEJMp1613981 [DOI] [PubMed] [Google Scholar]
- 60. Vogler J: Access to healthcare and criminal behavior: Evidence from the ACA Medicaid expansions. J Policy Anal Manage 39: 1166–1213, 2020. 10.1002/pam.22239 [Google Scholar]
- 61. Bachrach D, Boozang P, Herring A, Glanz Reyneri D: States expanding medicaid see significant budget savings and revenue gains. Princeton, NJ, Robert Wood Johnson Foundation State Health Reform Assistance Network, 2016. Available at: https://www.rwjf.org/en/library/research/2015/04/states-expanding-medicaid-see-significant-budget-savings-and-rev.html [Google Scholar]
- 62. Tummalapalli SL, Leonard S, Estrella MM, Keyhani S: The effect of Medicaid expansion on self-reported kidney disease. Clin J Am Soc Nephrol 14: 1238–1240, 2019. 10.2215/CJN.02310219 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Harhay MN, McKenna RM, Boyle SM, Ranganna K, Mizrahi LL, Guy S, et al.: Association between Medicaid expansion under the affordable care act and preemptive listings for kidney transplantation. Clin J Am Soc Nephrol 13: 1069–1078, 2018. 10.2215/CJN.00100118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Kurella-Tamura M, Goldstein BA, Hall YN, Mitani AA, Winkelmayer WC: State medicaid coverage, ESRD incidence, and access to care. J Am Soc Nephrol 25: 1321–1329, 2014. 10.1681/ASN.2013060658 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Baicker K, Taubman SL, Allen HL, Bernstein M, Gruber JH, Newhouse JP, et al.; Oregon Health Study Group: The Oregon experiment--effects of Medicaid on clinical outcomes. N Engl J Med 368: 1713–1722, 2013. 10.1056/NEJMsa1212321 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Courtemanche C, Marton J, Ukert B, Yelowitz A, Zapata D, Fazlul I: The three-year impact of the Affordable Care Act on disparities in insurance coverage. Health Serv Res 54[Suppl 1]: 307–316, 2019. 10.1111/1475-6773.13077 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Buchmueller TC, Levy HG: The ACA’s impact on racial and ethnic disparities in health insurance coverage and access to care. Health Aff (Millwood) 39: 395–402, 2020. 10.1377/hlthaff.2019.01394 [DOI] [PubMed] [Google Scholar]
- 68. Cervantes L, Mundo W, Powe NR: The status of provision of standard outpatient dialysis for US undocumented immigrants with ESKD. Clin J Am Soc Nephrol 14: 1258–1260, 2019. 10.2215/CJN.03460319 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Sommers BD, Baicker K, Epstein AM: Mortality and access to care among adults after state Medicaid expansions. N Engl J Med 367: 1025–1034, 2012. 10.1056/NEJMsa1202099 [DOI] [PubMed] [Google Scholar]
- 70. Sommers BD, Gawande AA, Baicker K: Health insurance coverage and health - what the recent evidence tells us. N Engl J Med 377: 586–593, 2017. 10.1056/NEJMsb1706645 [DOI] [PubMed] [Google Scholar]
- 71. Levey AS, Stevens LA, Schmid CH, Zhang YL, Castro AF 3rd, Feldman HI, et al.; CKD-EPI (Chronic Kidney Disease Epidemiology Collaboration): A new equation to estimate glomerular filtration rate [published correction appears in Ann Intern Med 155: 408, 2011]. Ann Intern Med 150: 604–612, 2009. 10.7326/0003-4819-150-9-200905050-00006 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.