Significance Statement
The humoral response over time against severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) is poorly understood. The authors investigated the long-term kinetics of the antibody response to SARS-CoV-2 (specifically, IgG against nucleocapsid and spike antigens), in 83 patients on in-center hemodialysis who recovered from coronavirus disease 2019 (COVID-19). They found that 10% of patients had no initial seroconversion, which was associated with immunocompromised status; in patients with seroconversion, IgG antibodies decayed over time. Factors associated with this decline included older age, female sex, and nonsevere clinical presentation. About 25% of patients had negative IgG antinucleocapsid serology after 6 months, whereas most patients maintained antispike antibodies. By characterizing the evolution of the SARS-CoV-2 antibody response, these findings might help better define future therapeutic and preventive approaches against COVID-19 in patients on hemodialysis.
Keywords: hemodialysis, SARS-CoV-2, serology, SARS-CoV-2 antibody, COVID-19
Abstract
Background
The humoral response against severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) in the hemodialysis population, including its dynamics over time, remains poorly understood.
Methods
To analyze initial and long-term humoral responses against SARS-CoV-2 in a hemodialysis population, we retrospectively evaluated findings from SARS-CoV-2 IgG serologic assays targeting the nucleocapsid antigen or spike antigen up to 6 months of follow-up in patients on hemodialysis in the Paris, France, region who had recovered from coronavirus disease 2019 (COVID-19).
Results
Our analysis included 83 patients (median age 65 years); 59 (71%) were male and 28 (34%) had presented with severe COVID-19. We observed positive initial SARS-CoV-2 IgG antinucleocapsid serology in 74 patients (89%) at a median of 67 days postdiagnosis. By multivariable analysis, immunocompromised status was the only factor significantly associated with lack of an IgG antinucleocapsid antibody response. Follow-up data were available at 6 months postdiagnosis for 60 of 74 patients (81%) with positive initial antinucleocapsid serology, and 15 (25%) of them had negative antinucleocapsid serology at month 6. In total, 14 of 15 sera were tested for antispike antibodies, 3 of 14 (21%) of which were also negative. Overall, 97% of antinucleocapsid-antibody–positive specimens were also antispike-antibody positive. Female sex, age >70 years, and nonsevere clinical presentation were independently associated with faster IgG antinucleocapsid titer decay in multivariable analysis. After adjustment for sex and age >70 years, nonsevere clinical presentation was the only factor associated with faster decay of IgG antispike antibodies.
Conclusions
This study characterizes evolution of the SARS-CoV-2 antibody response in patients on hemodialysis and identifies factors that are associated with lack of seroconversion and with IgG titer decay.
Coronavirus disease 2019 (COVID-19), caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection, is associated with a severe risk of mortality in patients on hemodialysis.1,2 The humoral response against SARS-CoV-2 in the hemodialysis population, including its dynamics over time, remains poorly understood.3,4 Given the pandemic’s ongoing waves of new infections and the need for future vaccination strategies, the characterization of this response appears to be an important unmet need. In this study, we analyzed the initial and long-term humoral response against SARS-CoV-2 in a hemodialysis population.
Methods
In this multicenter study, the study population included 83 patients undergoing hemodialysis in the Paris, France, area who had recovered from COVID-19; 76 patients were previously described.2
Clinical data were retrospectively recorded. A severe form of COVID-19 was defined by the need for oxygen therapy. Immunocompromised status was characterized by one of the following factors: former organ transplant, HIV infection, recent (within <6 months) immunosuppressive therapy, or chemotherapy.
We collected 241 sequential serum samples, which were analyzed with the Abbot SARS-CoV-2 IgG Architect system (targeting the nucleocapsid antigen). Of the 83 participants, 25 had two serial measurements of IgG levels, and 52 had at least three serial measurements. We used the Ortho Clinical Diagnostics Vitros IgG assay (targeting the spike antigen) to analyze 113 samples.
Data collection was declared to the French Commission Nationale de l’Informatique et des Libertés, registration 2218583. This protocol was submitted to the approbation of Paris Centre Institutional Review Board.
Statistical Analyses
Categorical and continuous variables were expressed as count (percentage) and median (interquartile range, IQR), respectively. When appropriate, chi-squared or Fisher’s exact tests were used for categorical comparison, and t test or Mann–Whitney for continuous variables.
Variables associated with seroconversion were analyzed by logistic regression. All variables with a P value <0.2 in univariable analysis were included in the multivariable analysis. Stepwise backward selection on the basis of the Akaike information criterion was then used for the final multivariable model. In the subset of patients who experienced seroconversion, we modeled the SARS-CoV-2 antibody decay with random-intercept linear models to account for intrasubject correlations. Antibody titers were log10 transformed to estimate the evolution of geometric mean titers after their peaks were reached, and factors associated with their decrease were identified by testing the interaction between time and patients’ characteristics.
Results were analyzed with GraphPad Prism software version 9.0.0 and R software version 4.0.3.
Results
We retrospectively studied SARS-CoV-2 serologic assay findings in 83 patients who received in-center hemodialysis at five different centers in the Paris area, and who were still alive after their diagnosis with COVID-19 in March 2020. Baseline patient characteristics are described in Supplemental Tables 1 and 2.
The first serologic evaluation was performed a median of 67 (IQR 39) days after COVID-19 diagnosis. Among the 83 patients, 74 (89%) had positive SARS-CoV-2 IgG antinucleocapsid or antispike serology (Figure 1A). Nine patients had negative initial IgG serology on the basis of the antinucleocapsid assay at a median of 51 (IQR 32.5) days postdiagnosis; sera from six of these nine patients were also tested for antispike antibodies, which were similarly negative. Detailed characteristics of these patients are provided in Supplemental Table 3.
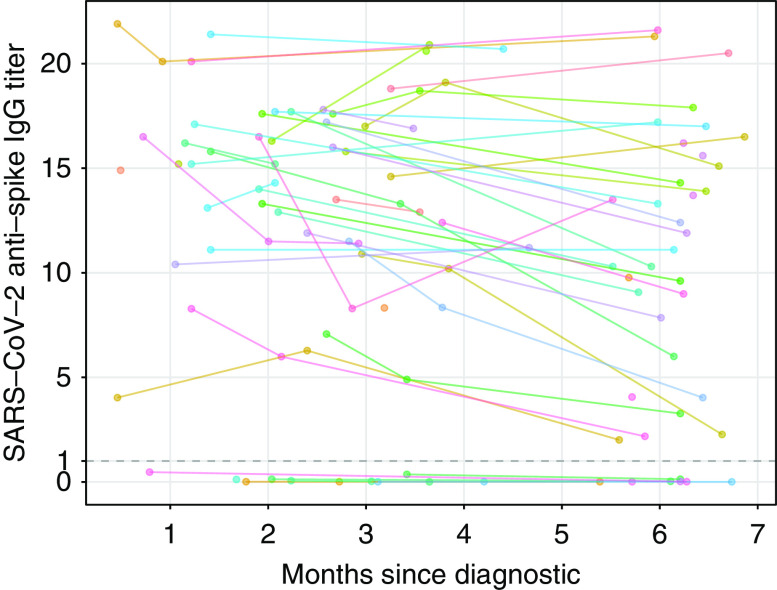
Figure 1.
Evolution of SARS-CoV-2 IgG antinucleocapsid (NC) antibody titer until 6 months after diagnosis. (A) Evolution of SARS-CoV-2 IgG titer for each patient over time (spaghetti plot). Cutoff for negative serology was defined according to the manufacturer (Index sample/control <1.4: dashed line). The zone between the dashed lines (1.4 and 0.5) represents the equivocal zone. The y-axis is plotted in logarithmic scale. (B) Predicted SARS-CoV-2 antibody decay according to age, sex, and disease severity (multivariable model). Cutoff for negative serology: index sample/control <1.4; dashed line. The zone between the dashed lines (1.4 and 0.5) represents the equivocal zone.
We found no association between the absence of IgG response and initial disease severity, but glomerular diseases and immunosuppression were more frequent among patients who did not exhibit a SARS-CoV-2 antibody response (Supplemental Table 2). We observed similar results after excluding patients without PCR-confirmed diagnosis (Supplemental Table 4).
By multivariable analysis, an immunocompromised status was the only factor significantly associated with the absence of IgG antinucleocapsid antibody response (odds ratio, 13.8; 95% confidence interval [95% CI], 2.76 to 69.13; P=0.001) (Supplemental Table 5).
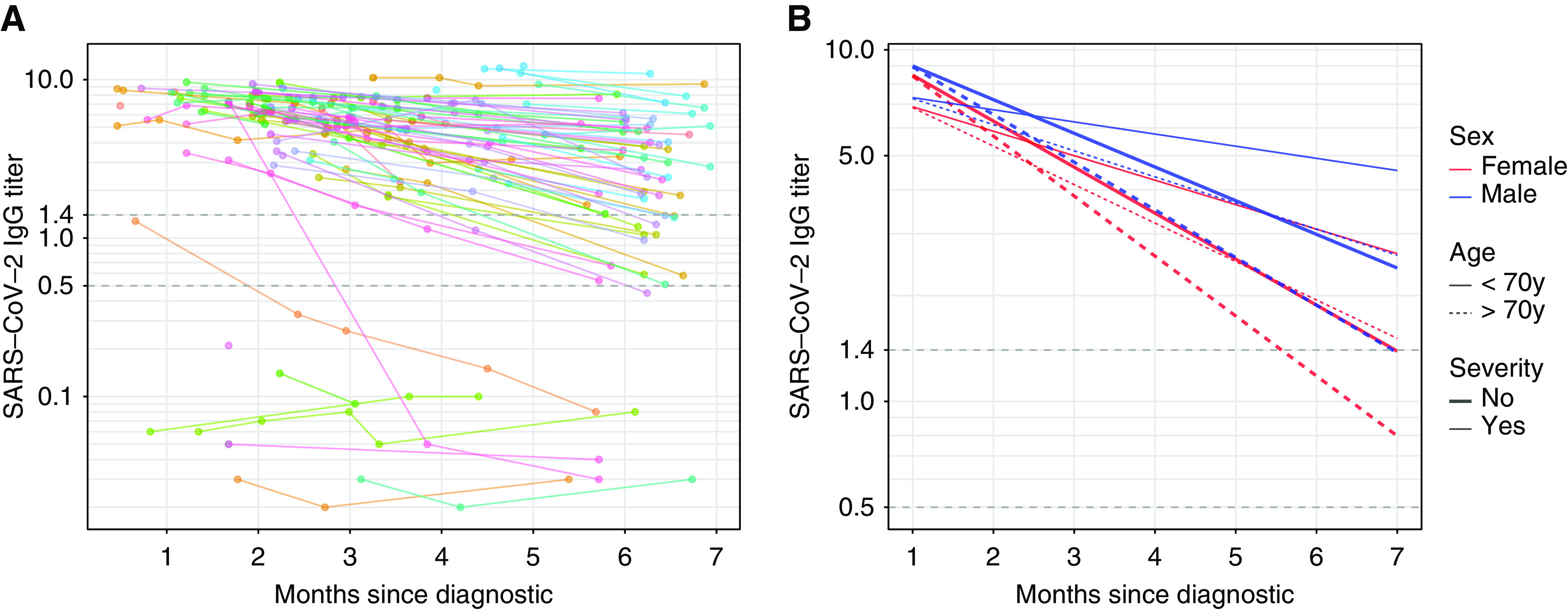
Follow-up until month 6 was available for 65 patients (78%). In 60 of these patients with positive initial antinucleocapsid serology, 15 (25%) had an antinucleocapsid antibody level below the limit of positivity (index ratio <1.4). Among these 15 patients, 13 (87%) had an index ratio between 0.5 and 1.4, and two (13%) had an index ratio <0.49 (Figure 1A). Only a low initial SARS-CoV-2 antibody value was associated with long-term negative antinucleocapsid antibody level (7.1; IQR, 2.3 versus 3.44; IQR, 1.6; P<0.0001) (Supplemental Table 6). Of the 15 sera samples with antinucleocapsid antibody level below the limit of positivity, 14 were tested for antispike antibodies, and three of the 14 (21%) were also negative with this assay (Figure 2).
Figure 2.
Evolution of SARS-CoV-2 IgG antispike antibody titers until 6 months after diagnosis. Evolution of SARS-CoV-2 IgG titer for each patient over time (spaghetti plot). Cutoff for negative serology was defined according to the manufacturer (Index S/C <1: dashed line).
The estimated slope of IgG antinucleocapsid titer weekly decrease was −0.022 log10 (95% CI, −0.03 to −0.02), meaning the geometric mean titer decreased weekly by 4.9% (95% CI, 4.1 to 5.7). Female sex (−0.0081 log10; 95% CI, −0.00026 to −0.016; P=0.05), age >70 years (−0.0091 log10; 95% CI, −0.017 to −0.0018; P=0.02), and nonsevere clinical presentation (−0.014 log10; 95% CI, −0.0069 to −0.021; P=<0.001) were independently associated with a faster IgG antinucleocapsid titer decay in multivariable analysis (Figure 1B). Regarding antispike assay, all 74 antinucleocapsid-positive specimens were also antispike positive, except for two (3%) patients, who repeatedly tested negative for antispike antibodies despite being positive for antinucleocapsid antibodies. The estimated slope of the antispike IgG titer weekly decrease was −0.0080 log10 (95% CI, −0.011 to −0.0045), meaning the geometric mean titer decreased weekly by 1.8% (95% CI, 1.0 to 2.6). After adjustment for sex and age >70 years, non-severe clinical presentation was the only factor associated with a steeper decay (−0.0082 log10; 95% CI, −0.015 to −0.0015; P=0.02).
Discussion
In this study, we describe the 6-month kinetics of IgG antibody response against SARS-CoV-2 in patients on hemodialysis. On the basis of assay findings for antinucleocapsid and antispike antibodies, we observed a lack of seroconversion in 10% of patients, as previously suggested in the general population and in rare patients on hemodialysis.4 Interestingly, we show that lack of seroconversion was associated with immunocompromised status, as previously suggested,3 which may explain the frequency of patients with glomerular disease in this group. Whether immunosuppression also affects seroconversion in patients not on dialysis remains to be studied. Interestingly, a lack of seroconversion was observed in 7.9%–33% of patients (depending on the assay) of a recent cohort of patients who had undergone kidney transplant.5
Long-term evolution in anti–SARS-CoV-2 antibodies is still a matter of debate, although virus-specific IgG decline seems to occur in most individuals.6,7 In our study, the antibody response of patients on hemodialysis seems similar to that of previously reported healthy individuals. Our models suggest IgG decline continues over time and is independently associated with female sex, nonsevere disease, and older age. Whether this decline is also associated with loss of neutralizing antibodies or cellular response to SARS-CoV-2 will require further study.7 Of note, this IgG decline leads to antinucleocapsid antibody titers below the cutoff value in 25% of patients 6 months after diagnosis, although most patients had levels in the gray zone (signal to cutoff ratio between 0.5 and 1.4, Figure 1A) and maintain antispike antibodies.
This retrospective study has some limitations. Lack of seroconversion in patients who are RT-PCR negative should be interpreted with caution, although reported RT-PCR sensitivity is approximately 80% in the hemodialysis population.3 In addition, our findings would have been enriched by the use of different serologic assays, earlier in disease evolution (notably in patients who did not survive), by evaluating different antibody subclasses and characterizing cellular immunity, which is not necessarily parallel to the humoral response.
However, this characterization of the evolution of the SARS-CoV-2 antibody response in patients on hemodialysis, and the identification of factors associated with lack of seroconversion and with IgG titer decay, might help to better define future therapeutic and preventive approaches, including vaccination strategies.
Disclosures
K. El Karoui reports receiving research funding from Amgen, Otsuka, and Sanofi, and honoraria from Alexion and Otsuka. S. Fourati reports receiving honoraria from Abbott Diagnostics. All remaining authors have nothing to disclose.
Funding
None.
Supplementary Material
Acknowledgments
Hamza Sakhi, Philippe Attias, Thomas Kofman, and Khalil El Karoui designed the study; Hamza Sakhi, Philippe Attias, Thomas Kofman, Djamal Dahmane, Larbi Lamriben, Slim Fourati, and Khalil El Karoui collected data; Hamza Sakhi, Philippe Attias, Thomas Kofman, Djamal Dahmane, Larbi Lamriben, Thomas Stehlé, Vincent Audard, Julie Oniszczuk, and Nizar Joher cared for the study patients; Hamza Sakhi, Philippe Attias, Thomas Kofman, Nathanael Lapidus, Slim Fourati, and Khalil El Karoui analyzed the data; Hamza Sakhi, Nathanael Lapidus, Slim Fourati, and Khalil El Karoui wrote the paper; and all authors provided feedback and critical review.
Footnotes
Published online ahead of print. Publication date available at www.jasn.org.
Contributor Information
Collaborators: Mondor NephroCov Study Group, Vincent Audard, Boutheina Bentaarit, Anna Boueilh, Sébastien Gallien, Philippe Grimbert, Sophie Hüe, Nizar Joher, Narindra Jouan, Larbi Lamriben, Jean-Daniel Lelièvre, Raphaël Lepeule, Matthieu Mahévas, Marie Matignon, Giovanna Melica, Julie Oniszczuk, Jean-Michel Pawlotsky, Thomas Stehlé, William Vindrios, and Charlotte Wemmert
Supplemental Material
This article contains the following supplemental material online at http://jasn.asnjournals.org/lookup/suppl/doi:10.1681/ASN.2020111618/-/DCSupplemental.
Supplemental Table 1. Clinical and biological presentation of patients at diagnosis.
Supplemental Table 2. Clinical characteristics of patients according to SARS-CoV-2 IgG antinucleocapsid response.
Supplemental Table 3. Detailed characteristics of patients with absence of SARS-CoV-2 IgG antinucleocapsid response.
Supplemental Table 4. Clinical characteristics of patients with RT-PCR confirmed diagnosis, according to their initial SARS-CoV-2 IgG antinucleocapsid antibody response.
Supplemental Table 5. Multivariable analysis of factors associated with the absence of initial SARS-CoV-2 IgG antinucleocapsid antibody response.
Supplemental Table 6. Patient characteristics according to their long-term SARS-CoV-2 IgG antinucleocapsid antibody response.
References
- 1. Couchoud C, Bayer F, Ayav C, Béchade C, Brunet P, Chantrel F, et al.: Low incidence of SARS-CoV-2, risk factors of mortality and the course of illness in the French national cohort of dialysis patients. Kidney Int 98: 1519–1529, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Chawki S, Buchard A, Sakhi H, Dardim K, El Sakhawi K, Chawki M, et al.; HD-CovIDF Study Group: Treatment impact on COVID-19 evolution in hemodialysis patients. Kidney Int 98: 1053–1054, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Clarke C, Prendecki M, Dhutia A, Ali MA, Sajjad H, Shivakumar O, et al.: High prevalence of asymptomatic COVID-19 infection in hemodialysis patients detected using serologic screening. J Am Soc Nephrol 31: 1969–1975, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Tang H, Tian J-B, Dong J-W, Tang X-T, Yan Z-Y, Zhao Y-Y, et al.: Serologic detection of SARS-CoV-2 infections in hemodialysis centers: A multicenter retrospective study in Wuhan, China. Am J Kidney Dis 76: 490–499.e1, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Prendecki M, Clarke C, Gleeson S, Greathead L, Santos E, McLean A, et al.: Detection of SARS-CoV-2 antibodies in kidney transplant recipients. J Am Soc Nephrol 31: 2753–2756, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Ripperger TJ, Uhrlaub JL, Watanabe M, Wong R, Castaneda Y, Pizzato HA, et al.: Orthogonal SARS-CoV-2 serological assays enable surveillance of low-prevalence communities and reveal durable humoral immunity. Immunity 53: 925–933.e4, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Wajnberg A, Amanat F, Firpo A, Altman DR, Bailey MJ, Mansour M, et al.: Robust neutralizing antibodies to SARS-CoV-2 infection persist for months. Science 370: 1227–1230, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.