Abstract
Objectives
To date, the clinical stability of dual-thread orthodontic miniscrews has not been studied. This study aimed to compare the primary stability and long-term clinical success rate of dual-thread and cylindrical orthodontic miniscrews and to examine the association between various clinical factors and the success rate of miniscrews.
Materials and Methods
A total of 145 cylindrical and 135 dual-thread miniscrews were inserted in the maxillary and mandibular buccal alveolar areas of 142 patients. The torque and Periotest (Siemens, Bensheim, Germany) values were recorded during insertion and removal. The effect of clinical variables such as sex, age, screw design, jaw, side of placement, root proximity, and site of placement on the success rate was examined using logistic regression analysis.
Results
There was no statistically significant difference (P = .595) in the overall clinical success rate between the two designs, with an overall success rate of 82.1% and 84.4% for the cylindrical and dual-thread miniscrews, respectively. Age and screw-root proximity were significantly associated with failure (P < .05).
Conclusions
The dual-thread miniscrews did not show superior long-term stability and clinical success rate as compared with the cylindrical miniscrews. The results of this study suggest that patient age and screw-root proximity influence the clinical success rate of miniscrews.
Keywords: Stability, Success rate, Orthodontic miniscrews, Dual-thread, Cylindrical, Screw-root proximity, Age
INTRODUCTION
The introduction of miniscrews to clinical orthodontics has provided a solution to absolute anchorage and allowed for more efficient and diverse orthodontic tooth movement. Despite successful treatment results using miniscrews, a wide range in the success rate, varying between approximately 75% and 90%, has been reported, limiting the predictability of achieving reliable clinical outcomes.1–3
Primary stability is considered important for the success of miniscrews.4 Key factors contributing to primary stability may be divided into host- and screw-related factors. Host factors include bone quality, bone quantity, cortical bone thickness, and the patient's age, whereas screw-related factors include the length, diameter, and design of the miniscrews.5 Clinically, because of the anatomical limitations of the buccal alveolar area, screw-related factors are more readily managed to acquire improved primary stability.
Primary stability can be improved by increasing the diameter and length of the miniscrew. However, the extent to which the diameter and length can be increased is limited by proximity to the adjacent tooth roots and risk of root contact.2,6,7 To compensate for this limitation, tapered miniscrews have been developed. The tapered shape increases primary stability by applying a compressive force to the cortical bone while reducing the risk of root contact. In a clinical study, tapered miniscrews showed higher initial stability than cylindrical miniscrews, while long-term stability was unaffected.8
Dual-thread miniscrews were developed based on the microthread concept of prosthetic implants. Prosthetic implants designed with microthreads in the neck region were considered to distribute stress more favorably to the peri-implant tissue.9 In artificial bone models, the dual-thread design reportedly improved mechanical stability.10 However, in a study using artificial bone models, it was found that excessive stress can be applied to the peri-implant bone in cases of thick cortical bone.11 To date, the clinical stability of dual-thread miniscrews has not been studied.
This study aimed to compare the stability and clinical success rate of dual-thread and cylindrical orthodontic miniscrews and to examine the association between various clinical factors and the success rate of miniscrews.
MATERIALS AND METHODS
Case records in which miniscrews were inserted for anchorage from February 2009 to August 2014 were retrospectively investigated. Two types of miniscrew designs were alternately selected during the period. Two hundred eighty self-drilling miniscrews (145 cylindrical and 135 dual-thread; Biomaterials Korea, Seoul, Korea) were inserted in the maxillary and mandibular buccal alveolar areas of 142 patients (56 male and 86 female). Patients with no relevant medical history and who required miniscrews for successful orthodontic treatment were included. A power analysis was performed using G power version 3.1.9.4 (Franz Faul, Universität Kiel, Germany). It was determined that a sample size of 105 miniscrews in each group would provide greater than 95% power to detect a significant difference with a 0.5 effect size at a significance level of α = .05. Therefore, the numbers of the two designs of miniscrews during this period were considered adequate. Each miniscrew was considered as independent. The mean age of the patients was 20.7 ± 7.5 years. All patients provided written informed consent prior to the placement of miniscrews. The ethics committee of Yonsei Dental Hospital approved the present study (2-2012-0011).
Two types of self-drilling miniscrews with a 1.5-mm diameter and 7.0-mm length were placed in the maxillary and mandibular buccal alveolar areas (Figure 1; Table 1). The miniscrews were installed using a manual hand driver, without predrilling. Each screw was placed by one of four orthodontic specialists, following a standardized protocol. Insertion and removal torque were measured using a torque sensor (MGT50, Mark-10, Copiague, NY) and mobility was measured using the Periotest (Siemens, Bensheim, Germany) device. Postoperative periapical radiographs were obtained for each case.
Figure 1.
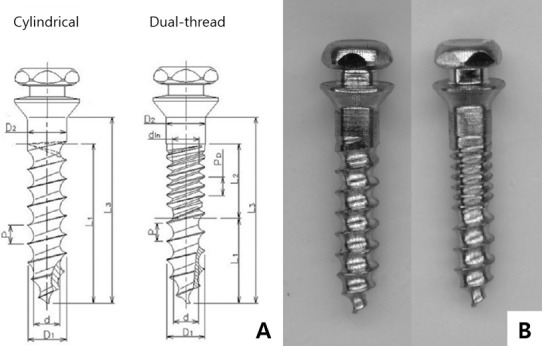
(A) Schematic diagram of cylindrical and dual-thread miniscrews (the abbreviations are described in Table 1). (B) Photograph of cylindrical and dual-thread miniscrews (left and right, respectively).
Table 1.
Description of Miniscrews Tested in This Study (Unit: mm)
| Abbreviation |
Measurement |
Type |
|
| Cylindrical |
Dual Thread |
||
| D1 | External diameter | 1.45 | 1.45 |
| D2 | Collar diameter | 1.50 | 1.50 |
| d | Internal diameter | 0.95 | 0.95 |
| dIn | Internal diameter of dual part | — | 1.03 |
| L1 | Length of spiral part | 6.00 | 3.20 |
| L2 | Length of dual part | — | 2.80 |
| L3 | Total length | 7.00 | 7.00 |
| P | Pitch | 0.70 | 0.70 |
| PD | Pitch of dual part | — | 0.35 |
Most of the screws were loaded with a 200–250 g force in the third week after placement. The average placement period was 18.8 months (cylindrical: 19.1 months; dual thread: 18.5 months). A successful miniscrew was defined as one that was maintained for longer than 6 months. Removal periods were not recorded in three patients because of transfer, despite a maintenance period longer than 6 months. Miniscrew loss or excessive mobility was indicative of failure. The patient's sex, age, date of surgery, miniscrew design, and insertion site were recorded.
An independent two-samples t-test was used to compare insertion torques and Periotest values (PTVs) between the cylindrical and dual-thread miniscrews. A chi-square analysis was performed to evaluate the success rates of the two miniscrew designs and to analyze the relationship between the success rates and various variables including the operator, sex, jaw, side of placement, root proximity, and site of placement. Logistic regression analyses were used to evaluate the association between the success rate and clinical variables. All statistical analyses were carried out using IBM SPSS 25 (IBM Corp., Armonk, NY). Statistical significance was set at P < .05.
RESULTS
There was no statistically significant difference in the overall success rate between the two miniscrew designs (P = .595). The overall success rates of the cylindrical and dual-thread miniscrews were 82.1% and 84.4%, respectively. Despite the absence of a significant difference (P > .05) in the success rate between the two designs, the dual-thread miniscrews had an enhanced success rate in the maxilla, while the cylindrical miniscrews had a superior success rate in the mandible (Table 2). The difference in the success rates between the maxilla and mandible was not statistically significant between cylindrical (P = .230) and dual-thread miniscrews (P = .113).
Table 2.
Success Rates of the Two Different Miniscrew Designs in the Maxilla and Mandible
| Cylindrical |
Dual Thread |
P (Chi-square) |
|
| Maxilla | 79.1% (72/91) | 88.2% (75/85) | .103 |
| Mandible | 87.0% (47/54) | 78.0% (39/50) | .224 |
| P (chi-square) | .230 | .113 | |
| Total | 82.1% (119/145) | 84.4% (114/135) | .595 |
In the maxilla, the insertion torque and implantation PTV did not significantly differ between the designs (P > .05). In the mandible, the insertion torque was significantly greater in the dual-thread (8.0 Ncm) than in the cylindrical (6.2 Ncm) miniscrews (P < .05). The insertion PTV in both the maxilla and mandible did not differ between the designs (P > .05). Similarly, there was no significant difference in the removal torque and PTV between the two designs in both the maxilla and mandible (P > .05; Table 3).
Table 3.
Peak Insertion and Removal Torque Values (in Ncm) and Periotest Values
| Insertion |
Removal |
|||||||||||
| Torque Value, Ncm |
Periotest Value |
Torque Value, Ncm |
Periotest Value |
|||||||||
| Cylindrical |
Dual-thread |
P |
Cylindrical |
Dual-thread |
P |
Cylindrical |
Dual-thread |
P |
Cylindrical |
Dual-thread |
P |
|
| Maxilla | 6.00 ± 3.17 | 6.19 ± 2.62 | .189 | 1.83 ± 5.77 | 1.15 ± 4.66 | .751 | 3.82 ± 2.60 | 3.94 ± 2.55 | .909 | 7.66 ± 6.26 | 6.43 ± 5.09 | .629 |
| Mandible | 6.48 ± 2.81 | 8.03 ± 3.88 | .013* | 3.69 ± 3.83 | 2.81 ± 5.13 | .255 | 3.92 ± 3.66 | 3.61 ± 2.09 | .100 | 7.12 ± 5.38 | 9.72 ± 6.05 | .522 |
Significance at the .05 level.
The chi-square test showed no difference in the success rates among the four operators (P = .260). In addition, sex, jaw, side of placement, and site of placement did not significantly influence the success rate (P > .05). However, the success rate was affected by screw-root proximity (P < .05). Miniscrews exhibited a higher success rate when placed in the middle of the interradicular space between adjacent teeth than when placed in close proximity to or in contact with the roots (Table 4).
Table 4.
Success Rates and Number of Miniscrews According to Clinical Variablesa
| Clinical Variable |
Success Rate, % |
Success/ Total Miniscrews, n |
P (Chi-square) |
| Sex | |||
| Male | 80.2 | 81/101 | .310 |
| Female | 84.9 | 152/179 | |
| Jaw of placement | |||
| Maxilla | 83.5 | 147/176 | .857 |
| Mandible | 82.7 | 86/104 | |
| Side of placement | |||
| Right | 81.8 | 112/137 | .522 |
| Left | 84.6 | 121/143 | |
| Root proximity | |||
| Center of roots | 91.9 | 181/197 | .000* |
| Close root | 67.6 | 46/68 | |
| Root contact | 40.0 | 6/15 | |
| Site of placement | |||
| Incisors to PM2 | 87.9 | 51/58 | .536 |
| PM2 to M1 | 81.7 | 161/197 | |
| M1 to M2 | 84.0 | 21/25 | |
PM2 indicates second premolar; M1, first molar; M2, second molar.
Significance at the .05 level.
In both the maxilla and mandible, the insertion torque and PTV did not significantly differ between the successful miniscrews and those that failed (P > .05; Table 5).
Table 5.
Mean and Range of Insertion Torques and Periotest Values for Success and Failure Group
| Location |
n |
Insertion Torque, Ncm |
Periotest Value |
||
| Mean ± SD |
P |
Mean ± SD |
P |
||
| Maxilla | |||||
| Success | 147 | 6.0 ± 2.88 | .295 | 1.21 ± 4.97 | .468 |
| Failure | 29 | 6.3 ± 3.15 | 2.97 ± 6.42 | ||
| Mandible | |||||
| Success | 86 | 7.3 ± 3.47 | .561 | 2.92 ± 4.20 | .371 |
| Failure | 18 | 7.0 ± 3.37 | 4.9 ± 5.57 | ||
Logistic regression analysis identified age, insertion PTV, and root proximity as variables affecting the failure rates (Table 6). The failure rate decreased as age increased and increased as the insertion PTV increased. In addition, the failure rate markedly increased when the miniscrew was placed in close proximity to or in contact with the tooth roots, as opposed to insertion in a position located midway between the roots of adjacent teeth. Sex, design, jaw, side of placement, insertion torque, and the operator did not affect the success rate.
Table 6.
Logistic Regression Analysis of Factors Associated With Failure of Miniscrews
| Clinical Variable |
Odds Ratio |
95% CI |
P Value* |
| Age | 0.932 | 0.878–0.990 | .021 |
| Insertion Periotest value | 1.126 | 1.043–1.216 | .002 |
| Contact | |||
| Center between roots | |||
| Close root | 7.421 | 3.239–17.001 | .000 |
| Root contact | 44.126 | 10.911–178.459 | .000 |
Significance at the .05 level.
DISCUSSION
This was the first clinical study to evaluate the stability and clinical success rate of dual-thread miniscrews. The torque and PTV during insertion and removal were investigated to assess initial and long-term stability. In addition, various clinical factors were examined to evaluate each factor's effect on the clinical success of miniscrews. Dalessandri et al. showed that the success rate did not differ among miniscrews with a diameter >1.3 mm.2,6,7 It is recommended that the length of miniscrews penetrating the bone should be >6 mm.1–3 In this study, 1.5-mm diameter and 7-mm length miniscrews were used to control screw-related variables other than the screw design.
The overall success rate achieved in this study was 83.2%, which is within the wide range of success rates reported. Many studies have shown success rates of 80–90%.1–3 Cheng et al.12 reported a success rate of 89%, whereas Motoyoshi et al.13 reported a success rate of 85.5%. Because each study was performed under different clinical conditions, applying different implantation methods, variable success rates have been reported.
In the current study, the success rates using the cylindrical and dual-thread miniscrews did not differ significantly. Only a limited number of studies evaluating the clinical success rate of dual-thread miniscrews have been undertaken. One split-mouth clinical trial reported that the clinical success rate of dual- and mono-thread miniscrews did not differ; however, the sample size was small.14 Meanwhile, studies have concluded that prosthetic implants with microthreads demonstrated reduced marginal bone loss and a higher clinical success rate due to improved stress distribution.9,15 However, the features of prosthetic implants differ from those of orthodontic miniscrews. Prosthetic implants have a rough surface, osseointegration is a prerequisite, and immediate loading is unnecessary.
In the mandible, dual-thread miniscrews had a higher insertion torque than cylindrical miniscrews, although there was no significant difference in the maxilla. Therefore, this finding was consistent with that of a previous in vitro study using an artificial bone model that found that dual-thread miniscrews resulted in a higher insertion torque. In addition, the insertion torque and strain on the surrounding bone have been observed to markedly increase as the cortical bone thickness increased.11 Therefore, it was presumed that the thicker cortical bone and higher bone density of the mandible created a significant difference in insertion torque between the designs only in the mandible.
The insertion torque reflects the initial stability. However, this parameter is not perfectly related to the stability of miniscrews. The results of this study showed no difference in the insertion torque between the miniscrews that were successful and those that failed, possibly because excessive insertion torque may induce pressure necrosis in the peri-implant bone.16 A group of researchers proposed that, because dual-thread miniscrews demonstrated a higher insertion torque and strain in comparison with single-thread miniscrews, dual-thread miniscrews should be placed in areas with thin cortical bone or low bone density.17 The findings of the present study support those of previous studies. The insertion torque of the dual-thread miniscrews was higher than that of the cylindrical miniscrews in the mandible; however, the success rate of the dual-thread miniscrews was 78.0% in the mandible, lower than their 88.2% success rate in the maxilla or the 87.0% success rate for the cylindrical miniscrews in the mandible. Although the differences were not statistically significant, these results suggested that dual-thread miniscrews were not appropriate for use in areas with high bone density or thick cortical bone.
No significant difference in the insertion PTV was found between the two designs in either the maxilla or mandible. It has been suggested that the stability of miniscrews can be evaluated using the insertion PTV, especially in the mandible.18 In this study, there was no difference in the insertion PTV between the miniscrews that were successful and those that failed. Conversely, according to the logistic regression analysis, the probability of failure increased with an increase in insertion PTV. These contradictory results may have been due to the wide range of insertion PTVs. Therefore, it would be difficult to predict long-term stability using the insertion PTV.
The removal torque and PTV did not differ between the two designs in either the maxilla or the mandible. Because the average placement period in the present study was 18.8 months, it was concluded that the long-term stability of the two designs did not differ. Despite a high insertion torque, long-term stability has been seen to decline over time, as the excessive stress initially distributed to the surrounding bone is balanced or micro-damage occurs.19
In this study, screw-root proximity and age were the factors affecting the success rate, whereas sex, jaw, placement side, and placement location did not. In instances in which the miniscrew contacted a root, the success rate was 40.0%. The success rate markedly improved to 91.9% when placed midway between the roots of adjacent teeth. Screw-root proximity is regarded as a major factor affecting the success of miniscrews, as the orthodontic force applied to teeth can be intermittently transmitted to the miniscrews, which can result in their subsequent loss.20,21
Age was also identified as an important factor influencing the success rate of miniscrews. Previous studies have also found that the success rate of miniscrews is lower in adolescent groups younger than 20 years.6,22,23 Miniscrews show superior stability in adults as compared with growing adolescents, because bone density and cortical bone thickness are greater in adults. There is poorer bone quality and a higher bone turnover rate in adolescents, complicating the achievement of optimal mechanical miniscrew stability in growing patients.6
Patient- and operator-related factors, such as bone quality or screw-root proximity, influenced the success rate of miniscrews to a greater extent than the design factor, and these variables should be considered when inserting miniscrews. Motoyoshi et al.24 suggested that, in adolescents, the success rate can be improved through delayed loading of 3 months. An interradicular distance greater than 3 mm is required for safe and successful miniscrew placement.25 As image distortion is common in two-dimensional panoramic images, a three-dimensional image could be acquired for more precise evaluation.26 In addition, a surgical guide can be fabricated to further increase the accuracy of miniscrew placement.27,28
CONCLUSIONS
The initial stability and long-term success rate of cylindrical and dual-thread miniscrews were similar.
The insertion torque of the dual-thread miniscrews was significantly higher than that of the cylindrical miniscrews in the mandible.
The insertion torque of the miniscrews that were deemed successful did not differ from that of those that failed.
Patient age and screw-root proximity influenced the clinical success rate, while miniscrew type, sex, jaw, side, and site of placement did not.
ACKNOWLEDGMENT
This study was supported by a faculty research grant from Yonsei University College of Dentistry (6-2016-0022).
REFERENCES
- 1.Chen Y, Kyung HM, Zhao WT, Yu WJ. Critical factors for the success of orthodontic mini-implants: a systematic review. Am J Orthod Dentofacial Orthop. 2009;135:284–291. doi: 10.1016/j.ajodo.2007.08.017. [DOI] [PubMed] [Google Scholar]
- 2.Crismani AG, Bertl MH, Celar AG, Bantleon HP, Burstone CJ. Miniscrews in orthodontic treatment: review and analysis of published clinical trials. Am J Orthod Dentofacial Orthop. 2010;137:108–113. doi: 10.1016/j.ajodo.2008.01.027. [DOI] [PubMed] [Google Scholar]
- 3.Reynders R, Ronchi L, Bipat S. Mini-implants in orthodontics: a systematic review of the literature. Am J Orthod Dentofacial Orthop. 2009;135:564–565. doi: 10.1016/j.ajodo.2008.09.026. [DOI] [PubMed] [Google Scholar]
- 4.Motoyoshi M, Uemura M, Ono A, Okazaki K, Shigeeda T, Shimizu N. Factors affecting the long-term stability of orthodontic mini-implants. Am J Orthod Dentofacial Orthop. 2010;137:588–589. doi: 10.1016/j.ajodo.2009.05.019. [DOI] [PubMed] [Google Scholar]
- 5.Cha JY, Kil JK, Yoon TM, Hwang CJ. Miniscrew stability evaluated with computerized tomography scanning. Am J Orthod Dentofacial Orthop. 2010;137:73–79. doi: 10.1016/j.ajodo.2008.03.024. [DOI] [PubMed] [Google Scholar]
- 6.Dalessandri D, Salgarello S, Dalessandri M, et al. Determinants for success rates of temporary anchorage devices in orthodontics: a meta-analysis (n > 50) Eur J Orthod. 2014;36:303–313. doi: 10.1093/ejo/cjt049. [DOI] [PubMed] [Google Scholar]
- 7.Lim JE, Lim WH, Chun YS. Quantitative evaluation of cortical bone thickness and root proximity at maxillary interradicular sites for orthodontic mini-implant placement. Clin Anat. 2008;21:486–491. doi: 10.1002/ca.20671. [DOI] [PubMed] [Google Scholar]
- 8.Yoo SH, Park YC, Hwang CJ, Kim JY, Choi EH, Cha JY. A comparison of tapered and cylindrical miniscrew stability. Eur J Orthod. 2014;36:557–562. doi: 10.1093/ejo/cjt092. [DOI] [PubMed] [Google Scholar]
- 9.Lima de Andrade C, Carvalho MA, Bordin D, da Silva WJ, Del Bel Cury AA, Sotto-Maior BS. Biomechanical behavior of the dental implant macrodesign. Int J Oral Maxillofac Implants. 2017;32:264–270. doi: 10.11607/jomi.4797. [DOI] [PubMed] [Google Scholar]
- 10.Kim JW, Cho IS, Lee SJ, Kim TW, Chang YI. Effect of dual pitch mini-implant design and diameter of an orthodontic mini-implant on the insertion and removal torque. Korean J Orthod. 2006;36:275–283. [Google Scholar]
- 11.Cha JY, Hwang CJ, Kwon SH, Jung HS, Kim KM, Yu HS. Strain of bone-implant interface and insertion torque regarding different miniscrew thread designs using an artificial bone model. Eur J Orthod. 2015;37:268–274. doi: 10.1093/ejo/cju037. [DOI] [PubMed] [Google Scholar]
- 12.Cheng SJ, Tseng IY, Lee JJ, Kok SH. A prospective study of the risk factors associated with failure of mini-implants used for orthodontic anchorage. Int J Oral Maxillofac Implants. 2004;19:100–106. [PubMed] [Google Scholar]
- 13.Motoyoshi M, Hirabayashi M, Uemura M, Shimizu N. Recommended placement torque when tightening an orthodontic mini-implant. Clin Oral Implants Res. 2006;17:109–114. doi: 10.1111/j.1600-0501.2005.01211.x. [DOI] [PubMed] [Google Scholar]
- 14.Durrani OK, Shaheed S, Khan A, Bashir U. Comparison of in-vivo failure of single-thread and dual-thread temporary anchorage devices over 18 months: a split-mouth randomized controlled trial. Am J Orthod Dentofacial Orthop. 2017;152:451–457. doi: 10.1016/j.ajodo.2017.05.019. [DOI] [PubMed] [Google Scholar]
- 15.Calvo-Guirado JL, Lopez-Lopez PJ, Perez-Albacete Martinez C, et al. Peri-implant bone loss clinical and radiographic evaluation around rough neck and microthread implants: a 5-year study. Clin Oral Implants Res. 2018;29:635–643. doi: 10.1111/clr.12775. [DOI] [PubMed] [Google Scholar]
- 16.Meredith N. Assessment of implant stability as a prognostic determinant. Int J Prosthodont. 1998;11:491–501. [PubMed] [Google Scholar]
- 17.Cha JY, Takano-Yamamoto T, Hwang CJ. The effect of miniscrew taper morphology on insertion and removal torque in dogs. Int J Oral Maxillofac Implants. 2010;25:777–783. [PubMed] [Google Scholar]
- 18.Cha JY, Yu HS, Hwang CJ. The validation of Periotest values for the evaluation of orthodontic mini-implants' stability. Korean J Orthod. 2010;40:167–175. [Google Scholar]
- 19.Cha JY, Yoon TM, Hwang CJ. Insertion and removal torques according to orthodontic mini-screw design. Korean J Orthod. 2008;38:5–12. [Google Scholar]
- 20.Kuroda S, Sugawara Y, Deguchi T, Kyung HM, Takano-Yamamoto T. Clinical use of miniscrew implants as orthodontic anchorage: success rates and postoperative discomfort. Am J Orthod Dentofacial Orthop. 2007;131:9–15. doi: 10.1016/j.ajodo.2005.02.032. [DOI] [PubMed] [Google Scholar]
- 21.Tsatalis AE, Watanabe K, Mitchell B, et al. Mechanical and clinical evaluation of the effect of microscrew on root proximity and cortical bone thickness. Eur J Orthod. 2020;42:206–210. doi: 10.1093/ejo/cjz017. [DOI] [PubMed] [Google Scholar]
- 22.Chen YJ, Chang HH, Huang CY, Hung HC, Lai EHH, Yao CCJ. A retrospective analysis of the failure rate of three different orthodontic skeletal anchorage systems. Clin Oral Implants Res. 2007;18:768–775. doi: 10.1111/j.1600-0501.2007.01405.x. [DOI] [PubMed] [Google Scholar]
- 23.Lee SJ, Ahn SJ, Lee JW, Kim SH, Kim TW. Survival analysis of orthodontic mini-implants. Am J Orthod Dentofacial Orthop. 2010;137:194–199. doi: 10.1016/j.ajodo.2008.03.031. [DOI] [PubMed] [Google Scholar]
- 24.Motoyoshi M, Matsuoka M, Shimizu N. Application of orthodontic mini-implants in adolescents. Int J Oral Maxillofac Surg. 2007;36:695–699. doi: 10.1016/j.ijom.2007.03.009. [DOI] [PubMed] [Google Scholar]
- 25.Schnelle MA, Beck FM, Jaynes RM, Huja SS. A radiographic evaluation of the availability of bone for placement of miniscrews. Angle Orthod. 2004;74:832–837. doi: 10.1043/0003-3219(2004)074<0832:AREOTA>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 26.Lee KJ, Joo E, Kim KD, Lee JS, Park YC, Yu HS. Computed tomographic analysis of tooth-bearing alveolar bone for orthodontic miniscrew placement. Am J Orthod Dentofacial Orthop. 2009;135:486–494. doi: 10.1016/j.ajodo.2007.05.019. [DOI] [PubMed] [Google Scholar]
- 27.Bae MJ, Kim JY, Park JT, et al. Accuracy of miniscrew surgical guides assessed from cone-beam computed tomography and digital models. Am J Orthod Dentofacial Orthop. 2013;143:893–901. doi: 10.1016/j.ajodo.2013.02.018. [DOI] [PubMed] [Google Scholar]
- 28.Kim SH, Choi YS, Hwang EH, Chung KR, Kook YA, Nelson G. Surgical positioning of orthodontic mini-implants with guides fabricated on models replicated with cone-beam computed tomography. Am J Orthod Dentofacial Orthop. 2007;131:S82–S89. doi: 10.1016/j.ajodo.2006.01.027. [DOI] [PubMed] [Google Scholar]


