Abstract
Objective:
To evaluate the contemporary geographic trends in cardiovascular health in the United States (US) and its relationship with the geographic distribution of cardiovascular mortality.
Patients and Methods:
Using a retrospective cross-sectional design, the 2011–2017 Behavioral Risk Factor Surveillance System (BRFSS) was queried to determine the age-adjusted prevalence of cardiovascular health index (CVHI) metrics (sum of ideal blood pressure, blood glucose, lipid levels, body-mass index, smoking, physical activity, and diet). Cardiovascular health was estimated as both continuous (0–7 points) and categorical (ideal, intermediate, poor) variables from BRFSS. Age-adjusted cardiovascular mortality for 2017 was obtained from the CDC WONDER database.
Results:
Among 1,362,529 American adult participants of BRFSS 2011–2017 and all American residents in 2017, the CVHI score increased from 3.89±0.004 in 2011 to 3.96±0.01 in 2017 (Ptrend<.001) nationally, with modest improvement across all regions (Ptrend<.05 for all). Ideal cardiovascular health prevalence improved in the northeastern (Ptrend=.03) and southern regions (Ptrend=.002). The prevalence of coronary heart disease [2017: 6.8% (95%CI:6.5–7.1%)] and stroke [2017: 3.7% (95%CI:3.4–3.9%)] was highest in the southern region. The CVHI score (3.81±0.01) and the prevalence of ideal cardiovascular health [2017:12.2% (95%CI:11.7–12.7%)] was lowest in the southern US. This corresponded to the higher cardiovascular mortality in the southern region (233.0 [95% CI: 232.2–233.8] per 100,000 persons).
Conclusion:
Despite a modest improvement in CVHI, only one-in-six Americans have ideal cardiovascular health with significant geographic differences. These differences correlate with the geographic distribution of cardiovascular mortality. An urgent unmet need exists to mitigate the geographic disparities in cardiovascular morbidity and mortality.
Keywords: Cardiovascular Health, Cardiovascular Mortality, Diabetes, Health Disparities, Hypertension, Hyperlipidemia, Obesity
Introduction
Geographic disparities in cardiovascular health are longstanding and pervasive in the United States of America (US).1–4 There is limited contemporary data on the state-level and regional trends in cardiovascular risk factors, health behaviors, and risk factors.1, 2 Additionally, it is unclear how these geographic trends in cardiovascular risk factors and diseases are associated with state-level cardiovascular mortality.5 When combined with the pre-existing geographic differences in cardiovascular disease and cardiovascular care delivery,1, 2 the cardiovascular mortality may be more significantly impacted in some areas than others. Evaluation of these critical trends in cardiovascular health may, therefore, guide resource utilization, public health planning, and risk factor control.
We hypothesized that there is geographic heterogeneity in the trends of ideal cardiovascular health and that the geographic dispersion of cardiovascular risk factors overlaps with cardiovascular mortality. We sought to evaluate 1) the nationwide and regional trends of overall cardiovascular health and the prevalence of cardiovascular risk factors, 2) regional distribution of cardiovascular mortality, and 3) the overlap of cardiovascular mortality with state-level cardiovascular health. We present the results of an investigation that evaluates these objectives using nationally representative and geographically stratified data from 2011–2017.
Methods
Data Sources
The Behavioral Risk Factor Surveillance System (BRFSS) is a health-related survey conducted via telephone (landline and cellphone), collecting data from more than 400,000 adults each year.1, 2 It assimilates data on chronic health conditions and health risk behaviors. It is one of the largest continuously conducted health survey system in the world and has been validated across various studies to evaluate and assess state-level health characteristics.
The national mortality and population data from the Centers for Disease Control and Prevention (CDC) Wide-Ranging Online Data for Epidemiologic Research (WONDER) database was evaluated to assess the geographic distribution of cardiovascular mortality.6 The database recognizes the underlying cause of death and the demographic characteristics of the population, using data derived from the death certificates of all US residents. The International Statistical Classification of Diseases and Related Health Problems, Tenth Revision (ICD-10) is used to code the underlying cause of death.6 The state-level population estimated were derived from the US Census Bureau. The study was non-human subjects research and was exempted by the Institutional Review Board.
Study Population
Individuals ≥18 years of age from the 2011, 2013, 2015, and 2017 BRFSS survey, living in the US, were included in the study sample. Complete assessments of cardiovascular risk factors, including essential metrics such as hypertension and dyslipidemia, were done every alternate year in the BRFSS surveys. Pregnant females (N=11,200) and those with missing data on cardiovascular health index (CVHI) components (N=518,436) were excluded. The final study population included 1,362,529 individuals.
The nationwide mortality data was assessed for all American residents in the year 2017. All the data were analyzed in the U.S. Census-defined geographic regions (i.e., Northeast, Midwest, South, and West).6
Measures
The demographic, socioeconomic, and health care data that were obtained which included age (18–44, 45–64, ≥65 years), sex (males/female), race (non-Hispanic Whites, non-Hispanic Blacks, Hispanics, and others), annual household income (<$15,000, $15,000-$25,000, $25,000-$35,000, $35,000-$50,000, >$50,000), insurance status (Yes/No) and education level (less than high school, high school, more than high school).
The CVHI was used to define cardiovascular health.1, 2 The CVHI was defined using seven cardiovascular health parameters: blood pressure, cholesterol, blood glucose, body-mass index, smoking behavior, physical activity, and healthy diet.1, 2 The CVHI components were described as ‘ideal’ or ‘not ideal’, as previously described.1, 2 The definitions of the cardiovascular risk factors, CVHI parameters, and cardiovascular disease, which included hypertension, diabetes, dyslipidemia, obesity, smoking status, physical activity, diet, coronary heart disease, and stroke, are defined in Supplementary Methods and Supplementary Table 1.
Total CVHI was computed by summation of the total number of ideal CVHI parameters across the 7 categories. We categorized the CVHI as “ideal” if a participant was categorized as “ideal” for >5 individual factors. Those with 3–5 ideal factors were termed as having “intermediate” cardiovascular health. Individuals with <3 ideal factors were determined to have “poor” cardiovascular health. The cardiovascular cause of death was identified from the CDC WONDER database using ICD-10 Codes (I00-I99).6
Statistical Analysis
The survey procedures in SAS version 9.4 (SAS Institute Inc., Cary, NC) were used to account for the complex survey design with stratified sampling and to analyze the BRFSS data. The sample weights, which account for the non-response and non-coverage in the sampling design, were used to estimate the national, regional, and state-level population estimates.7, 8 The baseline demographic and socioeconomic characteristics of all the BRFSS participants across the regions were summarized. The age-standardized prevalence estimates were computed using the 2010 US Census population proportions for the age-groups of 18–44, 45–64, ≥65 years. Multivariable-adjusted linear regression models with orthogonal polynomial contrast were used to evaluate the trends in the CVHI score. Multivariable-adjusted logistic regression models were used to examine the trends in the CVHI categories and cardiovascular risk factors. As the cardiovascular risk factors may be affected by demographic and socioeconomic factors, the trends were adjusted for sex, race, education level, annual household income, and health insurance status. The trends were also adjusted using the Bonferroni method for multiple comparisons (adjusted α=0.0083). The definition of these covariates and tests of model effects is described in Supplementary Methods. The data were post-stratified by regions to generate regional prevalence estimates and trends. The age-adjusted cardiovascular mortality was estimated in the cross-sectional analysis of the national mortality data for all American adults in 2017. Correlation between poor CVHI and age-adjusted cardiovascular mortality by states was evaluated. We evaluated the relationship in sub-groups of sex and race (non-Hispanic Whites and non-Hispanic Blacks) at the national level and at the level of census regions. Due to low counts and unreliable state-level BRFSS estimates, Hispanics and other races were not evaluated in this analysis.
Results
We included 1,362,529 participants of BRFSS with data for all CVHI metrics available. The demographic distribution and socioeconomic indicators of the study population across the census regions are described in Supplementary Table 2.
Trends in CVHI: Stratified by Geographic Regions
Nationally, the 7-point CVHI improved from 3.89±0.004 in 2011 to 3.96±0.005 in 2017 (Ptrend <.001) (Table 1). In the northeastern region, the CVHI increased from 3.96±0.01 in 2011 to 4.04±0.01 in 2017 (Ptrend=.001). CVHI increased from 3.82±0.01 in 2011 to 3.90±0.01 in 2017 (Ptrend=.001) in the midwestern region. In the southern region, CVHI improved from 3.74±0.01 in 2011 to 3.81±0.01 in 2017 (Ptrend=.002). CVHI improved from 4.11±0.01 in 2011 to 4.17±0.01 in 2017 (Ptrend=.04) in the western region. The western region had the highest CVHI in the US, and the southern region had the lowest CVHI in the US.
Table 1.
Age Standardized Weighted Prevalence of Ideal, Intermediate and Poor Cardiovascular Health: BRFSS 2011-2017
| 2011 | 2013 | 2015 | 2017 | Trend P-valued | |
|---|---|---|---|---|---|
| CVHI Scorea,b | |||||
| Overall | 3.89±0.004 | 3.85±0.004 | 3.89±0.004 | 3.96±0.01 | <.001 |
| Northeast | 3.96±0.01 | 3.91±0.01 | 3.96±0.01 | 4.04±0.01 | .001 |
| Midwest | 3.82±0.01 | 3.83±0.01 | 3.85±0.01 | 3.90±0.01 | .001 |
| South | 3.74±0.01 | 3.70±0.01 | 3.76±0.01 | 3.81±0.01 | .002 |
| West | 4.11±0.01 | 4.07±0.01 | 4.12±0.01 | 4.17±0.01 | .04 |
| Ideal CVHIa,c | |||||
| Overall | 13.4 (13.2–13.7) | 13.0 (12.8–13.3) | 13.7 (13.4–14.0) | 14.4 (14.1–14.7) | <.001 |
| Northeast | 14.7 (14.0–15.3) | 13.5 (13.0–14.1) | 14.6 (14.0–15.2) | 16.0 (15.3–16.6) | .03 |
| Midwest | 12.7 (12.2–13.2) | 12.9 (12.4–13.4) | 12.3 (11.8–12.8) | 13.2 (12.7–13.6) | .99 |
| South | 10.9 (10.5–11.4) | 10.7 (10.3–11.1) | 11.9 (11.5–12.4) | 12.2 (11.7–12.7) | .002 |
| West | 17.1 (16.5–17.7) | 16.6 (15.9–17.3) | 17.3 (16.6–17.9) | 17.7 (17.0–18.4) | .81 |
| Intermediate CVHIa,c | |||||
| Overall | 71.0 (70.6–71.3) | 71.4 (71.0–71.7) | 71.3 (71.0–71.7) | 71.2 (70.8–71.5) | .99 |
| Northeast | 71.3 (70.5–72.0) | 72.4 (71.7–73.1) | 71.9 (71.1–72.6) | 71.4 (70.7–72.2) | .99 |
| Midwest | 71.2 (70.5–71.8) | 71.7 (71.0–72.3) | 72.8 (72.2–73.4) | 72.0 (71.4–72.5) | .99 |
| South | 70.9 (70.3–71.4) | 70.8 (70.3–71.4) | 70.5 (70.0–71.1) | 70.7 (70.1–71.4) | .99 |
| West | 70.7 (70.0–71.4) | 71.1 (70.2–71.9) | 70.8 (70.1–71.6) | 70.9 (70.0–71.8) | .99 |
| Poor CVHIa,c | |||||
| Overall | 15.6 (15.4–15.9) | 15.6 (15.4–15.8) | 15.0 (14.7–15.2) | 14.5 (14.2–14.7) | .008 |
| Northeast | 14.0 (13.5–14.5) | 14.1 (13.5–14.6) | 13.5 (13.0–14.1) | 12.6 (12.2–13.1) | .07 |
| Midwest | 16.1 (15.6–16.6) | 15.4 (15.0–15.9) | 14.9 (14.4–15.3) | 14.8 (14.4–15.3) | .68 |
| South | 18.2 (17.8–18.6) | 18.5 (18.0–18.9) | 17.5 (17.1–17.9) | 17.1 (16.6–17.6) | .16 |
| West | 12.3 (11.8–12.7) | 12.3 (11.8–12.9) | 11.9 (11.4–12.4) | 11.4 (10.8–11.9) | .99 |
Abbreviations: CVHI: Cardiovascular Health Index;
Age-standardized as per 2010 United States Census population proportions.
Depicted as mean ± standard error.
Depicted as prevalence with 95% confidence interval.
Trend test is adjusted for sex, race, education level, annual household income, health insurance status, and Bonferroni correction for multiple comparisons
The prevalence and trends of ideal, intermediate, and poor CVHI stratified by the geographic regions are depicted in Table 1. The prevalence of ideal CVHI was highest in the western region and lowest in the southern region through the study period. In the northeastern region the prevalence of ideal CVHI improved from 14.7% (95%CI: 14.0–15.3%) in 2011 to 16.0% (95%CI: 15.3–16.6%) in 2017 (Ptrend=.03). The prevalence of ideal CVHI in the southern region improved from 10.9% (95%CI: 10.5–11.4%) in 2011 to 12.2% (95%CI: 11.7–12.7%) in 2017 (Ptrend=.002). The trends for ideal CVHI were stable in the midwestern and western regions (Ptrend>.05 for both). The majority of the population in all the regions had intermediate CVHI. The prevalence of poor CVHI was highest in the southern region [2017: 17.1% (95%CI: 16.6–17.6%)] and lowest in the western region [2017: 11.4% (95%CI: 10.8–11.9%)]. The prevalence of intermediate and poor CVHI was stable during the study period (Ptrend>.05 for all).
Trends in Cardiovascular Risk Factors
Nationally, the prevalence of self-reported hypertension was 33.3% (95%CI: 33.0–33.6%) in 2011 and 32.4% (95%CI: 32.1–32.8) in 2017 (Ptrend=.05) (Table 2, Supplementary Figure 1). The prevalence of self-reported hypertension in the northeastern region showed a decline (Ptrend=.04), while the trends remained stable in the midwestern, southern, and western regions (Ptrend<.05 for all). The highest levels of hypertension were seen in the southern US across the study period. The national prevalence of self-reported diabetes was 10.4% (95%CI: 10.2–10.6%) in 2011 and 10.7% (95%CI: 10.4–10.9%) in 2017 (Ptrend=.02). Self-reported diabetes prevalence was stable across the four regions, with the highest prevalence in the southern region. The prevalence of self-reported hypercholesterolemia decreased between 2011 (35.9% [95%CI: 35.6–36.2%]) and 2017 (31.2% [95%CI: 30.9–31.5%]) (Ptrend<.001). This decline was consistent across all the regions (Ptrend <.001 for all), with the southern region having the highest prevalence.
Table 2.
Age Standardized Weighted Prevalence of Cardiovascular Risk Factors Among American Adults: BRFSS 2011-2017
| 2011 | 2013 | 2015 | 2017 | T rend p-valueb | |
|---|---|---|---|---|---|
| Risk Factor | Percentage (95% CI)a | Percentage (95% CI)a | Percentage (95% CI)a | Percentage (95% CI)a | Linear |
| Diabetes Mellitus | |||||
| Overall | 10.4 (10.2–10.6) | 10.7(10.5–10.9) | 10.8 (10.6–11.0) | 10.7 (10.4–10.9) | .02 |
| Northeast | 9.5 (9.1–10.0) | 9.4 (9.0–9.8) | 9.2 (8.8–9.6) | 9.6 (9.2–10.0) | .99 |
| Midwest | 10.2 (9.8–10.6) | 10.1 (9.7–10.4) | 10.2 (9.8–10.5) | 10.3 (10.0–10.7) | .33 |
| South | 11.5 (11.1–11.8) | 11.9 (11.6–12.3) | 12.3 (11.9–12.6) | 11.8 (11.4–12.2) | .22 |
| West | 9.6 (9.2–10.0) | 10.3 (9.8–10.9) | 10.3 (9.8–10.8) | 9.9 (9.4–10.4) | .99 |
| Hypertension | |||||
| Overall | 33.3 (33.0–33.6) | 33.7(33.4–34.0) | 32.7 (32.4–33.0) | 32.4 (32.1–32.8) | .05 |
| Northeast | 30.9 (30.2–31.6) | 31.4 (30.8–32.1) | 30.2 (29.5–30.8) | 29.8(29.2–30.5) | .04 |
| Midwest | 33.2(32.6–33.8) | 32.6 (32.1–33.2) | 32.1(31.6–32.7) | 32.5(31.9–33.0) | .28 |
| South | 36.3 (35.8–36.9) | 36.9 (36.4–37.4) | 35.7 (35.1–36.2) | 35.5 (34.9–36.2) | .25 |
| West | 30.3(29.7–30.9) | 31.3 (30.5–32.1) | 30.3 (29.6–31.0) | 29.5(28.8–30.3) | .12 |
| Hypercholesterolemia | |||||
| Overall | 35.9 (35.6–36.2) | 35.4 (35.1–35.7) | 33.4 (33.0–33.7) | 31.2 (30.9–31.5) | <.001 |
| Northeast | 34.8 (34.0–35.5) | 35.2 (34.5–35.9) | 32.8 (32.1–33.5) | 30.6 (29.9–31.2) | <.001 |
| Midwest | 35.5 (34.8–36.1) | 34.1 (33.5–34.7) | 32.7 (32.1–33.3) | 30.5 (30.0–31.1) | <.001 |
| South | 37.4 (36.9–37.9) | 36.7 (36.1–37.2) | 34.7 (34.1–35.3) | 32.9 (32.3–33.6) | <.001 |
| West | 34.7 (34.1–35.4) | 34.8 (33.9–35.6) | 32.2 (31.5–33.0) | 29.5(28.8–30.3) | <.001 |
| Obesity | |||||
| Overall | 29.3 (28.9–29.6) | 30.4 (30.0–30.7) | 30.8 (30.4–31.1) | 31.4 (31.1–31.8) | <.001 |
| Northeast | 26.7 (26.0–27.4) | 27.9 (27.2–28.6) | 27.8 (27.1–28.6) | 28.6 (27.9–29.4) | <.001 |
| Midwest | 31.2 (30.5–31.9) | 32.8 (32.1–33.5) | 33.3 (32.6–34.0) | 33.8 (33.2–34.4) | <.001 |
| South | 31.6 (31.0–32.2) | 32.5(31.9–33.0) | 32.9 (32.3–33.5) | 33.9 (33.2–34.6) | <.001 |
| West | 25.6 (25.0–26.3) | 26.7 (25.8–27.5) | 27.1 (26.3–27.8) | 27.4(26.6–28.2) | <.001 |
| Smoking | |||||
| Overall | 18.4 (18.1–18.7) | 17.1 (16.8–17.4) | 15.9 (15.6–16.2) | 16.2 (15.9–16.5) | <.001 |
| Northeast | 17.9 (17.2–18.6) | 16.7 (16.1–17.4) | 15.4 (14.7–16.0) | 15.2 (14.6–15.8) | .02 |
| Midwest | 20.6 (20.0–21.3) | 18.9 (18.3–19.4) | 17.7 (17.1–18.3) | 18.1 (17.6–18.7) | .03 |
| South | 19.8 (19.3–20.4) | 18.6 (18.1–19.1) | 17.3 (16.8–17.8) | 17.8 (17.3–18.4) | .14 |
| West | 14.3 (13.7–14.9) | 13.3 (12.7–13.9) | 12.4 (11.9–13.0) | 12.7(12.1–13.4) | .99 |
| Physical Inactivity | |||||
| Overall | 46.3 (45.9–46.7) | 48.0 (47.6–48.4) | 47.2 (46.8–47.5) | 48.4 (48.0–48.8) | <.001 |
| Northeast | 45.7 (44.8–46.5) | 48.8 (48.0–49.6) | 48.4 (47.5–49.3) | 47.7 (46.8–48.5) | .002 |
| Midwest | 46.9 (46.1–47.6) | 47.9 (47.1–48.6) | 48.1(47.3–48.8) | 48.7(48.1–49.4) | <.001 |
| South | 49.8 (49.1–50.4) | 51.9(51.3–52.5) | 50.0(49.4–50.7) | 52.1 (51.4–52.9) | <.001 |
| West | 40.5 (39.8–41.3) | 41.2 (40.3–42.2) | 40.6 (39.7–41.4) | 42.5(41.5–43.4) | .38 |
| Poor Diet | |||||
| Overall | 91.6 (91.4–91.8) | 91.6 (91.3–91.8) | 91.4 (91.1–91.6) | 88.4 (88.1–88.6) | <.001 |
| Northeast | 91.1 (90.1–91.6) | 91.2 (90.7–91.6) | 91.1(90.6–91.5) | 87.9 (87.3–88.4) | <.001 |
| Midwest | 92.0 (91.6–92.4) | 91.9 (91.5–92.4) | 91.9 (91.4–92.3) | 89.4 (89.0–89.8) | <.001 |
| South | 93.3 (93.0–93.6) | 93.4 (93.1–93.7) | 92.4(92.0–92.8) | 89.4 (89.0–89.9) | <.001 |
| West | 88.8 (88.3–89.3) | 88.5 (87.9–89.1) | 89.4 (88.9–89.9) | 86.2(85.5–86.8) | <.001 |
| Myocardial Infarction/Coronary Heart Disease | |||||
| Overall | 6.8 (6.6–6.9) | 6.7 (6.5–6.8) | 6.3 (6.2–6.5) | 6.1 (6.0–6.3) | .002 |
| Northeast | 6.2 (5.9–6.5) | 6.4 (6.1–6.8) | 5.8 (5.5–6.1) | 5.9 (5.6–6.2) | .99 |
| Midwest | 6.9 (6.6–7.2) | 6.8 (6.5–7.1) | 6.3 (6.1–6.6) | 6.4 (6.2–6.6) | .99 |
| South | 7.5 (7.3–7.8) | 7.3 (7.1–7.6) | 7.2 (6.9–7.5) | 6.8 (6.5–7.1) | .047 |
| West | 5.9 (5.6–6.1) | 5.6 (5.2–5.9) | 5.3 (4.9–5.6) | 4.9 (4.6–5.2) | .007 |
| Stroke | |||||
| Overall | 2.9 (2.8–3.0) | 2.9 (2.8–3.0) | 3.0 (2.9–3.1) | 3.1 (2.9–3.2) | .005 |
| Northeast | 2.3 (2.1–2.4) | 2.6 (2.3–2.8) | 2.5 (2.3–2.7) | 2.5 (2.3–2.8) | .15 |
| Midwest | 3.1 (2.8–3.3) | 2.9 (2.7–3.1) | 3.0 (2.8–3.2) | 3.1 (2.9–3.2) | .89 |
| South | 3.4 (3.2–3.5) | 3.4 (3.2–3.6) | 3.5 (3.3–3.7) | 3.7 (3.4–3.9) | .15 |
| West | 2.6 (2.4–2.7) | 2.4 (2.2–2.6) | 2.5 (2.3–2.7) | 2.5 (2.2–2.7) | .99 |
Age standardized as per 2010 United States Census population proportions.
Adjusted for sex, race, education level, annual household income, health insurance status, and Bonferroni correction for multiple comparisons CI: Confidence Interval.
The prevalence of obesity increased from 29.3% (95%CI: 28.9–29.6%) in 2011 to 31.4% (95%CI: 31.1–31.8%) in 2017 (Ptrend<.001), and this was consistent in all regions (Ptrend<.001 for all). The highest prevalence of obesity was present in the southern and midwestern regions. Physical inactivity increased nationally between 2011 (46.3% [95%CI: 45.9–46.7%]) and 2017 (48.4% [95%CI: 48.0–48.8%]) (Ptrend<.001)(Table 2, Supplementary Figure 2). The northeastern, midwestern, and southern regions showed an increase in physical inactivity (Ptrend<.05 for all). Improvement in the healthy diet was seen nationally, and all of the census regions had a declining prevalence of poor diet (Ptrend<.001 for all). Smoking declined nationally from 18.4% (95%CI: 18.1–18.7%) in 2011 to 16.2% (95%CI: 15.9–16.5%) in 2017. Both the northeastern and midwestern regions showed a decline in smoking (Ptrend<.05 for both). Smoking prevalence was highest in the midwestern region (2017: 18.1% [95%CI: 17.6–18.7%]) and lowest in the western region (2017: 12.7% [95%CI: 12.1–13.4%]).
The self-reported prevalence of coronary heart disease decreased nationally from 6.8% (95%CI: 6.6-6-6.1% (95%CI: 6.0–6.3%) in 2017 (Ptrend=.002) (Table 2, Supplementary Figure 3). The prevalence of coronary heart disease declined in the southern and western regions (Ptrend<.05 for both). The prevalence of coronary heart disease was highest in the southern region (2017: 6.8% [95%CI: 6.5–7.1%]) and the lowest in the western region (2017: 4.9% [95%CI: 4.6–5.2%]). The self-reported stroke prevalence nationally was 2.9% (95%CI: 2.8–3.0%) in 2011 and 3.1% (95%CI: 2.9–3.2%) in 2017 (Ptrend=.005). Stroke prevalence was highest in the southern region (3.7% [95%CI: 3.4–3.9%]) and lowest in northeastern (2017: 2.5% [95%CI: 2.3–2.8%]) and western regions (2017: 2.5% [95%CI: 2.2–2.7%]).
Geographic Distribution of Cardiovascular Risk Factors: 2017
The state-level geographic distribution of cardiovascular risk factors in 2017 is depicted in Figures 1 and Supplementary Figures 4–8. The prevalence of cardiovascular risk factors was concentrated primarily in the southern states, with a relatively lower prevalence in the western states (Supplementary Figures 4–12).
Figure 1. Heatmap of Prevalence of Cardiovascular Risk Factors and Diseases: 2017.
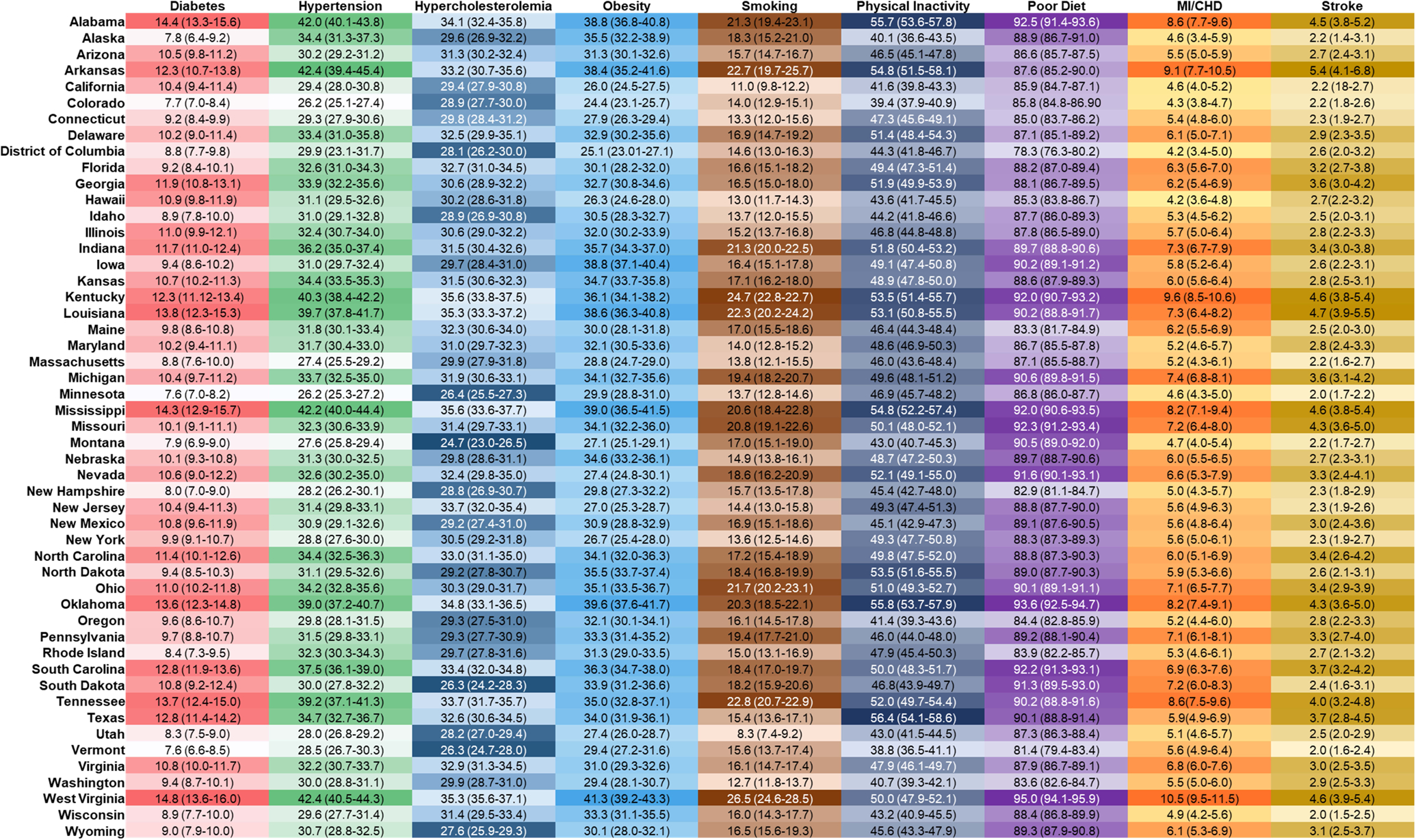
The figure shows the prevalence of cardiovascular risk factors and diseases in the United States. The darker shades indicate higher prevalence, and a lighter shade indicates a lower prevalence.
Geographic Distribution of Cardiovascular Mortality: 2017
In 2017, 859,125 deaths due to cardiovascular causes were identified nationally. The age-adjusted mortality rate for cardiovascular mortality (per 100,000 persons) was highest in the southern region (233.0 [95%CI: 232.2–233.8]), followed by the midwestern (227.7 [95%CI: 226.7–228.7]), northeastern (207.3 [95%CI: 206.3–208.3]), and western (197.5 [95%CI: 19.6–198.5]) regions. The state-level cardiovascular mortality in 2017 has been depicted in Figure 2. The states with a greater prevalence of poor cardiovascular health also had a higher cardiovascular mortality rate (r=0.85; P<.001) (Figure 2). A similar relationship was seen in the sub-groups of sex and race (Supplementary Figure 13–16). The region stratified relationship in the overall population and the subgroups of sex and race are depicted in Supplementary Table 3.
Figure 2. Geographic Distribution of Cardiovascular Mortality and Relationship with Prevalence of Poor Cardiovascular Health: 2017.
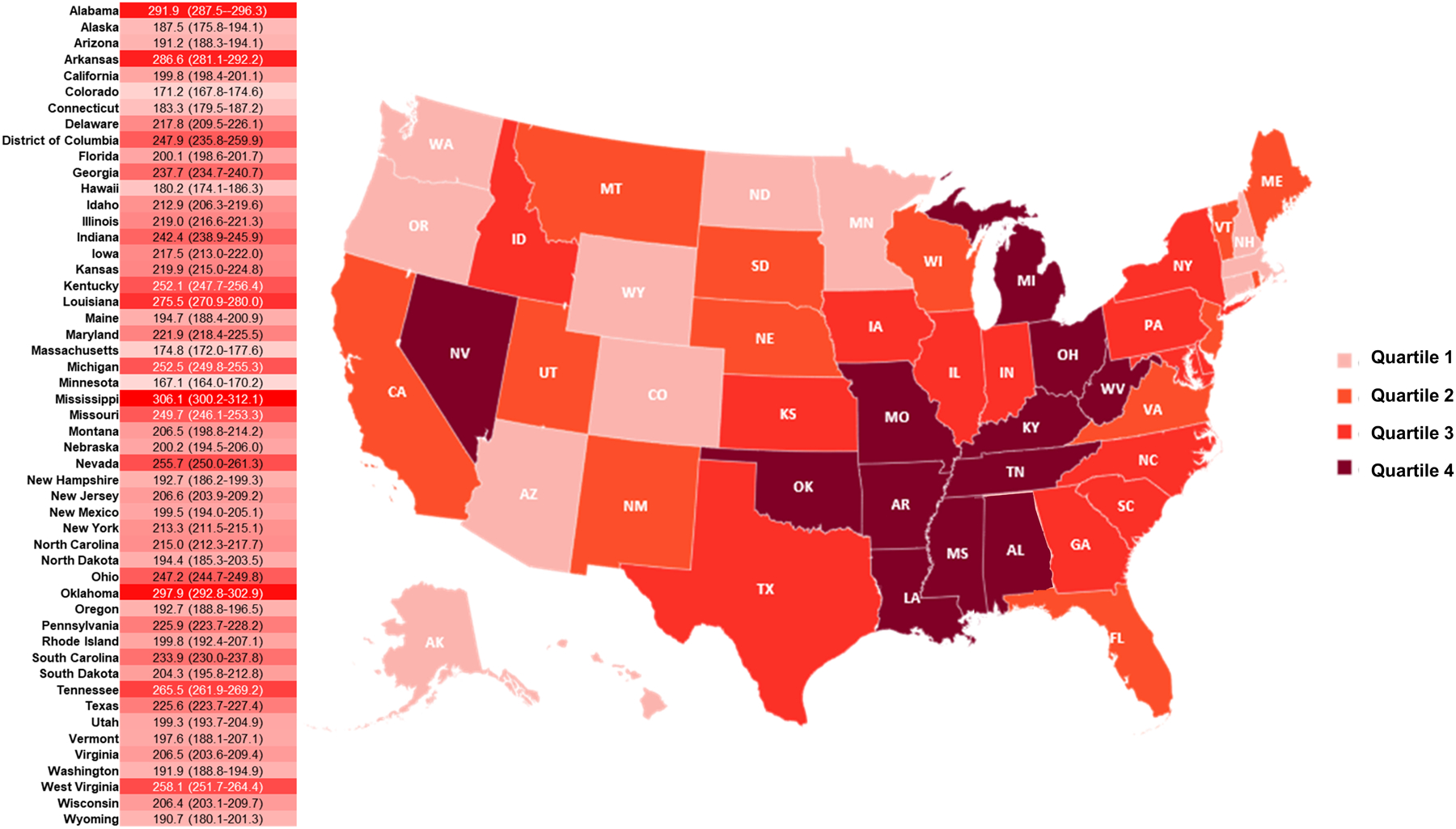
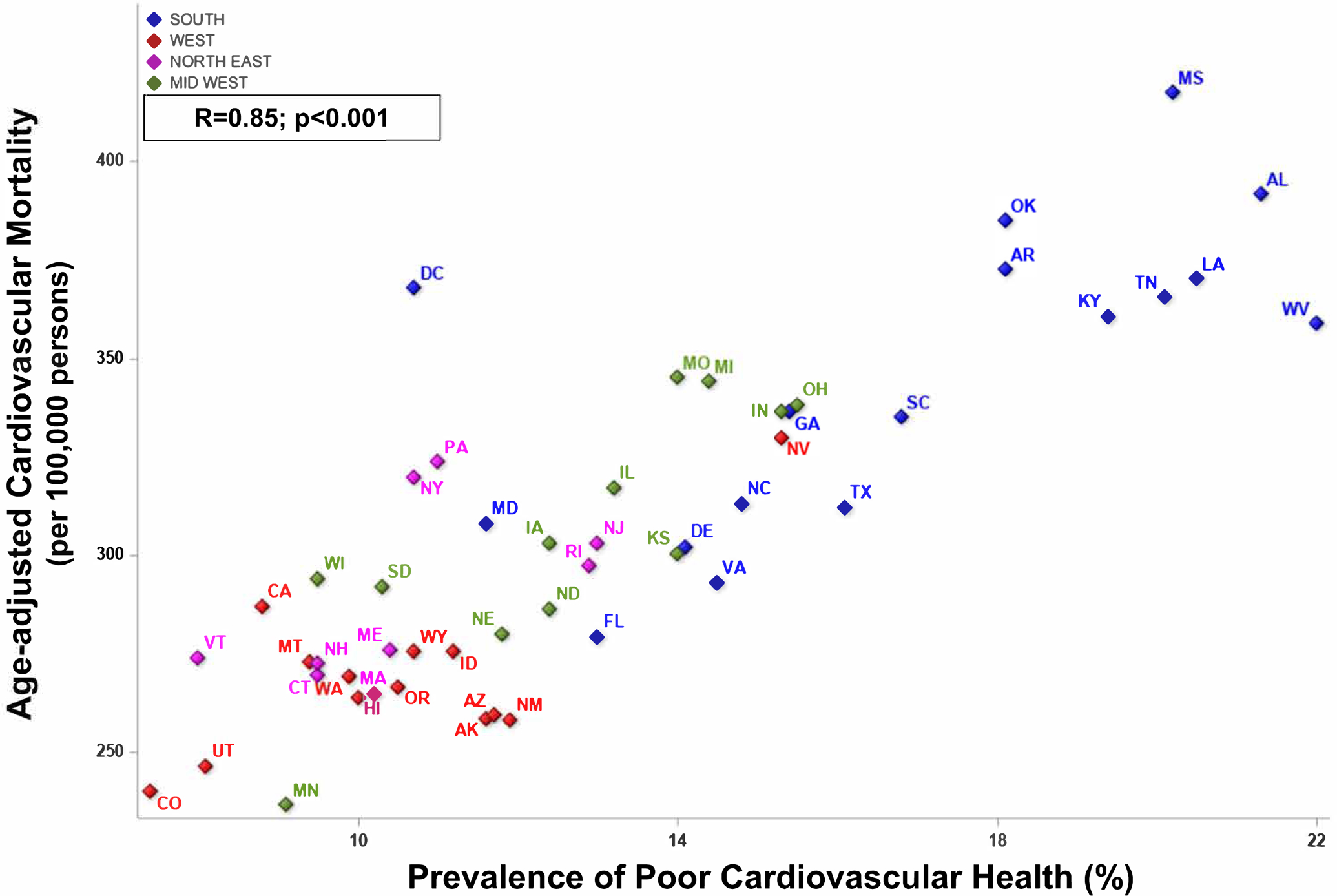
Panel A: Geographic Distribution of Cardiovascular Mortality. The heatmap depicts the age-adjusted cardiovascular mortality rate (per 100,000 persons). The darker shades indicate greater mortality, and lighter shade indicates lower mortality. The map shows the quartiles of cardiovascular mortality across the American states.
Panel B. Relationship of Cardiovascular Mortality and Prevalence of Poor Cardiovascular Health. The diamonds in blue indicate the states in the southern region. The red diamonds represent the states in the western region. The pink diamonds represent the states from the northeastern region. The green diamonds indicate the midwestern region states.
Among subgroups, males had higher mortality (265.5 [95%CI: 264.7–266.3]) than females (181.2 [95%CI: 180.7–181.8]) on a national level (Table 3). This held true across all census regions. Males in the southern US had the highest mortality across the regions (282.1 [95%CI: 280.8–283.5]). Age-adjusted cardiovascular mortality (per 100,000 persons) was highest in Non-Hispanic Blacks (287.9 [95%CI: 286.1–289.6]), followed by Non-Hispanic Whites (221.4 [95%CI: 220.8–221.9]), Non-Hispanic American Indians/Alaska Natives (200.7 [95%CI: 194.7–206.8]), Hispanics (159.0 [95%CI: 157.6–160.3]), and Non-Hispanic Asians/Pacific Islander (128.1 [95%CI: 126.4–129.7]). Non-Hispanic Blacks in the midwestern region had the highest mortality rate among all racial groups (307.3 [95%CI: 255.6–263.6] per 100,000 persons). Non-metropolitan regions had higher mortality rates than metropolitan regions across all census regions. The non-metropolitan (non-core) region in the southern US had the highest age-adjusted cardiovascular mortality (288.7 [95%CI: 285.6–291.7] per 100,000).
Table 3.
Age-Adjusted Cardiovascular Mortality Across the United States: 2017
| Northeast | Midwest | South | West | |
|---|---|---|---|---|
| AAMR (95% CI) | AAMR (95% CI) | AAMR (95% CI) | AAMR (95% CI) | |
| Overall | 207.3 (206.3–208.3) | 227.7 (226.7–228.7) | 233.0 (232.2–233.8) | 197.5 (196.6–198.5) |
| Sex | ||||
| Males | 253.4 (251.3–255.2) | 276.1 (274.3–277.8) | 282.1 (280.8–283.5) | 237.3 (235.7–238.9) |
| Females | 171.1 (169.9–172.3) | 188.2 (186.9–189.4) | 192.2 (191.2–193.1) | 163.4 (162.3–164.5) |
| Race/Ethnicity | ||||
| NH Whites | 208.3 (207.1–209.5) | 224.6 (223.5–225.7) | 233.5 (232.6–234.4) | 207.3 (206.1–208.5) |
| NH Blacks | 259.6 (255.6–263.6) | 307.3 (303.0–311.7) | 289.8 (287.5–292.2) | 291.6 (285.7–297.5) |
| NH Asians/Pacific Islanders | 112.6 (108.8–116.4) | 114.8 (109.2–120.4) | 112.6 (108.8–116.4) | 140.0 (137.6–142.3) |
| NH American Indians/Alaska Natives | 110.9 (94.4–127.4) | 211.3 (195.4–227.1) | 194.8 (184.8–204.8) | 216.9 (207.1–226.6) |
| Hispanics | 148.7 (145.3–152.1) | 126.4 (121.6–131.1) | 163.7 (161.5–165.9) | 163.8 (161.5–166.1) |
| Urbanization | ||||
| Large Central Metro | 211.9 (209.9–213.9) | 235.1 (232.8–237.3) | 217.0 (215.3–218.7) | 196.2 (194.8–197.6) |
| Large Fringe Metro | 198.8 (197.2–200.5) | 214.7 (212.7–216.7) | 209.1 (207.6–210.6) | 188.9 (186.4–191.4) |
| Medium Metro | 206.7 (204.4–209.1) | 227.1 (224.6–229.7) | 228.4 (226.9–230.0) | 201.0 (198.9–203.1) |
| Small Metro | 217.5 (213.1–221.8) | 223.5 (220.7–226.4) | 251.1 (248.5–253.7) | 202.0 (198.8–205.1) |
| Micropolitan (Nonmetro) | 222.5 (218.1–226.8) | 237.4 (234.6–240.1) | 279.8 (277.0–282.7) | 208.2 (204.4–211.9) |
| NonCore (Nonmetro) | 221.8 (215.6–228.1) | 238.6 (235.5–241.7) | 288.7 (285.6–291.7) | 201.0 (195.8–206.2) |
Abbreviations: AAMR: Age-adjusted Mortality Rates; CI: Confidence Interval; NH: Non-Hispanic.
Discussion
We demonstrate numerous important nationwide and regional trends in overall cardiovascular health, cardiovascular risk factors, and cardiovascular mortality in the US. The nationwide CVHI marginally, albeit not clinically significant, during the study period of 2011–2017. There were demonstrable differences of CVHI scores among the four major American geographic regions. Less than one-in-every six individuals in all the regions had ideal cardiovascular health. There was an increasing prevalence of obesity, along with the declining prevalence of dyslipidemia, physical inactivity, coronary heart disease, and smoking. The southern US exhibited the lowest CVHI score and the highest prevalence of cardiovascular risk factors and cardiovascular mortality. This relationship of poor cardiovascular health and higher cardiovascular mortality at the state-level was consistent across the sub-groups of sex and race. Collectively, our data suggest that there were widespread pre-existing geographic disparities in cardiovascular health, which overlaps with the geographic dispersion of cardiovascular mortality.
Cardiovascular health likely improved nationally due to the amalgam of major milestones that have been achieved in the last 20 years. We have previously described declining levels of total cholesterol, LDL, and triglycerides since 2005.9 This was accompanied by increasing statin usage nationally since the release of the 2013 American College of Cardiology/American Heart Association (ACC/AHA) guidelines for lipid management.9 Public smoking bans also led to nationwide declines in smoking prevalence, particularly in young adults.10
There may be alternate explanations for the diverse regional trends in cardiovascular health described in our study. Prior data indicates that even during dramatic nationwide improvements in cardiovascular health, this distribution is unequal. Kanjilal et al. demonstrated that the improvements in cardiovascular health between 1971–2002 were disproportionately lower in subjects from lower socioeconomic strata, especially for smoking and diabetes mellitus.11 Our data reiterates this in the contemporary trends, given that the midwestern and southern US have a lower standard of living and greater income inequality than the northeastern and western regions.12 Regional differences in cardiovascular mortality and cardiovascular risk factors may also be attributed to racial differences. Given the mortality disparity between Caucasian Americans and African-Americans, the higher proportion of African-Americans in the southern US may contribute to the higher cardiovascular mortality in the region.13 Prior evaluation of CVHI from the 2011 BRFSS survey cycle also observed a worse cardiovascular health status in the southern US.7 We advance these findings by suggesting that despite the modest improvements in cardiovascular health, there are persistent disparities between the southern US and other regions even after several years.
Access to healthcare is a major determinant of adequate management of cardiovascular diseases. There are several barriers to providing adequate access to healthcare in the southern and midwestern regions, which includes the number of clinicians per capita and rural setting that may have insufficient public transport to healthcare facilities.14 We previously noted that despite the increasing usage of statins nationwide, statin uptake was lower among high-risk groups such as patients with diabetes mellitus and those with established atherosclerotic cardiovascular disease.9 These clinical sub-groups are more prevalent in the southern US, which is also the site of the stroke,15 heart failure,16 and diabetes belts17. The correlation between the prevalence of poor CVHI and cardiovascular mortality seemed to be weaker in non-Hispanic Blacks compared with non-Hispanic Whites, indicating the role of socioeconomic factors such as health insurance and access to healthcare, especially in the rural and medically underserved regions with a disproportionately higher prevalence of minority populations.18 These findings also strengthen the understanding of race/ethnicity being a primarily social construct,18, 19 which adversely impacts cardiovascular health and associated outcomes.18, 19 The yield of public health interventions such as improving access to healthcare, strengthening health infrastructure, public health information and outreach campaigns, and promotion of heart-healthy lifestyle measures starting at an early age, maybe increased by targeting them to the worse performing geographical regions and among worst-affected communities.
Our data regarding nationwide cardiovascular health are aligned with prior work on this topic. We have recently shown that the American Heart Association’s Life’s Simple 7 score declined in American adults between 2007–2016.20 This was primarily driven by the decline in ideal fasting glucose and obesity scores.20 In contrast, the current investigation examines the prevalence trends of the same cardiovascular risk factors in the BRFSS database and classifies these CVHI components as ‘ideal’ or ‘not ideal,’ unlike Life Simple 7’s multilevel scoring. Poor diet in the BRFSS database showed a large change between 2015 and 2017, which is not concordant with the NHANES Life Simple 7 data, although the diet is evaluated differently. This large change may also be due to increasing awareness about dietary guidelines and adherence to healthy diets.21, 22 Sidney et al. reported a declining prevalence of national cardiovascular mortality from 2001–2014.23 We substantiate the reports of declining national cardiovascular mortality by providing a mechanistic understanding of these trends by identifying the declines in cardiovascular diseases such as smoking, hypercholesterolemia, and coronary heart disease. Our data shows rising levels of obesity, which aligns with prior data from the National Health and Nutrition Examination Survey24 and projected increase in the prevalence of obesity till 2030.25
We acknowledge that our investigation has several limitations. The BRFSS is a cross-sectional survey from which incident measures of the disease cannot be obtained. Moreover, causal inference cannot be made from this design. BRFSS includes self-report data, which are subject to various reporting biases. Despite this, prior evaluations of BRFSS data have reliably estimated the prevalence of risk factors.1, 2, 18, 25–27 The differences in BRFSS and estimation of CVHI have inherent methodological differences in comparison with other nationally representative datasets, and the difference in results from these databases may be attributable to variations in questionnaires, interview techniques, and measurement methods among surveys.28 Additionally, self-reporting of risk factors has inherent limitations such as the lack of awareness about the prevalence of these risk factors especially in those living in regions with poor access to healthcare. Hence, the estimated cardiovascular risk factor burden may be even worse in these regions. We have shown trends by census regions, and we may not have been able to capture the intra-regional and state-level variability in the cardiovascular risk factors.7 Additionally, the significant trends for change in the CVHI score in our investigation may be due to the large study population size and reflect a small improvement in the cardiovascular health across regions. Although these changes are in the right direction, they may not be meaningful in the clinical or public health perspective because of being modest in nature. There are many effect measure modifiers in cardiovascular disease that we are unable to account for using this study design. In particular, the social determinants of health and their relation to the delivery of cardiovascular care warrant further study. The relationship of CVHI and mortality may be prone to ecological fallacy due to non-overlapping populations. Therefore, we were not able to assess whether poor cardiovascular health was predictive of cardiovascular mortality.
Conclusions
There was a small, clinically insignificant improvement in cardiovascular health nationwide, with significant geographic differences in the prevalence of cardiovascular risk factors and mortality. Only one-in-six American adults have ideal cardiovascular health, which is even lower in the southern US. These data should guide tailored approaches to cardiovascular care delivery to address the longstanding geographic disparities in cardiovascular risk factors and disease.
Supplementary Material
Sources of Funding:
This work is supported by the Minority Health & Health Disparities Research Center, National Institute of Minority Health and Health Disparities [U54MD000502], and the National Institutes of Health Mentored-Patient Oriented Research Award [5K23 HL146887-02] to Dr. Pankaj Arora.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Disclosures: None of the authors had any conflicts of interest or financial disclosures to declare.
References
- 1.Pilkerton CS, Singh SS, Bias TK, Frisbee SJ. Changes in Cardiovascular Health in the United States, 2003–2011. J Am Heart Assoc. 2015;4:e001650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Fang J, Yang Q, Hong Y, Loustalot F. Status of cardiovascular health among adult Americans in the 50 States and the District of Columbia, 2009. J Am Heart Assoc. 2012;1:e005371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lanska DJ, Kuller LH. The geography of stroke mortality in the United States and the concept of a stroke belt. Stroke. 1995;26:1145–1149. [DOI] [PubMed] [Google Scholar]
- 4.Casper ML, Wing S, Anda RF, Knowles M, Pollard RA. The shifting stroke belt. Changes in the geographic pattern of stroke mortality in the United States, 1962 to 1988. Stroke. 1995;26:755–760. [DOI] [PubMed] [Google Scholar]
- 5.Ritchey MD, Wall HK, Owens PL, Wright JS. Vital Signs: State-Level Variation in Nonfatal and Fatal Cardiovascular Events Targeted for Prevention by Million Hearts 2022. MMWR Morb Mortal Wkly Rep. 2018;67:974–982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Centers for Disease Control and Prevention. Underlying Cause of Death, 1999–2018 Request. Vol 20202020. [Google Scholar]
- 7.Gebreab SY, Davis SK, Symanzik J, Mensah GA, Gibbons GH, Diez-Roux AV. Geographic variations in cardiovascular health in the United States: contributions of state- and individual-level factors. J Am Heart Assoc. 2015;4:e001673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mendy VL, Vargas R. Trends in major risk factors for cardiovascular disease among adults in the Mississippi Delta region, Mississippi Behavioral Risk Factor Surveillance System, 2001–2010. Prev Chronic Dis. 2015;12:E21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Patel N, Bhargava A, Kalra R, et al. Trends in Lipid, Lipoproteins, and Statin Use Among U.S. Adults: Impact of 2013 Cholesterol Guidelines. J Am Coll Cardiol. 2019;74:2525–2528. [DOI] [PubMed] [Google Scholar]
- 10.Kalra R, Parcha V, Patel N, et al. Increased awareness, inadequate treatment, and poor control of cardiovascular risk factors in American young adults: 2005–2016. Eur J Prev Cardiol. 2020:2047487320905190. [DOI] [PubMed] [Google Scholar]
- 11.Kanjilal S, Gregg EW, Cheng YJ, et al. Socioeconomic status and trends in disparities in 4 major risk factors for cardiovascular disease among US adults, 1971–2002. Arch Intern Med. 2006;166:2348–2355. [DOI] [PubMed] [Google Scholar]
- 12.United States Census Bureau. American Commity Survey Briefs - Household Income: 2018. Vol 20202020. [Google Scholar]
- 13.Mensah GA, Cooper RS, Siega-Riz AM, et al. Reducing Cardiovascular Disparities Through Community-Engaged Implementation Research: A National Heart, Lung, and Blood Institute Workshop Report. Circ Res. 2018;122:213–230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Douthit N, Kiv S, Dwolatzky T, Biswas S. Exposing some important barriers to health care access in the rural USA. Public Health. 2015;129:611–620. [DOI] [PubMed] [Google Scholar]
- 15.Howard G, Howard VJ. Twenty Years of Progress Toward Understanding the Stroke Belt. Stroke. 2020;51:742–750. [DOI] [PubMed] [Google Scholar]
- 16.Mujib M, Zhang Y, Feller MA, Ahmed A. Evidence of a “heart failure belt” in the southeastern United States. Am J Cardiol. 2011;107:935–937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Barker LE, Kirtland KA, Gregg EW, Geiss LS, Thompson TJ. Geographic distribution of diagnosed diabetes in the U.S.: a diabetes belt. Am J Prev Med. 2011;40:434–439. [DOI] [PubMed] [Google Scholar]
- 18.Parcha V, Malla G, Suri SS, et al. Geographic Variation of Racial Disparities in Health and COVID-19 Mortality. Mayo Clin Proc Innov Qual Outcomes. 2020. [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Parcha V, Patel N, Kalra R, Arora G, Arora P. Prevalence, Awareness, Treatment, and Poor Control of Hypertension Among Young American Adults: Race-Stratified Analysis of the National Health and Nutrition Examination Survey. Mayo Clin Proc. 2020;95:1390–1403. [DOI] [PubMed] [Google Scholar]
- 20.Patel N, Kalra R, Bhargava A, Arora G, Arora P. Ideal Cardiovascular Health Among American Adults After the Economic Recession of 2008–2009: Insights from NHANES. Am J Med. 2019;132:1182–1190.e1185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.United States Census Bureau. Research to Improve Data on Race and Ethnicity. Available at: https://www.census.gov/about/our-research/race-ethnicity.html. Accessed on: November 26. 2020.
- 22.United States Department of Health and Human Services. Dietary Guidelines for Americans 2015–2020. Available at: https://health.gov/our-work/food-nutrition/2015-2020-dietary-guidelines/guidelines/. Accessed on: December 3, 2020.
- 23.Sidney S, Quesenberry CP Jr., Jaffe MG, et al. Recent Trends in Cardiovascular Mortality in the United States and Public Health Goals. JAMA Cardiology. 2016;1:594–599. [DOI] [PubMed] [Google Scholar]
- 24.Hales CM, Fryar CD, Carroll MD, Freedman DS, Ogden CL. Trends in Obesity and Severe Obesity Prevalence in US Youth and Adults by Sex and Age, 2007–2008 to 2015–2016. JAMA. 2018;319:1723–1725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ward ZJ, Bleich SN, Cradock AL, et al. Projected U.S. State-Level Prevalence of Adult Obesity and Severe Obesity. New England Journal of Medicine. 2019;381:2440–2450. [DOI] [PubMed] [Google Scholar]
- 26.Ward ZJ, Bleich SN, Cradock AL, et al. Projected U.S. State-Level Prevalence of Adult Obesity and Severe Obesity. N Engl J Med. 2019;381:2440–2450. [DOI] [PubMed] [Google Scholar]
- 27.Stein AD, Lederman RI, Shea S. The Behavioral Risk Factor Surveillance System questionnaire: its reliability in a statewide sample. American Journal of Public Health. 1993;83:1768–1772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Carlson SA, Densmore D, Fulton JE, Yore MM, Kohl HW 3rd. Differences in physical activity prevalence and trends from 3 U.S. surveillance systems: NHIS, NHANES, and BRFSS. J Phys Act Health. 2009;6 Suppl 1:S18–27. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


