Abstract
OBJECTIVES
To estimate COVID-19 infection and outcomes among healthcare workers (HCWs) compared with non-HCWs.
METHODS
A prospective surveillance study was conducted among HCWs and non-HCWs eligible for treatment at a large tertiary care facility in Riyadh between March 1st to November 30th, 2020.
RESULTS
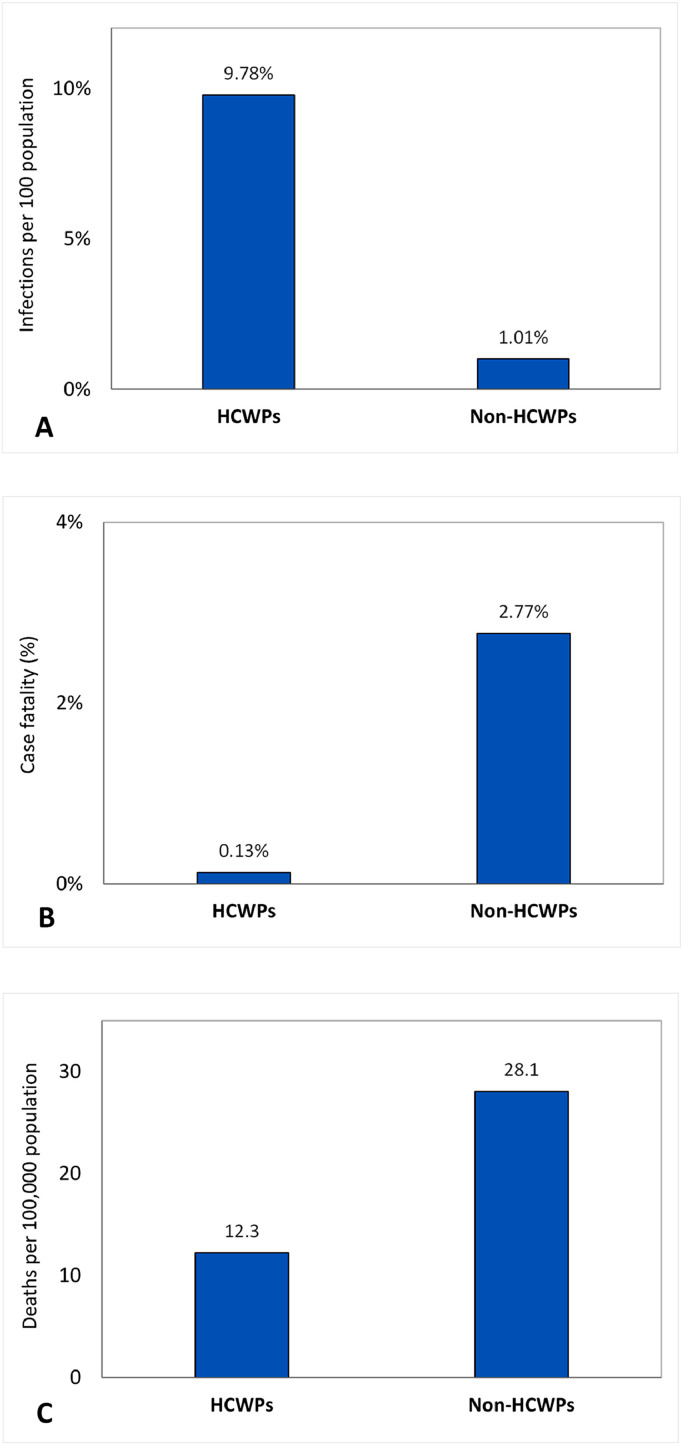
A total 13,219 cases with confirmed COVID-19 have been detected during the study; 1596 (12.1%) HCW patients (HCWPs) and 11623 (87.9%) non-HCWPs. Infection per 100 population was almost ten-fold higher in HCWs compared with non-HCWs (9.78 versus 1.01, p<0.001). The risk of infection in support staff (15.1%) was almost double the risk in other professional groups (p<0.001). Hospitalization (14.1% versus 1.8%, p<0.001), ICU admission (3.0% versus 0.5%, p<0.001), and case fatality (0.13% versus 2.77%, p<0.001) were significantly lower in HCWPs compared with non-HCWPs. The mortality per 100,000 population was significantly lower in HCWs compared with non-HCWs (12.3 and 28.1, p<0.001).
CONCLUSION
HCWs are at ten-fold higher risk of COVID-19 infection but have much better outcomes compared with non-HCWs. More strict infection control measures are still required to protect HCWs, including those who are not involved in direct patient care.
Key words: Coronavirus disease (COVID-19), pandemic, hospital, healthcare, Saudi Arabia
BACKGROUND
Since its first appearance in Wuhan (China) in late 2019, more than 100 million patients were infected with severe acute respiratory syndrome coronavirus number 2 (SARS-CoV-2) with more than 2.25 million related deaths by end of January 2021 (World Health Organization, 2020). Nevertheless, these numbers are considerably underestimated and the actual number of infected persons is probably 3 to 20 times higher than the reported numbers (Wu et al., 2020). This makes the current coronavirus disease (COVID-19) pandemic the largest pandemic in the twenty first century and the largest ever pandemic caused by one of the coronaviruses (Ashour et al., 2020).
The COVID-19 pandemic is considered an unprecedented physical and mental challenge for healthcare workers (HCWs) around the world (Salazar de Pablo et al., 2020, Shaukat et al., 2020). HCWs being at the frontline of treating patients with confirmed COVID-19 are at higher risk of exposure than the general population (Ali et al., 2020, Nguyen et al., 2020, Wei et al., 2020, Zheng et al., 2020). However, being more healthy they are expected to have better outcome in terms of hospitalization and mortality compared with non-HCWs (Misra-Hebert et al., 2020, Wei et al., 2020, Zheng et al., 2020). Infected HCWs represent a risk for their families, their fellow HCWs, and hospitalized patients (Shah et al., 2020, Souadka et al., 2020). The risk of exposure, risk of introducing infection to others, long working hours, and perceived stigma from family members and society can be manifested with a number of psychological morbidities including poor sleep quality, stress, post-traumatic stress symptoms, anxiety, and depression (Cabarkapa et al., 2020, Krishnamoorthy et al., 2020, Teo et al., 2020).
COVID-19 risk of infection and mortality among HCWs has not been the focus of COVID-19 research in Saudi Arabia. Quantifying such risk is essential for planning additional infection control measures to protect HCWs. Additionally, the finding may give indirect assessment of the currently implemented protective measures at the healthcare setting. The objective of the current study was to estimate COVID-19 infection and outcomes among HCWs compared with non-HCWs in Saudi Arabia.
METHODS
Setting
The current study was conducted at King Abdulaziz Medical City at Riyadh (KAMC-R), Saudi Arabia, which is an approximately 1488-bed tertiary care facility, composed of two hospitals. The facility provides healthcare services for almost 1.15 million eligible Saudi National Guard soldiers, employees and their families. The facility had a total 172 (11.6%) intensive care beds and 168 (11.3%) emergency beds. According to local hospital statistics for 2019, KAMC-R received 55,025 admissions and served 863,073 outpatient clinic visits. The facility is served by 16317 HCWs, including 2,451 physicians, 5,483 nurses, and 3101 other clinical HCWs, as well as 5,282 administrative and support jobs that involve no direct patient care.
Study design
The current study design was a prospective surveillance study for all COVID-19 confirmed HCW patients (HCWPs) and non-HCW patients (non-HCWPs) at KAMC-R during the pandemic period, March 1st to November 30th, 2020.
Definitions
The case definition used was based on the definition released by the Saudi Ministry of Health and the Saudi Center for Disease Prevention and Control at the beginning of the pandemic (Saudi Center for Disease Prevention and Control, 2020). Only confirmed cases who had a positive RT-PCR test for COVID-19 were included in the current study. The study outcomes included COVID-19 infection and related outcomes including hospitalization, ICU admission, case fatality, and mortality.
Case finding
All HCWPs and non-HCWPs attending KAMC-R during the study period and who met the suspected COVID-19 definition or as part of contact tracing had their nasopharyngeal swabs examined using RT-PCR test for COVID-19. Suspected COVID-19 definition included those with acute respiratory illness with epidemiologic link (contact with a confirmed case, working in a healthcare facility, or recent travel to an infected area) or severe acute respiratory illness without epidemiologic link [10]. There was no difference in the strategy of testing for HCWPs and non-HCWPs. The probable source of transmission (hospital versus community) was ascertained as reported by the HCWPs and non-HCWPs.
Infection control measures
Early in the outbreak and even before the diagnosis of first case in the hospital, infection control measures were strictly enforced including hand hygiene, environmental cleaning, and wearing personal protective equipment (PPE). Additionally, universal masking and measuring body temperature before starting the shift were stipulated. Several measures were done to reduce transmission and exposure to COVID-19 within the hospital, including triage, nasopharyngeal swabbing for all new admissions, dedicated COVID-19 units, contact tracing clinic, and changes in patient flow at each stage of care.
Source of data
Numerator data include all those who tested positive for COVID-19, irrespective of hospital admission. Numerator data were collected through active surveillance using a structured data collection tool. These included HCWs status, demographic data, disease course, and study outcomes. Denominator data (for infection and mortality) were obtained from the most recent hospital statistics. These include the number of HCWs working at KAMC-R by professional category and nationality as well as the number of non-HCW people eligible for treatment at KAMC-R.
Statistical methods
Epidemic curves for HCWPs and non-HCWPs at KAMC-R were created. Infection and outcomes parameters were compared between groups using Chi-square. All P-values were two-tailed. P-value <0.05 was considered as significant. SPSS (Version 22.0. Armonk, NY: IBM Corp) was used for all statistical analyses.
RESULTS
During the 9-month period of the study, a total 13,219 cases with confirmed COVID-19 were detected after 54622 RT-PCR tests done at the KAMC-R between March and November 2020. As shown in Table 1 , these included 1596 (12.1%) HCWPs and 11623 (87.9%) non-HCWPs. The mean age was slightly but significantly higher among HCWPs compared with non-HCWPs (38.0±10.0 versus 36.1±20.4 years, p<0.001). However, those above the age of 45 years were less frequent in HCWPs compared with non-HCWPs (22.6% versus 31.0%, p<0.001). The majority (57%) of confirmed cases were males, with no significant differences between HCWPs and non-HCWPs. Non-Saudi people represented 58.4% of HCWs but only 9.4% of the non-HCWPs (p<0.001). Symptomatic disease was more common in HCWPs compared with non-HCWPs (78.0% versus 56.9%, p<0.001). Hospital transmission represented the source of infection in the majority (48.0%) of HCWs while community transmission represented the source of infection in the majority (64.8%) of the non-HCWPs (p<0.001). Hospitalization (14.1% versus 1.8%, p<0.001), ICU admission (3.0% versus 0.5%, p<0.001), and case fatality (0.1% versus 2.8%, p<0.001) were significantly less frequent in HCWPs compared with non-HCWPs. The average number of tests per positive case was higher in HCWPs than non-HCWPs (5.1 versus 4.0 tests, p<0.001) and HCWPs were less likely to have their positive results after the first test done (87.8% versus 97.7%, p<0.001). After adjusting for age, gender, nationality, and number of tests done, the higher risk of hospital and ICU admission among non-HCWPs compared with HCWPs increased more than two or three times, respectively. However, the risk of death remained essentially the same (Table 2 ).
Table 1.
Comparisons of demographic characteristics and disease course between HCWPs and non-HCWPs examined at KAMC-R, March to November 2020
| HCWPs (N=1596) | Non-HCWPs (N=11623) | Total (N=13219) | p-value | |
|---|---|---|---|---|
| Age (years) | ||||
| Mean±SD | 38.0±10.0 | 36.1±20.4 | 36.3±19.5 | <0.001 |
| <30 | 348 (22.0%) | 4774 (42.2%) | 5122 (39.7%) | <0.001 |
| 30-45 | 878 (55.5%) | 3028 (26.8%) | 3906 (30.3%) | |
| >45 | 357 (22.6%) | 3503 (31.0%) | 3860 (30.0%) | |
| Gender | ||||
| Male | 902 (57.0%) | 6630 (57.2%) | 7532 (57.1%) | 0.898 |
| Female | 681 (43.0%) | 4971 (42.8%) | 5652 (42.9%) | |
| Nationality | ||||
| Saudi Arabia | 658 (41.6%) | 10088 (90.6%) | 10746 (84.5%) | <0.001 |
| Non-Saudi | 923 (58.4%) | 1041 (9.4%) | 1964 (15.5%) | |
| Symptoms | ||||
| Asymptomatic | 327 (22.0%) | 4682 (43.1%) | 5009 (40.6%) | <0.001 |
| Symptomatic | 1159 (78.0%) | 6181 (56.9%) | 7340 (59.4%) | |
| Probable source of infection | ||||
| Community-acquired | 499 (31.3%) | 8074 (69.5%) | 8573 (64.8%) | <0.001 |
| Hospital-acquired | 766 (48.0%) | 73 (0.6%) | 839 (6.3%) | |
| Unknown | 331 (20.7%) | 3477 (29.9%) | 3808 (28.8%) | |
| Hospitalization | ||||
| No | 1567 (98.2%) | 9983 (85.9%) | 11550 (87.4%) | <0.001 |
| Yes | 28 (1.8%) | 1640 (14.1%) | 1668 (12.6%) | |
| ICU admission | ||||
| No | 1588 (99.5%) | 11274 (97.0%) | 12862 (97.3%) | <0.001 |
| Yes | 8 (0.5%) | 350 (3.0%) | 358 (2.7%) | |
| Death | ||||
| No | 1594 (99.9%) | 11301 (97.2%) | 12895 (97.5%) | <0.001 |
| Yes | 2 (0.1%) | 322 (2.8%) | 324 (2.5%) | |
| Testing | ||||
| Number of tests done | 8130 | 46492 | 54622 | <0.001 |
| Tests per positive | 5.1 | 4.0 | 4.1 | |
| Order of positive result | ||||
| First | 1401 (87.8%) | 11358 (97.7%) | 12759 (96.5%) | <0.001 |
| Second or more | 194 (12.2%) | 265 (2.3%) | 459 (3.5%) |
HCWPs, healthcare worker patients; non-HCWPs, non-healthcare worker patients; KAMC-R, KAMC-R, King Abdulaziz Medical City at Riyadh
Table 2.
Adjusted outcomes in non-HCWPs compared with HCWPs working in KAMC-R, March to November 2020
| Odds ratio | 95% confidence |
p-value | ||
|---|---|---|---|---|
| Lower limit | Upper limit | |||
| Hospital admission | ||||
| Unadjusted | 8.3 | 5.8 | 11.9 | <0.001 |
| Adjusted | 17.1 | 11.7 | 25.0 | <0.001 |
| ICU admission | ||||
| Unadjusted | 6.1 | 3.0 | 12.4 | <0.001 |
| Adjusted | 19.4 | 9.2 | 41.0 | <0.001 |
| Death | ||||
| Unadjusted | 22.7 | 5.7 | 91.3 | <0.001 |
| Adjusted | 20.5 | 5.0 | 84.3 | <0.001 |
Abbreviations as in Table 1. *Adjusted for age, gender, nationality, and number of tests.
As shown in Figure 1 , the infections per 100 population were almost ten-fold higher in HCWs compared with non-HCWs (9.78 versus 1.01, p<0.001). The mortality per 100,000 population was significantly lower in HCWPs compared with non-HCWPs (12.3 and 28.1, p<0.001). As shown in Table 3 , the infection risk in support staff (15.1%) was almost double the risk in other professional groups (p<0.001) and was significantly higher in non-Saudi compared with Saudi HCWPs (11.6% versus 7.9%, p<0.001).
Figure 1.
Infection (A), case fatality (B), and mortality (C) of HCWPs compared to non-HCWPs at KAMC-R
Note: Abbreviations as in Table 1.
Table 3.
Infection* rates among HCWs working in KAMC-R, March to November 2020
| All HCWs | COVID-19 confirmed HCWPs |
p-value | ||||
|---|---|---|---|---|---|---|
| Number | Percentage | Number | Percentage | Infection* | ||
| Professional category | ||||||
| Nurse | 5483 | 33.6% | 385 | 24.1% | 7.0% | <0.001 |
| Physician | 2451 | 15.0% | 187 | 11.7% | 7.6% | |
| Other HCW | 3101 | 19.0% | 227 | 14.2% | 7.3% | |
| Support staff | 5282 | 32.4% | 797 | 49.9% | 15.1% | |
| Total | 16317 | 100.0% | 1596 | 100.0% | 9.8% | |
| Nationality | ||||||
| Saudi Arabia | 8330 | 51.1% | 658 | 41.6% | 7.9% | <0.001 |
| Non-Saudi | 7987 | 48.9% | 923 | 58.4% | 11.6% | |
| Total | 16317 | 100.0% | 1581 | 100.0% | 9.7% | |
Abbreviations as in Table 1. *Infection rate refer to the number of COVID-19 confirmed HCWs per 100 HCWs working in KAMC-R
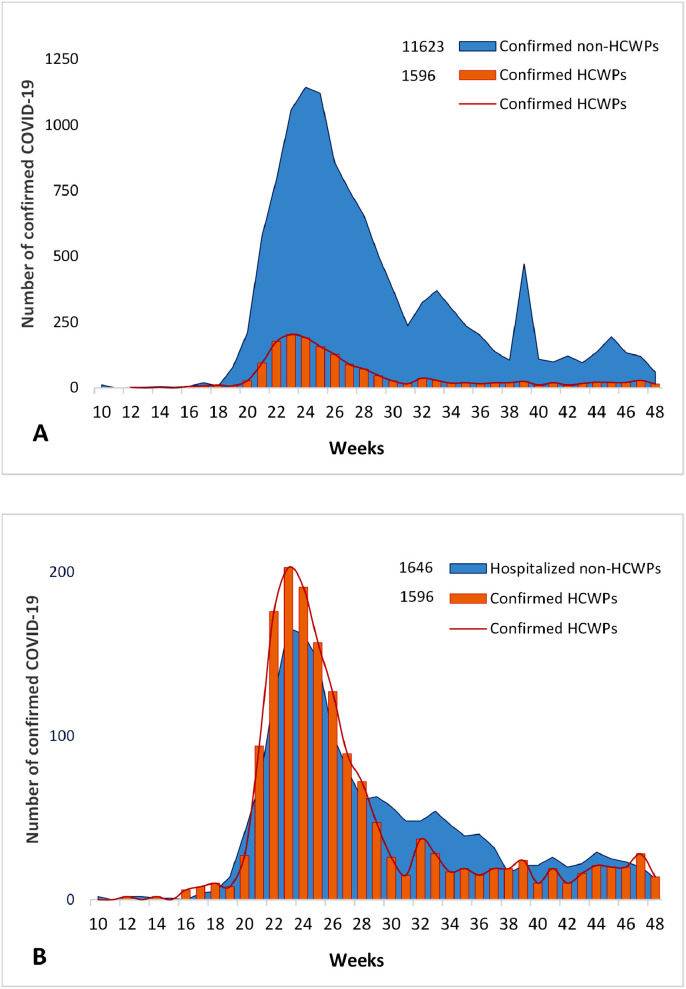
As shown in Figure 2 , the epidemic curve of confirmed COVID-19 infection in HCWPs was very similar to the curves of infected and hospitalized non-HCWPs, with all showing peaks at the 23rd week (early June 2020). Obviously, the HCWPs curve was much smaller compared with that of infected non-HCWPs but outnumbered that of the hospitalized non-HCWPs.
Figure 2.
Epidemic curve of confirmed COVID-19 infection in HCWPs compared with all (A) and hospitalized (B) non-HCWPs at KAMC-R
Note: Abbreviations as in Table 1.
DISCUSSION
The current study estimated the prevalence of COVID-19 infection at 10% among HCWs working at a large tertiary care facility in Saudi Arabia during the first 9 months of the pandemic. Comparing the current findings is challenging due to wide variability between studies estimating the prevalence of COVID-19 infection among HCWs (Chou et al., 2020, Sahu et al., 2020). The variability is probably caused by differences in inclusion criteria, testing type and policy, presence or absence of symptoms, period covered, implemented infection control measures, and finally real differences in COVID-19 risk in different parts of the world (Chou et al., 2021). For example, a meta-analysis that covered the first 4 months of 2020 confirmed wide variability between countries; 4.2% in China, 9% in Italy, and 17.8% in USA (Sahu et al., 2020). Nevertheless, the current infection prevalence is generally consistent with those reported in meta-analysis studies (Gomez-Ochoa et al., 2020, Sahu et al., 2020). For example, a meta-analysis of 97 studies done among HCWs working in different countries within the first 6 months of the pandemic estimated the prevalence of infection at 11% using PCR and 7% using antibodies testing (Gomez-Ochoa et al., 2020). In the same study, the prevalence was 8% in the PCR studies that included all HCWs and 19% in the PCR studies that included only symptomatic HCWs (Gomez-Ochoa et al., 2020). On the other hand, another meta-analysis covering the same period estimated the percentage of positivity among HCWs at a very high level (51.7%)(Gholami et al., 2021). Clearly, the report suffered from considerable methodological problems by including many fewer studies (N=30) and including studies that examined only HCWs with positive COVID-19 testing. It should be noted that the current and previous estimates of prevalence of COVID-19 infection are probably underestimated. Most COVID-19 testing is initiated after symptoms, missing many asymptomatic infections. Additionally, conservative testing policy and limited availability of tests in some countries can add to the underestimation.
The current findings showed a ten-fold higher risk of COVID-19 infection among HCWs at a large tertiary care facility compared with the patient population eligible for treatment at the same facility. Large studies that included data for both HCWs and non-HCWs consistently showed a higher risk of COVID-19 infection among HCWs, ranging from 1.4 to 12 times (Misra-Hebert et al., 2020, Nguyen et al., 2020, Wei et al., 2020, Zheng et al., 2020). For example, in a large study that was done in the USA and UK between February and March 2020 including more than two million community individuals and close to 100 thousand frontline HCWs, it was found the likelihood of testing positive for COVID-19 was 3•96% in HCWs compared with 0.33% in community residents (Nguyen et al., 2020). Previous studies showed that the factors associated with higher risk of COVID-19 infection in the healthcare setting may include unprotected exposure, inappropriate use or reuse of PPEs, inadequate hand hygiene, higher-risk care practices, higher-risk departments, and long working hours (Chou et al., 2020, Shaukat et al., 2020). Similar to previous studies, HCWs in the current study reported higher hospital source of infection, which is probably related to exposure to infected HCWs and non-HCWs (Ali et al., 2020, Chou et al., 2020, Shaukat et al., 2020). This was supported by the similar epidemic curves of HCWPs and non-HCWPs at KAMC-R (Figure 2). However, the higher infection risk among support staff in the current study who have no direct patient care role may point to the importance of hospital environment and community exposure (Al-Maani et al., 2021). Similarly, support staff in Oman had the highest seroprevalence among all HCWPs, which was mainly attributed to community sources (Al-Maani et al., 2021). Additionally, the lower perceived risk in support staff may have weakened their compliance with infection control measures. It should be noted that the observed higher risk of COVID-19 infection among HCWs in this and previous studies is probably overestimated. The difference in access to testing and awareness of disease symptomatology may have inflated the risk in HCWs and underestimated the risk in non-HCWs. However, the inflation in the current study should be minimal due to similar testing policy for HCWPs and non-HCWPs, the small difference in the number of tests per positive HCWPs and non-HCWPs observed in the current study and the liberal free testing policy in Saudi Arabia in general (Adly et al., 2020, Saudi Ministry of Health, 2020).
Unlike infection, HCWPs in the current study had 17-fold lower hospitalization, 19-fold lower ICU admission, and 21-fold lower case fatality compared with the non-HCWPs treated at the same facility. Similarly, previous studies showed much better outcomes in HCWs but with smaller magnitude than observed in the current study. For example, previous studies showed between 8- and 13-fold lower case fatality in HCWs (CDC COVID-19 Response Team, 2020, Shah et al., 2020, Wei et al., 2020, Zheng et al., 2020). Although very limited, previous data showed double risk of hospitalization and ICU admission in non-HCWs compared with HCWs (Misra-Hebert et al., 2020). HCWs in the current study had approximately 55% lower mortality compared with the population eligible for treatment at the same facility. We could not identify any mortality studies to compare, probably due to difficulty of obtaining the catchment population (denominator). Interestingly, the difference in mortality between HCWs and non-HCWs was much reduced compared with case fatality, probably due to the higher infection rate. The better outcome among HCWs can probably be explained by the relatively younger age, lower comorbidity, better awareness, and earlier access to treatment compared with non-HCWs (Gholami et al., 2021).
The current study is considered the first local study to estimate COVID-19 infection and outcomes among HCWs. The presence of a defined eligible population for our facility enabled us to compare the risk of infection and mortality among HCWs relative to non-HCWs. Additionally, the study had a relatively larger sample size and longer duration covered compared with many studies worldwide. Nevertheless, lack of stratification of denominator data by age, gender, and nationality did not allow for calculation/adjustment of respective infection and mortality rates. Despite being a large tertiary care facility composed of two hospitals, the findings should be generalized with caution to Saudi hospitals. The higher risk of infection in HCWs was probably inflated due to difference in access to testing and awareness of disease symptomatology. However, this is an inherent bias in all similar studies and unlikely to affect the comparison of current finding.
In conclusion, we are reporting a ten-fold higher risk of COVID-19 infection among HCWs at a large tertiary care facility compared with non-HCWs. The higher risk of infection cannot be fully explained by direct patient care. Unlike infection, HCWPs in the current study had several-fold lower hospitalization, ICU admission, and case fatality compared with the non-HCWPs treated at the same facility. The higher risk of COVID-19 infection among HCWs may indicate that more strict infection control measures are still required at healthcare settings. The higher risk among support staff may indicate that these measures should be enforced universally, irrespective of direct patient care.
Contributions
Majid Alshamrani: Idea, literature search and writing
Aiman El-Saed: analysis, literature search and writing
Mohammed Al Zunitan: Critical review and literature search
Rawabi Almulhem: Critical review and literature search
Saad Almohrij: Critical review and literature search
Declaration of Competing Interests
The authors declare no conflicts of interest.
Acknowledgments
ACKNOWLEDGEMENT
We acknowledge the help of all members of the infection control department at KAMC-R, specially Muayed Matalqah, and Irma Trofeo.
Ethical approval
Ethical approval was obtained from the IRB of King Abdullah International Medical Research Center
Funding Source
Minimal fund was obtained from King Abdullah International Medical Research Center (RC20/563/R) to cover data collection and entry.
References
- Adly HM, AlJahdali IA, Garout MA, Khafagy AA, Saati AA, Saleh SAK. Correlation of COVID-19 Pandemic with Healthcare System Response and Prevention Measures in Saudi Arabia. Int J Environ Res Public Health. 2020;17(18) doi: 10.3390/ijerph17186666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Al-Maani A, Al Wahaibi A, Al-Sooti J, Al Abri B, Al Shukri I, AlRisi E, et al. The role of supporting services in driving SARS-CoV-2 transmission within healthcare settings: A multicenter seroprevalence study. Int J Infect Dis. 2021;107:257–263. doi: 10.1016/j.ijid.2021.04.071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ali S, Noreen S, Farooq I, Bugshan A, Vohra F. Risk Assessment of Healthcare Workers at the Frontline against COVID-19. Pak J Med Sci. 2020;36(COVID19-S4):S99–S103. doi: 10.12669/pjms.36.COVID19-S4.2790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ashour HM, Elkhatib WF, Rahman MM, Elshabrawy HA. Insights into the Recent 2019 Novel Coronavirus (SARS-CoV-2) in Light of Past Human Coronavirus Outbreaks. Pathogens. 2020;9(3):186. doi: 10.3390/pathogens9030186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cabarkapa S, Nadjidai SE, Murgier J, Ng CH. The psychological impact of COVID-19 and other viral epidemics on frontline healthcare workers and ways to address it: A rapid systematic review. Brain Behav Immun Health. 2020;8 doi: 10.1016/j.bbih.2020.100144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- CDC COVID-19 Response Team. Characteristics of Health Care Personnel with COVID-19 - United States, February 12-April 9, 2020. MMWR Morbidity and mortality weekly report 2020;69(15):477-81. [DOI] [PMC free article] [PubMed]
- Chou R, Dana T, Buckley DI, Selph S, Fu R, Totten AM. Epidemiology of and Risk Factors for Coronavirus Infection in Health Care Workers: A Living Rapid Review. Ann Intern Med. 2020;173(2):120–136. doi: 10.7326/M20-1632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chou R, Dana T, Selph S, Totten AM, Buckley DI, Fu R. Update Alert 6: Epidemiology of and Risk Factors for Coronavirus Infection in Health Care Workers. Ann Intern Med. 2021;174(1):W18–Ww9. doi: 10.7326/L20-1323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gholami M, Fawad I, Shadan S, Rowaiee R, Ghanem H, Hassan Khamis A, et al. COVID-19 and healthcare workers: A systematic review and meta-analysis. International Journal of Infectious Diseases. 2021;104:335–346. doi: 10.1016/j.ijid.2021.01.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gomez-Ochoa SA, Franco OH, Rojas LZ, Raguindin PF, Roa-Diaz ZM, Wyssmann BM, et al. COVID-19 in Healthcare Workers: A Living Systematic Review and Meta-analysis of Prevalence, Risk Factors, Clinical Characteristics, and Outcomes. Am J Epidemiol. 2020 doi: 10.1093/aje/kwaa191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krishnamoorthy Y, Nagarajan R, Saya GK, Menon V. Prevalence of psychological morbidities among general population, healthcare workers and COVID-19 patients amidst the COVID-19 pandemic: A systematic review and meta-analysis. Psychiatry Res. 2020;293 doi: 10.1016/j.psychres.2020.113382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Misra-Hebert AD, Jehi L, Ji X, Nowacki AS, Gordon S, Terpeluk P, et al. Impact of the COVID-19 Pandemic on Healthcare Workers' Risk of Infection and Outcomes in a Large, Integrated Health System. J Gen Intern Med. 2020 doi: 10.1007/s11606-020-06171-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nguyen LH, Drew DA, Joshi AD, Guo CG, Ma W, Mehta RS, et al. 2020. Risk of COVID-19 among frontline healthcare workers and the general community: a prospective cohort study. medRxiv. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sahu AK, Amrithanand VT, Mathew R, Aggarwal P, Nayer J, Bhoi S. COVID-19 in health care workers - A systematic review and meta-analysis. Am J Emerg Med. 2020;38(9):1727–1731. doi: 10.1016/j.ajem.2020.05.113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salazar de Pablo G, Vaquerizo-Serrano J, Catalan A, Arango C, Moreno C, Ferre F, et al. Impact of coronavirus syndromes on physical and mental health of health care workers: Systematic review and meta-analysis. J Affect Disord. 2020;275:48–57. doi: 10.1016/j.jad.2020.06.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saudi Center for Disease Prevention and Control . 2020. Quick Guide to COVID-19 Surveillance Case Definitions and Disposition. 2 April 2020.https://covid19.cdc.gov.sa/professionals-health-workers/quick-guide-to-covid-19-surveillance-case-definitions-and-disposition/ URL. (Last accessed February 1, 2021) [Google Scholar]
- Saudi Ministry of Health . 2020. MOH COVID-19 dashboard.https://covid19.moh.gov.sa/ URL. Last accessed February 1, 2021. [Google Scholar]
- Shah ASV, Wood R, Gribben C, Caldwell D, Bishop J, Weir A, et al. Risk of hospital admission with coronavirus disease 2019 in healthcare workers and their households: nationwide linkage cohort study. BMJ. 2020;371:m3582. doi: 10.1136/bmj.m3582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shaukat N, Ali DM, Razzak J. Physical and mental health impacts of COVID-19 on healthcare workers: a scoping review. Int J Emerg Med. 2020;13(1):40. doi: 10.1186/s12245-020-00299-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Souadka A, Essangri H, Benkabbou A, Amrani L, Majbar MA. COVID-19 and Healthcare worker's families: behind the scenes of frontline response. EClinicalMedicine. 2020:23. doi: 10.1016/j.eclinm.2020.100373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teo WZY, Soo YE, Yip C, Lizhen O, Chun-Tsu L. The psychological impact of COVID-19 on 'hidden' frontline healthcare workers. Int J Soc Psychiatry. 2020 doi: 10.1177/0020764020950772. 20764020950772. [DOI] [PubMed] [Google Scholar]
- Wei JT, Liu ZD, Fan ZW, Zhao L, Cao WC. Epidemiology of and Risk Factors for COVID-19 Infection among Health Care Workers: A Multi-Centre Comparative Study. Int J Environ Res Public Health. 2020;17(19) doi: 10.3390/ijerph17197149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization . 2020. WHO Coronavirus Disease (COVID-19) Dashboard. Situation by Country, Territory & Area.https://covid19.who.int/table URL. (Last accessed February 1, 2021) [Google Scholar]
- Wu SL, Mertens AN, Crider YS, Nguyen A, Pokpongkiat NN, Djajadi S, et al. Substantial underestimation of SARS-CoV-2 infection in the United States. Nature Communications. 2020;11(1):4507. doi: 10.1038/s41467-020-18272-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zheng L, Wang X, Zhou C, Liu Q, Li S, Sun Q, et al. Analysis of the Infection Status of Healthcare Workers in Wuhan During the COVID-19 Outbreak: A Cross-sectional Study. Clinical Infectious Diseases. 2020;71(16):2109–2113. doi: 10.1093/cid/ciaa588. [DOI] [PMC free article] [PubMed] [Google Scholar]