Abstract
Background
Masking, which is known to decrease the transmission of respiratory viruses, was not widely practiced in the United States until the coronavirus disease 2019 (COVID-19) pandemic. This provides a natural experiment to determine whether the percentage of community masking was associated with decreases in emergency department (ED) visits due to non-COVID viral illnesses (NCVIs) and related respiratory conditions.
Methods
In this observational study of ED encounters in a 11-hospital system in Maryland during 2019-2020, year-on-year ratios for all complaints were calculated to account for “lockdowns” and the global drop in ED visits due to the pandemic. Encounters for specific complaints were identified using the International Classification of Diseases, version 10. Encounters with a positive COVID test were excluded. Linear regression was used to determine the association of publicly available masking data with ED visits for NCVI and exacerbations of asthma and chronic obstructive pulmonary disease (COPD), after adjusting for patient age, sex, and medical history.
Results
There were 285,967 and 252,598 ED visits across the hospital system in 2019 and 2020, respectively. There was a trend toward an association between the year-on-year ratio for all ED visits and the Maryland stay-at-home order (parameter estimate = -0.0804, P = .10). A 10% percent increase in the prevalence of community masking was associated with a 17.0%, 8.8%, and 9.4% decrease in ED visits for NCVI and exacerbations of asthma exacerbations and chronic obstructive pulmonary disease, respectively (P < .001 for all).
Conclusions
Increasing the prevalence of masking is associated with a decrease in ED visits for viral illnesses and exacerbations of asthma and COPD. These findings may be valuable for future public health responses, particularly in future pandemics with respiratory transmission or in severe influenza seasons.
Keywords: COVID, Emergency medicine, Epidemiology, Public health
Clinical Significance.
-
•
The 2020 influenza season in the United States was the mildest in decades, likely due to community masking for coronavirus disease 2019 (COVID-19).
-
•
Community masking was associated with decreased visits to the emergency department for non-COVID viral illnesses and exacerbations of asthma and chronic obstructive pulmonary disorder (COPD).
-
•
Seasonal variations in emergency department utilization for respiratory conditions may be mitigated by promoting masking among the general populace.
Alt-text: Unlabelled box
Introduction
Emergency departments (EDs) in the United States have experienced annual winter surges in visits for viral illnesses and exacerbations of asthma and chronic obstructive pulmonary disease (COPD) over the last decade.1 Viral illnesses are known to trigger exacerbations of underlying lung conditions like asthma and COPD.2 , 3 Masking has been shown to decrease the transmission of respiratory viruses,4 but widespread public masking was not practiced in the United States, even for previous pandemics,5 until the coronavirus disease 2019 (COVID-19) pandemic. The Centers for Disease Control and Prevention (CDC) reported unusually low influenza activity in the United States during the COVID-19 pandemic,6 though, it is unclear whether this is due to masking, stay-at-home orders, the public declining to visit the ED for fear of acquiring COVID-19, or some other effect. We hypothesize that increases in masking among the general population is associated with decreases in ED visits for non-COVID viral illnesses (NCVIs) and exacerbations of asthma and COPD.
Methods
This is an observational study based on ED encounters using electronic medical record data. We obtained information on all ED patient encounters across the University of Maryland Medical System (UMMS) (Maryland, 11 sites) from January 1 to October 3, 2019, and from January 1 to October 3, 2020. Encounter data included: patient age, sex, past medical history of asthma or COPD, encounter diagnoses, the time and date of the encounter, and whether the patient tested positive for COVID-19. All encounter data were extracted from the electronic medical record (Epic Systems) at each site in an automated fashion using Structured Query Language (SQL). This study was approved and considered exempt by the University of Maryland, Baltimore institutional review board.
ED visit for specific complaints were identified by having one of the following codes for the first 3 encounter diagnoses, as documented by the provider (using International Classification of Diseases, version 10, Clinical Modification [ICD-10-CM]): NCVI (J09-J11 or J20-J22), asthma exacerbation (J45.21-J45.22, J45.31-J45.32, J45.41, J45.42, J45.51, J45.52, J45.901, J45.902), or COPD exacerbation (J44.1). We excluded visits with a positive COVID result and those with encounter code for pneumonia (J12-J18) because patients with COVID-19 could be coded as pneumonia.
To control for stay-at-home orders (“lockdowns”) and the overall changes in ED visits seen in 2020 compared with 2019, we constructed year-on-year ratios on a per-week basis. We counted all ED visits (“Total Visits”) across all sites for the first week in 2020 (1/1/2020-1/7/2020), divided by the total number of ED visits across all sites for the first week in the prior year (1/1/2019-1/7/2019). We repeated this process through week 40 (the last week of the 2020 data) and for all end points (ED visits for NCVI, exacerbations of asthma and COPD) and control variables (average patient age, prevalence of female sex and preexisting asthma or COPD). Patients with asthma or COPD listed on their problem list were considered to have a past medical history of asthma (J45) or COPD (J41-J43).
The changes in ED patient volume and complaints between 2019 and 2020 was shown by plotting year-on-year ratios with the Maryland stay-at-home order (3/30/20-5/15/2020)7 and the percentage of masking in the general population. The percentage of masking in the general population of Maryland came from the Institute for Health Metrics and Evaluation (IHME) website.8 The IHME website publishes a combination of online surveys to provide a daily state-based estimate of the proportion of the population who say they always wear a mask in public. This estimate was averaged to provide a weekly percentage of masking. Our mathematical model followed the natural development of disease: a community dweller is inoculated with a virus, which could have been blocked by a mask, who later develops clinical disease and seeks treatment in an ED. We accounted for the time course of disease by shifting the daily prevalence of masking back 3, 7, and 12 days for NCVI, exacerbations of asthma and COPD, respectively.2 , 3 We used a similar approach to determine the impact of social distancing measures taken during the pandemic, as reported by the IHME.8
Linear regression was used to determine the association between the percentage of masking and year-on-year ratio of ED visits for All Visits, NCVI, and exacerbations of asthma and COPD. Controls included ratios of patient age, female sex, All Visits, and history of asthma and/or COPD. A dummy variable for encounters occurring after March 30, 2020 was created to estimate the association between ED visits and the Maryland stay-at-home order.7
Results
There were 285,967 ED encounters across the University of Maryland Medical System during the 2019 study period, of which 53.3% (N = 152,279) were female, had an average age of 43.0, SD = 23.1, and 7.8% (N = 22,399), and 0.2% (N = 698) came to the ED for an asthma or COPD exacerbation, respectively. During the 2020 study period there were 252,598 ED encounters; 52.1% (N = 131,496) were female, and 5.9% (N = 14,881) and 0.2% (N = 430) of visits were for asthma or COPD, respectively. The average age of subjects in 2020 was 45.0, SD = 22.7. There was a 3.3% relative decrease in ED visits for NVCI in 2020 (N = 4770) compared with 2019 (N = 4611). Similarly, there was a 47.9% decrease in ED visits for asthma exacerbations in 2020 (1619) compared with 2019 (N = 3107), and a 54.8% decrease in visits for COPD exacerbations in 2020 (N = 1069) compared with 2019 (N = 2363).
The percentage of masking in the community was highly correlated with social distancing measures (Pearson correlation = −0.82). Masking had a stronger association with our endpoints than social distancing, so we removed the social distancing from our mathematical model to avoid collinearity.
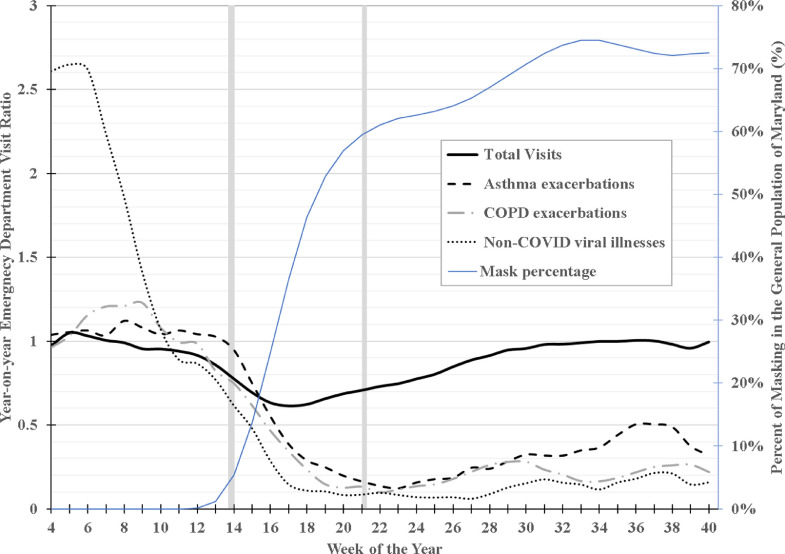
Year-on-year ratio for Total Visits fell 40% during weeks 18 and 19 (Figure ) but trended close to normal (values approached 1) after the stay-at-home order was lifted. Year-on-year ratios for NCVI, asthma, and COPD remained low (a fraction of 1) through week 40. An unadjusted linear regression analysis found a nonsignificant association between the year-on-year ratio for Total Visits and the start of the stay-at-home order (parameter estimate = −0.0804, P = .10). Similarly, masking percentage was not significantly associated with the year-on-year ratio for Total Visits (parameter estimate = 0.00204, P = .98). There were strong associations between masking percentage and year-on-year ratios for specific complaints, after adjusting for patient factors and Total Visits (Table ).
Figure.
Year-on-year ratio of emergency department visits in the University of Maryland Medical System for total visits, exacerbations of asthma and chronic pulmonary disease, and non-COVID-19 viral illness (NCVI) with the prevalence of masking in Maryland State (Jan-Oct 2019 and Jan-Oct 2020) and the stay-at-home order (March 30-May 15, 2020). Ratios presented are 4-week moving averages. COVID-19 = coronavirus disease 2019.
Table.
Linear Regression Results Showing the Association of Masking Percentage with Year-on-Year Ratios of ED Encounters for NCVI and Exacerbations of Asthma and COPD, Adjusted for Patient Factors and Total Visits, University of Maryland Medical System (Jan-Oct 2019 compared to Jan-Oct 2020).
| Outcome | Variable* | Estimate | Standard Error | P Value |
|---|---|---|---|---|
| NCVI | Masking Percentage | −1.702 | 0.422 | .0003 |
| Average Age | −3.605 | 3.711 | .34 | |
| Female Sex | 0.017 | 2.184 | .99 | |
| Total Visits | 1.681 | 2.542 | .51 | |
| Asthma Exacerbations | Masking Percentage | −0.881 | 0.196 | <.0001 |
| Average Age | −2.011 | 1.146 | .09 | |
| Female Sex | 0.342 | 0.495 | .49 | |
| Prevalence of Asthma | −0.112 | 0.422 | .79 | |
| Total Visits | 0.317 | 0.360 | .38 | |
| COPD Exacerbations | Masking Percentage | −0.939 | 0.143 | <.0001 |
| Average Age | −0.389 | 1.319 | .77 | |
| Female Sex | −0.102 | 0.343 | .77 | |
| Prevalence of COPD | 0.276 | 0.076 | .001 | |
| Total Visits | 0.655 | 0.313 | .04 |
COPD = chronic obstructive pulmonary disease; COVID-19 = coronavirus disease 2019; ED = emergency department; NCVI = non-COVID viral illness;
Masking: the percentage of persons who always wear a mask in public; Average Age: the ratio of the average age of ED patients during a given week in 2020 compared with 2019; Female sex: the proportion of female ED patients during a given week in 2020 divided by the proportion of female ED patients during the same week in 2019; Prevalence of Asthma: the proportion of patients who have a past medical history of asthma during a given week in 2020 divided by the proportion of patients who have a past medical history of asthma during the same week in 2019; Prevalence of COPD: the proportion of patients who have a past medical history of COPD during a given week in 2020 divided by the proportion of patients who have a past medical history of COPD during the same week in 2019; All-complaints: the number of ED patients for a given week in 2020 divided by the number of ED patients during the same week in 2019.
Discussion
Masking had not been widely adopted in the United States until the COVID pandemic, making it difficult to investigate how masking in the community could impact ED visits.5 The majority of Maryland citizens wore masks during the COVID-19 pandemic,8 and masks block a variety of respiratory viruses,4 providing a natural experiment to determine the effects of general masking on ED visits. The overall drop in ED visits during the pandemic seen in this study has been documented by other investigators.9 , 10 Yet when examining specific complaints, an increase in the percentage of community masking was reflected in a drop in ED visits for NCVI and exacerbations of asthma exacerbations and COPD in this retrospective multisite study. These findings suggest the well-known decrease in person-to-person transmission of respiratory viruses due to masking4 also has a measurable and positive impact on health systems. These results also suggest there is a public health benefit to community masking after the COVID-19 pandemic. For example, public health officials may mitigate the impact of respiratory conditions on health systems by promoting masking among the general populace during the influenza season. In a recent interview, Dr Anthony Fauci, director of the National Institute of Allergy and Infectious Disease, said much the same: “We've had practically a nonexistent flu season this year merely because people were doing the kinds of public health things that were directed predominantly against COVID-19.”11
This is a retrospective study and vulnerable to unmeasured biases. However, our ratio-based approach likely mitigates these effects by comparing 1 year to the other. The daily prevalence of masking is based on survey data and may not accurately represent the masking behavior in Maryland or in the communities around the study sites. Several public health measures, like an emphasis on social distancing, handwashing, stay-at-home-orders, and masking, were instituted in Maryland around the same time. We adjusted our analysis to account for the Maryland stay-at-home order. There are no public sources of data on the changes in handwashing behavior in Maryland during the pandemic. COVID is primarily transmitted via respiratory droplets, so the impact of increased handwashing is likely less than the impact of masking or social distancing. Social distancing almost certainly influences our endpoints, but this single-state study is not able to separate the impact of masking from social distancing. Multistate studies may be able to disentangle these effects. An interrupted time series (ITS) approach was considered because it is well-suited to model the impact of large single changes like stay-at-home orders. Unfortunately, interrupted time series does not model daily changes in masking behavior well, and it does not provide a measure of association between masking and ED utilization, which was the objective of this project.
The 2020 influenza season may have been mild regardless of the COVID-19 pandemic, which would serve to overestimate the impact of masking in this analysis. Some patients that would have had NCVI instead may have died from COVID-19 instead, effectively depressing the severity of the 2020 influenza season and the impact of masking in this analysis. Telehealth visits increased during this study period, which may have affected ED volume.
Conclusion
In conclusion, increasing the prevalence of masking is associated with a decrease in ED visits for viral illnesses and exacerbations of asthma and COPD. These findings may be valuable for future public health responses, particularly in future pandemics with respiratory transmission or in severe influenza seasons.
Footnotes
Funding: ZDWD, KSZ, the data extraction, and data analysis, were all supported through grants from National Foundation of Emergency Medicine. The National Foundation of Emergency Medicine was not involved in the development of the analysis or the contents of the report.
Conflicts of Interest: ZDWD reports serving on an advisory board for Perdue Pharmaceuticals to assist with the development medications to be used against the opioid epidemic. CBC reports serving as a consultant to bioMerieux on biomarkers; as the President of the Board of Directors of the National Foundation of Emergency Medicine (NFEM), a non-profit organization dedicated to the development of emergency medicine research, innovation and investigators; and receives funding for COVID-19 research from the National Institutes of Health (NIAID, NHLBI) and the Bill & Melinda Gates Foundation. BS, RMC, DM, LP, MS-K report none.
Authorship: All authors had access to the data and a role in writing this manuscript.
References
- 1.Garten R, Blanton L, Abd Elal AI, et al. Update: influenza activity in the United States during the 2017–18 season and composition of the 2018–19 influenza vaccine. MMWR Morb Mortal Wkly Rep. 2018;67(22):634–642. doi: 10.15585/mmwr.mm6722a4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Jackson DJ, Makrinioti H, Rana BM, et al. IL-33–dependent type 2 inflammation during rhinovirus-induced asthma exacerbations in vivo. Am J Respir Crit Care Med. 2014;190(12):1373–1382. doi: 10.1164/rccm.201406-1039OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mallia P, Kebadze T, Parker HL, Kon OM, Johnston SL. An experimental model of rhinovirus induced chronic obstructive pulmonary disease exacerbations: a pilot study. Respir Res. 2006;7(1):1–10. doi: 10.1186/1465-9921-7-116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chu DK, Akl EA, Duda S, et al. Physical distancing, face masks, and eye protection to prevent person-to-person transmission of SARS-CoV-2 and COVID-19: a systematic review and meta-analysis. Lancet. 2020;395(10242):1973–1987. doi: 10.1016/S0140-6736(20)31142-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.SteelFisher GK, Blendon RJ, Bekheit MM, Lubell K. The public's response to the 2009 H1N1 influenza pandemic. N Engl J Med. 2010;362(22):e65. doi: 10.1056/NEJMp1005102. [DOI] [PubMed] [Google Scholar]
- 6.Center for Disease Control and Prevention (CDC). Weekly U.S. Influenza Surveillance Report. Available at: https://www.cdc.gov/flu/weekly/index.htm. Accessed March 25, 2021.
- 7.Maryland Executive Order No. 20-03-30-01 (March 30th, 2020).
- 8.Institute for Health Metrics and Evaluation (IHME). COVID-19 Projections. Available at: https://covid19.healthdata.org/. Accessed March 25, 2021.
- 9.Hartnett KP, Kite-Powell A, DeVies J, et al. Impact of the COVID-19 pandemic on emergency department visits—United States, January 1, 2019–May 30, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(23):699–704. doi: 10.15585/mmwr.mm6923e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Haddadin Z, Blozinski A, Fernandez K, et al. Changes in pediatric emergency department visits during the COVID-19 pandemic. Hosp Pediatr. 2021;11(4):e57–e60. doi: 10.1542/hpeds.2020-005074. [DOI] [PubMed] [Google Scholar]
- 11.Villegas P. Fauci says wearing masks could become seasonal following the pandemic. Washington Post. Available at:https://www.washingtonpost.com/health/2021/05/09/fauci-covid-masks-seasonal-pandemic/. Accessed May 20, 2021.