INTRODUCTION
Older adults with cancer represent the largest and most rapidly growing population of patients with cancer.1,2 The majority of new cancer diagnoses occur in individuals age 65 and older, and the geriatric oncology population accounts for nearly three fourths of cancer deaths.2 Compared with younger patients, older patients with cancer experience worse survival outcomes, potentially related to increased frailty, diminished functional status, and differences in treatment patterns.3,4 Notably, studies suggest that inadequate symptom management and insufficient delivery of supportive care may contribute to poor clinical outcomes for the geriatric oncology population.5-8 Thus, rigorous research is critically needed to help address the unique geriatric and palliative care needs of older adults with cancer.
CONTEXT
Key Objective
How might the convergence of principles from geriatric oncology and palliative care help enhance the care of older adults with cancer?
Knowledge Generated
We first explain how the fields of geriatric oncology as well as palliative and supportive care have considerable overlap, yet also provide complementary care domains, which could synergize to optimize the cancer experience for older patients. We then discuss the unique geriatric and palliative care needs of older adults with cancer, underscoring the imperative to develop and test interventions targeting these needs with rigorously conducted research.
Relevance
Efforts to optimize care delivery and outcomes for older adults with cancer must effectively address these patients' distinct geriatric and palliative care needs.
In this article, we first discuss the need to merge principles from geriatric oncology and palliative care as a strategy to help enhance the care of older adults with cancer. We then describe the unique geriatric and palliative care needs of older adults with cancer, underscoring the imperative for interventions targeting these needs. Next, we review several existing efforts that could help address the geriatric and palliative care concerns of patients with cancer. Lastly, we discuss future directions that could help to improve care delivery and outcomes for older adults with cancer by effectively targeting the geriatric and palliative care needs of these individuals.
MERGING PRINCIPLES FROM GERIATRIC ONCOLOGY AND PALLIATIVE CARE
The fields of geriatric oncology as well as palliative and supportive care have considerable overlap, yet these specialties also provide complementary care domains, which could harmonize to enhance the cancer experience for older patients. Specifically, geriatric oncology focuses on the management of cancer in the older adult, usually defined as age 65 and older.9 Geriatric oncology care entails comprehensive evaluation and management of patients' physical, functional, social, cognitive, and psychologic well-being.9 The terms palliative care and supportive care are often used interchangeably in the context of interprofessional team-based care-seeking to optimize patients' quality of life (QOL).10 High-quality, holistic palliative and supportive care entails care delivered by a multidisciplinary team of clinicians with specialized training in symptom management, psychosocial care, spiritual support, communication about illness and prognosis, care coordination, complex decision making, caregiver support, and end-of-life care.10-12 The robust foundation of research from the fields of geriatric oncology and palliative care provides a comprehensive evidence base to help understand the distinct geriatric and palliative care needs of older adults with cancer, which could inform the development and testing of future interventions targeting these needs.
UNIQUE GERIATRIC AND PALLIATIVE CARE NEEDS OF OLDER ADULTS WITH CANCER
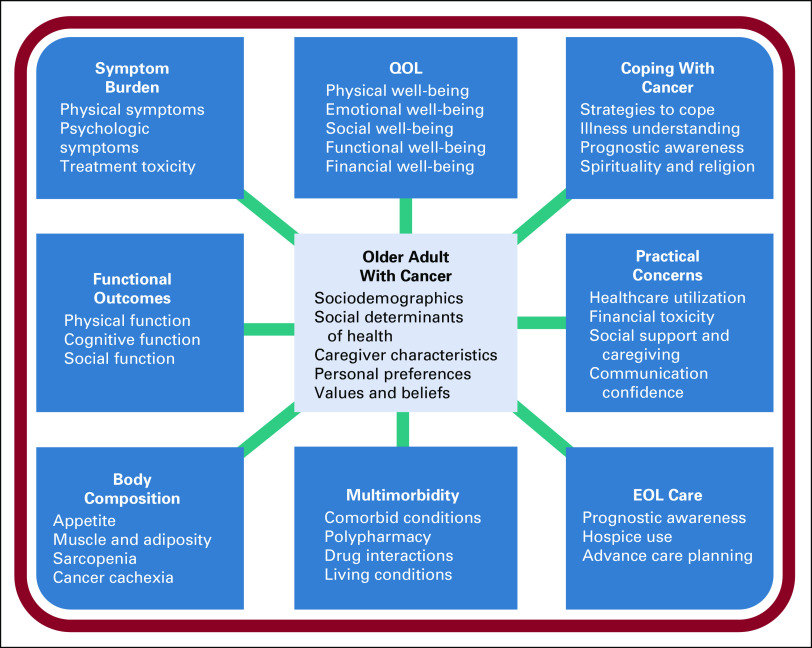
Older patients possess a challenging constellation of medical and psychosocial issues, often adding to the complexity of their care and influencing their experience with cancer. For example, older adults with cancer experience unique geriatric-specific concerns (eg, functional impairment, comorbidity, and polypharmacy) as well as palliative care–specific issues (eg, symptom burden, prognostic understanding, and coping).13-15 Patients with cancer manifest a wide range of symptoms of varying intensities, extending from those who are minimally symptomatic to others with a profound multidimensional complex of physical and psychosocial symptoms.8,16,17 As such, delivering patient-centered care hinges on the identification of the global symptom burden of each patient, with the subsequent design of comprehensive symptom management strategies.18-20 Additionally, although older adults with cancer have distinct needs, interventions targeting the unique geriatric and palliative care concerns of this population are limited.9,15,21,22 Interventions involving palliative care consultation alone may not fully address all the concurrent geriatric-specific needs of older adults with cancer, and vice versa, geriatric interventions may not completely target all of these patients' palliative care concerns.23,24 Thus, a detailed understanding of the complex geriatric and palliative care issues unique to older adults with cancer could help with future efforts to optimize care for the geriatric oncology population (Fig 1).
FIG 1.
Geriatric and palliative care needs in older adults with cancer. EOL, end of life; QOL, quality of life.
Treatment Tolerability, Symptom Burden, and QOL
The unique geriatric and palliative care needs of older adults with cancer often present a distinct set of challenges for oncology clinicians, particularly with regards to treatment tolerability, symptom burden, and QOL outcomes. When treated with chemotherapy, older adults with cancer frequently face a higher risk of experiencing treatment-associated toxicities and even treatment-related deaths than younger patients.25 Additionally, although older adults with cancer often report a lower symptom burden than younger patients, research suggests that their symptom clusters frequently include a larger and more diverse range of physical and psychologic symptoms.13,26 Furthermore, studies suggest that older adults with cancer receive less treatment for certain symptoms, such as pain.5,27 Notably, patients' symptom burden can influence their functional independence and QOL.7,28 QOL concerns are particularly salient and important to address when caring for older patients, and several tools exist specifically to help assess QOL in the geriatric oncology population.29-31 Importantly, older adults with cancer have a unique symptom burden and QOL experience, which merits additional research to understand how best to target these issues in geriatric oncology.5,16,27,29-31
Functional Outcomes, Body Composition Changes, and Frailty
The amalgamation of patients' symptoms, combined with functional impairment (ie, decrements in physical, cognitive, and social function) and body composition changes (ie, loss of muscle, decreased appetite, and cancer cachexia), helps characterize the concept of frailty.7,8,32,33 Notably, multiple measures of frailty exist, some in the broader older adult population and others specifically in those with cancer.33,34 A cancer-specific frailty index developed from the geriatric assessment has shown the ability to predict an incremental two-fold increase in all-cause mortality among frail versus robust older adults with cancer.33 Additionally, frailty and functional impairment demonstrate consistent associations with patients' symptoms.7,16 Functional impairment and frailty also correlate with body composition changes, which can lead to cancer cachexia.35 Cancer cachexia represents a syndrome encompassing the loss of weight, muscle (sarcopenia), and physical function, which occurs more frequently in older patients and negatively influences QOL, treatment tolerance, and survival outcomes.32,36
Social Support, Caregiving, and Financial Toxicity
The caregiving needs of older adults with cancer remain suboptimally characterized, and the domains of need identified in the general population without age specifications are often extrapolated to older adults.37 Informal caregiving refers to the uncompensated work provided by spouses, children, and other members of a patient's support system to meet their needs over the course of illness.38 The tasks of informal caregiving range from medical care to the familial and social needs of patients, including the handling of family dynamics and financial support. In recent years, the term financial toxicity has been coined as a way to describe the concept that the financial consequences of cancer and treatment can lead to considerable economic hardship and distress, which impairs patients' well‐being.39,40 Evidence suggests that older adults often experience lower financial burden than younger patients,39 yet recent work has demonstrated that older patients with cancer are not immune to economic hardship, and those who report greater financial distress also have higher levels of depression and anxiety, as well as lower QOL.40
Multimorbidity and Polypharmacy
Key components of comprehensive care for older patients with cancer include the management of multimorbidity and polypharmacy.41,42 Older adults with cancer often have greater numbers and severity of comorbid conditions than younger patients, and older patients' comorbidity frequently correlates with functional impairment.7,43 Additionally, patients with greater comorbidity burden may experience worse treatment and survival outcomes.43 In parallel with increased multimorbidity among older adults with cancer, these individuals also often experience challenges related to complex medication regimens and polypharmacy.44 Polypharmacy and difficulties with medication management place older adults with cancer at risk for adverse drug effects and drug-drug and drug-disease interactions.44 Consequently, polypharmacy in older adults with cancer may lead to greater risk for chemotherapy toxicity and worse survival outcomes.
Prognostic Understanding, Coping, Spirituality, and Religion
When addressing the geriatric and palliative care needs of older adults with cancer, clinicians must also attend to the concepts of illness understanding, prognostic awareness, coping mechanisms, and spiritual and/or religious needs.14,45 Measures of patients' understanding of their prognosis often correlate with other important health outcomes, including QOL, symptom burden, and overall survival.14,46 Importantly, data suggest that patients' understanding of their prognosis can influence their treatment decisions and preferences for end-of-life care.47,48 However, older patients with incurable cancer often report inaccurate perceptions of the curability of their cancer.14,45 When informing patients of a poor prognosis, clinicians may fear that this could negatively affect patients' hope, yet evidence suggests that this is not true, and efforts to enhance patients' prognostic awareness should strive to cultivate adaptive coping mechanisms.14,46,49 In addition, patients with cancer cope in numerous, multifaceted ways.50 Studies demonstrate that older and younger patients with cancer use different coping mechanisms, which could influence how they handle the highs and lows associated with a cancer diagnosis.13,21,50 Moreover, evidence suggests that patients and caregivers frequently report the importance of spirituality and religion to help with coping with a cancer diagnosis.51,52
End-of-Life Care
End-of-life care, caregiver support and bereavement, and advance care planning all represent important components of high-quality geriatric and palliative care. Optimal end-of-life care includes the appropriate use of hospice services and the provision of care that aligns with patients' and their loved ones' preferences and values.53,54 Prior work demonstrates that older patients are more likely than younger patients to receive hospice services and pursue less aggressive end-of-life care.53 Older patients often report a lower preference for, and receipt of, life-prolonging treatment than younger patients, yet research suggests that older patients who desire treatment are less likely to receive care that aligns with their preferences.55 Notably, overly aggressive care at the end of life can negatively affect patients' QOL and impair caregivers' bereavement adjustment.56 Thus, advance care planning represents an important opportunity to ensure patients receive care concordant with their wishes, while also helping to avoid overly aggressive care at the end of life.57 Consistent with the literature that older adults are less likely to receive aggressive care at the end of life and more likely to enroll in hospice services compared with their younger counterparts, older patients with cancer are also more likely to complete an advance directive and designate a surrogate decision maker.58
EFFORTS TO ADDRESS THE GERIATRIC AND PALLIATIVE CARE NEEDS OF OLDER PATIENTS WITH CANCER
Older adults with cancer experience multifaceted geriatric and palliative care issues, and thus integrating whole-person assessment and management strategies is needed to more comprehensively address these patients' complex care issues. Efforts to provide comprehensive oncologic care for older adults with cancer should seek to target important aspects of these patients' cancer experience, as illustrated by Figure 2. Several efforts exist, with growing evidence to support their use, which provide insights into potential strategies to help address the geriatric- and palliative care–specific needs unique to older patients with cancer.
FIG 2.
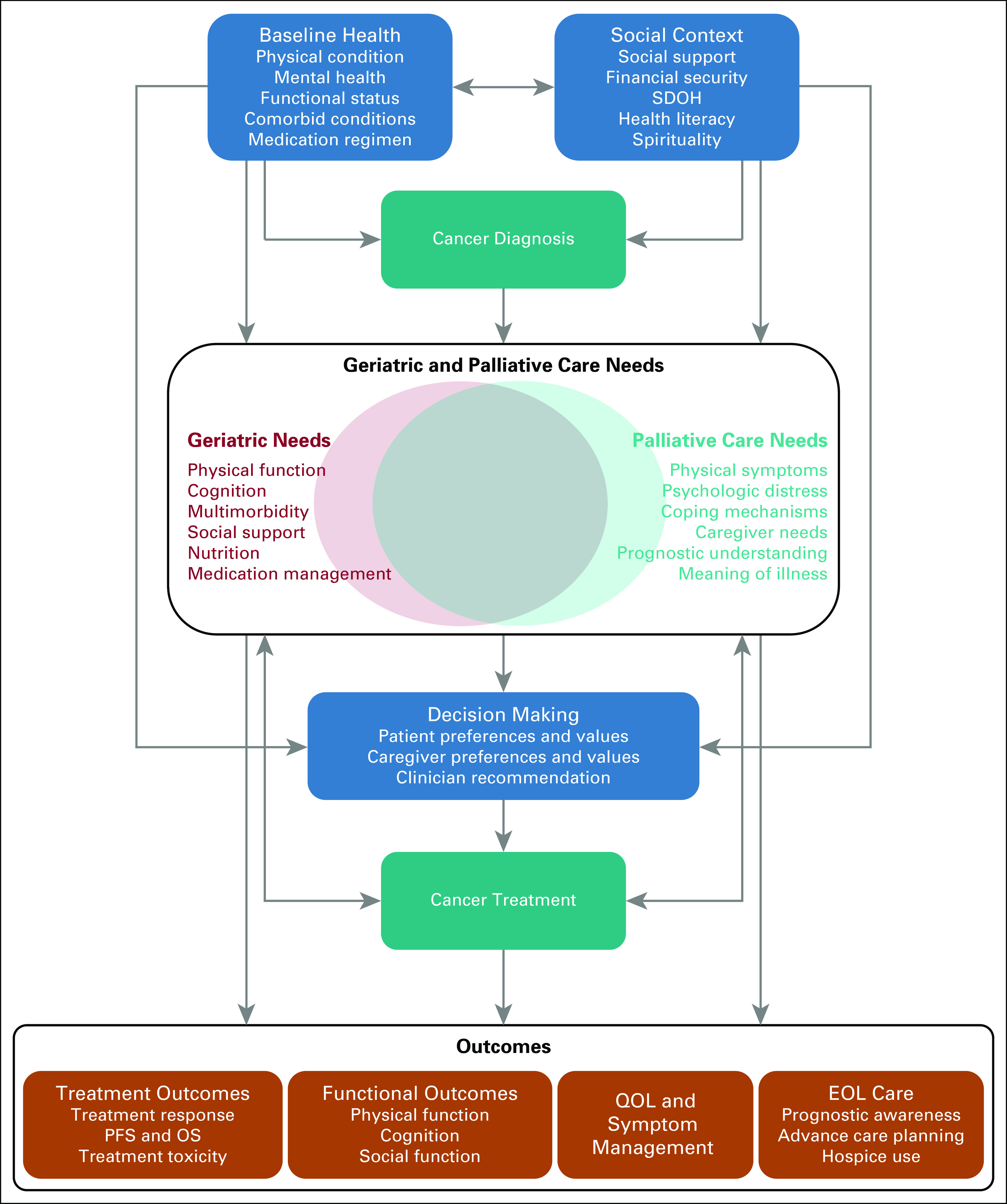
Foundational principles of the cancer experience in the older adult. EOL, end of life; OS, overall survival; PFS, progression-free survival; QOL, quality of life; SDOH, social determinants of health.
Geriatric Assessment–Guided Care
Incorporating geriatricians and geriatric assessment into the care for older adults with cancer represents a strategy for targeting these patients' geriatric and palliative care concerns.9,22,59 Notably, geriatric assessment alone may not target all of patients' palliative care–specific issues, while palliative care interventions may not comprehensively address all the geriatric-specific concerns of older patients with cancer.13,15,23,24 Thus, geriatric assessment–guided care interventions are needed, which address the multifaceted geriatric and palliative care issues unique to older adults with cancer. In prior work, provision of a geriatric assessment–guided intervention has demonstrated the ability to facilitate communication, improve care satisfaction, and increase advance care planning for older adults with advanced cancer.60 Another study has demonstrated the feasibility and acceptability of a transdisciplinary geriatric intervention, delivered by geriatricians, which targeted patients' geriatric and palliative care needs.61 Importantly, this transdisciplinary geriatric intervention showed promising results for helping to improve patients' QOL, symptom burden, and communication confidence. However, a long-standing shortage of geriatric clinicians limits patient access to these specialists, and thus future efforts will need to find scalable ways of delivering geriatric care to older adults with cancer.62,63
Early Integration of Palliative Care
Early integration of palliative care specialists alongside routine oncology care represents a potential strategy to ensure appropriate monitoring and management of patients' palliative and supportive care needs. Extensive research has consistently demonstrated the benefits of palliative care interventions for patients with cancer and their caregivers.64–72 Specifically, studies have shown that early integration of specialty palliative care for patients with cancer can enhance their QOL, symptom management, illness understanding, coping mechanisms, and end-of-life care.64-71 On the basis of this abundant research in palliative care, expert guidelines recommend that patients with advanced cancer should receive dedicated palliative care services, early in the disease course and alongside active treatment.11,12 However, a dearth of palliative care clinicians exists, and despite the extensive literature demonstrating the ability of palliative care interventions to improve outcomes for individuals with cancer, these studies are often conducted across a broad range of ages with their findings extrapolated to an older adult population.11,12 Notably, the benefits of palliative care may not always directly translate to older patients with cancer.23,24 For example, data from a randomized trial of early palliative care suggested that older patients did not experience the same levels of QOL and mood improvements related to early palliative care as younger patients.24 Another secondary analysis of data from a separate randomized trial of early palliative care demonstrated that older patients did not experience significant improvements in their use of coping strategies with early palliative care, whereas younger patients did.23 Collectively, these data suggest that older patients have specific issues that may not be fully addressed by standard oncology and palliative care, and thus future interventions should seek to comprehensively target these patients' unique geriatric and palliative care concerns.
Patient-Reported Symptom Monitoring
Enabling patients to self-report their symptoms represents a promising solution to ensure accurate and consistent monitoring of patient-reported outcomes.73 Evidence supports the use of patient-reported symptom monitoring interventions to effectively address patients' symptom burden, improve QOL, decrease the use of healthcare services, and potentially enhance survival outcomes.18-20,74,75 However, symptom monitoring interventions frequently necessitate that patients report their symptoms electronically, which could potentially create a barrier for less technologically savvy older patients. Additionally, prior work suggests that the benefits seen with an electronic patient-reported symptom monitoring intervention differ on the basis of patients' age.76 Specifically, a secondary analysis of a randomized trial of a patient-reported symptom monitoring intervention demonstrated that older patients did not experience significant intervention effects related to healthcare utilization or survival, whereas the younger patients did.76 Thus, future studies are needed to better understand how best to develop and tailor symptom monitoring interventions to the personalized care needs unique to the geriatric oncology population.
Screening for Supportive Care Needs
Increasingly, oncology clinics have begun incorporating screening instruments, which may help identify patients' supportive care needs. A care model used extensively at City of Hope entails the use of SupportScreen, which patients complete prior to meeting with their oncology team.77 SupportScreen enables patients to report distress related to physical limitations and symptoms, psychologic issues, and social barriers, while also encouraging them to share their perception of prognosis so their clinical team can focus on the most salient concerns during the clinical encounter.77-80 With SupportScreen, clinicians at City of Hope can identify the most frequent high-distress items, which often differ between younger and older patients.77-80 Other measures that could help to screen for patients' supportive care needs include the Supportive Care Needs Survey and Distress Thermometer.81,82 However, screening is not equivalent to assessment, but rather screening should lead to more nuanced assessment(s) on the basis of issues identified. Furthermore, screening is not an intervention by itself but rather should lead to detailed assessments, which can then inform interventions needed for each individual patient. Importantly, future work should investigate the use of brief screening tools to help guide a more comprehensive assessment of patients' geriatric and palliative care needs, with the goal of enhancing patient outcomes.59
Education and Training in Geriatric Oncology and Palliative Care
The integration of geriatric and palliative care principles into oncologic practice hinges on the foundational knowledge from the fields of geriatric oncology and palliative care. Notably, hematology and oncology fellows often report variability and lack of education about geriatric oncology, yet when asked, they consistently share a desire for more training and opportunities to participate in geriatric oncology clinics.83,84 Similarly, oncology fellows frequently report feeling inadequately prepared to provide palliative care for patients with cancer, further highlighting a critical gap and opportunity for improvement in training.85 For clinicians in training, formal didactics and dedicated rotations in geriatrics and palliative care provide an opportunity for foundational exposure to core principles. For those in clinical practice, opportunities for training in geriatrics and palliative care skills exist from organizations such as ASCO, the International Society of Geriatric Oncology, and the American Academy of Hospice and Palliative Medicine. Furthermore, prior work involving serious illness conversations training has demonstrated the ability for oncology clinicians to gain skills in communicating important and difficult topics with seriously ill patients about their illness understanding and care preferences.86 Future efforts could build upon experiences such as this to develop an integrated curriculum, focused on geriatrics and palliative care, for trainees and practicing clinicians across the multidisciplinary setting, while also investigating the efficacy of such efforts to improve patient outcomes.
FUTURE DIRECTIONS
Management of older patients' physical, perceptible symptoms alone will not sufficiently ensure the provision of patient-centered care for these individuals. Moreover, focusing solely on the traditional domains of the geriatric assessment may miss some critical palliative care concerns. Comprehensive assessment of the geriatric and palliative care domains within oncology could help with identifying management strategies, yet a dearth of studies limits the available evidence supporting any specific strategy for older patients with cancer. Here, we have identified several gaps in the literature, as outlined below, which future work should address to help optimize the care provided to older adults with cancer by effectively targeting the geriatric and palliative care needs of these individuals.
Need for Novel Care Models Focused on the Geriatric and Palliative Care Needs of Older Adults With Cancer
Considering the long-standing shortage of geriatricians and palliative care clinicians, scalable models are needed to reliably deliver personalized care addressing the geriatric and palliative care concerns of older adults with cancer. Care models should leverage the expertise of a multidisciplinary team inclusive of uniquely specialized clinical roles, such as physicians and advanced practice providers, as well as clinicians from social work, chaplaincy, physical and occupational therapy, nutrition, clinical psychology, pharmacy, and others.42,87 Future work to help disseminate key components of geriatric oncology and palliative care should consider the use of novel models of care such as collaborative care models and stepped-care approaches.88,89 Collaborative care models use a team-based approach to provide specialty-level care to complex patients in settings with limited numbers of trained specialists.88 In collaborative care models, care managers assess patients on a frequent basis, offer evidence-based treatment, and disseminate recommendations from a support team of specialist clinicians. Stepped-care approaches also represent a strategy to help ensure scalability. In stepped-care approaches, patients receive care with minimal contact with the specialist clinician, reserving more intensive care for those not responding to the minimal care level.89 Specifically, stepped-care approaches require systematic monitoring of patients to ensure care is appropriately stepped up to more intensive treatment if the minimal level does not achieve sufficient benefits. Additionally, considering the growing literature espousing the benefits of both geriatric assessment–guided interventions and patient-reported outcome monitoring, future work should seek to combine these strategies to focus on routinely monitoring geriatric assessment domains as well as palliative care concerns. However, such efforts will need to overcome technologic barriers inherent to the geriatric oncology population. Notably, telehealth represents a novel method of intervention delivery in geriatric oncology, previously avoided because of logistical and technologic barriers in older patients.90-92 The COVID-19 pandemic demonstrated the ability of patients, clinicians, and health systems to adopt telehealth as a safe and effective care modality.90,92 Thus, future efforts to ensure older adults with cancer can readily receive specialist-level care targeting their geriatric and palliative care concerns should leverage telehealth as a feasible modality to enhance access to care.
Need for Geriatric- and Palliative Care–Specific Outcomes in Cancer Clinical Trials
Studies designed for older adults with cancer should incorporate geriatric and palliative care outcomes. For example, many studies of palliative and supportive care interventions measure QOL as the primary outcome, but other geriatric-specific outcomes, including physical, social, and mental function as well as treatment tolerability, could elucidate a more complete understanding of the benefits of these interventions.93 Furthermore, validated QOL questionnaires specifically designed for the geriatric oncology population exist, which could provide more nuanced information when assessing the efficacy of interventions for older patients with cancer.30,31 Additional important outcomes to consider when designing studies in geriatric oncology include functional outcomes, treatment toxicity, communication confidence, prognostic and illness understanding, coping mechanisms, cancer cachexia, and healthcare utilization (including time spent in the hospital or at a care facility).9,14,32,60,93
Need for Efforts to Effectively Implement Geriatric and Palliative Care Initiatives in Oncology
Challenges with effective implementation and adoption of efforts to address the unique needs of older adults with cancer diminish the impact of such efforts within oncology.61,94-99 Successful implementation requires effectively training clinicians with the knowledge and skills related to both geriatric oncology and palliative care. The field of palliative care has previously defined the concepts of primary palliative care (skills all clinicians should acquire) and specialist palliative care (skills acquired by specialists to help manage complex and difficult circumstances).100 In geriatric oncology, future efforts should seek to define primary and specialist skills to help inform the training of oncologists in the skills all oncologists should acquire regarding geriatrics and palliative care, while also educating oncologists about when to refer to specialists. Additionally, the use of screening tools to personalize care is lacking from routine cancer care.23,24,76,101 Screening tools may help clinicians identify patients with impairments needing attention, and these tools could also guide decisions about when to refer for specialist geriatric and palliative care expertise.8,78,102 Moreover, institutional support and buy-in represent critically important factors lacking from many efforts to integrate geriatric and palliative care initiatives in oncology, which may be garnered by espousing the benefits of such efforts with rigorous, high-quality research. However, older patients with cancer experience barriers to participation in supportive care clinical trials, including difficulties with the added burden of study visits and the complexities of study procedures.61,94-97 Therefore, to effectively address the unique geriatric and palliative care needs of older adults with cancer, successful implementation strategies must be used, with such efforts supported by meticulously collected, robust data.
In summary, cancer disproportionately affects older individuals, and older adults with cancer often experience a unique set of geriatric and palliative care concerns. Older patients with cancer may benefit from interventions targeting their distinct geriatric and palliative care needs, with a growing body of literature supporting the need for efforts to develop and test such interventions.23,24,60,61,76 Importantly, interventions targeting the geriatric and palliative care concerns of older adults with cancer must be tested rigorously in randomized trials, as well as implementation and dissemination studies, to ensure the efficacy, applicability, and effectiveness of these efforts for improving geriatric oncology care. Collectively, we hope that this article will inform ongoing efforts, both clinical and academic, to help clinicians caring for older adults with cancer effectively address the geriatric and palliative care needs of these patients with the goal of enhancing their care delivery and outcomes.
Ishwaria M. Subbiah
Consulting or Advisory Role: MedImmune
Research Funding: Bayer, Novartis, GlaxoSmithKline, NanoCarrier, Celgene, Northwest Biotherapeutics, Incyte, Fujifilm, Pfizer, Amgen, Abbvie, Multivir, Exelixis, Loxo, Blueprint Medicines, Takeda
Travel, Accommodations, Expenses: Bayer, PharmaMar, Novartis, MedImmune
Matthew Loscalzo
Honoraria: Puma Biotechnology
Consulting or Advisory Role: AstraZeneca
Patents, Royalties, Other Intellectual Property: SupportScreen royalties via my employer City of Hope (non-profit)
No other potential conflicts of interest were reported.
DISCLAIMER
The contents of this article are solely the responsibility of the authors and do not necessarily represent the official view of NCI or NIH.
SUPPORT
Supported by the NIH/NCI K12 Program Number K12CA087723.
AUTHOR CONTRIBUTIONS
Conception and design: All authors
Collection and assembly of data: All authors
Data analysis and interpretation: All authors
Manuscript writing: All authors
Final approval of manuscript: All authors
Accountable for all aspects of the work: All authors
AUTHORS' DISCLOSURES OF POTENTIAL CONFLICTS OF INTEREST
Convergence of Geriatrics and Palliative Care to Deliver Personalized Supportive Care for Older Adults With Cancer
The following represents disclosure information provided by authors of this manuscript. All relationships are considered compensated unless otherwise noted. Relationships are self-held unless noted. I = Immediate Family Member, Inst = My Institution. Relationships may not relate to the subject matter of this manuscript. For more information about ASCO's conflict of interest policy, please refer to www.asco.org/rwc or ascopubs.org/jco/authors/author-center.
Open Payments is a public database containing information reported by companies about payments made to US-licensed physicians (Open Payments).
Ishwaria M. Subbiah
Consulting or Advisory Role: MedImmune
Research Funding: Bayer, Novartis, GlaxoSmithKline, NanoCarrier, Celgene, Northwest Biotherapeutics, Incyte, Fujifilm, Pfizer, Amgen, Abbvie, Multivir, Exelixis, Loxo, Blueprint Medicines, Takeda
Travel, Accommodations, Expenses: Bayer, PharmaMar, Novartis, MedImmune
Matthew Loscalzo
Honoraria: Puma Biotechnology
Consulting or Advisory Role: AstraZeneca
Patents, Royalties, Other Intellectual Property: SupportScreen royalties via my employer City of Hope (non-profit)
No other potential conflicts of interest were reported.
REFERENCES
- 1.Shapiro CL.Cancer survivorship N Engl J Med 3792438–24502018 [DOI] [PubMed] [Google Scholar]
- 2.Yancik R.Population aging and cancer: A cross-national concern Cancer J 11437–4412005 [DOI] [PubMed] [Google Scholar]
- 3.Sargent DJ, Goldberg RM, Jacobson SD, et al. A pooled analysis of adjuvant chemotherapy for resected colon cancer in elderly patients N Engl J Med 3451091–10972001 [DOI] [PubMed] [Google Scholar]
- 4.Nipp R, Tramontano AC, Kong CY, et al. Disparities in cancer outcomes across age, sex, and race/ethnicity among patients with pancreatic cancer Cancer Med 7525–5352018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bernabei R, Gambassi G, Lapane K, et al. Management of pain in elderly patients with cancer. SAGE Study Group. Systematic assessment of geriatric drug use via epidemiology JAMA 2791877–18821998 [DOI] [PubMed] [Google Scholar]
- 6.Kroenke CH, Kubzansky LD, Schernhammer ES, et al. Social networks, social support, and survival after breast cancer diagnosis J Clin Oncol 241105–11112006 [DOI] [PubMed] [Google Scholar]
- 7.Lage DE, El-Jawahri A, Fuh CX, et al. Functional impairment, symptom burden, and clinical outcomes among hospitalized patients with advanced cancer J Natl Compr Canc Netw 18747–7542020 [DOI] [PubMed] [Google Scholar]
- 8.Nipp RD, Thompson LL, Temel B, et al. Screening tool identifies older adults with cancer at risk for poor outcomes J Natl Compr Canc Netw 18305–3132020 [DOI] [PubMed] [Google Scholar]
- 9.Mohile SG, Velarde C, Hurria A, et al. Geriatric assessment-guided care processes for older adults: A delphi consensus of geriatric oncology experts J Natl Compr Canc Netw 131120–11302015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hui D, De La Cruz M, Mori M, et al. Concepts and definitions for “supportive care,” “best supportive care,” “palliative care,” and “hospice care” in the published literature, dictionaries, and textbooks Support Care Cancer 21659–6852013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ferrell BR, Temel JS, Temin S, et al. Integration of palliative care into standard oncology care: American Society of Clinical Oncology clinical practice guideline update J Clin Oncol 3596–1122017 [DOI] [PubMed] [Google Scholar]
- 12.Jordan K, Aapro M, Kaasa S, et al. European Society for Medical Oncology (ESMO) position paper on supportive and palliative care Ann Oncol 2936–432018 [DOI] [PubMed] [Google Scholar]
- 13.Mor V, Allen S, Malin M.The psychosocial impact of cancer on older versus younger patients and their families Cancer 742118–21271994 [DOI] [PubMed] [Google Scholar]
- 14.Nipp RD, Greer JA, El-Jawahri A, et al. Coping and prognostic awareness in patients with advanced cancer J Clin Oncol 352551–25572017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cheung WY, Le LW, Gagliese L, et al. Age and gender differences in symptom intensity and symptom clusters among patients with metastatic cancer Support Care Cancer 19417–4232011 [DOI] [PubMed] [Google Scholar]
- 16.Mohile SG, Heckler C, Fan L, et al. Age-related differences in symptoms and their interference with quality of life in 903 cancer patients undergoing radiation therapy J Geriatr Oncol 2225–2322011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Nipp RD, El-Jawahri A, Moran SM, et al. The relationship between physical and psychological symptoms and health care utilization in hospitalized patients with advanced cancer Cancer 1234720–47272017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Basch E, Deal AM, Kris MG, et al. Symptom monitoring with patient-reported outcomes during routine cancer treatment: A randomized controlled trial J Clin Oncol 34557–5652016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Denis F, Basch E, Septans AL, et al. Two-year survival comparing web-based symptom monitoring vs routine surveillance following treatment for lung cancer JAMA 321306–3072019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Strasser F, Blum D, von Moos R, et al. The effect of real-time electronic monitoring of patient-reported symptoms and clinical syndromes in outpatient workflow of medical oncologists: E-MOSAIC, a multicenter cluster-randomized phase III study (SAKK 95/06) Ann Oncol 27324–3322016 [DOI] [PubMed] [Google Scholar]
- 21.Blank TO, Bellizzi KM.A gerontologic perspective on cancer and aging Cancer 1122569–25762008 [DOI] [PubMed] [Google Scholar]
- 22.Mohile SG, Dale W, Somerfield MR, et al. Practical assessment and management of vulnerabilities in older patients receiving chemotherapy: ASCO guideline for geriatric oncology J Clin Oncol 362326–23472018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Nipp RD, El-Jawahri A, Traeger L, et al. Differential effects of early palliative care based on the age and sex of patients with advanced cancer from a randomized controlled trial Palliat Med 32757–7662018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Nipp RD, Greer JA, El-Jawahri A, et al. Age and gender moderate the impact of early palliative care in metastatic non-small cell lung cancer Oncologist 21119–1262016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hurria A, Togawa K, Mohile SG, et al. Predicting chemotherapy toxicity in older adults with cancer: A prospective multicenter study J Clin Oncol 293457–34652011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Yates P, Miaskowski C, Cataldo JK, et al. Differences in composition of symptom clusters between older and younger oncology patients J Pain Symptom Manage 491025–10342015 [DOI] [PubMed] [Google Scholar]
- 27.Rao A, Cohen HJ.Symptom management in the elderly cancer patient: Fatigue, pain, and depression J Natl Cancer Inst Monogr 150–1572004 [DOI] [PubMed] [Google Scholar]
- 28.Chang VT, Hwang SS, Feuerman M, et al. Symptom and quality of life survey of medical oncology patients at a veterans affairs medical center: A role for symptom assessment Cancer 881175–11832000 [DOI] [PubMed] [Google Scholar]
- 29.Scotte F, Bossi P, Carola E, et al. Addressing the quality of life needs of older patients with cancer: A SIOG consensus paper and practical guide Ann Oncol 291718–17262018 [DOI] [PubMed] [Google Scholar]
- 30.Wheelwright S, Darlington AS, Fitzsimmons D, et al. International validation of the EORTC QLQ-ELD14 questionnaire for assessment of health-related quality of life elderly patients with cancer Br J Cancer 109852–8582013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Soo WK, King M, Pope A, et al. The elderly functional index (ELFI), a patient-reported outcome measure of functional status in patients with cancer: A multicentre, prospective validation study Lancet 2E24–E332021 [DOI] [PubMed] [Google Scholar]
- 32.Nipp RD, Fuchs G, El-Jawahri A, et al. Sarcopenia is associated with quality of life and depression in patients with advanced cancer Oncologist 2397–1042018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Guerard EJ, Deal AM, Chang Y, et al. Frailty index developed from a cancer-specific geriatric assessment and the association with mortality among older adults with cancer J Natl Compr Canc Netw 15894–9022017 [DOI] [PubMed] [Google Scholar]
- 34.Ferrat E, Paillaud E, Caillet P, et al. Performance of four frailty classifications in older patients with cancer: Prospective elderly cancer patients cohort study J Clin Oncol 35766–7772017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Williams GR, Deal AM, Muss HB, et al. Frailty and skeletal muscle in older adults with cancer J Geriatr Oncol 968–732018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Shachar SS, Deal AM, Weinberg M, et al. Skeletal muscle measures as predictors of toxicity, hospitalization, and survival in patients with metastatic breast cancer receiving taxane-based chemotherapy Clin Cancer Res 23658–6652017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Adashek JJ, Subbiah IM. Caring for the caregiver: A systematic review characterising the experience of caregivers of older adults with advanced cancers. ESMO Open. 2020;5:e000862. doi: 10.1136/esmoopen-2020-000862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Romito F, Goldzweig G, Cormio C, et al. Informal caregiving for cancer patients Cancer 1192160–21692013suppl 11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Nipp RD, Zullig LL, Samsa G, et al. Identifying cancer patients who alter care or lifestyle due to treatment-related financial distress Psychooncology 25719–7252016 [DOI] [PubMed] [Google Scholar]
- 40.Arastu A, Patel A, Mohile SG, et al. Assessment of financial toxicity among older adults with advanced cancer. JAMA Netw Open. 2020;3:e2025810. doi: 10.1001/jamanetworkopen.2020.25810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Williams GR, Mackenzie A, Magnuson A, et al. Comorbidity in older adults with cancer J Geriatr Oncol 7249–2572016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Nipp RD, Ruddy M, Fuh CX, et al. Pilot randomized trial of a pharmacy intervention for older adults with cancer Oncologist 24211–2182019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Williams GR, Deal AM, Lund JL, et al. Patient-reported comorbidity and survival in older adults with cancer Oncologist 23433–4392018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Lees J, Chan A.Polypharmacy in elderly patients with cancer: Clinical implications and management Lancet Oncol 121249–12572011 [DOI] [PubMed] [Google Scholar]
- 45.Rose JH, O'Toole EE, Dawson NV, et al. Perspectives, preferences, care practices, and outcomes among older and middle-aged patients with late-stage cancer J Clin Oncol 224907–49172004 [DOI] [PubMed] [Google Scholar]
- 46.Thompson LL, Temel B, Fuh CX, et al. Perceptions of medical status and treatment goal among older adults with advanced cancer J Geriatr Oncol 11937–9432020 [DOI] [PubMed] [Google Scholar]
- 47.Weeks JC, Cook EF, O'Day SJ, et al. Relationship between cancer patients' predictions of prognosis and their treatment preferences JAMA 2791709–17141998 [DOI] [PubMed] [Google Scholar]
- 48.Brundage MD, Davidson JR, Mackillop WJ.Trading treatment toxicity for survival in locally advanced non-small cell lung cancer J Clin Oncol 15330–3401997 [DOI] [PubMed] [Google Scholar]
- 49.Mack JW, Wolfe J, Cook EF, et al. Hope and prognostic disclosure J Clin Oncol 255636–56422007 [DOI] [PubMed] [Google Scholar]
- 50.Nipp RD, El-Jawahri A, Fishbein JN, et al. The relationship between coping strategies, quality of life, and mood in patients with incurable cancer Cancer 1222110–21162016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Astrow AB, Wexler A, Texeira K, et al. Is failure to meet spiritual needs associated with cancer patients' perceptions of quality of care and their satisfaction with care? J Clin Oncol 255753–57572007 [DOI] [PubMed] [Google Scholar]
- 52.Balboni TA, Paulk ME, Balboni MJ, et al. Provision of spiritual care to patients with advanced cancer: Associations with medical care and quality of life near death J Clin Oncol 28445–4522010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Nipp RD, Tramontano AC, Kong CY, et al. Patterns and predictors of end-of-life care in older patients with pancreatic cancer Cancer Med 76401–64102018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Earle CC, Park ER, Lai B, et al. Identifying potential indicators of the quality of end-of-life cancer care from administrative data J Clin Oncol 211133–11382003 [DOI] [PubMed] [Google Scholar]
- 55.Parr JD, Zhang B, Nilsson ME, et al. The influence of age on the likelihood of receiving end-of-life care consistent with patient treatment preferences J Palliat Med 13719–7262010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Wright AA, Zhang B, Ray A, et al. Associations between end-of-life discussions, patient mental health, medical care near death, and caregiver bereavement adjustment JAMA 3001665–16732008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Bischoff KE, Sudore R, Miao Y, et al. Advance care planning and the quality of end-of-life care in older adults J Am Geriatr Soc 61209–2142013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Cohen MG, Althouse AD, Arnold RM, et al. Is advance care planning associated with decreased hope in advanced cancer? JCO Oncol Pract 17e248–e2562020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Mohile S, Dale W, Magnuson A, et al. Research priorities in geriatric oncology for 2013 and beyond Cancer Forum 37216–2212013 [PMC free article] [PubMed] [Google Scholar]
- 60.Mohile SG, Epstein RM, Hurria A, et al. Communication with older patients with cancer using geriatric assessment: A cluster-randomized clinical trial from the national cancer institute community oncology research program JAMA Oncol 6196–2042019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Nipp RD, Temel B, Fuh CX, et al. Pilot randomized trial of a transdisciplinary geriatric and palliative care intervention for older adults with cancer J Natl Compr Canc Netw 18591–5982020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Kane R, Solomon D, Beck J, et al. The future need for geriatric manpower in the United States N Engl J Med 3021327–13321980 [DOI] [PubMed] [Google Scholar]
- 63.Williams GR, Weaver KE, Lesser GJ, et al. Capacity to provide geriatric specialty care for older adults in community oncology practices Oncologist 251032–10382020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Bakitas M, Lyons KD, Hegel MT, et al. Effects of a palliative care intervention on clinical outcomes in patients with advanced cancer: The project ENABLE II randomized controlled trial JAMA 302741–7492009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Bakitas MA, Tosteson TD, Li Z, et al. Early versus delayed initiation of concurrent palliative oncology care: Patient outcomes in the ENABLE III randomized controlled trial J Clin Oncol 331438–14452015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Kavalieratos D, Corbelli J, Zhang D, et al. Association between palliative care and patient and caregiver outcomes: A systematic review and meta-analysis JAMA 3162104–21142016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Grudzen CR, Richardson LD, Johnson PN, et al. Emergency department-initiated palliative care in advanced cancer: A randomized clinical trial JAMA Oncol 2591–5982016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Zimmermann C, Swami N, Krzyzanowska M, et al. Early palliative care for patients with advanced cancer: A cluster-randomised controlled trial Lancet 3831721–17302014 [DOI] [PubMed] [Google Scholar]
- 69.Temel JS, Greer JA, Muzikansky A, et al. Early palliative care for patients with metastatic non-small-cell lung cancer N Engl J Med 363733–7422010 [DOI] [PubMed] [Google Scholar]
- 70.Temel JS, Greer JA, El-Jawahri A, et al. Effects of early integrated palliative care in patients with lung and gi cancer: A randomized clinical trial J Clin Oncol 35834–8412017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.El-Jawahri A, LeBlanc T, VanDusen H, et al. Effect of inpatient palliative care on quality of life 2 weeks after hematopoietic stem cell transplantation: A randomized clinical trial JAMA 3162094–21032016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Dionne-Odom JN, Azuero A, Lyons KD, et al. Benefits of early versus delayed palliative care to informal family caregivers of patients with advanced cancer: Outcomes from the ENABLE III randomized controlled trial J Clin Oncol 331446–14522015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Nipp RD, Temel JS.Harnessing the power of patient-reported outcomes in oncology Clin Cancer Res 241777–17792018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Basch E, Deal AM, Dueck AC, et al. Overall survival results of a trial assessing patient-reported outcomes for symptom monitoring during routine cancer treatment JAMA 318197–1982017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Nipp RD, El-Jawahri A, Ruddy M, et al. Pilot randomized trial of an electronic symptom monitoring intervention for hospitalized patients with cancer Ann Oncol 30274–2802019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Nipp RD, Horick NK, Deal AM, et al. Differential effects of an electronic symptom monitoring intervention based on the age of patients with advanced cancer Ann Oncol 31123–1302020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Loscalzo M, Clark K, Dillehunt J, et al. SupportScreen: A model for improving patient outcomes. JNCCN. 2010;8 [Google Scholar]
- 78.Hurria A, Akiba C, Kim J, et al. Reliability, validity, and feasibility of a computer-based geriatric assessment for older adults with cancer J Oncol Pract 12e1025–e10342016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Wong FL, Stiller T, Obenchain R, et al. Validation of a biopsychosocial distress screening tool, “you, your family and COH are a team” Psychooncology 282396–24052019 [DOI] [PubMed] [Google Scholar]
- 80.Clark K, Bergerot CD, Philip EJ, et al. Biopsychosocial problem-related distress in cancer: Examining the role of sex and age Psychooncology 261562–15682017 [DOI] [PubMed] [Google Scholar]
- 81.Boyes A, Girgis A, Lecathelinais C.Brief assessment of adult cancer patients' perceived needs: Development and validation of the 34-item supportive care needs survey (SCNS-SF34) J Eval Clin Pract 15602–6062009 [DOI] [PubMed] [Google Scholar]
- 82.Holland JC, Andersen B, Breitbart WS, et al. Distress management J Natl Compr Canc Netw 11190–2092013 [DOI] [PubMed] [Google Scholar]
- 83.Maggiore RJ, Gorawara-Bhat R, Levine SK, et al. Perceptions, attitudes, and experiences of hematology/oncology fellows toward incorporating geriatrics in their training J Geriatr Oncol 5106–1152014 [DOI] [PubMed] [Google Scholar]
- 84.Maggiore RJ, Dale W, Hurria A, et al. Hematology-oncology fellows' training in geriatrics and geriatric oncology: Findings from an American Society of Clinical Oncology-sponsored national survey J Oncol Pract 13e900–e9082017 [DOI] [PubMed] [Google Scholar]
- 85.Thomas RA, Curley B, Wen S, et al. Palliative care training during fellowship: A national survey of U.S. Hematology and Oncology Fellows J Palliat Med 18747–7512015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Paladino J, Bernacki R, Neville BA, et al. Evaluating an intervention to improve communication between oncology clinicians and patients with life-limiting cancer: A cluster randomized clinical trial of the serious illness care program JAMA Oncol 5801–8092019 [DOI] [PubMed] [Google Scholar]
- 87.Nightingale G, Burhenn PS, Puts M, et al. Integrating nurses and allied health professionals in the care of older adults with cancer: A report from the International Society of Geriatric Oncology Nursing and Allied Health Interest Group J Geriatr Oncol 11187–1902020 [DOI] [PubMed] [Google Scholar]
- 88.Huffman JC, Niazi SK, Rundell JR, et al. Essential articles on collaborative care models for the treatment of psychiatric disorders in medical settings: A publication by the academy of psychosomatic medicine research and evidence-based practice committee Psychosomatics 55109–1222014 [DOI] [PubMed] [Google Scholar]
- 89.Richards DA.Stepped care: A method to deliver increased access to psychological therapies Can J Psychiatry 57210–2152012 [DOI] [PubMed] [Google Scholar]
- 90.DiGiovanni G, Mousaw K, Lloyd T, et al. Development of a telehealth geriatric assessment model in response to the COVID-19 pandemic J Geriatr Oncol 11761–7632020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.McCleary NJ, Wigler D, Berry D, et al. Feasibility of computer-based self-administered cancer-specific geriatric assessment in older patients with gastrointestinal malignancy Oncologist 1864–722013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Levine DM, Lipsitz SR, Linder JA.Trends in seniors' use of digital health technology in the United States, 2011-2014 JAMA 316538–5402016 [DOI] [PubMed] [Google Scholar]
- 93.Nipp RD, Yao NA, Lowenstein LM, et al. Pragmatic study designs for older adults with cancer: Report from the U13 conference J Geriatr Oncol 7234–2412016 [DOI] [PubMed] [Google Scholar]
- 94.Qian CL, Knight HP, Ferrone CR, et al. Randomized trial of a perioperative geriatric intervention for older adults with cancer. J Clin Oncol. 2020;38(15_suppl):12012. doi: 10.1016/j.jgo.2022.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Baitar A, Kenis C, Moor R, et al. Implementation of geriatric assessment-based recommendations in older patients with cancer: A multicentre prospective study J Geriatr Oncol 6401–4102015 [DOI] [PubMed] [Google Scholar]
- 96.Magnuson A, Lemelman T, Pandya C, et al. Geriatric assessment with management intervention in older adults with cancer: A randomized pilot study Support Care Cancer 26605–6132018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Horgan AM, Leighl NB, Coate L, et al. Impact and feasibility of a comprehensive geriatric assessment in the oncology setting: A pilot study Am J Clin Oncol 35322–3282012 [DOI] [PubMed] [Google Scholar]
- 98.Ommundsen N, Wyller TB, Nesbakken A, et al. Preoperative geriatric assessment and tailored interventions in frail older patients with colorectal cancer: A randomized controlled trial Colorectal Dis 2016–252018 [DOI] [PubMed] [Google Scholar]
- 99.Hempenius L, Slaets JP, van Asselt D, et al. Outcomes of a geriatric liaison intervention to prevent the development of postoperative delirium in frail elderly cancer patients: Report on a multicentre, randomized, controlled trial. PLoS One. 2013;8:e64834. doi: 10.1371/journal.pone.0064834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Quill TE, Abernethy AP.Generalist plus specialist palliative care—Creating a more sustainable model N Engl J Med 3681173–11752013 [DOI] [PubMed] [Google Scholar]
- 101.Kenis C, Decoster L, Van Puyvelde K, et al. Performance of two geriatric screening tools in older patients with cancer J Clin Oncol 3219–262014 [DOI] [PubMed] [Google Scholar]
- 102.Mohile SG, Dale W, Somerfield MR, et al. Practical assessment and management of vulnerabilities in older patients receiving chemotherapy: ASCO guideline for geriatric oncology summary J Oncol Pract 14442–4462018 [DOI] [PMC free article] [PubMed] [Google Scholar]