Abstract
Alginate is an edible heteropolysaccharide that abundantly available in the brown seaweed and the capsule of bacteria such as Azotobacter sp. and Pseudomonas sp. Owing to alginate gel forming capability, it is widely used in food, textile and paper industries; and to a lesser extent in biomedical applications as biomaterial to promote wound healing and tissue regeneration. This is evident from the rising use of alginate-based dressing for heavily exuding wound and their mass availability in the market nowadays. However, alginate also has limitation. When in contact with physiological environment, alginate could gelate into softer structure, consequently limits its potential in the soft tissue regeneration and becomes inappropriate for the usage related to load bearing body parts. To cater this problem, wide range of materials have been added to alginate structure, producing sturdy composite materials. For instance, the incorporation of adhesive peptide and natural polymer or synthetic polymer to alginate moieties creates an improved composite material, which not only possesses better mechanical properties compared to native alginate, but also grants additional healing capability and promote better tissue regeneration. In addition, drug release kinetic and cell viability can be further improved when alginate composite is used as encapsulating agent. In this review, preparation of alginate and alginate composite in various forms (fibre, bead, hydrogel, and 3D-printed matrices) used for biomedical application is described first, followed by the discussion of latest trend related to alginate composite utilization in wound dressing, drug delivery, and tissue engineering applications.
Keywords: Alginate, Alginate composite, Tissue engineering, Wound dressing, Drug delivery
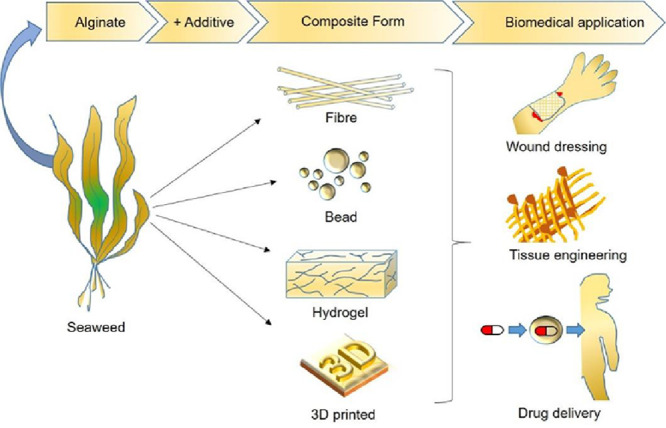
Graphical abstract
Alginate and alginate composite in four major forms (fibre, bead, hydrogel, and 3D printed matrices) and their use in selected biomedical application (wound dressing, tissue engineering, and drug delivery).
1. Introduction
Biomaterials either natural or synthetic are widely used in biomedical applications to support, enhance, or replace damaged tissues or biological functions. In clinical setting, biomaterials are used as medical implants and devices to promote healing and serve as a carrier for cells during human tissues regeneration process. It can also be utilised as a part of biosensors architecture, drug delivery carrier, and medical imaging material [1].
Utilisation of biomaterials dates far back into ancient civilisations in which Egyptians used animal sinew as suture while Chinese and Indians used waxes, glues, and tissues to reconstruct affected and injured body parts [2]. Over the centuries, as surgical techniques and production of synthetic material advances, detailed knowledge on biomaterial was steadily gained. Although natural material such as glue, rubber, wood and tissues are preferred choice during early days, continuous effort by biomaterial researchers around the globe have made synthetic materials like metals, ceramics, plastics and glass to be equally accepted for biomaterial construction. Nowadays, knowledge on which biomaterial will be tolerated or rejected by the body are largely known. In addition, synergistic performance while having compatible interaction between composite biomaterial and bodily tissues compared to non-composite biomaterial are also almost well understood [3]. With regards to healing and regenerating human tissues, natural materials still often utilised as they are biocompatible and most importantly biodegradable within the body. Although all biomaterials are biocompatible to prevent post-acute or -chronic adverse effects, biomaterials that able to degrade will avoid a second surgical event for removal of the material after the tissues are healed and regenerated [4]. Ability to control the rate of degradation of the biomaterials is another important criterion to ensure the tissues heal and regenerate properly [5]. Additionally, the degraded biomaterials should not be toxic and can be easily removed from the body [6].
Alginate is one of the biological substances that is continually used for healing and regenerating human tissue particularly for wound dressing [7]. As alginate is used in food preparation for human consumption, it is considered as safe for biomedical applications. Alginate is biodegradable as well since it dissolved slowly in the body when cross-linking agents in the alginate release and exchange reaction with the monovalent cations found in the body fluids. The rate of dissolution of alginate can be controlled by oxidation [8] and reduction of molecular weight [9] of the alginate. Ultimately, alginate capacity to form gel is the major reason for its uses mostly in soft tissue engineering and wound healing. Nowadays, alginate is mixed with other distinct materials to form alginate composites that suit the need of other types of biomedical applications [10], [11], [12], [13] and also to enhance its capacity in soft tissue engineering and healing [11,14,15]. In this review paper, we describe the preparation of alginate and alginate composites and discuss its biomedical applications, specifically wound dressing, drug delivery, and tissue engineering. Future outlooks on the preparation and biomedical applications of alginate and alginate composite are also included.
2. Alginate and alginate composites
Alginate is a polysaccharide that occurs naturally in the cell wall of algae and bacterial capsule of Azotobacter sp. and Pseudomonas sp. In brown algae (also called brown seaweeds), the presence of alginate in their cell walls provide flexibility and strong structure to the algae and buffer them from possible injury when the algae are exposed to strong sea water waves [16]. In bacteria, it forms protective capsule, aids in biofilm formation [17] and assists bacterial adherence and colonisation [18]. Because of alginate capability of forming hydrogel, alginate is widely known as stabiliser, thickener, gelling agent and emulsifier [19] since its discovery from kelp in 1881 by Stanford. After the patent of alginate extraction from algae was granted in 1930s, alginate had been extracted in large scale from brown algae (Phaeophyceae sp.) such as Laminaria hyperborea, Laminaria digitata, Laminaria japonica, Ascophyllum nodosum, and Macrocystis pyrifera [19]. Chemical companies around the world such as China Seaweed Industrial Association, Danisno Cultor (Denmark), Degussa Texturant Systems (Germany), FMC BioPolymer (USA), ISP Alginates Ltd (UK), and Kimitsu Chemical Industries Co. Ltd (Japan) have commercially extracted alginate [20] with total production is estimated 30 000 tons, primarily from the genera Laminaria and Macrocystis [17].
Extraction of alginate from brown algae involves multiple processes [21], including initial treatment with mineral acid to change salts of alginic acid (alginates) in the algae into free alginic acid. This is followed by neutralisation with either sodium carbonate or sodium hydroxide to form water soluble sodium alginate. To recover the soluble alginate, precipitation with either calcium chloride or mineral acid can be applied and insoluble calcium alginate fibre or alginic acid gel is obtained, respectively. Both calcium alginate and alginic acid are later mixed with sodium carbonate to produce sodium alginate. Sodium alginate is the common and largest alginate-base salt produced in the industry [22]. Other types of alginate salt produced are calcium alginate, potassium alginate and ammonium alginate [23]. Calcium alginate is produced in the process of alginate extraction as described earlier while potassium alginate and ammonium alginate are produced by adding appropriate alkali, usually potassium carbonate or ammonium hydroxide, respectively to the alginic acid gel.
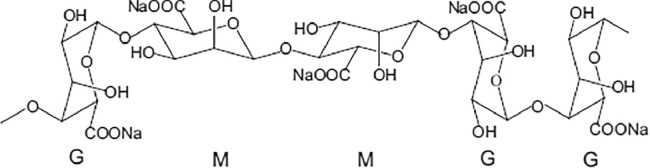
Alginates composed of 1,4-linked β-d-mannuronic acid (M) and 1,4 α-l-guluronic acid (G) residues (Fig. 1) that form blocks of repeated G residues, repeated M residues and alternating G and M residues [24]. The composition and the sequence of G and M residues depends on type of natural resources used to extract alginate. Alginate extracted from algae, L. hyperborean has 60% of G content while alginates from other commercial algae species have 14%−31% G content. It was suggested that only carboxylate groups of the G residues crosslink with divalent cations such as Ca2+, Mg2+ to form hydrogels. Thus, alginates with high G content form stiffer hydrogel while alginates with high M content generate softer elastic hydrogel [25]. The molecular weight of alginate ranges between 32 000 to 400 000 g/mol. The higher the molecular weight of the alginate, the more viscous it gets in the gel preparation. Although alginate is considered as biocompatible, non-toxic materials and non-immunogenic [26], there are claims that alginate with high M content tends be more immunogenic than alginate with high G content [27].
Fig. 1.
Chemical structure of alginate composed of 1,4-linked β-d-mannuronic acid M and 1,4 α-l-guluronic acid G residues. Adapted with permission from [24]. Copyright (2011), Elsevier.
To enhance alginate physical characteristics, other substances had been mixed with alginate to form alginate composite. Alginate composites are formed by adding natural polymer such as collagen, chitosan and gelatin, synthetic polymer such as polylactide and polypyrrole, and inorganic compounds such as tetraethylorthosilicate (TEOS) and hydroxyapatite (HA) [28,29]. Blending other types of material, for example ceramic, bioglass, inorganic nanoparticle, and inorganic carbon-based material had been explored as well [29], [30], [31]. Several alginate composites had shown successful results and available commercially particularly for wound dressing application [19] while others are still under investigation.
For both alginate and alginate composite to be used for various biomedical applications, they had to be made into different forms such as fibre, bead, hydrogel, or 3D printed material depending on the specific demand of each biomedical applications. In the following subsections, preparation of each form of both alginate and alginate composite are discussed.
2.1. Fibre form
The use of alginate in fibre form as biomedical materials has attracted extensive interest because of their high surface area, ease of handling, and its ability to retain mechanical integrity while in wet state. The later properties being crucial given the absorbent nature of alginate, especially when used as dressing for heavily exuding wound [32]. For example, 3M™ Tegaderm™ Alginate High Integrity and High Gelling Alginate Dressing, made from hydro-entangled nonwoven web of calcium alginate fibres [33], readily form a gelatinous mass which maintain a moist healing environment while maintaining its form factor integrity upon contact with exudates. Nevertheless, at low weight basis, alginate fibrous webs can collapse under its own weight when swollen due to insufficient entanglement, leaving fibrous residue at the wound site when the dressing is removed.
Blending the alginate fibres with fibres that do not swell in saline – a common solution used when cleaning wound site – not only increase the strength of overall fabric, but also reduce the cost of overall dressing. Improvement can be sought by incorporating reinforcing or bioactive material within the alginate fibre itself, creating a composite fibre which are not only stronger, but able to confer additional healing properties. Below are preparations of alginate fibre and alginate composite fibre using traditional wet-spinning method, electrospinning and microfluidic system.
2.1.1. Fibre formation via wet spinning
During traditional wet spinning process of pure alginate fibre, extruded spinning dope (i.e. water soluble sodium alginate) precipitate upon contact with calcium chloride solution in coagulation bath to produce water insoluble calcium alginate fibre [34]. The as-made calcium alginate fibre can then be stretched, washed and dried. Because physical stretching or drawing increases the degree of molecular alignment within the fibre which in turn improve overall fibre strength [35], care must be taken so that breakage does not occur during drawing. This care usually accomplished by adjusting the drawing ratio between output and input filament velocity in the drawing zone or ratio between length of drawn and undrawn fibre [36].
To prepare composite wet spun fibre, sodium alginate usually blended with substance of interest at certain ratio and extruded via spinneret with multiple holes or syringe. The extruded fibre then passed into coagulation bath that typically comprise of CaCl2 solution to crosslink the alginate. These fibres often stretched further to improve its final mechanical properties. To enhance wet-spun alginate fibre mechanical and liquid absorption capability, wet spun alginate fibre has been incorporated with reinforcing materials like (1) natural-based polymer such as chitin [37,38], chitosan [39], [40], [41], cellulose [42] carrageenan [43], gelatin [44], starch [45], (2) synthetic-based polymer such as polypyrrole [46], (3) carbon based material such as graphene oxide [47], carbon nanotube [30], or (4) inorganic nanoparticle such as silver [31] to produce composite fibre. Table 1 shows few additive materials that have been used lately to prepare alginate fibre composite using wet spinning method.
Table 1.
Alginate composite fibre prepared via wet spinning technique.
| Additive material | Additive material content (%,wt) | Composite preparation | Composite characterisation | Ref. |
|---|---|---|---|---|
| Graphene oxide | 2–8 | Sodium alginate/graphene oxide solution extruded via syringe into CaCl2 bath followed by fibre stretching in CaCl2 bath at 50% and 100% draw ratio | Highest modulus of 9.39 GPa (▲118%) and highest strength of 0.86 GPa (▲169%) obtained at 4% graphene oxide content Water absorbency ranged between 0.93 – 1.06 g/g and independent of graphene oxide content |
[47] |
| Carboxyl methyl chitosan | 10–70 |
4% sodium alginate/5% carboxylmethyl chitosan blend at 9/1, 7/3, 5/5, 3/7 ratio blend solution extruded via spinneret (30 holes, 0.08 mm diameter) into 5% cacl2 bath followed by fibre stretching in water at 20% draw ratio |
Highest tenacity of 13.8 cn/tex (▲35%) obtained at 30% filler content highest elongation of 23.1% (▲27%) obtained at 10% filler content water retention increased in range of 130% – 398% for filler loaded fibre compared to 91% for pure alginate fibre |
[39] |
| Gelatin | 9–33 |
4% sodium alginate/4% gelatin blend at 10/5, 10/4, 10/3, 10/2, 10/1 ratio 5% oxidized starch added to blend mixture sodium alginate/gelatin/starch solution extruded via spinneret (900 holes, 70 µm diameter) into 5% cacl2 bath followed by fibre stretching in ethanol at 150% draw ratio |
Highest tenacity of 1.29 cn/dtex and highest elongation of 4.41% obtained at 16.7% gelatin content highest water absorption of 335% (▲19%) and highest water retention of 311% (▲19%) obtained at 16.7% gelatin content |
[44] |
| Cellulose nanocrystal | 0.5–16 |
Sodium alginate/cellulose nanocrystal solution extruded via spinneret into 5% CaCl2 bath followed by fibre stretching at 1.2 draw ratio | Highest tenacity of 2.05 cN/dtex (▲33%) and highest elongation of 15% (▲82%) obtained at 2% cellulose nanocrystal content | [42] |
| Chitosan | 1–2 (w/v chitosan solution) | 10% sodium alginate solution extruded via spinneret (1 hole, 0.6 mm diameter) into 8% CaCl2 bath Extruded fibre immersed in 1% or 2% chitosan bath |
Highest modulus of 0.43 cN/dtex (▲13%), highest strength of 1.77 cN/dtex (▲13%) and highest elongation of 10% (▲4%) obtained when alginate fibre immersed in 1% chitosan bath | [40] |
| Methylene blue nanocapsule | 3–15 |
Nanocapsule first created by blending methylene blue and NaHCO3 with alginate solution Nanocapsule then mixed to 3.5% alginate solution and extruded via spinneret (50 holes, 70 µm diameter) into 2.5% CaCl2 bath followed by fibre stretching at 1:5 draw ratio |
Highest tenacity of 15 cN/dtex (▲16%) obtained at 6% nanocapsule content Absorption capacity enhanced from 1.1 – 1.2 g/g in water to 13 – 66 g/g in saline solution |
[48] |
| Chitin | 33–75 | Alginic acid/chitin dissolved in 1-ethyl-3-methylimidazolium acetate ionic liquid and extruded via syringe into CaCO3 bath. 1.75 wt% chitin to 0.58 wt% alginic acid in ionic liquid yield the optimal fibre |
Composite fibre exhibited 22% decrease in modulus (6.9 GPa), 16% decrease in strength (216 MPa), 9% decrease in elongation (4.1%), and 19% decrease in water uptake (2.06 g/g), but still strong enough to be used directly as structural material for wound care | [37] |
| Silver nanoparticle | 0.05 or 0.005 mM silver nitrate solution | 2% sodium alginate solution extruded via syringe into 1 M CaCl2 bath. Extruded fibre immersed in silver nitrate solution (1 h) followed by sodium borohydride (10 min) to obtain reduced metallic silver nanoparticle. |
Composite fibre promote faster wound closure, increased epidermal thickness, and decreased neutrophil at local wound site | [31] |
| Starch, salicylic acid drug | 10–70 | Sodium alginate/starch solution extruded via spinneret (30 holes, 0.08 mm diameter) into 10% CaCl2 bath followed by fibre stretching in water at 20% draw ratio Drug-laden fibre was loaded with salicylic acid |
Highest tenacity of 14.2 cN/tex (▲29%) obtained at 10% starch content. Highest elongation of 27% (▲69%) obtained at 30% starch content. |
[45] |
| Carrageenanchondrocyte cells | 20–50 | Two type of alginate used in blend: k-carrageenan and l-carrageenan. Sodium alginate/carrageenan solution extruded via syringe into CaCl2/2% KCl bath. For cell-laden fibre, chondrocyte cells (ATDC5) encapsulated in fibre precursor at concentration of 1 × 106 cells/ml |
Noncytotoxic. Higher viability of cells after 3 weeks in k- type compared to l- type alginate/carrageenan composite | [43] |
| Chitosan whisker | 0.2–1.0 | Sodium alginate/chitosan whisker solution extruded via spinneret (30 holes, 0.02 mm diameter) into 1st coagulation bath (5% CaCl2 in 50% MeOH) and 2nd coagulation bath (MeOH) followed by fibre stretching at 1.2 draw ratio | Highest tenacity of 10 cN/tex (▲67%) obtained at 1% whisker content. Highest elongation of 28% (▼42%) obtained at 0.6% whisker content. |
[41] |
| Chitin whisker | 0.05–2 | Sodium alginate/chitin whisker solution extruded via spinneret (30 holes, 0.02 mm diameter) into 1st coagulation bath (5% CaCl2 in 50% MeOH) and 2nd coagulation bath (MeOH) followed by fibre stretching at 1.2 draw ratio | Highest tenacity of 10.4 cN/tex (▲16%) obtained at 0.15% whisker content. Highest elongation of 26% (▲44%) obtained at 0.10% whisker content |
[38] |
| Single walled carbon nanotube (SWCNT) | 0.6–23 | Sodium alginate/SWCNT solution extruded via syringe (0.85 mm diameter) into 1st coagulation (15% CaCl2, 15 min) and 2nd coagulation bath (3% CaCl2, overnight) |
Highest modulus of 6.67 GPa (▲93%) and highest strength of 250 MPa (▲25%) obtained at 1.2% SWCNT content At 23 wt% filler loading, resistivity decreased one to two order of magnitude |
[30] |
| Polypyrrole | 72 | SWCNT is added for the final ratio of pyrrole monomer/sodium alginate/SWCNT at 2.63/1/0.04 Sodium alginate/polypyrrole and sodium alginate/polypyrrole/SWCNT solution extruded via continuous wet-spinning into 5% CaCl2 bath and polymerization line |
Addition of polypyrrole decrease composite strength by 61% (140 MPa) and elongation by 33% (8%), which may be attributed to the low compatibility of alginate and polypyrrole Addition of carbon nanotube increased composite fibre strength by 79% (250 MPa) and elongation by 25% (10%) Alginate/polypyrrole/SWCNT composite fibre gave significantly higher electrical conductivity compared to non-composite fibre, potential as support for biomedical sensor and actuators |
[46] |
2.1.2. Fibre formation via electrospinning
Compared to wet spinning, electrospinning allows the fabrication of ultrathin fibre by placing polymer melt in-between charged electrode. When strong electric field is introduced, typically in the region of kilovolt (kV), the polymer melt will be ejected towards collector electrode, forming a fibrous mat with individual fibre diameter ranging from 10 to hundreds of micrometres [49]. Electrospinning of alginate have found wide application in biomedical field because it can provide higher surface area compared to traditional wet-spun technique [50]. However, it is difficult to obtain continuous and uniform fibrous structure from pure alginate solutions via electrospinning due to lack of molecular entanglement and the rigid structure of alginate. Polymer such as polyvinyl alcohol (PVA) and polyethylene oxide (PEO) often used as spinning aid as they can provide sufficient entanglement with alginate at molecular level. Furthermore, addition of surfactant might reduce the high surface tension of alginate, leading to bead-free and uniform electrospun fibre [51]. Because of the addition of spinning aid, it is safe to say that almost all electrospun alginate fibres are composite fibres.
The morphology of electrospun fibre governed by parameters such as solution feeding flowrate, applied voltage, and distance between electrospinning needle to the target. Table 2 depicts different additive material and processing parameter used during electrospinning of alginate fibre composites.
Table 2.
Alginate fibre composite prepared via electrospinning technique.
| Additive material | Additive material content (wt%) | Composite preparation | Composite characterisation | Ref. |
|---|---|---|---|---|
| Essential oil | 0.5–1.5 | Carrier: PVA 2% sodium alginate/8% PVA blend at 20/80 and 30/70 ratio Filler is varied according to 3 different type of essential oil: clove, cinnamon, and lavender Sodium alginate/PVA/filler electrospun toward cotton gauze at varied voltage (15, 20, 25 kV), distance to target (10, 15, 20 cm), and flowrate (0.2, 0.25, 0.3 ml/h) |
Uniform fibres obtained in viscosity range 1120 – 1280 cP. Essential oil addition increase viscosity but reduce surface tension and conductivity of spinning solution Uniform and bead free fibre obtained at 20/80 sodium alginate/PVA blend with 1.5% clove oil at electrospinning parameter of 20 kV voltage, 15 cm distance, and 0.2 ml/h flowrate |
[52] |
| ZnO NPs | 0.5–5 | Carrier: PVA 2% sodium alginate/16% PVA blend at 1/3, 1/1, and 3/1 ratio Sodium alginate/PVA/ZnO electrospun toward aluminium target at 17 kV voltage, 5 cm distance to target, and 0.1 ml/h flow rate |
Average fibre diameter of 220 – 360 nm. | [53] |
| Chitosan | 70:30 filler/ PEO |
Carrier: PEO 2.4% sodium alginate/1.6% PEO blend at 1/1 Sodium alginate/PEO and chitosan/PEO coaxially electrospun toward aluminium target at varied voltage (22 to 30 kV), distance to target (7 to 15 cm) and flowrate (0.4 to 0.5 ml/h) |
Average fibre diameter of 154 nm. Mixture of polyanionic alginate and polycationic chitosan form a spontaneous ionic complex leading to core/shell nanofiber composite, where alginate as core and chitosan as shell Composite maintain its integrity after 24 h immersion in water |
[54] |
| Organic rectorite | 1 | Carrier: PVA 2% sodium alginate/10% PVA blend at 10/90, 20/80, 40/60, 60/40 ratio Sodium alginate/PVA/rectorite electrospun toward aluminium target at 17 kV voltage, 5 cm distance to target, and 0.1 ml/h flow rate |
Organic rectorite promote bacterial inhibition ability against E. coli and S. aureus | [55] |
| Soy protein isolate (SPI), vancomycin drug | 10–50 | Carrier:PEO 3% sodium alginate/3% PVA blend at 7/3, 6.3/2.7, 5.6/2.4, 4.9/2.1, 4.2/1.8, 3.5/1.5 ratio Sodium alginate/PEO/SPI with and without vancomycin drug electrospun toward aluminium target at 15 kV voltage, 15 cm distance to target, and 0.5 ml/h flowrate |
Uniform fibre with average diameter of 200 nm obtained at 5.6/2.4 sodium alginate/PEO blend with 20% filler and further loaded with vancomycin drug Upon immersion in water, drug release was found to be 4% at 4 h, 69% at 16 h and 85% after 30 h |
[56] |
| Glutamine | 35 mg/ml | Carrier: polyethylene oxide (PEO) 2% sodium alginate/6% PEO blend at 30/70 Sodium alginate/PEO/glutamine electrospun toward aluminium target at varied voltage (10 – 16 kV), distance to target (10 cm and 15 cm), and flowrate (0.1 – 1.0 ml/h) |
Average fibre diameter of 160 nm. Work of mucoadhesion, tensile strength and elongation at break values of the glutamine loaded nanofibers were found to be 0.165 mJ/cm2, 2.61 MPa and 6.62% respectively. 85% of drug diffused from nanofiber at the end of 4 h, shows potential as an oromucosal drug delivery system |
[57] |
| Gatifloxacin | 1 | Carrier: PVA 2% sodium alginate/10% PVA blend at 3/7, 2/8, 1/9 ratio Sodium alginate/PVA/gatifloxacin electrospun toward aluminium target at 20 kV voltage, 10 cm distance to target, and 0.1 ml/h flow rate |
Uniform fibre obtained at 3/7 NaAlg/PEO blend with 1% filler Upon immersion in saline solution, drug release was found to be 10% at 1 h, 44% at 3 h and 93% after 8 h |
[58] |
| Pullulan | 10 | Carrier: not used Sodium alginate concentration: 0.8%, 1.6%, 2.4% Sodium alginate/pullulan blend electrospun using free surface electrospinning machine at 30 kV with 300 mm length electrode positioned 180 mm above ground electrode |
Continuous and bead free fibre with diameter 57 – 87 nm obtained at sodium alginate concentration between 0.8% to 1.6% | [59] |
| Ciproflaxin | 0.02–0.48 | Carrier: PEO Surfactant added: Triton X-100 or Pluronic F-127 2%−5% sodium alginate/1.5%−2.0% PEO blend at 1/1 ratio Sodium alginate/PEO/ciproflaxin electrospun toward aluminium target at varied voltage (6 – 10 kV), distance to target (15 – 10 cm) and flowrate (0.1 – 1.0 ml/h) |
Uniform fibre with diameter 119 – 161 nm obtained only when surfactant is added Upon immersion in saline solution, drug release was found to be 24% in the first 20 h |
[60] |
| Nano hydroxyl apatite (nHAP) | 1.67–10.02 mg/ml | Carrier: PVA 2% sodium alginate/14% PVA blend at 1/2 ratio Sodium alginate/PVA/nHAP electrospun toward aluminium target at 11 kV voltage, 17 cm distance to target, and 0.32 ml/h flowrate |
Addition of 1.64 wt% nHAP enhanced fibre tensile strength enhanced about 45% | [61] |
| Poly-caprolactone (PCL) | 10 | Carrier: not used Sodium alginate concentration: 1%, 3%, 5% Sodium alginate/PCL dissolved in 20/80 methylene chloride/dimethyl formamide solution Electrospun at 1 kV voltage and 0.5 ml/h flowrate toward PCL strut that is immersed in ethanol |
Compared to pure PCL scaffold, scaffold that embed alginate/PCL fibre showed significantly enhanced hydrophilic behaviour, water absorption (∼8 fold) and significantly biological activities (∼1.6 fold for cell viability at 7 d ∼2.3 fold for osteogenic differentiation activity at 14 d, and 6.4 fold for calcium mineralisation at 14 d) | [62] |
| Methycrylated gelatin (GelMA) | 20–50 | Carrier: PEO Surfactant added: Pluronic F-127 20% – 50% (w/v) GelMA added to different sodium alginate/PEO ratio 0.1% photoinitiator is added to solution mixture in order to chemically crosslink GelMA upon 365 nm UV exposure on resulting composite fibre Sodium alginate/PEO/GelMA electrospun toward either aluminium target or ethanol bath at 7 kV voltage, 7 cm distance to target, and 0.1 ml/h flowrate |
[63] | |
| Chitosan, silver NP | 1% silver NP in chitosan solution | Carrier: PEO Surfactant added: Triton X-100 3% sodium alginate/3% PEO blend at 50/50 ratio Sodium alginate/PEO electrospun toward aluminium target at 17 kV voltage, 17 cm distance to target, and 0.8 ml/h flow rate Electrospun fibre immersed in chitosan/silver nanoparticle solution at varied duration (5, 10, 15 min) |
Silver nanoparticles impregnated into electrospun alginate nanofibres by complexion with chitosan Swelling of fibrous electrospun mat decrease from ∼276% to ∼150% with increasing immersion time in chitosan/silver nanoparticle solution |
[64] |
| MgO NP | 10 | Carrier: PVA 2% sodium alginate/10% MgO added to 10% PVA at 3/2 ratio Sodium alginate/PVA/MgO electrospun toward aluminium target at varied voltage (26 – 28 kV) and flowrate (8 – 10 µl/min) with distance to target of 10 cm |
Bead free fibre with diameter between 60 – 250 nm Enhanced mechanical (E = 0.17 GPa, ▲240%; σ = 4.33 MPa, ▲179%; ε = 6.73%, ▼26%) and improved thermal stability. |
[65] |
2.1.3. Fibre formation via microfluidic system
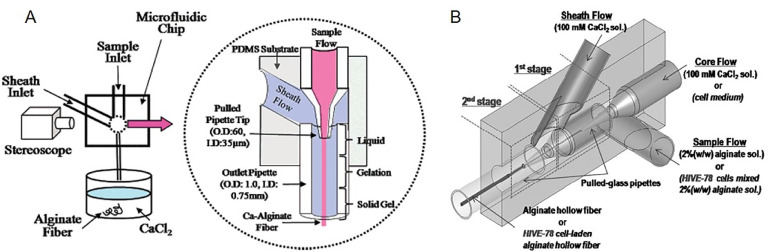
Microfluidic system allows precise control of dimensional and morphological characteristic of resulting microfibre due to the formation of stable laminar flow upon injection into microchannel [66]. Pioneering work that produced continuous alginate microfibres using microfluidic system based their work on coaxial flow, whereby the sample flow (sodium alginate) and sheath flow (CaCl2) met at intersection and leaving the outlet as microfibre [67]. The idea has been further refined to create a hollow fibre by introducing core fluid in the innermost layer which result in the formation of a three-layered coaxial flow that consists of core, sample, and sheath fluid [68]. Fig. 2 depicts the concept of coaxial flow in generating alginate microfibre.
Fig. 2.
Schematic of microfluidic concept for (A) continuous alginate microfiber generation. Adapted with permission from [67], Copyright (2007) American Chemical Society, and (B) continuous alginate hollow microfiber generation. Adapted with permission from [68]. Copyright (2009), John Wiley and Sons.
Most of alginate composite microfibre fabricated using microfluidic system often carries living cells within it. Compared to wet spinning method where thick fibre can impair cells nutrient and metabolic product exchange, or to electrospinning where high electrical field render cell encapsulation unfeasible, microfluidic system offer gentler and controllable microfibre fabrication, making cell encapsulation within fibre possible. To enhance composite microfibre fabricated using microfluidic system with incorporated cells within it, incorporation of extracellular matrix (ECM)-like constituent is crucial so that suitable cell microenvironment can be provided. Therefore, production of composite alginate microfibers enriched with different ECM constituents such as gelatine [69,70], collagen [71], hyaluronic acid [72], urinary bladder material [69], and chondroitin sulphate [72] has been investigated and successful results had been obtained. Table 3 depicts few microfluidic systems that have been employed to generate cell-laden alginate composite microfibre.
Table 3.
Alginate composite fibre prepared via microfluidic technique.
| Filler | Cell incorporation | Composite preparation | Composite characterisation | Ref. |
|---|---|---|---|---|
| ECM, Methacrylated gelatin (GelMA) | Liver HepG2, embryo fibroblast cells (NIH 3T3), Human umbilical vein endothelial cells (HUVECs) | Microfluidic system: multibarrel capillary inlet and several single-barrel capillaries inlet Sodium alginate/ECM/GelMA solution injected into tapered multibarrel capillary, while CaCl2 solution pumped along the same direction into collection capillary |
Addition of ECM filler reconstruct a microenvironment for cell growth. Addition of GelMA promotes construction of vessels for human umbilical vein endothelial cells |
[70] |
| GelMA | HUVECs, Human osteoblast-like cells (MG63) | Microfluidic system: double coaxial laminar flow microfluidic system with 3 capillary inlet. The system outlet is immersed in CaCl2 solution. 2% hyaluronic acid injected into 1st capillary while sodium alginate/GelMA was pumped into 2nd and 3rd capillary in order to prepare double-layer hollow composite Incorporation of human umbilical vascular endothelial cells (HUVACs) and human osteoblast-like cells (MG63) by mixing with sodium alginate/GelMA solution |
Addition of filler aimed to offer additional assembly network, strengthen mechanical and biological activity Composite fibre exhibited higher mechanical modulus, better stretching, and lower swelling compared to pure alginate fibre. |
[73] |
| Collagen | Pancreatic islets from sprague-dawley rat | Microfluidic system: polydimethylsiloxane (pdms) mould with integrated cylindrical and coaxial flow channels fabricated using soft lithography sodium alginate/filler with pancreatic islet injected at 1.2 ml/h into cylindrical channel, while cacl2 solution injected at 30 ml/h into coaxial channel |
Collagen added to mimic the native islet microenvironment. |
[71] |
| Gelatin or urinary bladder material (ubm) | Osteosarcoma cell (saos-2) | Microfluidic system: micromachined acetal resin serve as template during ‘hydrogel shrinking’ fabrication of microfluidic chip the chip comprises of two inlet channels integrated into one outlet output channel. the channel is either designed in straight fashion or designed with snake-like fashion to induce micromixing sodium alginate/gelatin or sodium alginate/ubm injected at 1.5 ml/min to one inlet channel, and sodium alginate/cells injected at 1.5 ml/min to another inlet channel, and the output fibre transferred into coagulation solution (either bacl2, cacl2, or srcl2) |
Gelatin or ubm promote extracellular matrix environment and positively influencing the viability and osteogenic mineralization. Composite fibre produced from microfluidic system with snake-like channel pattern promote homogenous distribution of embedded cells |
[69] |
| No filler | Mesenchymal stem cells (MSCs) | Microfluidic system: Main inlet channel comprised of 150 – 550 µm diameter glass channel inserted into 1.5 mm rectangular glass tube. Side channel of 1 mm diameter connected to the periphery of rectangular glass tube Sodium alginate/cells injected at varied flowrate (5 – 40 µl/min) to main inlet, while CaCl2 solution injected at 3.6 ml/min to side channel |
Composite fibre shows retention strength value of 0.54 N, which is within the range of the strength needed for tissue engineered tubular graft (0.5 – 0.7 N) Composite fibre with diameter 500 µm is used to encapsulate cell |
[74] |
| Methacrylated hyaluronic acid (MA-HA) or Methacrylated chondroitin sulfate (MA-CS) with chitosan as complexion agent | Human tendon derived cells (hTDCs) | Microfluidic system: Polydimethysiloxane chip designed with two inlet channel (1 mm diameter) joined to form one common outlet channel (1 mm diameter) Sodium alginate/MA-HA or sodium alginate/MA-CS injected at 0.2 ml/min to one inlet channel, while chitosan injected at 0.2 ml/min to another inlet channel. The fibre obtained at output channel crosslinked in 2% CaCl2 bath and methacrylate constituent within the fibre further cured with UV exposure (320 – 500 nm, 30 s) For cell-laden fibre, hTDC cells suspended at a density of 106/ml in either sodium alginate/MA-HA or sodium alginate/MA-CS solution |
Composite fibre did not affect cell viability and cells were also able to maintain their function of producing extracellular matrix up to 21 d in culture |
[72] |
| Chitosan | Liver HepG2 | Microfluidic system: Polydimethysiloxane chip with a tubular core (connected to 1st inlet channel) surrounded with 3 layer of sheath (inner-sheath layer connected to 2nd inlet channel, mid-sheath layer connected to 3rd inlet channel, and outer-sheath layer connected to 4th inlet channel) Methyl cellulose/cells solution injected into 1st inlet channel at varied flowrate (0.5 – 2.5 µl/min), chitosan solution injected into 2nd inlet channel at varied flowrate (0.1 – 0.8 µl/min), sodium alginate solution injected into 3rd inlet channel at varied flowrate (2.5 – 40 µl/min), and CaCl2 solution injected into 4th inlet channel designed with two inlet channel (1 mm diameter) joined to form one common outlet channel (1 mm diameter) |
The hollow region of fibre composite with chitosan inner coating is able to resist disintegration upon immersion in saline solution. Introduction of inner chitosan coating facilitated the cell adhesion and culture in the composite fibre |
[75] |
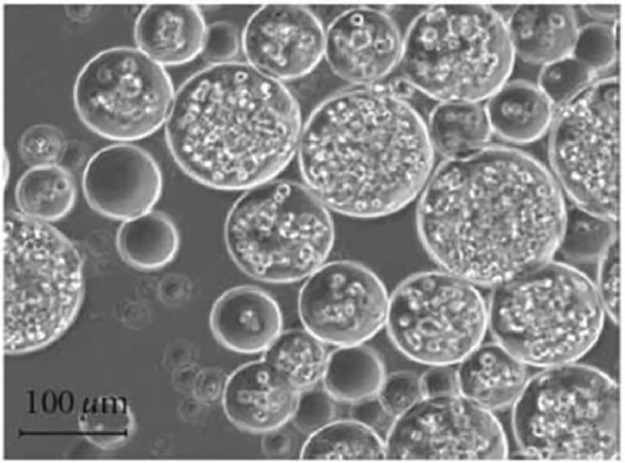
2.2. Bead form
Alginate bead can be produced through extrusion of alginate droplet into a crosslinking bath. This extrusion can be performed either using syringe or microfluidic system. In biomedical setting, the alginate bead mostly used as immobilisation medium for cells and drug. The bead can also be used as scaffold base for tissue repair. However, its structural integrity can be compromised if sufficient amount of sodium ion presents in bodily fluid diffuse into the bead construct, exchanging itself with Ca2+– a common ionotropic crosslinking agent used during bead formation. To alleviate this problem, Sarker et al. [76] used partially oxidized alginate which can react covalently with gelatin through Schiff's base formation due to the reaction of free amino group of lysine or hydroxylysine amino acid residues of gelatin and available aldehyde group of oxidized alginate. Mechanical properties of oxidised alginate/gelatin bead can be then tailored by changing the composition, by which higher amount of oxidized moieties lead to stiffer construct [77]. This composite bead also showed higher degradation rate compared to pure alginate bead because of lower molecular weight of oxidized alginate, which is desirable for tissue engineering. The rate of degradation of composite bead can be further regulated by tuning their composition, degree of oxidation, and degree of crosslinking.
Incorporation of inorganic material like nano-hydroxylapatite (nHAP) and bioglass to alginate for production of alginate composite bead can stimulate osteoblast cells which in turn create the nanocomposite structure of bone by secreting collagen fibril on which new apatite crystals subsequently form [78]. Apart from cells and inorganic material, incorporation with drug and other materials such as chitosan [79], strontium-substituted HA [80], and PVA [81] have been realized for production alginate composite bead.
2.3. Hydrogel form
Alginate-based hydrogel for biomedical purpose can be either non-injectable or injectable. Non-injectable alginate hydrogel is pre-formed prior its in vivo implantation. On the other hand, injectable hydrogel has wider gelation working windows before its final shape is assumed. This enables defect with irregular shape and size to be filled with minimally invasive procedure [82]. Both kind of hydrogel often incorporated with foreign material whether in particle or fibrous form to produce alginate composite hydrogel with improved overall structural integrity and desirable properties.
Cell clustering commonly observed when pure alginate is used as scaffold material. This is to be expected since alginate by itself does not support cell adhesion due to the lack of cell adhesion moieties. Therefore, alginate composite hydrogel incorporated with ECM such as gelatin or bioactive agent such as bioglass and cell adhesive peptides with the RGD sequence (Arg-Gly-Asp) is produced to stimulate cell adhesion and mimic native cell microenvironment to enhance cell growth and proliferation [83,84]. Natural ECM is bestowed with fibre-reinforced composite design, consisting of compliant aqueous matrix reinforced with fibrous collagenous protein. Using this biomimetic concept, the use of fibrous collagen with different arrangement within alginate hydrogel can lead to mechanically robust composite that can be tailored for specific tissue engineering applications [85]. When aligned electrospun gelatin nanofiber used to reinforce alginate hydrogel, up to 541% increase in tensile modulus and 1690% increase in tensile strength over non-composite hydrogel observed, while retaining good transparency at the thickness similar to human cornea [86].
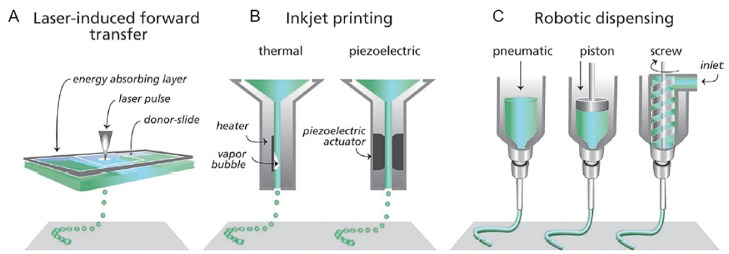
2.4. 3-D printed material
Bottom-up fabrication with bioprinting allows precise deposition of cells and biomaterial components from pre-defined computer generated design. Alginate found its use as bioink formulation as a result of its biocompatibility. Rastogi et al. [87] recently reviewed the use of alginate-based bioink for tissue engineering. Current bioprinting technologies are based on either extrusion, droplet bioprinting (also known as inkjet bioprinting), or laser mechanism (Fig. 3) [88]. For extrusion bioprinting, continuous bioink filament is extruded from printer nozzle using pneumatic or mechanical driven dispensing system. Although the use of nozzle inadvertently generates shear stress to the cell in cell-laden bioink which can lead to low cell viability, it remains the most common bioprinting method as it produces mechanically robust structure compared to inkjet and laser technology. In inkjet bioprinting, picoliter-sized droplets (∼50 µm droplet size) are generated using typical printhead from desktop inkjet printer allowing higher resolution construct to be printed. However, the viscosity of bioink must be very low to avoid nozzle clogging. In contrast to nozzle dependant technology, laser bioprinting typically operate based on laser induced forward transfer principle, whereby the laser beam evaporates the focal area of the absorbing layer, generating vapour bubble that pushes the bioink forward [89]. Although highest cell viability is possible for laser-based technology due to shear stress elimination, the associated cost and lack of commercial 3D laser bioprinter slowed down its progress forward.
Fig. 3.
Different type of bioprinting technique. (A) laser-based bioprinter use laser focused on an absorbing substrate to generate pressures that forward transfer cell-containing materials onto a collector substrate. (B) droplet-based bioprinting use either thermal or acoustic mechanism to dispense bioink droplet akin to typical inkjet printer. (C) extrusion-based bioprinting utilize pneumatic of mechanical (piston or screw) to dispense continuous bioink filament. Adapted with permission from [88]. Copyright (2013), John Wiley and Sons.
For extrusion-based bioprinting, the bioink should be formulated at optimal viscosity, which is not too low where printed construct can collapse and not too high to the point the nozzle become clogged. Although cells thrive in soft hydrogel (lower alginate molecular weight), it can be too watery for it to maintain shape for biofabrication purpose. Therefore, other materials such as nanocellulose [90], carrageenan [91] and gelatin [92,93] are mixed with alginate to form sturdy printed alginate composite structure. For inkjet-based bioprinting, collagen [94] and fibrinogen [95] had been added to fabricate printed composite structure and nHAp [96] and with chitosan [97] had been mixed with alginate to be used as bioink for laser bioprinting technology.
3. Biomedical applications of alginate and alginate composites
The good biocompatibility and promising physicochemical properties especially on the capability to form gel and retain the moisture content of alginate have promoted various biomedical applications such as wound dressing, drug delivery and tissue engineering of alginates and alginate composites [98]. The following sections describe the trend and summary of biomedical applications of alginate and alginate composites. More emphasis are given to the alginate composites because of their enhanced properties for biomedical applications.
3.1. Wound dressing application
Dermal wounds, both acute and chronic, represent significant clinical challenges such as poor vascularisation, protease susceptibility and microbial invasion at wound site which affect the early wound closure [99]. Conventionally, cloth dressings comprising of a sterile pad and cloth gauze are used as wound dressing due to their low cost. However, they are prone to bacterial infection and easily stick to the wound, causing suboptimal wound healing process. Thus, the ability of materials, especially natural polymers such as polysaccharides (e.g., chitosan, chitin, dextran, alginates, chondroitin and heparin), proteoglycans and proteins (e.g., collagen, gelatin, fibrin, silk fibroin and keratin) have been proposed and studied to accelerate wound healing and to control the infection [32,[99], [100], [101]].
Alginate as one of those materials has been attractive due to its good biocompatibility and water content [102]. The water content keeps the moist environment which maintains the optimal pH and accelerates the healing process [103]. For instance, KaltostatⓇAlginate dressing has been a well-known commercial wound dressing based on calcium alginate or sodium alginate in a form of absorbent gel-fibre matrices with fluid contact. It can maintain a moist wound environment which facilitates hemostatic effect, atraumatic removal and aids in the control of minor bleeding [99,104]. However, having alginate hydrogel alone as wound dressing is insufficient for preventing bacterial infection and promoting bioactivities, especially in chronic wound healing. Therefore, recently alginate composite dressings have been increasingly developed. The additional components may be functioning for high cell viability, cell adhesion, antibacterial activity, enhanced blood clotting and hemostasis (ability to prevent and stop bleeding). Table 4 summarized some recent studies on alginate composite for wound dressing application.
Table 4.
Recent studies on the alginate composites for wound dressing application.
| Additional components to alginate composite | Functions | Performances | Ref. |
|---|---|---|---|
| Chitosan | Bactericidal activity | Better bactericidal activity against Gram (-) bacteria (E. coli) than Gram (+) bacteria (S. aureus). | [105] |
| hemolytic properties | Slightly hemolytic. | ||
| Blood clotting | Activate blood-clotting faster than the commercial Celox™ material. |
||
| Nano-silica or hydroxyapatite (nHAP) | Tuning the physicochemical properties of alginate reinforced fibres | Addition of nano-silica or HAP delayed degradation and swelling behaviour and increase mechanical performances of the dressing and bioactivity of the wound healing process with no toxicity effects. | [106] |
| Poly(γ-glutamic acid) | Tuning the physicochemical properties of alginate hydrogel | Addition of poly(γ-glutamic acid) improved the swelling property, hemostats and removal of exudates due to the high hydrophilicity of poly(γ-glutamic acid). | [107] |
| Gelatin | Tuning the physicochemical properties of alginate hydrogel | Prolonged sustained the drug release. | [108] |
| Vancomycin | Antimicrobial drug | Antimicrobial activity towards gram positive bacteria. | |
| Halloysite nanotubes | Encapsulate the vancomycin | Extended the release of vancomycin (44% released amount) as compared to silica microcapsule (70% released amount). | |
| Natural polyols (i.e., polypropylene glycol) | Tuning the physicochemical properties of alginate foam dressing sheets | Nontoxic foam with higher density, lower porosity, better water absorption, higher strength and faster foam degradation than alginate foam without natural polyols. | [109] |
| Silver nanoparticles (Ag NPs) and asiaticoside (AS) | Antimicrobial agents | Combination of Ag NPs and AS showed better antibacterial activity toward P. aeruginosa, S. aureus, E. coli and B. subtilis. | |
| Ageratum conyzoides extract (ACE) | Tuning the physicochemical properties of alginate hydrogel film | Addition of ACE improved the tensile strength, swelling rate and thermal stability of alginate film. | [110] |
| Oxygen-releasing microspheres (ORM) containing hydrogen peroxide (H2O2) incorporated into poly(lactic-co-glycolic acid) | Forming a sustained release of oxygen to cells and tissues | Caused effective tissue regeneration wound healing by inducing neovascularization and promoting cell proliferation. | [111] |
| Manuka honey | Tuning the physicochemical properties of alginate hydrogel film | Addition of Manuka honey decreased the swelling rate and gel fraction but increased the Young Modulus and tensile strength. | [112] |
| Rana chensinensis skin peptides (RCSPs) extracted from discarded Rana chensinensis skin | Promote cell proliferation | Addition of RCSPs promoted collagen deposition, enhanced epidermal regeneration and faster hemostasis thus effectively promote wound healing. | [113] |
| Collagen @ polyacrylamide (PAM-Col) | Mix with oxidized sodium alginate as a new cross linker (COA) to form composite hydrogel | PAM-Col-COA composite hydrogel showed good mechanical properties, skin tissue adhesion, water absorption and sustained biological activity. | [114] |
| Chitosan | Forming stable shell (microcapsule) for drug delivery (Chinese nutgall) | Biocompatible and long-term durability for maintaining a long-term drug release. Ease of storage (−20 °C for more than 60 h). Also contribute to the antimicrobial activity | [115] |
| Chinese nutgall | Antimicrobial drug | Inhibition rate of 98.99% against S. aureus after 12 h and 100% after 12 h, 99.61% against E. coli after 6 h and 100% after 12 h. High antibacterial efficacy with S. aureus inhibition zones of 7.67 mm and E. coli inhibition zones of 5.27 mm | |
| Activated charcoal | As adsorbent | Adsorbed toxins, malodour molecules and tissue degradation products | [116] |
| Zinc ions (Zn2+) | Antimicrobial agent | Inhibit the E. coli growth after 1 hour of contact-time only |
In the composites, the alginate is mainly made into hydrogels by cross-linking mechanism using counter ions such as calcium or other multivalent ions (e.g., calcium and sodium ions) [117]. Although there are several reported making the alginate into fibre mat by electrospinning process [118], sponge [119], and foam sheet [109], the alginate dressings subsequently became hydrogel form when in-contact with water and the moist exudate. In an alginate composite, other materials such as poly(vinyl alcohol) [120,121], cellulose [122], chitosan [105,115,119,[123], [124], [125], [126], [127]], and gelatin [108] are also added during the formation of the hydrogel. The presence of poly(vinyl alcohol) affected the physicochemical properties of the hydrogel dressing such as its swelling ratio, tensile strength and elongation [121]. In many cases, the higher content of sodium alginate decreases the gel fraction, maximum strength and break elongation, but increases swelling ability, protein adsorption, hydrolytic degradation and thermal stability [120,121]. On the other hand, the presence of 10% alginate had effectively formed hydrogels with 90% cellulose nanofibrils [122]. The alginate had further increased the swelling of the composite by increasing the amount of charged groups inside the hydrogel and made the internal structure resembled a double network hydrogel with high toughness [122].
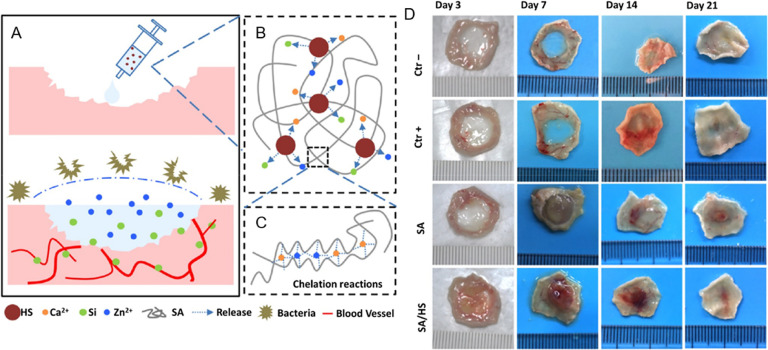
On the other hand, an inhibition of bacterial growth is another important criterion for the development of efficient wound dressing. In some studies, sodium alginate alone has been reported to have antimicrobial activity [120,124], but it is insufficient and less effective during wound healing process. Meanwhile, chitosan is widely used to promote antibacterial properties in biomedical field [128], [129], [130]. Usually sodium alginate is mixed with chitosan which has been reported to have antimicrobial activity [124,126,127]. Interestingly, research on this topic keeps increasing and more new materials have been investigated and added to the alginate composite dressing. For instance, a sodium alginate composite hydrogel had been integrated with bioactive hardystonite (HS) bioceramic and was found to inhibit bacterial growth and stimulate angiogenesis for enhanced wound healing as shown in Fig. 4 [102]. This alginate composite dressing also stimulated the proliferation and migration of both human dermal fibroblasts and human umbilical vein endothelial cells.
Fig. 4.
Design and principle of SA/HS composite hydrogel for wound healing. (A) Diagrammatic sketch of wound healing with hydrogel; (B) HS particles release ions into solution; (C) structure of SA/HS composite hydrogel. (D) Wound closure at Days 3, 7, 14, and 21 after treatment with the composite hydrogel dressing. Adapted with permission from [102]. Copyright (2017), American Chemical Society.
In some reported studies, metallic-based antimicrobial agent (e.g., silver [109,127,131] and zinc [116] nanoparticles), antibiotic drug (e.g., clindamycin [121], vancomycin [108], asiaticoside [109], aminoglycoside [132], etc.) or natural products with antimicrobial property (e.g., curcumin [119], Chinese nutgall [115], lentil seed extract [133],Aloe vera [127], essential oils such as melaleuca, copaiba and lemon oil [134], etc.) are also added into the alginate composite dressings in order to kill and inhibit the bacterial growth. A sustained drugs release has been one of the main targets for such alginate dressings. The high durability of the hydrogel could facilitate a sustained drug release. Recently, Xue et al. had reported that a long-term durable alginate-chitosan composite dressing created a prolonged antimicrobial system (i.e., a long-term release of Chinese nutgall antimicrobial drugs) for the wound dressing application. The sustained drug release system successfully inhibited the growth of both S. aureus and E. coli with a rate of 100% after 12 h) [115]. In another study, gelatin was added with alginate to form a biocompatible nontoxic hydrogel composite dressing which also prolonged and sustained release of antimicrobial drug (i.e., vancomycin encapsulated by halloysite nanotubes) [108]. However, the reduction of the drug release rate for alginate-gelatin hydrogel composite has worsen the antimicrobial effects of the dressing, thus a systematic study on the composition of alginate and gelatin could be performed to get an optimum performance (a sustained drug release with efficient antimicrobial activity).
The moist environment for wound healing does not only come from the water content of the alginate dressing but also from the exudate which contain several growth factors (e.g., platelet and vascular endothelial growth factors, transforming growth factors and a number of cytokines including interleukins) which regulate the granulation, epithelialization and angiogenesis in the healing process [103]. Recent study reported that sodium alginate composite hydrogel combined with bioglass (BG) and desferrioxamine (DFO) worked synergistically in promoting hypoxia inducible factor-1 (HIF-1α) and vascular endothelial growth factor (VEGF) expression and subsequently vascularization in the wound site, further facilitated diabetic skin wound healing [135]. In another reported study, the alginates were combined with human umbilical cord mesenchymal stem cells (hUCMSCs) where the alginates functioned as culture media. The wound dressing model of hUCMSCs-alginate mix had promoted faster wound healing because the hUCMSCs can proliferate well and express massive VEGF [136]. In addition, tissue regeneration for a fast wound healing requires optimum supply of oxygen. Therefore, recently, alginate composite dressing was also added with oxygen release microspheres (ORMs) which facilitate neovascularization and cell proliferation [111]. The ORMs contain hydrogen peroxide incorporated with poly(lactic-co-glycolic acid), prepared by double emulsion method [111].
On the other hand, a self-healing ability of a alginate composite hydrogel wound dressing containing dopamine-grafted oxidize sodium alginate and polyacrylamide chains was also reported [137]. Activated charcoal (AC) was also added in another alginate hydrogel as the AC could efficiently adsorb the malodor from the wound and the tissue degeneration products which are commonly associated with chronic wound with heavy exudate [116].
The presence of alginate- and alginate composite-based wound dressings in the market shows that some research have passed the clinical studies. Clinical studies are necessary and important before the wound dressings can be commercialized and used by patients. In the clinical studies, several aspects related to the performances and adverse effects of the wound dressings on the patients will be evaluated. Many clinical studies were reported on the alginate composite-based dressings with the integration of antimicrobial agent such as silver ions or silver nanoparticles [138], [139], [140], [141]. For example, the performance and efficacy of an ionic silver alginate/carboxymethylcellulose (SACMC) dressing had been clinically tested to thirty‐six patients with venous or pressure ulcers for over a four-week period [139]. The study found that the presence of silver showed better ability to prevent colonialization of microorganism (biofilm infected) to the wound, thus improved the healing process when compared to non-silver calcium alginate fibre (AF) dressing. The clinical study also reported one adverse effect (AE) of SACMC dressing which was wound maceration, lower than the five AEs from AF dressing (which were wound infection, serious sticking of the wound dressing, over‐granulation and rehospitalisation for additional wound care). In another study, an alginate silver wound dressing, commercially named as Askina Calgitrol AgⓇ was clinically tested to 65 patients to compare its performance with the 1% silversulfadiazine (AgSD) in the outpatient management of partial-thickness burn wounds [140]. The results showed that the Askina Calgitrol AgⓇ dressing had a lower average pain score, number of wound dressing change and nursing time and faster healing when compared to the AgSD.
3.2. Drug delivery
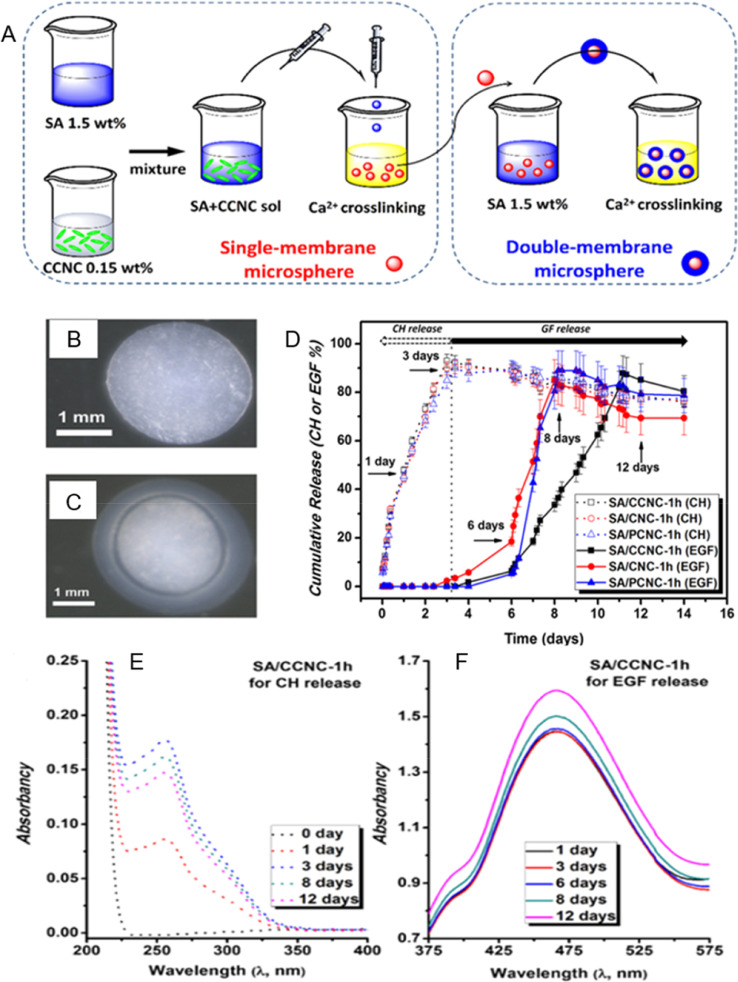
Ensuring the therapeutic molecules reaching the intended target organ or tissue for maximum effectiveness of the drug has been the main goal of drug delivery [142]. Various materials have been studied and tested for drug delivery. among all, alginate hydrogel has been attractive because the gentle gelation process of making them can be used for cell encapsulation and sustained drug release [98,143]. The drug delivery system of alginate is commonly associated with wound dressing applications. The alginate microcapsules were used for a sustained release of antimicrobial agents or drugs of the wound dressing [108,115]. Recently, a double membrane hydrogel composed of alginate and cellulose nanocrystals had shown a promising potential for a targeted released of antibiotic drugs via controlled swelling mechanisms [144]. As shown in Fig. 5, the outer hydrogel (composed of a neat alginate) was responsible for a rapid drug release, while the inner hydrogel (composed of cationic cellulose nanocrystals and anionic alginate, connected via electrostatic interactions) was responsible for a prolong drug release [144]. In addition, a dual-drug delivery system using alginate composite was also reported [145]. For examples, poly(d,l-lactide) (PDLLA) microspheres were embedded in alginate hydrogel beads [145] whereby the microspheres encapsulated glycyrrhetinic acid (GA, a hydrophobic drug) and the alginate hydrogel was loaded with bovine serum albumin (BSA) as a hydrophilic model protein drug [145,146].
Fig. 5.
(A) Preparation routine of single-membrane and double-membrane microsphere hydrogels; optical microscope images of (B) the SA/CCNC single-membrane microsphere hydrogel, (C) the SA/CCNC-1 h double-membrane microsphere hydrogel. Complexing drug release study involving ceftazidime hydrate (CH, the open symbols) and epidermal growth factor human (EGF, the solid symbols) of the double-membrane hydrogels in the pH 7.4 buffer solution (D) drug release profiles, (E) UV spectra of CH release for the SA/CCNC-1 h double-membrane hydrogel at the critical times, and (F) UV spectra of EGF release for the SA/CCNC-1 h double membrane hydrogel with the Bradford method at the critical times. Adapted with permission from [144]. Copyright (2016), American Chemical Society.
In another reported study, uniform alginate/CaCO3 composite microparticles (∼430 µm) synthesized using microfluidic technology had shown tunable compositions and pH-sensitive for sustainable release of drug (using a model drug of Trypan Blue) in wound healing application [147]. The alginate composite hydrogel can also be embedded with biologically active agents in their water-swollen network. For instance, an alginate sponge dressing which was further formed into hydrogel, incorporated with insulin-loaded poly(D,L-lactide-coglycolide) (PLGA) microparticles [148] has been reported to successfully stabilize and release insulin for up to 21 d, thus effective for a long-term delivery platform of bioactive insulin [148]. According to Omtvedt et al., -cyclodextrin can also be grafted to alginate hydrogel for a controlled-drug release system in drug delivery application [149]. The study reported that the -cyclodextrin was grafted to alginate in three-step synthesis using peroxiodate oxidation, reductive amination and copper(I)-catalysed azide-alkyne cycloaddition and the composite hydrogel were stable and able to form inclusion complex with the model drug (methyl orange) [149]. On the other hand, Leppiniemi et al. reported that the functionalization of the alginate composite (mixed with nanocellulose) was made using avidin for the immobilization of bioactive components through biotin−avidin interaction [150]. Interestingly, this alginate-nanocellulose composite is 3D-printable for the delivery of therapeutic agents.
In addition, the advancement of nanoscience and nanotechnology has enabled the fabrication and characterisation of alginate into smaller size, nanogels. As the alginate hydrogel is now in nano size, it offers several advantages owing to the high surface area of the nanogels. For example, the high surface area improved the performance of the alginate nanogel for drug delivery. For example, an alginate nanogel co-loaded with cisplatin and gold nanoparticles (AuNPs) has been reported for a combined photothermal therapy and chemotherapy [151]. The hydrodynamic diameter of alginate-cisplastin-AuNPs (ACA) nanogel complex measured by dynamic light scattering (DLS) analysis was in the range of 20–80 nm and it was reported that the combined action of chemo-photothermal therapy using the ACA nanocomplex dramatically suppressed tumour growth up to 95% as compared to control and the nanogel complex prolonged the survival rate of BALB/c mice bearing CT26 colon cancer. The ACA nanogel complex was also tested on U87-MG human glioblastoma cells [152]. In another study, a hybrid alginate nanogel with magnetic and dual responsive properties for a targeted nanotheranostic application was also developed [153]. The hybrid alginate nanogel consists of superparamagnetic iron oxide nanoparticles (SPIONs) which are covalently attached to a disulfide-modified alginate derivative and the nanogels are loaded with anticancer drug doxorubicin. Interestingly, the addition of other materials into the hybrid alginate nanogel also added more functionalities of the alginate drug delivery system such as magnetic-targeted characteristics and magnetic resonance imaging (MRI) functions other than improving the drug loading content, co-triggered release behaviour and high toxicity to tumour cells. In addition, the hybrid alginate nanogel was considerably biocompatible based on the low side effects to normal cells [153].
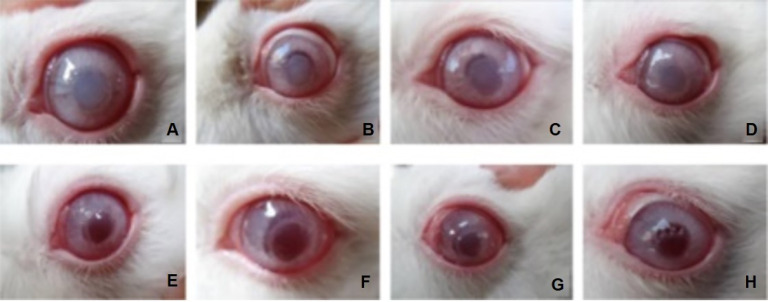
The clinical study of alginate- and alginate composite-based drug delivery system have been reported as well. However, as compared to wound dressing application the clinical study of the alginate- and alginate composite-based drug delivery system is still low and rare. Some existing reported studies are only at animal testing (preclinical test). For examples, alginate nanoparticles loaded with tuberculosis drugs, isoniazid (INH), rifampicin (RIF) and pyrazinamide (PZA), had been tested with Guinea pigs via inhalation administration [154]. The study was done to compare the inhalable alginate drug delivery system with the oral free drugs (the INH, RIF and PZA drugs were not encapsulated). The findings showed that the alginate-based drug nanocarrier had higher bioavailability when compared with the oral free drugs. The chemotherapeutic efficacy of three doses of the drugs using alginate-based drug nanocarrier nebulised 15 d apart was comparable with 45 daily doses of oral free drugs. Recently, in another study, alginate microsphere (about 95.7 µm in average diameter) had been tested with Chinchilla rabbits [155]. The alginate microspheres were loaded with retinoic acid (RA), a promising drug for the treatment of proliferative vitreoretinopathy. The study found that the alginate microspheres promoted a steady, long-term and effective level of RA. The alginate microspheres also had good biocompatibility as no inflammation and toxic responses were founds in the Hematoxylin and Eosin (HE) staining study [155].
Apart from drug delivery, alginate also can be used as a mediator in non-viral drug delivery when combined with other polycationic substrates such as chitosan. The cationic nature of chitosan allows it to interact with and easily form complexes with negatively charged DNA [156,157]. Nevertheless, the resulted chitosan-DNA interaction can be too strong, thereby preventing dissociation within the cell and ultimately hinder DNA translation, resulting in low transfection [158]. In order to reduce the strength of interaction between chitosan and DNA, Douglas and co-worker incorporated alginate as secondary polymer to chitosan nanoparticles [159]. It was found that alginate-chitosan composites were able to mediate transfection of 293T cells four times than that achieved by chitosan nanoparticles alone and after 48 h, the transfection efficiency yielded by the composites was as high as with positive control, Lipofectamine™, but with significantly reduced cytotoxicity.
3.3. Tissue engineering
Tissue engineering is an important tool in creating viable and functional tissue to restore, maintain, or improve defective tissues or organs [160]. In general, it involves propagation of cells that were either seeded onto or encapsulated in suitable material which support the growth and differentiation of the cells. The cell-material complex was then transplanted into the body to form tissue. Alginate has been extensively studied as a material to be used in tissue engineering applications [82]. It had been tested on bone [161,162], cartilage [163], liver [164,165], ocular tissues [166], and other body parts [167], [168], [169], [170] (Table 5). However, alginate is mechanically poor, possesses uncontrollable mechanical property due to variation in M and G contents and inferior material for cell attachment and proliferation for tissue engineering applications [26]. Thus, alginate is combined with other substances to produce alginate composites with improved features for tissue engineering applications. Both alginate and alginate composite applications in bone, cartilage, liver and other organ tissue engineering are discussed below.
Table 5.
Utilization of alginate for tissue engineering of various tissues/organs.
| Organ/cells | Function | Ref. |
|---|---|---|
| MC3T3-E1 osteoblast cells | Increase MC3T3-E1 osteoblast cells survivability in alginate beads | [161] |
| Femur in rabbits | Repair osteochondral defect in patella groove of the distal femur in rabbits (4.5 mm in diameter and 3 mm in depth) using ultrapurified alginate gel carrying stromal cell-derived factor-1 | [162] |
| Chondrocytes | Promotes both chondrocyte proliferation and maintenance of the chondrogenic phenotype in three dimensional alginate sulfate hydrogels | [163] |
| Liver | Proliferation of encapsulated HepG2/C3A liver cells for in vivo implantation | [164] |
| Liver | Generation of multilayered 3D structures of HepG2 liver cells using a bio-printed 3D alginate | [165] |
| Cornea | Propagating corneal epithelial cells for limbal epithelial therapeutic | [166] |
| Vascular | Propagation of human fat-derived stromal vascular fraction cells in 3D alginate spheroids. The 3D alginate spheroid was formed by direct-write three-dimensional printing system in which 1.5% (w/v) alginate solutions was mixed with human fat-derived stromal vascular fraction cells | [167] |
| Heart | Improved left ventricular function of rats suffered from myocardial infarct after injection of alginate hydrogel with a unique microstructure of uniform capillary-like channels | [168] |
| Testis | Improved seminiferous tubule integrity and spermatogonial recovery when grafted with alginate encapsulated immature testicular tissue | [169] |
| Vascular of adipose tissue | Promotes revascularization of mice adipose tissue when implanted with VEGF-calcium alginate microspheres loaded with adipocytes | [170] |
3.3.1. Bone
Bone is a complex and rigid organ that plays a major role in protection and movement of other organs, involves in production of blood and store minerals in human body [171]. Treatments for bone defects normally involve natural grafting from human donor (auto- and allograft) and from other species (xenograft) [16]. Synthetic grafting can also be used and numerous studies had been conducted to replace the natural grafting that has several limitations such as limited availability, risks associated with harvesting either from human or other species and requires additional surgeries that may cause infection to both the receivers and donors [29]. Alginate is one of the materials that was extensively studied for synthetic bone grafting [28]. It can act as scaffolding materials for bone construction and can be used to deliver cells for bone tissue regeneration [28,172].
Initial studies showed non-modified alginate supported long term growth for 8 months of chick embryo calvarial cells that were encapsulated in the alginate beads [173]. The encapsulated cells were found to be capable of elaboration and mineralization of ECM such as fibronectin, type III collagen and type I collagen. Later, it was demonstrated that alginate also supported the differentiation of murine embryonic stem cells (mESCs) to form bone cells [174]. However, alginate alone is incapable for load-bearing orthopaedic applications because it does not have mechanical strength [175]. Thus, many researches develop ‘stronger’ alginate composites for bone applications.
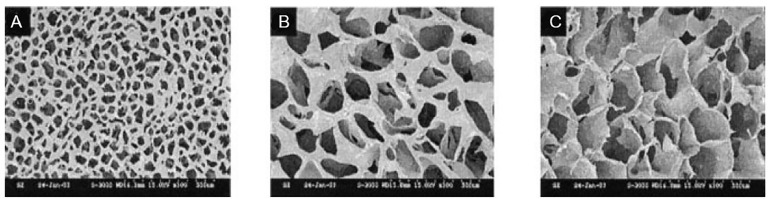
To make stiffer alginate composites, other materials such as ‘hard’ natural polymer, synthetic polymer and bioglass (combination of glass and ceramic) are mixed with the alginate. Alginate composite that contains ‘hard’ natural polymer such as chitosan in the presence of acetic acid demonstrated increase compressive property ranging from 0.79 to 1.41 MPa depending on the concentration of acetic acid [176]. It was observed in this study that the stiffer alginate/chitosan composite showed greater number of MG-63osteoblast-like cells grown on it. Adding synthetic polymer, poly(ethylene glycol) monomethacrylate (PEGmM) and poly(propyleneglycol) monomethacrylate (PPGmM) to methacrylic alginate at different mass fractions produce alginate composites of various charge density and hydrophobicity [177]. While blending alginate with bioglass in the presence of zinc and magnesium, gave alginate composite a greater compressive strength of 1.7 MPa [178]. In this alginate/bioglass/Zn/Mg composite, the presence of zinc and magnesium not only gave strength to the alginate, both of them also provide bacteria-free condition for bone formation. In all these studies above, natural and synthetic polymer, and bioglass which were added to the alginate not only gave strength, it also created a porous composite structure that mimics the bone (Fig. 6A).
Fig. 6.
Surface morphology of 50/50 alginate/HAP composite scaffolds (3% alginate, crosslinker: 0.03 M CaCl2, freezing temperature: −40 °C) at (A) bottom, (B) top, and (C) midsections of scaffolds. Magnification at 100 × . Adapted with permission from [180]. Copyright (2004), John Wiley and Sons.
Bone is a rigid structure due to the presence of HA that made 70% of the bone component [179]. Because of this, many studies develop alginate composites combine with HA. It was seen that adding HA to the alginate produced a composite with a well-interconnected porous structure with an average pore size of 150 µm and over 82% porosity [180] (Fig. 6). Seeded rat osteosarcoma UMR106 cells attach well onto this composite and propagate better than to the pure alginate scaffold. In more recent study, blending HA with alginate/chitosan composite although result in almost similar average pore size and porosity structure of alginate/HA composite, the HA-alginate/chitosan composite capacity for bone formation is improved in vivo [181]. It was observed that newly formed bone tissue filled the area of 3.0 mm (diameter) mouse calvarial bone defect implanted with HA-alginate/chitosan composite scaffold whereas none was observed when implanted with alginate/chitosan composite. In HA-alginate/chitosan composite scaffold, chitosan promotes cell attachment due to the presence of protonated amino groups on its backbone [182] and HA stimulates new bone cells formation on the composite graft. Based on this result, increasing studies is in trend nowadays to develop alginate composites by mixing alginate with more than one type of material that could provide strength and mimic the microenvironment of the bone to improve the scaffold capacity for bone formation.
In more recent study, Jo et al. [183] showed that grafting of alginate/HA composite that combine with silk fibroin (SF) in Sprague Dawley rats that possess central calvarial bone defects (diameter: 8.0 mm) result in higher new calvarial bone formation compared to that of alginate graft only at four weeks post implantation. This is due to the presence of HA and silk fibroin in the composite improved osteoinductivity and bone cell regeneration capacity, respectively. Regeneration of the bone tissue and rapid bone repair was observed as well when dopamine-modified alginate with chitosan/HA composite was implanted in femoral defect (4 mm in diameter and 5 mm deep) of New Zealand rabbits [184]. In this study, treating alginate with dopamine enhance composite to be stable and adhesive in the defected bone. Subcutaneous implantation of encapsulated rat bone marrow derived mesenchymal stem cells (MSC) in alginate dialdehyde/gelatin/nanoscaled bioactive glass (AD/G/nBG) microbeads into rats demonstrated higher cell survival compared to MSC encapsulated in microbeads without nBG, although the difference was not significant [185]. This indicates high compatibility of the multiple-material alginate composite microbeads in 3D environment compared to double-material alginate composite microbeads as multiple materials might better mimic the in vivo environment.
3.3.2. Cartilage
Cartilage is another rigid component in the body. It covers and protects bone ends from friction and made up the structure of ear, nose, bronchial tubes, intervertebral discs and other body components. Cartilage lacks of nerves and blood vessels thus it repairs damage slower than other tissues [186]. It did not heal spontaneously hence causes pain, inflammation and affected limb movement particularly for articular cartilage damage cases.
Grafting of engineered cartilage tissue to the cartilage defectives sites has shown encouraging results in stimulating cartilage growth [187,188]. This could lead to the restoration of the cartilage damage. Therefore, numerous studies were conducted to develop engineered cartilage tissue that involves cells and biodegradable scaffolds. Cells (chondrocytes) isolated from various parts of the body [189,190] and different types of stem cells were studied [191] and various materials to develop the scaffold were investigated [192]. One of the most studied materials to develop the scaffold is alginate. It has been shown in many studies that alginate supported the growth of chondrocytes and retained the typical chondrocytic appearance and properties [8,193]. However, it has also been demonstrated that initial cell loss was observed before alginate could support the chondrocyte growth [194]. Thus, alginate with reinforced hyaluronate was developed to increase the capacity of alginate for chondrocyte proliferation [195]. It was demonstrated that hyaluronate in this composite scaffold forms cross-linked structure with chondrocytes and interacts with CD44 on the cell surface of the chondrocytes hence increase the chondrocytes growth. Another alginate composite made by combining with jellyfish collagen was also shown to have better capacity in supporting human mesenchymal stem cells (hMSCs) chondrogenic differentiation and provide more stable constructs compared to pure alginate [196]. hMSCs chondrogenic differentiates better when seeded into to this polymer composite because jellyfish collagen in the composite is similar to human collagen type II which is the main tissue components of cartilage. During short-term pilot study in which 21 patients with lesion in the knee received alginate/fibrin matrix seeded with the allogenic cartilage cells, the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) and the Visual Analogue Scale (VAS) scores of the patients improved significantly and histology analysis showed significant repair tissues were present [197]. Twelve months follow-up of the patients showed 41.6% have complete filling or hypertrophy, 41.7% have bone-marrow edema and 25% have effusion [198].
For repairing articular cartilage damage, scaffold with high mechanical performance that can withstand the load-bearing stress is required. Pure alginate has limited mechanical strength and forming alginate composites by adding other material such as chitosan, natural inorganic polyphosphate, and nanocellulose increased alginate mechanical performance [199,200]. Furthermore, adding chitosan for example, upregulates the expression of genes encoding for collagen type II and aggregate of cartilage indicating increased chondrocyte growth [199]. While adding natural inorganic polyphosphate such as polyphosphate, gave flexibility for the composite scaffold to be moulded for replacement of damaged hard tibia bone regions [199]. Adding nanocellulose facilitates better gelation mechanism in hydrogels and enhances the dimensional stability [200].
Bioprinting is one of the methods used in tissue engineering that provides transplanted tissue with accurate architecture of affected site. Lately, alginate composites were used as bioinks for cartilage bioprinting applications [201,202]. Alginate alone gives weak printed constructs due to its rheological properties (low yield point). Mixing nanocellulose together with alginate retained stiffer printed alginate composite constructs that support chondrocytes proliferation and spreading as well as maintains chondrocyte properties [203]. Composite alginate bioink that contains collagen and polylactide also retain better 3D construct of bioprinting [204,205]. It was observed that when alginate/collagen was used as bioink, the resulting composite printed constructs not only possess enhanced cell adhesion, fasten cell proliferation and preserved chondrocyte phenotypes capacities, the composite constructs also has capabilities to suppressed dedifferentiation of chondrocytes [204].
3.3.3. Liver
Liver failure could cause approximately 2 million deaths per year worldwide [206,207]. The most effective therapy to treat terminal liver failure is liver transplant. However, problem arises to find liver donor to reduce graft rejection. Liver tissue engineering may be the best option to provide liver mass to replace the defective liver tissues [208]. Liver tissue engineering involves growing hepatocytes or stem cells that can be induced to differentiate to become hepatocyte on scaffold to create liver mass.
Extensive studies had been conducted and promising results showed encapsulated and seeded hepatocytes in and onto alginate remain viable and maintain their functional phenotype [209,210]. However, better results were demonstrated when alginate composites were used for hepatocyte growth. For example, alginate/galactosylated chitosan composite demonstrated higher cell attachment and viability than alginate alone [211]. This is owing to the presence of galactose in the composite that acts as specific signal for hepatocyte attachment and chitosan in the composite that mimic the ECM of the liver. Forming alginate composite by adding xyloglucan (XG) in which also act as synthetic ECM enhanced adhesion and proliferation of human hepatoma HepG2 cells with increasing concentration of XG [212]. Transplantation of liver-differentiated hMSCs seeded onto RGD-modified chitosan-alginate composite scaffold to defective rat liver (70% of the liver was removed) demonstrated that seeded cells remain at the transplantation site and function well with the remaining liver tissue [213]. The transdifferentiated hMSCs expressed hepatocyte function of glycogen storage although somewhat less and expressed the human hepatocyte markers such as AFP, CK19, CK18, albumin, HNF-3 and MRP-2.
Another approach to create liver mass for the liver transplant is formation of microcapsules. Microcapsules formation involves entrapment of cells within microbeads in which multiple microbeads were later enveloped by semipermeable membrane to produce microcapsules [214,215] (Fig. 7). Having the membrane surrounding microbead-containing cells provides the cells 3D microenvironment that recapitulates various aspects of the in vivo microenvironment in vitro [216]. The membrane also gave immuno-protection to the cells from the outside environment once the microcapsules transplanted inside the body and at the same time selectively allows diffusion of oxygen, nutrients and waste metabolites. Encapsulated HepG2 cells in alginate microbeads surrounded by chitosan membrane were shown to be viable, able to proliferate and secrete proteins for at least 12 d in the microcapsules [217]. Later, it was demonstrated that galactose/alginate composite microbeads have increased viability, proliferability and liver-specific functions of human hepatocyte, LO2 similar to the seeded hepatocytes onto galactosylated alginate scaffold although the former were wrapped with the chitosan membrane [218]. HepG2 cells were also observed to be viable and maintain hepatocyte function in sericin/alginate microbeads that were enveloped with chitosan shell [219]. Sericin is a protein that promotes proliferation as well as cell attachment. The cells were uniformly distributed within the sericin–alginate–chitosan microcapsules indicating that the microcapsules maintain favourable microenvironment for the cells.
Fig. 7.
Phase contrast image of poly(ethylene glycol)-microencapsulated mesenchymal stem cells for bone tissue engineering. Adapted with permission from [215]. Copyright (2012), Authors.
3.3.4. Other tissues and organs
Alginate and alginate composites had also been used for tissue engineering of other tissues and organs such as nerve, muscle, eye and heart. Earlier studies showed scientists used non-modified alginate or alginate only for nerve, muscle, eye and heart tissue engineering as scaffold and cell-encapsulated materials [19,26,82]. But later, many utilized alginate composites in their studies because the presence of various biological and synthetic materials in the composites allows formation of materials with desired properties that mimic the environment of these tissues and organs hence enable cells regeneration.
The following are the alginate composites that had been tested to be used as scaffold to regenerate the neural cells in vitro. It was demonstrated that alginate/HA composite supported the growth of mESCs and assisted differentiation of the cells towards neuronal lineages [220]. Electrically conductive polypyrrole/alginate (PPy/Alg) composites had also been shown to promote hMSCs cell adhesion, growth and differentiation to become neural cells when the cells were seeded onto the composite scaffold [221]. PPy is a conductive biomaterial that can be used to influence responses of various cells, including electrically excitable cells such as neurons. In more recent study, a novel microgel alginate composite, methacrylic anhydride modified-collagen/hyaluronic acid/alginate was observed to support the growth of induced pluripotent stem cells (iPSCs). The iPSCs capability to differentiate become neuron was enhanced when bioactive GRGDSP/Ln5-P4 was combined with the gel [222]. Other than using the alginate composites as scaffold for neural cell regeneration, it could also be utilized as nerve guidance scaffold for axonal regeneration. Freeze-dried alginate gel bar covered by polyglycolic acid mesh had been proven to guide axonal regeneration when cats with 50-mm gap sciatic nerve recovered motor and sensory nerves after 13 weeks of the implantation [223]. Alginate-polyornithine encapsulated porcine choroid plexus cells (NTCELLⓇ) have shown a suggestive signal of efficacy in neurodegenerative Parkinson's disease patients when NTCELLⓇ was implanted in the patients’ putamen during phase IIb clinical trial [224].
Successful muscle regeneration to repair and provide tissues for muscle defects depends on the specific tissue-like mechanical behaviours of the scaffold materials which could be appropriately provided by alginate composite compared to alginate. Alginate composite such as alginate/polyacrylamide and oxidised alginate/gelatin after refinement had been shown to have promising mechanical properties to be scaffold for muscle regeneration [225,226]. Recent study showed human skeletal muscle progenitor cells (hSMPCs) seeded onto skeletal muscle ECM treated-alginate/gelatin/heparin (Alg/G/H) scaffolds proliferated, differentiated, and matured [227]. It was also shown that the seeded hSMPCs cells onto the treated composite scaffold demonstrated better results than the seeded cells onto individual scaffold (i.e. gelatin, MatrigelⓇ, or ECM alone). This might be due to the combination of alginate with gelatin is a better matrix for cell adherence and it has proven that heparin provides growth factor retention and release in an extended manner for MPC proliferation and differentiation [228].
For ocular system, there is high interest in using alginate composites for tissue engineering to repair cornea. Attempts to repair cornea damage due to corneal endothelial disorders by growing in situ encapsulated corneal endothelial cells (CECs) in hydroxypropyl chitosan/oxidized alginate onto Descemet's membranes has been made [229]. After 60 d, rabbit corneas with transplanted encapsulated CECs resumed well and retained full transparency while rabbits that are not receiving polymer-cell complex became opaque, edema and thicken (Fig. 8). Repairing cornea damage due to alkali burn with transplantation of limbal stem cells (LSCs) encapsulated in carboxymethyl chitosan/oxidized alginate also produced successful results [230]. 28 d postburn, the rabbit corneal opacity completely recovered and was comparable to that in a normal cornea.
Fig. 8.
Typical eyeball images after operation. (A-D) Negative control group on the 15th, 30th, 45th and 60th day; (E-F) experimental group receiving encapsulated corneal endothelial cells (CECs) in hydroxypropyl chitosan/oxidized alginate on 15th, 30th, 45th and 60th day. Adapted with permission from [229]. Copyright (2011), Elsevier.
Utilization of alginate and its composites in treating heart problems had been intensively investigated and few are in the advance clinical trial [231,232]. However, injection of acellular alginate implant rather than alginate-embedded with stem cells implant into the heart wall showed clinical translation success. During clinical trials, injection of alginate based material, IK-5001 (Bellerophon Therapeutics, USA) and Algisyl (LoneStar Heart, Inc., USA) into left ventricle (LV) wall of acute and chronic heart failure patients prevent further remodelling of LV, increase ejection fraction and showed New York Heart Association functional class improvement [233,234]. Despite disadvantages of implantation of alginate-embedded-cells due to complex regulatory pathway, uncertainty of shelf availability and high costs, many recent studies were conducted to increase the efficacy of the cell/matrix-based technologies. One of the strategies is to improve the matrix used for entrapping the cells. Because alginate lack of appropriate motifs for adherent cells to attach, blending of natural ECM such as gelatin together with alginate enhances the cells to attach and proliferate [235]. gelatin is a denatured form of collagen type I that possess essential motifs required for cell proliferation and growth. It was observed that rat cardiomycetes encapsulated in alginate/gelatin showed increased cell viability after 7 d compared to when cardiomycetes were encapsulated by alginate alone [236]. The encapsulated cells in the blended polymer also able to retain stemness feature and cell multipotentiality compared to non-encapsulated cells. Other study showed different type of needle used to inject the encapsulated cells also play important role in maintaining the viability of the injected encapsulated cells. Curley et al. [237] found that encapsulated hMSCs metabolic activity reduced into half of control and had a significant decline in cell viability when helical needle was used.
4. Conclusion and future outlook
Gel forming capability and biocompatibility of alginate have made it become a go-to biomaterial in biomedical and pharmaceutical field. It provides moist healing environment during wound dressing, serve as scaffold during tissue regeneration, and function as carrier for drug or cell during targeted delivery process. Despite these advantages, native alginate gel suffers from the lack of mechanical integrity which can lead to distortion of scaffold structure or leakage of encapsulated substance. This requires incorporation of compatible reinforcing agent within alginate structure in order to improve alginate mechanical integrity especially in challenging psychological environment.
When the concern is solely about strength improvement, natural polymer (e.g. cellulose and chitin), synthetic polymer (e.g. polylactic acid and polycaprolactone), and carbon-based material (e.g. graphene and carbon nanotube) are generally used as reinforcing agent. Chitosan and metal nanoparticle, on the other hand, can provide respectable improvement in mechanical properties while simultaneously impart additional antibacterial properties. Inorganic material (e.g. nano-hydroxyapatite (nHAP) and bioglass) also provide additional strength reinforcement to alginate while being able to stimulate mineralized cell (e.g. osteoblast) growth and viability. However, if the concern of cell proliferation outweighs the need of mechanical stability, alginate can reservedly act as reinforcing agent instead. For example, during tissue regeneration, incorporation of ECM-like constituent (e.g. gelatin, collagen, and hyaluronic acid) is crucial so that suitable cell microenvironment can be provided. ECM itself lacked sufficient mechanical strength to be further manipulated, while alginate-based hydrogel, albeit being structurally stronger than ECM, does not possess receptor that can be recognized by cell for them to proliferate and differentiate. The symbiotic relationship of alginate as matrix to be reinforced or as reinforcing material itself, truly mark the versatility of this material. Adding to the fact that alginate composite can also be processed into various form (fibre, bead, hydrogel, and 3D-printed matrices) allows further fine-tuning the function-tailoring for specific biomedical applications.
Control of crosslinking agent densities and reinforcing material during alginate composite preparation allows different range of drug encapsulation medium with tuneable release kinetic to be developed. However, instantaneous external gelation of alginate upon contact with crosslinking agent during preparation process may limit it usage to pre-made tissue scaffold which requires surgeries for the scaffold to be embedded later in vivo. For this reason, research related to the formulation of injectable hydrogel, which relies on wider gelation working windows are gaining momentum nowadays. Typically, the use of low water solubility species relative to standard alginate crosslinking agent, CaCl2, allows more uniform distribution in alginate solution and provide longer gelation time. However, if the gelation occurs too late, the uncured injected gel might be flushed away and it can unnecessarily prolonged patient waiting time. Hence, control over gelation rate is crucial if injectable alginate based hydrogel is to be used in real clinical setting. If this can be achieved, not only alginate-based scaffold can be injected to harder-to-reach region, but also can effectively improve the efficacy of drug delivery targeting.
Research on bottom-up biofabrication using alginate-based bioink also trending recently. As natural microenvironment and tissue arrangement in vivo is typically complex, the ability to create intricate scaffold structure that simultaneously laden with living cells is biomimeticaly inspired. However, it should be noted that the use of alginate itself as scaffold can actually reduce cell-to-cell connection and residual scaffold polymer can disrupt normal cells organization, especially when cells need to be tightly interconnected such as in myocardial tissue. Although the strategies such as scaffold-free tissue construct had been reported recently, whereby alginate served as outer mould for tissue growth, it is limited to simple geometric construct which seems counterintuitive given the hallmark of bottom-up biofabrication is its ability to form complex construct. We believe that in order for tissue engineering to reach its fullest potential is by the preservation of complex and robust cell-only structure, mimicking the way Mother Natures intended.
As for now, alginate has successfully shows its credibility as wound dressing material, and continues to become material of choice for simple scaffold in tissue engineering and encapsulation medium for drug delivery. In the future, we envision more processing innovation towards intricate cell-laden alginate construct that can offer gentle and targeted alginate degradation without affecting embedded cells viability.
Conflict of interest
The authors declare that there is no conflict of interest. The authors alone are responsible for the content and writing of this article.
Acknowledgements
The authors acknowledge the financial support received from Ministry of Education Malaysia (FRGS/1/2018/TK05/UIAM/03/3). Writing on fibre preparation, chitin, and chitosan are directly related to the said grant.
References
- 1.Hasirci V., Hasirci N. Springer; New York: 2018. Fundamentals of biomaterials. [Google Scholar]
- 2.Ramakrishna S., Mayer J., Wintermantel E., Leong K.W. Biomedical applications of polymer-composite materials: a review. Compos Sci Technol. 2001;61(9):1189–1224. [Google Scholar]
- 3.Qizhi C., George T. CRC Press; 2018. Biomaterials: a basic introduction. [Google Scholar]
- 4.Wuisman P.I.J.M., Smit T.H. Bioresorbable polymers: heading for a new generation of spinal cages. Eur Spine J. 2006;15(2):133–148. doi: 10.1007/s00586-005-1003-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ozdil D., Wimpenny I., Aydin H.M., Yang Y. Biocompatibility of biodegradable medical polymers. In: Xiang Z., editor. Science and principles of biodegradable and bioresorbable medical polymers: materials and properties. Woodhead Publishing; USA: 2017. pp. 379–414. [Google Scholar]
- 6.Sheikh Z., Najeeb S., Khurshid Z., Verma V., Rashid H., Glogauer M. Biodegradable materials for bone repair and tissue engineering applications. Materials. 2015;8(9):5744–5794. doi: 10.3390/ma8095273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Varaprasad K., Jayaramudu T., Kanikireddy V., Toro C., Sadiku E.R. Alginate-based composite materials for wound dressing application: a mini review. Carbohydr Polym. 2020;236 doi: 10.1016/j.carbpol.2020.116025. [DOI] [PubMed] [Google Scholar]
- 8.Bouhadir K.H., Lee K.Y., Alsberg E., Damm K.L., Anderson K.W., Mooney D.J. Degradation of partially oxidized alginate and its potential application for tissue engineering. Biotechnol Prog. 2001;17(5):945–950. doi: 10.1021/bp010070p. [DOI] [PubMed] [Google Scholar]
- 9.Kong H.J., Kaigler D., Kim K., Mooney D.J. Controlling rigidity and degradation of alginate hydrogels via molecular weight distribution. Biomacromolecules. 2004;5(5):1720–1727. doi: 10.1021/bm049879r. [DOI] [PubMed] [Google Scholar]
- 10.Schipani R., Scheurer S., Florentin R., Critchley S.E., Kelly D.J. Reinforcing interpenetrating network hydrogels with 3D printed polymer networks to engineer cartilage mimetic composites. Biofabrication. 2020;12(3) doi: 10.1088/1758-5090/ab8708. [DOI] [PubMed] [Google Scholar]
- 11.Gong X., Dang G., Guo J., Liu Y., Gong Y. A sodium alginate/feather keratin composite fiber with skin-core structure as the carrier for sustained drug release. Int J Biol Macromol. 2020;155:386–392. doi: 10.1016/j.ijbiomac.2020.03.224. [DOI] [PubMed] [Google Scholar]
- 12.Ji M., Chen H., Yan Y., Ding Z., Ren H., Zhong Y. Effects of tricalcium silicate/sodium alginate/calcium sulfate hemihydrate composite cements on osteogenic performances in vitro and in vivo. J Biomater Appl. 2020;34(10):1422–1436. doi: 10.1177/0885328220907784. [DOI] [PubMed] [Google Scholar]
- 13.Choe G., Oh S., Seok J.M., Park S.A., Lee J.Y. Graphene oxide/alginate composites as novel bioinks for three-dimensional mesenchymal stem cell printing and bone regeneration applications. Nanoscale. 2019;11(48):23275–23285. doi: 10.1039/c9nr07643c. [DOI] [PubMed] [Google Scholar]
- 14.Zhang Y., Jiang G., Yu W., Liu D., Xu B. Microneedles fabricated from alginate and maltose for transdermal delivery of insulin on diabetic rats. Mater Sci Eng C Mater Biol Appl. 2018;85:18–26. doi: 10.1016/j.msec.2017.12.006. [DOI] [PubMed] [Google Scholar]
- 15.Liu Q.Q., Li Q.T., Xu S., Zheng Q.J., Cao X.D. Preparation and properties of 3D printed alginate(-)Chitosan polyion complex hydrogels for tissue engineering. Polymers. 2018;10(6):664. doi: 10.3390/polym10060664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Venkatesan J., Nithya R., Sudha P.N., Kim S.K. Role of alginate in bone tissue engineering. In: Kim S.K., editor. Advances in food and nutrition research. Academic Press; 2014. pp. 45–57. [DOI] [PubMed] [Google Scholar]
- 17.Hay I.D., Ur Rehman Z., Moradali M.F., Wang Y., Rehm B.H. Microbial alginate production, modification and its applications. Microb Biotechnol. 2013;6(6):637–650. doi: 10.1111/1751-7915.12076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Tipton P.A. Synthesis of alginate in bacteria. In: Liu H.W., Mander L., editors. Comprehensive natural products ii. Elsevier; Oxford: 2010. pp. 423–441. [Google Scholar]
- 19.Szekalska M., Puciłowska A., Szymańska E., Ciosek P., Winnicka K. Alginate: current use and future perspectives in pharmaceutical and biomedical applications. Int J Polym Sci. 2016;2016:1–17. [Google Scholar]
- 20.Niekraszewicz B., Niekraszewicz A. The structure of alginate, chitin and chitosan fibres. In: Eichhorn S.J., editor. Handbook of textile fibre structure. Woodhead Publishing; 2009. pp. 266–304. [Google Scholar]
- 21.Pawar S.N., Edgar K.J. Alginate derivatization: a review of chemistry, properties and applications. Biomaterials. 2012;33(11):3279–3305. doi: 10.1016/j.biomaterials.2012.01.007. [DOI] [PubMed] [Google Scholar]
- 22.Hallett J.P., Welton T. Room-temperature ionic liquids: solvents for synthesis and catalysis. 2. Chem Rev. 2011;111(5):3508–3576. doi: 10.1021/cr1003248. [DOI] [PubMed] [Google Scholar]
- 23.Younes M., Aggett P., Aguilar F., Crebelli R., Filipič M., Frutos M.J. Re‐evaluation of alginic acid and its sodium, potassium, ammonium and calcium salts (E 400–E 404) as food additives. EFSA J. 2017;15 doi: 10.2903/j.efsa.2017.5049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Yang J.S., Xie Y.J., He W. Research progress on chemical modification of alginate: a review. Carbohydr Polym. 2011;84(1):33–39. [Google Scholar]
- 25.Fu S., Thacker A., Sperger D.M., Boni R.L., Buckner I.S., Velankar S. Relevance of rheological properties of sodium alginate in solution to calcium alginate gel properties. AAPS PharmSciTech. 2011;12(2):453–460. doi: 10.1208/s12249-011-9587-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Goh C.H., Heng P.W.S., Chan L.W. Alginates as a useful natural polymer for microencapsulation and therapeutic applications. Carbohydr Polym. 2012;88(1):1–12. [Google Scholar]
- 27.Otterlei M., Østgaard K., Skjåk-Bræk G., Smidsrød O., Soon-Shiong P., Espevik T. Induction of cytokine production from human monocytes stimulated with alginate. J Immunother. 1991;10(4):286–291. doi: 10.1097/00002371-199108000-00007. [DOI] [PubMed] [Google Scholar]
- 28.Lee K.Y., Mooney D.J. Alginate: properties and biomedical applications. Prog Polym Sci. 2012;37(1):106–126. doi: 10.1016/j.progpolymsci.2011.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Venkatesan J., Bhatnagar I., Manivasagan P., Kang K.H., Kim S.K. Alginate composites for bone tissue engineering: a review. Int J Biol Macromol. 2015;72:269–281. doi: 10.1016/j.ijbiomac.2014.07.008. [DOI] [PubMed] [Google Scholar]
- 30.Sa V., Kornev K.G. A method for wet spinning of alginate fibers with a high concentration of single-walled carbon nanotubes. Carbon. 2011;49(6):1859–1868. [Google Scholar]
- 31.Neibert K., Gopishetty V., Grigoryev A., Tokarev I., Al-Hajaj N., Vorstenbosch J. Wound-healing with mechanically robust and biodegradable hydrogel fibers loaded with silver nanoparticles. Adv Healthc Mater. 2012;1(5):621–630. doi: 10.1002/adhm.201200075. [DOI] [PubMed] [Google Scholar]
- 32.Aderibigbe B.A., Buyana B. Alginate in wound dressings. Pharmaceutics. 2018;10(2):42. doi: 10.3390/pharmaceutics10020042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Cole S.M., Nelson. Alginate wound dressing of good integrity. USA, 5197945[P]. 1993-3-30.
- 34.Qin Y. Alginate fibres: an overview of the production processes and applications in wound management. Polym Int. 2008;57(2):171–180. [Google Scholar]
- 35.Ureña-Benavides E.E., Brown P.J., Kitchens C.L. Effect of jet stretch and particle load on cellulose nanocrystal-alginate nanocomposite fibers. Langmuir. 2010;26(17):14263–14270. doi: 10.1021/la102216v. [DOI] [PubMed] [Google Scholar]
- 36.Bunsell A.R. In: 2nd ed. Bunsell A.R., editor. Woodhead Publishing; 2018. [Google Scholar]
- 37.Shamshina J.L., Gurau G., Block L.E., Hansen L.K., Dingee C., Walters A. Chitin-calcium alginate composite fibers for wound care dressings spun from ionic liquid solution. J Mater Chem B. 2014;2(25):3924–3936. doi: 10.1039/c4tb00329b. [DOI] [PubMed] [Google Scholar]
- 38.Watthanaphanit A., Supaphol P., Tamura H., Tokura S., Rujiravanit R. Fabrication, structure, and properties of chitin whisker-reinforced alginate nanocomposite fibers. J Appl Polym Sci. 2008;110(2):890–899. [Google Scholar]
- 39.Fan L., Du Y., Zhang B., Yang J., Zhou J., Kennedy J.F. Preparation and properties of alginate/carboxymethyl chitosan blend fibers. Carbohydr Polym. 2006;65(4):447–452. [Google Scholar]
- 40.Dumont M., Villet R., Guirand M., Montembault A., Delair T., Lack S. Processing and antibacterial properties of chitosan-coated alginate fibers. Carbohydr Polym. 2018;190:31–42. doi: 10.1016/j.carbpol.2017.11.088. [DOI] [PubMed] [Google Scholar]
- 41.Watthanaphanit A., Supaphol P., Tamura H., Tokura S., Rujiravanit R. Wet-spun alginate/chitosan whiskers nanocomposite fibers: preparation, characterization and release characteristic of the whiskers. Carbohydr Polym. 2010;79(3):738–746. [Google Scholar]
- 42.Liu J., Zhang R., Ci M., Sui S., Zhu P. Sodium alginate/cellulose nanocrystal fibers with enhanced mechanical strength prepared by wet spinning. J Eng Fibers Fabr. 2019;14 [Google Scholar]
- 43.Popa E.G., Gomes M.E., Reis R.L. Cell delivery systems using alginate-carrageenan hydrogel beads and fibers for regenerative medicine applications. Biomacromolecules. 2011;12(11):3952–3961. doi: 10.1021/bm200965x. [DOI] [PubMed] [Google Scholar]
- 44.Wang Q.Q., Liu Y., Zhang C.J., Zhang C., Zhu P. Alginate/gelatin blended hydrogel fibers cross-linked by Ca2+ and oxidized starch: preparation and properties. Mater Sci Eng, C. 2019;99:1469–1476. doi: 10.1016/j.msec.2019.02.091. [DOI] [PubMed] [Google Scholar]
- 45.Wang Q., Hu X., Du Y., Kennedy J.F. Alginate/starch blend fibers and their properties for drug controlled release. Carbohydr Polym. 2010;82(3):842–847. [Google Scholar]
- 46.Foroughi J., Spinks G.M., Wallace G.G. A reactive wet spinning approach to polypyrrole fibres. J Mater Chem. 2011;21(17):6421–6426. [Google Scholar]
- 47.He Y., Zhang N., Gong Q., Qiu H., Wang W., Liu Y. Alginate/graphene oxide fibers with enhanced mechanical strength prepared by wet spinning. Carbohydr Polym. 2012;88(3):1100–1108. [Google Scholar]
- 48.Liu L., Jiang L., Xu G.K., Ma C., Yang X.G., Yao J.M. Potential of alginate fibers incorporated with drug-loaded nanocapsules as drug delivery systems. J Mater Chem B. 2014;2(43):7596–7604. doi: 10.1039/c4tb01392a. [DOI] [PubMed] [Google Scholar]
- 49.Greiner A., Wendorff J.H. Electrospinning: a fascinating method for the preparation of ultrathin fibers. Angew Chem Int Ed. 2007;46(30):5670–5703. doi: 10.1002/anie.200604646. [DOI] [PubMed] [Google Scholar]
- 50.Lee K.Y., Jeong L., Kang Y.O., Lee S.J., Park W.H. Electrospinning of polysaccharides for regenerative medicine. Adv Drug Del Rev. 2009;61(12):1020–1032. doi: 10.1016/j.addr.2009.07.006. [DOI] [PubMed] [Google Scholar]
- 51.Taemeh M.A., Shiravandi A., Korayem M.A., Daemi H. Fabrication challenges and trends in biomedical applications of alginate electrospun nanofibers. Carbohydr Polym. 2020;228 doi: 10.1016/j.carbpol.2019.115419. [DOI] [PubMed] [Google Scholar]
- 52.Rafiq M., Hussain T., Abid S., Nazir A., Masood R. Development of sodium alginate/PVA antibacterial nanofibers by the incorporation of essential oils. Mater Res Express. 2018;5(3) [Google Scholar]
- 53.Shalumon K.T., Anulekha K.H., Nair S.V., Nair S.V., Chennazhi K.P., Jayakumar R. Sodium alginate/poly(vinyl alcohol)/nano ZnO composite nanofibers for antibacterial wound dressings. Int J Biol Macromol. 2011;49(3):247–254. doi: 10.1016/j.ijbiomac.2011.04.005. [DOI] [PubMed] [Google Scholar]
- 54.Nista S.V.G., Bettini J., Mei L.H.I. Coaxial nanofibers of chitosan-alginate-PEO polycomplex obtained by electrospinning. Carbohydr Polym. 2015;127:222–228. doi: 10.1016/j.carbpol.2015.03.063. [DOI] [PubMed] [Google Scholar]
- 55.Li W., Li X., Chen Y., Li X., Deng H., Wang T. Poly(vinyl alcohol)/sodium alginate/layered silicate based nanofibrous mats for bacterial inhibition. Carbohydr Polym. 2013;92(2):2232–2238. doi: 10.1016/j.carbpol.2012.12.004. [DOI] [PubMed] [Google Scholar]
- 56.Wongkanya R., Chuysinuan P., Pengsuk C., Techasakul S., Lirdprapamongkol K., Svasti J. Electrospinning of alginate/soy protein isolated nanofibers and their release characteristics for biomedical applications. J Sci Adv Mater Dev. 2017;2(3):309–316. [Google Scholar]
- 57.Tort S., Acartürk F. Preparation and characterization of electrospun nanofibers containing glutamine. Carbohydr Polym. 2016;152:802–814. doi: 10.1016/j.carbpol.2016.07.028. [DOI] [PubMed] [Google Scholar]
- 58.Arthanari S., Mani G., Jang J.H., Choi J.O., Cho Y.H., Lee J.H. Preparation and characterization of gatifloxacin-loaded alginate/poly (vinyl alcohol) electrospun nanofibers. Artif Cells Nanomed Biotechnol. 2014;44(3):847–852. doi: 10.3109/21691401.2014.986676. [DOI] [PubMed] [Google Scholar]
- 59.Xiao Q., Lim L.T. Pullulan-alginate fibers produced using free surface electrospinning. Int J Biol Macromol. 2018;112:809–817. doi: 10.1016/j.ijbiomac.2018.02.005. [DOI] [PubMed] [Google Scholar]
- 60.Kyzioł A., Michna J., Moreno I., Gamez E., Irusta S. Preparation and characterization of electrospun alginate nanofibers loaded with ciprofloxacin hydrochloride. Eur Polym J. 2017;96:350–360. [Google Scholar]
- 61.Ni P., Bi H., Zhao G., Han Y., Wickramaratne M.N., Dai H. Electrospun preparation and biological properties in vitro of polyvinyl alcohol/sodium alginate/nano-hydroxyapatite composite fiber membrane. Colloids Surf B Biointerfaces. 2019;173:171–177. doi: 10.1016/j.colsurfb.2018.09.074. [DOI] [PubMed] [Google Scholar]
- 62.Kim M.S., Kim G. Three-dimensional electrospun polycaprolactone (PCL)/alginate hybrid composite scaffolds. Carbohydr Polym. 2014;114:213–221. doi: 10.1016/j.carbpol.2014.08.008. [DOI] [PubMed] [Google Scholar]
- 63.Majidi S.S., Slemming-Adamsen P., Hanif M., Zhang Z., Wang Z., Chen M. Wet electrospun alginate/gelatin hydrogel nanofibers for 3D cell culture. Int J Biol Macromol. 2018;118:1648–1654. doi: 10.1016/j.ijbiomac.2018.07.005. [DOI] [PubMed] [Google Scholar]
- 64.Mokhena T.C., Luyt A.S. Electrospun alginate nanofibres impregnated with silver nanoparticles: preparation, morphology and antibacterial properties. Carbohydr Polym. 2017;165:304–312. doi: 10.1016/j.carbpol.2017.02.068. [DOI] [PubMed] [Google Scholar]
- 65.De Silva R.T., Mantilaka M.M., Goh K.L., Ratnayake S.P., Amaratunga G.A.J., De Silva K.M.N. Magnesium oxide nanoparticles reinforced electrospun alginate-based nanofibrous scaffolds with improved physical properties. Int J Biomater. 2017;2017:1–9. doi: 10.1155/2017/1391298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Yamada M., Seki M. Multiphase microfluidic processes to produce alginate-based microparticles and fibers. J Chem Eng Jpn. 2018;51(4):318–330. [Google Scholar]
- 67.Shin S.J., Park J.Y., Lee J.Y., Park H., Park Y.D., Lee K.B. "On the fly" continuous generation of alginate fibers using a microfluidic device. Langmuir. 2007;23(17):9104–9108. doi: 10.1021/la700818q. [DOI] [PubMed] [Google Scholar]
- 68.Lee K.H., Shin S.J., Park Y., Lee S.H. Synthesis of cell-laden alginate hollow fibers using microfluidic chips and microvascularized tissue-engineering applications. Small. 2009;5(11):1264–1268. doi: 10.1002/smll.200801667. [DOI] [PubMed] [Google Scholar]
- 69.Angelozzi M., Miotto M., Penolazzi L., Mazzitelli S., Keane T., Badylak S.F. Composite ECM-alginate microfibers produced by microfluidics as scaffolds with biomineralization potential. Mater Sci Eng C. 2015;56:141–153. doi: 10.1016/j.msec.2015.06.004. [DOI] [PubMed] [Google Scholar]
- 70.Cheng Y., Yu Y., Fu F., Wang J., Shang L., Gu Z. Controlled fabrication of bioactive microfibers for creating tissue constructs using microfluidic techniques. ACS Appl Mater Interfaces. 2016;8(2):1080–1086. doi: 10.1021/acsami.5b11445. [DOI] [PubMed] [Google Scholar]
- 71.Jun Y., Kim M.J., Hwang Y.H., Jeon E.A., Kang A.R., Lee S.H. Microfluidics-generated pancreatic islet microfibers for enhanced immunoprotection. Biomaterials. 2013;34(33):8122–8130. doi: 10.1016/j.biomaterials.2013.07.079. [DOI] [PubMed] [Google Scholar]
- 72.Costa-Almeida R., Gasperini L., Borges J., Babo P.S., Rodrigues M.T., Mano J.F. Microengineered multicomponent hydrogel fibers: combining polyelectrolyte complexation and microfluidics. ACS Biomater Sci Eng. 2017;3(7):1322–1331. doi: 10.1021/acsbiomaterials.6b00331. [DOI] [PubMed] [Google Scholar]
- 73.Zuo Y., He X., Yang Y., Wei D., Sun J., Zhong M. Microfluidic-based generation of functional microfibers for biomimetic complex tissue construction. Acta Biomater. 2016;38:153–162. doi: 10.1016/j.actbio.2016.04.036. [DOI] [PubMed] [Google Scholar]
- 74.Liu M., Zhou Z., Chai Y., Zhang S., Wu X., Huang S. Synthesis of cell composite alginate microfibers by microfluidics with the application potential of small diameter vascular grafts. Biofabrication. 2017;9(2) doi: 10.1088/1758-5090/aa71da. [DOI] [PubMed] [Google Scholar]
- 75.Liu H., Wang Y., Yu Y., Chen W., Jiang L., Qin J. Simple fabrication of inner chitosan-coated alginate hollow microfiber with higher stability. J Biomed Mater Res Part B Appl Biomater. 2019;107(8):2527–2536. doi: 10.1002/jbm.b.34343. [DOI] [PubMed] [Google Scholar]
- 76.Sarker B., Papageorgiou D.G., Silva R., Zehnder T., Gul-E-Noor F., Bertmer M. Fabrication of alginate-gelatin crosslinked hydrogel microcapsules and evaluation of the microstructure and physico-chemical properties. J Mater Chem B. 2014;2(11):1470–1482. doi: 10.1039/c3tb21509a. [DOI] [PubMed] [Google Scholar]
- 77.Sarker B., Zehnder T., Rath S.N., Horch R.E., Kneser U., Detsch R. Oxidized alginate-gelatin hydrogel: a favorable matrix for growth and osteogenic differentiation of adipose-derived stem cells in 3D. ACS Biomater Sci Eng. 2017;3(8):1730–1737. doi: 10.1021/acsbiomaterials.7b00188. [DOI] [PubMed] [Google Scholar]
- 78.Boonrungsiman S., Gentleman E., Carzaniga R., Evans N.D., McComb D.W., Porter A.E. The role of intracellular calcium phosphate in osteoblast-mediated bone apatite formation. Proc Natl Acad Sci USA. 2012;109(35):14170–14175. doi: 10.1073/pnas.1208916109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Sharma C., Dinda A.K., Potdar P.D., Chou C.F., Mishra N.C. Fabrication and characterization of novel nano-biocomposite scaffold of chitosan-gelatin-alginate-hydroxyapatite for bone tissue engineering. Mater Sci Eng, C. 2016;64:416–427. doi: 10.1016/j.msec.2016.03.060. [DOI] [PubMed] [Google Scholar]
- 80.Li H., Jiang F., Ye S., Wu Y., Zhu K., Wang D. Bioactive apatite incorporated alginate microspheres with sustained drug-delivery for bone regeneration application. Mater Sci Eng, C. 2016;62:779–786. doi: 10.1016/j.msec.2016.02.012. [DOI] [PubMed] [Google Scholar]
- 81.Badruddoza A.Z.M., Godfrin P.D., Myerson A.S., Trout B.L., Doyle P.S. Core–shell composite hydrogels for controlled nanocrystal formation and release of hydrophobic active pharmaceutical ingredients. Adv Healthc Mater. 2016;5(15):1960–1968. doi: 10.1002/adhm.201600266. [DOI] [PubMed] [Google Scholar]
- 82.Bidarra S.J., Barrias C.C., Granja P.L. Injectable alginate hydrogels for cell delivery in tissue engineering. Acta Biomater. 2014;10(4):1646–1662. doi: 10.1016/j.actbio.2013.12.006. [DOI] [PubMed] [Google Scholar]
- 83.Rowley J.A., Madlambayan G., Mooney D.J. Alginate hydrogels as synthetic extracellular matrix materials. Biomaterials. 1999;20(1):45–53. doi: 10.1016/s0142-9612(98)00107-0. [DOI] [PubMed] [Google Scholar]
- 84.Shachar M., Tsur-Gang O., Dvir T., Leor J., Cohen S. The effect of immobilized RGD peptide in alginate scaffolds on cardiac tissue engineering. Acta Biomater. 2011;7(1):152–162. doi: 10.1016/j.actbio.2010.07.034. [DOI] [PubMed] [Google Scholar]
- 85.Tonsomboon K., Butcher A.L., Oyen M.L. Strong and tough nanofibrous hydrogel composites based on biomimetic principles. Mater Sci Eng C. 2017;72:220–227. doi: 10.1016/j.msec.2016.11.025. [DOI] [PubMed] [Google Scholar]
- 86.Tonsomboon K., Oyen M.L. Composite electrospun gelatin fiber-alginate gel scaffolds for mechanically robust tissue engineered cornea. J Mech Behav Biomed Mater. 2013;21:185–194. doi: 10.1016/j.jmbbm.2013.03.001. [DOI] [PubMed] [Google Scholar]
- 87.Rastogi P., Kandasubramanian B. Review of alginate-based hydrogel bioprinting for application in tissue engineering. Biofabrication. 2019;11(4) doi: 10.1088/1758-5090/ab331e. [DOI] [PubMed] [Google Scholar]
- 88.Malda J., Visser J., Melchels F.P., Jüngst T., Hennink W.E., Dhert W.J.A. 25th anniversary article: engineering hydrogels for biofabrication. Adv Mater. 2013;25(36):5011–5028. doi: 10.1002/adma.201302042. [DOI] [PubMed] [Google Scholar]
- 89.Antoshin A.A., Churbanov S.N., Minaev N.V., Zhang D., Zhang Y., Shpichka A.I. LIFT-bioprinting, is it worth it? Bioprinting. 2019;15 [Google Scholar]
- 90.Markstedt K., Mantas A., Tournier I., Martinez Avila H., Hagg D., Gatenholm P. 3D bioprinting human chondrocytes with nanocellulose-alginate bioink for cartilage tissue engineering aApplications. Biomacromolecules. 2015;16(5):1489–1496. doi: 10.1021/acs.biomac.5b00188. [DOI] [PubMed] [Google Scholar]
- 91.Kim M.H., Lee Y.W., Jung W.K., Oh J., Nam S.Y. Enhanced rheological behaviors of alginate hydrogels with carrageenan for extrusion-based bioprinting. J Mech Behav Biomed Mater. 2019;98:187–194. doi: 10.1016/j.jmbbm.2019.06.014. [DOI] [PubMed] [Google Scholar]
- 92.Jia W., Gungor-Ozkerim P.S., Zhang Y.S., Yue K., Zhu K., Liu W. Direct 3D bioprinting of perfusable vascular constructs using a blend bioink. Biomaterials. 2016;106:58–68. doi: 10.1016/j.biomaterials.2016.07.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Colosi C., Shin S.R., Manoharan V., Massa S., Costantini M., Barbetta A. Microfluidic bioprinting of heterogeneous 3D tissue constructs using low-viscosity bioink. Adv Mater. 2016;28(4):677–684. doi: 10.1002/adma.201503310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Xu T., Zhao W., Zhu J.M., Albanna M.Z., Yoo J.J., Atala A. Complex heterogeneous tissue constructs containing multiple cell types prepared by inkjet printing technology. Biomaterials. 2013;34(1):130–139. doi: 10.1016/j.biomaterials.2012.09.035. [DOI] [PubMed] [Google Scholar]
- 95.Hewes S., Wong A.D., Searson P.C. Bioprinting microvessels using an inkjet printer. Bioprinting. 2017;7:14–18. [Google Scholar]
- 96.Guillemot F., Souquet A., Catros S., Guillotin B., Lopez J., Faucon M. High-throughput laser printing of cells and biomaterials for tissue engineering. Acta Biomater. 2010;6(7):2494–2500. doi: 10.1016/j.actbio.2009.09.029. [DOI] [PubMed] [Google Scholar]
- 97.Kingsley D.M., Dias A.D., Corr D.T. Microcapsules and 3D customizable shelled microenvironments from laser direct-written microbeads. Biotechnol Bioeng. 2016;113(10):2264–2274. doi: 10.1002/bit.25987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Reakasame S., Boccaccini A.R. Oxidized alginate-based hydrogels for tissue engineering applications: a review. Biomacromolecules. 2018;19(1):3–21. doi: 10.1021/acs.biomac.7b01331. [DOI] [PubMed] [Google Scholar]
- 99.Parani M., Lokhande G., Singh A., Gaharwar A.K. Engineered nanomaterials for infection control and healing acute and chronic wounds. ACS Appl Mater Interfaces. 2016;8(16):10049–10069. doi: 10.1021/acsami.6b00291. [DOI] [PubMed] [Google Scholar]
- 100.Chen Z.G., Wang P.W., Wei B., Mo X.M., Cui F.Z. Electrospun collagen-chitosan nanofiber: a biomimetic extracellular matrix for endothelial cell and smooth muscle cell. Acta Biomater. 2010;6(2):372–382. doi: 10.1016/j.actbio.2009.07.024. [DOI] [PubMed] [Google Scholar]
- 101.Moura L.I., Dias A.M., Carvalho E., de Sousa H.C. Recent advances on the development of wound dressings for diabetic foot ulcer treatment-a review. Acta Biomater. 2013;9(7):7093–7114. doi: 10.1016/j.actbio.2013.03.033. [DOI] [PubMed] [Google Scholar]
- 102.Li Y., Han Y., Wang X., Peng J., Xu Y., Chang J. Multifunctional hydrogels prepared by dual ion cross-linking for chronic wound healing. ACS Appl Mater Interfaces. 2017;9(19):16054–16062. doi: 10.1021/acsami.7b04801. [DOI] [PubMed] [Google Scholar]
- 103.Orlowska J., Kurczewska U., Derwinska K., Orlowski W., Orszulak-Michalak D. In vitro evaluation of immunogenic properties of active dressings. Curr Issues Pharm Med Sci. 2014;27(1):55–60. [Google Scholar]
- 104.Sudheesh Kumar P.T., Raj N.M., Praveen G., Chennazhi K.P., Nair S.V., Jayakumar R. In vitro and in vivo evaluation of microporous chitosan hydrogel/nanofibrin composite bandage for skin tissue regeneration. Tissue Eng Part A. 2013;19(3–4):380–392. doi: 10.1089/ten.tea.2012.0376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Wiśniewska-Wrona M., Kucharska M., Struszczyk M.H., Cichecka M., Wilbik-Hałgas B., Szymonowicz M. Hemostatic, resorbable dressing of natural polymers-hemoguard. Autex Res J. 2016;16(1):29–34. [Google Scholar]
- 106.Zhang X., Huang C., Zhao Y., Jin X. Preparation and characterization of nanoparticle reinforced alginate fibers with high porosity for potential wound dressing application. RSC Adv. 2017;7(62):39349–39358. [Google Scholar]
- 107.Tong Z., Chen Y., Liu Y., Tong L., Chu J., Xiao K. Preparation, characterization and properties of alginate/poly(gamma-glutamic acid) composite microparticles. Mar Drugs. 2017;15(4):91. doi: 10.3390/md15040091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Kurczewska J., Pecyna P., Ratajczak M., Gajecka M., Schroeder G. Halloysite nanotubes as carriers of vancomycin in alginate-based wound dressing. Saudi Pharm J. 2017;25(6):911–920. doi: 10.1016/j.jsps.2017.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Namviriyachote N., Lipipun V., Akkhawattanangkul Y., Charoonrut P., Ritthidej G.C. Development of polyurethane foam dressing containing silver and asiaticoside for healing of dermal wound. Asian J Pharm Sci. 2019;14(1):63–77. doi: 10.1016/j.ajps.2018.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Abu Bakar A.J., Ghazali C.M.R., Mat Amin K.A. Sodium alginate/ageratum conyzoides extract film for wound dressing materials. IOP Conf Ser Mater Sci Eng. 2018;374 [Google Scholar]
- 111.Choi J., Hong G., Kwon T., Lim J. Fabrication of oxygen releasing scaffold by embedding H2O2-PLGA microspheres into alginate-based hydrogel sponge and its application for wound healing. Appl Sci. 2018;8(9):1492. [Google Scholar]
- 112.Azam N.A.N.M., Amin K.A.M. Influence of manuka honey on mechanical performance and swelling behaviour of alginate hydrogel film. IOP Conf Ser Mater Sci Eng. 2018;440 [Google Scholar]
- 113.Li R., Cheng Z., Wen R., Zhao X., Yu X., Sun L. Novel SA@Ca2+/RCSPs core–shell structure nanofibers by electrospinning for wound dressings. RSC Adv. 2018;8(28):15558–15566. doi: 10.1039/c8ra00784e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Bai Z., Dan W., Yu G., Wang Y., Chen Y., Huang Y. Tough and tissue-adhesive polyacrylamide/collagen hydrogel with dopamine-grafted oxidized sodium alginate as crosslinker for cutaneous wound healing. RSC Adv. 2018;8(73):42123–42132. doi: 10.1039/c8ra07697a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Xue W., Zhang M., Zhao F., Gao J., Wang L. Long-term durability antibacterial microcapsules with plant-derived Chinese nutgall and their applications in wound dressing. E-Polymers. 2019;19(1):268–276. [Google Scholar]
- 116.Osmokrovic A., Jancic I., Jankovic-Castvan I., Petrovic P., Milenkovic M., Obradovic B. Novel composite zinc-alginate hydrogels with activated charcoal aimed for potential applications in multifunctional primary wound dressings. Hemijska Ind. 2019;73(1):37–46. [Google Scholar]
- 117.Kuo C.K., Ma P.X. Ionically crosslinked alginate hydrogels as scaffolds for tissue engineering: part 1. Structure, gelation rate and mechanical properties. Biomaterials. 2001;22(6):511–521. doi: 10.1016/s0142-9612(00)00201-5. [DOI] [PubMed] [Google Scholar]
- 118.Grothe T., Grimmelsmann N., Homburg S.V., Ehrmann A. Possible applications of nano-spun fabrics and materials. Mater Today: Proc. 2017;4:S154–S159. [Google Scholar]
- 119.Dai M., Zheng X., Xu X., Kong X., Li X., Guo G. Chitosan-alginate sponge: preparation and application in curcumin delivery for dermal wound healing in rat. J Biomed Biotechnol. 2009;2009 doi: 10.1155/2009/595126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Kamoun E.A., Kenawy E.-R.S., Tamer T.M., El-Meligy M.A., Mohy Eldin M.S. Poly (vinyl alcohol)-alginate physically crosslinked hydrogel membranes for wound dressing applications: characterization and bio-evaluation. Arab J Chem. 2015;8(1):38–47. [Google Scholar]
- 121.Kim J.O., Choi J.Y., Park J.K., Kim J.H., Jin S.G., Chang S.W. Development of clindamycin-loaded wound dressing with polyvinyl alcohol and sodium alginate. Biol Pharm Bull. 2008;31(12):2277–2282. doi: 10.1248/bpb.31.2277. [DOI] [PubMed] [Google Scholar]
- 122.Benselfelt T., Wågberg L. Unidirectional swelling of dynamic cellulose nanofibril networks: a platform for tunable hydrogels and aerogels with 3D shapeability. Biomacromolecules. 2019;20(6):2406–2412. doi: 10.1021/acs.biomac.9b00401. [DOI] [PubMed] [Google Scholar]
- 123.Yan X., Khor E., Lim L.Y. PEC films prepared from chitosan-alginate coacervates. Chem Pharm Bull. 2000;48(7):941–946. doi: 10.1248/cpb.48.941. [DOI] [PubMed] [Google Scholar]
- 124.Venkatrajah B., Vanitha Malathy V., Elayarajah B., Mohan, Rajendran R., Rammohan R. Biopolymer and Bletilla Striata herbal extract coated cotton gauze preparation for wound healing. J Med Sci (Faisalabad) 2012;12(6):148–160. [Google Scholar]
- 125.Holak P., Adamiak Z., Babinska I., Jalynski M., Jastrzebski P., Grabarczyk L. The influence of haemostatic dressing prototypes for the emergency services on the histopathological parameters of porcine muscle. In Vivo. 2019;33(3):723–729. doi: 10.21873/invivo.11531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Straccia M.C., d'Ayala G.G., Romano I., Oliva A., Laurienzo P. Alginate hydrogels coated with chitosan for wound dressing. Mar Drugs. 2015;13(5):2890–2908. doi: 10.3390/md13052890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Gomez Chabala L.F., Cuartas C.E.E., Lopez M.E.L. Release behavior and antibacterial activity of chitosan/alginate blends with aloe vera and silver nanoparticles. Mar Drugs. 2017;15(10):328. doi: 10.3390/md15100328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Raafat D., Von Bargen K., Haas A., Sahl H.G. Insights into the mode of action of chitosan as an antibacterial compound. Appl Environ Microbiol. 2008;74(12):3764–3773. doi: 10.1128/AEM.00453-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Dash M., Chiellini F., Ottenbrite R.M., Chiellini E. Chitosan - a versatile semi-synthetic polymer in biomedical applications. Prog Polym Sci. 2011;36(8):981–1014. [Google Scholar]
- 130.Yu H., Xu X., Chen X., Hao J., Jing X. Medicated wound dressings based on poly(vinyl alcohol)/poly(N-vinyl pyrrolidone)/chitosan hydrogels. J Appl Polym Sci. 2006;101(4):2453–2463. [Google Scholar]
- 131.Cai J., Chen X., Wang X., Tan Y., Ye D., Jia Y. High-water-absorbing calcium alginate fibrous scaffold fabricated by microfluidic spinning for use in chronic wound dressings. RSC Adv. 2018;8(69):39463–39469. doi: 10.1039/c8ra06922k. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Kumar L., Brice J., Toberer L., Klein-Seetharaman J., Knauss D., Sarkar S.K. Antimicrobial biopolymer formation from sodium alginate and algae extract using aminoglycosides. PLoS One. 2019;14(3) doi: 10.1371/journal.pone.0214411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Vidyavathi M., Mobeen Farhana S.K., Sreedevi A., Suresh kumar R.V. Design and evaluation of lentil seed extract loaded bio scaffolds for wound healing activity. Biomed Pharmacol J. 2018;11(1):503–511. [Google Scholar]
- 134.Pires V., Moura M. Preparation of new nanocomposites containing nanoemulsions of melaleuca, copaiba, and lemon oil for application as biomaterial. Quim Nova. 2016 [Google Scholar]
- 135.Kong L., Wu Z., Zhao H., Cui H., Shen J., Chang J. Bioactive injectable hydrogels containing desferrioxamine and bioglass for diabetic wound healing. ACS Appl Mater Interfaces. 2018;10(36):30103–30114. doi: 10.1021/acsami.8b09191. [DOI] [PubMed] [Google Scholar]
- 136.Wang S., Yang H., Tang Z., Long G., Huang W. Wound dressing model of human umbilical cord mesenchymal stem cells-alginates complex promotes skin wound healing by paracrine signaling. Stem Cells Int. 2016;2016 doi: 10.1155/2016/3269267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Chen T., Chen Y., Rehman H.U., Chen Z., Yang Z., Wang M. Ultratough, self-healing, and tissue-adhesive hydrogel for wound dressing. ACS Appl Mater Interfaces. 2018;10(39):33523–33531. doi: 10.1021/acsami.8b10064. [DOI] [PubMed] [Google Scholar]
- 138.Percival S.L., Slone W., Linton S., Okel T., Corum L., Thomas J.G. The antimicrobial efficacy of a silver alginate dressing against a broad spectrum of clinically relevant wound isolates. Int Wound J. 2011;8(3):237–243. doi: 10.1111/j.1742-481X.2011.00774.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Beele H., Meuleneire F., Nahuys M., Percival S.L. A prospective randomised open label study to evaluate the potential of a new silver alginate/carboxymethylcellulose antimicrobial wound dressing to promote wound healing. Int Wound J. 2010;7(4):262–270. doi: 10.1111/j.1742-481X.2010.00669.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Opasanon S., Muangman P., Namviriyachote N. Clinical effectiveness of alginate silver dressing in outpatient management of partial-thickness burns. Int Wound J. 2010;7(6):467–471. doi: 10.1111/j.1742-481X.2010.00718.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Trial C., Darbas H., Lavigne J.P., Sotto A., Simoneau G., Tillet Y. Assessment of the antimicrobial effectiveness of a new silver alginate wound dressing: a RCT. J Wound Care. 2010;19(1):20–26. doi: 10.12968/jowc.2010.19.1.46095. [DOI] [PubMed] [Google Scholar]
- 142.Sharifi F., Sooriyarachchi A.C., Altural H., Montazami R., Rylander M.N., Hashemi N. Fiber based approaches as medicine delivery systems. ACS Biomater Sci Eng. 2016;2(9):1411–1431. doi: 10.1021/acsbiomaterials.6b00281. [DOI] [PubMed] [Google Scholar]
- 143.Lai W.F., Rogach A.L. Hydrogel-based materials for delivery of herbal medicines. ACS Appl Mater Interfaces. 2017;9(13):11309–11320. doi: 10.1021/acsami.6b16120. [DOI] [PubMed] [Google Scholar]
- 144.Lin N., Geze A., Wouessidjewe D., Huang J., Dufresne A. Biocompatible double-membrane hydrogels from cationic cellulose nanocrystals and anionic alginate as complexing drugscodelivery. ACS Appl Mater Interfaces. 2016;8(11):6880–6889. doi: 10.1021/acsami.6b00555. [DOI] [PubMed] [Google Scholar]
- 145.Zhong D., Liu Z., Xie S., Zhang W., Zhang Y., Xue W. Study on poly(D,L-lactic) microspheres embedded in calcium alginate hydrogel beads as dual drug delivery systems. J Appl Polym Sci. 2013;129(2):767–772. [Google Scholar]
- 146.Cidonio G., Glinka M., Dawson J.I., Oreffo R.O.C. The cell in the ink: improving biofabrication by printing stem cells for skeletal regenerative medicine. Biomaterials. 2019;209:10–24. doi: 10.1016/j.biomaterials.2019.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Shi M., Zhang H., Song T., Liu X., Gao Y., Zhou J. Sustainable dual release of antibiotic and growth factor from pH-responsive uniform alginate composite microparticles to enhance wound healing. ACS Appl Mater Interfaces. 2019;11(25):22730–22744. doi: 10.1021/acsami.9b04750. [DOI] [PubMed] [Google Scholar]
- 148.Hrynyk M., Martins-Green M., Barron A.E., Neufeld R.J. Alginate-PEG sponge architecture and role in the design of insulin release dressings. Biomacromolecules. 2012;13(5):1478–1485. doi: 10.1021/bm300186k. [DOI] [PubMed] [Google Scholar]
- 149.Omtvedt L.A., Dalheim M.O., Nielsen T.T., Larsen K.L., Strand B.L., Aachmann F.L. Efficient grafting of cyclodextrin to alginate and performance of the hydrogel for release of model drug. Sci Rep. 2019;9(1):9325. doi: 10.1038/s41598-019-45761-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Leppiniemi J., Lahtinen P., Paajanen A., Mahlberg R., Metsa-Kortelainen S., Pinomaa T. 3D-printable bioactivated nanocellulose-alginate hydrogels. ACS Appl Mater Interfaces. 2017;9(26):21959–21970. doi: 10.1021/acsami.7b02756. [DOI] [PubMed] [Google Scholar]
- 151.Mirrahimi M., Abed Z., Beik J., Shiri I., Shiralizadeh Dezfuli A., Mahabadi V.P. A thermo-responsive alginate nanogel platform co-loaded with gold nanoparticles and cisplatin for combined cancer chemo-photothermal therapy. Pharmacol Res. 2019;143:178–185. doi: 10.1016/j.phrs.2019.01.005. [DOI] [PubMed] [Google Scholar]
- 152.Neshastehriz A., Khateri M., Ghaznavi H., Shakeri-Zadeh A. Investigating the therapeutic effects of alginate nanogel co-loaded with gold nanoparticles and cisplatin on U87-MG human glioblastoma cells. Anticancer Agents Med Chem. 2018;18(6):882–890. doi: 10.2174/1871520618666180131112914. [DOI] [PubMed] [Google Scholar]
- 153.Peng N., Ding X., Wang Z., Cheng Y., Gong Z., Xu X. Novel dual responsive alginate-based magnetic nanogels for onco-theranostics. Carbohydr Polym. 2019;204:32–41. doi: 10.1016/j.carbpol.2018.09.084. [DOI] [PubMed] [Google Scholar]
- 154.Zahoor A., Sharma S., Khuller G.K. Inhalable alginate nanoparticles as antitubercular drug carriers against experimental tuberculosis. Int J Antimicrob Agents. 2005;26(4):298–303. doi: 10.1016/j.ijantimicag.2005.07.012. [DOI] [PubMed] [Google Scholar]
- 155.Wang F., He S., Chen B. Retinoic acid-loaded alginate microspheres as a slow release drug delivery carrier for intravitreal treatment. Biomed Pharmacother. 2018;97:722–728. doi: 10.1016/j.biopha.2017.10.109. [DOI] [PubMed] [Google Scholar]
- 156.Yu H., Chen X., Lu T., Sun J., Tian H., Hu J. Poly(L-lysine)-graft-chitosan copolymers: synthesis characterization, and gene transfection effect. Biomacromolecules. 2007;8(5):1425–1435. doi: 10.1021/bm060910u. [DOI] [PubMed] [Google Scholar]
- 157.Yu H., Deng C., Tian H., Lu T., Chen X., Jing X. Chemo-physical and biological evaluation of poly(L-lysine)-grafted chitosan copolymers used for highly efficient gene delivery. Macromol Biosci. 2011;11(3):352–361. doi: 10.1002/mabi.201000283. [DOI] [PubMed] [Google Scholar]
- 158.MacLaughlin F.C., Mumper R.J., Wang J., Tagliaferri J.M., Gill I., Hinchcliffe M. Chitosan and depolymerized chitosan oligomers as condensing carriers for in vivo plasmid delivery. J Control Rel. 1998;56(1–3):259–272. doi: 10.1016/s0168-3659(98)00097-2. [DOI] [PubMed] [Google Scholar]
- 159.Douglas K.L., Piccirillo C.A., Tabrizian M. Effects of alginate inclusion on the vector properties of chitosan-based nanoparticles. J Control Rel. 2006;115(3):354–361. doi: 10.1016/j.jconrel.2006.08.021. [DOI] [PubMed] [Google Scholar]
- 160.Langer R., Vacanti J. Advances in tissue engineering. J Pediatr Surg. 2016;51(1):8–12. doi: 10.1016/j.jpedsurg.2015.10.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Lee B.H., Li B., Guelcher S.A. Gel microstructure regulates proliferation and differentiation of MC3T3-E1 cells encapsulated in alginate beads. Acta Biomater. 2012;8(5):1693–1702. doi: 10.1016/j.actbio.2012.01.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Sukegawa A., Iwasaki N., Kasahara Y., Onodera T., Igarashi T., Minami A. Repair of rabbit osteochondral defects by an acellular technique with an ultrapurified alginate gel containing stromal cell-derived factor-1. Tissue Eng Part A. 2012;18(9–10):934–945. doi: 10.1089/ten.TEA.2011.0380. [DOI] [PubMed] [Google Scholar]
- 163.Mhanna R., Kashyap A., Palazzolo G., Vallmajo-Martin Q., Becher J., Moller S. Chondrocyte culture in three dimensional alginate sulfate hydrogels promotes proliferation while maintaining expression of chondrogenic markers. Tissue Eng Part A. 2014;20(9–10):1454–1464. doi: 10.1089/ten.tea.2013.0544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Capone S.H., Dufresne M., Rechel M., Fleury M.J., Salsac A.V., Paullier P. Impact of alginate composition: from bead mechanical properties to encapsulated HepG2/C3A cell activities for in vivo implantation. PLoS One. 2013;8(4):e62032. doi: 10.1371/journal.pone.0062032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Jeon H., Kang K., Park S.A., Kim W.D., Paik S.S., Lee S.H. Generation of multilayered 3D structures of HepG2 cells using a bio-printing technique. Gut Liver. 2017;11(1):121–128. doi: 10.5009/gnl16010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Wright B., Cave R.A., Cook J.P., Khutoryanskiy V.V., Mi S., Chen B. Enhanced viability of corneal epithelial cells for efficient transport/storage using a structurally modified calcium alginate hydrogel. Regen Med. 2012;7(3):295–307. doi: 10.2217/rme.12.7. [DOI] [PubMed] [Google Scholar]
- 167.Williams S.K., Touroo J.S., Church K.H., Hoying J.B. Encapsulation of adipose stromal vascular fraction cells in alginate hydrogel spheroids using a direct-write three-dimensional printing system. Biores Open Access. 2013;2(6):448–454. doi: 10.1089/biores.2013.0046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Rocca D.G., Willenberg B.J., Qi Y., Simmons C.S., Rubiano A., Ferreira L.F. An injectable capillary-like microstructured alginate hydrogel improves left ventricular function after myocardial infarction in rats. Int J Cardiol. 2016;220:149–154. doi: 10.1016/j.ijcard.2016.06.158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Poels J., Abou-Ghannam G., Decamps A., Leyman M., Rieux A., Wyns C. Transplantation of testicular tissue in alginate hydrogel loaded with VEGF nanoparticles improves spermatogonial recovery. J Control Rel. 2016;234:79–89. doi: 10.1016/j.jconrel.2016.05.037. [DOI] [PubMed] [Google Scholar]
- 170.Ding S.L., Zhang M.Y., Tang S.J., Yang H., Tan W.Q. Effect of calcium alginate microsphere loaded with vascular endothelial growth factor on adipose tissue transplantation. Ann Plast Surg. 2015;75(6):644–651. doi: 10.1097/SAP.0000000000000201. [DOI] [PubMed] [Google Scholar]
- 171.Burr D.B., Akkus O. Bone morphology and organization. In: Burr D.B., Allen M.R., editors. Basic and applied bone biology. Academic Press; San Diego: 2014. pp. 3–25. [Google Scholar]
- 172.Giri T.K., Thakur D., Alexander A., Ajazuddin, Badwaik H., Tripathi D.K. Alginate based hydrogel as a potential biopolymeric carrier for drug delivery and cell delivery systems: present status and applications. Curr Drug Del. 2012;9(6):539–555. doi: 10.2174/156720112803529800. [DOI] [PubMed] [Google Scholar]
- 173.Majmudar G., Bole D., Goldstein S.A., Bonadio J. Bone cell culture in a three-dimensional polymer bead stabilizes the differentiated phenotype and provides evidence that osteoblastic cells synthesize type III collagen and fibronectin. J Bone Miner Res. 1991;6(8):869–881. doi: 10.1002/jbmr.5650060813. [DOI] [PubMed] [Google Scholar]
- 174.Hwang Y.S., Cho J., Tay F., Heng J.Y., Ho R., Kazarian S.G. The use of murine embryonic stem cells, alginate encapsulation, and rotary microgravity bioreactor in bone tissue engineering. Biomaterials. 2009;30(4):499–507. doi: 10.1016/j.biomaterials.2008.07.028. [DOI] [PubMed] [Google Scholar]
- 175.Zhao L., Weir M.D., Xu H.H. An injectable calcium phosphate-alginate hydrogel-umbilical cord mesenchymal stem cell paste for bone tissue engineering. Biomaterials. 2010;31(25):6502–6510. doi: 10.1016/j.biomaterials.2010.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Florczyk S.J., Kim D.J., Wood D.L., Zhang M. Influence of processing parameters on pore structure of 3D porous chitosan-alginate polyelectrolyte complex scaffolds. J Biomed Mater Res A. 2011;98(4):614–620. doi: 10.1002/jbm.a.33153. [DOI] [PubMed] [Google Scholar]
- 177.Cha C., Kim E.S., Kim I.W., Kong H. Integrative design of a poly(ethylene glycol)-poly(propylene glycol)-alginate hydrogel to control three dimensional biomineralization. Biomaterials. 2011;32(11):2695–2703. doi: 10.1016/j.biomaterials.2010.12.038. [DOI] [PubMed] [Google Scholar]
- 178.Zamani D., Moztarzadeh F., Bizari D. Alginate-bioactive glass containing Zn and Mg composite scaffolds for bone tissue engineering. Int J Biol Macromol. 2019;137:1256–1267. doi: 10.1016/j.ijbiomac.2019.06.182. [DOI] [PubMed] [Google Scholar]
- 179.Fay D., Halsey J. World Technologies; USA: 2012. Anatomy of bones. [Google Scholar]
- 180.Lin H.R., Yeh Y.J. Porous alginate/hydroxyapatite composite scaffolds for bone tissue engineering: preparation, characterization, and in vitro studies. J Biomed Mater Res Part B Appl Biomater. 2004;71B(1):52–65. doi: 10.1002/jbm.b.30065. [DOI] [PubMed] [Google Scholar]
- 181.Jin H.H., Kim D.H., Kim T.W., Shin K.K., Jung J.S., Park H.C. In vivo evaluation of porous hydroxyapatite/chitosan-alginate composite scaffolds for bone tissue engineering. Int J Biol Macromol. 2012;51(5):1079–1085. doi: 10.1016/j.ijbiomac.2012.08.027. [DOI] [PubMed] [Google Scholar]
- 182.Croisier F., Jérôme C. Chitosan-based biomaterials for tissue engineering. Eur Polym J. 2013;49(4):780–792. [Google Scholar]
- 183.Jo Y.Y., Kim S.G., Kwon K.J., Kweon H., Chae W.S., Yang W.G. Silk fibroin-alginate-hydroxyapatite composite particles in bone tissue engineering applications in vivo. Int J Mol Sci. 2017;18(4):858. doi: 10.3390/ijms18040858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Shi D., Shen J., Zhang Z., Shi C., Chen M., Gu Y. Preparation and properties of dopamine-modified alginate/chitosan-hydroxyapatite scaffolds with gradient structure for bone tissue engineering. J Biomed Mater Res A. 2019;107(8):1615–1627. doi: 10.1002/jbm.a.36678. [DOI] [PubMed] [Google Scholar]
- 185.Rottensteiner-Brandl U., Detsch R., Sarker B., Lingens L., Kohn K., Kneser U. Encapsulation of rat bone marrow derived mesenchymal stem cells in alginate dialdehyde/gelatin microbeads with and without nanoscaled bioactive Glass for in vivo bone tissue engineering. Materials (Basel) 2018;11(10) doi: 10.3390/ma11101880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Jiang Y., Lin H., Tuan R.S. Overview: state of the art and future prospectives for cartilage repair. In: Grässel, S. and Aszódi, A., editors. Cartilage. Cham: Springer, Cham; 2017, p. 1–34.
- 187.Jahr H. Tissue engineering strategies for cartilage repair. In: Grässel, S. and Aszódi, A., editors. Cartilage. Cham: Springer, Cham; 2017, p. 169–87.
- 188.Vega S.L., Kwon M.Y., Burdick J.A. Recent advances in hydrogels for cartilage tissue engineering. Eur Cell Mater. 2017;33:59–75. doi: 10.22203/eCM.v033a05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.Pelttari K., Pippenger B., Mumme M., Feliciano S., Scotti C., Mainil-Varlet P. Adult human neural crest–derived cells for articular cartilage repair. Sci Transl Med. 2014;6(251):251ra119. doi: 10.1126/scitranslmed.3009688. [DOI] [PubMed] [Google Scholar]
- 190.Pleumeekers M.M., Nimeskern L., Koevoet W.L., Kops N., Poublon R.M., Stok K.S. The in vitro and in vivo capacity of culture-expanded human cells from several sources encapsulated in alginate to form cartilage. Eur Cell Mater. 2014;27:264–280. doi: 10.22203/ecm.v027a19. ; discussion 78-80. [DOI] [PubMed] [Google Scholar]
- 191.Studer D., Cavalli E., Formica F.A., Kuhn G.A., Salzmann G., Mumme M. Human chondroprogenitors in alginate–collagen hybrid scaffolds produce stable cartilage in vivo. J Tissue Eng Regen Med. 2017;11(11):3014–3026. doi: 10.1002/term.2203. [DOI] [PubMed] [Google Scholar]
- 192.Fu N., Dong T., Meng A., Meng Z., Zhu B., Lin Y. Research orogress of the types and preparation techniques of scaffold materials in cartilage tissue engineering. Curr Stem Cell Res Ther. 2018;13(7):583–590. doi: 10.2174/1574888X12666170718152611. [DOI] [PubMed] [Google Scholar]
- 193.Van Osch G.J.V.M., Van Der Veen S.W., Burger E.H., Verwoerd-Verhoef H.L. Chondrogenic potential of in vitro multiplied rabbit perichondrium cells cultured in alginate beads in defined medium. Tissue Eng. 2000;6(4):321–330. doi: 10.1089/107632700418047. [DOI] [PubMed] [Google Scholar]
- 194.van Susante J., Buma P., Osch G., Versleyen D., Kraan P., Berg W. Culture of chondrocytes in alginate and collagen carrier gels. Acta Orthop Scand. 1996;66:549–556. doi: 10.3109/17453679509002314. [DOI] [PubMed] [Google Scholar]
- 195.Park H., Lee K.Y. Facile control of RGD-alginate/hyaluronate hydrogel formation for cartilage regeneration. Carbohydr Polym. 2011;86(3):1107–1112. [Google Scholar]
- 196.Pustlauk W., Paul B., Gelinsky M., Bernhardt A. Jellyfish collagen and alginate: combined marine materials for superior chondrogenesis of hMSC. Mater Sci Eng C Mater Biol Appl. 2016;64:190–198. doi: 10.1016/j.msec.2016.03.081. [DOI] [PubMed] [Google Scholar]
- 197.Almqvist K.F., Dhollander A.A.M., Verdonk P.C.M., Forsyth R., Verdonk R., Verbruggen G. Treatment of cartilage defects in the knee using alginate beads containing human mature allogenic chondrocytes. Am J Sports Med. 2009;37(10):1920–1929. doi: 10.1177/0363546509335463. [DOI] [PubMed] [Google Scholar]
- 198.Dhollander A.A.M., Huysse W.C.J., Verdonk P.C.M., Verstraete K.L., Verdonk R., Verbruggen G. MRI evaluation of a new scaffold-based allogenic chondrocyte implantation for cartilage repair. Eur J Radiol. 2010;75(1):72–81. doi: 10.1016/j.ejrad.2009.03.056. [DOI] [PubMed] [Google Scholar]
- 199.Muller W.E., Neufurth M., Wang S., Tolba E., Schroder H.C., Wang X. Morphogenetically active scaffold for osteochondral repair (polyphosphate/alginate/N,O-carboxymethyl chitosan) Eur Cell Mater. 2016;31:174–190. doi: 10.22203/ecm.v031a12. [DOI] [PubMed] [Google Scholar]
- 200.Naseri N., Deepa B., Mathew A.P., Oksman K., Girandon L. Nanocellulose-based interpenetrating polymer network (IPN) hydrogels for cartilage applications. Biomacromolecules. 2016;17(11):3714–3723. doi: 10.1021/acs.biomac.6b01243. [DOI] [PubMed] [Google Scholar]
- 201.Axpe E., Oyen M.L. Applications of alginate-based bioinks in 3D bioprinting. Int J Mol Sci. 2016;17(12) doi: 10.3390/ijms17121976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202.Panwar A., Tan L.P. Current Status of Bioinks for micro-extrusion-based 3D bioprinting. Molecules. 2016;21(6) doi: 10.3390/molecules21060685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203.Muller M., Ozturk E., Arlov O., Gatenholm P., Zenobi-Wong M. Alginate sulfate-nanocellulose bioinks for cartilage bioprinting applications. Ann Biomed Eng. 2017;45(1):210–223. doi: 10.1007/s10439-016-1704-5. [DOI] [PubMed] [Google Scholar]
- 204.Yang X., Lu Z., Wu H., Li W., Zheng L., Zhao J. Collagen-alginate as bioink for three-dimensional (3D) cell printing based cartilage tissue engineering. Mater Sci Eng C Mater Biol Appl. 2018;83:195–201. doi: 10.1016/j.msec.2017.09.002. [DOI] [PubMed] [Google Scholar]
- 205.Kosik-Koziol A., Costantini M., Bolek T., Szoke K., Barbetta A., Brinchmann J. PLA short sub-micron fiber reinforcement of 3D bioprinted alginate constructs for cartilage regeneration. Biofabrication. 2017;9(4) doi: 10.1088/1758-5090/aa90d7. [DOI] [PubMed] [Google Scholar]
- 206.Marcellin P., Kutala B.K. Liver diseases: a major, neglected global public health problem requiring urgent actions and large-scale screening. Liver Int. 2018;38(Suppl 1):2–6. doi: 10.1111/liv.13682. [DOI] [PubMed] [Google Scholar]
- 207.Asrani S.K., Devarbhavi H., Eaton J., Kamath P.S. Burden of liver diseases in the world. J Hepatol. 2019;70(1):151–171. doi: 10.1016/j.jhep.2018.09.014. [DOI] [PubMed] [Google Scholar]
- 208.Mazza G., Al-Akkad W., Rombouts K., Pinzani M. Liver tissue engineering: from implantable tissue to whole organ engineering. Hepatol Commun. 2018;2(2):131–141. doi: 10.1002/hep4.1136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 209.Dvir-Ginzberg M., Gamlieli-Bonshtein I., Agbaria R., Cohen S. Liver tissue engineering within alginate scaffolds: effects of cell-seeding density on hepatocyte viability, morphology, and function. Tissue Eng. 2003;9(4):757–766. doi: 10.1089/107632703768247430. [DOI] [PubMed] [Google Scholar]
- 210.Lan S.F., Safiejko-Mroczka B., Starly B. Long-term cultivation of HepG2 liver cells encapsulated in alginate hydrogels: a study of cell viability, morphology and drug metabolism. Toxicol In Vitro. 2010;24(4):1314–1323. doi: 10.1016/j.tiv.2010.02.015. [DOI] [PubMed] [Google Scholar]
- 211.Seo S.J., Kim I.Y., Choi Y.J., Akaike T., Cho C.S. Enhanced liver functions of hepatocytes cocultured with NIH 3T3 in the alginate/galactosylated chitosan scaffold. Biomaterials. 2006;27(8):1487–1495. doi: 10.1016/j.biomaterials.2005.09.018. [DOI] [PubMed] [Google Scholar]
- 212.Deng X., Cao Y., Yan H., Yang J., Xiong G., Yao H. Enhanced liver functions of HepG2 cells in the alginate/xyloglucan scaffold. Biotechnol Lett. 2015;37(1):235–240. doi: 10.1007/s10529-014-1663-6. [DOI] [PubMed] [Google Scholar]
- 213.Tai B.C., Du C., Gao S., Wan A.C., Ying J.Y. The use of a polyelectrolyte fibrous scaffold to deliver differentiated hMSCs to the liver. Biomaterials. 2010;31(1):48–57. doi: 10.1016/j.biomaterials.2009.09.022. [DOI] [PubMed] [Google Scholar]
- 214.Majewski R.L., Zhang W., Ma X., Cui Z., Ren W., Markel D.C. Bioencapsulation technologies in tissue engineering. J Appl Biomater Funct Mater. 2016;14(4):e395–e403. doi: 10.5301/jabfm.5000299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 215.Mumaw J., Jordan E.T., Sonnet C., Olabisi R.M., Olmsted-Davis E.A., Davis A.R. Rapid heterotrophic ossification with cryopreserved poly(ethylene glycol-) microencapsulated BMP2-expressing MSCs. Int J Biomater. 2012;2012 doi: 10.1155/2012/861794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 216.Du J., Yarema K.J. Cell Microencapsulation for Tissue engineering and regenerative medicine. In: Karp J.M., Zhao W., editors. Micro- and nanoengineering of the cell surface. William Andrew Publishing; Oxford: 2014. pp. 215–239. [Google Scholar]
- 217.Haque T., Chen H., Ouyang W., Martoni C., Lawuyi B., Urbanska A.M. In vitro study of alginate–chitosan microcapsules: an alternative to liver cell transplants for the treatment of liver failure. Biotechnol Lett. 2005;27(5):317–322. doi: 10.1007/s10529-005-0687-3. [DOI] [PubMed] [Google Scholar]
- 218.Tian M., Han B., Tan H., You C. Preparation and characterization of galactosylated alginate-chitosan oligomer microcapsule for hepatocytes microencapsulation. Carbohydr Polym. 2014;112:502–511. doi: 10.1016/j.carbpol.2014.06.025. [DOI] [PubMed] [Google Scholar]
- 219.Nayak S., Dey S., Kundu S.C. Silk sericin-alginate-chitosan microcapsules: hepatocytes encapsulation for enhanced cellular functions. Int J Biol Macromol. 2014;65:258–266. doi: 10.1016/j.ijbiomac.2014.01.042. [DOI] [PubMed] [Google Scholar]
- 220.Bozza A., Coates E.E., Incitti T., Ferlin K.M., Messina A., Menna E. Neural differentiation of pluripotent cells in 3D alginate-based cultures. Biomaterials. 2014;35(16):4636–4645. doi: 10.1016/j.biomaterials.2014.02.039. [DOI] [PubMed] [Google Scholar]
- 221.Yang S., Jang L., Kim S., Yang J., Yang K., Cho S.W. Polypyrrole/alginate hybrid hydrogels: electrically conductive and soft biomaterials for human mesenchymal stem cell culture and potential neural tissue engineering applications. Macromol Biosci. 2016;16(11):1653–1661. doi: 10.1002/mabi.201600148. [DOI] [PubMed] [Google Scholar]
- 222.Kuo Y.C., Hsueh C.H. Neuronal production from induced pluripotent stem cells in self-assembled collagen-hyaluronic acid-alginate microgel scaffolds with grafted GRGDSP/Ln5-P4. Mater Sci Eng C Mater Biol Appl. 2017;76:760–774. doi: 10.1016/j.msec.2017.03.133. [DOI] [PubMed] [Google Scholar]
- 223.Suzuki Y., Tanihara M., Ohnishi K., Suzuki K., Endo K., Nishimura Y. Cat peripheral nerve regeneration across 50mm gap repaired with a novel nerve guide composed of freeze-dried alginate gel. Neurosci Lett. 1999;259(2):75–78. doi: 10.1016/s0304-3940(98)00924-0. [DOI] [PubMed] [Google Scholar]
- 224.Snow B., Mulroy E., Bok A., Simpson M., Smith A., Taylor K. A phase IIb, randomised, double-blind, placebo-controlled, dose-ranging investigation of the safety and efficacy of NTCELLⓇ [immunoprotected (alginate-encapsulated) porcine choroid plexus cells for xenotransplantation] in patients with Parkinson's disease. Parkinsonism Relat Disord. 2019;61:88–93. doi: 10.1016/j.parkreldis.2018.11.015. [DOI] [PubMed] [Google Scholar]
- 225.Fitzgerald M.M., Bootsma K., Berberich J.A., Sparks J.L. Tunable stress relaxation behavior of an alginate-polyacrylamide hydrogel: comparison with muscle tissue. Biomacromolecules. 2015;16(5):1497–1505. doi: 10.1021/bm501845j. [DOI] [PubMed] [Google Scholar]
- 226.Baniasadi H., Mashayekhan S., Fadaoddini S., Haghirsharifzamini Y. Design, fabrication and characterization of oxidized alginate-gelatin hydrogels for muscle tissue engineering applications. J Biomater Appl. 2016;31(1):152–161. doi: 10.1177/0885328216634057. [DOI] [PubMed] [Google Scholar]
- 227.Yi H., Forsythe S., He Y., Liu Q., Xiong G., Wei S. Tissue-specific extracellular matrix promotes myogenic differentiation of human muscle progenitor cells on gelatin and heparin conjugated alginate hydrogels. Acta Biomater. 2017;62:222–233. doi: 10.1016/j.actbio.2017.08.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 228.Kiick K.L. Peptide- and protein-mediated assembly of heparinized hydrogels. Soft Matter. 2008;4(1):29–37. doi: 10.1039/b711319f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 229.Liang Y., Liu W., Han B., Yang C., Ma Q., Song F. An in situ formed biodegradable hydrogel for reconstruction of the corneal endothelium. Colloids Surf B Biointerfaces. 2011;82(1):1–7. doi: 10.1016/j.colsurfb.2010.07.043. [DOI] [PubMed] [Google Scholar]
- 230.Xu W., Liu K., Li T., Zhang W., Dong Y., Lv J. An in situ hydrogel based on carboxymethyl chitosan and sodium alginate dialdehyde for corneal wound healing after alkali burn. J Biomed Mater Res A. 2019;107(4):742–754. doi: 10.1002/jbm.a.36589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 231.Liberski A., Latif N., Raynaud C., Bollensdorff C., Yacoub M. Alginate for cardiac regeneration: from seaweed to clinical trials. Glob Cardiol Sci Pract. 2016;2016(1) doi: 10.21542/gcsp.2016.4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 232.Pena B., Laughter M., Jett S., Rowland T.J., Taylor M.R.G., Mestroni L. Injectable hydrogels for cardiac tissue engineering. Macromol Biosci. 2018;18(6) doi: 10.1002/mabi.201800079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 233.Frey N., Linke A., Suselbeck T., Muller-Ehmsen J., Vermeersch P., Schoors D. Intracoronary delivery of injectable bioabsorbable scaffold (IK-5001) to treat left ventricular remodeling after ST-elevation myocardial infarction: a first-in-man study. Circ Cardiovasc Interv. 2014;7(6):806–812. doi: 10.1161/CIRCINTERVENTIONS.114.001478. [DOI] [PubMed] [Google Scholar]
- 234.Mann D.L., Lee R.J., Coats A.J., Neagoe G., Dragomir D., Pusineri E. One-year follow-up results from AUGMENT-HF: a multicentre randomized controlled clinical trial of the efficacy of left ventricular augmentation with Algisyl in the treatment of heart failure. Eur J Heart Fail. 2016;18(3):314–325. doi: 10.1002/ejhf.449. [DOI] [PubMed] [Google Scholar]
- 235.Nemati S., Rezabakhsh A., Khoshfetrat A.B., Nourazarian A., Biray Avci C., Goker Bagca B. Alginate-gelatin encapsulation of human endothelial cells promoted angiogenesis in in vivo and in vitro milieu. Biotechnol Bioeng. 2017;114(12):2920–2930. doi: 10.1002/bit.26395. [DOI] [PubMed] [Google Scholar]
- 236.Saberianpour S., Karimi A., Nemati S., Amini H., Alizadeh Sardroud H., Khaksar M. Encapsulation of rat cardiomyoblasts with alginate-gelatin microspheres preserves stemness feature in vitro. Biomed Pharmacother. 2019;109:402–407. doi: 10.1016/j.biopha.2018.10.119. [DOI] [PubMed] [Google Scholar]
- 237.Curley C.J., Dolan E.B., Cavanagh B., O'Sullivan J., Duffy G.P., Murphy B.P. An in vitro investigation to assess procedure parameters for injecting therapeutic hydrogels into the myocardium. J Biomed Mater Res B Appl Biomater. 2017;105(8):2618–2629. doi: 10.1002/jbm.b.33802. [DOI] [PubMed] [Google Scholar]