Abstract
Background
Early in the pandemic, inadequate SARS-CoV-2 testing limited understanding of transmission. Chief among barriers to large-scale testing was unknown feasibility, particularly in non-urban areas. Our objective was to report methods of high-volume, comprehensive SARS-CoV-2 testing, offering one model to augment disease surveillance in a rural community.
Methods
A community-university partnership created an operational site used to test most residents of Bolinas, California regardless of symptoms in 4 days (April 20th – April 23rd, 2020). Prior to testing, key preparatory elements included community mobilization, pre-registration, volunteer recruitment, and data management. On day of testing, participants were directed to a testing lane after site entry. An administrator viewed the lane-specific queue and pre-prepared test kits, linked to participants’ records. Medical personnel performed sample collection, which included finger prick with blood collection to run laboratory-based antibody testing and respiratory specimen collection for polymerase chain reaction (PCR).
Results
Using this 4-lane model, 1,840 participants were tested in 4 days. A median of 57 participants (IQR 47–67) were tested hourly. The fewest participants were tested on day 1 (n = 338 participants), an intentionally lower volume day, increasing to n = 571 participants on day 4. The number of testing teams was also increased to two per lane to allow simultaneous testing of multiple participants on days 2–4. Consistent staffing on all days helped optimize proficiency, and strong community partnership was essential from planning through execution.
Conclusions
High-volume ascertainment of SARS-CoV-2 prevalence by PCR and antibody testing was feasible when conducted in a community-led, drive-through model in a non-urban area.
Supplementary Information
The online version contains supplementary material available at 10.1186/s13690-021-00647-8.
Keywords: COVID-19, COVID-19 diagnostic testing, Rural Population, Feasability Studies
Background
In the beginning of the COVID-19 pandemic, impaired access to testing across the United States limited our understanding of epidemiology and thus limited disease control. With clear evidence of asymptomatic infection [1] but minimal systematic active surveillance across larger communities, additional efforts to conduct large-scale testing were needed to understand the breadth of COVID-19 disease.
While there have been other efforts to provide drive-through testing (mostly using polymerase chain reaction [PCR] for symptomatic or exposed individuals) [2–5], no standard procedures existed to safely and efficiently conduct “pop-up” testing using PCR and antibodies for an entire community, particularly in a non-urban setting. The town of Bolinas, California is a coastal town in rural Northern California with a high proportion of elderly residents [6]; early in the pandemic, community leaders were eager to develop university partnerships in order to increase access to SARS-CoV-2 testing. Our objective was to describe the procedures and methodology we used to perform safe, high volume comprehensive testing for SARS-CoV-2 in a non-urban community. To our knowledge, this was the first effort to execute universal PCR and antibody testing for an entire town. By obtaining rapid, comprehensive information about active and past infection, we offer this as one model to augment disease surveillance for rural or suburban populations.
Methods
Prior to testing
Community mobilization (patient and public involvement)
Support from key stakeholders in the community was crucial to this project’s success. In Bolinas, this project was initiated by and co-led by community members, who served as leaders throughout the planning and operational process. Other key stakeholders included the major community-based health organization, the Department of Public Health, and the Fire Department. Most of these groups, together with study leadership, participated in a virtual community meeting the week prior to study start to introduce the study to the community and answer questions. Additionally, specific community liaisons engaged people experiencing homelessness, the Latinx community, and home-bound elders to maximize participation. In summary, while each community has distinct needs, we found that an early needs assessment with regard to community mobilization to identify essential community partners was a most important early step.
Registration & pre-test survey
Town residents and local emergency service providers (such as firefighters, paramedics, etc.) were invited to register online, using a custom interface created on a Health Insurance Portability and Accountability Act (HIPAA) compliant platform in partnership with study leadership and community liaisons. Residents were directed to begin the process by providing contact information for 2-factor authentication (either phone or email) to ensure security and confirm ability to return results. If they were not able to use the online interface, they could call a local facility, where trained volunteers helped people register online.
Participant inclusion in the study was confirmed by providing their zip code or indicating their status as emergency personnel (and/or Bolinas residents). Participants completed an online consent and survey, which included questions about the household as well as demographics, contact information, travel and movement information, symptoms, and medical history. Each household was scheduled for 15-minute appointments allowing no more than five persons per car, and they received a confirmation of their appointment time by their desired mode of contact (mobile phone text message, email). The registration process (via website, telephone, and/or in person) was available in both English and Spanish languages. On the day of testing, participants were emailed or texted with a brief summary of what to expect during their testing experience.
Sample data management
Robust sample identification was a key aspect to ensuring successful data management, and an important challenge to address in the community-based, “pop-up” context. In accordance with Clinical Laboratory Improvement Amendments (CLIA) regulations specified by the clinical laboratory, our labels contained two identifiers, name and date of birth (see example below). Labels additionally contained a random letter code in human readable and quick response (QR) code format, to serve as a scannable identifier linking each specimen to a unique participant record in the online database.
Our site was not equipped for on-demand label printing in each lane, so all pre-registered participants had labels pre-printed the morning prior to testing. Each lane contained a packet of alphabetized, pre-printed water-resistant cryo labels. Each participant had 4 identical labels per sheet: two to be used on the two specimen containers, one on a lab requisition sheet, and one spare label. If the participant registered onsite, the administrator either: (1) used an onsite label printer available in some lanes or (2) used a set of labels with a unique barcode but otherwise blank, and handwrote the participant’s name and date of birth on the labels and requisition form.
During test days
Staffing & flow
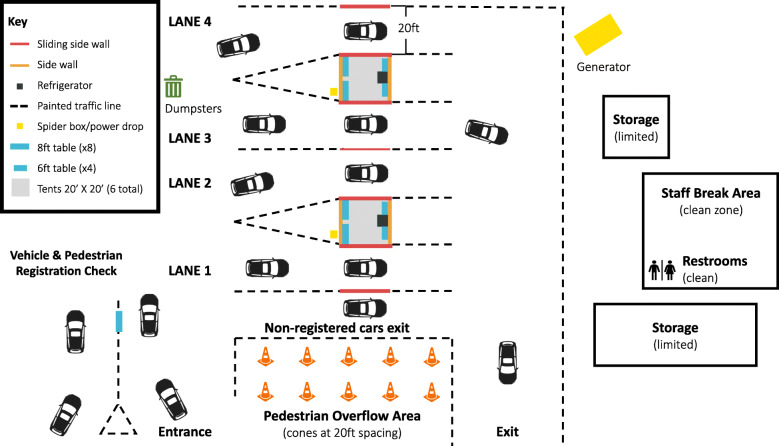
In order to complete testing of more than 1,800 individuals over four days, two tents were set up in a large lot with a lane on either side of each tent, to create four total lanes for testing (Fig. 1). Participants’ first interactions were with primarily community volunteers outside the testing area, who then directed participants toward medical staff and volunteers in each lane for testing.
Fig. 1.
Depicts overall flow through the testing site. Participants entered the site in the lower left corner, and moved clockwise through the site, pausing for specimen collection in each lane while in closest proximity to the tent. Participants on foot were directed to Lane 1, where there were chairs available to set up in the middle of the lane. The staff break area and restrooms were only entered after doffing personal protective equipment.
Site entry & lane triage
To help facilitate entry into the site and prevent interference with regular traffic flow in the area, traffic controllers were stationed at the intersection of the main road. Once cars arrived in the designated area, participants were met by a “greeter” who passed out surgical masks to all participants (Additional file 1: Appendix 1). If Spanish-English translation were required, a volunteer translator was engaged at this point (site entry) to help navigate the testing site experience. Local community members volunteered for these three roles, as healthcare experience was not required but local knowledge and a welcoming presence was very helpful.
Next, a “triage greeter” with a tablet confirmed participants’ pre-registration and appointment time and screened for symptoms of COVID-19, including fever, cough, shortness of breath, fatigue, myalgias, anosmia, and dysgeusia. If a participant (or anyone in the vehicle) were symptomatic, they were directed to the specified symptomatic lane. If asymptomatic, the triage greeter directed participants to the shortest lane. Because of the symptom assessment, triage greeters were volunteers in the healthcare field who were comfortable with tablet use. Using the online platform on the tablet, the triage greeter indicated which lane the participant moved into, allowing each lane’s administrator (sitting in the tent) to view the queue of participants in their lane and prepare for their arrival.
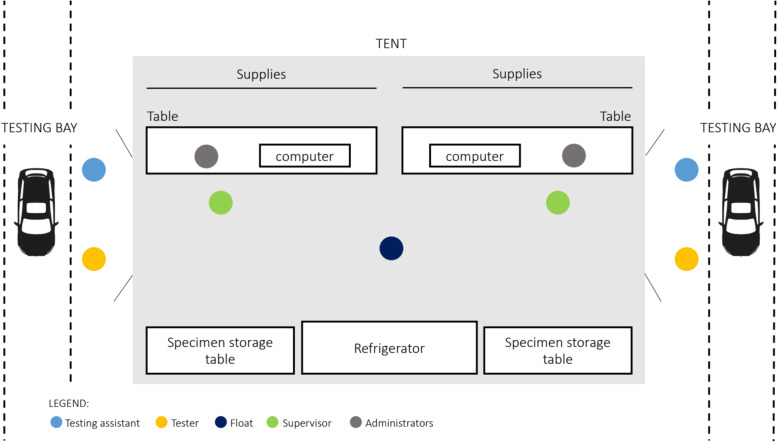
Testing bay & tent staffing/flow
There was one testing bay per lane, each staffed by 4 people: two dyads of 1) professional phlebotomist who performed testing (”tester”) and 2) a healthcare volunteer (primarily nursing, medical, and pharmacy students) who served as the “test assistant” (Fig. 2). Inside the tent, an additional volunteer provided administrative support to each lane. Finally, each tent had two tent supervisors, each of whom was a graduate-level trained nurse, physician, or trained volunteer. As a participant approached the testing bay in any given lane, the test assistant confirmed the participant’s name, date of birth, and whether they had symptoms that day. Without entering the tent themselves, the test assistant in the bay relayed this information back to the administrator in the tent, who logged symptoms and prepared a test kit for each participant.
Fig. 2.
Depicts staffing, set up, and flow of two testing lanes, serviced by one tent. Participants slowly pulled forward into the testing lane and were stopped next to the tent. The testing assistant confirmed participant identifiers and verified match with administrator, who handed off pre-made testing kit with materials necessary for specimen collection. The tester explained procedures to the participant and collected samples, with support from testing assistant as needed. The float ensured the specimens were stored correctly, and the administrator logged that testing was complete as the participant exited the testing bay
To facilitate throughput, test kits containing all supplies necessary to complete testing in the bay (alcohol wipe, lancet, microtainer, gauze, tongue depressor, swab, viral transport media, biohazard bag) were assembled in advance. The administrator’s role was primarily to locate the appropriate participant labels and afix labels to (1) the microtainer, (2) the viral transport media tube, and (3) requisition sheet. Labeling and test kit preparation was ideally performed in advance of the participant reaching the testing bay, facilitated by the administrator’s ability to view their lane’s queue in the online platform.
In the testing bay, a car pulled into the bay and turned off the engine. If participants arrived on foot or other vehicle, to accommodate those without access to a car, they were seated in a chair in the middle of the lane. The tester explained the procedure, and completed finger stick then oropharyngeal/mid-turbinate swab (see Test Procedures for more detail). The test assistant maintained distance from the participant during specimen collection, but was on hand to pass items to the testers. Extra test assistants were trained, with additional test assistants helping as runners/quality control leads when not working actively in the testing bays. Once a participant had completed testing, the test assistant verbally reported completion to the in-tent administrator, and the administrator noted whether tests were successfully administered and that the label barcode matched the database barcode. The participant exited the lane and testing site.
Each tent was also staffed with two tent supervisors, whose role was to trouble-shoot all activities in the testing bay and tent, including responding to participant questions, and ensuring operations ran efficiently. See Additional file 1: Appendix 1 for summary of staffing required per day. Finally, on-site staff were screened with an email-based questionnaire before each day to ensure they did not have symptoms associated with COVID-19 (Additional file 2: Appendix 2).
Test procedures
Our testing strategy employed both blood collection for antibody testing and upper respiratory tract sampling for PCR testing. With regard to collection of blood, our goal was to maximize community participation by lowering barriers to sampling through use of a finger prick technique (vs. phlebotomy), while collecting enough blood to be sufficient to run quantitative, laboratory-based tests [7]. Please see Additional file 3: Appendix 3 for detailed procedures utilized for sample collection.
PPE requirements
We constructed personal protective equipment (PPE) requirements using the following framework adapted from World Health Organization guiding principles: (1) consider the type of contact with participants, (2) incorporate transmission dynamics and environmental factors pertinent to the testing site, and (3) utilize stewardship and appropriate PPE re-use when possible [8].
For each role, we defined the degree of contact with participants and whether possible to adhere to physical distancing while performing the role. For example, the tester role involved physical contact with participants’ hands and proximity to unmasked participants during oropharyngeal and mid-turbinate specimen collection that may lead to sneeze or cough. As follows, PPE requirements for this role were the most stringent, including coveralls (or gown), gloves, respirator, and face shield. Conversely, the test assistant did not have physical contact with participants nor were they in close proximity during specimen collection but did talk with participants prior to testing and were also handling specimens after collection. As such, the recommended PPE for this role was a surgical mask, face shield, and gloves. Please see Additional file 1: Appendix 1 for detailed PPE recommendations for all roles. When considering generalizability to other testing approaches, the most important consideration should be given to the movements and participant interactions involved in each role with PPE recommendations based on associated exposure risk.
Finally, with regard to PPE reuse, we modeled our guidelines after our medical center and CDC guidelines to minimize waste of materials (all materials listed in Additional file 4: Appendix 4) [9, 10]. In brief, gowns and gloves were never reused, but face shields and masks (either surgical or respirators) were safely removed, cleaned and stored for reuse throughout the day.
Post-testing
At end of each testing day, blood samples in microtainers were stored upright in small cardboard specimen boxes, and viral transport media in biohazard bags was ideally stored upright as well. Specimens were transported to the lab each evening for accessioning overnight. Participants were counseled to expect PCR results within 3–7 days and antibody results within 4–6 weeks. Study staff planned to call each participant with a positive PCR result and direct their results to the Department of Public Health. Additionally, both positive and negative results were delivered via the same online platform through which participants registered. Participants received a text message or email with a code that allowed them to login to view their results. Alternatively, they had the option of calling a hotline for additional support.
Results
Testing site throughput
In total, 1,840 participants were tested over 4 days (April 20th - April 23rd, 2020) using this 4-lane drive-through or walk-up model. Seven participants received home-based testing on a supplemental 5th and final day of testing, to total 1,847 participants overall. As previously published, this represented estimated community ascertainment over 80 % [11].
Fewer participants were scheduled on the first day of testing to allow for study staff and volunteer acclimation to their roles. On Day 1, the fewest number of participants were tested (n = 338 participants), increasing to the highest number tested on Day 4 (n = 571 participants). Notably, performance on Days 2–4 reflects staffing described above, whereas there were fewer personnel available to staff the testing bays on Day 1.
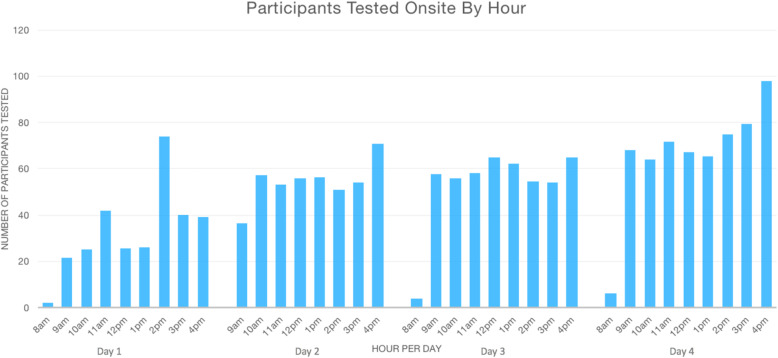
Figure 3 depicts the number of participants tested per hour across all lanes for each of the four days of onsite testing. When including the hours during which time the testing site was fully open for appointments (9am − 5pm), the median number of participants tested per hour onsite was 57 (interquartile range 47–67). The participants included in this analysis were 1,801 participants with time-stamped checkouts (compared to the total of 1,847), slightly underestimating actual throughput.
Fig. 3.
Number of participants with onsite testing completed and logged (on the Y-axis) per hour of day (on the X-axis.) The testing site was fully open for appointments between 9am - 5pm.
Discussion
Using the aforementioned methods, we utilized close community partnership and a 4-lane, drive-through and walk-up model to test 1,840 participants for SARS-CoV-2 with both PCR and antibody testing in 4 days. Few methodologic papers have described detailed procedures in this way, but our reported throughput exceeds another study conducted early in the pandemic described testing 1,153 participants for SARS-CoV-2 with PCR only in 7 days [2]. In addition to the identified areas for improvement below, an additional limitation of our methodologic reporting is the changing (and possibly diminished) utility of SARS-CoV-2 mass testing as the pandemic evolves. On the other hand, these methods will likely prove useful to those planning mass testing campaigns in the context of either emerging SARS-CoV-2 variants or other pandemics due to respiratory viral illnesses.
Identified areas for improvement
While this was overall a successful endeavor, we faced a number of challenges that others may improve upon in the future. Our labeling system largely worked well when participants were pre-registered, but when participants registered onsite or identified an error in their name or date of birth, handwriting labels was both time-consuming and error prone. Possible improvements include using an onsite label printer along with a barcode scanner in each lane to automate this process as much as possible.
Another challenge was verification of participant identifiers when all parties were wearing masks and maintaining physical distancing. While tent supervisors emphasized ongoing closed-loop communication between team and participants, alternative strategies to verbal communication may offer an improvement. For example, test assistants could use a small white board to write participant identifiers and visually confirm these details with the participant and the administrator.
Finally, despite quality control measures, a small number of viral transport media tubes leaked material upon receipt in the lab. As such, we recommend using tightly sealing vials, inspecting vials prior to testing and upright storage of samples in individual biohazard bags.
An additional suggestion would be to test the entire process in advance of testing roll out, from onsite registration to sample collection to lab reporting. Given the speed with which our efforts were planned, we were limited to testing of individual pieces of the protocol with a final “dress rehearsal” conducted just prior to opening. This issue could also be mitigated by having an experienced team performing the same operations in other locations. That said, our results demonstrate that even in face of rapid planning and new operational system development, we were able to successfully exceed our goals for testing.
Conclusions
In summary, high-volume, community-wide ascertainment of SARS-CoV-2 prevalence by PCR and antibody testing was feasible and could be performed successfully when conducted in a community-led, drive-through model, with minimal start up time. This operational model may be generalizable to those conducting any sort of high-throughput testing for SARS-CoV-2, regardless of sampling methodology.
Supplementary information
Appendix 1.
Appendix 2.
Appendix 3.
Appendix 4.
Acknowledgements
We would like to acknowledge Andrew Kobylinkski for contributing his considerable technical expertise to this project.
Abbreviations
- PCR
Polymerase chain reaction
- HIPAA
Health Insurance Portability and Accountability Act
- CLIA
Clinical Laboratory Improvement Amendments
- QR
Quick Response
- PPE
Personal Protective Equipment
Authors’ contributions
AA helped design the work, collected data, and primarily drafted the manuscript. GC, DH, and BG conceived of the project, helped interpret data, and critically revised manuscript. AS, KB contributed substantially to design and implemention of the project, drafted portions of the manuscript. KD, SR, ED, JV, and CLIAHUB Consortium contributed key aspects of project design and data management, in addition to critical review of the manuscript. JKF, SR, DM, KN, JI contributed markedly to acquisition of data in addition to critical review of the manuscript. The author(s) read and approved the final manuscript.
Funding
This work was primarily supported by the Bolinas Community Land Trust. Additional sources of support included funding from the Chan Zuckerberg Biohub Investigator program (BG) and the National Institutes of Health grant 5T32AI007641-17 (AA).
Availability of data and materials
Most materials generated as part of this study are included in this published article. The corresponding author welcomes email requests for additional materials, if this would be helpful.
Declarations
Ethics approval and consent to participate
The aforementioned procedures were submitted to the University of California San Francisco institutional review board for approval, and the study was deemed public health surveillance not requiring IRB oversight [IRB number 20-30636].
Consent for publication
Not applicable.
Competing interest
None of the authors have potential conflicts of interest or competing interests to disclose.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Furukawa NW, Brooks JT, Sobel J. Evidence Supporting Transmission of Severe Acute Respiratory Syndrome Coronavirus 2 While Presymptomatic or Asymptomatic - Volume 26, Number 7—July 2020 - Emerging Infectious Diseases journal - CDC. 10.3201/eid2607.201595. [DOI] [PMC free article] [PubMed]
- 2.Ton AN, Jethwa T, Waters K, Speicher LL, Francis D. COVID-19 drive through testing: An effective strategy for conserving personal protective equipment. Am J Infect Control. 2020;48:731–2. doi: 10.1016/j.ajic.2020.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kwon KT, Ko JH, Shin H, Sung M, Kim JY. Drive-Through Screening Center for COVID-19: a Safe and Efficient Screening System against Massive Community Outbreak. J Korean Med Sci. 2020;35:e123. doi: 10.3346/jkms.2020.35.e123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.UW COVID-19 Drive Thru Clinic AKA. “The CARVID” Clinic | Technical Resources. ASPR TRACIE. https://asprtracie.hhs.gov/technical-resources/resource/7856/uw-covid-19-drive-thru-clinic-aka-the-carvid-clinic. Accessed 17 May 2021.
- 5.COVID-19 Community Based Testing Guide | Project Baseline by Verily. https://www.projectbaseline.com/covid-19-guide/. Accessed 17 May 2021.
- 6.Bolinas CA, Population -. Census 2010 and 2000 Interactive Map, Demographics, Statistics, Quick Facts - CensusViewer. http://censusviewer.com/city/CA/Bolinas. Accessed 19 Jul 2020.
- 7.Krammer F, Simon V. Serology assays to manage COVID-19. Science. 2020;368:1060–1. doi: 10.1126/science.abc1227. [DOI] [PubMed] [Google Scholar]
- 8.World Health Organization. Rational use of personal protective equipment (PPE) for coronavirus disease (COVID-19): interim guidance, 19 March 2020. 2020. https://apps.who.int/iris/handle/10665/331498. Accessed 17 May 2021.
- 9.COVID-19. Personal Protective Equipment (PPE) | UCSF Health Hospital Epidemiology and Infection Prevention. https://infectioncontrol.ucsfmedicalcenter.org/coronavirus/ppe. Accessed 17 May 2021.
- 10.CDC. COVID-19 guidance, tools, and resources for healthcare workers. Centers for Disease Control and Prevention. 2020. https://www.cdc.gov/coronavirus/2019-ncov/hcp/guidance-risk-assesment-hcp.html. Accessed 17 May 2021.
- 11.Appa A, Takahashi S, Rodriguez-Barraquer I, Chamie G, Sawyer A, Duarte E, et al. Universal Polymerase Chain Reaction and Antibody Testing Demonstrate Little to No Transmission of Severe Acute Respiratory Syndrome Coronavirus 2 in a Rural Community. Open Forum Infect Dis. 2020;8(1):ofaa531. 10.1093/ofid/ofaa531. eCollection 2021 Jan. [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix 1.
Appendix 2.
Appendix 3.
Appendix 4.
Data Availability Statement
Most materials generated as part of this study are included in this published article. The corresponding author welcomes email requests for additional materials, if this would be helpful.