Abstract
Background
Many women experience fear of childbirth (FOC). While fears about childbirth may be normal during pregnancy, some women experience high to severe FOC. At the extreme end of the fear spectrum is tocophobia, which is considered a specific condition that may cause distress, affect well‐being during pregnancy and impede the transition to parenthood. Various interventions have been trialled, which support women to reduce and manage high to severe FOC, including tocophobia.
Objectives
To investigate the effectiveness of non‐pharmacological interventions for reducing fear of childbirth (FOC) compared with standard maternity care in pregnant women with high to severe FOC, including tocophobia.
Search methods
In July 2020, we searched Cochrane Pregnancy and Childbirth’s Trials Register, ClinicalTrials.gov, the World Health Organization (WHO) International Clinical Trials Registry Platform (ICTRP), and reference lists of retrieved studies. We contacted researchers of trials which were registered and appeared to be ongoing.
Selection criteria
We included randomised clinical trials which recruited pregnant women with high or severe FOC (as defined by the individual trial), for treatment intended to reduce FOC. Two review authors independently screened and selected titles and abstracts for inclusion. We excluded quasi‐randomised and cross‐over trials.
Data collection and analysis
We used standard methodological approaches as recommended by Cochrane. Two review authors independently extracted data and assessed the studies for risk of bias. A third review author checked the data analysis for accuracy. We used GRADE to assess the certainty of the evidence. The primary outcome was a reduction in FOC. Secondary outcomes were caesarean section, depression, birth preference for caesarean section or spontaneous vaginal delivery, and epidural use.
Main results
We included seven trials with a total of 1357 participants. The interventions included psychoeducation, cognitive behavioural therapy, group discussion, peer education and art therapy.
We judged four studies as high or unclear risk of bias in terms of allocation concealment; we judged three studies as high risk in terms of incomplete outcome data; and in all studies, there was a high risk of bias due to lack of blinding. We downgraded the certainty of the evidence due to concerns about risk of bias, imprecision and inconsistency. None of the studies reported data about women's anxiety.
Participating in non‐pharmacological interventions may reduce levels of fear of childbirth, as measured by the Wijma Delivery Expectancy Questionnaire (W‐DEQ), but the reduction may not be clinically meaningful (mean difference (MD) ‐7.08, 95% confidence interval (CI) ‐12.19 to ‐1.97; 7 studies, 828 women; low‐certainty evidence). The W‐DEQ tool is scored from 0 to 165 (higher score = greater fear).
Non‐pharmacological interventions probably reduce the number of women having a caesarean section (RR 0.70, 95% CI 0.55 to 0.89; 5 studies, 557 women; moderate‐certainty evidence).
There may be little to no difference between non‐pharmacological interventions and usual care in depression scores measured with the Edinburgh Postnatal Depression Scale (EPDS) (MD 0.09, 95% CI ‐1.23 to 1.40; 2 studies, 399 women; low‐certainty evidence). The EPDS tool is scored from 0 to 30 (higher score = greater depression).
Non‐pharmacological interventions probably lead to fewer women preferring a caesarean section (RR 0.37, 95% CI 0.15 to 0.89; 3 studies, 276 women; moderate‐certainty evidence).
Non‐pharmacological interventions may increase epidural use compared with usual care, but the 95% CI includes the possibility of a slight reduction in epidural use (RR 1.21, 95% CI 0.98 to 1.48; 2 studies, 380 women; low‐certainty evidence).
Authors' conclusions
The effect of non‐pharmacological interventions for women with high to severe fear of childbirth in terms of reducing fear is uncertain. Fear of childbirth, as measured by W‐DEQ, may be reduced but it is not certain if this represents a meaningful clinical reduction of fear. There may be little or no difference in depression, but there may be a reduction in caesarean section delivery. Future trials should recruit adequate numbers of women and measure birth satisfaction and anxiety.
Plain language summary
Non‐pharmacological interventions for fear of childbirth (tocophobia) in pregnancy
Key messages
While non‐medicine treatments may reduce levels of fear for pregnant women with a high to severe fear of childbirth compared to standard maternity care, the reduction may not represent a meaningful change in their level of fear.Non‐medicine treatments probably reduce the number of women who have a caesarean section, where the baby is born surgically. Future research in this area should focus on measuring anxiety levels in women with a high or severe fear of childbirth.
What is fear of childbirth?
Fear of childbirth can range from minor worries and anxieties about giving birth, to a severe fear of childbirth that has a considerable impact on women's lives, causing distress and affecting their mental well‐being. A high to severe level of childbirth fear may include extreme levels of fear also known as ‘tocophobia’.
It is normal for pregnant women – particularly first‐time mothers – to be anxious, worried or fearful about giving birth. However, some women have high fear related to childbirth and a smaller number have a severe fear of childbirth or ‘tocophobia’. These women:
‐ may have feelings of isolation, guilt and shame;may choose to terminate a healthy pregnancy, hide a pregnancy or be in denial about a pregnancy;
‐ may find it difficult to prepare for birth or access pregnancy information because of their fear and may experience problems bonding with their baby;
‐ may have sleeplessness, nightmares, stomach aches, depression and anxiety that leads to panic attacks.
Women with a high to severe fear of childbirth are more likely to have a planned or emergency caesarean birth, instrumental birth and experience physical effects related to fear, such as prolonged labour. Women with high fear of childbirth without a history of depression are more likely to experience postnatal depression.
How is fear of childbirth treated?
The causes of fear of childbirth are complex and unique for each woman. High to severe fear of childbirth is not recognised or provided for in maternity care in many places in the world. Ways of treating fear of childbirth need to be investigated.
Effective treatments would help women to have confidence in their ability to give birth, give them ways of coping with labour, and empower their decision‐making during pregnancy and the birth process.
Treatments aim to provide extra support to women and include:
‐ sensitive education about the birth process;development of problem‐solving skills;
‐ teaching coping strategies for labour;
‐ and affirming that negative childbirth events can be managed.
What did we want to find out?
We wanted to find out if non‐pharmacological (non‐medicine) treatments were better than the standard maternity care provided to pregnant women in terms of:
‐ reducing women’s level of fear, as measured by a widely‐used questionnaire for childbirth fear;
‐ reducing the number of women having a caesarean birthsection;
‐ reducing anxiety and depression.
What did we do?
We searched for studies that investigated non‐pharmacological treatments aimed at reducing fear of childbirth. We compared and summarised the results of the studies and rated our confidence in the evidence, based on factors such as study methods and number of participants.
What did we find?
We found seven studies that involved 1357 pregnant women with a high to severe fear of childbirth including tocophobia. The studies investigated different types of treatment, including:
‐ psychoeducation (a structured form of education offered to people with mental health conditions);
‐ cognitive behavioural therapy (a ‘talking therapy’ that aims to help identify and change underlying thought patterns);
‐ group discussion;peer teaching from other pregnant women;
‐ and art therapy.
The studies were conducted in five different countries (Australia, Iran, Sweden, Finland and Turkey).
We found that non‐pharmacological treatments:
‐ may reduce fear of childbirth when measured by a widely‐used questionnaire, though the reduction may not represent a meaningful change in women's level of fear.
‐ probably reduce the number of women who go on to have caesarean births (28% of women receiving non‐drug treatments had caesarean sections, compared to 40% of women not receiving treatment for fear of childbirth).
‐ may make little to no difference compared to standard maternity care in terms of women’s depression scores.
What are the limitations of the evidence?
Our confidence in the evidence is limited because the studies were done in such a way that their results may be inaccurate, and because there were low numbers of women in the studies.
How up to date is this evidence?
The evidence in this review is up to date to July 2020.
Summary of findings
Summary of findings 1. Non‐pharmacological interventions for fear of childbirth (tocophobia) compared to usual care.
| Non‐pharmacological interventions for fear of childbirth (tocophobia) compared to usual care | ||||||
| Patient or population: women with fear of childbirth (tocophobia) Setting: antenatal clinics in hospitals in Australia, Sweden, Finland and Turkey, and primary care setting in Iran Intervention: non‐pharmacological interventions for fear of childbirth (psychoeducation, discussion, Internet cognitive behavioural therapy, art therapy, peer education) Comparison: usual care | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | № of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Risk with usual care | Risk with non‐pharmacological interventions for fear of childbirth | |||||
| Fear of childbirth assessed with: Wijma Delivery Expectancy Questionnaire Scale from 0 to 165; higher score = greater fear | The mean fear of childbirth score in the control group ranged from 57 to 108 | MD 7.08 lower (12.19 lower to 1.97 lower) | ‐ | 828 (7 RCTs) | ⊕⊕⊝⊝ LOWa,b | May reduce fear of childbirth score but the reduction may not be clinically meaningful |
| Caesarean section | Study population | RR 0.70 (0.55 to 0.89) | 557 (5 RCTs) | ⊕⊕⊕⊝ MODERATEa | Probably reduces number of women having caesarean section | |
| 400 per 1000 | 280 per 1000 (220 to 356) | |||||
| Anxiety ‐ not reported | ‐ | ‐ | ‐ | ‐ | ‐ | |
| Depression
assessed with: Edinburgh Postnatal Depression Scale Scale from 0 to 30; higher score = greater depression |
The mean depression score in the control group ranged from 5.46 to 8.1 | MD 0.09 higher (1.23 lower to 1.4 higher) | ‐ | 399 (2 RCTs) | ⊕⊕⊝⊝ LOWa,c | May be little to no difference in postnatal depression |
| Birth preferences: prefer caesarean section | Study population | RR 0.38 (0.08 to 1.85) | 208 (2 RCTs) | ⊕⊕⊝⊝ LOWa,c | It is uncertain if there is any effect on number of women who prefer caesarean section | |
| 314 per 1000 | 119 per 1000 (25 to 581) | |||||
| Epidural analgesia during labour | Study population | RR 1.21 (0.98 to 1.48) | 380 (2 RCTs) | ⊕⊕⊝⊝ LOWa,d | May increase number of women having epidural | |
| 442 per 1000 | 535 per 1000 (433 to 654) | |||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; RR: risk ratio; OR: odds ratio | ||||||
| GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect Moderate certainty: we are moderately confident in the effect estimate. The true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different Low certainty: our confidence in the effect estimate is limited. The true effect may be substantially different from the estimate of the effect Very low certainty: we have very little confidence in the effect estimate. The true effect is likely to be substantially different from the estimate of effect | ||||||
aDowngraded one level for risk of bias (due to lack of blinding of participants and outcome assessors). bDowngraded one level for inconsistency (due to lack of overlap of 95% confidence intervals and differing size and direction of effect). cDowngraded one level for imprecision (due to few participants and 95% confidence intervals crossing the line of no effect). dDowngraded one level for imprecision (single trial only with 95% confidence intervals crossing the line of no effect).
Background
In order to be inclusive we have used neutral or gender neutral terms to include all people who experience pregnancy and birth and avoid gendering the issue since fear of childbirth may affect transgender people.
Description of the condition
Introduction
The childbirth experience is described as a profound landmark and is a life‐affirming event for many women (Larkin 2009). However, women experience many different emotions during pregnancy, from happiness and joy, to anxiety, fear and horror. Therefore, the experience of pregnancy and birth is individual, subjective, complex and multidimensional (Larkin 2009). It is common for pregnant women ‐ particularly first‐time mothers ‐ to experience anxiety, worry or fear with varying severity in relation to childbirth (Melender 2002; Nilsson 2018; Salomonsson 2010; Zar 2001). Women are three times more likely to be diagnosed with an anxiety disorder than depression in the postnatal period (Fairbrother 2007). Yet research on anxiety in the perinatal period has lacked attention to date, in comparison with the focus on perinatal depression (Hofberg 2003; Howard 2014). There is a growing body of literature which recognises the importance of identifying fear of childbirth (FOC) and pregnancy‐related anxieties in maintaining women's perinatal mental health (Hofberg 2003; Stoll 2018; Toohill 2014; Weaver 2013). There is cumulative evidence that FOC predisposes women to postnatal depression (Alipour 2012; Räisänen 2014), and post‐traumatic stress disorder (PTSD) (Ayers 2016). In addition, various epidemiological studies and Cochrane Reviews have identified the significance of recognising ‐ in the antenatal period ‐ the psychological and psychosocial risk factors for postnatal depression (Alipour 2012; Ayers 2016; Dennis 2013; Dennis 2017; Räisänen 2014; Stoll 2018).
For some women, FOC is so severe that it affects their daily lives, and spoils their experience of pregnancy (Salomonsson 2010). Feelings of isolation, guilt and shame, due to perceived stigma, have been reported by women with high to severe FOC, since pregnancy is generally seen as a time of happiness and women may feel unable to talk about their fears with their partners or midwives (Eriksson 2006; Lyberg 2010; Nilsson 2009). Moreover, high to severe FOC can negatively impact partner relationships (Salomonsson 2010), which is important as low levels of social support and partner dissatisfaction are significantly associated with FOC (Gao 2015; Salomonsson 2010; Toohill 2014). There is evidence that information provided to women in the clinical setting may have a positive or negative influence on FOC (Salomonsson 2010). In extreme cases, women may use scrupulous methods of contraception to avoid pregnancy, experience psycho‐sexual difficulty, choose to terminate a healthy pregnancy, or conceal or be in denial about pregnancy (Gutteridge 2013). In the latter case, women refuse scans and demonstrate avoidance behaviours by mentally blocking out feelings of being pregnant such as fetal movement (Gutteridge 2013). Moreover, physical and psychological effects such as sleeplessness, nightmares, stomach aches, depression and anxiety leading to panic attacks have been reported (Hall 2009; Laursen 2008; Räisänen 2014; Zar 2001). Women who are in denial about pregnancy may avoid birth preparation classes (Salomonsson 2010), and as a result, experience low self‐efficacy in the ability to give birth (Lowe 2000). Furthermore, it is well‐established that women with high to severe FOC are more likely to have a caesarean birth (both emergency and due to maternal request), and experience physiological effects related to fear, such as prolonged labour (Adams 2012; Haines 2012; Karlström 2009; O'Donovan 2018; Räisänen 2014; Ryding 2015; Saisto 2001; Weaver 2013).
Women may have different attitudes towards or cultural beliefs about childbirth, which can influence how they experience the birth process (Gutteridge 2013; Haines 2012). The culture of birth can influence these attitudes and beliefs. For example, risk‐averse medical models tend to influence women's decisions about interventions during childbirth, and whether women take an active or passive role during childbirth (Haines 2012). In general, a cultural shift in women's attitudes towards birth has been noted, corresponding with the increased use of medical interventions, such as induction of labour and epidural use, leading to women losing confidence in their ability to give birth and to cope with labour pain (Green 2003; Haines 2012). There has also been a shift in women's expectations of birth (Darvill 2010).
In theory, maternity care aims to place women at the centre of decision‐making about their care. However, in actual clinical practice, it seems evident that the terms 'woman‐centred care' and 'informed choice' are often simply rhetoric (Haines 2012). There has been a growing trend of neglectful, disrespectful or abusive behaviour in some contexts and settings, which has lacked attention from healthcare professions, but which has affected women (Bohren 2014; Freedman 2014). Examples of the mistreatment of women globally include physical abuse, such as slapping or pinching, sexual abuse, verbal abuse, stigma, neglect during the birth, poor or ineffective communication, loss of autonomy and inadequately resourced health systems which fail to provide women with privacy and dignity during birth (Bohren 2014). The attitudes of healthcare professionals, such as midwives and obstetricians, play a significant role in women's perceptions of risk and their consequent fear. In one study, 31% of female obstetricians in London, United Kingdom (UK), indicated a birth preference for caesarean sections (CS) for their own births (Al Mufti 1997), which suggests that there may be a personal bias or an influence when presenting information to women (Dahlen 2010). Aiming to provide pregnant women with a trusting relationship could help reduce fear (Dahlen 2010; Hildingsson 2018; Lyberg 2010).
Social norms and the emotional experiences of women, such as perceptions about lack of control and safety, could influence women's decision to request a caesarean section, according to a qualitative systematic review (O'Donovan 2018). In some cultures, caesarean section is now perceived as 'normal' and as a mark of empowerment and social status in a consumerist world (Faisal 2014; Fenwick 2010). This shift in cultural beliefs is deep‐rooted and ultimately underpinned by fear (O'Donovan 2018). Qualitative evidence suggests that FOC may be transmitted from generation to generation through vicarious experiences of family members who had difficult labours or negative births, leading to the perception of caesarean section as a 'safer' option (Hull 2011; O'Donovan 2018).
Various studies have investigated the causes and consequences of high to severe FOC. Typical sources of fear include (but are not limited to): fear of the unknown, fear of pain, fear of perineal trauma, feeling lack of involvement in decision‐making during birth, being left alone in labour, fear for the infant's health or own health or death (Fenwick 2015; O'Donovan 2018; Salomonsson 2010). FOC is strongly associated with intimate partner violence, sexual abuse, rape and unintended pregnancy (Gutteridge 2013; Miller 2010). A large epidemiological study reported that women with high to severe FOC were more likely to have had anaemia, miscarriages, a previous early termination of pregnancy, assisted reproductive procedures, or chorionic villus sampling (a test which may be offered during pregnancy to check if the baby has a genetic or chromosomal condition) (Räisänen 2014). A large Australian study (n = 510,006) which looked at all singleton births in New South Wales in 2000 to 2008 found that women who experienced severe perineal trauma during their first birth were less likely to have a subsequent baby (Priddis 2013).
Defining high to severe FOC
FOC exists on a spectrum from low fear to high and phobic fear, but it is difficult to assess when fear of childbirth becomes 'tocophobia'. Typically, a phobia is characterised by avoidance behaviours. From a psychiatric perspective, a Structured Clinical Interview for DSM 5 (SCID‐5) may be performed to assess women. However, there is a dearth of perinatal psychiatrists and such interviews are not common practice in maternity care (Brockington 2017; Nath 2018). When a psychiatric assessment is performed, women with FOC will usually receive a diagnosis of generalised anxiety disorder; thus, high to severe FOC comes under the umbrella of anxiety disorders (Stoll 2018; Striebich 2018). In Scandinavia, FOC has been categorised in the International Classification of Diseases, 10th revision (ICD‐10; World Health Organization 2018). However, FOC has not specifically been included in the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM‐5; Americian Psychiatric Association 2013). Unlike most phobias, which are irrational, high to severe FOC is usually not a pathological fear, but a situational fear which is personal to the individual. The most common definition of tocophobia is a self‐reported Wijma Delivery Expectancy Questionnaire version A (W‐DEQ A) score greater than or equal to 85 (O'Connell 2017; Wijma 1998). Further details of the tool are outlined below.
Tools for measuring FOC
FOC can be assessed using a range of self‐reported questionnaires or diagnostic interviews (Lowe 2000; O'Connell 2017; Rouhe 2011; Stoll 2018; Striebich 2018; Wijma 1998). The most common tool used to assess severity of FOC is the W‐DEQ A in the antenatal period, with the W‐DEQ B used to assess childbirth fear in the postnatal period, which can help determine when women may benefit from treatment (Wijma 1998). The tool was developed originally in Sweden by Klaas Wijma, and psychometric analysis has shown it to be valid and reliable for women of all parity (Wijma 1998). The questionnaire consists of 33 questions on a Likert scale (zero to six) that aim to evaluate women's cognitive appraisal of the upcoming birth in the antenatal period, and evaluate their experiences after birth in the postnatal period (Wijma 1998). Wijma himself recommended using cut‐offs of greater than or equal to 85 to define severe FOC and tocophobia and greater than or equal to 66 to represent high fear (Wijma 1998). However, various other cut‐offs have been used in research studies (W‐DEQ A ≥ 71, W‐DEQ A ≥ 86, W‐DEQ A ≥ 100) (Nilsson 2018; O'Connell 2017; Wijma 1998).
Epidemiology of FOC
FOC exists on a spectrum, from minor worries and anxieties, to moderate FOC which does not impact women's everyday life, to high and severe FOC, and tocophobia, which has a considerable impact on women's lives and affects their psychological well‐being (Areskog 1981; Larsson 2017; Nilsson 2018; O'Connell 2017).
A multidisciplinary approach encompassing a holistic package of care may be beneficial to provide emotional support for women with FOC (Jomeen 2021). The majority of people with moderate FOC may be managed by midwifery counselling, education, discussing the birth and continuity of care (Jomeen 2021). Tocophobia may be treated by specific, targetted interventions like Cognitive Behavioural Therapy or exposure therapy (Jomeen 2021; Stoll 2018). To date, tocophobia has been examined from a psychiatric perspective, rather than by obstetricians or midwives, and there is a significant association between previous sexual abuse and rape (Gutteridge 2013). Various definitions are used for tocophobia (O'Connell 2017), which is a key challenge when estimating prevalence, assessing women for high to severe FOC, designing interventions, and evaluating outcomes. It is possible that there are cultural factors influencing this variation, as well as the obvious limitations of self‐reported measures (O'Connell 2017Haines 2012). However, due to increased interest in the topic, more women are finding the courage to speak about their experience of tocophobia. Prevalence reports of severe FOC range from 3.7% to 43% and a meta‐analysis estimated a global pooled prevalence of 14% (95% confidence interval 0.12 to 0.16), using a random‐effects model (O'Connell 2017). Furthermore, approximately 20% of women experience high fear (O'Connell 2017; Toohill 2014). The majority of prevalence studies have reported that high to severe FOC is more common in nulliparous women (who have never given birth to a child), but some studies have found the opposite (O'Connell 2017). In parous women, previous mode of birth (instrumental or emergency caesarean section) is associated with high FOC (Rouhe 2011; Toohill 2014), and high FOC in one pregnancy is the strongest risk factor for high FOC in a subsequent pregnancy (Storksen 2012). Ternström and colleagues have described high FOC in 'foreign‐born women', who report feeling isolated since they lack the network of family and friends to support them and may have specific, sensitive cultural requirements in maternity care (Ternström 2015; Ternström 2016). Thus, identifying women with high to severe FOC and interventions for high to severe FOC need to be inclusive of vulnerable groups such as migrant women, who may be at even higher risk of postnatal depression (Ternström 2015). Given the prevalence of high to severe FOC, the condition is a key concern for midwives and obstetricians because of its multi‐factorial impact on the mother as well as her partner and infant.
Management of high to severe FOC
The majority of research in this field has been conducted where care pathways are well‐established, but in parts of the western world, high to severe FOC is not currently recognised or provided for in maternity care (O'Connell 2017). Even in countries where high to severe FOC is recognised, approaches to care vary widely and are not based on empirical evidence (Bewley 2002; Richens 2015). In Sweden, women with high to severe FOC are referred for counselling with midwives in Aurora clinics ‐ specialty clinics introduced by midwives with an interest in childbirth fear that serve women using a personalised approach (Larsson 2016; Larsson 2017). This involves an interdisciplinary team of midwives, obstetricians, social workers and psychologists, as appropriate, for each individual woman (Larsson 2016). The advent of the clinics was not preceded by a randomised controlled trial, and a retrospective evaluation reported that they did not reduce caesarean section rates (Larsson 2017; Ryding 2003). However, women were satisfied with the care and half the women experienced a reduction in FOC (Larsson 2017; Ryding 2003).
There is a lack of information about current services available to women with high to severe FOC. A national survey in Sweden in 2016 revealed that whilst it is usual for obstetric clinics in Sweden to provide treatment for women with childbirth fear, disparities in the treatment offered to women exist in the 43 obstetric clinics in Sweden that responded to the survey (of a possible 45). Moreover, the survey findings report variations in the education of midwives and time allocated to counselling women (Larsson 2016). Thus, the researchers called for standardisation of care and the potential for a national healthcare program for high to severe FOC (Larsson 2016). The results of the availability of services in Sweden were in contrast to the findings of a UK national survey on availability of services for women with FOC (in which 128 out of 202 maternity units responded) (Richens 2015). Specialist services for women with high to severe FOC were available in just over half of the UK maternity units surveyed (Richens 2015). It was reported that 52 maternity units did not offer any specialist support for women with FOC (Richens 2015). As in Sweden, the standards of available services varied, and a number of different healthcare professionals were named as leading the care (Richens 2015). Thus, a summary of the best available empirical evidence is needed to inform the best practice to support women with high or severe FOC.
A Cochrane Review of mind‐body interventions during pregnancy for preventing or treating women's anxiety investigated interventions such as autogenic training (a relaxation technique), biofeedback, hypnotherapy, imagery, meditation, prayer, auto‐suggestion, tai chi and yoga in comparison with standard care (Marc 2011). This review included eight trials with 556 participants in total; thus, no meta‐analysis (formal epidemiological study to systematically assess the results) was possible. The review concluded that mind‐body interventions, such as autogenic training, may reduce anxiety in pregnancy, and the use of imagery during labour and in the postnatal period may have benefits for women in labour and in the postnatal period (Marc 2011). Moreover, there were no harmful effects from any mind‐body interventions (Marc 2011). However, the evidence was limited because of the small number of studies included and their methodological limitations (such as lack of blinding — where study participants are prevented from knowing certain information that may somehow influence them — thereby tainting the results, and lack of detail in relation to the randomisation) (Marc 2011). There has been no Cochrane Review on interventions for high to severe FOC including tocophobia to date. There has been much debate about FOC, and an upsurge in research in the field, but little evidence as to which interventions are effective, limited understanding of the aetiology of tocophobia and variation in outcomes measured (Moghaddam Hosseini 2017; Smith 2019; Stoll 2018; Weaver 2013). To date, much of the research has focused on reducing caesarean section at maternal request, rather than on reducing fear and evaluating the overall outcome for the woman (physical, psychological and emotional). Therefore, supporting women with FOC to manage fear and have a positive transition to motherhood is an emerging area of concern for women, obstetricians and midwives.
Description of the intervention
Since the reasons for high to severe FOC are multifactorial and different for each individual, ideally, interventions should address the complex nature of the fear, taking into consideration the social, physical, psychological and emotional factors in women’s lives. There is a need to investigate: (a) the severity of FOC, and the effect on women’s day‐to‐day lives; (b) the aetiology, cause or nature of the fear (i.e. lack of self‐efficacy in the ability to birth, previous sexual abuse, previous negative birth experience, low social support, fear of the unknown); (c) concurrent symptoms (i.e. antenatal depression, any other complications of pregnancy); (d) parity and risk factors; (e) social factors (i.e. social networks available, partner support, access to treatment); and (f) values and world views in relation to the available treatment (i.e. culture, religion, beliefs, expectations of the treatment). Therefore, a range of different antenatal interventions will be considered in this review, such as group and individual cognitive behavioural therapy (CBT) in person and via the Internet, group psychoeducation by midwives, counselling for FOC by midwives, childbirth preparation classes, yoga, relaxation and mindfulness techniques.
How the intervention might work
Given that the potential risk factors for high to severe FOC are low social support, single marital status, low maternal age, and co‐morbid depression or anxiety (Räisänen 2014; Rouhe 2011; Stoll 2018), the importance of psychosocial factors is evident for women with FOC. Therefore, interventions usually target these psychosocial factors using a combination of various approaches. These interventions aim to promote not only a reduction in fear but also a positive birth experience, which could then help to prepare the mother for a positive transition to motherhood (Airo Toivanen 2018). It has been proposed that providing a sense of security and safety is particularly important for women with FOC throughout the antenatal period (Airo Toivanen 2018). Other approaches have focused on understanding the birth process and awareness of the body in general, in order to prepare women emotionally for childbirth (Airo Toivanen 2018).
There is an increasing focus on applying a salutogenic model of health to birth (meaning an approach that focuses on overall maternal health and well‐being rather than pathology) (Antonovsky 1987; Greer 2014). According to this theory, the main aim should be for mothers to make a smooth transition to parenthood with their physical, psychological and emotional health intact, and have a birth experience which they evaluate as positive. Whilst various interventions exist, how treatment works is still unclear. However, women have seen benefits from non‐pharmacological approaches, such as psychological interventions (CBT or psychoeducation) which focus on psychological factors, and informational interventions which focus on delivering education and preparing women for the birth and transition to motherhood (Nieminen 2015; Toohill 2014). CBT has demonstrated an improvement in symptoms of FOC in this population, as well as decreased caesarean section on request (Larsson 2018; Saisto 2001). CBT is well‐recognised as an effective treatment for a range of psychological disorders (Andersson 2014; Ghazaie 2016), but the causal mechanism of the treatment is largely unknown. A recent study investigating CBT for major depressive disorder and post‐traumatic stress disorder (PTSD) suggested that the CBT mechanism may work by enhancing the cognitive control region connectivity (the amygdala and fronto‐parietal region of the brain) (Shou 2017). The study suggests that strengthening these connections through CBT may lead to improved control of affective processes (mood or psychological state) particularly (Shou 2017). The findings of this study are an important development in understanding the mechanism of CBT, but may not be generalisable due to the limitations of the study (small sample size (n = 65) and a slight variation in the therapy used in the study). Therapeutic interventions may be appropriate for assisting women to understand the source of the fear and equip them with tools to manage it (e.g. conversation, music or art therapy).
There is limited evidence in relation to the use of pharmacological interventions in women with high to severe FOC. Pain catastrophising is a concept which denotes "an exaggerated negative mental set brought to bear during painful experiences" (Sullivan 2001). It has been suggested that women with high FOC are prone to catastrophise pain in labour and birth, leading to more intense perceived pain (Rondung 2016). Therefore, they may be more likely to utilise epidural analgesia during labour (Rondung 2016). In addition, previous research reported that women with high FOC had reduced tolerance of labour pain during labour and after birth (Saisto 2001 A). In a study by Adams and colleagues, women with high FOC were significantly more likely to request an epidural than women without FOC (Adams 2012). More recently, a study by Logtenberg and colleagues also found that women with high FOC were more likely to request pharmacological pain relief in labour, but the finding was not statistically significant (Logtenberg 2018).
Some interventions have included partners, while others have focused solely on the mother. The prevalence of high to severe FOC in partners is similar to the prevalence in pregnant women; for example, 13% in a Swedish study (n = 329) (Eriksson 2005). Thus, it is conceivable that partners should be included in interventions. A small study of 100 women in Sweden in 1997 reported that 22% of partners demanded a caesarean section (Sjogren 1997). This study also reported that partners of women who had previously experienced a complicated birth were significantly more likely to be fearful (Sjogren 1997). A qualitative study of 20 Swedish men with severe FOC highlighted the need for strategies to identify and support fathers as well as mothers (Eriksson 2007). Following on from this, a qualitative study of Swedish midwives' perceptions of FOC indicates that partners with FOC may give poor support to labouring women, and the researchers recommend that midwives should also ask partners about FOC (Salomonsson 2010). Thus, interventions which welcome both partners should be considered in comparison with those that focus solely on the woman.
Why it is important to do this review
Traditionally, research in the area of perinatal mental health focuses on depression, but anxiety is prevalent (Howard 2014). Therefore, more evidence is required to address this knowledge gap with regard to anxiety and fear in the perinatal period. Moreover, it is increasingly apparent that high to severe FOC may be a predictor for maternal psychological health and well‐being in the perinatal period. There is consistent evidence that high to severe FOC is strongly associated with impaired psychological well‐being during pregnancy (e.g. women are more likely to have antenatal depression (Rouhe 2011)), and it may be a predictor for their postnatal mental health (Howard 2014). Women with high to severe FOC may ruminate or worry; sometimes, what may start out as a little worry or anxiety in early pregnancy can become magnified and escalate to high or severe FOC as birth becomes more imminent. Severe FOC has been linked to physical complaints, such as sleep disturbances such as insomnia and nightmares, to stomach aches and headaches, which may result in increased visits to individuals' general practitioner, midwife or hospital. Effective treatment for high to severe FOC may have trans‐generational effects. If untreated, FOC may be passed on from mother to daughter, where a mother had a traumatic experience which may be experienced in the imagination by her daughter when she relives the birth as described to her (Hofberg 2003). Therefore, supporting mothers in the perinatal period may have long‐term benefits for their own health and that of their infant.
Objectives
To investigate the effectiveness of non‐pharmacological interventions for reducing fear of childbirth (FOC) compared with standard maternity care in pregnant women with high to severe FOC, including tocophobia.
Methods
Criteria for considering studies for this review
Types of studies
All published, unpublished and ongoing randomised controlled trials (RCTs) and cluster‐randomised controlled trials of non‐pharmacological interventions in which the primary or secondary aim is to treat fear of childbirth (FOC) were eligible for inclusion.
We excluded quasi‐randomised trials (e.g. those randomised by even versus odd medical record numbers) and cross‐over trials from the analysis. When studies were published in abstract form, we listed the study as 'awaiting classification' and contacted study authors to attempt to retrieve raw data or the full publication of the study as soon as it was available.
Types of participants
We included women with high or severe FOC in pregnancy, as defined in each individual trial.
Diagnosis
We included women who were identified as having FOC, according to each individual study, with levels of severity varying from high to severe. This included women with high or severe levels of fear, using the threshold cut‐off on each self‐report assessment tool as designated by each individual trial protocol (i.e. Wijma Delivery Expectancy Questionnaire version A (W‐DEQ A) (Wijma 1998), and women who received a diagnosis of tocophobia according to a clinical assessment, using a structured clinical interview by a psychologist or psychiatrist.
Setting
We included women from all settings (e.g. primary care setting, outpatients, home and hospital), who participated in the various clinical trials.
Co‐morbidities
We included women with a co‐morbid medical condition if the main focus of the study was high to severe FOC, rather than the co‐morbid condition (such as depression).
Exclusion criteria
None.
Types of interventions
We considered any non‐pharmacological antenatal intervention aimed at reducing high to severe levels of FOC in women. Non‐pharmacological approaches consisted of psychosocial and psychological interventions (e.g. behavioural and educational strategies), physical exercise interventions (e.g. mind‐body interventions including mindfulness, relaxation, yoga and Pilates) and therapeutic interventions (e.g. music and art therapy). Psychosocial interventions included diverse supportive interactions. Examples of psychological interventions include cognitive behavioural therapy (CBT) and psychotherapy. Psychosocial and psychological interventions may have been delivered in group or individual sessions, face‐to‐face, by telephone or via the Internet. The intervention may have been delivered by a trained professional (e.g. psychiatrist, psychologist, social worker, midwife or obstetrician) or by a trained lay person or a trained therapist (art or music therapist), and may, or may not, have included the partner in the intervention. Any type, frequency and duration of intervention were considered in both clinical and non‐clinical settings. Two review authors (MOC, SON) independently determined the type of interventions as either psychosocial, psychological or therapeutic. In case of disagreement, we consulted a third review author (AK) to reach an agreement. Sometimes interventions are used in combinations.
Comparison interventions
We included comparisons of intervention groups versus standard or usual maternity care groups, as defined by the trialists. Standard or usual care included health care as appropriate during the clinical trial.
Types of outcome measures
We examined a number of outcomes as relevant for the mother, infant and family in this review.
We used time points of measurements as reported in the trials and assessed the outcome measures at the end of treatment.
Primary outcomes
Fear of childbirth as measured by a validated tool such as the Wijma Delivery Expectancy Questionnaire version A (W‐DEQ A) (Wijma 1998), or a visual analogue scale (VAS) known as the Fear of Birth Scale (FOBS) (Rouhe 2011).
Secondary outcomes
Number of women having a caesarean section.
Anxiety (as measured on generally accepted scales (e.g. State Trait Anxiety Index (STAI) (Brunton 2015), Generalised Anxiety Disorder Scale (GAD‐2) (Nath 2018), Beck Anxiety Inventory (BAI) (Beck 1993), the anxiety subscale of the Hospital Anxiety and Depression Scale (HADS‐A) (Zigmond 1983), Pregnancy Specific Anxiety Scale (PSAS) (Roesch 2004), Pregnancy Related Anxiety Questionnaire (PRAQ, PRAQ‐R and PRAQ‐S) (Brunton 2015)).
Depression (as measured on generally accepted scales, e.g. Edinburgh Postnatal Depression Scale (EPDS) (Cox 1987).
Birth preferences (as reported by the woman using any self‐report scale).
Epidural analgesia during labour.
Search methods for identification of studies
Electronic searches
We searched Cochrane Pregnancy and Childbirth’s Trials Register by contacting their Information Specialist (3 July 2021).
The Register is a database containing over 27,000 reports of controlled trials in the field of pregnancy and childbirth. It represents over 30 years of searching. For full current search methods used to populate Pregnancy and Childbirth’s Trials Register including the detailed search strategies for CENTRAL, MEDLINE, Embase and CINAHL; the list of hand‐searched journals and conference proceedings, and the list of journals reviewed via the current awareness service, please follow this link.
Briefly, Cochrane Pregnancy and Childbirth’s Trials Register is maintained by their Information Specialist and contains trials identified from:
monthly searches of the Cochrane Central Register of Controlled Trials (CENTRAL);
weekly searches of MEDLINE (Ovid);
weekly searches of Embase (Ovid);
monthly searches of CINAHL (EBSCO);
hand‐searches of 30 journals and the proceedings of major conferences;
weekly current awareness alerts for a further 44 journals plus monthly BioMed Central email alerts.
Search results are screened by two people and the full text of all relevant trial reports identified through the searching activities described above is reviewed. Based on the intervention described, each trial report is assigned a number that corresponds to a specific Pregnancy and Childbirth review topic (or topics), and is then added to the Register. The Information Specialist searches the Register for each review using this topic number rather than keywords. This results in a more specific search set that has been fully accounted for in the relevant review sections (Included studies, Excluded studies, Studies awaiting classification or Ongoing studies).
In addition, we searched ClinicalTrials.gov and the World Health Organization (WHO) International Clinical Trials Registry Platform (ICTRP) for unpublished, planned and ongoing trial reports (3 July 2020) (see Appendix 1).
We did not apply any language or date restrictions.
Searching other resources
We handsearched the reference lists of all relevant studies identified. Where only abstracts of studies were available, we contacted authors for further details. We did not apply any language or publication date restrictions.
Data collection and analysis
The following methods section of this Cochrane Review is based on a standard template used by the Cochrane Pregnancy and Childbirth Group.
Selection of studies
Two review authors (MOC, SON) independently assessed for inclusion all the potential studies identified by the searches. We resolved any disagreements through discussion or, if required, we consulted a third review author (AK).
We created a study flow diagram to map out the number of records identified, included and excluded.
Data extraction and management
We used a standardised data extraction form for eligible studies. Two review authors (MOC, SON) independently extracted the data. This standardised data extraction form included the type of study, study setting, characteristics of participants, interventions, main outcome measures, trial dates, duration of study, results of main outcome measures, sources of trial funding and the trial authors' declarations of interest. We resolved discrepancies through discussion or, if required, we consulted a third review author (AK). One review author (MOC) entered the study data into Review Manager software (Review Manager 2014), and another (AK) checked the data for accuracy.
Assessment of risk of bias in included studies
Two review authors (MOC, SON) independently assessed risk of bias for each study using the criteria outlined in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011, hereafter referred to as the Cochrane Handbook). We resolved any disagreement through discussion or by involving a third assessor (AK).
(1) Random sequence generation (checking for possible selection bias)
We described for each included study the method used to generate the allocation sequence in sufficient detail to allow an assessment of whether it should produce comparable groups.
We assessed the method as:
low risk of bias (any truly random process, e.g. random number table; computer random number generator);
high risk of bias (any non‐random process, e.g. odd or even date of birth; hospital or clinic record number);
unclear risk of bias.
(2) Allocation concealment (checking for possible selection bias)
We described for each included study the method used to conceal allocation to interventions prior to assignment, and assessed whether intervention allocation could have been foreseen in advance of, or during recruitment, or changed after assignment.
We assessed the methods as:
low risk of bias (e.g. telephone or central randomisation; consecutively numbered sealed opaque envelopes);
high risk of bias (open random allocation; unsealed or non‐opaque envelopes; alternation; date of birth);
unclear risk of bias.
(3.1) Blinding of participants and personnel (checking for possible performance bias)
We described for each included study the methods used, if any, to blind study participants and personnel from knowledge of which intervention a participant received. We considered studies at low risk of bias if they were blinded, or if we judged that the lack of blinding would be unlikely to affect results. We assessed blinding separately for different outcomes or classes of outcomes.
We assessed the methods as:
low, high or unclear risk of bias for participants;
low, high or unclear risk of bias for personnel.
(3.2) Blinding of outcome assessment (checking for possible detection bias)
We described for each included study the methods used, if any, to blind outcome assessors from knowledge of which intervention a participant received. We assessed blinding separately for different outcomes or classes of outcomes.
We assessed methods used to blind outcome assessment as:
low, high or unclear risk of bias.
(4) Incomplete outcome data (checking for possible attrition bias due to the amount, nature and handling of incomplete outcome data)
We described for each included study, and for each outcome or class of outcomes, the completeness of data including attrition and exclusions from the analysis. We stated whether attrition and exclusions were reported and the numbers included in the analysis at each stage (compared with the total randomised participants), reasons for attrition or exclusion where reported, and whether missing data were balanced across groups or were related to outcomes. Where sufficient information was reported, or could be supplied by the trial authors, we aimed to re‐include missing data in the analyses which we undertook.
We assessed methods as:
low risk of bias (e.g. no missing outcome data; missing outcome data balanced across groups);
high risk of bias (e.g. numbers or reasons for missing data imbalanced across groups; ‘as treated’ analysis done with substantial departure of intervention received from that assigned at randomisation);
unclear risk of bias.
(5) Selective reporting (checking for reporting bias)
We described for each included study how we investigated the possibility of selective outcome reporting bias and what we found.
We assessed the methods as:
low risk of bias (where it is clear that all of the study’s pre‐specified outcomes and all expected outcomes of interest to the review have been reported);
high risk of bias (where not all the study’s pre‐specified outcomes have been reported; one or more reported primary outcomes were not pre‐specified; outcomes of interest are reported incompletely and so cannot be used; study fails to include results of a key outcome that would have been expected to have been reported);
unclear risk of bias.
(6) Other bias (checking for bias due to problems not covered by (1) to (5) above)
We described for each included study any important concerns we have about other possible sources of bias.
We assessed whether each study was free of other problems that could put it at risk of bias:
low risk of other bias;
high risk of other bias;
unclear whether there is risk of other bias.
(7) Overall risk of bias
We made explicit judgements about whether studies are at high risk of bias, according to the criteria given in the Cochrane Handbook (Higgins 2011). With reference to (1) to (6) above, we assessed the likely magnitude and direction of the bias and whether we considered it is likely to impact on the findings. We explored the impact of the level of bias through undertaking sensitivity analyses; see Sensitivity analysis.
Measures of treatment effect
Dichotomous data
For dichotomous data, we presented results as summary risk ratios (RR) with 95% confidence intervals (CI).
Continuous data
For continuous data, we used the mean difference if outcomes were measured in the same way between trials.
In future updates, we will used standardised mean difference (SMD) to combine trials that measure the same outcome, but using different methods. We will use these thresholds to interpret SMD:
SMD 0.8 or greater = large effect;
SMD greater than 0.49 and less than 0.8 = medium effect;
SMD greater than 0.19 and less than 0.5 = small effect;
SMD less than 0.2 = trivial or no effect.
Unit of analysis issues
Cluster‐randomised trials
We included cluster‐randomised trials in the analyses along with individually‐randomised trials. We adjusted their standard errors using the methods described in the Cochrane Handbook (Higgins 2021), using an estimate of the intracluster correlation co‐efficient (ICC) derived from other studies of a similar population. Where we used ICCs from other sources, we reported this and conducted sensitivity analyses to investigate the effect of variation in the ICC.
Where we identified both cluster‐randomised trials and individually‐randomised trials for the same outcome, we synthesised the data in the same meta‐analysis. We considered it reasonable to combine the results from both if there was little heterogeneity between the interventions, and the interaction between the effect of intervention and the choice of randomisation unit was considered to be unlikely.
Cross‐over trials
We did not include cross‐over trials.
Multi‐armed trials
We included a multi‐armed trial in the analysis. This trial included two intervention arms and a control arm. To include the data in the analysis without double‐counting participants, we split the denominator in the control arm by two in order to create two pairwise comparisons.
Dealing with missing data
For included studies, we noted levels of attrition.
For all outcomes, we carried out analyses, as far as possible, on an intention‐to‐treat basis; that is, we attempted to include all participants randomised to each group in the analyses, and all participants were analysed in the group to which they were allocated, regardless of whether or not they received the allocated intervention. The denominator for each outcome in each trial was the number randomised minus any participants whose outcomes were known to be missing. If the study did not report our primary outcome, we contacted the study authors to request this. If there was no reply after one contact and a reminder, we considered there were no data available.
Assessment of heterogeneity
We assessed statistical heterogeneity in each meta‐analysis firstly by visual inspection of a forest plot, and then by using Tau², I² and Chi² statistics. We regarded heterogeneity as substantial if I² was greater than 50% and either Tau² was greater than zero, or there was a low P value (less than 0.10) in the Chi² test for heterogeneity.
Assessment of reporting biases
If there were 10 or more studies in the meta‐analysis, we planned to investigate reporting biases (such as publication bias) using funnel plots. We planned to assess funnel plot asymmetry visually. If asymmetry was suggested by a visual assessment, we planned to perform exploratory analyses to investigate it.
Data synthesis
We carried out statistical analysis using Review Manager 5 (RevMan 5) software (Review Manager 2014). We used a random‐effects model for combining data because of variation in the interventions, meaning that it likely that the underlying treatment effects differ between trials.
Where we used random‐effects analyses, the results were presented as the average treatment effect with 95% confidence intervals, and I².
Subgroup analysis and investigation of heterogeneity
Where we identified substantial heterogeneity, we investigated it using subgroup analyses and sensitivity analyses.
We planned to carry out the following subgroup analyses.
Mode of Intervention: individual versus group.
Presence of co‐morbidity: depression (yes versus no).
Timing of the intervention during pregnancy: first versus second versus third trimester.
However, data were not available for timing of intervention during pregnancy and so the third subgroup analysis was not performed.
Subgroup analyses were restricted to the review's primary outcome (fear of childbirth).
We assessed subgroup differences by interaction tests available within RevMan 5 (Review Manager 2014). We report the results of subgroup analyses quoting the Chi2 statistic and P value, and the interaction test I2 value.
Sensitivity analysis
We performed sensitivity analyses according to the risk of bias in the included studies where possible. We explored the impact of risk of bias by investigating the change in the effect estimate when studies at high risk of bias (for allocation concealment and blinding of outcome assessors) were removed from the analyses.
To investigate the impact of missing data on our primary outcome, we carried out sensitivity analysis by removing from the analysis trials with high risk of incomplete outcome data.
We also conducted sensitivity analysis to examine the impact of different ICC estimates where we included data from cluster‐RCTs in the meta‐analysis.
Summary of findings and assessment of the certainty of the evidence
We assessed the certainty of the evidence using the GRADE approach, as outlined in the GRADE handbook, for the following outcomes in all comparisons.
Fear of childbirth (measured by a validated tool such as the Wijma Delivery Expectancy Questionnaire version A (W‐DEQ A)).
Caesarean section.
Anxiety (as measured on generally accepted scales (e.g. State Trait Anxiety Index (STAI)).
Depression (as measured on generally accepted scales, e.g. Edinburgh Postnatal Depression Scale).
Birth preference.
Epidural analgesia during labour.
We used the GRADEpro Guideline Development Tool to import data from Review Manager 5 (https://revman.cochrane.org/#/477318052509241879/dashboard/htmlView/1.31.8?revertEnabled=true#REF‐RevMan‐2014) in order to create summary of findings tables. A summary of the intervention effect and a measure of certainty for each of the above outcomes was produced using the GRADE approach. The GRADE approach uses five domains (risk of bias, consistency of effect, imprecision, indirectness and publication bias) to assess the quality of the body of evidence for each outcome. The evidence was downgraded from 'high certainty' by one level for serious (or by two levels for very serious) limitations, depending on the assessments for each GRADE domain.
Results
Description of studies
Results of the search
We assessed 115 trial reports. We included seven trials (31 reports) and excluded 47 trials (62 reports). There are 15 trials (16 reports) awaiting further classification and six trials are ongoing. See Figure 1.
1.
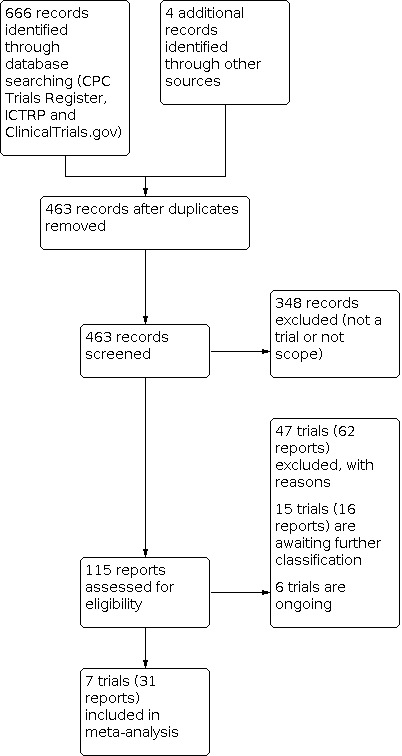
Study flow diagram
Included studies
We included seven randomised controlled trials (involving 1357 women) in this review (Boz 2020; Kordi 2017; Rahmani 2020; Rondung 2018; Rouhe 2015; Toohill 2014; Wahlbeck 2020).
All the included studies were published in English between 2012 and 2020 and were carried out in five different countries (Australia, Iran, Sweden, Finland and Turkey). Three of the studies were published in 2020 (Boz 2020; Rahmani 2020; Wahlbeck 2020).
These studies compared the effects of various non‐pharmacological interventions for childbirth‐related fear with usual maternity care. Interventions under evaluation were: psychoeducation (group or individual) (Kordi 2017; Rouhe 2015; Toohill 2014); Internet cognitive behavioural therapy (CBT); art therapy (Wahlbeck 2020); peer teaching (Rahmani 2020); and group discussion (Rahmani 2020). In the Wahlbeck study, the art therapy was an adjunct to midwifery counselling, which is the standard in Sweden (Wahlbeck 2020). Control groups consisted of: usual maternity care; antenatal education (Boz 2020); and midwifery counselling (Rouhe 2015; Wahlbeck 2020). The Rahmani study had two intervention arms ‐ peer teaching and group discussion (Rahmani 2020).
Interventions were performed during pregnancy (Boz 2020; Kordi 2017; Rahmani 2020; Rondung 2018; Rouhe 2015; Toohill 2014; Wahlbeck 2020). Two trials included one follow‐up session in the postnatal period (Rondung 2018; Rouhe 2015). The number of intervention sessions during pregnancy ranged from two (Toohill 2014) to 16 (Rahmani 2020). The CBT intervention included eight modules for which one to three homework items also needed to be completed and feedback given (Rondung 2018).
Funding and declarations of interest
All trials reported their sources of funding. One trial received no financial assistance (Boz 2020). Three trials were supported by local university research funding (Kordi 2017; Rahmani 2020; Rondung 2018). One received charitable funding (Rouhe 2015). One received funding from a pharmaceutical company with no commercial interest in the trial (Wahlbeck 2020). One received state funding (Toohill 2014).
All the trials reported declarations of interest. None of the author teams declared a conflict of interest in any of the trials. However, in the Wahlbeck trial, the first author is an art therapist; therefore, there may be a potential conflict of interest (Wahlbeck 2020).
Designs
Nine reports from seven randomised controlled trials were included. There was one single‐blinded RCT (Boz 2020), two multisite two‐armed open trials (Rondung 2018; Toohill 2014), two single‐site two‐armed open trials (Rouhe 2015; Wahlbeck 2020), one single‐site three‐armed open trial (Rahmani 2020), and one cluster‐RCT (Kordi 2017).
Sample sizes
Sample sizes varied: the smallest trial recruited 24 participants (Boz 2020), whilst the largest trial recruited 371 women (Rouhe 2015).
Setting
Studies were conducted in a variety of settings from Australia, Iran, Sweden, Finland and Turkey. Australia contributed one trial which was conducted in the antenatal clinics of three public hospitals in South East Queensland, Australia (Toohill 2014). Iran contributed two trials: one was performed in health centres of Mashhad (Kordi 2017); and a second took place in community health centres affiliated to Gonabad University of Medical Sciences (Rahmani 2020). Finland contributed one trial which was set in maternity clinics at the Department of Obstetrics & Gynaecology, University of Helsinki, Helsinki University Central Hospital (Rouhe 2015). Sweden contributed two trials: one in a clinic in southern Sweden (Wahlbeck 2020); the other took place in a university hospital and 2 referral hospitals (Rondung 2018). The Turkish trial took place in the antenatal clinic of a Turkish hospital (Boz 2020).
Participants
Participants were women with high to severe fear of childbirth, as defined in each individual study (n = 1357). Three trials included nulliparous women (Boz 2020; Kordi 2017; Rouhe 2015), and four trials included both nulliparous and parous women (Rahmani 2020; Rondung 2018; Toohill 2014; Wahlbeck 2020).
Interventions and comparisons
1. Psychoeducation
Four trials compared psychoeducation to a control group.
One trial compared psychoeducation based on human caring theory – consisting of relaxation, music, aromatherapy, massage, education about infant care, listening to each other, developing loving, trusting relationships, problem‐solving and creating a healing environment – to antenatal education, in which the focus was on the physiology of labour and was not based on a theory or model (Boz 2020).
One trial used the Birth Emotions and Looking to Improve Expectant Fear (BELIEF) intervention which helps women to develop individualised supports for the present and near future, affirming that negative events can be coped with by using simple problem‐solving skills. In addition, birth expectations are reviewed, distressing elements of childbirth are unpicked, strategies to develop support networks are employed, and a birth plan created (Toohill 2014).
One trial based the intervention on Rosenbaum's resourcefulness theory and utilised cognitive rehabilitation training and problem‐solving skills for pregnant women. In the first training session, stages of labour and pain relief methods were discussed by a midwife for 15 minutes. At the end of each session, coping skills for labour were taught by a clinical psychologist. This involved relaxation techniques (deep‐release, differential, and conditioned relaxation techniques, and childbirth‐related imagery) (Kordi 2017).
One trial compared psychoeducation with guided relaxation, with usual maternity care, which is midwifery counselling in Finland (Rouhe 2015). Partners were also included in one session in this study.
2. Internet cognitive behavioural therapy (CBT)
One trial compared Internet CBT to a control group (Rondung 2018). This intervention used a guided, Internet‐based, self‐help CBT program. The intervention aimed to help participants observe and understand their childbirth‐related fear and find new ways of coping with difficult thoughts and emotions. The control group received the standard care in Sweden, which consists of two to four counselling sessions either by antenatal midwives, counselling midwives and obstetricians, or a psychosocial unit consisting of midwives, obstetricians and psychologists. Trialists describe the aims of counselling as: understanding the origin of fear, reducing fear, preparing for childbirth, empowering women in their ability to give birth, and making the birth experience as positive as possible, regardless of birth mode.
3. Peer teaching
One trial compared peer teaching using training, which included the nature of delivery, labour pain and methods for reducing FOC, with a control group who received usual maternity care (Rahmani 2020). All peers completed training courses under the supervision of an expert. In the peer teaching group, training was held over four two‐hour sessions over four days for a period of four weeks.
4. Group discussion
The same trial compared group discussion in the other trial arm with a control group who received usual maternity care (Rahmani 2020). In the group discussion group, training sessions were conducted with the presence of a specialist for four two‐hour sessions over four days for a period of four weeks.
5. Art therapy and midwifery counselling
One trial (n = 103) compared art therapy and midwifery counselling with a control group who received usual maternity care, which is midwifery counselling in Sweden (Wahlbeck 2020). In addition, participants' partners were invited to one of the sessions. Participants in the intervention were invited to five sessions of art therapy. This intervention aimed to reduce FOC and motivate more women to give birth vaginally. When only one participant was recruited, sessions were individual. When more than one was recruited, participants could choose individual or group art therapy with a limitation of three participants per group. Midwifery counselling is guided by the individual needs of the woman. Each woman has a one‐to‐one meeting with a midwife from the specialist team to assess their needs. In the case of multiparous women, the case notes are used as a guide for the discussion where the woman is encouraged to talk about her experience of what is described in the notes. It is an opportunity to discuss and clarify uncertainties about events in the previous birth, where possible. A visit to the birth unit is offered if the woman is not familiar with the birthing environment. Usually, the woman and midwife draw up a plan for the approaching birth together. Continued sessions are based on the woman’s individual and personally expressed needs. An obstetrician may be asked to join the discussion when a woman expresses a wish for a planned induction or caesarean section, in accordance with Swedish national guidelines.
Outcomes
Primary outcome
All of the included studies reported the primary outcome, fear of childbirth, which was measured using various scales. The W‐DEQ A was the most commonly‐used measure of FOC.
Secondary outcomes
No study reported a measure of anxiety as an outcome. All of our other secondary outcomes were reported in at least one study.
Ongoing studies
We identified four ongoing studies (see Characteristics of ongoing studies), all of which are investigating different non‐pharmacological interventions: eye movement desensitization and reprocessing (Baas 2017); Beck cognitive counselling therapy (IRCT20120718010324N43); a novel cognitive behavioral protocol (NCT02972112); peer support (NCT03393637).
Excluded studies
We excluded 47 trials. We describe reasons for excluding trials in Figure 1 and Excluded studies. We excluded 36 studies as they did not include our population of interest (i.e. participants did not have high or severe fear of childbirth as defined in the trial). We excluded two studies because they were not randomised. We excluded nine studies because they were quasi‐experimental studies or cross‐over trials.
Risk of bias in included studies
We describe the risk of bias of included studies in the risk of bias tables attached to the characteristics of included studies tables. Our judgements about risk of bias are summarised in Figure 2 and Figure 3.
2.

Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies
3.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study
Allocation
Random sequence generation
We judged one trial to have unclear risk of bias for random sequence generation because it did not report sufficient information about the randomisation process (Rahmani 2020). We judged the other six studies to be low risk of bias because they described adequate methods of randomisation, such as computer‐generated random numbers.
Allocation concealment
We judged three studies as low risk of bias for allocation concealment because they described using adequate methods such as closed, sealed envelopes (Boz 2020; Rouhe 2015; Toohill 2014). We judged one study as high risk because it reported having assigned women to the intervention groups after having received their completed baseline questionnaires (Wahlbeck 2020). The remaining three studies did not report sufficient information about allocation concealment so we judged them as unclear risk of bias (Kordi 2017; Rahmani 2020; Rondung 2018).
Blinding
Blinding of participants and personnel
As is often the case in trials evaluating non‐pharmacological interventions, blinding of participants and the intervention provider was not possible in most of the trials. We judged six trials as high risk due to lack of blinding because knowledge of the intervention could have an effect on self‐reported outcomes (Boz 2020; Kordi 2017; Rondung 2018; Rouhe 2015; Toohill 2014; Wahlbeck 2020). We judged one trial as unclear risk for blinding of participants and personnel because the women were not told to which group they were allocated, but it is unclear if they could have guessed their allocation (Rahmani 2020).
Blinding of outcome assessment
We judged two trials as high risk of bias because there was no attempt to blind outcome assessors (Kordi 2017; Rondung 2018). There was insufficient information in the remaining trials for us to judge whether outcome assessors were blinded or not, so we rated them as unclear (Boz 2020; Rouhe 2015; Toohill 2014; Wahlbeck 2020).
Incomplete outcome data
We judged three studies which reported low or no attrition in the trial report as low risk of bias (Rahmani 2020; Rondung 2018; Toohill 2014). We judged one study as unclear risk because it did not provide enough information to ascertain whether women withdrew from the study for reasons related to the intervention and it did not report any intention‐to‐treat analysis (Kordi 2017). We judged three studies as high risk because they had high or differential attrition, or both (Boz 2020; Rouhe 2015; Wahlbeck 2020).
Selective reporting
We evaluated each individual trial for possible risk of selective reporting bias. Four trials appeared to have low risk of reporting bias with outcomes reported as per protocol (Kordi 2017; Rondung 2018; Toohill 2014; Wahlbeck 2020). Two studies were judged to be high risk for possible selective reporting bias since they had planned to report different outcomes to those actually reported (Rahmani 2020; Rouhe 2015). We judged one trial as unclear risk since we could not locate the trial protocol to determine if the planned outcomes were reported (Boz 2020).
Other potential sources of bias
We examined the included trials for other possible sources of bias. We assessed four studies as low risk of bias (Boz 2020; Rahmani 2020; Rouhe 2015; Toohill 2014). We assessed two studies as unclear risk of bias: one because it was conducted by a midwife who was an art therapist and it was unclear whether this could have affected the outcomes (Wahlbeck 2020); and the other because it used a tool to measure FOC that was not validated in the local language (Kordi 2017). We assessed one study as high risk of bias because of variation in the treatment received in the control group (Rondung 2018).
Effects of interventions
See: Table 1
Non‐pharmacological interventions versus usual care
Primary outcomes
Overall reduction in W‐DEQ A
Overall, participating in non‐pharmacological interventions may reduce levels of fear of childbirth as measured by W‐DEQ but the reduction may not be clinically meaningful (mean difference (MD) ‐7.08, 95% CI ‐12.19 to ‐1.97; I2 = 63%; 7 studies, 828 women; low‐certainty evidence; Analysis 1.1; Table 1). Heterogeneity was noted to be moderately high which might be explained by the differences in the control groups (some studies had midwifery counselling as usual care) or due to the small sample size. The test for subgroup differences also suggested that delivering interventions in a group setting or to individuals may be an effect modifier (P = 0.001, I2 = 85.5%), although the small number of studies in the subgroups means that we cannot be certain about the cause of the difference between subgroups.
1.1. Analysis.

Comparison 1: Comparison of non‐pharmacological interventions for fear of childbirth versus usual care, Outcome 1: Fear of childbirth: measured with WDEQ
Sensitivity analysis removing three trials at high risk of bias for allocation concealment or blinding of outcome assessors, or both, did not change the effect estimate substantially (MD ‐10.04, 95% CI ‐14.67 to ‐5.41) (Kordi 2017; Rondung 2018; Wahlbeck 2020). Sensitivity analysis removing three trials with high risk of incomplete outcome data changed the size of the effect estimate but this may not represent a clinically important difference (MD ‐5.99, 95% CI ‐11.92 to ‐0.06) (Boz 2020; Rouhe 2015; Wahlbeck 2020).
We also conducted sensitivity analysis to examine the impact of different ICC estimates to account for the cluster design in one of the studies (see Table 2). The effect estimate did not change substantially when different ICC estimates were used.
1. Sensitivity analysis exploring different ICC estimates for cluster trial .
| Outcome |
Overall effect estimate with ICC 0.024 Effective sample sizes for Kordi 2017: Intervention: 35 Control: 36 |
Overall effect estimate with ICC 0.03 Effective sample sizes for Kordi 2017: Intervention: 32 Control: 33 |
Overall effect estimate with ICC 0.05 Effective sample sizes for Kordi 2017: Intervention: 24 Control: 25 |
| Fear of childbirth measured with W‐DEQ | MD ‐7.08 (95% CI ‐12.19 to ‐1.97) | MD ‐7.07 (95% CI ‐12.21 to ‐1.94) | MD ‐7.05 (95% CI ‐12.25 to ‐1.85) |
| Caesarean section | RR 0.70 (95% CI 0.55 to 0.89) (Kordi 2017: adjusted data 12/35 and 17/36) |
RR 0.70 (95% CI 0.55 to 0.89) (Kordi 2017: adjusted data 11/32 and 15/33 |
RR 0.69 (95% CI 0.54 to 0.89) (Kordi 2017: adjusted data 8/24 and 12/25) |
W‐DEQ: Wijma Delivery Expectancy Questionnaire
Secondary outcomes
Anxiety
This outcome was not reported by included studies.
Depression (assessed with Edinburgh Postnatal Depression Scale (EPDS))
Two trials reported possible depression; both used psychoeducation interventions (Rouhe 2015; Toohill 2014). There may be little to no difference between psychoeducation interventions and usual care in depression scores measured with the Edinburgh Postnatal Depression Scale (MD 0.09, 95% CI ‐1.23 to 1.40; I2 = 44%; low‐certainty evidence; Analysis 1.3; Table 1).
1.3. Analysis.

Comparison 1: Comparison of non‐pharmacological interventions for fear of childbirth versus usual care, Outcome 3: Depression: measured with Edinburgh Postnatal Depression Scale
Number of women having a caesarean section
Five trials reported numbers of women who had a caesarean section (Boz 2020; Kordi 2017; Rouhe 2015; Toohill 2014; Wahlbeck 2020).
Non‐pharmacological interventions probably reduce the number of women having a caesarean section (RR 0.70, 95% CI 0.55 to 0.89; I2 = 0%; 5 studies, 557 women; moderate‐certainty evidence; Analysis 1.2; Table 1).
1.2. Analysis.

Comparison 1: Comparison of non‐pharmacological interventions for fear of childbirth versus usual care, Outcome 2: Number of women having caesarean section
Sensitivity analysis removing two trials at high risk of bias for allocation concealment or blinding of outcome assessors, or both, did not change the effect estimate substantially (RR 0.72, 95% CI 0.55 to 0.94) (Kordi 2017; Wahlbeck 2020).
We also conducted sensitivity analysis to examine the impact of different ICC estimates to account for the cluster design in one of the studies (see Table 2). The effect estimate did not change substantially when different ICC estimates were used.
Birth preferences
Two trials reported preference for caesarean section after intervention (Boz 2020; Toohill 2014). Both offered psychoeducation as an intervention. Non‐pharmacological interventions probably lead to fewer women preferring a caesarean section (RR 0.37; 95% CI 0.15 to 0.89; I2 = 42%; 2 studies, 276 women; moderate‐certainty evidence; Analysis 1.4; Table 1).
1.4. Analysis.

Comparison 1: Comparison of non‐pharmacological interventions for fear of childbirth versus usual care, Outcome 4: Prefer caesarean section after intervention
Epidural analgesia in labour
Two trials reported use of epidural analgesia in labour (Rouhe 2015; Toohill 2014). Non‐pharmacological interventions may increase epidural use compared with usual care, but the 95% CI includes the possibility of a slight reduction in epidural use (RR 1.21, 95% CI 0.98 to 1.48; I2 = 3%; low‐certainty evidence; Analysis 1.5; Table 1).
1.5. Analysis.

Comparison 1: Comparison of non‐pharmacological interventions for fear of childbirth versus usual care, Outcome 5: Epidural analgesia during labour
Discussion
Summary of main results
The primary objective of this review was to evaluate the effectiveness of non‐pharmacological interventions on fear of childbirth. To date, seven randomised controlled trials with 1357 participants are available for evaluation.
None of the included studies reported anxiety as an outcome.
Non‐pharmacological interventions may reduce levels of fear of childbirth as measured by the Wijma Delivery Expectancy Questionnaire A (W‐DEQ A), but the reduction may not be clinically meaningful (low‐certainty evidence; Table 1).
There may be little to no difference between non‐pharmacological interventions and usual care in depression scores measured with the Edinburgh Postnatal Depression scale (low‐certainty evidence; Table 1).
Non‐pharmacological interventions probably reduce the number of women having a caesarean section (moderate‐certainty evidence; Table 1).
It is uncertain if non‐pharmacological interventions have any effect on the number of women preferring a caesarean section (low‐certainty evidence; Table 1).
Non‐pharmacological interventions may increase epidural use compared with usual care but the 95% CI includes the possibility of a slight reduction in epidural use (low‐certainty evidence; Table 1).
Overall completeness and applicability of evidence
The studies available for inclusion in this review were few ‐ from Sweden, Finland, Iran, Turkey and Australia ‐ and the numbers of participants were small. Therefore, generalisability of the review findings is limited. In addition, we found two ongoing trials: one investigating the use of Eye Movement Desensitisation and Reprocessing (EMDR) (Baas 2017), and the other investigating a short CBT intervention (IRCT20120718010324N43). Therefore, this body of evidence will continue to grow.
This is a relatively new area of research in which interest has grown exponentially in recent years. Three of the seven included trials were published in 2020 (Boz 2020; Rahmani 2020; Wahlbeck 2020). This review was conducted based on the strength of the W‐DEQ A tool, which has been widely accepted as the optimal measure for fear of childbirth to date. Considering the heterogeneity of the concept of fear of childbirth (Jomeen 2021; O'Connell 2017), and recent evidence which suggests that the W‐DEQ A may be multi‐dimensional rather than uni‐dimensional and may not be widely understood by English speaking women (Martin 2021; Slade 2020), there is a need to further explore the concept of fear of childbirth and tocophobia, in order to address women's needs. There have been preliminary studies into a questionnaire which was developed in the UK in the English language (Fear of Childbirth Questionnaire (FCQ) to facilitate the valid, reliable and acceptable assessment of fear of childbirth, but further research to determine its reliability and validity are required (Slade 2021).
Moreover, definitions of fear of childbirth and tocophobia have been further investigated and challenged in terms of accuracy (Martin 2021; Slade 2020). Since the concept is poorly defined and measurements lacking, efforts to better define the concept and produce operational definitions would improve the completeness and applicability of the evidence. Furthermore, secondary outcomes were not reported for the most part in trials. It was surprising that anxiety measures in particular were not measured, considering the overlap with FOC. Measuring birth satisfaction would be important in terms of women's experience of birth.
The interventions were described well overall but none of the trials included in our review described adherence to the trial protocol, which is a limitation. Additionally, different control groups were used. In Sweden and Finland, midwifery counselling is the normal pathway of care; thus, it would be unethical not to provide this care to women identified as having fear of birth.
Quality of the evidence
Despite the contributions made by the authors of the seven trials and 828 participants included in this review, we found the evidence to be at high risk of bias due to lack of blinding of women, staff and outcome assessment (performance and detection bias), allocation concealment (selection bias), incomplete outcome data (attrition bias) and selective reporting (reporting bias), as well as other possible biases. Small sample size and high dropout rate were concerns in some of the trials, as these would reduce the detection of effects.
We downgraded the certainty of evidence for several reasons. We judged the risk of bias, as discussed above, to be serious enough to downgrade one level. Additionally, we downgraded for imprecision due to the small numbers of women participating in the studies. See Table 1.
Potential biases in the review process
All available randomised controlled trials investigating non‐pharmacological interventions for fear of childbirth and tocophobia in pregnant women were included in this review, with no language restrictions. We attempted to be as inclusive as possible by going to great lengths to contact authors of reports, requesting clarification of methodology or results.
We acknowledge that the review process has a potential for risk of bias. It is not an exact science and may be considered subjective. We attempted to minimise this risk of bias by: (1) having two review authors independently assess risk of bias and carry out data extraction; and (2) contacting study authors to clarify study methods.
Agreements and disagreements with other studies or reviews
Our findings with regard to reducing fear of childbirth scores are in agreement with three previous reviews that included non‐randomised studies as well as RCTs (Akgun 2020; Moghaddam Hosseini 2017; Stoll 2018). These reviews concluded that non‐pharmacological interventions may be beneficial for reducing fear of childbirth. However, the clinical relevance of this reduction should not be conflated with effectiveness of the intervention. The findings of this review with regard to reduction in caesarean section are in congruence with another reviews (Striebich 2018). In other reviews, authors highlighted the importance of social support in addition to education, quality improvement strategies and counselling (Aguila 2021; Smith 2019).
Authors' conclusions
Implications for practice.
Based on a small number of RCTs (with small sample sizes), the effects of non‐pharmacological interventions for women with high to severe fear of childbirth are uncertain. While the interventions appear to reduce W‐DEQ A scores, in clinical terms, this may not translate to a meaningful reduction in fear for women. Participating in interventions, however, may facilitate an informed discussion around the birth process and empower women to decide on mode of birth.
Non‐pharmacological interventions probably reduce the number of women having a caesarean section.
Despite an obvious overlap between anxiety and fear of childbirth, this was not investigated as an outcome by trials included in this review. Clinicians and future researchers should recognise the importance of measuring anxiety.
A small number of included RCTs examined depression following non‐pharmacological interventions. There may be little to no difference in depression scores.
Non‐pharmacological interventions for high to severe fear of childbirth may lead to more epidural use in women.
Focusing on how women experience giving birth rather than the mode of birth is important for women with high to severe fear of childbirth, since there is evidence that women who have a vaginal birth despite requesting a caesarean section may have a negative experience of birth.
Implications for research.
Fear of childbirth may be a predictor of poor psychological outcomes for women in the perinatal period. Women with fear of childbirth in pregnancy may consider specific interventions to reduce their level of fear. Further research is required in the field to determine a better construct of the concept of fear of childbirth and the underpinning aetiology before further research on interventions is warranted. RCTs with standardised protocols, validated measurements and adequately powered samples are required. Future research should investigate birth satisfaction as well as other measures of psychological well‐being such as anxiety and depression.
What's new
| Date | Event | Description |
|---|---|---|
| 12 July 2021 | Amended | Included Gene Dempsey in the acknowledgments |
History
Protocol first published: Issue 5, 2019 Review first published: Issue 7, 2021
Acknowledgements
We would like to acknowledge the assistance of the Pregnancy and Childbirth Group Editors and Information Specialist for their guidance with the development of this protocol. We are grateful to Narges Ghoreishi, epidemiologist at Bundesinsitut fur Risikobewertung, Berlin, Germany, for her help in translation as necessary. Thanks to Gillian Maher, Postdoctoral Researcher at the Irish Centre for Maternal and Child Health Research (INFANT), Cork University Maternity Hospital and University College Cork, Cork, Ireland, for support with RevMan 5 software. Thank you to Dr Ilkay Boz for providing information about their trial, which was included in this Cochrane Review.
This project was supported by the Health Research Board, Ireland, as part of a Cochrane Training Fellowship, and through funding from Science Foundation Ireland (SFI) and by the National Institute for Health Research, via Cochrane Infrastructure funding to Cochrane Pregnancy and Childbirth. The views and opinions expressed are those of the authors and do not necessarily reflect those of the Systematic Reviews programme, NIHR, NHS or the Department of Health.
As part of the pre‐publication editorial process, this review has been commented on by two peers (an editor and referee who is external to the editorial team), two members of Cochrane Pregnancy and Childbirth's international panel of consumers and the Group's Statistical Adviser. The authors are grateful to the following peer reviewers for their time and comments: Dr Kathryn EA Gutteridge, Alina Bishop, Helen Sassoon.
We thank Rebecca MD Smyth, Louise C Kenny and Gene Dempsey for their contributions to the protocol for this review (O'Connell 2019).
Appendices
Appendix 1. Search terms used for ClinicalTrials.gov and the WHO ICTRP
We planned to run each line separately.
Draft search terms for the WHO International Clinical Trials Registry Platform (ICTRP)
fear AND childbirth
tocophobia
tokophobia
parturiphobia
lockiophobia
fear AND labour
fear AND pregnancy
fear AND birth
pregnancy AND anxiety
childbirth AND anxiety
birth AND anxiety
Draft search terms for ClinicalTrials.gov
Advanced search
Interventional Studies | Tocophobia
Interventional Studies | Tokophobia
Interventional Studies | Fear of Childbirth
childbirth | Interventional Studies | Anxiety ('childbirth' also searches for delivery and birth)
pregnancy | Interventional Studies | Anxiety
childbirth | Interventional Studies | Fear
pregnancy | Interventional Studies | Fear
Data and analyses
Comparison 1. Comparison of non‐pharmacological interventions for fear of childbirth versus usual care.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1.1 Fear of childbirth: measured with WDEQ | 7 | 828 | Mean Difference (IV, Random, 95% CI) | ‐7.08 [‐12.19, ‐1.97] |
| 1.1.1 Individual | 3 | 429 | Mean Difference (IV, Random, 95% CI) | 0.26 [‐4.32, 4.84] |
| 1.1.2 Unclear if delivered to groups or individuals | 1 | 51 | Mean Difference (IV, Random, 95% CI) | ‐12.03 [‐21.14, ‐2.92] |
| 1.1.3 Group | 4 | 348 | Mean Difference (IV, Random, 95% CI) | ‐11.19 [‐15.77, ‐6.61] |
| 1.2 Number of women having caesarean section | 5 | 557 | Risk Ratio (M‐H, Random, 95% CI) | 0.70 [0.55, 0.89] |
| 1.3 Depression: measured with Edinburgh Postnatal Depression Scale | 2 | 399 | Mean Difference (IV, Random, 95% CI) | 0.09 [‐1.23, 1.40] |
| 1.4 Prefer caesarean section after intervention | 2 | 208 | Risk Ratio (M‐H, Random, 95% CI) | 0.38 [0.08, 1.85] |
| 1.5 Epidural analgesia during labour | 2 | 380 | Risk Ratio (M‐H, Random, 95% CI) | 1.21 [0.98, 1.48] |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Boz 2020.
| Study characteristics | ||
| Methods | Study was conducted as a single‐blinded, randomised controlled trial between July and October 2018. | |
| Participants |
Inclusion criteria: The sample of the study consisted of the nulliparous women admitted to the outpatient clinic in their second trimester. Inclusion criteria were: (a) age between 18 and 45 years old; (b) the 20th or later gestational weeks; (c) at least moderate level (≥ 66) FOC in terms of the Wijma Delivery Expectancy /Experience Questionnaire A; and (d) could speak and understand Turkish without any communication barrier. Exclusion criteria: Exclusion criteria were: (a) 1st and 3rd trimesters of pregnancy; (b) a high‐risk pregnancy; (c) contraindication at physical activity; (d) a communication barrier; and (e) multiparity. |
|
| Interventions |
Intervention (n = 28): psychoeducation group, based on Human Caring Theory "based on preserving, developing, and improving the individual’s mind‐body‐spirit harmony with a holistic approach" Control (n = 28): antenatal education |
|
| Outcomes | The primary outcome was the level of the FOC in prenatal period, and the secondary outcomes were the rate of preference for vaginal birth (VB) in prenatal period, the rate of vaginal birth, and the level of the FOC within 2 weeks following the birth in postnatal period. | |
| Notes | Supplementary table not included ‐ authors contacted for this table which included further details of the intervention according to the manuscript. Received appendix from authors. On 13/06/2021 Dr Boz commented in relation to the intervention, "As a practitioner of the psychoeducation program, I can say that the decrease in women's fear of childbirth and the change in their birth preferences are a natural result of such devotedly structured and applied nursing care. The philosophy of Human Caring Theory is adopted in this program. In this philosophy, individuals are considered as a whole consisting of mind body and spirit harmony. Ethical, deep transpersonal interaction process with women has been established. The program was supported by caring healing methods, also known as complementary therapies. We believe that the combination of the philosophy of Human Caring Theory, deeply interactions and some of the complementary therapies may have enabled this program to run effectively and provided a significant difference between the groups." Study funding sources: “There was no financial assistance for the study”. Study authors’ declarations of interest: The authors declare that they have no potential conflicts of interest with respect to the research, authorship, and/or publication of this article. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | “Simple randomization was performed by a independent statistician using the SAS (Statistical Analysis System Institute, Cary, North Caroline) program version 8.2.” |
| Allocation concealment (selection bias) | Low risk | “This was performed by using closed envelope method”. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Unable to blind participants in this type of study. Knowledge of the allocated intervention could have an impact on outcomes. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Attrition greater than 57% 12 in each group completed treatment out of 28 |
| Selective reporting (reporting bias) | Unclear risk | Cannot locate a protocol to determine whether any selective outcome reporting occurred. But outcomes reported in methods are presented in results. |
| Other bias | Low risk | No indication of other bias |
Kordi 2017.
| Study characteristics | ||
| Methods | Cluster randomised clinical trial | |
| Participants | This randomised clinical trial was conducted on 122 primigravid women referred to the healthcare centres of Mashhad, Iran, from 21 January 2016 to 19 February 2017. In this study, the cluster sampling method was performed, and centres No. 2 and 3 were chosen randomly as clusters among the 5 healthcare centres in Mashhad, Iran (1, 2, 3, 5, and Samen). Thereafter, 2 subsets of each centre (Vahdat and Shahid Hasheminezhad from centre No. 2, and Sahraee and Ahmadi from centre No. 3) were selected as the study units. The centres were randomly allocated to the control and intervention groups. To do so, the names of the 2 centres were written on 2 separate sheets and placed in a draw bag. The first paper was considered as the intervention group and the other one was the control group. Therefore, the Vahdat and Sahraee Centers were considered to be the intervention group and Shahid Hasheminezhad and Ahmadi centres the control group. Sampling was performed using the convenience sampling method in each centre. Inclusion criteria: the inclusion criteria were Iranian nationality, primigravidity, residence in Mashhad, reading and writing literacy, age between 18 and 35 years, singleton low‐risk pregnancy, gestational age of 14 to 28 weeks, no history of mental illnesses and FOC score of 66 or higher. Exclusion criteria: the exclusion criteria included congenital anomalies in the fetus as confirmed by ultrasonography, abortion, stillbirth and absence from the educational sessions. |
|
| Interventions |
Intervention (n = 60): women in the intervention group were divided into 7 groups of 10 members and received the psychoeducational program for 3 weeks (one 90‐minute session per week) by a clinical psychologist. The overall approach was based on Rosenbaum's resourcefulness theory, and the interventions based on cognitive rehabilitation training and problem‐solving skills for pregnant women. In the first training session, a midwife described the labour stages and pain relief methods for 15 minutes. At the end of each session, a clinical psychologist explained the relaxation techniques (i.e. deep‐release, differential, and conditioned relaxation techniques, as well as childbirth‐related imagery) as a coping skill to deal with labour. Control/Comparison intervention (n = 62): routine prenatal care. |
|
| Outcomes |
Primary outcome: FOC post intervention (6 weeks postpartum) measured using W‐DEQ A tool. Secondary outcome: rates of CS |
|
| Notes | WDEQ‐A validated in Farsi in 2017 Ethics: This study was a part of a research project approved by the Ethics Committee of Islamic Azad University, Quchan Branch, Quchan, Iran (No. 12965) Trial registration: Iranian Registry of Clinical Trials (No. 2017071135008N1 IRCT) Sources of trial funding: funded by Deputy of Research, Islamic Azad University, Quchan Branch, Quchan, Iran. Trial author declaration of interest: The authors declare that there are no conflicts of interest regarding the publication of the article. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | In this study, the cluster sampling method was performed, and centres No. 2 and 3 were chosen randomly as clusters among 5 healthcare centres in Mashhad, Iran (1, 2, 3, 5, and Samen). Thereafter, 2 subsets of each centre (Vahdat and Shahid Hasheminezhad from centre No. 2, and Sahraee and Ahmadi from centre No. 3) were selected as the study units. The centres were randomly allocated to the control and intervention groups. To do so, the names of the 2 centres were written on 2 separate sheets and placed in a draw bag. The first paper was considered as the intervention group and the other one was the control group. Therefore, the Vahdat and Sahraee Centres were considered to be the intervention group and Shahid Hasheminezhad and Ahmadi centres the control group. Sampling was performed using the convenience sampling method in each centre. |
| Allocation concealment (selection bias) | Unclear risk | Randomly allocated centres (clusters) for intervention and control by drawing names from hat but there is no mention of allocation concealment techniques. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Unable to blind participants in this type of study. Knowledge of the allocated intervention could have an impact on outcomes. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Not blinded. The first author was the researcher and delivered the intervention. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 60/70 in the intervention group are not included in the analysis because they did not attend training classes or had stillbirth or abortion. 62/70 in the control group are not included in the analysis because of "abortion or displacement". It is not clear how many women were not included in the analysis because of reasons related to the intervention. The trial does not report any intention‐to‐treat analysis. |
| Selective reporting (reporting bias) | Low risk | FOC outcome reported. |
| Other bias | Unclear risk | FOC tool not validated in Persian. |
Rahmani 2020.
| Study characteristics | ||
| Methods | This randomised controlled clinical trial included all pregnant women with an electronic health record in community health centres affiliated to Gonabad University of Medical Sciences, Iran, during 2017/2018. | |
| Participants |
Setting: All pregnant women with an electronic health record in community health centres affiliated to Gonabad University of Medical Sciences during 2017/2018. Inclusion criteria: "The inclusion criteria were being in the age range of 18 to 35 years old and gestational age of 24 to 34 weeks, having a low‐risk pregnancy, obtaining a score of less than 85 for FOC before entering the study, not having a history of dystocia, postpartum bleeding and fetal abnormalities, showing willingness to participate in the study, having Persian reading and writing skills, lacking any physical and mental illness, and not having indicators for caesarean section in accordance with the Mothers’ Electronic‐Health Record." Exclusion criteria: "The exclusion criteria were absence from or irregular presence in the sessions, the incidence of any complications of pregnancy (e.g. pre‐eclampsia, bleeding, diabetes, intrauterine death, and preterm delivery), history of physical injury caused by accidents, beatings, violence, along with falling from a height in person or in his family." |
|
| Interventions |
Intervention 1 (n = 36) Peer teaching group: "the training lasted for four 2‐hour sessions for 4 days for a period of 4 weeks, and in the peer group meeting with the attendance of an eligible trainee counterpart" Intervention 2 (n = 36)Group discussion group: "the training sessions were conducted with the presence of a specialist for four 2‐hour sessions for 4 days for a period of 4 weeks." Control/Comparison intervention (n = 36): control group. Did not receive intervention but not stated what control group received (i.e. what standard care was). The trial protocol states “the control group received only routine training for pregnant mothers.” |
|
| Outcomes | Primary outcome: Mean (SD) fear at baseline and 4 weeks after the intervention using the Widget’s questionnaire. | |
| Notes | Iranian study reported using poor English. In the protocol, authors state “Reduce fear of normal delivery; reduce labor pain; increase normal delivery” Study authors contacted April 2021 to ask for clarification regarding inclusion criteria. Awaiting reply. Ethical approval: The study was approved by the Ethics Committee of Gonabad University of Medical Sciences under the number IR.KAUMS.REC.1397.007 Trial registration: Registered in the Iranian Registry of Clinical Trials (identifier: IRCT20180320039132N1; https://irct.ir/trial/30331). Sources of trial funding: This study was supported by the Social Development and Health Promotion Research Center, Gonabad University of Medical Sciences, Gonabad, Iran. Trial author declaration of interest: The authors declare that there are no conflicts of interest regarding the publication of this article. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Two‐stage sampling was used in this study. First, a convenient sampling method was performed to determine the research population. Then, participants were randomly assigned to 3 groups using a quadruple blocking method. |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | "Research blindness was done by placing pregnant mothers in peer education, discussion, and control groups based on the list of blocking with the researcher’s assistance." The trial protocol states that ‘the mothers were not informed about which group they were assigned to.’ The trial protocol states that it was ‘single blinded’. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Only states that analysis was conducted using SPSS (in the abstract only). No mention of blinding outcome assessors. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 36/36 in both interventions groups included in analysis. 5/36 lost to follow‐up in the control group |
| Selective reporting (reporting bias) | High risk | Trialists only report mean fear of childbirth 4 weeks after intervention in the paper, but in the trial protocol they list “Reduce fear of normal delivery; reduce labor pain; increase normal delivery” as the key outcomes. |
| Other bias | Low risk | Nothing to suggest any other source of bias. |
Rondung 2018.
| Study characteristics | ||
| Methods | Non‐blinded, multicentre randomised controlled trial (U‐CARE) | |
| Participants |
Inclusion criteria: Pregnant women reporting clinically significant levels of fear of birth and who gave consent to take part in the study. The inclusion criteria were an ongoing pregnancy in gestational weeks 17‐20, an ultrasound screening examination with no reported adverse findings, Fear of Birth Scale (FOBS) ≥ 60, proficiency in Swedish language, and personal access to a mobile phone and computer with Internet connection. Exclusion criteria: Women who had an abnormal ultrasound report, FOBS < 59, not proficient in Swedish, no personal access to a phone or computer with the Internet. |
|
| Interventions |
Experimental intervention (n = 127): guided Internet‐based self‐help program based on cognitive behavioral therapy (guided ICBT) Control/Comparison intervention (n = 131): standard care (which in Sweden is counselling by midwives) |
|
| Outcomes | Primary outcome: levels of fear of birth (FOB), measured in late pregnancy using FOBS | |
| Notes |
Ethical approval: Registered at ClinicalTrials.gov (NCT02306434) and approved by the Regional Ethical Review Board in Uppsala (No. 2013/209). Trial Registration: ClinicalTrials.gov NCT02306434; https://clinicaltrials.gov/ct2/show/NCT02306434 (Archived by WebCite at http://www.webcitation.org/70sj83qat) Sources of trial funding: Uppsala University and Uppsala University Hospital Trial author declaration of interest: The authors declare that there are no conflicts of interest regarding the publication of this article. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Participants were randomised by the U‐CARE portal (1:1) to either the guided ICBT or the standard care group." |
| Allocation concealment (selection bias) | Unclear risk | Not reported. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Unable to blind participants in this type of study. Knowledge of the allocated intervention could have an impact on outcomes. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | "Non‐blinded study". |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | "Participants lost to follow‐up were more likely to belong to the guided ICBT group (P < 0.001)." However, this would not affect differences between groups. |
| Selective reporting (reporting bias) | Low risk | The primary outcome FOB was reported at 4 time points in the pregnancy: at screening, pre‐intervention, post‐intervention, and follow‐up. |
| Other bias | High risk | Variation in standard care (SC) across the 3 study centres. “All hospitals in Sweden provide SC for pregnant women with FOB. Although guidelines exist, the content of SC and the time set aside for it differ between hospitals. Women with FOB usually receive 2‐4 counselling sessions either by antenatal midwives, counselling midwives and obstetricians, or a psychosocial unit consisting of midwives, obstetricians, and psychologists. The counselling aims at understanding the origin of fear, reducing the fear, preparing for childbirth, empowering women in their ability to give birth, and making the birth experience as positive as possible, regardless of the mode of birth [24]. Since SC is organized differently across the country, this also applies to SC at the study centres in this study. Depending on which study centre a participant belonged to, SC started either in the next meeting with the antenatal midwife or after referral to a counselling midwife or a psychosocial unit”. |
Rouhe 2015.
| Study characteristics | ||
| Methods | A randomised controlled trial. | |
| Participants |
Setting: Gynaecology and Obstetrics, Otology, Ophthalmology, Neurology and Neurosurgery of Helsinki University Central Hospital. Routine ultrasonography screening at the gestational age of 11–13 weeks. Inclusion criteria: those who scored > 100 W‐DEQ A were included. Exclusion criteria: twin pregnancies (included in protocol, not mentioned in paper). |
|
| Interventions |
Intervention (n = 131): Women in the intervention group were contacted by mail and offered group psychoeducation in connection with fear of childbirth. After screening and randomisation (Time 0), the women and their partners in both groups separately received 3 questionnaires. The intervention method used to treat women with severe fear of childbirth was group psychoeducation with relaxation exercises. "Six group sessions were held during pregnancy (starting at mean the 28th week of pregnancy) and one session 6–8 weeks after delivery. Sessions were led by a psychologist with specialised skills in group therapy and pregnancy issues. Each group consisted of a maximum of 6 nulliparous women. The sessions (2 hours) had a fixed structure: a focused topic and a 30‐minute relaxation with mindfulness guided exercise, using a compact audio disk developed for this purpose. Every session began with the therapist setting the agenda for the coming session and the sharing of feelings and thoughts that came up after the previous session. Then there was a guided discussion on the topic of the session and the session ended with the relaxation exercise. The guided relaxation exercise took participants through all stages of delivery in a relaxed state of mind with positive, calming and supportive suggestions or alternatively, a breathing exercise. The development of the group intervention was based on experience with therapeutic group work, attachment theory, social cognitive theories and individual coping strategies. The aim of the intervention was to enhance preparedness for childbirth among nulliparous women with severe fear of childbirth. The focus of the intervention was to share the difficult emotions and fears concerning the delivery and increase the feelings of safety and trust within the participants. Another aim was to strengthen the participants’ confidence in themselves regarding childbirth and motherhood, and also to increase their knowledge of the stages of delivery." Comparator (n = 240): "those randomised to the control group received a letter in which they were advised, if necessary, to discuss their fear of childbirth in their maternity unit in primary health care." |
|
| Outcomes | Primary outcome: Psycho‐emotional and psychosocial evaluations (Edinburgh Postnatal Depression Scale (EPDS), social support, Maternal Adjustment and Attitudes (MAMA), Traumatic Events Scale (TES) and the Wijma Delivery Experience Questionnaire (W‐DEQ B)) were completed twice during pregnancy (once at mid‐pregnancy and again at late pregnancy) and then at 3 months after giving birth. | |
| Notes |
Sources of trial funding: funded with grants from the Emil Aaltonen Foundation and the Signe and Ane Gyllenberg Foundation. Trial dates: Between October 2007 and August 2009 Ethical approval: This study was approved by the Ethics Committee for Gynaecology and Obstetrics, Otology, Ophthalmology, Neurology and Neurosurgery of Helsinki University Central Hospital (376/E9/05 from 27 October 2005) and informed consent was collected from everyone who filled in any of the questionnaires. Study prospectively registered? Clinical Research Register at Helsinki University Central Hospital Number: 228/2006 and ClinicalTrials.gov ID: NTC01548131. Trial author declaration of interest: The authors report no conflicts of interest. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Women were randomised in a proportion of 1:2 in balanced blocks of 18 via sealed opaque envelopes to the intervention group and to the control group |
| Allocation concealment (selection bias) | Low risk | "sealed opaque envelopes" |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Blinding not possible in this kind of study. Knowledge of the allocated intervention could have an impact on outcomes. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not reported. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | W‐DEQ scores only reported for 70/131 and 124/240 women who were randomised. |
| Selective reporting (reporting bias) | High risk | The results are presented in the following order: maternal adjustment, childbirth experience, depressive symptoms and traumatic symptoms. However, the protocol planned to present outcomes at 3 months and 2 years but only 3 months reported. |
| Other bias | Low risk | Nothing to suggest any other source of bias. |
Toohill 2014.
| Study characteristics | ||
| Methods | A multisite randomised controlled trial using a 2‐arm non‐blinded parallel trial design. | |
| Participants |
Setting: “Women in their second trimester attending antenatal clinics of 3 hospitals in South East Queensland, Australia (3 public hospitals)” Inclusion criteria: Women scoring high for childbirth fear (W‐DEQ A ≥ 66). “Women in their second trimester attending antenatal clinics of 3 hospitals in South East Queensland, Australia able to communicate sufficiently in English, and aged 16 years or older were recruited by research assistants”. Exclusion criteria: “Women requiring an interpreter, younger than 16 years, or more than 24 weeks pregnant, and anticipating or experiencing a perinatal death (e.g. congenital abnormality incompatible) or stillbirth were excluded”. |
|
| Interventions |
Intervention (n = 170): BELIEF is a telephone psychoeducation counselling intervention offered by midwives. The intervention aims to review women’s current expectations and feelings around fear of childbirth, support the expression of feelings, and provide a framework for women to identify and work through distressing elements of childbirth. The intervention was adapted from a midwifery counselling framework for distressed postpartum women developed by Gamble and Creedy. The BELIEF intervention aimed to help women develop individual situational supports for the present and near future affirming that negative things can be managed with a simple plan developed to achieve this. All participants received a copy of a decision‐aid booklet entitled 'Having a baby in Queensland'. The telephone counselling intervention was offered at 24 and 34 weeks of pregnancy. Comparator (n = 169): "Women in the control group will receive standard care. All women will be given the evidence‐based consumer resource “Choosing how to birth your baby” developed by the Queensland Centre for Mothers and Babies." Comparator group received the same written information as the intervention group. |
|
| Outcomes |
Primary outcome: childbirth fear (W‐DEQ A). Secondary outcomes: conducted using independent samples t‐test. Change scores for fear (W‐DEQ A), decisional conflict scale (DCS), and depression (Edinburgh Postnatal Depression Scale ‐ EPDS) were calculated for both groups comparing post treatment scores for the intervention and control groups with the baseline score as the covariate. |
|
| Notes | Author (Jenny Gamble) contacted for W‐DEQ A mean and SD post intervention. Replied 7 November 2020 Ethics: Human research ethics approval was obtained from Griffith University and Queensland Health multisite hospital Human Research Ethics Committee for the 3 participating hospitals. Human research ethics committee approval number HREC/11/QGC/162 (Queensland Health); NRS/45/11/HREC (Griffith University). Trial registration: Australian New Zealand Controlled Trials Registry ACTRN12612000526875, 17 May 2012. Trial dates: Recruitment between May 2012 and June 2013. Sources of trial funding: National Health and Medical Research Grant (Australia) APP9011023. Trial author declaration of interest: None declared. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | “A research assistant not involved in recruitment or provision of the intervention accessed the randomisation service following receipt of participant’s written consent and completed baseline measures. Participants were allocated in blocks of ten and stratified by hospital site and parity using a centralised web‐based service to either intervention or control group.” |
| Allocation concealment (selection bias) | Low risk | “A research assistant not involved in recruitment or provision of the intervention accessed the randomisation service following receipt of participant’s written consent and completed baseline measures. Participants were allocated in blocks of ten and stratified by hospital site and parity using a centralised web‐based service to either intervention or control group.” |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible to blind participants in this kind of trial. Knowledge of the allocation intervention could have an impact on outcomes. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not specifically mentioned that outcome assessors were blinded to the outcomes. They enlisted the help of a statistician and the study authors interpreted findings. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | High attrition rate (41%). No significant differences were reported between women returning all data (n = 198) and women lost to follow‐up (n = 141) for age, country of birth, parity, previous mode of birth, marital status, DCS, EPDS, Childbirth Self‐Efficacy Inventory, and W‐DEQ A scores. However, statistically significant differences in education and household income. This would not be likely to affect differences between groups. |
| Selective reporting (reporting bias) | Low risk | All outcomes reported. |
| Other bias | Low risk | Nothing to indicate any other source of bias. |
Wahlbeck 2020.
| Study characteristics | ||
| Methods | An open, randomised, controlled trial with 2 arms to compare treatment alternatives for severe FOC. | |
| Participants |
Setting: Participants were recruited between March 2011 and March 2017 from 10 antenatal clinics in southern Sweden. At these clinics, all women who register their pregnancy are asked to indicate, on a visual analogue scale, the extent of their fear of the approaching birth. Scores above 7 are considered high enough to require treatment and these women are referred to a specialist group at the obstetric unit at the regional hospital. When contact was made with the specialist group, these women were invited to join the study. Inclusion criteria: Scores above 7 are considered high enough to require treatment and these women are referred to a specialist group at the obstetric unit at the regional hospital. When contact was made with the specialist group, these women were invited to join the study. Statistics from the unit (unpublished) show that 4.3% of pregnant women were referred to the specialist group because of severe FOC during the data collection period. Exclusion criteria: Pregnant women who did not understand or speak Swedish, had physical hindrance for a vaginal birth or were diagnosed with obstetrical complications, a current depression requiring medical intervention, acute psychosis or current substance abuse were excluded from the study. Women who registered later than the 35th gestational week were also excluded since there was a risk that the treatment could not be finished before the birth. |
|
| Interventions |
Experimental intervention (n = 55): midwife‐led counselling plus art therapy (AT). Women in the intervention group invited to 5 AT sessions. The aims were to reduce FOC and motivate more women to give vaginal birth. When only 1 participant was recruited, AT was provided individually. When more than 1 was recruited, participants could choose individual or group AT. A group was limited to 3 participants. 27 women were treated individually and 12 in the group. The sessions were given between 28 and 36 gestational weeks and held in a locality outside of the hospital surroundings. Painting was offered as a tool for self‐reflection to release feelings they were unable to express elsewhere, to strengthen the process of bonding with their baby, and to initiate the counselling component of AT. The sessions were given once per week and lasted between 90 and 120 minutes. The art therapist was a midwife and first author in this study. Comparator (n = 48): midwife‐led counselling only |
|
| Outcomes |
Outcomes: Pregnant women whose FOC decreased from severe (≥ 100 W‐DEQ points) to any level below this (≤ 99 W‐DEQ points) after treatment in Study Group (SG) or Control Group (CG). Secondary outcomes: (1) comparison of changes in the mean W‐DEQ between measurements at recruitment and at the end of treatment for SG and CG; (2) comparison of number of Midwifery Counselling (MC) sessions required by SG and CG; (3) comparison of type of birth; normal vaginal birth versus all other types of birth between SG and CG; and (4) number of women with higher levels of FOC after treatment. |
|
| Notes |
Sources of trial funding: This research received a grant of 2,500 US dollars from Procter and Gamble. The company had no commercial interest in the use of AT. Trial author declaration of interest: Nothing reported. First author was a midwife and conducted the art therapy sessions. Author (Kajsa Landgren) contacted for WDEQ A mean and SD on 13/11/20202 and data provided 16/11/2020 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | When the questionnaires were completed, randomisation was carried out via a computer‐generated randomisation chart and the individual was informed whether she had been randomised to the control group (CG) or the study group (SG). Randomisation was preceded by stratification. |
| Allocation concealment (selection bias) | High risk | When the questionnaires were completed, randomisation was carried out via a computer‐generated randomisation chart. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Open unblinded trial. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Outcomes were analysed with the on‐treatment technique using SPSS version 25. No mention of blinding of outcome assessors. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 39/55 and 43/48 included in the analysis. Differential attrition and no indication that any statistical adjustment was made to account for missing data. |
| Selective reporting (reporting bias) | Low risk | All reported as specified in the paper and protocol. |
| Other bias | Unclear risk | Lead author was a midwife and delivered the art therapy sessions (intervention) ‐ unclear if author's involvement could have had any effect on outcomes. |
CS: caesarean section; FOB: fear of birth; FOBS: Fear of Birth Scale; FOC: fear of childbirth; SG: Study Group; CG: Control Group;MC: Midwifery Counselling
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Abdollahi 2020 | Not our population of interest. Participants’ mean W‐DEQ A score prior to intervention was 56; therefore, ineligible for our review |
| Ahmadi 2017 | Population of interest did not have high or severe FOC. After discussion, ruled out since 28 was considered high fear on the Childbirth Attitudes Questionnaire (CAQ). The CAQ has a range from 14 to 56. |
| Andaroon 2017 | Not our population of interest. Women scored 34 to 84 on W‐DEQ A. |
| Bergstrom 2009 | Not our population of interest. Participants did not have fear of childbirth. |
| Bittner 2014 | Not our population of interest. Participants had anxiety, stress and depression. Fear of childbirth was not assessed. |
| Boryri 2019 | Quasi‐randomised design |
| Cankaya 2020 | Not our population of interest. Participants did not have fear of childbirth. |
| ChiCTR1900025309 | Quasi‐experimental design |
| CTRI/2019/11/021950 | Quasi‐experimental design |
| Downe 2015 | Not our population of interest. Participants did not have fear of childbirth. |
| Duncan 2017 | Not our population of interest. Participants did not have fear of childbirth. |
| Ghazaie 2016 | Not our population of interest. Participants did not have fear of childbirth. |
| Gonenc 2020 | Not our population of interest. Participants did not have fear of childbirth. |
| Haapio 2017 | Not our population of interest. Participants did not have fear of childbirth. |
| IRCT20110228005931N5 | Not our population of interest. Participants did not have fear of childbirth. |
| IRCT20120215009014N317 | Not our population of interest. Participants did not have fear of childbirth. |
| IRCT201312073034N13 | Not our population of interest. Participants did not have fear of childbirth. |
| IRCT20150608022609N6 | Not our population of interest. Participants were fathers. |
| IRCT2015120625399N1 | Not our population of interest. Participants did not have fear of childbirth. Results not published, only registration. CAQ > 28 for inclusion in study. |
| IRCT2016060828352N1 | Quasi‐experimental design |
| IRCT20160625028630N2 | Quasi‐experimental design |
| IRCT2016082429506N1 | Ineligible population: inclusion criteria do not specifiy FOC. |
| IRCT2017030627557N3 | Not our population of interest. Participants did not have high or severe fear of childbirth. Inclusion: W‐DEQ A < 66 |
| IRCT20171026037015N3 | Participants with moderate FOC: W‐DEQ A > 55 |
| IRCT20171129037676N2 | Not our population of interest. Participants did not have fear of childbirth. |
| IRCT20171230038133N1 | Quasi‐randomised design |
| IRCT20180131038579N1 | Not our population of interest. Participants did not have fear of childbirth. Ruled out since 28 was considered high fear on the CAQ. The CAQ has a range from 14 to 56. |
| IRCT20180427039436N3 | Non‐randomised trial according to protocol registration. |
| IRCT20180520039729N1 | Not our population of interest. Participants did not have fear of childbirth. |
| IRCT20180721040544N1 | Not our population of interest. Participants did not have fear of childbirth. Ruled out since 28 was considered high fear on the CAQ. The CAQ has a range from 14 to 56. |
| IRCT20190210042672N1 | Non‐randomised trial according to protocol registration |
| IRCT20200122046227N1 | Not our population of interest. Participants did not have fear of childbirth. Inclusion: W‐DEQ A > 38 |
| Irmak 2019 | Not our population of interest. Participants did not have fear of childbirth. |
| Jamali 2018 | Not our population of interest. Participants did not have fear of childbirth. Participants were women "referred for delivery preparation", not women with fear of childbirth. |
| Klabbers 2019 | After data extraction, we realised that it was a cross‐over trial. After discussion between review authors, we excluded it. |
| Lonnberg 2020 | Ineligible population |
| Masoumi 2016 | Not our population of interest. Participants did not have fear of childbirth. |
| Mehrabadi 2020 | Not our population of interest. Participants did not have fear of childbirth. |
| Navaee 2015 | Not our population of interest. Participants did not have fear of childbirth. |
| Nosratabadi 2018 | Not our population of interest. Participants did not have fear of childbirth. |
| NTR4661 | Quasi‐experimental design |
| Sharifzadeh 2018 | Upon translation of this publication, we realised the women had low FOC, and were thus ineligible. |
| Soltani 2017 | Ineligible population: defines FOC as 28 on CAQ, we did not consider this to be high fear as per our protocol. |
| TCTR20190501001 2019 | Not population of interest |
| Vakilian 2018 | Not our population of interest. |
| Veringa 2016 | Quasi‐experimental design |
| Werner 2013 | Not our population of interest. |
| Zarenejad 2020 | Not our population of interest. Participants did not have fear of childbirth. |
CAQ: Childbirth Attitudes Questionnaire
Characteristics of studies awaiting classification [ordered by study ID]
Firouzan 2020.
| Methods | Randomised controlled trial |
| Participants |
Inclusion criteria: The inclusion criteria were being: 1) 18 to 35 years old, 2) able to speak and read Persian (since some women were from the less privileged parts of Zanjan province in which all people do not speak Persian and did not have enough reading and speaking language skills), 3) having a single fetus, 4) scoring ≥ 66 on the Wijma Delivery Expectancy/Experience Questionnaire (23), and 5) first time pregnancy. Exclusion criteria: Women were excluded if they had any history of infertility, and mental or physical chronic diseases. |
| Interventions |
Intervention (n = 40): BELIEF Psychoeducaton by Midwives (Birth emotions looking into improve expectant fear) Control/Comparison intervention (n = 40): Usual routine maternity care |
| Outcomes | Childbirth fear (WDEQA) and self‐efficacy |
| Notes |
Ethics: The ethics committee of Zanjan University of Medical Sciences approved the procedure of the research (IR.ZUMS.REC.1397.025). Participants signed a written consent before participating in the study. Trial registration: IRCT20101219005417N3, Date of Registration: 2018‐12‐19. Study funding sources: This research is supported by the Zanjan University of Medical Sciences. The university had no role in designing, gathering and analysing the data, and preparing the manuscript. Trial authors’ declarations of interest: The authors have no actual or potential conflicts of interest including any financial, personal or other relationships with other people or organizations within 3 years of beginning the work submitted that could inappropriately influence their work. We attempted to contacted the trial authors to establish details in relation to the intervention, the calculation of the sample size and we requested raw data if possible from Dr Jafari. Contacted on 02/06/2021 and 08/06/2021 but we have not received a reply. |
IRCT2015111625066N1.
| Methods | Single blind, semi‐experimental study with pre‐ and post‐test and control group. After pretest and selecting 50 people with fear of childbirth and anxiety level equal to 80 and above, participants will be allocated into 2 groups using random number table. |
| Participants | W‐DEQ A > 80 Inclusion criteria: "Age between 18 and 40 years; first pregnancy; gestational age between 18 and 28 weeks; educational level from diploma to masters; mental health; not receiving any types of meditation [sic]; concentration and attention education till before the pre‐test time and also in the period between pre‐test and establishment of mindfulness training (which will last about a month and a half) and then up to the end of the final stage of research (post‐test)." Exclusion criteria: "Receiving psychotherapy; antidepressants; anti‐anxiety and antipsychotic medications; high‐risk pregnancy; use of certain medications." |
| Interventions | Intervention group will receive mindfulness training according to the Nancy Bardak learning model in 8 sessions, in addition to routine care of childbirth preparation classes, over one and a half months. Each session will take 1 hour and 30 minutes and will be delivered as a group education. |
| Outcomes | W‐DEQ A |
| Notes | Not published |
IRCT201705011113N8.
| Methods | RCT |
| Participants |
Inclusion criteria: "20‐30 weeks pregnant women with low danger pregnancy,first pregnancy, singleton pregnancy, ability to read and write؛, scores 28 and more in the fear of accouchement questionnaire, availability and follow up. Men inclusion criteria: men who would like to participate in research؛, ability to read and write, availability and follow up." Exclusion criteria: "Women who would not like to participate for any reason ؛women who suffering by chronic disease including high blood pressure, diabetes, cardiovascular disease and etc.؛sterility history and pregnancy using assist reproduction method, mental disease history or using medicine. Men Exclusion criteria: men who would not like to participate for any reason" |
| Interventions | "The intervention group will participate in 6 session (90 minutes per each session) in accouchement preparation class and their fear of accouchement and choosing type of accouchement will be assessed before and after the intervention. For the control group, accouchement preparation class will be held without husband." |
| Outcomes | Fear of childbirth Type of delivery |
| Notes | MSc midwifery project. Unpublished. |
IRCT20170827035934N2.
| Methods | RCT |
| Participants |
Inclusion criteria: Gestational age 20‐24; willingness to participate in research; Have reading and writing skills; first or second pregnancy; assessment of delivery as a scary event (score of 3 or more 5 Likert scale); age range 18‐35; single pregnancy; wanted pregnancy Exclusion criteria: Cchronic disease such as heart disease, hypertension, diabetes mellitus; history of abortion and cesarean section; bleeding placenta previa; use of certain drugs; mental illness during the last year; drug addiction and cigarette smoking |
| Interventions | Intervention group: In the intervention group, training program runs in 8, 90‐minute sessions starting from the 20th week to the 24th week of pregnancy. Each session consists of 2 parts: a training unit (45 minutes) and a practical training section (45 minutes). |
| Outcomes | Primary outcome: Fear of Childbirth Secondary outcome: Mode of birth |
| Notes | Registered while recruiting. No results published. (MSC project: Mortazafi and Mehrabadi) |
IRCT20170827035934N3.
| Methods | RCT |
| Participants |
Inclusion criteria: Gestational age 28‐36; willingness to participate in research; have reading and writing skills; first pregnancy; age range 18‐45; single pregnancy; wanted pregnancy Exclusion criteria: Chronic disease such as heart disease, hypertension, diabetes mellitus; history of abortion; bleeding; placenta previa; use of certain drugs; mental illness during the last year; drug addiction and cigarette smoking. |
| Interventions | In the intervention group, group counselling with a solution‐focused approach runs in 4, 90‐minute sessions starting from the 28th week to the 36th week of pregnancy. The control group, only attend in physiologic delivery training classes in Mobini hospital. |
| Outcomes | Fear of childbirth; caesarean preference; pregnancy anxiety |
| Notes | Registered 09/5/2019. Recruitment complete according to protocol. No results published. |
IRCT20170921036302N3.
| Methods | RCT |
| Participants |
Inclusion criteria: Age range of 18‐35 years; hospitalisation at the beginning of the active phase in maternity hospital; single embryo; fit the head of the fetus with the mother's hip; participation in childbirth preparation classes. Exclusion criteria: Physical and mental disease; the occurrence of any complications of pregnancy such as pre‐eclampsia; bleeding; diabetes; intrauterine fetal death; and tearing of an amniotic fluid bag during hospitalisation. |
| Interventions |
Intervention: The test group is supported by a private midwife (who has completed a physiological delivery course for 60 hours) from the beginning of admission to 2 hours after delivery, will receive all midwifery services. Control: Receive routine care from the non‐private midwife. |
| Outcomes | The amount of anxiety and fear of delivery in the 2 groups, by Hamilton's Anxiety Inventory and Hartmann's Maternity Distress Questionnaire. |
| Notes | Recruitment complete but only protocol available. |
IRCT20180901040916N1.
| Methods | RCT Setting: medical centres in Iran |
| Participants | Two different sets of inclusion criteria are reported in the trial registry: Inclusion criteria: 1‐ Having no hearing and mental problems in the mother that prevents communication with the researcher 2‐ Age between 18 and 35 years. 3‐ Gestational age between 28 weeks and 32 weeks. 4‐ low‐risk singleton pregnancies and is showing head. 5‐ Being primigravid. 6. Do not have a history of infertility. 7‐ Not having a medical cause for cesarean section, such as a transverse position, previous uterine surgery, etc. Non‐entry terms: 1‐ Earn more than 85 scores from Vijma's fears questionnaire. 2‐ She or her husband should be employed by the hospital staff. 3‐ In the last 6 months, she has severe mental problems. Inclusion criteria: 1‐ Residence in Mashhad 2‐ Access to Telephone 3‐ Having at least elementary education 4‐ Do not have a mother's hearing and speech problems that can not communicate with a researcher 5‐ Age between 18 and 35 6‐ Gestational age between 28 weeks to 32 weeks 7‐ Single and low‐risk pregnancy 8‐ Primigravid 9‐ Willingness to cooperate 10‐ The sample has no history of infertility 11‐ The sample does not have a medical cause for cesarean section (such as a transverse or transverse placement, an uterine surgeon, etc.). Exclusion criteria: 1‐ Do not be staffed by a hospital 2‐ She has not had severe mental problems in the last 6 months 3‐ In the Vijma's fear questionnaire,she scored less than 85 points Age: From 18 years old to 35 years old Recruitment target: 70 women |
| Interventions | Intervention group: group counseling sessions for 4 consecutive weeks Control group: Routine care of childbirth classes |
| Outcomes | Fear, Attitude, Intention to choose a type of delivery, Social support, Self‐efficacy, Decision conflict, Subjective norms |
| Notes | Protocol published with contradicting information in the exclusion criteria. Author emailed 26/04/2021 for clarity but no reply Registered May 2019 Expected recruitment start date: October 2010 Expected recruitment end date: March 2019 |
IRCT20190129042538N1.
| Methods | RCT Setting: medical centres in Iran |
| Participants | Two different versions of inclusion criteria appear in the trial registry record: Inclusion criteria Age:18‐35 years old; Primiparous; Gestational age: 36‐37 weeks; Not having depression, anxiety, stress; Having average and high level of hypnotic susceptibility; Having average and high level of fear of childbirth. Inclusion criteria: Gestational age: 36‐37 weeks Willingness to have a normal delivery Having moderate to high degree of hypnotic susceptibility Exclusion criteria: Having high risk pregnancy. Having psychological disorders including depression, anxiety, stress. Having clinical fear (scoring greater than 85 points according to Wijma Expectancy/Experience Delivery Questioner type A) Age: 18‐35 years Target sample size: 70 |
| Interventions | Intervention group will receive two training sessions of 15‐20 minutes self‐hypnosis education in 37‐38th weeks of pregnancy in addition to usual prenatal cares. Audio file (15‐20 minutes) of pain and fear control dialogues derived from sessions will be recorded by mother’s mobile phone and will be given to the pregnant woman in which listening and practicing self‐hypnosis twice a day at home (morning and afternoon) until delivery time and then doing it at delivery. Comparator: routine prenatal care |
| Outcomes | WDEQ score Pain of labour measured on VAS Childbirth satisfaction measured on Mackey Childbirth Satisfaction Rating Scale |
| Notes | It is not clear if the study included women with fear of childbirth. Study authors contacted by email April 2021 for clarification but no response as yet. |
IRCT20190203042607N1.
| Methods | RCT |
| Participants |
Inclusion criteria: "Age range between 18 and 35 years. Gestational age at least 20 weeks and a maximum of 28 weeks. First pregnancy and singleton pregnancy. Literate (reading and writing). Willing to participate in antenatal preparation classes." Exclusion criteria: "Multipara. Addiction. Use of psychiatric drugs in the last 6 months. Major life stress in the last 6 months, such as death of kin. Early medical conditions (diabetes, chronic hypertension history)." |
| Interventions |
Intervention: participation in preparation classes for delivery and solution‐focused counselling Control: participation in preparation classes for childbirth |
| Outcomes | Childbirth self‐efficacy, fear of childbirth |
| Notes | Protocol only available. Registered in April 2019. |
NCT01687907.
| Methods | RCT Setting: Helsinki University Central Hospital, Finland |
| Participants | Inclusion criteria: "fear of childbirth in arms 1 and 2, nulliparous in arms 3 and 4" Exclusion Criteria: "not able to answer the questionnaires" |
| Interventions | Music: women with fear of childbirth "advised to active music listening." |
| Outcomes |
Primary outcome: Spontaneous vaginal delivery Secondary outcome measures: Delivery satisfaction Other outcome measures: Early mother‐infant relationship measured 6 months after delivery Mental wellbeing during pregnancy and up to 6 months after delivery |
| Notes | Contacted 2 authors by email but no response‐ no mention of WDEQ A as outcome We attempted to contact the trial authors by email on 23rd October 2020 but did not receive a reply. We attempted to contact Prof Sten on 28 October using a different email address but have not received any reply. |
NCT02266186.
| Methods | RCT Setting: Linkoeping University, Sweden |
| Participants | Pregnant women aged 18‐50 years Inclusion criteria: Pregnant women in 16‐30 weeks of pregnancy at time for enrolment. Able to read and write Swedish language having the possibility to use the Internet during the therapy. Exclusion criteria: Suicidal, psychotic or schizophrenic symptoms. Not motivated to work with their fear. Ongoing psychological therapy because of fear of childbirthNon Swedish‐ speaking women |
| Interventions | Internet CBT Traditional CBT |
| Outcomes |
Primary outcome measures: Level of fear of childbirth [Time Frame: Change baseline to after 8 weeks of treatment] self rating with: Wijma Expectancy/Experience Questionnaire version A (W‐DEQ vers. A) Secondary outcome measures: Level of trauma [Time Frame: Change from baseline to 3 months after delivery ]self rating with: Traumatic Event Scale (TES) Level of anxiety and depression [Time Frame: Change from baseline to 3 months after delivery] self rating with: Hospital anxiety and depression scale (HADS) |
| Notes | Reported as completed in January 2018. Authors emailed. |
NCT04097782.
| Methods | RCT |
| Participants | "Inclusion Criteria:
Exclusion Criteria:
|
| Interventions | "Following the pretests between the 28th and the 34th gestational weeks, nulliparous women in the intervention group received a presentation on childbirth preparation at a room of the obstetrics clinic. The education was completed in two sections in a single day. Each session took about 45 minutes there was a 15‐minute break between the sessions. Following the education, the questions of the participants were responded and educational brochures on childbirth preparation were given to the participants. One of the researchers of this study telephoned the participant women in the intervention group one week after the childbirth education and provided counseling service about the demands and the points that the nulliparous women wondered." |
| Outcomes |
Primary outcome measures
|
| Notes | Recruitment completed November 2019, no results published. Not clear if FOC was inclusion criteria. |
NCT04214431.
| Methods | RCT |
| Participants |
Inclusion criteria:
Exclusion criteria:
|
| Interventions | Intervention: 8‐week mindfulness‐based childbirth education |
| Outcomes |
Primary outcome measures Fear of childbirth measured by the Wijma Delivery Expectancy/ Experience Questionnaire. Secondary outcome measures Anxiety measured by State‐Trait Anxiety Inventory, STAI Depression measured by Edinburgh Postnatal Depression Scale Mindfulness measured by Chinese Version Mindful Attention Awareness Scale Birth outcomes: vaginal delivery or caesarean delivery. |
| Notes | Completed early 2020 but not published yet |
Weng 2016.
| Methods | RCT Setting: USA |
| Participants | Inclusion and exclusion criteria not explicitly stated |
| Interventions | Intervention (n = 15): "Mind in Labor (MIL; a 16‐hour workshop version of Mindfulness‐Based Childbirth and Parenting)" Comparator (n = 15): "childbirth education without a mind‐body focus" |
| Outcomes | Pain catastrophising |
| Notes | FOC not an outcome in the abstract Contact: Helen Weng, helen.weng@ucsf.edu |
W‐DEQ: Wijma Delivery Expectancy/Experience Questionnaire
Characteristics of ongoing studies [ordered by study ID]
Baas 2017.
| Study name | The optiMUM study |
| Methods | Multi‐centre RCT 2 2‐armed RCT Setting: one university hospital, two teaching hospitals and several community midwifery practices in Amsterdam, the Netherlands. |
| Participants |
Inclusion criteria: Pregnant women between 8 and 20 weeks with PTSD or FOC Exclusion criteria "age <18 years old, current psychological treatment, intermediate or high suicide risk (based on the mini international neuropsychiatric interview‐plus; MINI‐plus), or severe psychotic disorder, such as schizophrenia or current psychosis (based on MINI‐plus)" |
| Interventions |
Intervention: eye movement desensitization and reprocessing (EMDR). "The EMDR therapy group will receive a maximum of three 90‐min sessions, in addition to standard care during pregnancy" Comparator: "standard care during pregnancy, with routine obstetrical checks. Assuming good clinical care, anxious pregnant women and those with traumatic childbirth experiences may receive more counselling compared to not‐anxious pregnant women, but will (probably) not be referred for EMDR therapy. Type and frequency of any form of professional care will be registered." |
| Outcomes |
Primary outcome measures are severity of childbirth‐related PTSD or FoC symptoms. Secondary outcomes are percentage of PTSD diagnoses, percentage caesarean sections, subjective childbirth experience, obstetrical and neonatal complications, and healthcare costs. |
| Starting date | April 2015 |
| Contact information | optimum@olvg.nl |
| Notes |
IRCT20120718010324N43.
| Study name | The effect of counseling with Beck’s cognitive therapy on anxiety and childbirth fear: a randomized controlled clinical trial |
| Methods | Randomized controlled clinical trial with two parallel arms. Setting: Health centres of Ardebil city, Iran |
| Participants | Participants will be nulliparous pregnant women ages 18‐35 years old with gestational age 26‐28 weeks. Inclusion criteria: WDEQA > 38, from 18 years old to 35 years old, no history of infertility, having a depression score lower than 12 according to the Edinburgh questionnaire and non‐use of psychoactive drugs and antidepressants based on the patient's statement. Lack of psychological problems before pregnancy, not having medical problems during pregnancy, including high blood pressure, gestational diabetes, twin and multiple pregnancy and multiple, Placenta and amniotic fluid disorders and having at least secondary education Exclusion criteria: "Having an indication for cesarean including abnormal fetal presentation, pelvic stenosis, large fetus and ... Change the location to another city until delivery Uncertainty about being able to attend all consultation sessions. Having cardiovascular disease, high blood pressure and liver diseases according to the statement of participant, Unwanted pregnancy" Target sample size: 68 |
| Interventions | Intervention: The intervention group will receive counselling with the Beck cognitive therapy approach. Six 60 to 90 minute group counselling sessions once a week. Comparator: the control group will receive routine pregnancy care. |
| Outcomes | Primary outcome: Anxiety. measured with State – Trait Anxiety Inventory Secondary outcomes:
|
| Starting date | Registered March 2018 (registered while recruiting) |
| Contact information | mirghafourvandm@tbzmed.ac.ir |
| Notes | Registered while recruiting in 2018. Author contacted by email to enquire re: results. Author replied, article submitted for publication yesterday (11/11/2020). Funding source: Tabriz University of Medical Sciences |
NCT02972112.
| Study name | Ultrashort Cognitive Behavioral Intervention for Tokophobia ‐ A Prospective Randomized Single Blinded Controlled Trial |
| Methods | RCT |
| Participants |
Inclusion criteria:
Exclusion criteria:
|
| Interventions | Novel cognitive behavioral protocol for the treatment of tocophobia |
| Outcomes | Pregnancy‐Related Anxiety Questionnaire [Time Frame: In the end of second session of intervention‐ up to 4 weeks from screening] a widely used instrument to assess and identify pregnancy‐specific anxiety in women |
| Starting date | Nov 2016 |
| Contact information | gabiar@tlvmc.gov.il |
| Notes | Estimated recruitment study date October 2020, no study results published. Emailed July 2020/ Nov 2020 |
NCT03393637.
| Study name | MOMS [Mentors offering maternal support] |
| Methods | A longitudinal, multi‐site, randomised controlled trial Setting: military communities in USA |
| Participants | Inclusion criteria:
Exclusion criteria:
|
| Interventions |
Experimental intervention: M‐O‐M‐S Intervention M‐O‐M‐S intervention is 10, 1 hour prenatal mentored support groups |
| Outcomes |
|
| Starting date | 1 December 2017 Estimated completion date: December 2021 |
| Contact information | Karen Weis, weis@uiwtx.edu |
| Notes | Currently recruiting ‐ only protocol available. Estimated study completion 31 December 2021 |
Differences between protocol and review
There are some differences between the published protocol (O'Connell 2019), and the full review. Details are below.
Changes in authorship:
The first author's affiliation and contact details have been updated.
We added Fiona Stewart as a new co‐author to this review. Rebecca MD Smyth and Louise C Kenny have left the review team for the full review.
Contributions of authors
All authors were involved in the review. Maeve O'Connell co‐ordinated and drafted the review, and is the guarantor of the review. Patricia Leahy‐Warren assisted in conceiving the review and gave her clinical perspective on the final draft of the review. Fiona Stewart, Sinéad O'Neill and Ali Khashan assisted with the data extraction, risk of bias assessment, checking of the statistical analyses for accuracy, and assessing the certainty of the evidence using the GRADE criteria, and commented on the final draft of the review.
Sources of support
Internal sources
-
University College Cork, Ireland, Ireland
AK and PLW are employees of UCC and receive support from the University in the form of a salary.
External sources
-
Health Research Board (HRB), Ireland, Ireland
MOC is the recipient of a full Cochrane Training Fellowship (Grant no CT‐2016‐1858) from the HRB, Ireland.
Declarations of interest
Maeve A O'Connell: is the recipient of a full Cochrane Training Fellowship supported by the Health Research Board, Ireland (Grant No: CTF‐2016‐1858).
Patricia Leahy‐Warren: none known.
Ali S Khashan: none known.
Sinéad M O'Neill: none known.
Fiona Stewart: none known.
Edited (no change to conclusions)
References
References to studies included in this review
Boz 2020 {published and unpublished data}
- Boz I, Akgun M, Duman F. A feasibility study of a psychoeducation intervention based on Human Caring Theory in nulliparous women with fear of childbirth. Journal of Psychosomatic Obstetrics and Gynaecology 2020;41:1-13. [CENTRAL: CN-02093893] [EMBASE: 2004733633] [PMID: ] [DOI] [PubMed] [Google Scholar]
Kordi 2017 {published data only}
- IRCT2017071135008N1. Investigating the effect of the group psychoeducational program on the severity of childbirth fear and childbirth satisfaction in primigravida women. http://en.irct.ir/trial/26590 (first received 15 August 2017).
- Kordi M, Bakhshi M, Masoudi S, Esmaily H. Effect of a childbirth psychoeducation program on the level of fear in primigravid women. Evidence Based Care Journal 2017;7(3):26-34. [CENTRAL: CN-02093892] [Google Scholar]
Rahmani 2020 {published data only}
- Rahmani R, Moghadam FY, Hadizadeh-Talasaz F, Rahmani MR. The effect of peer education on fear of childbirth in pregnant women: a randomized clinical trial. International Journal of Women's Health and Reproduction Sciences 2020;8(2):209-14. [CENTRAL: CN-02100717] [EMBASE: 2004149437] [Google Scholar]
Rondung 2018 {published data only}
- Baylis R, Ekdahl J, Haines H, Rubertsson C. Women's experiences of internet-delivered cognitive behaviour therapy (ICBT) for fear of birth. Women and Birth: Journal of the Australian College of Midwives 2020;33(3):e227-e233. [DOI: ] [DOI] [PubMed]
- Hildingsson I, Rubertsson C. Childbirth experiences among women with fear of birth randomized to internet-based cognitive therapy or midwife counseling. Journal of Psychosomatic Obstetrics and Gynaecology 2019 [Epub ahead of print]:1-10. [DOI] [PubMed]
- Larsson B. Treatment for childbirth fear with a focus on midwife-led counselling [thesis]. Uppsala, Sweden: Uppsala University, 2017. [Google Scholar]
- NCT02306434. Fear of childbirth - comparison of two treatment options: internet given behavioral therapy and counseling by midwife- a clinical randomized controlled trial. https://clinicaltrials.gov/ct2/show/NCT02306434 (first received 3 December 2014).
- Rondung E, Ternstrom E, Hildingsson I, Haines HM, Sundin O, Ekdahl J, et al. Comparing internet-based cognitive behavioral therapy with standard care for women with fear of birth: randomized controlled trial. JMIR Mental Health 2018;5(3):e10420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ternstrom E, Hildingsson I, Haines H, Rubertsson C. Changes in fear of birth during pregnancy - a randomized controlled trial comparing internet-based cognitive behavioral therapy with standard care. In: 31st International Confederation of Midwives Triennial Congress. Midwives - Making a Difference in the World; 2017 June 18-22; Toronto, Canada. 2017:Abstract no: P1.155.
- Ternstrom E, Hildingsson I, Larsson B, Rubertsson C, Haines H, Karlstrom A, et al. A randomized controlled study comparing internet-based cognitive behavioral therapy and counselling by standard care for fear of birth - a study protocol. Sexual and Reproductive Healthcare 2017;13:75-82. [DOI] [PubMed] [Google Scholar]
- Ternstrom U. Identification and Treatment of Women with a Fear of Birth [Doctoral thesis]. Uppsala, Sweden: Uppsala University, 2018. [Google Scholar]
Rouhe 2015 {published data only}
- Bergstrom M, Rudman A, Waldenstrom U, Kieler H. Fear of childbirth in expectant fathers, subsequent childbirth experience and impact of antenatal education: subanalysis of results from a randomized controlled trial. Acta Obstetricia et Gynecologica Scandinavica 2013;92(8):967-73. [DOI] [PubMed] [Google Scholar]
- NCT01548131. A randomized longitudinal trial about treatment for severe fear of childbirth. https://clinicaltrials.gov/ct2/show/NCT01548131 (first received 8 March 2012).
- Rouhe H, Salmela-Aro K, Toivanen R, Tokola M, Halmesma E, Saisto T. Obstetric outcome after intervention for severe fear of childbirth in nulliparous - randomised trial. Acta Obstetricia et Gynecologica Scandinavica 2012;91(Suppl 159):28. [Google Scholar]
- Rouhe H, Salmela-Aro K, Toivanen R, Tokola M, Halmesmaki E, Ryding EL, et al. Group psychoeducation with relaxation for severe fear of childbirth improves maternal adjustment and childbirth experience - a randomised controlled trial. Journal of Psychosomatic Obstetrics and Gynaecology 2015;36(1):1-9. [DOI] [PubMed] [Google Scholar]
- Rouhe H, Salmela-Aro K, Toivanen R, Tokola M, Halmesmaki E, Saisto T. Life satisfaction, general wellbeing and costs of treatment for severe fear of childbirth in nulliparous women by psychoeducative group or conventional care attendance. Acta Obstetricia et Gynecologica Scandinavica 2015;94:527-33. [DOI] [PubMed] [Google Scholar]
- Rouhe H, Salmela-Aro K, Toivanen R, Tokola M, Halmesmaki E, Saisto T. Obstetric outcome after intervention for severe fear of childbirth in nulliparous women - randomised trial. BJOG: an International Journal of Obstetrics and Gynaecology 2013;120(1):75-84. [DOI] [PubMed] [Google Scholar]
- Salmela-Aro K, Read S, Rouhe H, Halmesmäki E, Toivanen RM, Tokola MI, et al. Promoting positive motherhood among nulliparous pregnant women with an intense fear of childbirth: RCT intervention. Journal of Health Psychology 2012;17(4):520-34. [DOI] [PubMed] [Google Scholar]
- Salmela-Aro K, Rouhe H, Erja H, Toivanen R, Tokola M, Saisto T. Intervention promoting positive motherhood among nulliparous pregnant women with an intense fear of childbirth. European Child and Adolescent Psychiatry 2011;20(Suppl 1):S49. [Google Scholar]
Toohill 2014 {published data only}
- ACTRN12612000526875. What is the effect of an antenatal midwife-led psycho-education intervention in reducing childbirth related fear in women reporting a high level of fear? www.anzctr.org.au/Trial/Registration/TrialReview.aspx?ACTRN=12612000526875 (first received 8 May 2012).
- Fenwick J, Gamble J, Creedy DK, Buist A, Turkstra E, Sneddon A, et al. Study protocol for reducing childbirth fear: a midwife-led psycho-education intervention. BMC Pregnancy and Childbirth 2013;13(1):190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fenwick J, Toohill J, Gamble J, Creedy DK, Buist A, Turkstra E, et al. Effects of a midwife psycho-education intervention to reduce childbirth fear on women's birth outcomes and postpartum psychological wellbeing. BMC Pregnancy and Childbirth 2015;15(1):284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gamble J, Toohill, Fenwick J. Competency based training for midwives to deliver psycho-education for women with childbirth fear. In: International Confederation of Midwives 30th Triennial Congress. Midwives: Improving Women’s Health; 2014 June 1-4; Prague, Czech Republic. 2014:C230.
- Toohill J, Callander E, Gamble J, Creedy DK, Fenwick J. A cost effectiveness analysis of midwife psycho-education for fearful pregnant women - a health system perspective for the antenatal period. BMC Pregnancy and Childbirth 2017;17(1):217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Toohill J, Fenwick J, Gamble J, Creedy DK, Buist A, Turkstra E, et al. A randomized controlled trial of a psycho-education intervention by midwives in reducing childbirth fear in pregnant women. Birth 2014;41(4):384-94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Toohill J, Fenwick J, Gamble J. Randomised controlled trial of a midwife-led psycho-education intervention for women with childbirth fear. In: International Confederation of Midwives 30th Triennial Congress. Midwives: Improving Women’s Health; 2014 June 1-4; Prague, Czech Republic. 2014:C396.
- Toohill J, Gamble J, Creedy DK, Callander E, Fenwick J. Cost-effectiveness of midwife psycho-education for women with childbirth fear: A randomized controlled trial. In: 31st International Confederation of Midwives Triennial Congress. Midwives - Making a Difference in the World; 2017 June 18-22; Toronto, Canada. 2017:Abstract no: P3.526.
- Turkstra E, Mihala G, Scuffham PA, Creedy DK, Gamble J, Toohill J, et al. An economic evaluation alongside a randomised controlled trial on psycho-education counselling intervention offered by midwives to address women's fear of childbirth in Australia. Sexual & Reproductive Healthcare 2017;11:1-6. [DOI: ] [DOI] [PubMed] [Google Scholar]
Wahlbeck 2020 {published data only}
- NCT01457482. Art therapy as treatment for fear of childbirth. https://clinicaltrials.gov/ct2/show/NCT01457482 (first received 24 October 2011).
- Wahlbeck H, Kvist LJ, Landgren K. Art Therapy and counseling for fear of childbirth: a randomized controlled trial. Art Therapy: Journal of the American Art Therapy Assocation 2020;37:1-8. [Google Scholar]
References to studies excluded from this review
Abdollahi 2020 {published data only}
- Abdollahi S, Faramarzi M, Delavar MA, Bakouei F, Chehrazi M, Gholinia H. Effect of psychotherapy on reduction of fear of childbirth and pregnancy stress: a randomized controlled trial. Frontiers in Psychology 2020;11:787. [CENTRAL: CN-02129810] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Ahmadi 2017 {published data only}
- Ahmadi L, Bagheri F. The effectiveness of educating mindfulness on anxiety, fear of delivery, pain catastrophizing and selecting caesarian section as the delivery method among nulliparous pregnant women. Nursing Practice Today 2017;4(1):52-63. [CENTRAL: CN-02129812] [Google Scholar]
Andaroon 2017 {published data only}
- Andaroon N, Kordi M, Kimiaei SA, Esmaeily H. The effect of individual counseling program by a midwife on fear of childbirth in primiparous women. Journal of Education and Health Promotion 2017;6:97. [CENTRAL: CN-02093890] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- IRCT2016042827653N1. The effect of individual consultation on the reduced fear of childbirth among nulliparous women. http://en.irct.ir/trial/22610 (first received 2 September 2016).
Bergstrom 2009 {published data only}
- Bergstrom M, Kieler H, Waldenstrom U. Effects of natural childbirth preparation versus standard antenatal education on epidural rates, experience of childbirth and parental stress in mothers and fathers: a randomised controlled multicentre trial. BJOG: an international journal of obstetrics and gynaecology 2009;116(9):1167-76. [DOI] [PMC free article] [PubMed] [Google Scholar]
Bittner 2014 {published data only}
- Bittner A, Peukert J, Zimmermann C, Junge-Hoffmeister J, Parker LS, Stobel-Richter Y, et al. Early intervention in pregnant women with elevated anxiety and depressive symptoms: efficacy of a cognitive-behavioral group program. Journal of Perinatal & Neonatal Nursing 2014;28(3):185-95. [DOI] [PubMed] [Google Scholar]
Boryri 2019 {published data only}
- Boryri T, Navidian A, Marghzari N. Comparison of the effect of muscle relaxation and guided imagery on happiness and fear of childbirth in primiparous women admitted to health care centers. International Journal of Women's Health and Reproduction Sciences 2019;7(4):490-5. [CENTRAL: CN-02005657] [EMBASE: 2002875511] [Google Scholar]
Cankaya 2020 {published data only}
- Cankaya S, Simsek B. Effects of antenatal education on fear of birth, depression, anxiety, childbirth self-efficacy, and mode of delivery in primiparous pregnant women: a prospective randomized controlled study. Clinical Nursing Research 2020;29(3):1054773820916984. [CENTRAL: CN-02096138] [EMBASE: 631501282] [PMID: ] [DOI] [PubMed] [Google Scholar]
- NCT04097782. Effects of antenatal education on fear of birth, depression, anxiety, childbirth self-efficacy, and mode of delivery in primiparous pregnant women. https://clinicaltrials.gov/show/nct04097782 (first received 20 Sept 2019). [CENTRAL: CN-01992057] [DOI] [PubMed]
ChiCTR1900025309 {published data only}
- ChiCTR1900025309. The effects of simulation-based childbirth education on fear of childbirth of Chinese primiparas [Comprehensive health management during pregnancy and delivery period (yoga training during pregnancy, simulation-based childbirth education, postpartum feeding guidance)]. www.who.int/trialsearch/Trial2.aspx?TrialID=ChiCTR1900025309 2019. [CENTRAL: CN-01975343]
CTRI/2019/11/021950 {published data only}
- CTRI/2019/11/021950. To study whether brief interventions are effective in reducing fear of childbirth and impact self-efficacy among first time mothers [Effectiveness of brief interventions on fear of childbirth and self-efficacy among primigravidae]. Http://www.who.int/trialsearch/Trial2.aspx?TrialID=CTRI/2019/11/021950 2019. [CENTRAL: CN-02066854]
Downe 2015 {published data only}ISRCTN27575146
- Downe S, Finlayson K, Melvin C, Spiby H, Ali S, Diggle P, et al. Self-hypnosis for intrapartum pain management in pregnant nulliparous women: a randomised controlled trial of clinical effectiveness. BJOG: an international journal of obstetrics and gynaecology 2015;122(9):1226-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Downe S. The SHIP trial - a randomised controlled trial of self-hypnosis during labour. www.midirs.org/development/MIDIRSEssence.nsf/articles/F329431A7FF3E593802578A90052BFA5 (accessed 14 December 2011).
- Finlayson K, Downe S, Hinder S, Carr H, Spiby H, Whorwell P. Unexpected consequences: women's experiences of a self-hypnosis intervention to help with pain relief during labour. BMC Pregnancy and Childbirth 2015;15(1):229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- ISRCTN27575146. Self-hypnosis for intrapartum pain management (ship) trial. www.isrctn.com/ISRCTN27575146 (first received 25 March 2011).
Duncan 2017 {published data only}
- Duncan LG, Cohn MA, Chao MT, Cook JG, Riccobono J, Bardacke N. Benefits of preparing for childbirth with mindfulness training: a randomized controlled trial with active comparison. BMC Pregnancy and Childbirth 2017;17(1):140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- NCT02327559. Randomized controlled trial of a mindfulness intervention for labor-related pain and fear. https://clinicaltrials.gov/ct2/show/NCT02327559 (first received 30 December 2014).
Ghazaie 2016 {published data only}
- Ghazaie M, Davoodi I, Honarmand MM, Nejad SB, Neysi A. The effectiveness of cognitive-behavioral therapy on fear of childbirth, fear of pain, self-efficacy of childbirth and tendency to caesarean in nulliparous women. Iranian Journal of Obstetrics, Gynecology and Infertility 2016;19(31):1-12. [Google Scholar]
Gonenc 2020 {published data only}
- Gonenc IM, Dikmen HA. Effects of dance and music on pain and fear during childbirth. Journal of Obstetric, Gynecologic, and Neonatal Nursing : JOGNN 2020;49(2):144-53. [CENTRAL: CN-02085669] [EMBASE: 630949158] [PMID: ] [DOI] [PubMed] [Google Scholar]
- NCT03648099. Effect of labor dance and music on labor pain and fear of childbirth. https://clinicaltrials.gov/show/nct03648099 (first received 27 August 2018).
Haapio 2017 {published data only}
- Haapio S, Kaunonen M, Arffman M, Astedt-Kurki P. Effects of extended childbirth education by midwives on the childbirth fear of first-time mothers: an RCT. Scandinavian Journal of Caring Sciences 2017;31(2):293-301. [DOI] [PubMed] [Google Scholar]
IRCT20110228005931N5 {published data only}
- IRCT20110228005931N5. Study the effect of group counseling based on motivational interviewing approach on self-efficacy, anxiety, and fear of childbirth, in pregnant women. http://en.irct.ir/trial/33468 (first received 4 September 2018).
IRCT20120215009014N317 {published data only}
- IRCT20120215009014N317. Effect progressive muscle relaxation technique versus control group on the fear related to pregnancy and childbirth in primiparous women. Http://www.who.int/trialsearch/Trial2.aspx?TrialID=IRCT20120215009014N317 2019. [CENTRAL: CN-02068899]
IRCT201312073034N13 {published data only}
- IRCT201312073034N13. Effectiveness of snoezelen room on fear, anxiety and satisfaction of childbirth in primiparous women. https://www.irct.ir/trial/3024 (first received 30 October 2015).
IRCT20150608022609N6 {published data only}
- IRCT20150608022609N6. The effect of midwife-led counseling on fear of childbirth. http://www.who.int/trialsearch/Trial2.aspx?TrialID=IRCT20150608022609N6 2019. [CENTRAL: CN-02069079]
IRCT2015120625399N1 {published data only}
- IRCT2015120625399N1. The effect of health education based on theory of planned behavior on fear of natural childbirth in pregnant women. http://en.irct.ir/trial/21254 (first received 5 June 2016).
IRCT2016060828352N1 {published data only}
- IRCT2016060828352N1. The effect of couples counseling based on problem solving approach on the childbirth fear, childbirth self-efficacy and the choice of the type of delivery in primigravid women requesting elective cesarean section. http://en.irct.ir/trial/23023 (first received 22 August 2016).
IRCT20160625028630N2 {published data only}
- IRCT20160625028630N2. The effect of companion’s support on fear and self-efficacy of delivery. http://en.irct.ir/trial/23184 (first received 18 February 2018).
IRCT2016082429506N1 {published data only}
- IRCT2016082429506N1. The effectiveness of cognitive behavior therapy based on self- management on the fear, anxiety and delivery outcome in nulliparous women. http://en.irct.ir/trial/23696 (first received 20 September 2016).
IRCT2017030627557N3 {published data only}
- IRCT2017030627557N3. A comparative assessment of midwife-led counseling and "music and evidence based booklet package" on birth fear and its outcomes in pregnant women referred to the comprehensive health care centers. http://en.irct.ir/trial/22548 (first received 28 May 2017).
IRCT20171026037015N3 {published data only}
- IRCT20171026037015N3. Evaluation of the effect of education on fear of childbirth in nulliparous women. http://en.irct.ir/trial/27502 (first received 16 June 2018).
IRCT20171129037676N2 {published data only}
- IRCT20171129037676N2. Effect of Mindfulness Based Stress Reduction (MBSR) approach on the fear of childbirth rate in one- child women. http://en.irct.ir/trial/28518 (first received 3 March 2018).
IRCT20171230038133N1 {published data only}
- IRCT20171230038133N1. Comparison muscle relaxation and guided imagery on happiness and fear of childbirth in primiparous women referred to health centers in Zahedan in 2017. http://en.irct.ir/trial/28610 (first received 30 April 2018).
IRCT20180131038579N1 {published data only}
- IRCT20180131038579N1. Evaluating effectiveness of dialectic behavioral therapy on fear of childbirth and preferred mode of delivery. http://en.irct.ir/trial/30188 (first received 30 June 2018).
IRCT20180427039436N3 {published data only}
- IRCT20180427039436N3. Effect of cognitive- behavioral educations on childbirth self-efficacy and maternal role adaptation and fear of childbirth in nulliparous women. http://en.irct.ir/trial/31593 (first received 31 December 2018).
IRCT20180520039729N1 {published data only}
- IRCT20180520039729N1. The effectiveness of meta-cognitive therapy group on intense fear of normal vaginal delivery in primiparous pregnant women. http://en.irct.ir/trial/31290 (first received 24 May 2018).
IRCT20180721040544N1 {published data only}
- IRCT20180721040544N1. The effect of education on the choice of painless delivery in primiparous women [The effect of education based on the theory of planned behavior on the choice of painless delivery with epidural analgesia in primiparous women]. Http://www.who.int/trialsearch/Trial2.aspx?TrialID=IRCT20180721040544N1 2018. [CENTRAL: CN-01909326]
IRCT20190210042672N1 {published data only}
- IRCT20190210042672N1. Investigation of emotion regulation educations' effect on fear of childbirth in primigravida women. http://en.irct.ir/trial/38068 (first received 9 March 2019).
IRCT20200122046227N1 {published data only}
- IRCT20200122046227N1. The effect of Tele-midwifery on fear of childbirth, self-efficacy in coping with childbirth and delivery mode in primparous women. Https://www.irct.ir/trial/45272 2020. [CENTRAL: CN-02129786]
Irmak 2019 {published data only}
- Irmak Vural P, Aslan E. Emotional freedom techniques and breathing awareness to reduce childbirth fear: a randomized controlled study. Complementary Therapies in Clinical Practice 2019;35:224-31. [DOI] [PubMed] [Google Scholar]
Jamali 2018 {published data only}
- Jamali F, Olfati S, Oveisi F, Ranjkesh F. Effects of spouses' involvement in pregnancy on fear of childbirth in nulliparous women. Journal of Qazvin University of Medical Sciences 2018;22(2):38-7. [CENTRAL: CN-02093887] [Google Scholar]
Klabbers 2019 {published data only}
- Klabbers GA, Wijma K, Paarlberg KM, Emons WH, Vingerhoets AJ. Treatment of severe fear of childbirth with haptotherapy: design of a multicenter randomized controlled trial. BMC Complementary and Alternative Medicine 2014;14(1):385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klabbers GA, Wijma K, Paarlberg KM, Emons WHM, Vingerhoets AJJM. Haptotherapy as a new intervention for treating fear of childbirth: a randomized controlled trial. Journal of Psychosomatic Obstetrics & Gynecology 2019;40(1):38-47. [DOI] [PubMed]
- NTR3339. Treatment of severe fear of childbirth with haptotherapy. https://www.trialregister.nl/trial/3188 (first received 4 March 2012).
Lonnberg 2020 {published data only}
- Lonnberg G, Jonas W, Unternaehrer E, Branstrom R, Nissen E, Niemi M. Effects of a mindfulness based childbirth and parenting program on pregnant women's perceived stress and risk of perinatal depression-Results from a randomized controlled trial. Journal of Affective Disorders 2019;262:133-42. [CENTRAL: CN-02009757] [EMBASE: 2003760406] [PMID: ] [DOI] [PubMed] [Google Scholar]
Masoumi 2016 {published data only}
- IRCT2014072713405N4. Effect of education of physiological delivery in reducing the cesarean rate in pregnant women. http://en.irct.ir/trial/13262 (first received 14 November 2011).
- Masoumi SZ, Kazemi F, Oshvandi K, Jalali M, Esmaeili-Vardanjani A, Rafiei H. Effect of training preparation for childbirth on fear of normal vaginal delivery and choosing the type of delivery among pregnant women in Hamadan, Iran: a randomized controlled trial. Journal of Family and Reproductive Health 2016;10(3):115-21. [PMC free article] [PubMed] [Google Scholar]
Mehrabadi 2020 {published data only}
- Mehrabadi M, Masoudifar M, Parvizi A, Rakhshani MH, Mortazavi F. Effects of childbirth preparation classes program based on national guideline on fear of childbirth in pregnant women: a randomized clinical trial. Iranian Journal of Obstetrics, Gynecology and Infertility 2020;23(1):58-68. [Google Scholar]
Navaee 2015 {published data only}
- Navaee M, Abedian Z. Effect of role play education on primiparous women's fear of natural delivery and their decision on the mode of delivery. Iranian Journal of Nursing and Midwifery Research 2015;20(1):40-6. [CENTRAL: CN-02064641] [PMID: ] [PMC free article] [PubMed] [Google Scholar]
Nosratabadi 2018 {published data only}
- Nosratabadi M, Hekmat K, Dencker A, Abbaspoor Z. Individual and group psycho-educational counseling on knowledge, attitude and preference for birth method in nulliparous women: a randomized controlled trial. Journal of Family and Reproductive Health 2018;12(2):103-10. [CENTRAL: CN-01793866] [EMBASE: 2001516694] [PMC free article] [PubMed] [Google Scholar]
NTR4661 {published data only}
- NTR4661. The effects of the Mindfulness-Based Childbirth and Parenting (MBCP) programme and the Fear of Childbirth Consultation (FCC) programme in pregnant women with fear of childbirth and early parenting (and their partners). https://www.trialregister.nl/trial/4526 (first received 29 June 2014).
Sharifzadeh 2018 {published data only}
- Sharifzadeh M, Haghighi NB, Keramat A, Motaghi Z, Goli M. Effectiveness of midwifery counseling based on solution-focused approaches on fear of childbirth. Koomesh 2018;20(2):375-83. [Google Scholar]
Soltani 2017 {published data only}
- IRCT2015101623640N4. The effect of self-efficacy based consultation on the fear of childbirth among nulliparous women. http://en.irct.ir/trial/20149 (first received 1 June 2016).
- Soltani F, Khodakarami B, Eskandari Z, Parsa P, Roshanaei G. The effect of self-efficacy oriented counselling on controlling the fear of natural delivery in primigravida women. Journal of Pharmaceutical Sciences and Research 2017;9(10):1757-61. [Google Scholar]
TCTR20190501001 2019 {published data only}
- TCTR20190501001. Effect of prenatal care education on spouses of primiparous women, in face-to-face and social network based on Pregnancy Experience and Fear of Child Birth. http://www.clinicaltrials.in.th/index.php?tp=regtrials&menu=trialsearch&smenu=fulltext&task=search&task2=view1&id=4694 (first received 24 April 2019).
Vakilian 2018 {published data only}
- IRCT2014120920259N1. Effectiveness of cognitive-behavioral group therapy focused on self-esteem on fear of childbirth in nulliparous women. http://en.irct.ir/trial/18003 (first received 29 July 2015).
- Vakilian C, Poorjandaghi M, Khorsandi M. The effect of cognitive-behavior group counseling on the self-esteem in nulliparous women: a clinical study. Journal of Clinical Nursing and Midwifery 2018;7(1):67-74. [Google Scholar]
Veringa 2016 {published data only}
- Veringa IK, Bruin EI, Bardacke N, Duncan LG, Steensel FJ, Dirksen CD, et al. 'I've Changed My Mind', Mindfulness-Based Childbirth and Parenting (MBCP) for pregnant women with a high level of fear of childbirth and their partners: study protocol of the quasi-experimental controlled trial. BMC Psychiatry 2016;16(1):377. [DOI] [PMC free article] [PubMed] [Google Scholar]
Werner 2013 {published data only}
- NCT00914082. The effect of mental training on childbirth measured on pain experience and other birth outcomes. https://clinicaltrials.gov/ct2/show/NCT00914082 (first received 4 June 2009).
- Werner A, Uldbjerg N, Zachariae R, Nohr EA. Effect of self-hypnosis on duration of labor and maternal and neonatal outcomes: a randomized controlled trial. Acta Obstetricia et Gynecologica Scandinavica 2013;92(7):816-23. [DOI] [PubMed] [Google Scholar]
- Werner A, Uldbjerg N, Zachariae R, Rosen G, Nohr E. Self-hypnosis for coping with labour pain: a randomised controlled trial. BJOG: an international journal of obstetrics and gynaecology 2013;120(3):346-53. [DOI] [PubMed] [Google Scholar]
- Werner A, Uldbjerg N, Zachariae R, Wu CS, Nohr EA. Antenatal hypnosis training and childbirth experience: a randomized controlled trial. Birth 2013;40(4):272-80. [DOI] [PubMed] [Google Scholar]
Zarenejad 2020 {published data only}
- Zarenejad M, Yazdkhasti M, Rahimzadeh M, Mehdizadeh Tourzani Z, Esmaelzadeh-Saeieh S. The effect of mindfulness-based stress reduction on maternal anxiety and self-efficacy: a randomized controlled trial. Brain and Behavior 2020;10(4):e01561. [CENTRAL: CN-02102508] [EMBASE: 2004401001] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
References to studies awaiting assessment
Firouzan 2020 {published data only}
- Firouzan L, Kharaghani R, Zenoozian S, Moloodi R, Jafari E. The effect of midwifery led counseling based on Gamble’s approach on childbirth fear and self-efficacy in nulligravida women. BMC Pregnancy and Childbirth 2020;20:522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Firouzan L, Kharaghani R, Zenoozian S, Moloodi R, Jafari E. Effectiveness of a psychoeducation intervention by midwives on childbirth fear and childbirth self-efficacy in fearful first time pregnant women: a randomized controlled trial. Research Square 2020.
IRCT2015111625066N1 {published data only}
- IRCT2015111625066N1. Comparison of routine care mindfulness and childbirth preparation classes on the reduction of cesarean delivery rate in nulliparous women who are volunteers for cesarean delivery: a clinical trial. http://en.irct.ir/trial/21036 (first received 21 December 2016).
IRCT201705011113N8 {published data only}
- IRCT201705011113N8. The effects of spouse participation in childbirth preparation classes on fear of childbirth and select the type of delivery in nulliparous women. http://en.irct.ir/trial/148 (first received 10 September 2017).
IRCT20170827035934N2 {published data only}
- IRCT20170827035934N2. The effects of normal delivery education on childbirth fear and cesarean preference in pregnancy and postpartum in women referred to health clinics. http://en.irct.ir/trial/27010 (first received 5 February 2018).
IRCT20170827035934N3 {published data only}
- IRCT20170827035934N3. The effectiveness of group counseling with a solution- focused approach on childbirth fear, pregnancy, anxiety and cesarean preference in women participating in physiologic delivery training classes. http://en.irct.ir/trial/38700 (first received 9 May 2019).
IRCT20170921036302N3 {published data only}
- IRCT20170921036302N3. The effect of the presence of private midwife on anxiety and fear of giving birth in pregnant women referring to Hakim hospital in Neishabour city. http://en.irct.ir/trial/27181 (first received 5 January 2018).
IRCT20180901040916N1 {published data only}
- IRCT20180901040916N1. Investigate the impact of counseling with an approach based on acceptance and commitment therapy to the fear, attitude and intention of choosing the type of delivery in primigravid women. http://en.irct.ir/trial/33795 (first received 13 May 2019).
IRCT20190129042538N1 {published data only}
- IRCT20190129042538N1. Effect of self-hypnosis on fear and pain of normal delivery [Evaluation of self-hypnosis effect on fear and pain of normal delivery in primiparous women]. Http://www.who.int/trialsearch/Trial2.aspx?TrialID=IRCT20190129042538N1 2019. [CENTRAL: CN-02069383]
IRCT20190203042607N1 {published data only}
- IRCT20190203042607N1. The Effectiveness Of Solution-focused Group Counseling on Fear of Childbirth & Self efficacy in Nulliparous Women. http://en.irct.ir/trial/38016 (first received 18 April 2019).
NCT01687907 {published data only}
- NCT01687907. A randomized longitudinal trial about the effects of music on fear of childbirth and outcome of delivery. https://clinicaltrials.gov/ct2/show/NCT01687907 (first received 19 September 2012).
NCT02266186 {published data only}
- NCT02266186. Treatment of severe fear of childbirth with CBT, comparison of ICBT with traditional live therapy. https://clinicaltrials.gov/ct2/show/NCT02266186 (first received 16 October 2014).
NCT04097782 {published data only}
- NCT04173351. The effects of antenatal education and counseling on childbirth fear of nulliparous women [The Effects of Antenatal Education and Counseling on Childbirth Fear of Nulliparous Women and Their Attitudes Towards Childbirth]. Https://clinicaltrials.gov/show/NCT04173351 2019 Nov 21. [CENTRAL: CN-02010064]
NCT04214431 {published data only}
- NCT04214431. Reducing fear of childbirth among pregnant women [Reducing Fear of Childbirth Among Pregnant Women: Women's Lived Experience, Predictors, and Effects of Mindfulness-based Childbirth Education]. Https://clinicaltrials.gov/show/NCT04214431 (first received 31 Dec 2019). [CENTRAL: CN-02048304]
Weng 2016 {published data only}
- Weng H, Duncan L, Cohn M, Cook J, Hecht F, Bardacke N, et al. Mindfulness to alleviate fear and pain in childbirth increases body awareness and decreases pain catastrophizing. Journal of Alternative and Complementary Medicine 2016;22(6):A90. [Google Scholar]
References to ongoing studies
Baas 2017 {published data only}
- Baas MAM, Stramrood CAI, Dijksman LM, Jongh A, Pampus MG. The optiMUM study: EMDR therapy in pregnant women with posttraumatic stress disorder after previous childbirth and pregnant women with fear of childbirth: design of a multicentre randomized controlled trial. European Journal of Psychotraumatology 2017;8(1):1293315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- NTR5122. EMDR in pregnant women with fear of childbirth (FoC). https://www.trialregister.nl/trial/4885 (first received 28 March 2015).
- Pampus MG. EMDR in pregnant women with PTSD after previous childbirth. https://www.trialregister.nl/trial/4886 (first received 30 March 2015).
IRCT20120718010324N43 {published data only}
- IRCT20120718010324N43. The effect of counseling with Beck’s cognitive therapy on anxiety and childbirth fear: a randomized controlled clinical trial. http://en.irct.ir/trial/10817 (first received 10 March 2018).
NCT02972112 {published data only}
- NCT02972112. Ultrashort cognitive behavioral intervention for tokophobia a prospective randomized single blinded controlled trial. https://clinicaltrials.gov/ct2/show/NCT02972112 (first received 23 November 2016).
NCT03393637 {published data only}
- NCT03393637. Mentors Offering Maternal Support (M-O-M-S™): A Prenatal Program Building Maternal Self-Esteem, Coping, and Resilience and Decreasing Depression. https://clinicaltrials.gov/ct2/show/NCT03393637 (first received 8 January 2018).
Additional references
Adams 2012
- Adams SS, Eberhard-Gran M, Eskild A. Fear of childbirth and duration of labour: a study of 2206 women with intended vaginal delivery. BJOG: an international journal of obstetrics and gynaecology 2012;119(10):1238-46. [DOI] [PubMed] [Google Scholar]
Aguila 2021
- Aguila A, Galvez-Lara M, Blanco-Ruiz M, Garica-Torres F. Psychological, educational, and alternative interventions for reducing fear of childbirth in pregnant women: a systematic review. Journal of Clinical Psychology 20/10/2020;77(3):525-555. [PMID: ] [DOI] [PubMed] [Google Scholar]
Airo Toivanen 2018
- Airo Toivanen R, Korja R, Saisto T, Rouhe H, Muotka J, Salmela–Aro K. Changes in emotions and personal goals in primiparous pregnant women during group intervention for fear of childbirth. Journal of Reproductive and Infant Psychology 2018;36(4):363-80. [DOI: 10.1080/02646838.2018.1462477] [DOI] [PubMed] [Google Scholar]
Akgun 2020
- Akgun M, Boz I, Ozer Z. The effect of psychoeducation on fear of childbirth and birth type: systematic review and meta-analysis. Journal of Psychosomatic Obstetrics & Gynaecology 2020;41(4):253-65. [DOI: ] [DOI] [PubMed] [Google Scholar]
Alipour 2012
- Alipour Z, Lamyian M, Hajizadeh E. Anxiety and fear of childbirth as predictors of postnatal depression in nulliparous women. Women and Birth 2012;25(3):e37-43. [DOI] [PubMed] [Google Scholar]
Al Mufti 1997
- Al-Mufti R, McCarthy A, Fisk NM. Survey of obstetricians' personal preference and discretionary practice. European Journal of Obstetrics, Gynaecology and Reproductive Biology 1997;73(1):1-4. [DOI] [PubMed] [Google Scholar]
Americian Psychiatric Association 2013
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (DSM-5). Arlington, VA: American Psychiatric Association, 2013. [Google Scholar]
Andersson 2014
- Andersson G, Cuijpers P, Carlbring P, Riper H, Hedman E. Guided Internet‐based vs. face‐to‐face cognitive behavior therapy for psychiatric and somatic disorders: a systematic review and meta‐analysis. World Psychiatry 2014;13(3):288-95. [DOI] [PMC free article] [PubMed] [Google Scholar]
Antonovsky 1987
- Antonovsky A. The salutogenic perspective: toward a new view of health and illness. Advances 1987;4(1):47-55. [Google Scholar]
Areskog 1981
- Areskog B, Uddenberg N, Kjessler B. Fear of childbirth in late pregnancy. Gynecologic and Obstetric investigation 1981;12(5):262-6. [DOI] [PubMed] [Google Scholar]
Ayers 2016
- Ayers S, Bond R, Bertullies S, Wijma K. The aetiology of post-traumatic stress disorder following childbirth: a meta-analysis and theoretical framework. Psychological Medicine 2016;16:1121-34. [DOI] [PubMed] [Google Scholar]
Beck 1993
- Beck AT, Steer RA. Beck Anxiety Inventory. San Antonio (TX): Harcourt Brace & Company, 1993. [Google Scholar]
Bewley 2002
- Bewley S, Cockburn J. Responding to fear of childbirth. Lancet 2002;359(9324):2128-9. [DOI] [PubMed] [Google Scholar]
Bohren 2014
- Bohren MA, Vogel JP, Hunter EC, Lutsiv O, Makh SK, Souza JP, et al. The mistreatment of women during childbirth in health facilities globally: a mixed-methods systematic review. PLOS Medicine 2015;12(6):e1001847. [DOI] [PMC free article] [PubMed] [Google Scholar]
Brockington 2017
- Brockington I, Butterworth R, Glangeaud-Freudenthal N. An international position paper on mother-infant (perinatal) mental health, with guidelines for clinical practice. Archives of Women's Mental Health 2017;20(1):113-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
Brunton 2015
- Brunton RJ, Dryer R, Saliba A, Kohlhoff J. Pregnancy anxiety: a systematic review of current scales. Journal of Affective Disorders 2015;176:24-34. [DOI: 10.1016/j.jad.2015.01.039] [DOI] [PubMed] [Google Scholar]
Cox 1987
- Cox, J, Holden JM, Sagovsky, R. Detection of postnatal depression: Development of the 10-item Edinburgh Postnatal Depression Scale. British Journal of Psychiatry 1987;150:782-6. [DOI] [PubMed] [Google Scholar]
Dahlen 2010
- Dahlen, H. Undone by fear? Deluded by trust? Midwifery 2010;26(2):156-62. [DOI] [PubMed] [Google Scholar]
Darvill 2010
- Darvill, R, Skirton, H, Farrand, P. Psychological factors that impact on women's experiences of first-time motherhood: a qualitative study of the transition. Midwifery 2010;26(3):357-366. [DOI: ] [DOI] [PubMed] [Google Scholar]
Dennis 2013
- Dennis CL, Dowswell T. Psychosocial and psychological interventions for preventing postpartum depression. Cochrane Database of Systematic Reviews 2013, Issue 2. Art. No: CD001134. [DOI: 10.1002/14651858.CD001134.pub3] [DOI] [PubMed] [Google Scholar]
Dennis 2017
- Dennis CL, Brown HK. Psychosocial, psychological, and pharmacological interventions for treating antenatal anxiety. Cochrane Database of Systematic Reviews 2017, Issue 11. Art. No: CD012870. [DOI: 10.1002/14651858.CD012870] [DOI] [Google Scholar]
Eriksson 2005
- Eriksson C, Westman G, Hamberg K. Experiential factors associated with childbirth-related fear in Swedish women and men: a population based study. Journal of Psychosomatic Obstetrics & Gynecology 2005;26(1):63-72. [DOI] [PubMed] [Google Scholar]
Eriksson 2006
- Eriksson C, Jansson L, Hamberg K. Women's experiences of intense fear related to childbirth investigated in a Swedish qualitative study. Midwifery 2006;22(3):240-8. [DOI] [PubMed] [Google Scholar]
Eriksson 2007
- Eriksson C, Salander P, Hamberg K. Men's experiences of intense fear related to childbirth investigated in a Swedish qualitative study. Journal of Men's Health and Gender 2007;4(4):409-18. [Google Scholar]
Fairbrother 2007
- Fairbrother N, Woody SR. Fear of childbirth and obstetrical events as predictors of postnatal symptoms of depression and post-traumatic stress disorder. Journal of Psychosomatic Obstetrics & Gynecology 2007;28(4):239-42. [DOI] [PubMed] [Google Scholar]
Faisal 2014
- Faisal, I, Matinnia, N, Hejar, AR, Khodakarami, Z. Why do primigravidae request caesarean section in a normal pregnancy? a qualitative study in Iran. Midwifery February 2014;30(2):227-233. [DOI: ] [DOI] [PubMed] [Google Scholar]
Fenwick 2010
- Fenwick, J, Staff, L, Gamble, J, Creedy, D, Bayes, S. Why do women request caesarean section in a normal pregnancy? Midwifery August 2010;26(4):394-400. [DOI: ] [DOI] [PubMed] [Google Scholar]
Fenwick 2015
- Fenwick J, Toohill J, Creedy DK, Smith J, Gamble J. Sources, responses and moderators of childbirth fear in Australian women: a qualitative investigation. Midwifery 2015;31(1):239-46. [DOI] [PubMed] [Google Scholar]
Freedman 2014
- Freedman LP, Kruk ME. Disrespect and abuse of women in childbirth: challenging the global quality and accountability agendas. Lancet. 2014;384(9948):42-4. [DOI] [PubMed] [Google Scholar]
Gao 2015
- Gao LL, Liu XJ, Fu BL, Xie W. Predictors of childbirth fear among pregnant Chinese women: a cross-sectional questionnaire survey. Midwifery 2015;31(9):865-70. [DOI: ] [DOI] [PubMed] [Google Scholar]
Ghazaie 2016
- Ghazaie M, Davoodi I, Neysi A, Mehrabizadeh Honarmand M, Bassak Nejad S. The effectiveness of cognitive-behavioral therapy on fear of childbirth, fear of pain, self-efficacy of childbirth and tendency to caesarean in nulliparous women. Iranian Journal of Obstetrics, Gynecology and Infertility 2016;19(31):1-2. [Google Scholar]
Green 2003
- Green J, Baston HA, Easton S, McCormick F. Greater Expectations? Summary Report. Inter-relationships between women’s expectations and experiences of decision making, continuity, choice and control in labour, and psychological outcomes. Mother & Infant Research Unit, Leeds 1 December 2011.
Greer 2014
- Greer J, Lazenbatt A, Dunne L. 'Fear of childbirth' and ways of coping for pregnant women and their partners during the birthing process: a salutogenic analysis. Evidence Based Midwifery 2014;12(3):95-100. [Google Scholar]
Gutteridge 2013
- Gutteridge K. Who's afraid of the big bad birth? MIDIRS Midwifery Digest April 2013;23(4):441-6. [Google Scholar]
Haines 2012
- Haines HM, Rubertsson C, Pallant JF, Hildingsson I. The influence of women’s fear, attitudes and beliefs of childbirth on mode and experience of birth. BMC Pregnancy and Childbirth 2012;12(1):55. [DOI: 10.1186/1471-2393-12-55] [DOI] [PMC free article] [PubMed] [Google Scholar]
Hall 2009
- Hall WA, Hauck YL, Carty EM, Hutton EK, Fenwick J, Stoll K. Childbirth fear, anxiety, fatigue, and sleep deprivation in pregnant women. Journal of Obstetric, Gynecologic, and Neonatal Nursing 2009;38(5):567-76. [DOI] [PubMed] [Google Scholar]
Higgins 2011
- Higgins JP, Green S, editors. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from www.cochrane-handbook.org.
Higgins 2021
- Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al (editors). Cochrane Handbook for Systematic Reviews of Interventions version 6.2 (updated February 2021). Cochrane, 2021. Available from www.training.cochrane.org/handbook.
Hildingsson 2018
- Hildingsson I, Rubertsson C, Karlström A, Haines H. Caseload midwifery for women with fear of birth is a feasible option. Sexual & Reproductive Healthcare 2018;1(16):50-5. [DOI] [PubMed] [Google Scholar]
Hofberg 2003
- Hofberg K, Ward MR. Fear of pregnancy and childbirth. Postgraduate Medical Journal 2003;79(935):505-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
Howard 2014
- Howard LM, Molyneaux E, Dennis CL, Rochat T, Stein A, Milgrom J. Non-psychotic mental disorders in the perinatal period. Lancet 2014;384(9956):1775-88. [DOI] [PubMed] [Google Scholar]
Hull 2011
- Hull, PM, Bedwell CT. Why do some women prefer birth by caesarean? An Internet survey. British Journal of Midwifery 2011;19:708-17. [Google Scholar]
Jomeen 2021
- Jomeen J, Martin CR, Jones C, Marshall C, Ayers S, Burt K, et al. Tokophobia and fear of birth: a workshop consensus statement on current issues and recommendations for future research. Journal of Reproductive and Infant Psychology 2021;39(1):2-15. [DOI] [PubMed] [Google Scholar]
Karlström 2009
- Karlström A, Engström-Olofsson R, Nystedt A, Thomas J, Hildingsson I. Swedish caregivers’ attitudes towards caesarean section on maternal request. Women and Birth 2009;22(2):57-63. [DOI] [PubMed] [Google Scholar]
Larkin 2009
- Larkin P, Begley CM, Devane D. Women's experiences of labour and birth: An evolutionary concept analysis. Midwifery 2009;25(2):e49-59. [DOI: ] [DOI] [PubMed] [Google Scholar]
Larsson 2016
- Larsson B, Karlström A, Rubertsson C, Hildingsson I. Counseling for childbirth fear–a national survey. Sexual & Reproductive Healthcare 2016;8:82-7. [DOI] [PubMed] [Google Scholar]
Larsson 2017
- Larsson B. Treatment for Childbirth Fear with a Focus on Midwife-led Counselling: A National Overview, Women’s Birth Preferences and Experiences of Counselling [Doctoral dissertation]. Uppsala, Sweden: Acta Universitatis Upsaliensis, 2017. [Google Scholar]
Larsson 2018
Laursen 2008
- Laursen M, Hedegaard M, Johansen C. Fear of childbirth: predictors and temporal changes among nulliparous women in the Danish National Birth Cohort. BJOG: an international journal of obstetrics and gynaecology 2008;115(3):354-60. [DOI] [PubMed] [Google Scholar]
Logtenberg 2018
- Logtenberg SL, Verhoeven CJ, Rengerink KO, Sluijs AM, Freeman LM, Schellevis FG, et al. Pharmacological pain relief and fear of childbirth in low risk women; secondary analysis of the RAVEL study. BMC Pregnancy and Childbirth 2018;18(1):347. [DOI] [PMC free article] [PubMed] [Google Scholar]
Lowe 2000
- Lowe NK. Self-efficacy for labor and childbirth fears in nulliparous pregnant women. Journal of Psychosomatic Obstetrics & Gynecology 2000;21(4):219-24. [DOI] [PubMed] [Google Scholar]
Lyberg 2010
- Lyberg A, Severinsson E. Midwives' supervisory styles and leadership role as experienced by Norwegian mothers in the context of a fear of childbirth. Journal of Nursing Management 2010;18(4):391-9. [DOI] [PubMed] [Google Scholar]
Marc 2011
- Marc I, Toureche N, Ernst E, Hodnett ED, Blanchet C, Dodin S, et al. Mind‐body interventions during pregnancy for preventing or treating women's anxiety. Cochrane Database of Systematic Reviews 2011, Issue 7. Art. No: CD007559. [DOI: 10.1002/14651858.CD007559.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Martin 2021
- Martin C, Jones C, Marshall CA, Huang C, Reeve J, Fleming MP et al. Fear of childbirth measurement: appraisal of the content overlap of four instruments. Journal of Reproductive and Infant Psychology 2021;39(1):1-13. [DOI] [PubMed] [Google Scholar]
Melender 2002
- Melender HL. Experiences of fears associated with pregnancy and childbirth: a study of 329 pregnant women. Birth 2002;29(2):101-11. [doi.org/10.1046/j.1523-536X.2002.00170.x] [DOI] [PubMed] [Google Scholar]
Miller 2010
- Miller E, Decker MR, McCauley HL, Tancredi DJ, Levenson RR, Waldman J, et al. Pregnancy coercion, intimate partner violence and unintended pregnancy. Contraception April 1;81(4):316-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
Moghaddam Hosseini 2017
- Moghaddam Hosseini V, Nazarzadeh M, Jahanfar S. Interventions for reducing fear of childbirth: A systematic review and meta-analysis of clinical trials. Women and Birth 2017;31(4):254-62. [DOI: ] [DOI] [PubMed] [Google Scholar]
Nath 2018
- Nath S, Ryan EG, Trevillion K, Bick D, Demilew J, Milgrom J, et al. Prevalence and identification of anxiety disorders in pregnancy: the diagnostic accuracy of the two-item Generalised Anxiety Disorder scale (GAD-2). BMJ Open 2018;8:e023766. [DOI] [PMC free article] [PubMed] [Google Scholar]
Nieminen 2015
- Nieminen K, Malmquist A, Wijma B, Ryding EL, Andersson G, Wijma K. Nulliparous pregnant women's narratives of imminent childbirth before and after internet-based cognitive behavioural therapy for severe fear of childbirth: a qualitative study. BJOG: an international journal of obstetrics and gynaecology 2015;122(9):1259-65. [DOI] [PubMed] [Google Scholar]
Nilsson 2009
- Nilsson C, Lundgren I. Women's lived experience of fear of childbirth. Midwifery 2009;25(2):e1-9. [DOI] [PubMed] [Google Scholar]
Nilsson 2018
- Nilsson C, Hessman E, Sjöblom H, Dencker A, Jangsten E, Mollberg M, et al. Definitions, measurements and prevalence of fear of childbirth: a systematic review. BMC Pregnancy and Childbirth 2018;18(1):28. [DOI] [PMC free article] [PubMed] [Google Scholar]
O'Connell 2017
- O'Connell MA, Leahy‐Warren P, Khashan AS, Kenny LC, O'Neill SM. Worldwide prevalence of tocophobia in pregnant women: systematic review and meta‐analysis. Acta Obstetricia et Gynecologica Scandinavica 2017;96(8):907-20. [DOI: ] [DOI] [PubMed] [Google Scholar]
O'Donovan 2018
- O'Donovan C, O'Donovan J. Why do women request an elective cesarean delivery for non‐medical reasons? A systematic review of the qualitative literature. Birth 2018;45(2):109-19. [DOI: 10.1111/birt.12319] [DOI] [PubMed] [Google Scholar]
Priddis 2013
- Priddis H, Dahlen HG, Schmied V, Sneddon A, Kettle C, Brown C, et al. Risk of recurrence, subsequent mode of birth and morbidity for women who experienced severe perineal trauma in a first birth in New South Wales between 2000–2008: a population based data linkage study. BMC Pregnancy & Childbirth 2013;13:89. [DOI] [PMC free article] [PubMed] [Google Scholar]
Räisänen 2014
- Räisänen S, Lehto SM, Nielsen HS, Gissler M, Kramer MR, Heinonen S. Fear of childbirth in nulliparous and multiparous women: a population‐based analysis of all singleton births in Finland in 1997–2010. BJOG: an international journal of obstetrics and gynaecology 2014;121(8):965-70. [DOI] [PubMed] [Google Scholar]
Review Manager 2014 [Computer program]
- The Nordic Cochrane Centre, The Cochrane Collaboration Review Manager 5 (RevMan 5). Version 5.3. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2014.
Richens 2015
- Richens Y, Hindley C, Lavender T. A national online survey of UK maternity unit service provision for women with fear of birth. British Journal of Midwifery 2015;23(8):574-9. [Google Scholar]
Roesch 2004
- Roesch, SC, Dunkel-Schetter, C, Woo, G, Hobel, CJ. Modeling the types of and timing of stress in pregnancy. Anxiety, Stress, Coping 2004;17:87-102. [Google Scholar]
Rondung 2016
- Rondung E, Thomtén J, Sundin Ö. Psychological perspectives on fear of childbirth. Journal of Anxiety Disorders 2016;44:80-91. [DOI] [PubMed] [Google Scholar]
Rouhe 2011
- Rouhe H, Salmela-Aro K, Gissler M, Halmesmäki E, Saisto T. Mental health problems common in women with fear of childbirth. BJOG: an international journal of obstetrics and gynaecology 2011;118(9):1104-11. [DOI] [PubMed] [Google Scholar]
Ryding 2003
- Ryding EL, Persson A, Onell C, Kvist L. An evaluation of midwives' counseling of pregnant women in fear of childbirth. Acta Obstetricia et Gynecologica Scandinavica 2003;82(1):10-7. [DOI] [PubMed] [Google Scholar]
Ryding 2015
- Ryding EL, Lukasse M, Parys AS, Wangel AM, Karro H, Kristjansdottir H, et al. Fear of childbirth and risk of cesarean delivery: a cohort study in six European countries. Birth 2015;42(1):48-55. [DOI] [PubMed] [Google Scholar]
Saisto 2001
- Saisto T, Salmela‐Aro K, Nurmi JE, Halmesmäki E. Psychosocial characteristics of women and their partners fearing vaginal childbirth. BJOG: an international journal of obstetrics and gynaecology 2001;108(5):492-8. [DOI] [PubMed] [Google Scholar]
Saisto 2001 A
- Saisto T, Kaaja R, Ylikorkala O, Halmesmäki E. Reduced pain tolerance during and after pregnancy in women suffering from fear of labor. Pain 2001;93(2):123-7. [DOI] [PubMed] [Google Scholar]
Salomonsson 2010
- Salomonsson B, Wijma K, Alehagen S. Swedish midwives’ perceptions of fear of childbirth. Midwifery 2010;26(3):327-37. [DOI] [PubMed] [Google Scholar]
Shou 2017
- Shou H, Yang Z, Satterthwaite TD, Cook PA, Bruce SE, Shinohara RT, et al. Cognitive behavioral therapy increases amygdala connectivity with the cognitive control network in both MDD and PTSD. NeuroImage: Clinical 2017;14:464-70. [DOI] [PMC free article] [PubMed] [Google Scholar]
Sjogren 1997
- Sjogren B. Reasons for anxiety about childbirth in 100 pregnant women. Journal of Psychosomatic Obstetrics & Gynecology 1997;18:266-72. [DOI] [PubMed] [Google Scholar]
Slade 2020
- Slade P, Balling K, Sheen K, Houghton G. Identifying fear of childbirth in a UK population: qualitative examination of the clarity and acceptability of existing measurement tools in a small UK sample. BMC Pregnancy and Childbirth 2020;20(1):1-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
Slade 2021
- Slade P, Balling K, Houghton G, Sheen K. A new scale for fear of childbirth: the Fear of Childbirth Questionnaire (FCQ). Journal of Reproductive and Infant Psychology 2021;39:1-11. [DOI: ] [DOI] [PubMed] [Google Scholar]
Smith 2019
- Smith V, Gallagher L, Carroll M, Hannon K, Begley C. Antenatal and intrapartum interventions for reducing caesarean section, promoting vaginal birth, and reducing fear of childbirth: an overview of systematic reviews. PloS One 2019;14(10):e0224313. [DOI] [PMC free article] [PubMed] [Google Scholar]
Stoll 2018
- Stoll K, Swift EM, Fairbrother N, Nethery E, Janssen P. A systematic review of nonpharmacological prenatal interventions for pregnancy-specific anxiety and fear of childbirth. Birth 2018;45(1):7-18. [DOI] [PubMed] [Google Scholar]
Storksen 2012
- Storksen HT, Eberhard-Gran M, Garthus-Niegel SU, Eskild A. Fear of childbirth; the relation to anxiety and depression. Acta Obstetricia et Gynecologica Scandinavica 2012;91(2):237-42. [DOI] [PubMed] [Google Scholar]
Striebich 2018
- Striebich S, Mattern E, Ayerle GM. Support for pregnant women identified with fear of childbirth (FOC)/tokophobia - a systematic review of approaches and interventions. Midwifery 2018;61:97-115. [DOI] [PubMed] [Google Scholar]
Sullivan 2001
- Sullivan MJ, Thorn B, Haythornthwaite JA, Keefe F, Martin M, Bradley LA, et al. Theoretical perspectives on the relation between catastrophizing and pain. Clinical Journal of Pain 2001;17(1):52-64. [DOI] [PubMed] [Google Scholar]
Ternström 2015
- Ternström E, Hildingsson I, Haines H, Rubertsson C. Higher prevalence of childbirth related fear in foreign born pregnant women--findings from a community sample in Sweden. Midwifery 2015;31(4):445-50. [DOI] [PubMed] [Google Scholar]
Ternström 2016
- Ternström E, Hildingsson I, Haines H, Rubertsson C. Pregnant women's thoughts when assessing fear of birth on the Fear of Birth Scale. Women and Birth 2016;29(3):e44-9. [DOI] [PubMed] [Google Scholar]
Toohill 2014
- Toohill J, Fenwick J, Gamble J, Creedy DK, Buist A, Turkstra E, et al. A randomized controlled trial of a psycho‐education intervention by midwives in reducing childbirth fear in pregnant women. Birth 2014;41(4):384-94. [DOI] [PMC free article] [PubMed] [Google Scholar]
Weaver 2013
- Weaver J, Browne J, Aras-Payne A, Magill-Cuerden J. A comprehensive systematic review of the impact of planned interventions offered to pregnant women who have requested a caesarean section as a result of tokophobia (fear of childbirth). JBI Database of Systematic Reviews and Implementation Reports 2013;11(1):70-122. [DOI] [PubMed] [Google Scholar]
Wijma 1998
- Wijma K, Wijma B, Zar M. Psychometric aspects of the W-DEQ; a new questionnaire for the measurement of fear of childbirth. Journal of Psychosomatic Obstetrics & Gynecology 1998;19(2):84-97. [DOI] [PubMed] [Google Scholar]
World Health Organization 2018
- World Health Organization. The ICD-10-CM Official Guidelines for Coding and Reporting. Geneva: World Health Organization, 2018. [Google Scholar]
Zar 2001
- Zar M, Wijma K, Wijma B. Pre-and postpartum fear of childbirth in nulliparous and parous women. Scandinavian Journal of Behaviour Therapy 2001;30(2):75-84. [Google Scholar]
Zigmond 1983
- Zigmund, AS, Snaith, RP. The hospital anxiety and depression scale. Acta Psychiatrica Scandinavica 1983;67:361-70. [DOI] [PubMed] [Google Scholar]
References to other published versions of this review
O'Connell 2019
- O'Connell MA, O'Neill SM, Dempsey E, Khashan AS, Leahy‐Warren P, Smyth RMD, Kenny LC. Interventions for fear of childbirth (tocophobia). Cochrane Database of Systematic Reviews 2019, Issue 5. Art. No: CD013321. [DOI: 10.1002/14651858.CD013321] [DOI] [PMC free article] [PubMed] [Google Scholar]


