Abstract
Background
During the COVID-19 pandemic, the health professionals who are at the frontline of this crisis have been facing extreme psychological disorders. This research aims to provide an overall scenario of the prevalence of depression, anxiety, stress, as well as insomnia and to inspect the changes in these prevalence over time by analyzing the existing evidence during this COVID-19 pandemic.
Methods
A systematic search was performed on March 30, 2021, in PubMed, MEDLINE, Google Scholar databases, and Web of Science. To assess the heterogeneity, Q-test, statistics, and Meta regression and to search for the publication bias, Eggers's test and funnel plot were used. The random-effect model and subgroup analysis were performed due to the significant heterogeneity.
Results
Among eighty-three eligible studies in the final synthesis, 69 studies (n = 144649) assessed the depression prevalence of 37.12% (95% CI: 31.80–42.43), 75 studies (n = 147435) reported the anxiety prevalence of 41.42% (95% CI: 36.17–46.54), 41 studies (n = 82783) assessed the stress prevalence of 44.86% (95% CI: 36.98–52.74), 21 studies (n = 33370) enunciated the insomnia prevalence of 43.76% (95% CI: 35.83–51.68). The severity of the mental health problems among health professionals increased over the time during January 2020 to September 2020.
Limitations
A significant level of heterogeneity was found among psychological measurement tools and across studies.
Conclusions
Therefore, it is an emergency to develop psychological interventions that can protect the mental health of vulnerable groups like health professionals.
Keywords: COVID-19, Depression, Anxiety, Stress, Insomnia, Meta-analysis, Health professionals
Highlights
-
•
The Coronavirus (COVID-19) pandemic has caused unprecedented risks to mental health among health workers globally.
-
•
The prevalence of mental health disorder namely depression, anxiety, stress, and insomnia were significantly increased over the time from January 2020 to September 2020 among the teams working closer to infected patients.
-
•
Comparatively higher prevalence of depression, anxiety, stress, and insomnia were observed from previous studies on medical health professionals during COVID-19 pandemic.
-
•
It is an emergency to develop psychological interventions that can protect the mental health of vulnerable groups like health professionals.
COVID-19; Depression; Anxiety; Stress; Insomnia; Meta-analysis; Health professionals.
1. Introduction
Since the first case was observed in December 2019 in Wuhan, the novel coronavirus has become a global health threat [1] by spreading among all the countries of the world [2, 3]. Afterward, the disease caused by the novel coronavirus (2019-nCoV) was named COVID-19 and declared a pandemic by the WHO [4, 5]. Though in recent times, many regions of the world have been experiencing eventually less transmission [1], the psychological crisis may insist for months or years [6]. Several studies showed that COVID-19 is highly associated with mental health problems in the general population and medical health workers. The health care workers are considered as the front liner for privation and controlling the current pandemic and taking care of a large number of infected and suspected patients [7]. “The COVID-19 pandemic has reminded us of the vital role health workers play to relieve suffering and save lives,” said Dr. Tedros Adhanom Ghebreyesus, WHO Director-General. Despite having a high risk of getting infected by the COVID-19, health workers are constantly providing services with huge work pressure and negative emotional stress. This breakneck and dubious environment and traumatic situations have an impact not only on the health professionals, but also, their family members, friends, and colleagues. This psychological crisis among health personals is instigated by fear, mental distress, anxiety, depression, and insomnia [8, 9, 10]. During this pandemic, health workers lost their lives not only from the virus itself but also from cardiac arrest and other conditions caused by being overworked, depressed, and having insomnia. Thus, as the most vulnerable group of being affected in direct dealing with coronavirus, the physical and mental health of health professionals deserve extensive attention [9].
During the pandemic, plenty of studies have been carried out to investigate the prevalence of clinical symptoms namely emotional distress, depression, stress, mood swings, irritability, insomnia, attention deficit hyperactivity disorder, post-traumatic stress in different countries or territories. However, the prevalence estimates differ remarkably from place to place and time to time, and from population to population. As the available studies showed different findings all over the world for the impact of the COVID-19 pandemic on mental health, a meta-analysis will be reasonable to understand the overall picture of the prevalence of depression, anxiety, stress, and insomnia among health care workers.
Though few systematic reviews and meta-analyses had been done on this, all the studies included very few articles and were mostly collected only from China. A meta-analysis and systematic review of 19 studies [11] considered studies that were conducted only in China. A systematic review with 29 studies (21 studies from China and 8 studies from 6 other countries) observed the prevalence of depression anxiety and stress among frontline healthcare workers [12]. Another meta-analysis and systematic review [13] of 12 studies was conducted that included studies only from China (11 studies) and Singapore (1 study). Mental health was considered in a meta-analysis of 12 studies among Chinese health workers [14]. Furthermore, several systematic reviews and meta-analyses [15, 16, 17, 18] were also conducted to inspect the prevalence of clinical symptoms such as depression, anxiety, sleep disturbance, and stress among the general population. However, not a single of the studies did inspect the variation over time in the prevalence of depression, anxiety, stress, and insomnia. Hence, we decided to conduct an extensive systematic review and meta-analysis by considering a large number of studies on the prevalence of those mental health problems among health care workers during the COVID-19 pandemic. Our vision also is to sketch the changes in the prevalence of depression, anxiety, stress, and insomnia among health professionals during the pandemic.
2. Methods
This systematic review was conducted and recoded according to the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) Statement [19].
2.1. Search strategy and selection criteria
This comprehensive systematic review of published research papers on the prevalence of depression, anxiety, stress, and insomnia among health professionals during the COVID-19 pandemic was conducted by searching the following databases: PubMed, MEDLINE, Google Scholar, and Web of Science. The searches were performed on March 30, 2021, using the keywords “Coronavirus”, “COVID-19”, “SARS-Cov-2”, “Mental health problem”, “Mental health condition”, “Depression”, “Anxiety”, “Stress”, “Insomnia”, “Health care workers”, “Health professionals” and all possible combination of keywords were used.
(((((((((((((Coronavirus [Title]) OR (COVID-19 [Title])) OR (SARS-cov- [Title])) AND (2019-ncov [Title])) AND (Mental health problem [Title])) OR (Mental health condition [Title])) AND (Depression [Title])) OR (Anxiety [Title])) OR (Stress [Title])) OR (Insomnia [Title])) AND (health professionals [Title])) OR (Health care worker [Title]))))))))))))
For maximizing the comprehensiveness of the study, the list of article references was manually reviewed. However, we considered only those studies published in English, and no time and geographical constraints were imposed in the searching procedure. The preprints published on medrxiv, PsyArXiv, bioRxiv, and SSRN were also considered due to the rapid transmission of the information during the COVID-19 pandemic. All the identified research articles were transformed into EndNote (Version X8.1) reference management software.
2.2. Inclusion/exclusion criteria
Studies that satisfied the following criteria were included in the review: 1) the prevalence of stress/anxiety/depression/insomnia among healthcare workers during the COVID-19 pandemic, 2) written in English, 3) observational study (non-interventional study), 4) studies with available full text. The exclusion criteria were considered as follows: 1) unrelated topic, 2) studies without sufficient data such as where study site, study period, and sample size were not reported clearly, 3) more than one sources, 4) interventional studies/case reports/Editorial comments/Letters to Editor, etc. 5) articles that do not contain at least one of the information of depression, anxiety, stress, and insomnia, and 6) articles for that the full text is not available.
2.3. Study selection
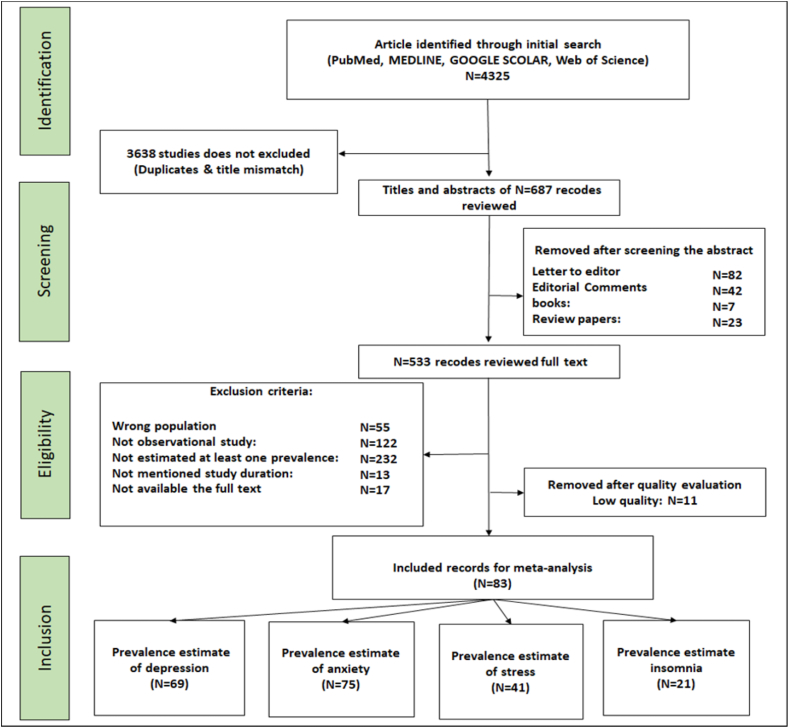
The study selection processes are sketched as follows (Figure 1). Initially, we identified articles according to PRISMA guidelines and listed them in Endnote (version X.8). In the next stage, the titles and abstracts were screened and the unrelated articles to the topics or duplicates records were removed. Then, in the eligibility checking stage, we examined the full text and skipped some articles because of not having the relevant information. In the last or final stage, all articles selected in the previous stages were reviewed or checked for quality assessment and the low-quality studies were removed.
Figure 1.
Flowchart describing the search strategy and inclusion/exclusion of studies by following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA 2009) guidelines.
2.4. Quality evaluation
The quality evaluation was carried out using the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statements by two independent reviewers (AM and SH) along with the help of a third reviewer (SM) in case of any disagreement. The STROBE checklists contain a total of 32 scales that can be organized into six general sections/scales such as title, abstract, introduction, methods, results, and discussion. These checklists are commonly used to evaluate the quality of the observational studies in a sense of methodological aspect including sampling and data collection approaches, study population, study design, statistical methods, and so on. The maximum possible score for STROBE checklists is 32, studies with a quality evaluation score less than 14 using STROBE checklists were excluded by considering 14 as a cut-off point [15, 16].
2.5. Screening and extraction
Two investigators (SM and SH) independently screened and extracted data from selected articles using standardized abstraction sheets following a predefined protocol. The following information was extracted from eligible studies: first author and published year; population size; study period; response rate; geographical region (study location); ration of respondents (Doctors, nurses, others); the percentage of male in the sample; psychological assessment tools (GAD-7, PHQ-9, ISI, DASS-21, etc.) and cut-point for each of the tools; and prevalence measure of depression, anxiety, stress, and insomnia.
2.6. Statistical analysis
In this systematic review and meta-analysis, the data analysis was done by using Stata 16 statistical software version [20]. The Q-test and statistics [21] with a 5% level of significance were applied to assess the heterogeneity of the included studies. The random-effects model was used in case of significant heterogeneity. The Eggers’ test and funnel plot were used to search for publication bias. The subgroup analysis also was conducted by the study duration and assessment tools. To inspect the trend in psychological morbidities we inspected the prevalence of depression, anxiety, stress, and insomnia after every three months. In the article searching steps, we included studies that were conducted between January 2020 to September 2020. Then we classified all the studies into three groups: January 2020 to March 2020, April 2020 to June 2020, July 2020 to September 2020. We also used Meta-regression [22, 23] to observe the association between study duration and prevalence of psychological morbidity (prevalence of depression, anxiety, stress, and insomnia).
2.7. Ethical standards disclosure
This study depended on the examination of previous relevant research studies on the mental health of health professionals during COVID-19. The systematic review was done by considering all standard formats of doing systematic review given https://link.springer.com/chapter/10.1007/978-3-658-27602-7_3. This study only applies to medical health professionals and only considering mental health issues. This study removed all types of biases and provide maximum transparency of research findings to the audience.
3. Results
In this systematic review and meta-analysis, the prevalence of depression, anxiety, stress, and insomnia were assessed during the COVID-19 pandemic among health professionals. The PRISMA guidelines were followed for collecting and reviewing the articles in this focus. In the initial search, we identified 4325 articles, then 3638 articles were removed that were unrelated to the topics or duplicate records after screening the titles and abstracts. Next, the full texts were examined for the remaining 533 articles and 436 records were skipped because of not having the relevant information. The rest of the articles were reviewed or checked for quality and 11 studies were excluded due to the low quality. After the quality evaluation, 86 studies entered into the meta-synthesis. The article searching and selecting processes were demonstrated in the Flow Diagram following the PRISMA statements (Figure 1).
3.1. Study design
The studies selected for the final analysis are observational studies with a cross-sectional study design.
3.2. Study characteristics
Table 1 abbreviates the characteristics of the selected studies [2,8,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75,76,77,78,79,80,81,82,83,84,85,86,87,88,89,90,91,92,93,94,95,96,97,98,99,100,101,102,103,104], 30 of which were from China, 6 from Italy, 6 from India, 4 from the United States, 3 from each of Pakistan and Iran, 2 from each of the country: Canada, Bangladesh, Egypt, Oman, Spain, Turkey, United Kingdom, 1 study from each of the country: Australia, Croatia, Finland, Germany, Ghana, Greek, Jordan, Korea, Lebanon, Nepal, Philippines, Poland, Singapore, South Korea, Vietnam, 1 jointly from Singapore and India, and another 1 jointly from Egypt and Saudi Arabia. The characteristics of the included articles were described by Study duration, Study type, First authors and year of publication, Study population, Response rate (%), Region, Physicians (%), Nurses (%), Other health professionals (%), Male (%), Assessment tools with Cut-off pint. A total of 83 studies along with an average of 78.01% response rate and with 160477 participants were considered for the final analysis. The median number of respondents was 668 (range 57–44992) with a median response rate of 90.7% (range 15–100). Among the total participants, on an average, 37.51% (median = 30.28%, range: 0%–100%) were physicians, 50.16% (median = 46.75%, range: 0%–100%) were nurses, and 30.33% (median = 29.66%, range: 0%–82%) were other health professionals. Also, among all the health professionals who participated, 29.97% were male. The average STROBE score was 21.54 with a median score of 22 (range: 15–28).
Table 1.
Characteristics of the included studies.
| Author | Duration | Study type | Study population | Response rate | Region | Physicians % | Nurses % | Other % | Male % | Assessment tools with cut-off points | STROBE score | Depression % (95% CI) | Anxiety % (95% CI) | Stress % (95% CI) | Insomnia % (95% CI) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Guo et al. (2020) [45] | February, 2020 | Cross-sectional | 11118 | N.A. | China | 30.28 | 53.07 | 16.65 | 25.2 | SDS ≥ 50 SAS ≥ 50 | 26 | 13.4 (12.77–14.03) | 4.98 (4.58–5.38) | N.A. | N.A. |
| Huang and Zhao (2020) [49] | Feb 3-Feb 17, 2020 | Cross-sectional | 7236 | 85.3 | China | N.A. | N.A. | N.A. | 45.4 | CES-D ≥ 28 GAD-7 ≥ 9 PSQI > 7 | 22 | 20.1 (19.18–21.02) | 35.1 (34–36.2) | N.A. | 18.2 (17.31–19.09) |
| Lai et al. (2020) [54] | Jan 29-Feb 3, 2020 | Cross-sectional | 1257 | 68.7 | China | 39.2 | 60.8 | 0 | 23.3 | PHQ-9 ≥ 5 GAD-7 ≥ 5 IES-R ≥ 9 ISI ≥ 8 | 24 | 50.4 (47.64–53.16) | 44.6 (41.85–47.35) | 71.5 (69–74) | 34 (31.38–36.62) |
| Liu et al. (2020a) [61] | Feb 10-Feb 20, 2020 | Cross-sectional | 512 | 85.4 | China | N.A. | N.A. | N.A. | 15.4 | SAS ≥ 50 | 23 | N.A. | 12.5 (9.64–15.36) | N.A. | N.A. |
| Lu et al. (2020) [64] | Feb 25–26, 2020 | Cross-sectional | 2299 | 94.88 | China | 88.8 | N.A. | 11.2 | 22.4 | HAM-D ≥ 7 HAM-A ≥ 7 | 17 | 11.8 (10.48–13.12) | 22.6 (20.89–24.31) | N.A. | N.A. |
| Qi et al. (2020) [75] | February, 2020 | Cross-sectional | 1306 | 93.6 | China | N.A. | N.A. | N.A. | 19.6 | AIS >6 | 20 | N.A. | N.A. | N.A. | 45.5 (42.8–48.2) |
| Zhang et al. (2020a) [2] | Jan 29-Feb 3, 2020 | Cross-sectional | 1563 | N.A. | China | 29 | 62.9 | 8.1 | 13.5 | PHQ-9 ≥ 5 GAD-7 ≥ 5 IES-R ≥ 9 ISI ≥ 8 | 22 | 50.7 (48.22–53.18) | 44.7 (42.24–47.16) | 73.4 (71.21–75.59) | 36.1 (33.72–38.48) |
| Zhang et al. (2020c) [8] | Feb 19-Mar 6, 2020 | Cross-sectional | 2182 | N.A. | China | 31.2 | 11.3 | 57.5 | 35.8 | PHQ-2 ≥ 3 GAD-2 ≥ 3 ISI >8 | 22 | 10.6 (9.31–11.89) | 10.4 (9.12–11.68) | N.A. | 33.9 (31.91–35.89) |
| Zhu et al. (2020a) [97] | Feb 8–10, 2020 | Cross-sectional | 5062 | 77.1 | China | 19.8 | 67.5 | 12.7 | 15 | PHQ-9 ≥ 10 GAD-7 ≥ 8 IES-R ≥ 33 | 22 | 13.45 (12.51–14.39) | 24.06 (22.88–25.24) | 29.8 (28.54–31.06) | N.A. |
| Chew et al. (2020) [34] | Feb 19-April 17, 2020 | Cross-sectional | 906 | 90.6 | Singapore and India | 29.6 | 39.2 | 31.2 | 35.7 | DASS-21 > 9 DASS-21 > 7 DASS-21 > 14 | 16 | 10.6 (8.6–12.6) | 15.7 (13.33–18.07) | 5.2 (3.75–6.65) | N.A. |
| Mrklas et al. (2020) [69] | Mar 23-May 4, 2020 | Cross-sectional | 44992 | 19.4 | Canada | N.A. | N.A. | N.A. | 13.8 | PHQ-9 ≥ 10 GAD-7 ≥ 10 PSS ≥ 14 | 22 | 44 (43.54–44.46) | 47.47 (47.01–47.93) | 85.6 (85.28–85.92) | N.A. |
| Xing et al. (2020) [93] | February 7 to February 21, 2020 | Cross-sectional | 309 | 100 | China | 12.3 | 88.7 | N.A. | 2.6 | SDS ≥ 53 SAS ≥ 50 | 23 | 56 (50.47–61.53) | 28.5 (23.47–33.53) | N.A. | N.A. |
| Huang et al. (2020) [101] | Feb 7–9, 2020 | Cross-sectional | 364 | 96.55 | China | N.A. | N.A. | N.A. | 41.2 | SAS ≥ 50 | 21 | N.A. | 23.4 (19.05–27.75) | N.A. | N.A. |
| Pan et al.(2020) [102] | Feb 7–21, 2020 | Cross-sectional | 194 | 97 | China | 21.6 | 76.3 | 2.1 | 18.6 | PHQ-9 ≥ 5 GAD-7 ≥ 5 | 22 | 37.6 (30.78–44.42) | 32.5 (25.91–39.09) | N.A. | N.A. |
| AraçI & Dönmezdil (2020) [85] | 13-Mar-20 | Cross-sectional | 210 | 94.28 | Turkey | 32.32 | 35.85 | 31.83 | 60.61 | HADS> 11 HADS> 11 | 25 | 31.31 (25.04–37.58) | 39.39 (32.78–46) | N.A. | N.A. |
| Alshekaili et al. (2020) [27] | 8–17 Apr, 2020 | Cross-sectional | 1139 | N.A. | Oman | 33.7 | 39.5 | 26.8 | 20 | DASS-21 ≥ 10 DASS-21 ≥ 8 DASS-21 ≥ 16 ISI ≥ 14 | 21 | 32.3 (29.58–35.02) | 34.1 (31.35–36.85) | 23.8 (21.33–26.27) | 18.5 (16.24–20.76) |
| Khanal et al. (2020) [53] | Apr 26- May 12, 2020 | Cross-sectional | 475 | N.A. | Nepal | 33.9 | 35.2 | 30.9 | 47.4 | HADS> 7 HADS> 7 ISI> 7 | 26 | 37.5 (33.15–41.85) | 41.9 (37.46–46.34) | N.A. | 33.9 (29.64–38.16) |
| Elkholy et al. (2020) [24] | Apr–May, 2020 | Cross-sectional | 502 | N.A. | Egypt | 60 | 16.1 | 23.9 | 50 | PHQ-9 ≥ 5 GAD-7 ≥ 5 PSS ≥ 9 ISI ≥ 8 | 24 | 77.2 (73.53–80.87) | 76.4 (72.69–80.11) | 80.9 (77.46–84.34) | 67.7 (63.61–71.79) |
| Smith et al. (2020) [84] | Apr 07 - May 13, 2020 | Cross-sectional | 7298 | 82.04 | Canada | N.A. | N.A. | N.A. | 9 | PHQ-2 ≥ 3 GAD-2 ≥ 3 | 24 | 42.3 (41.17–43.43) | 54.8 (53.66–55.94) | N.A. | N.A. |
| Liang et al. (2020) [60] | Feb 14- Mar 29, 2020 | Cross-sectional | 899 | 81.43 | China | 24.91 | 45.16 | 29.93 | 18.69 | PHQ-9 ≥ 5 GAD-7 ≥ 5 ISI≥ 8 | 20 | 82.53 (80.05–85.01) | 61.4 (58.22–64.58) | N.A. | 43.04 (39.8–46.28) |
| Prasad et al. (2020) [74] | Apr 14–25, 2020 | Cross-sectional | 347 | N.A. | United States | N.A. | 71.5 | 28.5 | 9.2 | PHQ-2 ≥ 3 GAD-7 ≥ 5 IES≥ 9 | 25 | 22.8 (18.39–27.21) | 69.5 (64.66–74.34) | 84.2 (80.36–88.04) | N.A. |
| Liu et al. (2020b) [62] | Feb 17 - Feb 23, 2020 | Cross-sectional | 2031 | N.A. | China | 42.25 | 57.75 | N.A. | 14.48 | DASS-21 ≥ 3 DASS-21 ≥ 8 DASS-21 ≥ 15 | 20 | 14.81 (13.27–16.35) | 18.3 (16.62–19.98) | 9.98 (8.68–11.28) | N.A. |
| Evanoff et al. (2020) [40] | Apr 17- May 1, 2020 | Cross-sectional | 5550 | 34.3 | United States | 19.45 | N.A. | 80.55 | 21.4 | DASS-21 | 21 | 15.29 (14.34–16.24) | 13 (12.12–13.88) | N.A. | N.A. |
| Wańkowicz et al. (2020) [91] | 3 May 2020 to 17 May 2020 | Cross-sectional | 441 | N.A. | Poland | N.A. | N.A. | N.A. | 47.84 | PHQ-9 > 4 GAD-7 > 4 ISI > 8 | 23 | 70.74 (66.49–74.99) | 64.39 (59.92–68.86) | N.A. | 58.04 (53.43–62.65) |
| Que et al. (2020) [50] | 16–23 Feb, 2020 | Cross-sectional | 2285 | N.A. | China | 37.67 | 9.1 | 53.23 | 30.94 | PHQ-9 ≥ 5 GAD-7 ≥ 5 ISI ≥ 15 | 23 | 89 (87.72–90.28) | 92.07 (90.96–93.18) | N.A. | 57.5 (55.47–59.53) |
| Luceño-Moreno et al. (2020) [65] | 1 to 30 of April, 2020 | Cross-sectional | 1422 | 92.39 | Spanish | 10 | 34.2 | 55.8 | 13.6 | HADS ≥ 7 HADS ≥ 7 IES-R ≥ 20 | 23 | 51.3 (48.7–53.9) | 79.3 (77.19–81.41) | 83 (81.05–84.95) | N.A. |
| Sandesh et al. (2020) [81] | 20-May | Cross-sectional | 112 | N.A. | Pakistan | N.A. | N.A. | N.A. | 57.1 | DASS-21 | 15 | 71.32 (62.94–79.7) | 85.71 (79.23–92.19) | N.A. | N.A. |
| Giusti et al. (2020) [42] | April 16- May 11 2020 | Cross-sectional | 330 | 41.25 | Italy | 42.2 | 26 | 31.8 | 37.4 | DASS-21 > 9 DASS-21 > 7 DASS-21 > 14 | 18 | 26.8 (22.02–31.58) | 31.3 (26.3–36.3) | 34.3 (29.18–39.42) | N.A. |
| Chatterjee et al. (2020) [33] | April 20- May 20 2020 | Cross-sectional | 308 | 81.16 | India | 40 | 32.9 | 27.1 | 43.6 | ISI > 7 | 28 | N.A. | N.A. | N.A. | 47.9 (42.32–53.48) |
| Zhu et al. (2020b) [98] | February 1- February 29, 2020 | Cross-sectional | 165 | N.A. | China | 47.9 | 52.2 | N.A. | 17 | SDS > 50 SAS > 50 | 25 | 45.6 (38–53.2) | 11.4 (7.97–14.83) | N.A. | N.A. |
| Alnazly et al. (2021) [26] | August 16th to 23rd, 2020. | Cross-sectional | 365 | 100 | Jordan | 10 | 63 | 27 | 44.4 | DASS-21 > 9 DASS-21 > 7 DASS-21 > 14 | 27 | 80 (75.9–84.1) | 85 (81.15–88.85) | 75 (70.33–79.67) | N.A. |
| Ni at al. (2021) [71] | 4-Mar-20 | Cross-sectional | 57 | 100 | China | 83 | 17 | N.A. | 17 | SDS > 53 SAS > 50 | 15 | 42 (29.19–54.81) | 9 (5.91–12.09) | N.A. | N.A. |
| Du et al. (2020) [38] | March 19-April 7, 2020 | Cross-sectional | 403 | N.A. | China | 39.21 | 54.84 | 5.96 | 27.27 | DASS-21 > 9 DASS-21 > 7 DASS-21 > 14 | 24 | 17 (13.33–20.67) | 32 (26.97–37.03) | 88 (84.49–91.51) | N.A. |
| Hong et al. (2020) [48] | February 8 to 14, 2020 | Cross-sectional | 4692 | N.A. | China | N.A. | 100 | N.A. | 3.1 | PHQ-9 > 10 GAD-7 > 10 | 20 | 9.4 (8.56–10.24) | 8.1 (5.16–11.04) | N.A. | N.A. |
| Gorini et al. (2020) [43] | April 1st to May 1st 2020. | Cross-sectional | 650 | 84.4 | Italy | 27 | 32.9 | 40.1 | 67.5 | PHQ-9 > 3 GAD-7 > 9 | 18 | 22.8 (19.57–26.03) | 29.6 (24.67–34.53) | 44.9 (39.53–50.27) | N.A. |
| Lee et al. (2020) [56] | June 22 to July 8, 2020 | Cross-sectional | 406 | N.A. | Korea | 20 | 55.7 | 24.3 | 28.3 | PHQ-9 ≥ 10 GAD-7 ≥ 5 ISI≥8 | 19 | 14.3 (10.89–17.71) | 39.4 (34.13–44.67) | 52 (46.61–57.39) | 36.2 (30.83–41.57) |
| Ning et. al (2020) [72] | 20-Feb | Cross-sectional | 612 | N.A. | China | 51.8 | 48.2 | 0 | 27.1 | SDS ≥ 53 SAS ≥ 50 | 22 | 25 (21.57–28.43) | 16.3 (12.31–20.29) | N.A. | N.A. |
| Ahn et al. (2020) [25] | 20–30 April 2020, | Cross-sectional | 1783 | N.A. | South Korea | 16.4 | 54.2 | 29.4 | 23.9 | PHQ-9 ≥ 10 GAD-7 ≥ 5 | 18 | 10 (8.61–11.39) | 10 (6.76–13.24) | N.A. | N.A. |
| Tan et al. (2020) [31] | May 29 -June 24, 2020 | Cross-sectional | 3075 | 27.2 | Singapore | 14.9 | 45.3 | 39.8 | 25.8 | HADS > 7 HADS > 7 | 23 | 31.8 (30.15–33.45) | 40.7 (35.4–46) | N.A. | N.A. |
| Conti et al. (2020) [35] | March 30- May 03, 2020 | Cross-sectional | 933 | 76.3 | Italy | 24 | 42.3 | 33.7 | 23.5 | PHQ-9 ≥5 GAD-7 ≥5 PHQ-15 ≥ 5 | 20 | 57.9 (54.73–61.07) | 65.2 (60.06–70.34) | 55 (49.63–60.37) | N.A. |
| Wang et al. (2020) [90] | 2nd -3rd February 2020 | Cross-sectional | 1045 | 80.1 | China | 14.3 | 74 | 11.7 | 14.2 | HADS > 7 ISI ≥ 8 | 26 | 39.4 (36.44–42.36) | 47.8 (42.41–53.19) | N.A. | 49.9 (44.32–55.48) |
| Lasalvia et al. (2021) [55] | 21 April-6 May 2020 | Cross-sectional | 2195 | 36.9 | Italy | 13.9 | 35.7 | 50.4 | 24.7 | PHQ-9 ≥ 10 SAS ≥ 36 IES-R ≥ 24 | 20 | 26.6 (24.75–28.45) | 50.1 (44.71–55.49) | 53.8 (48.42–59.18) | N.A. |
| Zheng et al. (2021) [96] | March 6, 2020, to March 9, 2020 | Cross-sectional | 617 | N.A. | China | N.A. | 100 | N.A. | 8.5 | DASS-21 > 9 DASS-21 > 7 DASS-21 > 14 | 26 | 15.4 (12.55–18.25) | 32.6 (27.54–37.66) | 18 (13.85–22.15) | N.A. |
| Arafa et al. (2021) [30] | 14th and 24th of April 2020 | Cross-sectional | 426 | N.A. | Egypt and Saudi Arabia | 48.4 | 24.2 | 27.4 | 50.2 | DASS-21 > 9 DASS-21 > 7 DASS-21 > 14 | 25 | 69 (64.61–73.39) | 58.9 (53.59–64.21) | 55.9 (50.54–61.26) | N.A. |
| Lenzo et al. (2021) [58] | April 27 to May 4, 2020 | Cross-sectional | 214 | N.A. | Italy | 19.6 | 80.4 | 0 | 39 | DASS-21 > 9 DASS-21 > 7 DASS-21 > 14 | 25 | 23 (17.36–28.64) | 18 (13.85–22.15) | 24 (19.39–28.61) | N.A. |
| Sunil et al. (2021) [86] | June 1, 2020, to July 4, 2020 | Cross-sectional | 313 | N.A. | India | 100 | N.A. | N.A. | 35.5 | PHQ-4>2 PHQ-4>2 PSS>13 ISI>7 | 24 | 47 (41.47–52.53) | 47 (41.61–52.39) | 54 (48.62–59.38) | 31.9 (26.69–37.11) |
| Hennein et al. (2021) [47] | 20-May | Cross-sectional | 1092 | 96.5 | US | 31.2 | 19 | 49.8 | 28 | PHQ-9 ≥ 10 GAD-7 ≥ 10 PTSD ≥ 3 | 22 | 13.9 (11.85–15.95) | 15.6 (11.68–19.52) | 22.8 (18.27–27.33) | N.A. |
| Mathur et al. (2020) [67] | 20-Jun | Cross-sectional | 200 | N.A. | India | 87 | 13 | N.A. | 69 | DASS-21 ≥ 10 DASS-21 ≥ 8 DASS-21 ≥ 15 | 22 | 17 (11.79–22.21) | 19.5 (15.23–23.77) | 9.5 (6.34–12.66) | N.A. |
| Liu et al. (2021) [63] | 24 February to 9 March, 2020 | Cross-sectional | 1090 | N.A. | China | 40.6 | 59.4 | N.A. | 19.8 | PHQ-9 ≥ 15 GAD-7 ≥ 15 PSS-10 ≥ 15 | 22 | 18.4 (16.1–20.7) | 13.3 (9.64–16.96) | 48.07 (42.68–53.46) | N.A. |
| Tasnim et al. (2020) [87] | July and August 2020 | Cross-sectional | 803 | 97 | Bangladesh | 68 | 10 | 22 | 50.7 | HADS ≥ 8 HADS ≥ 8 | 23 | 39.5 (36.12–42.88) | 69.5 (64.53–74.47) | N.A. | N.A. |
| Greene et al. (2021) [44] | 27 May to 23 July, 2020 | Cross-sectional | 1194 | 49 | UK | 3.85 | 42.21 | 53.94 | 7.04 | PHQ-9 ≥ 10 GAD-7 ≥ 8 | 16 | 47 (44.17–49.83) | 47 (41.61–52.39) | N.A. | N.A. |
| Ranjan et al. (2021) [76] | 23 April to 24 May, 2020 | Cross-sectional | 373 | N.A. | India | 19.3 | 42.1 | 38.6 | 47.7 | DASS-21 | 15 | 39.1 (34.15–44.05) | 53.6 (48.22–58.98) | 62.5 (57.28–67.72) | N.A. |
| Si et al. (2020) [83] | 23 February to 5 March, 2020 | Cross-sectional | 863 | 76 | China | 43.7 | 24.4 | 31.9 | 29.3 | DASS-21 ≥ 10 DASS-21 ≥ 10 IES-6 ≥ 10 | 23 | 13.6 (11.31–15.89) | 13.9 (10.17–17.63) | 8.6 (5.58–11.62) | N.A. |
| Khalaf et al. (2020) [52] | March to May, 2020 | Cross-sectional | 170 | N.A. | Egypt | 100 | N.A. | N.A. | 38.8 | DASS-21 ≥ 10 DASS-21 ≥ 8 DASS-21 ≥ 15 | 24 | 63 (55.74–70.26) | 77.6 (73.1–82.1) | 72 (67.16–76.84) | N.A. |
| Tu et al. (2020) [89] | 7 February to 25 February, 2020 | Cross-sectional | 100 | 100 | China | N.A. | 100 | N.A. | N.A. | PHQ-9 ≥ 15 GAD-7 ≥ 4 | 23 | 46 (36.23–55.77) | 40 (34.71–45.29) | N.A. | 60 (54.53–65.47) |
| Nguyen et al. (2021) [70] | 22 April to 12 May, 2020 | Cross-sectional | 761 | 98.3 | Vietnam | 59.9 | N.A. | 40.1 | 41.8 | IES-R ≥ 24 | 17 | N.A. | N.A. | 34.3 (29.18–39.42) | N.A. |
| Ferini-Strambi et al. (2020) [41] | Feb, 2020–May, 2020 | Cross-sectional | 7236 | N.A. | Italy | 30 | 70 | N.A. | 30 | PSQI>5 | 20 | N.A. | N.A. | N.A. | 35 (29.67–40.33) |
| Mattila et al. (2021) [39] | Mar 20-June 20, 2020 | Cross-sectional | 1995 | 19.13 | Finland | 6 | 66 | 28 | 13 | GAD-7 ≥ 5 | 24 | N.A. | 45 (39.63–50.37) | N.A. | N.A. |
| Chen et al. (2020) [104] | Jan 23-Mar 22, 2020 | Cross-sectional | 1493 | 93.31 | China | 28.27 | N.A. | N.A. | 55.39 | SDS>53 PSS-10 > 20 | 19 | 3.79 (2.82–4.76) | N.A. | 71.56 (66.69–76.43) | N.A. |
| Li et al. (2020) [77] | Jan–Feb 2020 | Cross-sectional | 176 | 100 | China | N.A. | 100 | N.A. | 22.7 | HAM-A>7 | 18 | N.A. | 77.3 (72.78–81.82) | N.A. | N.A. |
| An et al. (2020) [94] | Mar 15-Mar 20, 2020 | Cross-sectional | 1103 | 100 | China | N.A. | 100 | N.A. | N.A. | PHQ-9 ≥ 5 | 21 | 43.61 (40.68–46.54) | N.A. | N.A. | N.A. |
| Holton et al. (2020) [82] | May 15- June 10, 2020 | Cross-sectional | 668 | 15 | Australia | 20.65 | 58.53 | 20.82 | N.A. | DASS-21 ≥ 5 DASS-21 ≥ 5 DASS-21 ≥ 5 | 19 | 23 (19.81–26.19) | 29 (24.1–33.9) | 25 (20.33–29.67) | N.A. |
| Ofori et al. (2021) [28] | July 11- August 12, 2020 | Cross-sectional | 272 | 90.7 | Ghana | N.A. | N.A. | N.A. | 48.73 | DASS-21 ≥ 10 DASS-21 ≥ 8 DASS-21 ≥ 15 | 22 | 21.1 (16.25–25.95) | 27.8 (22.97–32.63) | 8.2 (5.24–11.16) | N.A. |
| Bizri et al. (2021) [68] | Apr–May, 2020 | Cross-sectional | 150 | 18.75 | Lebanon | 27.7 | 37.3 | 35 | 44 | IES-R ≥ 33 | 23 | N.A. | N.A. | 33 (27.93–38.07) | N.A. |
| Wilson et al. (2020) [103] | Apr 10-Apr 25, 2020 | Cross-sectional | 433 | 80.83 | India | 84.3 | 15.7 | N.A. | 53.4 | PHQ-9 ≥ 10 GAD-7 ≥ 5 PSS ≥ 9 | 18 | 49.4 (44.69–54.11) | 66.7 (61.62–71.78) | 82.6 (78.51–86.69) | N.A. |
| Badahdah et al. (2020) [100] | Apr 1- Apr 14, 2020 | Cross-sectional | 509 | N.A. | Oman | 38.1 | 61.9 | N.A. | 19.7 | GAD-7 ≥ 5 PSS ≥ 24 | 22 | N.A. | 74.1 (69.37–78.83) | 43.6 (38.25–48.95) | N.A. |
| Wasim et al. (2020) [88] | May 20-June 3rd, 2020 | Cross-sectional | 356 | N.A. | India | 60.11 | 21.91 | 17.98 | 48.03 | DASS-21 ≥ 10 DASS-21 ≥ 8 DASS-21 ≥ 15 ISI ≥ 8 | 19 | 62.35 (57.32–67.38) | 64.76 (59.61–69.91) | 55.33 (49.97–60.69) | 53.37 (47.8–58.94) |
| Lamb et al. (2021) [36] | Apr–June, 2020 | Cross-sectional | 4378 | 94 | UK | 12.8 | 26.7 | 60.5 | 24.6 | PHQ-9 ≥ 10 GAD-7 ≥ 10 PTSD-8 ≥ 14 | 18 | 27.3 (25.98–28.62) | 23.2 (18.65–27.75) | 30.2 (25.25–35.15) | N.A. |
| Blekas et al. (2020) [29] | Apr 10 -Apr 13, 2020 | Cross-sectional | 2427 | 96 | Greek | N.A. | N.A. | N.A. | 21.9 | PHQ-9>6 PDI>10 PTSD-8>9 AIS>10 | 19 | 27.23 (25.46–29) | 41.33 (36.02–46.64) | 34.13 (29.01–39.25) | 15.34 (11.32–19.36) |
| Hasan et al. (2020) [46] | Apr 21-May 10, 2020 | Cross-sectional | 442 | 93.21 | Bangladesh | 100 | N.A. | N.A. | 44.2 | HADS ≥ 8 HADS ≥ 8 | 25 | 67.72 (63.36–72.08) | 48.5 (43.11–53.89) | N.A. | N.A. |
| Labrague et al. (2020) [59] | Apr 25-May 25, 2020 | Cross-sectional | 350 | 92.85 | Philippines | N.A. | 100 | N.A. | N.A. | PSSQ ≥ 5 | 21 | N.A. | 37.8 (32.57–43.03) | N.A. | N.A. |
| Salman et al. (2020) [79] | Apr 15-May 20, 2020 | Cross-sectional | 398 | N.A. | Pakistan | 52 | N.A. | 48 | N.A. | PHQ-9 ≥ 10 GAD-7 ≥ 10 | 19 | 21.9 (17.84–25.96) | 21.4 (16.97–25.83) | N.A. | N.A. |
| Hassannia et al. (2020) [57] | Apr 6-Apr 15, 2020 | Cross-sectional | 2200 | 93 | Iran | 6.2 | 5.1 | N.A. | 32.5 | HADS>8 HADS>8 | 22 | 42.3 (40.24–44.36) | 65.6 (60.47–70.73) | N.A. | N.A. |
| Hassamal et al. (2021) [80] | April 30 to May 22, 2020 | Cross-sectional | 3500 | 36 | US | 12.2 | 39.8 | 48 | 22.2 | PHQ-9 ≥ 10 GAD-7 ≥ 8 | 24 | 21 (19.65–22.35) | 33 (27.93–38.07) | N.A. | N.A. |
| Kaveh et al. (2020) [66] | Mar 25- Mar 31, 2020 | Cross-sectional | 1072 | 96.82 | Iran | N.A. | 49.5 | N.A. | 12.4 | BAI ≥ 8 | 18 | N.A. | 39.6 (34.32–44.88) | N.A. | N.A. |
| Saleem et al. (2020) [99] | 4-Apr-20 | Cross-sectional | 404 | N.A. | Pakistan | 30.7 | 18.8 | 50.5 | 34.9 | FCV-19S ≥ 10 | 20 | N.A. | 79.7 (75.36–84.04) | N.A. | N.A. |
| Aziznejadroshan et al. (2020) [73] | May–June, 2020 | Cross-sectional | 224 | N.A. | Iran | N.A. | 100 | N.A. | 25.4 | DASS-21 ≥ 10 DASS-21 ≥ 8 DASS-21 ≥ 10 | 20 | 43 (36.52–49.48) | 54 (48.62–59.38) | 17.4 (13.31–21.49) | N.A. |
| Zhang et al. (2020b) [95] | Jun 6- Jun 13, 2020 | Cross-sectional | 721 | 90 | China | 25.66 | 69.03 | 5.31 | 14.95 | HADS ≥ 8 HADS ≥ 8 ISI ≥ 8 | 25 | 82.09 (79.29–84.89) | 88.88 (85.49–92.27) | N.A. | 95.52 (93.21–97.83) |
| Cai et al. (2020) [32] | Feb 11- Feb 26, 2020 | Cross-sectional | 1173 | N.A. | China | 98.6 | N.A. | 1.4 | 30.2 | PHQ-9>10 BAI>15 ISI ≥ 9 | 26 | 14.3 (12.3–16.3) | 15.7 (11.77–19.63) | N.A. | 47.8 (42.22–53.38) |
| Elbay et al. (2020) [78] | Mar 10-Mar 15, 2020 | Cross-sectional | 442 | 100 | Turkey | 17.2 | N.A. | 82.8 | 43.21 | N.A. | 25 | 64.7 (60.24–69.16) | 51.6 (46.21–56.99) | 41.2 (35.89–46.51) | N.A. |
| Mira et al. (2020) [51] | Mar 18-May 17, 2020 | Cross-sectional | 685 | 33.33 | Spain | 28.6 | 39 | 32.4 | N.A. | EASE ≥ 10 | 18 | N.A. | N.A. | 27.4 (22.59–32.21) | N.A. |
| Salopek-Žiha et al. (2020) [37] | Mar 26 -Apr 6 2020 | Cross-sectional | 124 | 100 | Croatia | 22 | 78 | 0 | N.A. | N.A. | 20 | 11 (5.49–16.51) | 17 (12.95–21.05) | 10 (6.76–13.24) | N.A. |
| Weibelzahl et al. (2021) [92] | May 22-July 22, 2020 | Cross-sectional | 300 | 98.67 | Germany | N.A. | N.A. | N.A. | 18.91 | ISR ≥ 10 ISR ≥ 10 | 21 | 82 (77.65–86.35) | 47.77 (42.38–53.16) | N.A. | N.A. |
N.A., Not available; CES-D, Center for Epidemiologic Studies Depression Scale; DASS-21, The Depression, Anxiety and Stress Scale; GAD-7, Generalized Anxiety Disorder 7-item; PHQ-9, Patient Health Questionnaire; SAS, The Zung Self-Rating Anxiety Scale; SDS, The Zung Self-Rating Depression Scale; HAM-A, Hamilton Anxiety Scale Rating; HAM-D, Hamilton Rating Depression Scale; IES-R, Impact of Events Scale – Revised; PSQI, The Pittsburgh Sleep Quality Index; ISI, The Insomnia Severity Index; HADS, Hospital Anxiety and Depression Scale; IES, Impact of Event Scale; PSS, The Perceived Stress Scale; PTSD-8, The Post-traumatic Stress Disorder-8 Scale; EASE, The Examination of Anomalous Self-Experience Scale; FCV-19S, The Fear of COVID-19 Scale.
3.3. Statistical heterogeneity and publication bias
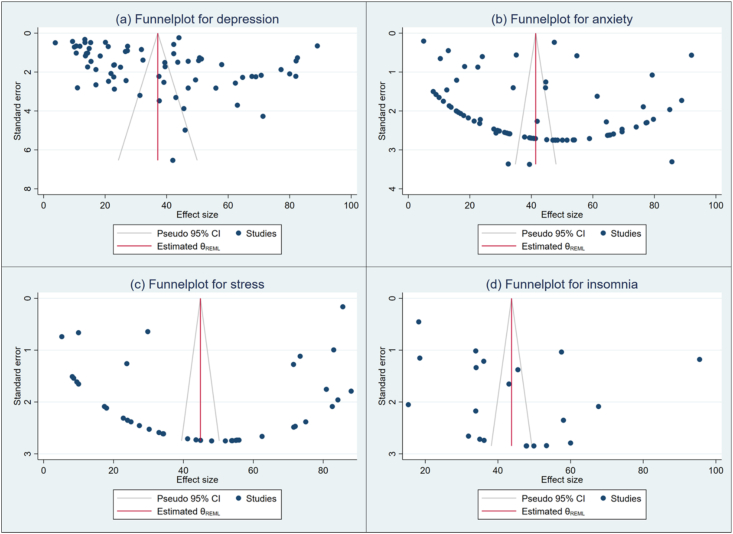
Two statistical tools Q-test and (%) were used to investigate the heterogeneity of the included studies. Here, we obtained for depression (Q (68) = 34675.82, P < 0.05) = 99.84%, anxiety (Q (74) = 47974.95, P < 0.05) = 99.79%, stress (Q (40) = 40900.83, P < 0.05) = 99.78%, and, insomnia (Q (20) = 5390.03, P < 0.05) = 99.41%. We prefer to use a random-effects model for analyzing the outputs due to higher heterogeneity among the studies. We also performed the Meta-regression to search for the source of heterogeneity. The results of individual variable meta-regression models show (Table 2) that the high heterogeneity of the included studies for depression and anxiety was associated with study duration and sample size. The high heterogeneity among the included studies for stress was associated with measurement tools and for insomnia with study duration. The Funnel plot and Eggers's test indices were used to investigate the publication bias for selected studies. The results indicate that there is no significant publication bias for stress (Z = 0.33, P = 0.74) (Figure 2c), and insomnia (Z = 0.67, P = 0.50) (Figure 2d). However, a significant publication bias was found for depression (Z = 2.77, P = 0.005) (Figure 2a), and anxiety (Z = 2.22, P = 0.02) (Figure 2b).
Table 2.
Result of individual variable meta-regression models for each stratified meta-analysis.
| Variables | Label | Prevalence (95% CI) | Coefficient (95% CI) | P-value |
|---|---|---|---|---|
| Depression | ||||
| Study duration | January to March, 2020 | 32.5 (23.86–41.15) | (Ref) | |
| April to June, 2020 | 39.62 (32.01–47.24) | 7.13 (-4.58–18.84) | 0.03 | |
| July to September, 2020 | 46.88 (12.8–80.96) | 14.39 (-12.26–41.05) | 0.02 | |
| Response rate | Less than 60% | 29.43 (21.75–37.12 | (Ref) | |
| Greater than 60% | 40.11 (32.05–48.17) | 10.67 (-5.97–27.31) | 0.21 | |
| Sample size | Greater than 600 | 30.96 (24.28–37.63) | (Ref) | |
| Less than 600 | 45.24 (37.43–53.05) | 14.28 (4.03–24.54) | 0.01 | |
| Measurement tools | CES-D | 20.1 (19.18–21.02) | (Ref) | |
| DASS-21 | 34.83 (24.81–44.84) | 14.72 (-30.69–60.13) | 0.53 | |
| HADS | 47.02 (35.74–58.3) | 26.91 (-19.86–73.68) | 0.26 | |
| PHQ | 38.11 (29.03–47.19) | 15.5 (-31.93–62.93) | 0.52 | |
| SDS | 30.63 (14.27–46.99) | 18.01 (-27.23–63.25) | 0.44 | |
| Other# | 35.62 (15.28–55.96) | 10.59 (-37.39–58.57) | 0.67 | |
| Anxiety | ||||
| Study duration | January to March, 2020 | 30.68 (22.97–38.39) | (Ref) | |
| April to June, 2020 | 48.57 (40.68–56.47) | 17.88 (5.9–29.87) | 0.00 | |
| July to September, 2020 | 60.79 (27.31–94.27) | 30.11 (1.75–58.47) | 0.04 | |
| Response rate | Less than 60% | 37.3 (29.34–45.26) | (Ref) | |
| Greater than 60% | 42.34 (34.97–49.72) | 4.98 (-10.2–20.16) | 0.52 | |
| Sample size | Greater than 600 | 36.99 (29.84–44.15) | (Ref) | |
| Less than 600 | 46.24 (38.71–53.76) | 9.24 (-1.13–19.62) | 0.08 | |
| Measurement tools | BAI | 27.58 (4.16–51) | (Ref) | |
| DASS-21 | 39.62 (29.41–49.84) | -19.97 (-67.69–27.74) | 0.41 | |
| GAD | 43.66 (35.27–52.05) | 3.72 (-44.42–51.85) | 0.88 | |
| HADS | 58.06 (46.02–70.1) | 29.2 (-36.39–94.79) | 0.38 | |
| HAMA | 49.91 (-3.7–103.51) | (empty) | ||
| SAS | 19.39 (9.4–29.37) | (empty) | ||
| Other@ | 43.91 (25.94–61.88) | -11.4 (-61.63–38.83) | 0.66 | |
| Stress | ||||
| Study duration | January to March, 2020 | 38.14 (21.41–54.87) | (Ref) | |
| April to June, 2020 | 46.31 (36.47–56.15) | 8.17 (-10.84–27.17) | 0.40 | |
| July to September, 2020 | 41.58 (-23.89–107.04) | 3.37 (-34.62–41.37) | 0.86 | |
| Response rate | Less than 60% | 43.26 (24.64–61.88) | (Ref) | |
| Greater than 60% | 41.63 (28.72–54.54) | -1.62 (-26.08–22.85) | 0.90 | |
| Sample size | Greater than 600 | 40.77 (30.12–51.42) | (Ref) | |
| Less than 600 | 49.17 (37.53–60.81) | 8.4 (-7.35–24.15) | 0.30 | |
| Measurement tools | DASS-21 | 35.25 (23.03–47.46) | (Ref) | |
| IES | 65.95 (49.26–82.64) | 30.71 (7.92–53.5) | 0.01 | |
| PSS | 69.46 (52.68–86.23) | 5.63 (-13.48–24.74) | 0.56 | |
| PTSD | 26.43 (19.18–33.68) | 34.17 (9.7–58.64) | 0.01 | |
| Other$ | 40.84 (30.04–51.65) | -8.74 (-44.85–27.37) | 0.64 | |
| Insomnia | ||||
| Study duration | January to March, 2020 | 42.46 (34.68–50.23) | (Ref) | |
| April to June, 2020 | 48.79 (30.38–67.19) | 6.25 (-12.28–24.78) | 0.05 | |
| July to September, 2020 | - | (empty) | ||
| Response rate | Less than 60% | - | (Ref) | |
| Greater than 60% | 45.47 (29.87–61.07) | (empty) | ||
| Sample size | Greater than 600 | 40.79 (29.4–52.18) | (Ref) | |
| Less than 600 | 48.64 (39.32–57.96) | 7.85 (-8.54–24.24) | 0.35 | |
| Measurement tools | AIS | 30.46 (0.9–60.01) | (Ref) | |
| ISI | 46.58 (37.7–55.46) | 44.643 (-43.421–132.707) | 0.32 | |
| PSQI | 26.39 (9.93–42.85) | 85.516 (-149.536–320.568) | 0.47 | |
Ref, reference group.
Other # includes ISR and HAMD.
Other@ includes FCV-19S, ISR, PDI, PHQ-4, PSSQ.
Other$ includes EASE, PHQ-15, SAVE-9.
Figure 2.
Funnel plot of result of the prevalence of depression (a), anxiety (b), stress (c), and insomnia (d) among health professionals.
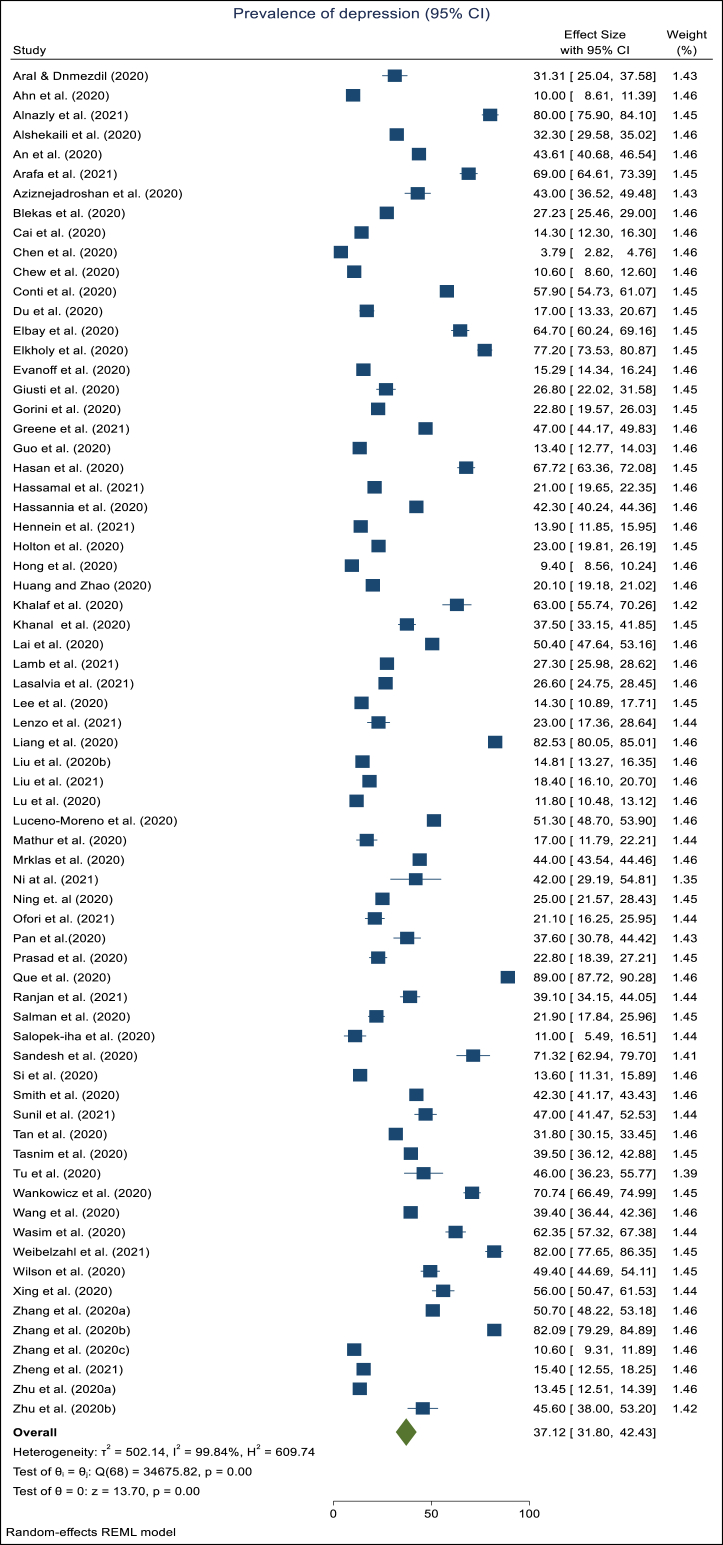
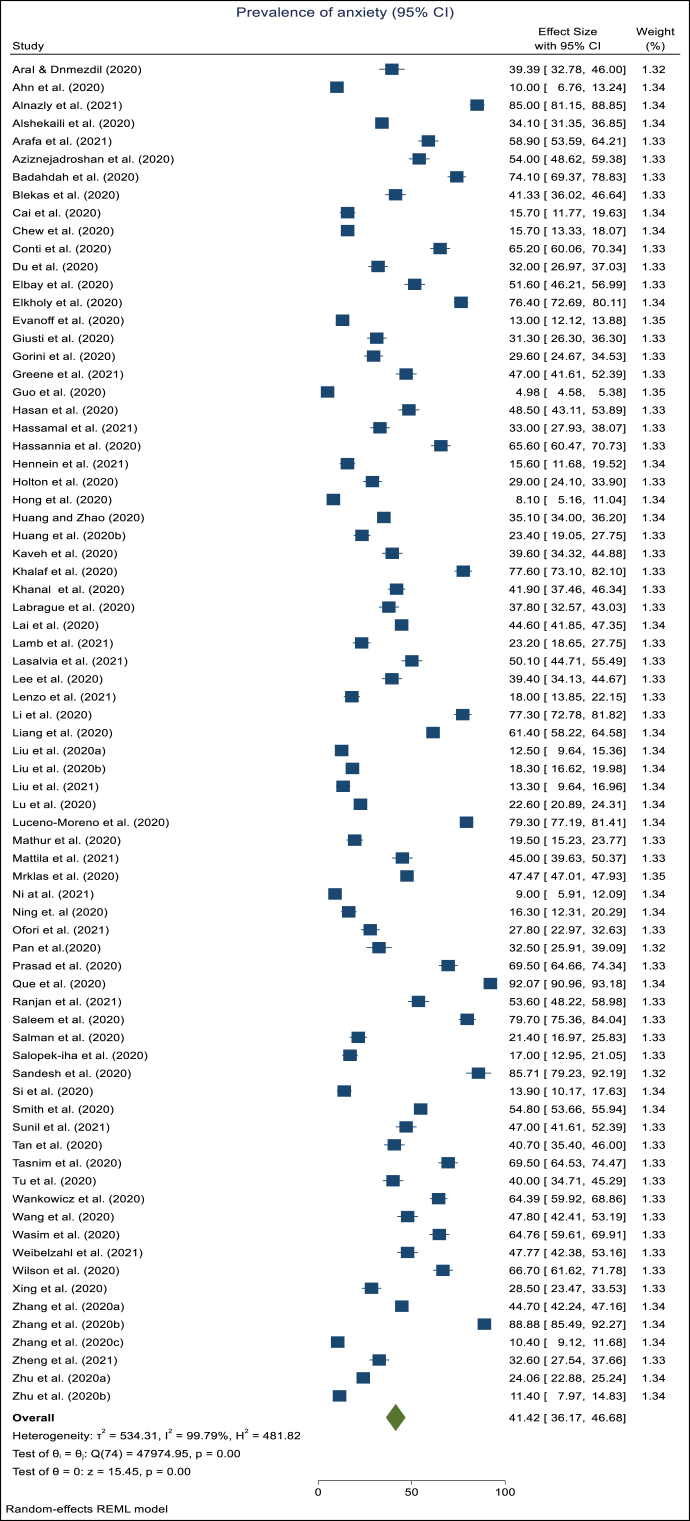
3.4. The pooled prevalence
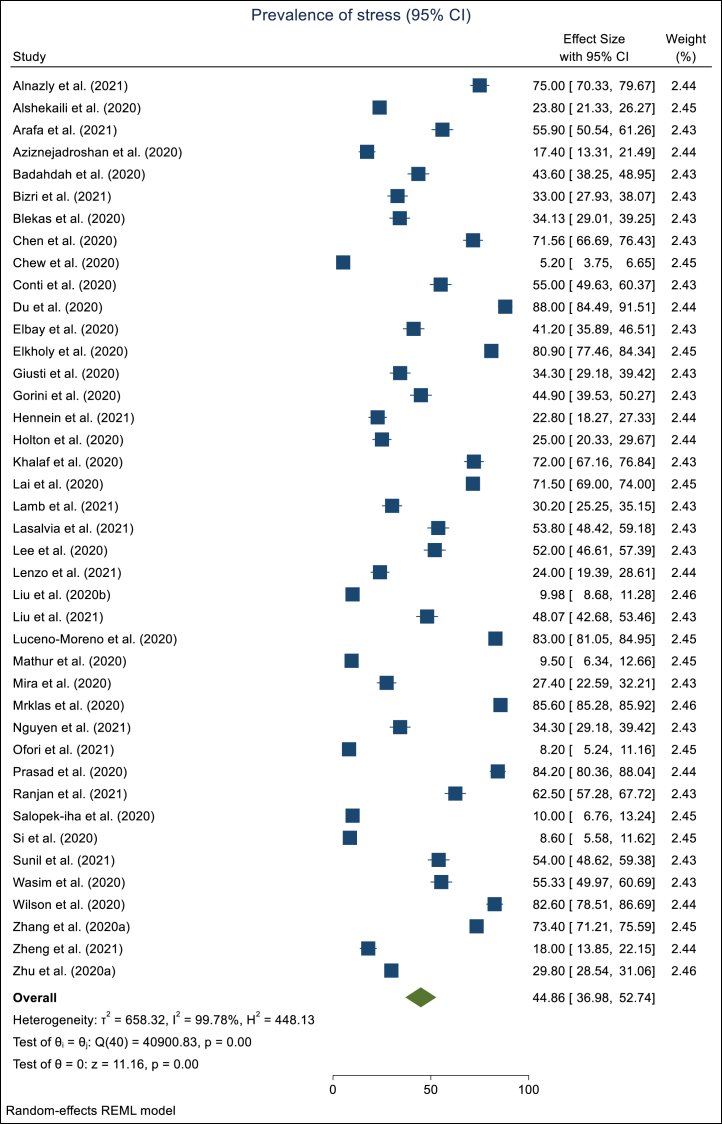
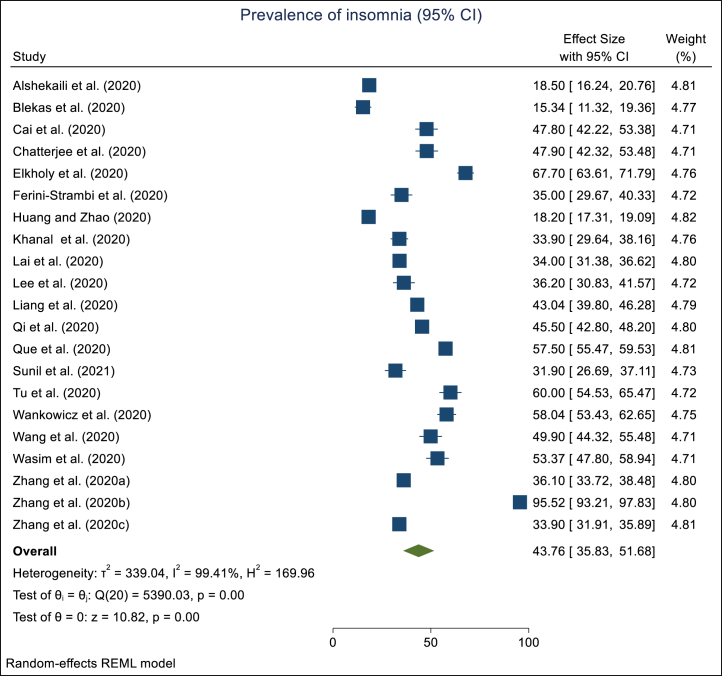
Depression was reported in 69 studies (n = 144649) out of 83 studies. The pooled prevalence was estimated as 37.12% (95% CI: 31.80–42.43) (Figure 3). The between study heterogeneity was found statistically significant (= 99.84%, P-value = 0.00) (Figure 3). Anxiety was mentioned in 75 studies (n = 147435) from 83 studies. The pooled prevalence of anxiety was assessed as 41.42% (95% CI: 36.17–46.54) (Figure 4) with a significant between study heterogeneity (= 99.79%, P-value = 0.00) (Figure 4). Stress was reported in 41 studies (n = 82783) with a pooled prevalence of 44.86% (95% CI: 36.98–52.74) (Figure 5). There was significant serious between-study heterogeneity (= 99.78%, P-value = 0.00) (Figure 5). Similarly, the pooled prevalence of insomnia was estimated from 21 studies (n = 33370) as 43.76% (95% CI: 35.83–51.68) (Figure 6). A severe (= 99.41%, P-value = 0.00) between study heterogeneity was also found (Figure 6).
Figure 3.
Forest plot showing the meta-analyses of the pooled prevalence of depression among health professionals during the pandemic.
Figure 4.
Forest plot showing the meta-analyses of the pooled prevalence of anxiety among health professionals during the pandemic.
Figure 5.
Forest plot showing the meta-analyses of the pooled prevalence of stress among health professionals during the pandemic.
Figure 6.
Forest plot showing the meta-analyses of the pooled prevalence of insomnia among health professionals during the pandemic.
3.5. Subgroup analysis
The subgroup analysis of depression, anxiety, stress, and insomnia was conducted by study duration, assessment tools, and country.
3.5.1. Study duration subgroups
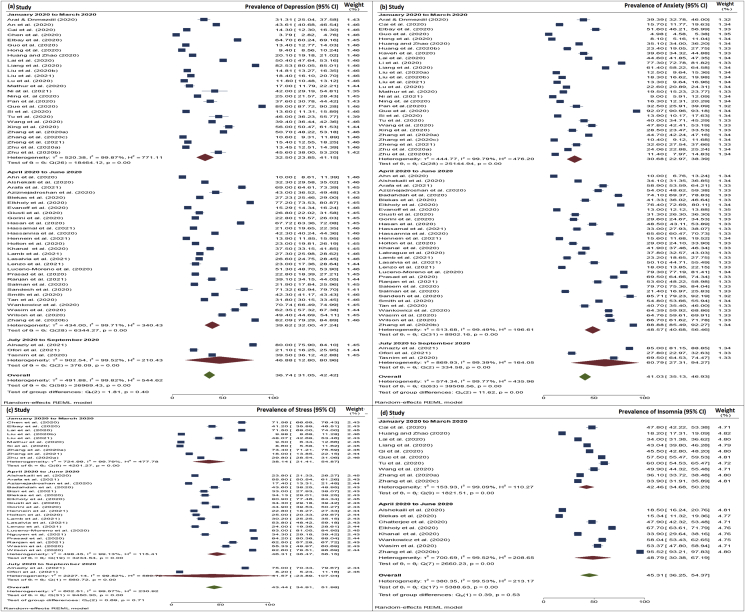
Based on the availability of data, all the studies were further classified into three three-month groups: January 2020 to March 2020, April 2020 to June 2020, July 2020 to September 2020. However, 13 studies [34, 35, 37, 38, 39, 41, 44, 51, 52, 56, 69, 86, 92] out of the 83 were not classified into any of those groups due to inconvenient study duration. Finally, 70 studies were included in the subgroup analysis based on study duration. Among them, 59 studies have the estimates of depression prevalence, 64 studies have the estimates of anxiety prevalence, 32 studies have the estimates of stress prevalence and 18 studies have estimates of insomnia prevalence.
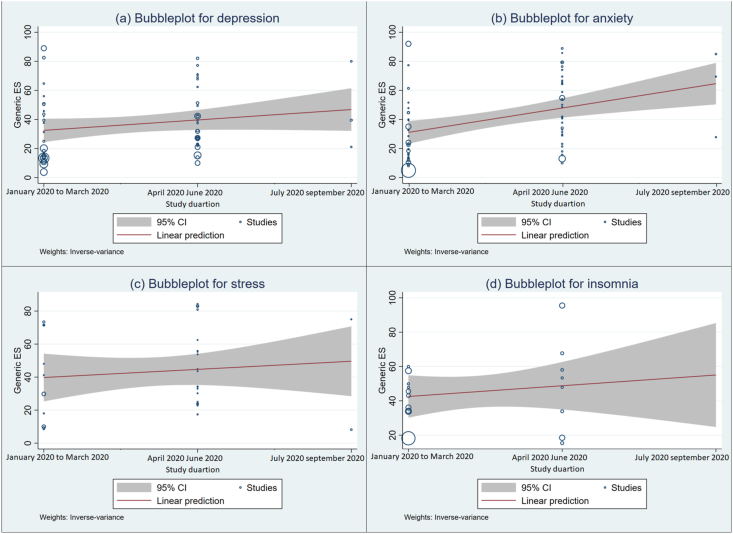
Twenty-seven studies were conducted between January 2020 to March 2020, with a pooled depression prevalence of 32.50%. Twenty-eight studies took place between April 2020 to June 2020 with a pooled depression prevalence of 39.62%. Three studies took place between July 2020 to September 2020 with a pooled depression prevalence of 46.88% (Please see Figure 7(a)). With a pooled anxiety prevalence of 30.68%, twenty-nine studies occurred between January 2020 to March 2020, thirty-two studies with a pooled anxiety prevalence of 48.57% were conducted between April 2020 to June 2020, and three studies were conducted between July 2020 to September 2020 with a pooled anxiety prevalence of 60.79% (Please see Figure 7(b)). Ten studies were conducted between January to March 2020 with a pooled stress prevalence of 38.14%, and four studies were carried out during April 2020 and June 2020, with a pooled stress prevalence of 46.31%, and two studies were carried out from July 2020 to September 2020 with a pooled stress prevalence of 41.57% (Please see Figure 7(c)). With a pooled insomnia prevalence of 42.46%, fourteen studies were done between January 2020 to March 2020, eight studies with a pooled insomnia prevalence of 48.79% were conducted from April 2020 to June 2020, and no study has been conducted from July 2020 to September 2020 with an estimate of insomnia prevalence (Please see Figure 7(d)). An upward trend in the prevalence of depression and anxiety was observed from January 2020 to September 2020 which was also satisfied by the Meta-regression findings (Figure 8 and Table 2).
Figure 7.
Forest plot showing changes of the pooled prevalence of depression (a), anxiety (b), stress (c), and insomnia (d) between study duration January 2020 to September 2020, among health professionals.
Figure 8.
Bubble plots from meta-regression showing the changes in the prevalence of depression (a), anxiety (b), stress (c), and insomnia (d) with study duration.
3.5.2. Country subgroups
Table 3 narrated the results of subgroup analysis of depression, anxiety, stress, and insomnia prevalence by country. Two studies [30, 34] covered populations from two different countries, and those were not included in this subgroup analysis. The results show the pooled prevalence of depression was the highest in Germany, (82.00% with 95% CI: 77.65–86.35) and the lowest in South Korea (10.00% with 95% CI: 8.61–11.93), anxiety was the highest in Jordan (85.00% with 95% CI: 81.33–88.67), and the lowest in South Korea, (10% with 95% CI: 6.92–13.08), stress was the highest in Canada (85.60% with 95% CI: 85.28–85.92) [69] and the lowest in Ghana (8.20% with 95% CI: 5.38–11.02), insomnia was the highest in Egypt (67.70% with 95% CI: 64.59–70.81) and the lowest in Greece (15.34% with 95% CI: 11.64–19.04).
Table 3.
Subgroup analysis of depression, anxiety, stress, and, insomnia prevalence by country.
| Region | Depression % (95% CI) (, Q (df.) P-value) | Anxiety % (95% CI) (, Q (df.) P-value) | Stress % (95% CI) (, Q (df.) P-value) | Insomnia % (95% CI) (, Q (df.) P-value) |
|---|---|---|---|---|
| Australia | 23.00 (19.81–26.19)∗ | ∗ | ∗ | - |
| China | 33.23 (23.80–42.67) (Q (25) = 19950.90, = 99.89, p-value<0.001) |
31.89 (22.78–41.00) (Q (26) = 26562.16, , p-value < 0.001) |
46.53 (26.43–66.63) (Q (8) = 4954.56, , p-value < 0.001) |
44.50 (34.76–54.21) (Q (13) = 5197.16, , p-value < 0.001) |
| Bangladesh | 53.57 (25.92–81.23) (Q (1) = 100.53, , p-value<0.001) |
59.03 (38.45–79.60) (Q (1) = 34.76, , p-value < 0.001) |
- | - |
| Canada | 43.23 (41.57–44.89) (Q (1) = 7.46, , p-value = 0.006) |
51.12 (43.93–58.30) (Q (1) = 136.58, , p-value < 0.001) |
∗ | - |
| Croatia | ∗ | ∗ | ∗ | - |
| Egypt | 70.46 (56.56–84.36) (Q (2) = 13.04, p-value = 0.001) |
76.88 (74.02–79.75) (Q (1) = 0.16, p-value = 0.68) |
76.62 (67.91–85.34) (Q (1) = 8.63, , p-value = 0.003) |
67.7 (64.59–70.81)∗ |
| Finland | - | ∗ | - | - |
| Germany | ∗ | ∗ | - | - |
| Ghana | ∗ | ∗ | ∗ | - |
| Greek | ∗ | ∗ | ∗ | ∗ |
| India | 42.98 (28.30–57.66) (Q (4) = 164, p-value < 0.001) |
50.28 (33.55–67.01) (Q (4) = 295.14, , p-value < 0.001) |
52.76 (29.23–76.29) (Q (4) = 966.73, , p-value < 0.001) |
44.36 (31.71–57.01) (Q (2) = 39.57, , p-value < 0.001) |
| Iran | 42.36 (40.40–44.33) (Q (1) = 0.04, p-value = 0.84) |
53.08 (38.33–67.83) (Q (2) = 53.04, , p-value < 0.001) |
∗ | - |
| Italy | 31.47 (18.33–44.61) (Q (4) = 334.06, , p-value < 0.001) |
38.81 (22.41–55.20) (Q (4) = 256.35, , p-value < 0.001) |
42.36 (30.74–53.97) (Q (4) = 119.98, , p-value < 0.001) |
∗ |
| Jordan | ∗ | ∗ | ∗ | - |
| Korea | ∗ | ∗ | ∗ | ∗ |
| Lebanon | - | ∗ | - | |
| Nepal | ∗ | ∗ | - | ∗ |
| Oman | ∗ | 54.06 (14.86–93.26) (Q (1) = 220.95, , p-value < 0.001) |
33.57 (14.17–52.97) (Q (1) = 46.98, , p-value < 0.001) |
∗ |
| Pakistan | 46.47 (-1.96–94.90) (Q (1) = 108.17, , p-value < 0.001) |
62.23 (22.01–102.45) (Q (2) = 465.58, , p-value < 0.001) |
- | - |
| Philippines | - | - | ||
| Poland | ∗ | ∗ | - | |
| Singapore | ∗ | ∗ | - | - |
| South Korea | ∗ | ∗ | - | - |
| Spain | ∗ | ∗ | 55.24 (0.75–109.73) (Q (1) = 478.91, , p-value < 0.001) |
- |
| Turkey | 48.08 (15.36–80.08) (Q (1) = 72.39, p-value<0.001) |
45.68 (33.72–57.64) (Q (1) = 8.18, , p-value = 0.004) |
∗ | - |
| United Kingdom | 37.11 (17.80–56.41) (Q (1) = 152.81, , p-value < 0.001) |
35.06 (11.73–58.38) (Q (1) = 48.25, , p-value < 0.001) |
∗ | - |
| United States | 18.01 (13.91–22.11) (Q (3) = 61.64, , p-value < 0.001) |
32.72 (7.22–58.22) (Q (3) = 559.53, , p-value < 0.001) |
53.51 (-6.66–113.69) (Q (1) = 434.61, , p-value < 0.001) |
- |
| Vietnam | - | - | ∗ | - |
| Overall | 37.04 (31.71–42.37) (Q (66) = 34051.22, , p-value < 0.001) |
41.54 (36.20–46.87) (Q (72) = 47722.64, , p-value < 0.001) |
45.60 (37.59–53.62) (Q (38) = 32786, , p-value < 0.001) |
58.04 (53.43–62.65) (Q (24) = 6102.53, , p-value < 0.001) |
- refers there is no studies were considered in this subgroup.
CI, Confidence Interval.
refers only one studies were included in this subgroup.
3.5.3. Assessment tools subgroups
Table 4 shows the highest pooled depression prevalence of 47.02% (95% CI: 35.74–58.30) for the HADS tool reported in nine studies and the lowest pooled depression prevalence of 20.10% (95% CI: 19.10–21.02) for the CES-D tool reported in only one study. The highest pooled anxiety prevalence of 58.06% (95% CI: 46.02–70.10) for the HADS tool was reported in nine studies and the lowest pooled anxiety prevalence of 19.39% (95% CI: 9.40–29.37) for the SAS tool was reported in eight studies. The highest stress and insomnia pooled prevalence of 65.95% (95% CI: 49.26–82.64) for IES and 46.58% (95% CI: 37.70–55.46) for ISI were reported in twenty-seven and sixteen studies respectively and the lowest stress and insomnia pooled prevalence of 26.43% (95% CI: 19.18–33.68) for PTSD was reported in two studies and 26.39% (95% CI: 9.93–42.84) for PSQI was reported in two studies respectively.
Table 4.
Subgroup analysis of depression, anxiety, stress, and, insomnia prevalence by assessment tools.
| Tools | Prevalence of Depression (%) (95% CI) (, Q (df), P-value) | Tools | Prevalence of Anxiety (%) (95% CI) ( , Q (df), P-value) | Tools | Prevalence of Stress (%) (95% CI) (, Q (df), P-value) | Tools | Prevalence of Stress (%) (95% CI) (, Q (df), P-value) |
|---|---|---|---|---|---|---|---|
| SDS | 30.63 (14.27, 46.98) (= 99.81, Q (5) = 684.88, p-value < 0.001) |
SAS | 19.39 (9.40, 29.37) (= 99.08, Q (7) = 478.65, p-value < 0.001) |
PSS | 69.46 (52.68, 86.23) (= 99.32, Q (4) = 374.70, p-value < 0.001) |
AIS | 30.46 (0.90, 60.01) (= 99.33, Q (1) = 149.01, p-value < 0.001) |
| CES-D | BAI | 27.58 (4.16, 51.00) (= 98.03, Q (1) = 50.69, p-value < 0.001) |
PTSD | 26.43 (19.18, 33.68) (= 78.60, Q (1) = 4.67, p-value = 0.03) |
PSQI | 26.39 (9.93, 42.84) (= 97.31, Q (1) = 37.17, p-value < 0.001) |
|
| PHQ-9 | 38.11 (29.03, 47.19) (= 99.59, Q (20) = 2698.05, p-value < 0.001) |
GAD | 43.65 (35.27, 52.05) (= 99.81, Q (26) = 13807.06, p-value < 0.001) |
IES | 65.95 (49.26, 82.64) (= 99.81, Q (26) = 13807.06, p-value < 0.001) |
ISI | 46.58 (37.70, 55.46) (= 99.20, Q (15) = 2964.36, p-value < 0.001) |
| DASS-21 | 34.83 (24.81, 44.84) (= 99.88, Q (24) = 19749.36, p-value < 0.001) |
HAMA | 49.91 (-3.70, 103.51) (= 99.80, Q (1) = 492.23, p-value < 0.001) |
DASS-21 | 35.24 (23.03, 47.46) (= 99.69, Q (5) = 2989.42, p-value < 0.001) |
- | - |
| HADS | 47.02 (35.74, 58.30) (= 99.30, Q (8) = 1107.94, p-value < 0.001) |
DASS-21 | 39.62 (29.41, 49.84) (= 99.55, Q (20) = 3420.53, p-value < 0.001) |
Other | 40.84 (30.04, 51.65) (= 98.03, Q (9) = 647.01, p-value < 0.001) |
- | - |
| Other | 35.62 (15.28, 55.96) (= 99.84, Q (6) = 2018.09, p-value < 0.001) |
HADS | 58.06 (46.02, 70.10) (= 98.63, Q (8) = 667.96, p-value < 0.001) |
- | - | - | - |
| - | - | Other | 43.91 (25.94, 61.88) (= 98.88, Q (5) = 665.18, p-value < 0.001) |
- | - | - | - |
| Overall | 37.12 (31.80, 42.43) (= 99.84, Q (68) = 34675.82, p-value < 0.001) |
Overall | 41.42 (36.17, 46.68) (= 99.79, Q (74) = 47974.95, p-value < 0.001) |
Overall | 44.86 (36.98, 52.74) (= 99.78, Q (40) = 40900.83, p-value < 0.001) |
Overall | 42.95 (34.79, 51.12) (= 99.44, Q (19) = 5306.39, p-value < 0.001) |
∗refers only one studies were included in this subgroup
- refers there is no studies were considered in this subgroup.
CI, Confidence Interval.
4. Discussion
In March 2020, SARS-CoV-2 was announced as a pandemic by the WHO and more than 200 nations are at present struggling with this pandemic [105]. During the COVID-19 pandemic, the mental health of HPs faced serious problems. Death to their colleagues and threats to their lives, the fear of getting infected, the nonattendance of a strong psychological supportive system, and high workload all expanded mental health disorders among HPs [53, 106, 107]. However, only a few studies have investigated the psychiatric morbidity and mental health problems among HPs during the COVID-19 pandemic and no study has yet been conducted to find the variation of psychological status over time among health workers during the COVID-19 pandemic. In light of information extracted from the included studies, a significant proportion of the analyzed sample demonstrated a level of mental health problems among HPs.
In this meta-analysis, 83 studies were included after evaluating the overall quality of the articles with a 90.70% response rate. Among the total participants, on average, 37.51% were physicians, 50.16% were nurses, and 30.33% were other health professionals. Besides, 29.97% were males among the participated HPs (See Table 1). The pooled prevalence of depression, anxiety, stress, and insomnia was 37.12% (95% CI: 31.86–42.43) (Figure 3), 41.42% (95% CI: 36.17–46.68) (Figure 4), 44.86% (95% CI: 36.98–52.74) (Figure 5), and 43.76% (95% CI: 35.83–51.68) (Figure 6), respectively. These prevalence estimates were consistently lower in earlier studies [12, 13]. The sub-group analysis based on study duration shows that the pooled prevalence of depression and anxiety was increasing over time during the pandemic (Figures 7 and 8). The pooled prevalence of depression increased from 32.50% from January to March 2020 to 39.62% from April to June 2020. Then during July and September 2020, the prevalence estimate became 46.88% (Figures 7a and 8). Similarly, the prevalence of anxiety increased from 30.68% during January–March 2020 to 48% during April–June 2020 and then further increased to 60.79% during June–September 2020 (Figures 7b and 8). The pooled prevalence of stress during April–June 2020 rose upward to 46.31% from 38.14% during January–March 2020 but then decreased to 41.57% during June–September 2020 (Figures 7c and 8). The pooled prevalence of insomnia became 48.79% during April–June 2020 from 42.46% during January–March 2020 (see Figures 7d and 8). In our subgroup analysis, it is vivid that the prevalence of psychological morbidities varies across countries of the world. The healthcare workers in Germany were found to have the highest level of depression. HPs in Jordan faced the highest level of anxiety, in Canada the highest level of stress, and in Egypt the highest level of insomnia. The reverse scenarios (lowest estimates) were found for depression and anxiety in South Korea, for stress in Ghana, and for insomnia in Greece [28] (Table 3). The psychological tools that measured the highest pooled prevalence of depression of 47.02% using 9 studies [2, 31, 46, 53, 57, 65, 85, 87, 90], anxiety of 58.06% using 9 studies [2, 31, 46, 53, 57, 65, 85, 87, 90], stress of 69.46% using 5 studies [24, 69, 86, 100, 103], and insomnia of 46.58% using 16 studies [8, 24, 27, 32, 33, 50, 53, 54, 56, 60, 86, 88, 90, 91, 95] were HADS, HADS, PSS and ISI respectively. On the contrary, HAMD, SAS, PTSD, and PSQI tools were used to measure the lowest pooled prevalence of depression of 20.10% using one studies [49], anxiety of 19.39% using 8 studies [45, 55, 61, 71, 72, 93, 98, 101], stress of 26.43% using 2 studies [36, 47], and insomnia of 26.39% using 2 studies [41, 49] (Table 4).
Previous reports of SARS infections' acute effect on health professionals' mental health revealed that high levels of depression, anxiety, stress, fear, and insomnia were common [61, 108]. SARS virus outbreaks occurred over the last decade as an emerging infectious disease, observed first in China and afterward spread to 29 nations in 2002 [109]. A study observed that 89% of the health professionals faced psychological problems during that SARS outbreak period [54]. Another study observed the psychological impact of SARS and found the prevalence of depression, anxiety, insomnia in HPs as 74.20%, 77.4%, and 52.3%, respectively. A study [110] using the GHQ-2 questionnaire showed that around 57% of HPs suffered from psychological distress during the SARS outbreak. Similarly, in the initial stages of the COVID-19 outbreak, HPs showed higher psychological distress like depression, anxiety, stress, and insomnia which were assessed through PHQ-9, GAD-7, DASS-21, and AIS in several studies. Our findings were also consistent with the previous studies on psychological health among HPs during SARS and COVID-19 outbreak.
A worldwide pandemic can be a significant reason for fear and stress. During the SARS epidemic, HPs expressed anxiety, fear and some of them wanted to leave their job [111]. As compared to the SARS epidemic, nowadays the quick spread of information (misinformation) may cause greater public fear, depression, and trouble. HPs’ care for patients with a contagious disease (COVID-19 patients) resulted in fear, panic, and distress among them [112, 113]. Furthermore, they feared getting infected and additionally transmitting the disease to their family members and relatives [111]. Isolation and working with high-hazard departments and contact with contaminated individuals were considered as the most contributing reasons for trauma, fear, etc. [114] among HPs. A study showed that a substantial proportion (70.6%) of HPs reported stress during the COVID-19 pandemic [115]. Additionally, several studies demonstrated that the HPs experienced mental disturbances, anxiety, and nervousness to various degrees [102]. Our findings of a higher prevalence of depression, anxiety, stress, and insomnia are also consistent with previous findings.
Globally, COVID-19 has affected an enormous number of frontline HPs. In China, more than 3000 HPs were infected by COVID-19 until March 2020 [116]. A similar situation was also observed in previous outbreaks of SARS [117]. During the Middle East Respiratory Syndrome (MERS) outbreak, a Saudi report published that very nearly two-third of HPs felt in danger of getting infected with MERS-CoV and felt hazardous at work [118]. Several studies in Sierra Leone, Guinea, and Liberia observed nearly 6–8% of HPs infected by the Ebola virus [119]. Similarly, many early studies of COVID-19 among HPs found the reason for becoming infected by COVID-19 and as a result (Cavallo, Donoho, and Forman 2020), emerged fear and distress among HPs. As a result, the HPs are at an increased risk of contamination by COVID-19 and it would additionally worsen the current situation which could result in the lack of skilled health workers. Furthermore, HPs also feel vulnerable to getting contaminated and feared about the shortage of emergency medical equipment supplies and PPEs [120]. As a result, the HPs faced considerable stress, depression, obsession-compulsion, and feel unsafe to work as the infection rate increases [118]. Our findings are also consistent with the previous studies and found the higher pooled prevalence of depression, stress, anxiety, and insomnia.
Even though the present meta-studies found that mental issues are emergency health issues among the HPs as they are struggling with a highly infectious disease, most HPs are working in isolated wards without accepting sufficient support to improve their psychological health status. High-quality data on the mental health effects caused by the COVID-19 pandemic across vulnerable groups such as healthcare professionals is of massive importance [121]. Reviews and meta-analyses of this type are inevitable for supporting public health worldwide and to cut out the knowledge gap in the care of mental health disorders [122]. Therefore appropriate psychological support, encouragement, and motivational interventions, protective intervention, and staff support measures are urgently needed to address those issues. The funding bodies and governments can use these study results as a tool to ensure sustainable development in mental health by supporting the prioritization and allocation of funds for mental health.
5. Strengths
The main strength of this systematic review and meta-analysis was that we conducted the first comprehensive review on four major psychological morbidities namely depression, anxiety, stress, and insomnia during the COVID-19 pandemic. As per our knowledge, for the first time, we depicted the changes in the prevalence estimates of those psychological morbidities by three periods during the COVID-19 pandemic.
6. Limitations
Our studies have few limitations. First, all the studies we included, in the final analysis, were cross-sectional. Second, for the same test, different studies were considered by different assessment scales for screening health professionals. Third, among the included studies, some of the studies may consider the same population as the studies were conducted within the same country. Fourth, we may have missed including some articles in the final analysis as those were not published in English.
7. Recommendation
This study exhibited the need for further research and intervention on the mental health of healthcare workers. Especially, future investigations need to focus on identifying the responsible factors that are associated with the increase of the prevalence of depression, anxiety, stress, and insomnia. It is also crucial to observe the changes in those psychological morbidities from pre-COVID to COVID scenarios. Additionally, from the methodological point of view, to get more reliable estimates of psychological prevalence, researchers need to use the same assessment tools. We would like to recommend DASS-21 for assessing depression, anxiety, and stress because of its excellent consistency, convenience, and discriminative validity in results [123]. In some previous studies, this tool also showed adequate psychometric properties in the validation for healthcare workers and the general population [78, 124, 125]. As the most established and useful tool to quantify insomnia severity [126, 127], ISI should be selected.
8. Conclusions
To conclude, our systematic review and meta-analysis give a convenient and far-reaching amalgamation of the existing manifestation highlighting the high prevalence rates of depression, anxiety, stress, and insomnia among healthcare workers. The knowledge of the physical and mental health of the health care workers can help to implement interventions that are essential to enhance psychological resilience and strengthen the healthcare systems’ capacity.
Declarations
Author contribution statement
SM and MM conceived of the presented idea. SH and AM conducted the searches. They also completed the screening text, extraction, and analysis of the data with the input from SM. SH and SM wrote the first draft of the manuscript with input from MI and MM. MI, AM, and MM provided critical feedback. All authors discussed the results and contributed to the final manuscript.
Funding statement
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Data availability statement
Data included in article/supplementary material/referenced in article.
Declaration of interests statement
The authors declare no conflict of interest.
Additional information
No additional information is available for this paper.
References
- 1.Wang C., Horby P.W., Hayden F.G., Gao G.F. A novel coronavirus outbreak of global health concern. Lancet. 2020;395:470–473. doi: 10.1016/S0140-6736(20)30185-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zhang C., Yang L., Liu S., Ma S., Wang Y., Cai Z., Du H., Li R., Kang L., Su M., Zhang J., Liu Z., Zhang B. Survey of insomnia and related social psychological factors among medical staff involved in the 2019 novel coronavirus disease outbreak. Front. Psychiatr. 2020;11 doi: 10.3389/fpsyt.2020.00306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Arora T., Grey I. Health behaviour changes during COVID-19 and the potential consequences: a mini-review. J. Health Psychol. 2020;25:1155–1163. doi: 10.1177/1359105320937053. [DOI] [PubMed] [Google Scholar]
- 4.Keni R., Alexander A., Nayak P.G., Mudgal J., Nandakumar K. COVID-19: emergence, spread, possible treatments, and global burden. Front. Public Health. 2020;8 doi: 10.3389/fpubh.2020.00216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Xiong J., Lipsitz O., Nasri F., Lui L.M.W., Gill H., Phan L., Chen-Li D., Iacobucci M., Ho R., Majeed A., McIntyre R.S. Impact of COVID-19 pandemic on mental health in the general population: a systematic review. J. Affect. Disord. 2020;277:55–64. doi: 10.1016/j.jad.2020.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sher L. The impact of the COVID-19 pandemic on suicide rates. QJM Int. J. Med. 2020;113:707–712. doi: 10.1093/qjmed/hcaa202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Li Z., Ge J., Yang M., Feng J., Qiao M., Jiang R., Bi J., Zhan G., Xu X., Wang L., Zhou Q., Zhou C., Pan Y., Liu S., Zhang H., Yang J., Zhu B., Hu Y., Hashimoto K., Jia Y., Wang H., Wang R., Liu C., Yang C. Vicarious traumatization in the general public, members, and non-members of medical teams aiding in COVID-19 control. Brain Behav. Immun. 2020;88:916–919. doi: 10.1016/j.bbi.2020.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zhang W., Wang K., Yin L., Zhao W., Xue Q., Peng M., Min B., Tian Q., Leng H., Du J., Chang H., Yang Y., Li W., Shangguan F., Yan T., Dong H., Han Y., Wang Y., Cosci F., Wang H. Mental health and psychosocial problems of medical health workers during the COVID-19 epidemic in China, psychother. Psychosom. 2020;89:242–250. doi: 10.1159/000507639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zhang Y., Xie S., Wang P., Wang G., Zhang L., Cao X., Wu W., Bian Y., Huang F., Luo N., Luo M., Xiao Q. Factors influencing mental health of medical workers during the COVID-19 outbreak. Front. Public Health. 2020;8 doi: 10.3389/fpubh.2020.00491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wilson J.P., Sigman M.R. Psychol. Debriefing Theory Pract. Evid. Cambridge University Press; New York, NY, US: 2000. Theoretical perspectives of traumatic stress and debriefings; pp. 58–68. [Google Scholar]
- 11.da Silva Neto R.M., Benjamim C.J.R., de Medeiros Carvalho P.M., Neto M.L.R. Psychological effects caused by the COVID-19 pandemic in health professionals: a systematic review with meta-analysis. Prog. Neuro-Psychopharmacol. Biol. Psychiatry. 2021;104:110062. doi: 10.1016/j.pnpbp.2020.110062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Salari N., Khazaie H., Hosseinian-Far A., Khaledi-Paveh B., Kazeminia M., Mohammadi M., Shohaimi S., Daneshkhah A., Eskandari S. The prevalence of stress, anxiety and depression within front-line healthcare workers caring for COVID-19 patients: a systematic review and meta-regression. Hum. Resour. Health. 2020;18:100. doi: 10.1186/s12960-020-00544-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pappa S., Ntella V., Giannakas T., Giannakoulis V.G., Papoutsi E., Katsaounou P. Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: a systematic review and meta-analysis. Brain Behav. Immun. 2020;88:901–907. doi: 10.1016/j.bbi.2020.05.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ren X., Huang W., Pan H., Huang T., Wang X., Ma Y. Mental health during the covid-19 outbreak in China: a meta-analysis. Psychiatr. Q. 2020;91:1033–1045. doi: 10.1007/s11126-020-09796-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Salari N., Hosseinian-Far A., Jalali R., Vaisi-Raygani A., Rasoulpoor S., Mohammadi M., Rasoulpoor S., Khaledi-Paveh B. Prevalence of stress, anxiety, depression among the general population during the COVID-19 pandemic: a systematic review and meta-analysis. Glob. Health. 2020;16:57. doi: 10.1186/s12992-020-00589-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Salari N., Mohammadi M., Vaisi-Raygani A., Abdi A., Shohaimi S., Khaledipaveh B., Daneshkhah A., Jalali R. The prevalence of severe depression in Iranian older adult: a meta-analysis and meta-regression. BMC Geriatr. 2020;20:39. doi: 10.1186/s12877-020-1444-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Deng J., Zhou F., Hou W., Silver Z., Wong C.Y., Chang O., Huang E., Zuo Q.K. The prevalence of depression, anxiety, and sleep disturbances in COVID-19 patients: a meta-analysis. Ann. N. Y. Acad. Sci. 2020 doi: 10.1111/nyas.14506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cooke J.E., Eirich R., Racine N., Madigan S. Prevalence of posttraumatic and general psychological stress during COVID-19: a rapid review and meta-analysis. Psychiatr. Res. 2020;292:113347. doi: 10.1016/j.psychres.2020.113347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Liberati A., Altman D.G., Tetzlaff J., Mulrow C., Gøtzsche P.C., Ioannidis J.P.A., Clarke M., Devereaux P.J., Kleijnen J., Moher D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. J. Clin. Epidemiol. 2009;62:e1–e34. doi: 10.1016/j.jclinepi.2009.06.006. [DOI] [PubMed] [Google Scholar]
- 20.StataCorp. StataCorp LLC, n.d; College Station, TX: 2019. Stata Statistical Software: Release 16. [Google Scholar]
- 21.Higgins J.P.T., Thompson S.G., Deeks J.J., Altman D.G. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557–560. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Baker W.L., White C.M., Cappelleri J.C., Kluger J., Coleman C.I. Health outcomes, policy, and economics (HOPE) collaborative group, understanding heterogeneity in meta-analysis: the role of meta-regression. Int. J. Clin. Pract. 2009;63:1426–1434. doi: 10.1111/j.1742-1241.2009.02168.x. [DOI] [PubMed] [Google Scholar]
- 23.Petitti D.B. Approaches to heterogeneity in meta-analysis. Stat. Med. 2001;20:3625–3633. doi: 10.1002/sim.1091. [DOI] [PubMed] [Google Scholar]
- 24.Elkholy H., Tawfik F., Ibrahim I., Salah El-din W., Sabry M., Mohammed S., Hamza M., Alaa M., Fawzy A.Z., Ashmawy R., Sayed M., Omar A.N. Mental health of frontline healthcare workers exposed to COVID-19 in Egypt: a call for action. Int. J. Soc. Psychiatr. 2020 doi: 10.1177/0020764020960192. [DOI] [PubMed] [Google Scholar]
- 25.Ahn M.H., Shin Y.-W., Suh S., Kim J.H., Kim H.J., Lee K.-U., Chung S. 2020. High Work-Related Stress and Anxiety Response to COVID-19 Among Healthcare Workers in South Korea: SAVE Study. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Alnazly E., Khraisat O.M., Al-Bashaireh A.M., Bryant C.L. Anxiety, depression, stress, fear and social support during COVID-19 pandemic among Jordanian healthcare workers. PloS One. 2021;16 doi: 10.1371/journal.pone.0247679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Alshekaili M., Hassan W., Said N.A., Sulaimani F.A., Jayapal S.K., Al-Mawali A., Chan M.F., Mahadevan S., Al-Adawi S. Factors associated with mental health outcomes across healthcare settings in Oman during COVID-19: frontline versus non-frontline healthcare workers. BMJ Open. 2020;10 doi: 10.1136/bmjopen-2020-042030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ofori A.A., Osarfo J., Agbeno E.K., Manu D.O., Amoah E. Vol. 9. SAGE Open Med; 2021. Psychological Impact of COVID-19 on Health Workers in Ghana: A Multicentre, Cross-Sectional Study. 20503121211000920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Blekas A., Voitsidis P., Athanasiadou M., Parlapani E., Chatzigeorgiou A.F., Skoupra M., Syngelakis M., Holeva V., Diakogiannis I. COVID-19: PTSD symptoms in Greek health care professionals. Psychol. Trauma Theory Res. Pract. Pol. 2020;12:812. doi: 10.1037/tra0000914. [DOI] [PubMed] [Google Scholar]
- 30.Arafa A., Mohammed Z., Mahmoud O., Elshazley M., Ewis A. Depressed, anxious, and stressed: what have healthcare workers on the frontlines in Egypt and Saudi Arabia experienced during the COVID-19 pandemic? J. Affect. Disord. 2021;278:365–371. doi: 10.1016/j.jad.2020.09.080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Tan B.Y.Q., Kanneganti A., Lim L.J.H., Tan M., Chua Y.X., Tan L., Sia C.H., Denning M., Goh E.T., Purkayastha S., Kinross J., Sim K., Chan Y.H., Ooi S.B.S. Burnout and associated factors among health care workers in Singapore during the COVID-19 pandemic. J. Am. Med. Dir. Assoc. 2020;21:1751–1758. doi: 10.1016/j.jamda.2020.09.035. e5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Cai Q., Feng H., Huang J., Wang M., Wang Q., Lu X., Xie Y., Wang X., Liu Z., Hou B., Ouyang K., Pan J., Li Q., Fu B., Deng Y., Liu Y. The mental health of frontline and non-frontline medical workers during the coronavirus disease 2019 (COVID-19) outbreak in China: a case-control study. J. Affect. Disord. 2020;275:210–215. doi: 10.1016/j.jad.2020.06.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Chatterjee S.S., Chakrabarty M., Banerjee D., Grover S., Chatterjee S.S., Dan U. Stress, sleep and psychological impact in healthcare workers during the early phase of COVID-19 in India: a factor Analysis. Front. Psychol. 2021;12 doi: 10.3389/fpsyg.2021.611314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Chew N.W.S., Lee G.K.H., Tan B.Y.Q., Jing M., Goh Y., Ngiam N.J.H., Yeo L.L.L., Ahmad A., Ahmed Khan F., Napolean Shanmugam G., Sharma A.K., Komalkumar R.N., Meenakshi P.V., Shah K., Patel B., Chan B.P.L., Sunny S., Chandra B., Ong J.J.Y., Paliwal P.R., Wong L.Y.H., Sagayanathan R., Chen J.T., Ying Ng A.Y., Teoh H.L., Tsivgoulis G., Ho C.S., Ho R.C., Sharma V.K. A multinational, multicentre study on the psychological outcomes and associated physical symptoms amongst healthcare workers during COVID-19 outbreak. Brain Behav. Immun. 2020;88:559–565. doi: 10.1016/j.bbi.2020.04.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Conti C., Fontanesi L., Lanzara R., Rosa I., Porcelli P. Fragile heroes. The psychological impact of the COVID-19 pandemic on health-care workers in Italy. PloS One. 2020;15 doi: 10.1371/journal.pone.0242538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Lamb D., Gnanapragasam S., Greenberg N., Bhundia R., Carr E., Hotopf M., Razavi R., Raine R., Cross S., Dewar A., Docherty M., Dorrington S., Hatch S.L., Wilson-Jones C., Leightley D., Madan I., Marlow S., McMullen I., Rafferty A.M., Parsons M., Polling C., Serfioti D., Aitken P., French V., Gaunt H., Morris-Bone J., Harris R., Simela C., Stevelink S.A.M., Wessely S., O. behalf of the N.C. Consortium The psychosocial impact of the COVID-19 pandemic on 4,378 UK healthcare workers and ancillary staff: initial baseline data from a cohort study collected during the first wave of the pandemic. MedRxiv. 2021:2021. doi: 10.1136/oemed-2020-107276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Salopek-Žiha D., Hlavati M., Gvozdanović Z., Gašić M., Placento H., Jakić H., Klapan D., Šimić H. Differences IN distress and coping with the COVID-19 stressor IN nurses and physicians. Psychiatr. Danub. 2020;32:287–293. doi: 10.24869/psyd.2020.287. [DOI] [PubMed] [Google Scholar]
- 38.Du J., Mayer G., Hummel S., Oetjen N., Gronewold N., Zafar A., Schultz J.-H. Mental health burden in different professions during the final stage of the COVID-19 lockdown in China: cross-sectional survey study. J. Med. Internet Res. 2020;22 doi: 10.2196/24240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Mattila E., Peltokoski J., Neva M.H., Kaunonen M., Helminen M., Parkkila A.-K. COVID-19: anxiety among hospital staff and associated factors. Ann. Med. 2021;53:237–246. doi: 10.1080/07853890.2020.1862905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Evanoff B.A., Strickland J.R., Dale A.M., Hayibor L., Page E., Duncan J.G., Kannampallil T., Gray D.L. Work-related and personal factors associated with mental well-being during the COVID-19 response: survey of health care and other workers. J. Med. Internet Res. 2020;22 doi: 10.2196/21366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ferini-Strambi L., Zucconi M., Casoni F., Salsone M. COVID-19 and sleep in medical staff: reflections, clinical evidences, and perspectives. Curr. Treat. Options Neurol. 2020;22:29. doi: 10.1007/s11940-020-00642-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Giusti E.M., Pedroli E., D’Aniello G.E., Stramba Badiale C., Pietrabissa G., Manna C., Stramba Badiale M., Riva G., Castelnuovo G., Molinari E. The psychological impact of the COVID-19 outbreak on health professionals: a cross-sectional study. Front. Psychol. 2020;11 doi: 10.3389/fpsyg.2020.01684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Gorini A., Fiabane E., Sommaruga M., Barbieri S., Sottotetti F., La Rovere M.T., Tremoli E., Gabanelli P. Mental health and risk perception among Italian healthcare workers during the second month of the Covid-19 pandemic. Arch. Psychiatr. Nurs. 2020;34:537–544. doi: 10.1016/j.apnu.2020.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Greene T., Harju-Seppänen J., Adeniji M., Steel C., Grey N., Brewin C.R., Bloomfield M.A., Billings J. Predictors and rates of PTSD, depression and anxiety in UK frontline health and social care workers during COVID-19. Eur. J. Psychotraumatol. 2021;12:1882781. doi: 10.1080/20008198.2021.1882781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Guo J., Liao L., Wang B., Li X., Guo L., Tong Z., Guan Q., Zhou M., Wu Y., Zhang J., Gu Y. Social Science Research Network; Rochester, NY: 2020. Psychological Effects of COVID-19 on Hospital Staff: A National Cross-Sectional Survey of China Mainland. [Google Scholar]
- 46.Hasan M.T., Hossain S., Safa F., Anjum A., Khan A.H., Koly K.N., Alam S.F., Rafi M.A., Podder V., Trisa T.I., Nodi R.N., Azad D.T., Ashraf F., Akther S.M.Q., Ahmed H.U., Rosenbaum S., Thornicroft G. Prevalence of anxiety and depressive symptoms among physicians during the COVID-19 pandemic in Bangladesh: a cross-sectional study. MedRxiv. 2020:2020. doi: 10.1017/gmh.2022.30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Hennein R., Mew E.J., Lowe S.R. Socio-ecological predictors of mental health outcomes among healthcare workers during the COVID-19 pandemic in the United States. PloS One. 2021;16 doi: 10.1371/journal.pone.0246602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Hong S., Ai M., Xu X., Wang W., Chen J., Zhang Q., Wang L., Kuang L. Immediate psychological impact on nurses working at 42 government-designated hospitals during COVID-19 outbreak in China: a cross-sectional study. Nurs. Outlook. 2021;69:6–12. doi: 10.1016/j.outlook.2020.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Huang Y., Zhao N. Generalized anxiety disorder, depressive symptoms and sleep quality during COVID-19 outbreak in China: a web-based cross-sectional survey. Psychiatr. Res. 2020;288:112954. doi: 10.1016/j.psychres.2020.112954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Que J., Shi L., Deng J., Liu J., Zhang L., Wu S., Gong Y., Huang W., Yuan K., Yan W., Sun Y., Ran M., Bao Y., Lu L. Psychological impact of the COVID-19 pandemic on healthcare workers: a cross-sectional study in China. Gen. Psychiat. 2020;33 doi: 10.1136/gpsych-2020-100259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Mira J.J., Carrillo I., Guilabert M., Mula A., Martin-Delgado J., Pérez-Jover M.V., Vicente M.A., Fernández C. Acute stress of the healthcare workforce during the COVID-19 pandemic evolution: a cross-sectional study in Spain. BMJ Open. 2020;10 doi: 10.1136/bmjopen-2020-042555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Khalaf O.O., Khalil M.A., Abdelmaksoud R. Coping with depression and anxiety in Egyptian physicians during COVID-19 pandemic, Middle East. Curr. Psychiat. 2020;27:63. [Google Scholar]
- 53.Khanal P., Devkota N., Dahal M., Paudel K., Joshi D. Mental health impacts among health workers during COVID-19 in a low resource setting: a cross-sectional survey from Nepal. Glob. Health. 2020;16:89. doi: 10.1186/s12992-020-00621-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Lai J., Ma S., Wang Y., Cai Z., Hu J., Wei N., Wu J., Du H., Chen T., Li R., Tan H., Kang L., Yao L., Huang M., Wang H., Wang G., Liu Z., Hu S. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw. Open. 2020;3 doi: 10.1001/jamanetworkopen.2020.3976. e203976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Lasalvia A., Bonetto C., Porru S., Carta A., Tardivo S., Bovo C., Ruggeri M., Amaddeo F. Psychological impact of COVID-19 pandemic on healthcare workers in a highly burdened area of north-east Italy. Epidemiol. Psychiatr. Sci. 2021;30 doi: 10.1017/S2045796020001158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Lee J., Lee H.J., Hong Y., Shin Y.-W., Chung S., Park J. Risk perception, unhealthy behavior, and anxiety due to viral epidemic among healthcare workers: the relationships with depressive and insomnia symptoms during COVID-19. Front. Psychiatr. 2021;12 doi: 10.3389/fpsyt.2021.615387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Hassannia L., Taghizadeh F., Moosazadeh M., Zarghami M., Taghizadeh H., Dooki A.F., Fathi M., Navaei R.A., Hedayatizadeh-Omran A. Anxiety and depression in health workers and general population during COVID-19 epidemic in Iran: a web-based cross-sectional study. MedRxiv. 2020 doi: 10.1002/npr2.12153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Lenzo V., Quattropani M.C., Sardella A., Martino G., Bonanno G.A. Depression, anxiety, and stress among healthcare workers during the COVID-19 outbreak and relationships with expressive flexibility and context sensitivity. Front. Psychol. 2021;12 doi: 10.3389/fpsyg.2021.623033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Labrague L.J. COVID-19 anxiety among frontline nurses: predictive role of organisational support. Pers. Res. Soc. Support. 2020:25. doi: 10.1111/jonm.13121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Liang Y., Wu K., Zhou Y., Huang X., Zhou Y., Liu Z. Mental health in frontline medical workers during the 2019 novel coronavirus disease epidemic in China: a comparison with the general population. Int. J. Environ. Res. Publ. Health. 2020;17:6550. doi: 10.3390/ijerph17186550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Liu C.-Y., Yang Y., Zhang X.-M., Xu X., Dou Q.-L., Zhang W.-W., Cheng A.S.K. The prevalence and influencing factors in anxiety in medical workers fighting COVID-19 in China: a cross-sectional survey, Epidemiol. Infect. 2020;148 doi: 10.1017/S0950268820001107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Liu Y., Wang L., Chen L., Zhang X., Bao L., Shi Y. Mental health status of paediatric medical workers in China during the COVID-19 outbreak. Front. Psychiatr. 2020;11 doi: 10.3389/fpsyt.2020.00702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Liu Y., Chen H., Zhang N., Wang X., Fan Q., Zhang Y., Huang L., Hu B., Li M. Anxiety and depression symptoms of medical staff under COVID-19 epidemic in China. J. Affect. Disord. 2021;278:144–148. doi: 10.1016/j.jad.2020.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Lu W., Wang H., Lin Y., Li L. Psychological status of medical workforce during the COVID-19 pandemic: a cross-sectional study. Psychiatr. Res. 2020;288:112936. doi: 10.1016/j.psychres.2020.112936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Luceño-Moreno L., Talavera-Velasco B., García-Albuerne Y., Martín-García J. Symptoms of posttraumatic stress, anxiety, depression, levels of resilience and burnout in Spanish health personnel during the COVID-19 pandemic. Int. J. Environ. Res. Publ. Health. 2020;17:5514. doi: 10.3390/ijerph17155514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Kaveh M., Davari-tanha F., Varaei S., Shirali E., Shokouhi N., Nazemi P., Ghajarzadeh M., Feizabad E., Ashraf M.A. Anxiety levels among Iranian health care workers during the COVID-19 surge: a cross-sectional study. MedRxiv. 2020:2020. [Google Scholar]
- 67.Mathur S., Sharma D., Solanki R.K., Goyal M.K. Stress-related disorders in health-care workers in COVID-19 pandemic: a cross-sectional study from India. Indian J. Med. Specialities. 2020;11:180. [Google Scholar]
- 68.Bizri M., Kassir G., Tamim H., Kobeissy F., Hayek S.E. Psychological distress experienced by physicians and nurses at a tertiary care center in Lebanon during the COVID-19 outbreak. J. Health Psychol. 2021 doi: 10.1177/1359105321991630. 1359105321991630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Mrklas K., Shalaby R., Hrabok M., Gusnowski A., Vuong W., Surood S., Urichuk L., Li D., Li X.-M., Greenshaw A.J., Agyapong V.I.O. Prevalence of perceived stress, anxiety, depression, and obsessive-compulsive symptoms in health care workers and other workers in alberta during the COVID-19 pandemic: cross-sectional survey, JMIR ment. Health. 2020;7 doi: 10.2196/22408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Nguyen P.T.L., Nguyen T.B.L., Pham A.G., Duong K.N.C., Gloria M.A.J., Vo T.V., Vo B.V., Phung T.L. Psychological stress risk factors, concerns and mental health support among health care workers in Vietnam during the coronavirus disease 2019 (COVID-19) outbreak. Front. Public Health. 2021;9 doi: 10.3389/fpubh.2021.628341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Ni J., Wang F., Liu Y., Wu M., Jiang Y., Zhou Y., Sha D. Psychological impact of the COVID-19 pandemic on Chinese health care workers: cross-sectional survey study. JMIR Ment. Health. 2021;8 doi: 10.2196/23125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Ning X., Yu F., Huang Q., Li X., Luo Y., Huang Q., Chen C. The mental health of neurological doctors and nurses in Hunan Province, China during the initial stages of the COVID-19 outbreak. BMC Psychiatr. 2020;20:436. doi: 10.1186/s12888-020-02838-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Aziznejadroshan P., Qalehsari M.Q., Zavardehi F.S. Stress, anxiety, depression among nurses caring for COVID-19 patients in babol, Iran: a logestic regression. Review. 2020 [Google Scholar]
- 74.Prasad A., Civantos A.M., Byrnes Y., Chorath K., Poonia S., Chang C., Graboyes E.M., Bur A.M., Thakkar P., Deng J., Seth R., Trosman S., Wong A., Laitman B.M., Shah J., Stubbs V., Long Q., Choby G., Rassekh C.H., Thaler E.R., Rajasekaran K. Snapshot impact of COVID-19 on mental wellness in nonphysician otolaryngology health care workers: a national study. OTO Open. 2020;4 doi: 10.1177/2473974X20948835. 2473974X20948835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Qi J., Xu J., Li B.-Z., Huang J.-S., Yang Y., Zhang Z.-T., Yao D.-A., Liu Q.-H., Jia M., Gong D.-K., Ni X.-H., Zhang Q.-M., Shang F.-R., Xiong N., Zhu C.-L., Wang T., Zhang X. The evaluation of sleep disturbances for Chinese frontline medical workers under the outbreak of COVID-19. Sleep Med. 2020;72:1–4. doi: 10.1016/j.sleep.2020.05.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Ranjan L., Gupta P., Gujar N., Baraik S. Psychological distress and quality of life among hospital staff in India during COVID-19 pandemic. Shanlax Int. J. Arts Sci. Humanit. 2021;8:55–60. [Google Scholar]
- 77.Li R., Chen Y., Lv J., Liu L., Zong S., Li H., Li H. Anxiety and related factors in frontline clinical nurses fighting COVID-19 in Wuhan. Medicine (Baltim.) 2020:99. doi: 10.1097/MD.0000000000021413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Elbay R.Y., Kurtulmuş A., Arpacıoğlu S., Karadere E. Depression, anxiety, stress levels of physicians and associated factors in Covid-19 pandemics. Psychiatr. Res. 2020;290:113130. doi: 10.1016/j.psychres.2020.113130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Salman M., Raza M.H., Mustafa Z.U., Khan T.M., Asif N., Tahir H., Shehzadi N., Hussain K. The psychological effects of COVID-19 on frontline healthcare workers and how they are coping: a web-based, cross-sectional study from Pakistan. MedRxiv. 2020:2020. doi: 10.1017/dmp.2022.4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Hassamal S., Dong F., Hassamal S., Lee C., Ogunyemi D., Neeki M.M. The psychological impact of COVID-19 on hospital staff, west. J. Emerg. Med. 2021;22:346–352. doi: 10.5811/westjem.2020.11.49015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Sandesh R., Shahid W., Dev K., Mandhan N., Shankar P., Shaikh A., Rizwan A. Impact of COVID-19 on the mental health of healthcare professionals in Pakistan. Cureus. 2020;12 doi: 10.7759/cureus.8974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Holton S., Wynter K., Trueman M., Bruce S., Sweeney S., Crowe S., Dabscheck A., Eleftheriou P., Booth S., Hitch D., Said C.M., Haines K.J., Rasmussen B., Holton S., Wynter K., Trueman M., Bruce S., Sweeney S., Crowe S., Dabscheck A., Eleftheriou P., Booth S., Hitch D., Said C.M., Haines K.J., Rasmussen B. Psychological well-being of Australian hospital clinical staff during the COVID-19 pandemic. Aust. Health Rev. 2020 doi: 10.1071/AH20203. [DOI] [PubMed] [Google Scholar]
- 83.Si M.-Y., Su X.-Y., Jiang Y., Wang W.-J., Gu X.-F., Ma L., Li J., Zhang S.-K., Ren Z.-F., Ren R., Liu Y.-L., Qiao Y.-L. Psychological impact of COVID-19 on medical care workers in China. Infect. Dis. Poverty. 2020;9:113. doi: 10.1186/s40249-020-00724-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Smith P.M., Oudyk J., Potter G., Mustard C. The Association between the Perceived Adequacy of Workplace Infection Control Procedures and Personal Protective Equipment with Mental Health Symptoms: a Cross-sectional Survey of Canadian Health-care Workers during the COVID-19 Pandemic: L’association entre le caractère adéquat perçu des procédures de contrôle des infections au travail et de l’équipement de protection personnel pour les symptômes de santé mentale. Un sondage transversal des travailleurs de la santé canadiens durant la pandémie COVID-19. Can. J. Psychiatr. 2020;66:17–24. doi: 10.1177/0706743720961729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Araç S., Dönmezdil S., Araç S., Dönmezdil S. Investigation of mental health among hospital workers in the COVID-19 pandemic: a cross-sectional study. Sao Paulo Med. J. 2020;138:433–440. doi: 10.1590/1516-3180.2020.0272.R3.21072020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Sunil R., Bhatt M.T., Bhumika T.V., Thomas N., Puranik A., Chaudhuri S., Shwethapriya R. Weathering the storm: psychological impact of COVID-19 pandemic on clinical and nonclinical healthcare workers in India. Indian J. Crit. Care Med. Peer-Rev. Off. Publ. Indian Soc. Crit. Care Med. 2021;25:16–20. doi: 10.5005/jp-journals-10071-23702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Tasnim R., Sujan M.S.H., Islam M.S., Ritu A.H., Siddique M.A.B., Toma T.Y., Nowshin R., Hasan A., Hossain S., Nahar S., Islam S., Islam M.S., Potenza M.N., van Os J. 2020. Prevalence and Correlates of Anxiety and Depression in Frontline Healthcare Workers Treating People with COVID-19 in Bangladesh. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Wasim T., e Raana G., Bushra N., Riaz A. Effect of COVID-19 pandemic on mental wellbeing of healthcare workers in tertiary care hospital. Ann. King Edw. Med. Univ. 2020;26:140–144. [Google Scholar]
- 89.Tu Z., He J., Zhou N. Sleep quality and mood symptoms in conscripted frontline nurse in Wuhan, China during COVID-19 outbreak. Medicine (Baltim.) 2020:99. doi: 10.1097/MD.0000000000020769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Wang H., Huang D., Huang H., Zhang J., Guo L., Liu Y., Ma H., Geng Q. The psychological impact of COVID-19 pandemic on medical staff in Guangdong, China: a cross-sectional study. Psychol. Med. 2020:1–9. doi: 10.1017/S0033291720002561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Wańkowicz P., Szylińska A., Rotter I. Assessment of mental health factors among health professionals depending on their contact with COVID-19 patients. Int. J. Environ. Res. Publ. Health. 2020;17:5849. doi: 10.3390/ijerph17165849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Weibelzahl S., Reiter J., Duden G. Depression and anxiety in healthcare professionals during the COVID-19 pandemic. Epidemiol. Infect. 2021;149 doi: 10.1017/S0950268821000303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Xing L., Xu M., Sun J., Wang Q.-X., Ge D., Jiang M., Du W., Li Q. Anxiety and depression in frontline health care workers during the outbreak of Covid-19. Int. J. Soc. Psychiatr. 2020 doi: 10.1177/0020764020968119. [DOI] [PubMed] [Google Scholar]
- 94.An Y., Yang Y., Wang A., Li Y., Zhang Q., Cheung T., Ungvari G.S., Qin M.-Z., An F.-R., Xiang Y.-T. Prevalence of depression and its impact on quality of life among frontline nurses in emergency departments during the COVID-19 outbreak. J. Affect. Disord. 2020;276:312–315. doi: 10.1016/j.jad.2020.06.047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Zhang H., Shi Y., Jing P., Zhan P., Fang Y., Wang F. Posttraumatic stress disorder symptoms in healthcare workers after the peak of the COVID-19 outbreak: a survey of a large tertiary care hospital in Wuhan. Psychiatr. Res. 2020;294:113541. doi: 10.1016/j.psychres.2020.113541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Zheng R., Zhou Y., Qiu M., Yan Y., Yue J., Yu L., Lei X., Tu D., Hu Y. Prevalence and associated factors of depression, anxiety, and stress among Hubei pediatric nurses during COVID-19 pandemic, Compr. Psychiatry. 2021;104:152217. doi: 10.1016/j.comppsych.2020.152217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Zhu Z., Xu S., Wang H., Liu Z., Wu J., Li G., Miao J., Zhang C., Yang Y., Sun W., Zhu S., Fan Y., Hu J., Liu J., Wang W. COVID-19 in wuhan: immediate psychological impact on 5062 health workers. Psychiatry Clin. Psychol. 2020 [Google Scholar]
- 98.Zhu J., Sun L., Zhang L., Wang H., Fan A., Yang B., Li W., Xiao S. Prevalence and influencing factors of anxiety and depression symptoms in the first-line medical staff fighting against COVID-19 in gansu. Front. Psychiatr. 2020;11 doi: 10.3389/fpsyt.2020.00386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Saleem Z., Majeed M.M., Rafique S., Siqqiqui Z., Ghandhi D., Tariq H., Zegarra-Valdivia J.A. COVID-19 pandemic fear and anxiety among healthcare professionals in Pakistan. Review. 2020 [Google Scholar]
- 100.Badahdah A., Khamis F., Al Mahyijari N., Al Balushi M., Al Hatmi H., Al Salmi I., Albulushi Z., Al Noomani J. The mental health of health care workers in Oman during the COVID-19 pandemic. Int. J. Soc. Psychiatr. 2020 doi: 10.1177/0020764020939596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Huang L., Wang Y., Liu J., Ye P., Chen X., Xu H., Qu H., Ning G. Factors influencing anxiety of health care workers in the radiology department with high exposure risk to COVID-19. Med. Sci. Monit. Int. Med. J. Exp. Clin. Res. 2020;26 doi: 10.12659/MSM.926008. 1-e926008-e926009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Pan X., Xiao Y., Ren D., Xu Z.-M., Zhang Q., Yang L.-Y., Liu F., Hao Y.-S., Zhao F., Bai Y.-H. Prevalence of mental health problems and associated risk factors among military healthcare workers in specialized COVID-19 hospitals in Wuhan, China: a cross-sectional survey. Asia Pac. Psychiatr. 2020 doi: 10.1111/appy.12427. n/a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Wilson W., Raj J.P., Rao S., Ghiya M., Nedungalaparambil N.M., Mundra H., Mathew R. Prevalence and predictors of stress, anxiety, and depression among healthcare workers managing COVID-19 pandemic in India: a nationwide observational study. Indian J. Psychol. Med. 2020;42:353–358. doi: 10.1177/0253717620933992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Chen B., Li Q., Zhang H., Zhu J., Yang X., Wu Y., Xiong J., Li F., Wang H., Chen Z. The psychological impact of COVID-19 outbreak on medical staff and the general public. Curr. Psychol. 2020 doi: 10.1007/s12144-020-01109-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Montemurro N. The emotional impact of COVID-19: from medical staff to common people. Brain Behav. Immun. 2020;87:23–24. doi: 10.1016/j.bbi.2020.03.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Ji D., Ji Y.-J., Duan X.-Z., Li W.-G., Sun Z.-Q., Song X.-A., Meng Y.-H., Tang H.-M., Chu F., Niu X.-X., Chen G.-F., Li J., Duan H.-J. Prevalence of psychological symptoms among Ebola survivors and healthcare workers during the 2014-2015 Ebola outbreak in Sierra Leone: a cross-sectional study. Oncotarget. 2017;8:12784–12791. doi: 10.18632/oncotarget.14498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Adams J.G., Walls R.M. Supporting the health care workforce during the COVID-19 global epidemic. J. Am. Med. Assoc. 2020;323:1439–1440. doi: 10.1001/jama.2020.3972. [DOI] [PubMed] [Google Scholar]
- 108.Maunder R.G., Lancee W.J., Rourke S., Hunter J.J., Goldbloom D., Balderson K., Petryshen P., Steinberg R., Wasylenki D., Koh D., Fones C.S.L. Factors associated with the psychological impact of severe acute respiratory syndrome on nurses and other hospital workers in toronto. Psychosom. Med. 2004;66:938–942. doi: 10.1097/01.psy.0000145673.84698.18. [DOI] [PubMed] [Google Scholar]
- 109.Brooks S.K., Dunn R., Amlôt R., Rubin G.J., Greenberg N. A systematic, thematic review of social and occupational factors associated with psychological outcomes in healthcare employees during an infectious disease outbreak. J. Occup. Environ. Med. 2018;60:248–257. doi: 10.1097/JOM.0000000000001235. [DOI] [PubMed] [Google Scholar]
- 110.Tam C.W.C., Pang E.P.F., Lam L.C.W., Chiu H.F.K. Severe acute respiratory syndrome (SARS) in Hong Kong in 2003: stress and psychological impact among frontline healthcare workers. Psychol. Med. 2004;34:1197–1204. doi: 10.1017/s0033291704002247. [DOI] [PubMed] [Google Scholar]
- 111.Chen R., Chou K.-R., Huang Y.-J., Wang T.-S., Liu S.-Y., Ho L.-Y. Effects of a SARS prevention programme in Taiwan on nursing staff’s anxiety, depression and sleep quality: a longitudinal survey. Int. J. Nurs. Stud. 2006;43:215–225. doi: 10.1016/j.ijnurstu.2005.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Wheaton M.G., Prikhidko A., Messner G. Is fear of COVID-19 contagious? The effects of emotion contagion and social media use on anxiety in response to the coronavirus pandemic. Front. Psychol. 2020;11:3594. doi: 10.3389/fpsyg.2020.567379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Bendau A., Petzold M.B., Pyrkosch L., Mascarell Maricic L., Betzler F., Rogoll J., Große J., Ströhle A., Plag J. Associations between COVID-19 related media consumption and symptoms of anxiety, depression and COVID-19 related fear in the general population in Germany. Eur. Arch. Psychiatr. Clin. Neurosci. 2021;271:283–291. doi: 10.1007/s00406-020-01171-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Kang L., Ma S., Chen M., Yang J., Wang Y., Li R., Yao L., Bai H., Cai Z., Xiang Yang B., Hu S., Zhang K., Wang G., Ma C., Liu Z. Impact on mental health and perceptions of psychological care among medical and nursing staff in Wuhan during the 2019 novel coronavirus disease outbreak: a cross-sectional study. Brain Behav. Immun. 2020;87:11–17. doi: 10.1016/j.bbi.2020.03.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Lu W., Wang H., Lin Y., Li L. Psychological status of medical workforce during the COVID-19 pandemic: a cross-sectional study. Psychiatr. Res. 2020;288:112936. doi: 10.1016/j.psychres.2020.112936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Remuzzi A., Remuzzi G. COVID-19 and Italy: what next? Lancet. 2020;395:1225–1228. doi: 10.1016/S0140-6736(20)30627-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Chan-Yeung M. Severe acute respiratory syndrome (SARS) and healthcare workers. Int. J. Occup. Environ. Health. 2004;10:421–427. doi: 10.1179/oeh.2004.10.4.421. [DOI] [PubMed] [Google Scholar]
- 118.Abolfotouh M.A., AlQarni A.A., Al-Ghamdi S.M., Salam M., Al-Assiri M.H., Balkhy H.H. An assessment of the level of concern among hospital-based health-care workers regarding MERS outbreaks in Saudi Arabia. BMC Infect. Dis. 2017;17:4. doi: 10.1186/s12879-016-2096-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Zhou P., Huang Z., Xiao Y., Huang X., Fan X.-G. Protecting Chinese healthcare workers while combating the 2019 novel coronavirus. Infect. Control Hosp. Epidemiol. 2020;41:745–746. doi: 10.1017/ice.2020.60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Wang X., Zhang X., He J. Challenges to the system of reserve medical supplies for public health emergencies: reflections on the outbreak of the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) epidemic in China. Biosci. Trends. 2020;14:3–8. doi: 10.5582/bst.2020.01043. [DOI] [PubMed] [Google Scholar]
- 121.Holmes E.A., O’Connor R.C., Perry V.H., Tracey I., Wessely S., Arseneault L., Ballard C., Christensen H., Cohen Silver R., Everall I., Ford T., John A., Kabir T., King K., Madan I., Michie S., Przybylski A.K., Shafran R., Sweeney A., Worthman C.M., Yardley L., Cowan K., Cope C., Hotopf M., Bullmore E. Multidisciplinary research priorities for the COVID-19 pandemic: a call for action for mental health science. Lancet Psychiat. 2020;7:547–560. doi: 10.1016/S2215-0366(20)30168-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Javadi D., Feldhaus I., Mancuso A., Ghaffar A. Applying systems thinking to task shifting for mental health using lay providers: a review of the evidence. Glob. Ment. Health. 2017;4 doi: 10.1017/gmh.2017.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Lovibond P.F., Lovibond S.H. The structure of negative emotional states: comparison of the depression anxiety stress scales (DASS) with the beck depression and anxiety inventories. Behav. Res. Ther. 1995;33:335–343. doi: 10.1016/0005-7967(94)00075-u. [DOI] [PubMed] [Google Scholar]
- 124.Coker A.O., Coker O.O., Sanni D. Psychometric properties of the 21-item depression anxiety stress scale (DASS-21) Afr. Res. Rev. 2018;12:135–142. [Google Scholar]
- 125.Sarıçam H. 2018. The Psychometric Properties of Turkish Version of Depression Anxiety Stress Scale-21 (DASS-21) in Health Control and Clinical Samples, Depresyon Anksiyete Stres-21 Ölçeğinin (DASÖ-21) normal Ve Klinik Örneklemde Türkçe Versiyonun Psikometrik Özellikleri. [Google Scholar]
- 126.Crönlein T., Langguth B., Popp R., Lukesch H., Pieh C., Hajak G., Geisler P. Regensburg Insomnia Scale (RIS): a new short rating scale for the assessment of psychological symptoms and sleep in insomnia; Study design: development and validation of a new short self-rating scale in a sample of 218 patients suffering from insomnia and 94 healthy controls. Health Qual. Life Outcome. 2013;11:65. doi: 10.1186/1477-7525-11-65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Sadeghniiat-Haghighi K., Yazdi Z., Firoozeh M. Comparison of two assessment tools that measure insomnia: the insomnia severity Index and polysomnography. Indian J. Psychol. Med. 2014;36:54–57. doi: 10.4103/0253-7176.127251. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data included in article/supplementary material/referenced in article.