Version Changes
Revised. Amendments from Version 1
We have edited our manuscript as suggested by the reviewers. In the abstract section, we rectified the minor punctuation and grammatical errors that were present when we first submitted the manuscript. Similarly, we paraphrased a couple of sentences towards the end of abstract. We corrected the tenses of few sentences in the introduction section of the main text. Few redundant words and a sentence were removed and few words were added where necessary to add more meaning to the content. In the method section as well, redundant words and sentences were removed, rearrangement of words was necessary in some sentences and was done. Tenses, verb and voice (active/passive) of few sentences were modified as suggested by the reviewers. Similarly, minor punctuation and grammatical errors were corrected in the result and discussion sections along with paraphrasing of a sentence in the discussion section.
Abstract
Background
Good sleep quality is associated with a diverse range of positive outcomes such as better health, less daytime sleepiness, well-being and proper psychological functioning. Sleep deprivation or poor sleep quality leads to many metabolic, endocrine, and immune changes. Many studies have shown changes in sleep schedule along with worsening of sleep quality during the COVID-19 pandemic.
Methods
This cross-sectional study was conducted among students of a medical college in Kathmandu, Nepal from January 13, 2021 to February 15, 2021. A stratified random sampling technique was used. Data were collected using the Pittsburgh Sleep Quality Index (PSQI). Questionnaires that were completely filled were included and analyzed using STATA vs. 15.
Results
168(n=190) medical students filled out the questionnaires with a response rate of 88.42%. Around 30% (n=51) of respondents had poor sleep quality (PSQI total score of > 5) with an average PSQI score of 4.24±2.19. Unadjusted logistic regression analysis showed significantly higher odds of poor sleep quality among females (OR, 2.25; CI, 1.14-4.43) compared with male and the relation persists even after adjusting with age and year in medical school (aOR, 2.81; CI, 1.35-5.86). Adjusting with age and gender, 4 th-year MBBS students had 82% lesser odds of having poor sleep quality compared to 2 nd-year MBBS students (aOR, 0.18; CI, 0.04-0.76). Our study is suggestive of poor sleep quality common among medical students.
Conclusions
More than a quarter of medical students have a poor sleep quality as per our study. So, education and awareness should be raised among medical students regarding the detrimental effects of poor quality sleep on daily activities, physical and mental well-being, and the overall quality of life.
Keywords: COVID-19, Medical students, Nepal, Sleep, Sleep Deprivation
1. Introduction
The novel coronavirus (COVID-19) that first appeared in Wuhan has been spreading around the world. 1 The World Health Organization declared it a pandemic in March 2020. 2 The pandemic has brought not only fear of infection & death but also unbearable psychological pressure and disturbances. 3, 4 Good sleep quality is associated with a diverse range of positive outcomes such as better health, less daytime sleepiness, well-being, and proper psychological functioning. 5 Sleep deprivation or poor sleep quality leads to many metabolic, endocrine, and immune changes. 6 So, the importance of good quality sleep cannot be stressed enough.
Many studies have shown changes in sleep schedule along with worsening of sleep quality during the lockdown. 7 Findings regarding sleep duration and sleep quality are mixed during the COVID-19 pandemic. 7– 13 Most studies examining differences in sleep quality have shown poor sleep quality during the pandemic. 12– 16 Studies in different parts of the world showed that sleep quality has been poorer during lockdown period relative to the pre-lockdown period. 7, 10– 12, 14 When compared to pre-lockdown period, there has been a shift to a later bedtime and waking time, with a reduction in nighttime sleep and an increase in daytime napping during lockdown period. Also, there is evidence of greater sleep latency and poorer sleep efficiency during the pandemic. 13, 17 Especially, undergraduate medical students have poor sleep quality, internet addiction, and depression. 18– 20
Sufficient studies have not been done in Nepal regarding the sleep quality of medical students during the COVID-19 pandemic. A study on Nepalese college students has shown the poor sleep quality among the majority of students. 21 Higher prevalence of poor sleep quality among medical students as compared to other non-medical students and the general population has also been reported and several factors including medical students’ attitudes, knowledge of sleep, and academic demands have been identified as the causative factors. 22
This study aims to assess the impact of this enormous change caused by the COVID-19 pandemic on the sleep quality of medical students of a medical college in Nepal during the COVID-19 pandemic.
2. Methods
2.1 Study design and settings
This is a cross-sectional study done among the undergraduate medical students (first to the fourth year) of Nepalese Army Institute of Health Sciences (NAIHS), Kathmandu, Nepal from January 13, 2021, to February 15, 2021. The Institutional Review Committee (IRC) of Nepalese Army Institute of Health Sciences approved the study (Reference number: 374). At the time of data collection, all the participants were informed about the study and its objectives. Consent was taken from the participants by incorporating the consent form in the questionnaire itself. So, all the participants are understood to have given consent (details of questionnaire and consent form attached as extended data).
The study participants were not recruited as front-liners to tackle the COVID-19 pandemic during or before the study period. All of them were restricted in their homes during the lockdown period. None of the participants had been infected by COVID-19 up until the study period. Data was collected from the participants after receiving their consent, via Google forms sent out by email explaining the objective of the study in the form itself. The participation was voluntary and anonymity was assured to the participants. The participants didn’t receive any incentives.
2.2 Study sample
The sample size for the study was calculated using the Cochrane formula. Total students from 1st to 4th year in NAIHS are 423. The calculated sample size was 169. Considering and adding 10% as a non-response rate, the final sample size was 186. The questionnaire was emailed to 190 participants, among which only 168 responded giving a response rate of 88.42%. Detail of sample size calculation is as follows:
Sampling method: Stratified random sampling
Sample size: n = Z 2*p*q/e 2
= (1.96) 2*0.76*(1-0.76)/0.05 2
= 280.28
= 280
where,
n = calculated sample size
Z = 1.96 at 95% Confidence Interval
p = prevalence of poor sleep quality taken from previous study (76%)
q = 1-p
e = Margin of error (5%)
Total students from 1 st to 4 th year in NAIHS-COM (N) = 423
Adjusted sample size (n′) = n/ [1+ {(n − 1)/N}]
= 280/ [1+ {(280 − 1)/423}]
= 168.72
= 169
Considering and adding 10% as a non-response rate, our final sample size = 186.
Participants were selected using stratified random sampling in such a way that every student from first to fourth year had an equal chance of being selected. Firstly, a name list of students of the first to the fourth year was obtained from the administration of the institute, and each student was assigned a particular random number. An equal proportion of the male and female students from each year were selected for the study. Since the total number of students in each year was different, the total number of participants was different in each year. Then the study participants were selected randomly using the computer random number generator maintaining an equal proportion of students from each year and an equal proportion of males and females in each year [(first year: 45; female = 15, male = 30); (second year: 45; female = 13, male = 32); (third year: 50; female = 17, male = 33); (fourth year: 50; female = 15, male = 35)].
We emailed the questionnaire to the participants as everyone was at their homes because of the COVID-19 pandemic imposed lockdown.
2.3 Study instrument
We used the standard and validated Pittsburgh Sleep Quality Index (PSQI), which was developed by researchers at the University of Pittsburgh in 1988 AD. The questionnaire included baseline variables like age, sex, academic year, and questions addressing participants’ sleep habits and quality i.e. PSQI. The PSQI assesses the sleep quality during the previous month and contains 19 self-rated questions that yield seven components: subjective sleep quality, sleep latency, sleep duration, sleep efficiency, sleep disturbance, use of sleeping medications and daytime dysfunction. Each component was assigned a score that ranges from zero to three, yielding a PSQI score in a range that goes from 0 to 21. A total score of 0 to 4 is considered as normal sleep quality; whereas, scores greater than 4 are categorized as poor sleep quality. 23 The questionnaire was typed in the Google form and was sent via email to the randomly selected study participants.
2.4 Statistical methods
Data collected from students through the Google forms was extracted to Google sheets, cleaned in Excel, and then imported and analyzed using STATA software v.15. Simple descriptive analysis was performed to see the response for every PSQI variable. Then calculation performed following PSQI form administration instructions (attached in the extended data). Logistic regression analysis was done taking PSQI score-based category as the dependent variable and age, gender, and years in medical school as the independent variable. Poor sleep quality was the outcome of interest so logistic regression analysis was run for the occurrence of poor sleep quality to good sleep quality. Firstly, binary logistic regression analysis was run across the sleep quality to gender, age, and year in medical school to estimate the unadjusted odds ratio (OR). Then multiple logistic regression ran to estimate adjusted OR across the sleep quality to gender, age, and year in medical school. For logistic regression purposes, PSQI score-based sleep quality was labeled as zero for good sleep quality and one for poor sleep quality, and odds of occurrence of poor quality of sleep to good sleep quality estimated.
3. Results
Among the mailed 190 individuals from 1 st to 4 th year of a medical school, only 168 filled the Google form making the response rate of 88.42%. The majority (n = 108, 64.29%) were male with a mean age of 21.57 ± 1.52 years. A majority (n = 110, 65.48%) of students were staying single while the rest used to share their room. The average sleep hour in the last month was 7:27:20.09 ± 1:25:49.79 hour and sleep latency was 24.92 ± 25.97 minutes. 30.36% (n = 51) of respondents were having poor sleep quality (PSQI total score of > five) with an average PSQI score of 4.24 ± 2.19 ( Table 1).
Table 1. Participant’s basic details and sleep quality.
| Variables | Frequency | Percent | |
|---|---|---|---|
| Gender | Female | 60 | 35.71 |
| Male | 108 | 64.29 | |
| Age: Mean ± SD = 21.57 ± 1.52 (Median: 22, IQR: 20-23) | |||
| Medical school class | 1st year, MBBS | 39 | 23.21 |
| 2nd year, MBBS | 38 | 22.62 | |
| 3rd year, MBBS | 47 | 27.98 | |
| 4th year, MBBS | 44 | 26.19 | |
| Do you have a bed partner or roommate? | No bed partner or roommate | 110 | 65.48 |
| Partner in the same bed | 3 | 1.79 | |
| Partner in the same room, but not the same bed | 52 | 30.95 | |
| Partner/roommate in other room | 3 | 1.79 | |
| During the past month, hours of actual sleep (Mean ± SD): 7:27:20.09 ± 1:25:49.79 (Median: 7:30:00.00) | |||
| During the past month, sleep latency (in minutes) (Mean ± SD): 24.92 ± 25.97 (Median: 15.5) | |||
| PSQI total score (Mean ± SD): 4.24 ± 2.19 (Median:4) | |||
| PSQI category (sum score < 5 or > 5) | Good sleep quality | 117 | 69.64 |
| Poor sleep quality | 51 | 30.36 | |
Specific questions on trouble sleeping in last month showed 24(14.3%) were having trouble getting sleep within 30 minutes three or for more times a week. Similarly, 12(7.1%) mentioned they wake up in the middle of the night or early morning for three or more times a week. Majority i.e. 44% did not get up to use the bathroom during the past month. Likewise, only 1.2% and 1.8% had trouble sleeping because they could not breathe comfortably and coughed or snored loudly respectively for three or more times a week. When questioned if they had difficulty sleeping because of too cold or too hot feeling three or more times a week, 4.8% and 2.4% responded positively. The majority, 36.9%, and 75.6% did not have trouble sleeping because of bad dreams and of pain respectively during the last month. 98.8% of the participants did not have to take medicine to help him/her sleep during the last month. However, 1.2% had trouble staying awake while driving, eating meals, or engaging in social activities during the past month. Among those who had a roommate or bed partner, 6.9%, 1.7%, and 3.4% snored loudly, took long pause between breaths while asleep, and twitched or jerked legs while asleep respectively for three or more times a week during the past month whereas none of them had episodes of disorientation or confusion during sleep ( Table 2).
Table 2. Factors affecting sleep in last month at the time of response to the survey.
| PSQI scale based questionnaires | Less than once a week | Not during the past month | Once or twice a week | Three or more times a week | Total |
|---|---|---|---|---|---|
| 5. During the past month, how often have you had trouble sleeping because of you... | |||||
|
29(17.3%) | 77(45.8%) | 38(22.6%) | 24(14.3%) | 168(100.0%) |
|
48(28.6%) | 75(44.6%) | 33(19.6%) | 12(7.1%) | 168(100.0%) |
|
36(21.4%) | 74(44.0%) | 47(28.0%) | 11(6.5%) | 168(100.0%) |
|
19(11.3%) | 141(83.9%) | 6(3.6%) | 2(1.2%) | 168(100.0%) |
|
20(11.9%) | 139(82.7%) | 6(3.6%) | 3(1.8%) | 168(100.0%) |
|
41(24.4%) | 95(56.5%) | 24(14.3%) | 8(4.8%) | 168(100.0%) |
|
27(16.1%) | 127(75.6%) | 10(6.0%) | 4(2.4%) | 168(100.0%) |
|
60(35.7%) | 62(36.9%) | 31(18.5%) | 15(8.9%) | 168(100.0%) |
|
26(15.5%) | 127(75.6%) | 10(6.0%) | 5(3.0%) | 168(100.0%) |
| 7. During the past month, how often have you taken medicine to help you sleep (prescribed or "over the counter")? | 1(0.6%) | 166(98.8%) | 1(0.6%) | - | 168(100.0%) |
| 8. During the past month, how often have you had trouble staying awake while driving, eating meals, or engaging in the social activity? | 18(10.7%) | 130(77.4%) | 18(10.7%) | 2(1.2%) | 168(100.0%) |
| 10. If you have a roommate or bed partner, ask him/her how often in the past month you have had... | |||||
|
9(15.5%) | 42(72.4%) | 3(5.2%) | 4(6.9%) | 58(100.0%) |
|
5(8.6%) | 50(86.2%) | 2(3.4%) | 1(1.7%) | 58(100.0%) |
|
8(13.8%) | 41(70.7%) | 7(12.1%) | 2(3.4%) | 58(100.0%) |
|
4(6.9%) | 52(89.7%) | 2(3.4%) | - | 58(100.0%) |
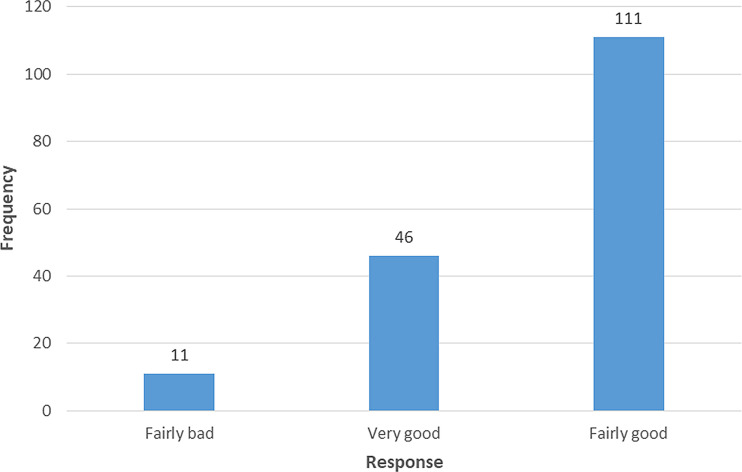
Among 168 respondents, 111(66.1%) responded to have a fairly good sleep quality when asked to rate their overall sleep quality in the last month ( Figure 1).
Figure 1. Response on “During the past month, how would you rate your sleep quality overall?”.
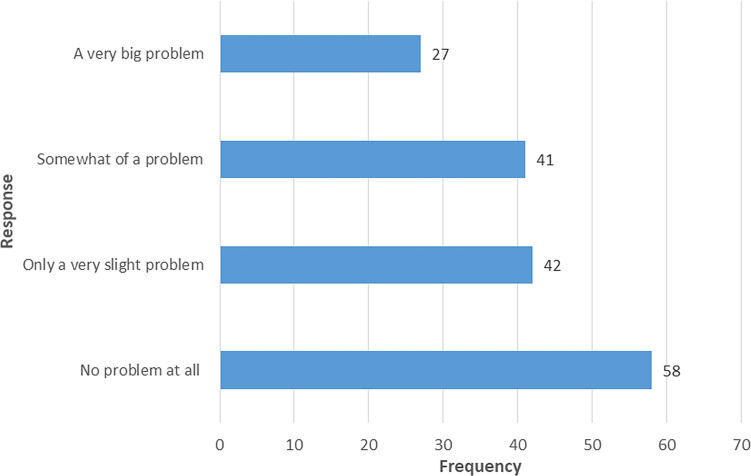
Fifty-eight (34.5%) responded no problem at all when asked for a problem to keep up enough enthusiasm to get things done during the past month, while 27 (16.1%) responded a very big problem ( Figure 2).
Figure 2. Response on “During the past month, how much of a problem has it been for you to keep up enough enthusiasm to get things done?”.
Unadjusted logistic regression analysis showed significantly higher odds of poor sleep quality among females (OR, 2.25; CI, 1.14-4.43) comparing to male and the relation persisted even adjusting with age and year in medical school (aOR, 2.81; CI, 1.35-5.86) ( Table 3). There was no significant difference in the sleep quality across years in medical school while running an unadjusted logistic regression analysis. But, adjusting with age and gender 4 th-year MBBS students had 82% lesser odds of having a poor quality of sleep compared with 2 nd-year MBBS students (aOR, 0.18; CI, 0.04-0.76) ( Table 3).
Table 3. Binary and multiple logistic regression taking age, gender, and years in medical school for PSQI score.
| Variables | Unadjusted | Adjusted | |||||||
|---|---|---|---|---|---|---|---|---|---|
| OR | [95% Conf. Interval] | p-value | OR | [95% Conf. Interval] | p-value | ||||
| Years in Medical school | 1st year, MBBS ® | ||||||||
| 2nd year, MBBS | 1.04 | .4043604 | 2.674842 | 0.935 | .7708897 | .2731356 | 2.175736 | 0.623 | |
| 3rd year, MBBS | 1.133333 | .4640643 | 2.767816 | 0.784 | .5756672 | .174416 | 1.900014 | 0.365 | |
| 4th year, MBBS | .4444445 | .1610749 | 1.226329 | 0.117 | .1766567 | .0412005 | .7574558 | 0.020* | |
| Age | .9777632 | .7871435 | 1.214545 | 0.839 | 1.361479 | .9609949 | 1.928861 | 0.083 | |
| Gender | Male ® | ||||||||
| Female | 2.252747 | 1.144979 | 4.432282 | 0.019* | 2.811422 | 1.348437 | 5.86167 | 0.006* | |
Note ®: Reference category, 95% Confidence interval, and 5% standard error considered with p-value or <0.05 as a level of significance. * Significant result. PSQI score based category for sleep was assigned as 0/1 [good quality of sleep (0) to poor quality of sleep (1)].
4. Discussion
The COVID-19 pandemic in 2020 has imposed a substantial effect on psychological, health, and social issues all over the world. Medical students, like everyone else, have also suffered from these issues. Medical education is based more on a practical approach rather than just a theoretical core. Therefore, classes shifting from the classroom to online platforms have, without any doubt, affected medical education more than anything else. However, the impact of the pandemic on the psychological well-being and sleep quality of medical students has not been assessed and addressed to a good extent in Nepal. Therefore, this study uses the PSQI to determine the sleep quality among the medical students of a medical college in Kathmandu, Nepal during the COVID-19 pandemic.
Our study showed that 30.36% of medical students had poor sleep quality (PSQI global score >5) but a study done just before the pandemic in the Nepalese medical students showed that 44.23% of students had poor sleep quality. 24 A study in India during the COVID-19 pandemic had 34.6% of medical students with poor sleep quality which was in line with the result of our study. 25 Previous studies from Pakistan on medical students in 2013 and Nepal on undergraduate students in 2015 showed 39.5% and 35.4% poor quality sleepers respectively. 19, 26 Our findings were in contrast to a study in China which showed a high prevalence of sleep disorders among adolescents and young adult students due to the stress and anxiety caused by the pandemic. 27 Previous studies in the Nepalese general population and health care workers found a low level of psychological distress due to the COVID-19 pandemic in Nepal which may explain better sleep quality among medical students in Nepal. 28, 29
One of the positive findings of this study is that none of the participants had to take medication to help them sleep whereas 10.2% of Saudi Arabian physicians used sleeping pills once or twice a week during the COVID-19 pandemic. 30 14.3% of our study participants had trouble falling asleep within 30 minutes thrice or more in a week, which was less compared to 24.7% in Saudi Arabian physicians during the COVID-19 pandemic. 30 Our study showed significantly higher odds of poor quality sleep among female students (OR, 2.25; CI, 1.14-4.43). A study on Pakistani medical students in 2013 also showed that females had poorer quality sleep i.e. 44% as compared to 32.8% male poor sleepers. 26 Similarly, Goweda RA et al. also found that sleep disorders were more common among female medical students based on a study done in Saudi Arabia during the COVID-19 pandemic. 31 Increased incidence of poor sleep quality among females is justifiable as sleep disorder symptoms are usually greater in women as compared to men. 28, 32 So, more focus should be shed upon female students when programs are formulated to improve the sleep quality among medical students. Sleep quality among students across years in medical school was not significantly different while running unadjusted logistic regression analysis in the case of our study. Studies from Brazil and Saudi Arabia assessed the sleep quality of first and second-year medical students to be poor as compared to other years. 30, 33 We found that the fourth-year medical students were less likely to have a poor sleep quality compared to second-year students which may be due to greater academic experience, and exposures during higher academic classes. In contrast, a previous study in China found that senior high school students had greater sleep problems due to increased academic burden and difficulty compared to junior school students. 27
Though our study shows less number of poor quality sleepers as compared to other studies discussed, 19, 24, 25 30.36% is still a big number. We cannot stay still and be satisfied based on the result of this study and the concerned authorities should try their best on bringing this number down to as minimum as possible. Because, poor quality sleep, without a doubt, will have a long-term impact on the mental well-being of the students. And no country would want future doctors who are not mentally healthy.
The number of students with poor sleep quality might decrease after the fear and restrictions because of COVID-19 subsides and life will return to normality. Alternatively, the number might go up, as the students return to their hectic schedules of classes, clinical postings, and a lot of studying. Since the scenario post-COVID is still unpredictable, frequent monitoring of sleep health and habits in medical students for raising awareness about sleep quality and problems should be planned and implemented.
Our study is not without limitations. We used a self-reporting questionnaire. Therefore, information bias is a major risk for this study. Our study was conducted among the students of a single institution. Therefore, the results might not be extrapolated to all the medical colleges of Nepal. Likewise, recall bias and subjectivity bias could have also affected the result of our study. Despite the limitations and biases, this study will surely provide a reference for further researches in this particular field.
5. Conclusions
Poor sleep quality is prevalent in 30.36% of medical students of a medical college in Nepal during the COVID-19 pandemic. Further studies have to be done to delve deeper into the sleep habits and problems of the medical students to determine the risk factors and causation of poor sleep quality. Furthermore, awareness should be raised about the importance of proper amount and sleep quality as well as detrimental effects of poor quality sleep on daily activities, physical and mental well-being, and the overall quality of life.
Data availability
Underlying data
Figshare. Sleep quality among undergraduate students of a medical college in Nepal during COVID-19 pandemic: an online survey. DOI: https://doi.org/10.6084/m9.figshare.14770182.v2. 34
This project contains the following underlying data:
-
-
We used the standard and validated Pittsburgh Sleep Quality Index (PSQI), which was developed by researchers at the University of Pittsburgh in 1988 AD. The questionnaire included baseline variables like age, sex, academic year, and questions addressing participants’ sleep habits and quality i.e. PSQI. The PSQI assesses the sleep quality during the previous month and contains 19 self-rated questions that yield seven components: subjective sleep quality sleep, latency, sleep duration, sleep efficiency and sleep disturbance, and daytime dysfunction. Each component is to be assigned a scored that ranges from zero to three, yielding a PSQI score in a range that goes from 0 to 21. A total score of 0 to 4 is considered as normal sleep quality; whereas, scores greater than 4 are categorized as poor sleep quality.
-
-
Data collected from students through the Google forms were extracted to Google sheets, cleaned in Excel, and then imported and analyzed using STATA 15. Simple descriptive analysis was performed to see the response for every PSQI variable. Then calculation performed following PSQI form administration instructions.
Data are available under the terms of the Creative Commons Zero “No rights reserved” data waiver (CC BY 4.0 Public domain dedication).
Extended data
Figshare. Sleep quality among undergraduate students of a medical college in Nepal during COVID-19 pandemic: an online survey. DOI: https://doi.org/10.6084/m9.figshare.14770182.v2. 34
Data are available under the terms of the Creative Commons Zero “No rights reserved” data waiver (CC BY 4.0 Public domain dedication).
Authors’ contributions
DBS, SPA, NR, PB, SP, YA, PR, and UR contributed to the concept and design, methodology, and data collection. DBS contributed to the analysis, and interpretation of data. DBS, PB, SP, YA, PR, and UR contributed to the literature search, and initial manuscript drafting. SPA, NR involved in the revision and intellectual interpretation of the manuscript.
All authors were involved in drafting and revising the manuscript and approved the final version.
Acknowledgments
We would like to thank all the participants in this research for their voluntary participation.
Funding Statement
The author(s) declared that no grants were involved in supporting this work.
[version 2; peer review: 2 approved]
References
- 1. WHO|Novel Coronavirus – China: WHO [Internet]. 2020 [cited 2021 May 18]. http://www.who.int/csr/don/12-january-2020-novel-coronavirus-china/en/
- 2. WHO Director-General’s opening remarks at the media briefing on COVID-19-11 March 2020 [Internet]. [cited 2021 May 18]. Reference Source
- 3. Cao W, Fang Z, Hou G, et al. : The psychological impact of the COVID-19 epidemic on college students in China. Psychiatry Res. 2020 May 1;287:112934. 10.1016/j.psychres.2020.112934 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Luo M, Guo L, Yu M, et al. : The psychological and mental impact of coronavirus disease 2019 (COVID-19) on medical staff and general public – A systematic review and meta-analysis. Psychiatry Res. Elsevier Ireland Ltd;2020;291: p.113190. 10.1016/j.psychres.2020.113190 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Harvey AG, Stinson K, Whitaker KL, et al. : The subjective meaning of sleep quality: A comparison of individuals with and without insomnia. Sleep. 2008 Mar 1 [cited 2021 May 18];31(3):383–393. 10.1093/sleep/31.3.383 Reference Source [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. AlDabal L: Metabolic, Endocrine, and Immune Consequences of Sleep Deprivation. Open Respir Med J. 2011 Jun 30;5(1):31–43. 10.2174/1874306401105010031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Cellini N, Canale N, Mioni G, et al. : Changes in sleep pattern, sense of time and digital media use during COVID-19 lockdown in Italy. J Sleep Res. 2020 Aug 1 [cited 2021 May 18];29(4):e13074. 10.1111/jsr.13074 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. yu LL, Wang J, yong O-y X, et al. : The immediate impact of the 2019 novel coronavirus (COVID-19) outbreak on subjective sleep status. Sleep Med. 2021 Jan;77:348–54. 10.1016/j.sleep.2020.05.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Wright KP, Linton SK, Withrow D, et al. : Sleep in university students prior to and during COVID-19 Stay-at-Home orders. Curr Biol. Cell Press;2020;30: p.R797–8. 10.1016/j.cub.2020.06.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Coiro MJ, Asraf K, Tzischinsky O, et al. : Sleep quality and COVID-19-related stress in relation to mental health symptoms among Israeli and U.S. adults. Sleep Heal. 2021 Apr;7(2):127–33. 10.1016/j.sleh.2021.02.006 [DOI] [PubMed] [Google Scholar]
- 11. Blume C, Schmidt MH, Cajochen C: Effects of the COVID-19 lockdown on human sleep and rest-activity rhythms. Curr Biol. Cell Press;2020;30: p.R795–7. 10.1016/j.cub.2020.06.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Marelli S, Castelnuovo A, Somma A, et al. : Impact of COVID-19 lockdown on sleep quality in university students and administration staff. J Neurol. 2021 Jan;268(1):8–15. 10.1007/s00415-020-10056-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Gupta R, Grover S, Basu A, et al. : Changes in sleep pattern and sleep quality during COVID-19 lockdown. Indian J Psychiatry. 2020 Jul;62(4):370–8. 10.4103/psychiatry.IndianJPsychiatry_523_20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Casagrande M, Favieri F, Tambelli R, et al. : The enemy who sealed the world: effects quarantine due to the COVID-19 on sleep quality, anxiety, and psychological distress in the Italian population. Sleep Med. 2020 Nov;75:12–20. 10.1016/j.sleep.2020.05.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Cellini N, Conte F, De Rosa O, et al. : Changes in sleep timing and subjective sleep quality during the COVID-19 lockdown in Italy and Belgium: age, gender and working status as modulating factors. Sleep Med. 2021 Jan;77:112–9. 10.1016/j.sleep.2020.11.027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Gao C, Scullin MK: Sleep health early in the coronavirus disease 2019 (COVID-19) outbreak in the United States: integrating longitudinal, cross-sectional, and retrospective recall data. Sleep Med. 2020 Sep;73:1–10. 10.1016/j.sleep.2020.06.032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Benham G: Stress and sleep in college students prior to and during the COVID-19 pandemic. Stress Heal. 2020. 10.1002/smi.3016 [DOI] [PubMed] [Google Scholar]
- 18. Attal BA, Bezdan M, Abdulqader A: Sleep Quality and Its Correlates among Yemeni Medical Students: A Cross-Sectional Study. Sleep Disord. 2021 Jan;2021:1–10. 10.1155/2021/8887870 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Bhandari PM, Neupane D, Rijal S, et al. : Sleep quality, internet addiction and depressive symptoms among undergraduate students in Nepal. BMC Psychiatry. 2017 Mar 21 [cited 2021 May 18];17(1):1–8. 10.1186/s12888-017-1275-5 Reference Source [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Aylie NS, Mekonen MA, Mekuria RM: The psychological impacts of COVID-19 pandemic among university students in bench-sheko zone, South-West Ethiopia: A community-based cross-sectional study. Psychol Res Behav Manag. 2020 Sep 30 [cited 2021 May 18];13:813–21. 10.2147/PRBM.S275593 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Khadka R, Bista S, Baskota S, et al. : Sleep Quality among College Students in Kathmandu Valley, Nepal. Nepal Med J. 2019 Dec;2(2):1–4. 10.37080/nmj.61 [DOI] [Google Scholar]
- 22. Azad MC, Fraser K, Rumana N, et al. : Sleep disturbances among medical students: A global perspective. J Clin Sleep Med. American Academy of Sleep Medicine;2015;11: p.69–74. 10.5664/jcsm.4370 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Buysse DJ, Reynolds CF, Monk TH, et al. : The Pittsburgh sleep quality index: A new instrument for psychiatric practice and research. Psychiatry Res. 1989 May 1;28(2):193–213. 10.1016/0165-1781(89)90047-4 [DOI] [PubMed] [Google Scholar]
- 24. Sundas N, Ghimire S, Bhusal S, et al. : Sleep quality among medical students of a tertiary care hospital: A descriptive cross-sectional study. J Nepal Med Assoc. 2020 Feb 29 [cited 2021 May 18];58(222):76–9. 10.31729/jnma.4813 Reference Source [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Saraswathi I, Saikarthik J, Kumar KS, et al. : Impact of COVID-19 outbreak on the mental health status of undergraduate medical students in a COVID-19 treating medical college: A prospective longitudinal study. PeerJ. 2020 Oct 16 [cited 2021 May 18];8. 10.7717/peerj.10164 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Surani AA, Zahid S, Surani A, et al. : Sleep quality among medical students of Karachi. Pak. J Pak Med Assoc. 2015 Apr;65(4):380–2. [PubMed] [Google Scholar]
- 27. Zhou SJ, Wang LL, Yang R, et al. : Sleep problems among Chinese adolescents and young adults during the coronavirus-2019 pandemic. Sleep Med. 2020 Oct 1 [cited 2021 Feb 20];74:39–47. 10.1016/j.sleep.2020.06.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Shrestha DB, Thapa BB, Katuwal N, et al. : Psychological distress in Nepalese residents during COVID-19 pandemic: A community level survey. BMC Psychiatry. BioMed Central Ltd;2020 [cited 2021 Feb 20]:20. 10.1186/s12888-020-02904-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Kafle K, Shrestha DB, Baniya A, et al. : Psychological distress among health service providers during COVID-19 pandemic in Nepal. PLoS One. 2021 Feb 1 [cited 2021 May 18];16(2 February):e0246784. 10.1371/journal.pone.0246784 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Alnofaiey YH, Alshehri HA, Alosaimi MM, et al. : Sleep disturbances among physicians during COVID-19 pandemic. BMC Res Notes. 2020 Dec 1 [cited 2021 May 18];13(1):1–7. 10.1186/s13104-020-05341-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Goweda RA, Hassan-Hussein A, Alqahtani MA, et al. : Prevalence of sleep disorders among medical students of Umm Al-Qura University, Makkah, Kingdom of Saudi Arabia. J Public health Res. 2020 [cited 2021 May 18];9(S1):45–9. 10.4081/jphr.2020.1921 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Klink M, Quan SF: Prevalence of reported sleep disturbances in a general adult population and their relationship to obstructive airways diseases. Chest. 1987 Apr 1 [cited 2021 May 18];91(4):540–6. 10.1378/chest.91.4.540 Reference Source [DOI] [PubMed] [Google Scholar]
- 33. de C CC, de Oliveira FK, Pizzamiglio DS, et al. : Qualidade de sono em estudantes de medicina: Comparação das diferentes fases do curso. J Bras Pneumol. 2017 Jul 1 [cited 2021 May 18];43(4):285–9. 10.1590/S1806-37562016000000178 [DOI] [Google Scholar]
- 34. Shrestha D, Adhikari SP, Rawal N: Sleep quality among undergraduate students of a medical college in Nepal during COVID-19 pandemic: an online survey. figshare. Online resource. 2021. 10.6084/m9.figshare.14770182.v2 [DOI] [PMC free article] [PubMed]